#medical diagnosis software
Text
Medical Diagnosis Software: Enhancing Healthcare Decision-Making
Medical diagnosis software refers to advanced technological tools designed to assist healthcare professionals in diagnosing diseases and conditions accurately and efficiently. These software solutions utilize sophisticated algorithms, artificial intelligence (AI), and large databases of medical knowledge to analyze patient data comprehensively.
Key Features and Functions:
Data Integration and Analysis: Medical diagnostics software integrates and analyzes diverse patient data sources such as symptoms, medical history, laboratory results, and medical imaging. By processing this data, the software identifies patterns, correlations, and anomalies that aid in generating potential diagnoses.
Decision Support: One of the primary functions of medical diagnosis software is to provide decision support to healthcare providers. Through AI-driven algorithms, these tools suggest differential diagnoses, recommend appropriate tests or procedures, and assist in interpreting complex medical data to guide clinical decision-making.
Automation and Efficiency: By automating data analysis and interpretation tasks, medical diagnosis software improves diagnostic efficiency and reduces the time required for diagnosis. This automation also helps in minimizing errors and variability in diagnostic processes.
Personalized Medicine: Some advanced medical diagnosic software platforms support personalized medicine approaches by considering individual patient characteristics, genetic information, and treatment responses. This customization enhances the accuracy and effectiveness of diagnostic recommendations and treatment plans tailored to each patient's unique needs.
Integration with Healthcare Systems: Medical diagnosis software integrates seamlessly with electronic health records (EHRs), laboratory information systems (LIS), and other healthcare IT infrastructure. This integration ensures that healthcare providers have access to up-to-date patient information and facilitates collaborative decision-making across care teams.
Security and Compliance: Given the sensitivity of medical data, medical diagnosis software adheres to stringent security protocols and regulatory compliance standards (e.g., HIPAA in the United States). Robust encryption, access controls, and data anonymization techniques safeguard patient information from unauthorized access or breaches.
In conclusion, medical diagnosis software plays a crucial role in modern healthcare by augmenting the diagnostic capabilities of healthcare professionals with advanced technology and data analytics. By leveraging AI and comprehensive data analysis, these tools contribute to more accurate diagnoses, personalized treatment plans, and improved patient outcomes, ultimately advancing the quality and efficiency of healthcare delivery.
#medical diagnosis software#medical diagnostic software#medical diagnostic#medical diagnostic solutions#medical diagnostic software solutions
0 notes
Text
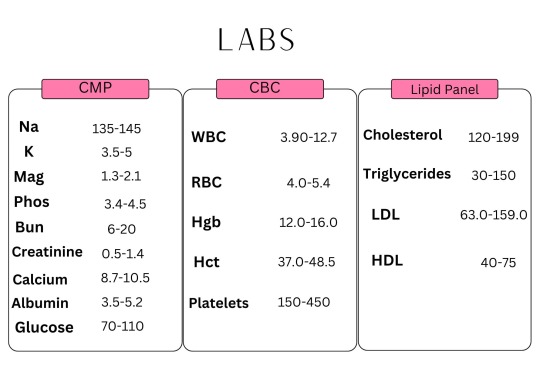
#icunurse#nursing school#nursing#etsy#icucare#hospital#icu#health and wellness#healthcare#diagnosis#diagnostic management software#medblr#patientcare#patientsafety#medical care#bloodwork#labs#note cards#reference#nursing studyblr#nursing student
5 notes
·
View notes
Text
Slimming Success: My Positive Experience with
There are a lot of weight-loss supplements out there, and many promise the world but deliver little. I've been on my weight-loss journey for a while now, and I've tried a fair few products with mixed results. That's why I'm so excited to share my positive experience with .Feeling Fuller for Longe
One of the biggest struggles I had with weight loss was managing hunger pangs. I'd constantly feel like reaching for snacks, and it was hard to stick to a calorie deficit. Since incorporating [Product Name] into my routine, I've noticed a significant difference in my appetite. The supplement helps me feel fuller for longer, which means I'm less likely to overeat throughout the day.Increased Energy LevelsAnother fantastic benefit of [Product Name] is the boost it's given my energy levels. In the past, feeling sluggish and tired was a common obstacle during weight loss. However, [Product Name] seems to have helped improve my metabolism, leaving me feeling more energized throughout the day. This newfound energy has not only aided my workouts but also improved my overall well-being.Aiding My Weight Loss GoalsWhile [Product Name] isn't a magic bullet, it's definitely become a valuable tool in my weight-loss journey. Combined with a healthy diet and regular exercise, I've seen consistent progress on the scales. The feeling of my clothes fitting looser and having more energy is truly motivating.Overall, I'm incredibly happy with the positive impact [Product Name] has had on my weight-loss efforts. If you're looking for a supplement to support your weight-loss goals, I highly recommend giving it a try.Disclaimer: It's important to consult with your doctor before starting any new supplement, especially if you have any underlying health conditions.
#healthyfood#Etactics | Revenue Cycle Software#The Best Health Hashtags to Use on Each Platform (More Than 55!)#Maria Clark August 6#2020#HealthHashtag_820.jpg#If your medical practice is on social media#it’s most likely because you want to interact with more patients and audiences. These platforms make it so much easier to reach more people#especially if they’re looking for self-diagnosis answers.#But there are intentional ways to categorize your account’s content so that it’s associated with the healthcare space. A common tool for do#HealthHashtag_ExpandAudience_820.png#Hashtags are words and phrases preceded by the hash sign (#). They revolutionized the social media space and grew so popular that they changed the name of the pound sign#think about that.#They identify related content posts. That way#users can search for a particular hashtag in what they’re interested in and find all posts that used that tag. Alternatively#they can click on a hashtag within a post and it will take them to the page of posts.#This helps users find similar content to what they’re viewing. It makes it much easier to expand your audience so more people learn about y#leading to more traffic to your page.#So now that you understand what this tool is#what are the best ones to include in healthcare practice’s posts? You’ll definitely want to use them considering that posts that include at#You don’t need to look too hard#because we’ve done the work for you. Here are some of the most popular health hashtags on each platform to get you more traffic.#Table of Contents#Instagram#TikTok#LinkedIn#Twitter#Conclusion#Most Popular:
0 notes
Text
How To Use FT500 Sniper Bot To Make Money On Friend.Tech $FTD
How To Use FT500 Sniper Bot To Make Money On Friend.Tech $FTD
How To Use FT500 Sniper Bot To Make Money On Friend.Tech $FTD
https://ifttt.com/images/no_image_card.png https://www.youtube.com/watch?v=M1xWKTWZy48
https://ifttt.com/images/no_image_card.png https://cryptoncars.wordpress.com/2023/09/10/how-to-use-ft500-sniper-bot-to-make-money-on-friend-tech-ftd/
View On WordPress
#billing#classification#clinics#coding#diagnosis#healthcare#hospitals#insurance#Medical#physician#reimbursement#software#specialists
0 notes
Text
Comparing Final Expense Insurance Policies
Comparing Final Expense Insurance Policies
Comparing Final Expense Insurance Policies
Comparing Final Expense Insurance Policies
The burial insurance, known as final expense insurance, the market is set to increase by 3.6% by 2030.
This shows that more people are becoming concerned with having their end-of-life insurance in place. Then, the process can become less stressful for family members who are left behind.
Burial insurance covers…
View On WordPress
#billing#classification#clinics#coding#diagnosis#healthcare#hospitals#insurance#Medical#physician#reimbursement#software#specialists
0 notes
Text
Claudia, one of your friends, invited you to attend to her beach volley match. The match is held indoor so, given the fact that its summer and in this country summer is also very humid, temperatures are going to be torrid. Beside this fact you're still quite surprised to see that the majority of the players are playing naked, females too (in this parallel univers human are not ashamed by their own bodies). After all sweating is the best way to cool down. She's quite skinny but look really good with that blue bikini, you always liked her so, secretely, you're very happy to see her playing covered just with air.
Given the fact that the playground is going to be free the whole day, organizers decided to complete the tournament without skippying to next day.
Some hours have passed and she has played for a lot of time now. Room temperature went higher than 36°C for the whole last matches and now Claudia looks pretty torn. She's always been a warrior, someone who don't surrender easily but all that jumping in this particular condition had an effect on her too. She's covered by sweat, her skin has assumed a reddish tone and her panting has become so deep anyone can clearly hear her fast inspirations and exales. The thing that tunrs on a light in your mind though is the fact that her entire upper body is rhythmically shaking like it's thrusted by a sort of internal earthquake. You suddenly realize that you recently activated a medical app on your phone developped at the laboratory where you work that makes possible medical analises through the phone camera thanks to experimental sensors placed in the camera.
You activate the app and feel pretty lifted up by the fact you already added her profile. A thin ensamble of laser rays, almost invisible, is projeced towards her and the selected target orgal (obviously Claudia's heart) becomes visible on the screen.
Her heart is beating like crazy, not only considering the pace but also the strenght of each beat, the app says her heart is beating at around 195 bpm but it's probably even higher. It's something that is completely out of any safety zone for someone who is 34 years old... and not even a younger person should push its heart like this. The device can also work as a digital stethoscope and by wearing headphones to listen to her you remained schoked. Her blood is pushed so violently that it's making strange wooshing-like noises by rubbing against her heart internal structures, sounds that almost cover up her slamming valves.
Suddenly the software gives a diagnosis: High cardiac risk- probability of a sudden cardiac arrest of 89%-potentially lethal arrhythias occurring. By looking at her detected heart electrical activities, her organ is so over-stimulated that PVCs and VTACs burst are already present.
You know exactly what to do, Claudia's life has an 89% probability to end in the next few minutes and it's increasing.
You decide to get up from your seat and run towards the referee to show him the analysis of your device. One of the players' heart is going to stop very soon.
A second before you move, on the ecg a strange beat appears and suddenly Claudia's heart interrupts any activity, it doesn't even fibrillate, it just ceases to beat as silence arises from your headphones. Terrified you see her taking a couple of deep breath, the ball she was holding fell on the ground and her left hand is placed in between her bare breasts... after a moment she collapses on the ground.
You have always wanted to place your hand on her chest to feel her heartbeat but now you have to do this to make it beat again. CPR has to be started immediately.
121 notes
·
View notes
Text
Getting past ‘it’s IBS’ (Xi Chen, Aeon, June 04 2024)
"In the late 1980s, aged 12, Taryn was taken to her doctor’s office with cramping, bloating, and constipation after eating, and was told that she had ‘a nervous stomach’.
As a white girl growing up in New Jersey, she met a stereotype, and when initial bloodwork and imaging was negative for evidence of a ‘real’, or organic disease in her gut, one of Taryn’s doctors began writing in her charts that she had irritable bowel syndrome (IBS), a misdiagnosis that would follow Taryn for life.
At the time, IBS was considered by many to be a medically unexplained and therefore controversial illness, keeping company with conditions such as fibromyalgia and chronic fatigue syndrome.
As a result, it carried the stigma of being a psychosomatic illness, caused primarily by stress and anxiety, and Taryn was sent home with prescriptions for diet and exercise. (…)
Today, unlike in the 1990s, it is well established that conditions like IBS, collectively known as disorders of gut-brain interaction (DGBIs), are real diseases that disrupt the communication between the nervous system of the brain and spine, and the nervous system of the intestines.
First mentioned in the book The Irritable Gut (1979) by the gastroenterologist W Grant Thompson, the conditions were labelled ‘functional’ disorders – characterised not by structural damage to the hardware of the gut, but by a glitch in its ‘software’, in other words, its nervous system, charged with processing, receiving or relaying information coming in or going out.
Software is not as easily observed as hardware, however, and much of academic medicine views the mind and the body as two separate and distinct entities, a viewpoint called mind-body dualism.
Over time, and despite the more nuanced meaning intended by Thompson, the term ‘functional’ became associated exclusively with disorders of the mind.
This is part of the reason why there is still stigma against conditions like IBS, and why attempts to establish diagnostic criteria for IBS in particular suffered from vagueness. (…)
When academics read that IBS patients have higher rates of anxiety and depression, or that antidepressants are a treatment for IBS, many assume that this is because psychiatric symptoms cause symptoms of IBS without considering the inverse, that chronic undiagnosed abdominal pain predisposes patients to having mood disorders.
The real reason these drugs are effective, however, is that, in utero, the precursor cells for our gut and our brain actually share the same nervous system, and only later separate in embryonic development.
As a result, the two nervous systems utilise the same neurotransmitters, such as serotonin, to send messages between neurons.
This is why we sometimes feel butterflies in our stomach when we’re nervous, and why stress and anxiety often worsen symptoms of IBS, but do not necessarily cause it.
As Brown’s quote above implies, the stereotype of the anxious patient in pain applies not only to IBS but all patients who present to clinics with vague abdominal distress (including those with non-gastrointestinal conditions like endometriosis, who experience delayed diagnosis because providers take women’s pain less seriously than men’s).
A classic example is peptic ulcer disease, a cause of severe abdominal pain that for decades was denounced as a psychosomatic illness until Barry Marshall and Robin Warren discovered in 1983 that it was caused by a species of bacteria.
Before their findings, peptic ulcers were managed with diet and, frequently, surgery, when what patients needed were antibiotics. (…)
In my opinion, the root of the problem is medical education itself.
Unless a medical trainee becomes a gastroenterologist, it is unlikely that they will receive any specialised education in IBS, let alone the history of IBS research proving it to be an organic condition, despite 40 per cent of the general population having functional gastrointestinal disorders.
Partly, this is because a majority of medical education in countries including the US, the UK and Canada takes place in academic centres associated with hospitals, where medical students will probably never encounter a patient for whom their IBS symptoms are the primary reason for them appearing in the emergency room, and especially not for their admission to the hospital itself.
As a consequence, medical students also don’t get their knowledge of IBS tested by board examinations.
This speaks to the fact that, echoing Osler, IBS generally doesn’t kill patients, and our current healthcare system values measures of mortality and cure in response to acute complaints more than quality of life and the management of suffering from chronic issues such as IBS.
The same could be said about long COVID (which, to this day, is sometimes challenged as illegitimate) and chronic fatigue syndrome, where sufferers are often sent off to a psychiatrist for care.
The thinking is that these ongoing problems, where there is no mainstream route for testing and treatment, are not as important for medical students to know about compared with, say, a patient crashing after a cardiac arrest, even though most of the global disease burden across the developed and the developing world is caused by chronic, not acute, illness. (…)
These demographic patterns don’t explain who really has the disease – they just reveal medical and social bias and entrenched stereotypes: women are perceived as hysterical and diagnosis-seeking, while men are stoic and avoidant, for instance; or white women are thought to tolerate less pain than people of colour.
None of this, in reality, is true – but it is part of the reason why so many patients assume that what they suffer from won’t be justified by the presence of organic disease and therefore doesn’t warrant a doctor’s visit in the first place.
Such patients, treated so poorly within the medical mainstream, now have a community and identity of their own in the Wild West of alternative medicine that flourishes online.
Such groups, seeking to empower themselves and especially hoping to get well, today stand at loggerheads with the practices and physicians they have left behind.
Some accuse their former doctors of gaslighting them, and they deserve to be heard.
Much of what I have discussed regarding misdiagnoses of IBS assumes that healthcare providers, even when in error, always have good intentions and are sincere about using the diagnosis to clarify the patient’s medical case.
There were several elements of Taryn’s story, however, and in my own experiences of how DGBIs are taught in medical school, that make it difficult for me to believe that this assumption holds in most doctor visits.
Although one could argue that the blasé diagnoses of IBS and disordered eating for Taryn could be down to simple carelessness and negligence, honest errors, or someone being ‘just a bad doctor’, it’s obvious to me that a pattern was developing with Taryn’s interactions with different providers who weren’t taking her lived experience itself seriously, just as I had stopped taking my own experiences seriously.
What holds our stories together, I believe, is this phenomenon where both of our perceptions of our own ability to know what’s true or not were put into question."
11 notes
·
View notes
Text
17 // diagnostic (extra credit)

Welcome to SelfMed, your online personal medical evaluation assistant! If this is a medical emergency, please contact local authorities or Trauma Team for immediate help.
How can SelfMed assist you today?
>> diagnosis
Please list up to five major symptoms for a diagnosis using our QuickMatch™ technology.
[1] fever
[2] headache
[3] mania
[4] hallucinations
[5] not recognizing faces
———
QuickMatch™ Potential Diagnoses*
The symptoms listed are a complete or partial match to the diseases and disorders below:
Click for more information and recommended treatment options.
Schizophrenia [+]
Post-Traumatic Stress Disorder (PTSD) [+]
Cyberpsychosis [–]
Cyberpsychosis is a collective term for all psychotic and anxiety-related personality disorders caused by hardware implanted in the body and any and all behavioral mods, including software. Often this begins as changes to the personality, followed by increasingly erratic and even violent behavior. Some medications and substance abuse can worsen these behaviors.
Recommended treatment options:
- Therapy
- Implant deactivation and/or removal
- Bethaloperidol
While antipsychotics are widely used to slow the onset of cyberpsychosis, therapy has also proven effective for some patients after years of treatment. Those experiencing aggressive cyberpsychotic symptoms such as violent outbursts should be kept away from public spaces and denied access to weapons until they can be incapacitated, restrained, and removed for treatment.
If you or someone you know is experiencing symptoms of cyberpsychosis that result in erratic or violent behavior, remove yourself from any potentially dangerous situations and call MaxTac. Do NOT interrupt MaxTac officers during an ongoing violent situation. DO put as many walls between the situation and yourself as is possible to avoid stray projectiles and bodily harm.
*QuickMatch™ diagnoses are a quick-screening technology and should not be used to replace the services of a trained medical professional.
———
Your free trial SelfMed membership is valid for the next [7 DAYS].
By upgrading to a premium membership, you can access an additional seven diagnoses. Would you like to upgrade to a SelfMed premium membership today? (€$199 per mo.)
Enter promo code HEALTH10NOW for a limited time offer of 10% your first month of premium service!
———
Is there something else SelfMed can assist with?
>> nethaloperidol
We’re sorry, but we didn’t recognize that prompt.
Is there something else SelfMed can assist with?
>> bethaloperidol
Searching “bethaloperidol” yielded the following articles:
Bethaloperidol [–]
Bethaloperidol is an antipsychotic used to treat a broad range of disorders, ranging from Schizophrenia to hyperactivity. When prescribed by a doctor in combination with therapy, bethaloperidol has been proven effective in helping patients recover. Bethaloperidol can be taken in pill form or through injection. The most widely used brands are Bethal and Novadol.
Though black market bethaloperidol is frequently sold, it is not created in a lab environment where product quality is overseen, it is likely a cheaper alternative that will not address symptoms adequately, and/or it has been cut with other drugs that could be a potentially dangerous cocktail. Brand names are always recommended and more effective than their black market counterparts.
———
Searching for the nearest retailer that carries BETHALOPERIDOL? We’ve found 10 locations near you, less than 5 minutes away!
Upgrade to a premium membership to find trusted pharmaceutical outlets near you. (€$199 per mo.)
Enter promo code HEALTH10NOW for a limited time offer of 10% your first month of premium service!
———
Is there something else SelfMed can assist with?
>> ripperdoc
Searching “ripperdoc” yielded the following articles:
Ripperdocs: the new GP or back alley surgeon? [+]
Top 10 most horrifying ripperdoc patient stories [+]
Confessions of a street doctor: ripper reveals all [+]
Is there something else SelfMed can assist with?
>> nearest ripperdoc
We’re sorry, but we didn’t recognize that prompt.
Is there something else SelfMed can assist with?
>> fuck off
———
Thank you for using SelfMed!
Your feedback matters! Please rate your experience.
☆☆☆☆☆
#ffxivwrite2023#[ ffxivwrite2023 ]#[ cyberpunk ]#sunday is au day#sometimes writing cyberpunk means exercising the corporate copywriter in me for cynical purposes
15 notes
·
View notes
Text
Jazmin Evans had been waiting for a new kidney for four years when her hospital revealed shocking news: She should have been put on the transplant list in 2015 instead of 2019 — and a racially biased organ test was to blame.
As upsetting as that notification was, it also was part of an unprecedented move to mitigate the racial inequity. Evans is among more than 14,000 Black kidney transplant candidates so far given credit for lost waiting time, moving them up the priority list for their transplant.
“I remember just reading that letter over and over again,” said Evans, 29, of Philadelphia, who shared the notice in a TikTok video to educate other patients. “How could this happen?”
At issue is a once widely used test that overestimated how well Black people’s kidneys were functioning, making them look healthier than they really were — all because of an automated formula that calculated results for Black and non-Black patients differently. That race-based equation could delay diagnosis of organ failure and evaluation for a transplant, exacerbating other disparities that already make Black patients more at risk of needing a new kidney but less likely to get one.
A few years ago, the National Kidney Foundation and American Society of Nephrology prodded laboratories to switch to race-free equations in calculating kidney function. Then the U.S. organ transplant network ordered hospitals to use only race-neutral test results in adding new patients to the kidney waiting list.
“The immediate question came up: What about the people on the list right now? You can’t just leave them behind,” said Dr. Martha Pavlakis of Boston’s Beth Israel Deaconess Medical Center and former chair of the network’s kidney committee.
Pavlakis calls what happened next an attempt at restorative justice: The transplant network gave hospitals a year to uncover which Black kidney candidates could have qualified for a new kidney sooner if not for the race-based test — and adjust their waiting time to make up for it. That lookback continues for each newly listed Black patient to see if they, too, should have been referred sooner.
Between January 2023 and mid-March, more than 14,300 Black kidney transplant candidates have had their wait times modified, by an average of two years, according to the United Network for Organ Sharing, which runs the transplant system. So far more than 2,800 of them, including Evans, have received a transplant.
But it’s just one example of a larger problem permeating health care. Numerous formulas or “algorithms” used in medical decisions — treatment guidelines, diagnostic tests, risk calculators — adjust the answers according to race or ethnicity in a way that puts people of color at disadvantage.
Given how embedded these equations are in medical software and electronic records, even doctors may not realize how widely they impact care decisions.
“Health equity scholars have been raising alarm bells about the way race has been misused in clinical algorithms for decades,” said Dr. Michelle Morse, New York City’s chief medical officer.
Change is beginning, slowly. No longer are obstetricians supposed to include race in determining the risk of a pregnant woman attempting vaginal birth after a prior C-section. The American Heart Association just removed race from a commonly used calculator of people’s heart disease risk. The American Thoracic Society has urged replacing race-based lung function evaluation.
The kidney saga is unique because of the effort to remedy a past wrong.
“Lots of time when we see health inequities, we just assume there’s nothing we can do about it,” Morse said. “We can make changes to restore faith in the health system and to actually address the unfair and avoidable outcomes that Black people and other people of color face.”
Black Americans are over three times more likely than white people to experience kidney failure. Of the roughly 89,000 people currently on the waiting list for a new kidney, about 30% are Black.
Race isn’t a biological factor like age, sex or weight — it’s a social construct. So how did it make its way into calculations of kidney function?
The eGFR, or estimated glomerular filtration rate, evaluates kidney health based on how quickly a waste compound called creatinine gets filtered from blood. In 1999, an equation used to calculate eGFR was modified to adjust Black people’s results compared to everyone else’s, based on some studies with small numbers of Black patients and a long-ago false theory about differences in creatinine levels. Until recently that meant many lab reports would list two results — one calculated for non-Black patients and another for Black patients that could overestimate kidney function by as much as 16%.
Not every Black kidney candidate was affected. Some may have had kidney failure diagnosed without that test. For others to have a chance at benefitting from UNOS’ mandated lookback, transplant center staff-turned-detectives often worked after hours and weekends, hunting years-old records for a test that, recalculated without the race adjustment, might make the difference.
“You’re reaching out to the nephrologist, their primary care doctors, the dialysis units to get those records,” said Dr. Pooja Singh of Jefferson Health’s transplant institute in Philadelphia, where Evans received her new kidney. “That first patient getting transplanted for us was such a great moment for our program that the work didn’t feel like work after that.”
A high school sports physical first spotted Evans’ kidney disease at age 17. While finishing her master’s degree and beginning to earn her Ph.D. at Temple University, she started dialysis — for nine hours a night while she slept — and was placed on the transplant list.
How long it takes to get a kidney transplant depends on patients’ blood type, medical urgency and a mix of other factors — including how long they’ve spent on the waiting list. Evans was first listed in April 2019. When the Jefferson transplant center unearthed her old lab tests, they found she should have qualified in September 2015.
“Just for context, when I was still an undergrad I should have been on the list,” she said, recalling the anger she felt as she read the letter. What she called “a mind-blowing” credit of 3½ more years waiting also provided “a glimmer of hope” that she’d be offered a matching kidney soon.
Evans got a new kidney on July 4 and is healthy again, and grateful the policy change came in time for her.
“You don’t know if people would be alive today” if it had been enacted earlier, she said. Still, that extra step of “making amends to fix the situation for those that we can — I feel like it’s very important and it’s very necessary if you’re truly wanting to bring more equity and equality into the medical field.”
#us politics#news#ap#2024#the associated press#kidney transplant#racial bias#us healthcare#eGFR#estimated glomerular filtration rate#transplant surgery
4 notes
·
View notes
Text
Fishbone #010
the human cost rolls downhill
5 source images, 9 layers.
I hate having to write this. I hate that this is a thing that happened to be written about.
In early 2024 a private virtual clinic providing medical care for a vulnerable and underserved patient demographic allegedly replaced 80% of its human staff with machine learning software.
As far as I can find this hasn't been reported on in the media so far and many of the details are currently not public record. I can't confirm how many staff were laid off, how many quit, how many remain, and how many of those are medics vs how many are admin. I can't confirm exact dates or software applications. This uncertainty about key details is why I'm not naming the clinic. I don't want to accidentally do a libel.
I'm not a journalist and ancestors willing researching this post is as close as I'll ever have to get. It's been extremely depressing. The patient testimonials are abundant and harrowing.
What I have been able to confirm is that the clinic has publicly announced they are "embracing AI," and their FAQs state that their "algorithms" assess patients' medical history, create personalised treatment plans, and make recommendations for therapies, tests, and medications. This made me scream out loud in horror.
Exploring the clinic's family of sites I found that they're using Zoho to manage appointment scheduling. I don't know what if any other applications they're using Zoho for, or whether they're using other software alongside it. Zoho provides office, collaboration, and customer relationship management products; things like scheduling, videocalls, document sharing, mail sorting, etc.
The clinic's recent Glassdoor reviews are appalling, and make reference to increased automation, layoffs, and hasty ai implementation.
The patient community have been reporting abnormally high rates of inadequate and inappropriate care since late February/early March, including:
Wrong or incomplete prescriptions
Inability to contact the clinic
Inability to cancel recurring payments
Appointments being cancelled
Staff simply failing to attend appointments
Delayed prescriptions
Wrong or incomplete treatment summaries
Unannounced dosage or medication changes
The clinic's FAQ suggests that this is a temporary disruption while the new automation workflows are implemented, and service should stabilise in a few months as the new workflows come online. Frankly I consider this an unacceptable attitude towards human lives and health. Existing stable workflows should not be abandoned until new ones are fully operational and stable. Ensuring consistent and appropriate care should be the highest priority at all times.
The push to introduce general-use machine learning into specialised areas of medicine is a deadly one. There are a small number of experimental machine learning models that may eventually have limited use in highly specific medical contexts, to my knowledge none are currently commercially available. No commercially available current generation general use machine learning model is suitable or safe for medical use, and it's almost certain none ever will be.
Machine learning simply doesn't have the capacity to parse the nuances of individual health needs. It doesn't have the capacity to understand anything, let alone the complexities of medical care. It amplifies bias and it "hallucinates" and current research indicates there's no way to avoid either. All it will take for patients to die is for a ML model to hallucinate an improper diagnosis or treatment that's rubber stamped by an overworked doctor.
Yet despite the fact that it is not and will never be fit for purpose, general use machine learning has been pushed fait accompli into the medical lives of real patients, in service to profit. Whether the clinic itself or the software developers or both, someone is profiting from this while already underserved and vulnerable patients are further neglected and endangered.
This is inevitable by design. Maximising profit necessitates inserting the product into as many use cases as possible irrespective of appropriateness. If not this underserved patient group, another underserved patient group would have been pressed, unconsenting, into unsupervised experiments in ML medicine--and may still. The fewer options and resources people have, the easier they are to coerce. You can do whatever you want to those who have no alternative but to endure it.
For profit to flow upwards, cost must flow downwards. This isn't an abstract numerical principle it's a deadly material fact. Human beings, not abstractions, bear the cost of the AI bubble. The more marginalised and exploited the human beings, the more of the cost they bear. Overexploited nations bear the burden of mining, manufacture, and pollution for the physical infrastructure to exist, overexploited workers bear the burden of making machine learning function at all (all of which I will write more about another day), and now patients who don't have the option to refuse it bear the burden of its overuse. There have been others. There will be more. If the profit isn't flowing to you, the cost is--or it will soon.
It doesn't have to be like this. It's like this because humans made it this way, we could change it. Indeed, we must if we are to survive.
3 notes
·
View notes
Text
Bare with me, I've got an idea that combines TFP Shockwave's invention of the cortical psychic patch, what motivation a Shattered Glass Shockwave might have made it, plus more broad cybertronian biology headcanons and how it lead to the invention of the cortical psychic patch in the first place-
Um... let's go!
To start, let's go in reverse order by talking cybertronian biology, or more specifically the more wire based functions of a more literal less sex version of interface panels. Because cybertronians are biomechanical aliens who's only method of 'reproduction' canonically (in most series) is through being birthed by the planet itself - on hold while Primus and Cybertron are dead - when I say 'interface panels' I mean panels housing plugs and ports that are typically there for medical stuff and otherwise data transfers or for use in hardware depending on the individual. The number of panels is relatively consistent and the number of in/out connections depends on the size of the bot (more for larger frames, less for smaller) and are kinda paired to whatever systems they are nearest location wise; two on either side of the hips or one each at the top of the legs, two on either side of the chest or one each at the top of the arms.
Depending on the location you can read the diagnostics of that part of the frame in more detail than if you tried investigating the same part in an entirely different panel; you're gonna get a more accurate read on damages to the left arm in the left arm panels then you are on the right leg. And for particular frames, the interface panels are used to control objects using the relevant limb or part - like a robotic arm to lift things heavier than your frame can handle - and probably even to have your frame be used AS a limb; combiner limbs would connect to whoever's the main body and interface with the relevant limb panel.
But there are panels that are explicitly medical use only, that being internal panels adjunct to the sparkchamber as well as another for specific monitoring of a cybertronian's organs, and paneling at the back of the helm or where it meets the neck for the processor and all the delicate software it holds. Bots with medical programing like Ratchet can interface with those panels directly in the event of a lack of resources (AKA the entirety of Transformers: Prime), and in fact the panel along the sparkchamber would be the easiest way to get a general systems check on a patient. Mecha like Knock Out who may or may not have actual history with being a medical doctor probably would have a harder time directly interfacing with the more delicate sparkchamber, organ, and processor panels, but he and Ratchet (and other bots with even the vaguest sense of medical training) can set up a line running to a monitor or sparkreader or any other medical hardware to fully take in a data analysis, even if it means more resources are used or that vulnerabilities could be introduced.
To the processor panel, much like brain surgery you kinda need a signal in the first place in order to get a read on it's damages, hardware or software. A spark read can let you know if the body is alive and all the damages that IT can diagnose for a general check, but operating on an offline or barely awake processor can lead to issues that you may not even be aware of at the time of procedure. It's why a direct connection (with appropriate medical coding) is better for processor diagnosis as the hardware bypass might have a signal delay between patient and doctor.
And here's where the cortical psychic patch comes in.
When Megan was otherwise comatose, the cortical psychic patch was able to allow access into his processor that had been percolating with activity (one described by Knock Out to be like 'a dream he may never wake from'), and though far from being an actual medical use of the patch it did allow for a non-medical bot to access the processor of a very much comatose patient. It was even Ratchet himself - resident medic of the Autobots - that knew how to create the patch even if it was banned for Autobot use.
Keeping in this reverse order, perhaps a SG Shockwave had invented the cortical psychic patch for an intended medical use, a tool meant for mecha who may not have been forged nor coded to BE medics but have enough training to be such (typically self-taught in the early stages of revolution, then mentored by forged medics when the war really picked up speed) in order to allow direct access to the processor interface panel. The design of it would be - rather than a plug that just magnetically sticks on to the back of a cybertronian's head - would be a series of plugs and ports of mostly universal design, adjustable to a degree for multiple frames, allowing the medic irrespective of coding to have full access to diagnose what the fuck is up with the processor.
Unfortuneately for SG Shockers (and fully intentional by TFP Shockwave) the patch isn't quite as synonymous as the medic's coding is to processor interfacing, being rather invasive of a connection even as it is, let alone the patch being more of a hardware connection which in of itself introduces vulnerabilities. Heck, it's not even safe for the operator themselves to use the patch, seeing as how Bumblebee got a head full of Megan; I mean, Bumblebee isn't a trained medic, but the fact that it happened at all is evidence to it's flaws. And that's to a patient who isn't of mind enough to struggle, Shockwave himself says that resisting the patch may cause damage to the patient/subject, combine that with the second option of 'let it happen and let them walk unabated in your head' and you're pretty much shit out of luck.
The base Shockwave would most certainly be fully aware of the intent, a direct hardline to an individual's processor is most definitely a connection to some very vulnerable software and thus information, the cortical psychic patch probably battling a lot of firewalls off with the ease of a medical interface. And in the base TFP universe, Autobots with only recent war-based medical training as opposed to previous education probably early on DID resort to using the patch as a crutch, Ratchet after all knew how to make one. It's probably a combination of Shockwave's brutal interrogation method USING the cortical psychic patch and the relatively inexperienced Autobot medics opting to use direct processor interface rather than the comparably safer hardware bypass that lead to it's banned status in the Autobot ranks, too many 'Bots were having trauma responses at the hands of young medic's servo's who didn't know any better and actively resisting the patch, which just so happened to lead to more Autobot casualties and thus probably shellshocking the medics in training to get them to fear the daunting prospect of actually losing a patient by THEIR OWN hands.
It's one thing to be using a tool made by someone who has been known to do lots of dubious shit, it's another to see a tool that you made to help be manipulated into an interrogation technique, made all the worse now that you have significantly more emotional capacity to not only feel guilty but feel solely responsible for the patch induced trauma of your own allies; the cortical psychic patch was banned by the Shattered Glass Decepticons for about similar reasons, but it's near worse for a lot of medics (even the experienced ones) had been relying on it solely for the fact that they weren't forged with the coding. The stagnated use of the cortical psychic patch in the base verse was mostly because Shockwave himself had been the inventor of it and main user of the patch, the Autobots avoiding it's use for the ban and the Decepticons not very experienced with the tool. In Shattered Glass however, the only real limit to it's perpetuity would be if the Autobots managed to learn how to create the patch at all, which if even in the base verse Ratchet knew how to make one, probably means that there's more than enough patch use in SG even if Shockwave gets caught in a spacebridge explosion or not.
And that's that I think- funny to talk about interface panels in a transformers post without doing it in a sex way haha- I just want these guys to be alien 😫
#shockwave#tfp shockwave#shattered glass#tfp shattered glass#transformers#tfp#maccadam#xenobiology#i like to conceptualise that there are 6-8 maybe interface panels at a minimum#with a number of ports and plugs that i haven't determined yet but maybe depending on what panel 4ish? idk#i would probably not count because the number might seem off so i'll just say that there's probably a few each#even though i mentioned interface panels in more of a machine or medical way i guess technically it can be used for recreation#those tend to be the external panels though or if 'intimate' aka low-key dangerous and definitely vulnerable#it would be through the sparkchamber panel/s that a doctor would not recommend you doing all willy nilly#even though ko actually goes ahead and implies 'interfacing' is akin to human sex (see 'plus one')#i do believe it's more 'how do i translate what i see to what words i know' plus 'this is a kids show we can't say sex'#the act of connecting one person to another? interfacing#because these bitches are alien they still have interfacing panels in altmode#it's wherever their limbs go and if their spark is anywhere near where the people go#since two wheelers and open four wheelers (like quad bikes and technically dune buggies) don't have a cabin#you're not gonna particularly find any paneling inside a cockpit or under a roof#you could probably have some 'technically' internal panels but functionally not not THE internal panels#internal panels would be actual organ and brain stuff not paneling that happens to reside inside a cockpit or in a dashboard#all these tags are talking about the details of interface panels i realise this post isn't completely about the panels#i would say in recreational interfacing between bots or through hardware you're not gonna be able to access a lot of stuff medics can#unless you're a super hacker like soundwave your firewalls prevent fuckers from reading your mind and can only really be described as#feeling what it's like to have another person's frame which is- technically intimate i suppose#sparkchamber to sparkchamber you might get some extra with the same stipulation that sparkchamber panels offer a global general check#still up to the behest of actual medical coding (or hacker mode) to get actually 'interactive' between systems but you get a bit more info#on the other through sparkchamber connections
12 notes
·
View notes
Text
How does Remote Patient Monitoring in Medical Diagnostic Software?
In today's fast-paced world, technological advancements have made significant strides in reshaping various sectors, and healthcare is no exception. Among the most groundbreaking innovations is remote patient monitoring (RPM), a concept that has transformed the landscape of medical diagnosis and patient care. Integrated within sophisticated medical diagnostic software, RPM offers unparalleled benefits in terms of early detection, continuous monitoring, and personalized treatment plans.
Medical diagnostic software serves as the cornerstone of modern healthcare facilities, providing clinicians with comprehensive tools to analyze patient data, interpret symptoms, and make informed decisions. By incorporating RPM capabilities, this software extends its functionalities beyond the confines of hospital walls, enabling healthcare providers to remotely monitor patients' vital signs, symptoms, and overall health status in real-time.
One of the primary advantages of remote patient monitoring through medical diagnostic software is its ability to enhance the management of chronic conditions. Patients with conditions such as diabetes, hypertension, or heart disease often require regular monitoring of vital signs and adherence to treatment regimens. With RPM, healthcare providers can track patients' health metrics, such as blood glucose levels, blood pressure, and heart rate, without the need for frequent in-person visits. This not only improves patient compliance but also allows for timely intervention in case of any deviations from normal parameters, thus preventing complications and reducing healthcare costs.
Moreover, remote patient monitoring facilitated by medical diagnosis software plays a pivotal role in early disease detection and prevention. By continuously collecting and analyzing patient data, healthcare professionals can identify subtle changes or patterns indicative of underlying health issues before they escalate into serious conditions. For instance, RPM can detect irregularities in cardiac activity, respiratory function, or sleep patterns, prompting timely interventions and personalized treatment strategies. This proactive approach not only improves patient outcomes but also alleviates the burden on healthcare systems by reducing hospital admissions and emergency room visits.
Furthermore, RPM in medical diagnostic software empowers patients to take an active role in managing their health and well-being. Through user-friendly interfaces and wearable devices, individuals can easily monitor their vital signs, track symptoms, and communicate with their healthcare providers remotely. This fosters greater patient engagement, adherence to treatment plans, and self-awareness regarding health-related behaviors. Additionally, RPM enables virtual consultations and telemedicine services, providing patients with convenient access to healthcare professionals regardless of geographical barriers or mobility constraints.
The integration of remote patient monitoring into medical diagnostic software also holds tremendous potential for improving the efficiency and efficacy of clinical trials and research studies. By remotely collecting real-world patient data, researchers can gather insights into the effectiveness of new treatments, medications, or interventions in diverse populations and settings. This not only accelerates the pace of medical innovation but also ensures that healthcare interventions are tailored to the needs and preferences of individual patients.
In conclusion, the synergy between remote patient monitoring and medical diagnostic software represents a paradigm shift in healthcare delivery, offering unprecedented opportunities for proactive, personalized, and patient-centered care. By harnessing the power of technology to monitor patients remotely, healthcare providers can optimize clinical outcomes, enhance patient engagement, and advance medical research. As the healthcare industry continues to embrace digital transformation, the integration of RPM into medical diagnostic software is poised to revolutionize the way we diagnose, treat, and manage health conditions in the 21st century.
0 notes
Text
Robert Pearl, a professor at Stanford medical school, was previously CEO of Kaiser Permanente, a US medical group with more than 12 million patients. If he was still in charge, he’d insist that all of its 24,000 physicians start using ChatGPT in their practice now.
“I think it will be more important to doctors than the stethoscope was in the past,” Pearl says. “No physician who practices high-quality medicine will do so without accessing ChatGPT or other forms of generative AI.”
Pearl no longer practices medicine but says he knows physicians using ChatGPT to summarize patient care, write letters, and even—when stumped—ask for ideas on how to diagnose patients. He suspects doctors will discover hundreds of thousands of useful applications of the bot for the betterment of human health.
As technology like OpenAI’s ChatGPT challenges the supremacy of Google search and triggers talks of industry transformation, language models are starting to show the ability to take on tasks previously reserved for white-collar workers like programmers, lawyers, and doctors. That has sparked conversations among doctors about how the tech can help them serve patients. Medical professionals hope language models can unearth information in digital health records or supply patients with summaries of lengthy, technical notes, but there’s also fear they can fool doctors or provide inaccurate responses that lead to an incorrect diagnosis or treatment plan.
Companies developing AI technology have made medical school exams a benchmark in the competition to build more capable systems. Last year, Microsoft Research introduced BioGPT, a language model that achieved high marks on a range of medical tasks, and a paper from OpenAI, Massachusetts General Hospital, and AnsibleHealth claimed that ChatGPT can meet or exceed the 60 percent passing score of the US Medical Licensing Exam. Weeks later, Google and DeepMind researchers introduced Med-PaLM, which achieved 67 percent accuracy on the same test, although they also wrote that, while encouraging, their results “remain inferior to clinicians.” Microsoft and one of the world’s largest health care software providers, Epic Systems, have announced plans to use OpenAI’s GPT-4, which underpins ChatGPT, to search for trends in electronic health records.
Heather Mattie, a lecturer in public health at Harvard University who studies the impact of AI on health care, was impressed the first time she used ChatGPT. She asked for a summary of how modeling social connections has been used to study HIV, a topic she researches. Eventually the model touched on subjects outside of her knowledge, and she could no longer discern whether it was factual. She found herself wondering how ChatGPT reconciles two completely different or opposing conclusions from medical papers, and who determines whether an answer is suitable or harmful.
Mattie now describes herself as less pessimistic than she was after that early experience. It can be a useful tool for tasks like summarizing text, she says, so long as the user knows that the bot may not be 100 percent correct and can generate biased results. She particularly worries about how ChatGPT treats diagnostic tools for cardiovascular disease and intensive care injury scoring, which have track records of race and gender bias. But she remains cautious about ChatGPT in a clinical setting, because sometimes it fabricates facts and doesn’t make clear when the information it is drawing on dates from.
“Medical knowledge and practices change and evolve over time, and there’s no telling where in the timeline of medicine ChatGPT pulls its information from when stating a typical treatment,” she says. “Is that information recent or is it dated?”
Users also need to beware how ChatGPT-style bots can present fabricated, or “hallucinated,” information in a superficially fluent way, potentially leading to serious errors if a person doesn't fact-check an algorithm's responses. And AI-generated text can influence humans in subtle ways. A study published in January, which has not been peer reviewed, that posed ethical teasers to ChatGPT concluded that the chatbot makes for an inconsistent moral adviser that can influence human decisionmaking even when people know that the advice is coming from AI software.
Being a doctor is about much more than regurgitating encyclopedic medical knowledge. While many physicians are enthusiastic about using ChatGPT for low-risk tasks like text summarization, some bioethicists worry that doctors will turn to the bot for advice when they encounter a tough ethical decision like whether surgery is the right choice for a patient with a low likelihood of survival or recovery.
“You can't outsource or automate that kind of process to a generative AI model,” says Jamie Webb, a bioethicist at the Center for Technomoral Futures at the University of Edinburgh.
Last year, Webb and a team of moral psychologists explored what it would take to build an AI-powered “moral adviser” for use in medicine, inspired by previous research that suggested the idea. Webb and his coauthors concluded that it would be tricky for such systems to reliably balance different ethical principles and that doctors and other staff might suffer “moral de-skilling” if they were to grow overly reliant on a bot instead of thinking through tricky decisions themselves.
Webb points out that doctors have been told before that AI that processes language will revolutionize their work, only to be disappointed. After Jeopardy! wins in 2010 and 2011, the Watson division at IBM turned to oncology and made claims about effectiveness fighting cancer with AI. But that solution, initially dubbed Memorial Sloan Kettering in a box, wasn’t as successful in clinical settings as the hype would suggest, and in 2020 IBM shut down the project.
When hype rings hollow, there could be lasting consequences. During a discussion panel at Harvard on the potential for AI in medicine in February, primary care physician Trishan Panch recalled seeing a colleague post on Twitter to share the results of asking ChatGPT to diagnose an illness, soon after the chatbot’s release.
Excited clinicians quickly responded with pledges to use the tech in their own practices, Panch recalled, but by around the 20th reply, another doctor chimed in and said every reference generated by the model was fake. “It only takes one or two things like that to erode trust in the whole thing,” said Panch, who is cofounder of health care software startup Wellframe.
Despite AI’s sometimes glaring mistakes, Robert Pearl, formerly of Kaiser Permanente, remains extremely bullish on language models like ChatGPT. He believes that in the years ahead, language models in health care will become more like the iPhone, packed with features and power that can augment doctors and help patients manage chronic disease. He even suspects language models like ChatGPT can help reduce the more than 250,000 deaths that occur annually in the US as a result of medical errors.
Pearl does consider some things off-limits for AI. Helping people cope with grief and loss, end-of-life conversations with families, and talk about procedures involving a high risk of complications should not involve a bot, he says, because every patient’s needs are so variable that you have to have those conversations to get there.
“Those are human-to-human conversations,” Pearl says, predicting that what’s available today is just a small percentage of the potential. “If I'm wrong, it's because I'm overestimating the pace of improvement in the technology. But every time I look, it's moving faster than even I thought.”
For now, he likens ChatGPT to a medical student: capable of providing care to patients and pitching in, but everything it does must be reviewed by an attending physician.
8 notes
·
View notes
Text
Hello intro time!
I have a degree in games design and programming, I'm not working in games right now because of that very fun market collapse going on, but I have some personal projects going on that I'll post about! I know C# and C++ and can use both unity and unreal.
I'm currently a junior software tester but I'm hoping to move into development when I can.
I really like debugging and problem solving so if you have bugs or any programming issues (especially game dev related) send em over! I'm being genuine i actually really enjoy messing with that kinda stuff.
I'm conversational in danish! I'm around a B1 level, though I haven't been able to practice as much lately, I'm hoping to get back into it when I'm more settled in my job.
I know way too much about NieR lore and have got all endings on both main games, I could infodump for hours about them if you want that.
I was diagnosed with ADHD at 18, along with suspected autism (basically confirmed but I didn't want to pay extra for the diagnosis so I'm fine just knowing), I got diagnosed with OCD at 20 which is now basically under control because of my medication! Im open to talking about my experience.
GitHub
6 notes
·
View notes
Text
$FTD How To Make Money On Friend.Tech With Sniper Bot
$FTD How To Make Money On Friend.Tech With Sniper Bot
$FTD How To Make Money On Friend.Tech With Sniper Bot
https://ifttt.com/images/no_image_card.png https://www.youtube.com/watch?v=Ch2bXDHEwBs
https://ifttt.com/images/no_image_card.png https://cryptoncars.wordpress.com/2023/09/09/ftd-how-to-make-money-on-friend-tech-with-sniper-bot/
View On WordPress
#billing#classification#clinics#coding#diagnosis#healthcare#hospitals#insurance#Medical#physician#reimbursement#software#specialists
0 notes
Text
3 Things to Know About Different Kinds of Basic Life Policies
3 Things to Know About Different Kinds of Basic Life Policies
3 Things to Know About Different Kinds of Basic Life Policies
3 Things to Know About Different Kinds of Basic Life Policies
No one wants to think about life insurance, but it’s essential if you’re going to protect your family.
106 million Americans lack sufficient life insurance coverage, mostly due to a lack of knowledge on the subject. It’s never too early to start thinking about different…
View On WordPress
#billing#classification#clinics#coding#diagnosis#healthcare#hospitals#insurance#Medical#physician#reimbursement#software#specialists
0 notes