#my hemoglobin should be between 12 and 15
Text
when you catch a mistake in ur tags or ur post but its too late
this wouldn’t keep happening to me if there was a way to better edit and rearrange already typed tags 8|
#@ tumblr get with it bitch#maison speaks#throwing this unrelated bit on the end bc i dont feel like making a whole other post BUT#i spent most of yesterday afternoon and evening in the emergency room after my body had some weird#kind of fit that was absolutely terrifying while i was leaving emdr. i had to text my mom to come get me bc driving wasnt safe#turned out to be a good decision bc by the time they had me sitting on a bed in er it was just.. not good#at some point i took a nap and my mom said later that it continued while i was asleep and i kept getting really close to violently#twitching my dumb ass off the bed. limb control?? yeah i've heard of her. we've had a falling out of sorts apparently#GOOD NEWS HOWEVER - its nothing really serious. they think its new medication side effects + caffeine (it was a med that could be#affected by caffeine take and nobody thought to tell me that until i felt like i was going to die?? coolcoolcool i guess#the whole thing has been put on hold until my next psych appointment at least#oh yeah!! and i'm anemic!! which i already knew but i didnt realize just how bad it was until today#my hemoglobin should be between 12 and 15#its 8#hematocrit should be between like 35 and 45 i think??#yeah mine is 11#im really out here filling the role of pre-serum steve without the skinniness huh
2 notes
·
View notes
Text
Here is an NGO that helps Ukrainian Romani women!
Svitlana’s eyes began to shine with happiness as she entered the hotel room in Odesa. She had never spent a night in a hotel, or any place that to her seemed so beautifully decorated. She had come here to change her life.
Svitlana* was attending a women’s leadership training from CARE and the charity foundation Winds of Change.
Throughout her childhood and adolescence, Svitlana had lived in a compact settlement for Roma families in Odesa region. Women’s health was never discussed there. She didn’t go to school, because she had to take care of her younger siblings.
Only recently, at 28, has she learned to write her own name.
Winds of Change, a CARE partner organization, has been working with the Roma community for over four years.
Roma, also called Romany, is an ethnic group of traditionally itinerant people who originated in northern India but now live principally in Europe.
The word “Roma” means “man” and refers to different communities, including Kalderash in southeastern Europe, Romanichals in England, Sinti in Germany, Italy, and France, Kalé in Wales, Finland, Spain and Portugal, and Gitano from Spain, as well as many others around the world — there are an estimated 400,000 Roma people in Ukraine.
As part of CARE’s Women’s Lead in Emergencies model, Winds of Change is working with the Roma communities in Ukraine to train women to take part in leadership.
‘I dreamed of being an artist’
Svitlana was 15 when she got married. She married her husband “under the Roma law.” They have no legal marriage documents.
“He stole me from my parents, and since then we have been living together,” Svitlana says. “This is how most Roma girls live. [They say] women should only look after children, clean and cook… But when I was a child, I dreamed of being an artist. To paint beautiful patterns on the facades of the house. It’s a pity that I never did.”
Some 80 percent of girls in the Roma community have similar stories. From a young age they help their parents look after younger children, and between the ages of 12 and 15 they are coerced into marriage where they then start their adult life.
Now she has six children.
She dreams that all her children will be educated. So, this year, with the support of the Winds of Change Foundation, three of her six children went to the first grade, and two went to the second grade.
For Svitlana, it was an indescribable joy.
A double standard
“Very often, representatives of local authorities, especially in rural areas, turn a blind eye to Roma needs,” says Yulia Hladka, a Winds of Change representative. “Children may not go to school, because it is their tradition. They are Roma; they are married early and have different ‘duties’” — this is how social services often react to the remarks of Roma human rights organizations. If a Ukrainian woman was in a similar situation, she would have been noticed and social services would have intervened.”
Roma people feel this indifference, even from the medical community. When Svitlana fell ill, the local hospital was reluctant to admit her. It was the same with the pediatrician. He simply recorded the visits in a log, although he did not actually examine her children.
It was only with Yulia Hladka’s help that Svitlana finally decided to see a gynecologist to find out the cause of her irregular cycle and heavy bleeding. But it wasn’t easy, because of ethnic discrimination. Only at a private medical center was Svitlana thoroughly examined and found to have cervical erosion, a damaged cyst, and critically low hemoglobin.
Now she is undergoing a long course of treatment.
A double discrimination
As Winds of Change has learned, changing the lives of Roma women is not always easy. These women have suffered discrimination, and sometimes violence, and are understandably reluctant to trust.
Human rights organizations call the Roma community one of the most discriminated against social groups in Ukraine.
Roma women in Ukraine are subject to double discrimination — on ethnic and gender grounds. They face limitations in various aspects of their lives, such as being compelled to marry at a young age and having more than two or three children. Because their community considers them responsible for caring for younger children, they also have restricted access to education compared to boys. They face challenges in finding employment and accessing healthcare.
Life undocumented
Many problems are caused by the lack of documents, as usually Roma people live in isolation and very rarely turn to government institutions. Women give birth at home and do not even apply for birth certificates. The absence of passports also makes it difficult for Roma to obtain documents, so they cannot receive assistance from the state, and their number in the country cannot be officially counted.
According to Roma NGOs like Winds of Change, charitable foundation “Planet of Good People,” just over a third of Ukrainian Roma are employed. For Roma women, this is often complicated by the fact that they are mothers of many children, so they face discrimination on this basis as well.
This was the case with Svitlana. She has been dependent on her husband’s decisions almost since childhood. All her time was taken up with housework and caring for her six children and her husband’s sister’s 13 children.
“At one of the focus groups, we realized that a very big problem for Roma women is the lack of access to basic services and jobs,” says Yulia. “They usually live in rural areas where there are not many employment opportunities.”
“But even if vacancies do appear, Roma are usually rejected, because of stereotypes and ethnicity.”
“We came up with the idea to create a social enterprise where these women could get hard skills — sewing home textiles and clothes — and soft skills, like communication, psychological self-regulation. We organized a small sewing company in Odesa called Petalenca, where Roma women sew bedding and home clothes. We train them and help them promote their products.”
After the escalation of the situation in Ukraine, many internally displaced women also found their place here and started working together with Roma women. Some women had some stereotypes about Roma before but working together helped to dispel them. Now this company employs Roma and women who have been displaced.
*name changed
They accept donations!
170 notes
·
View notes
Text
So. I went into premature labor at work, without REALIZING it, just felt a lot of fucking pain. Apparently they were contractions because my water was pushing against my cervix. Hospital broke my water and then they just stopped. No more contractions.
So THEN they want to try to keep me pregnant till I'm 34 weeks - I'm BARELY 24 weeks at this point - and I'm freaking the feck out at this point because at this point I'm told I have a high probability of losing my son if he decides he does want to come now.
BUT baby decides to stay in for a bit. Fast forward 2 days. I'm transferred to a better hospital that is equipped to take care of my baby should he come. By this point I've had 4 steroid shots - those burn like a mfker - to help my babies lungs. While this is going on they've been taking blood from me. Quite a bit. I'm told my hemoglobin is at 7.1. It should be between 12 and 15. I'm anemic as fk. They had such difficult times getting blood out of me. They stuck me 5 times at one point trying to get blood. Ended up trying the artery in my arm. If you've never had blood taken from your artery, be thankful. It was so goddamn painful.
Anyway, I end up getting 3 IVs altogether, and as someone who HATES needles, I am shitting myself. The powerglide was horrific to put in.
After I am transferred, I am told I need iron infusions. Badly. Was supposed to get a blood transfusion as well but that never happened. I'm AB+ so I can take anything. Dunno why they just forgot about it but whatever.
Fast forward 2 more miserable damn days, I end up having contractions the night before thanksgiving. Doctor comes in to check me around 7 after I told the nurse I felt pressure down there. She takes one damn look and stops, pauses, and says she sees my baby's head. Next thing I know, like 10 damn people are in the room and I have my baby 10 minutes later.
I'm all alone by myself up there because I'm only allowed 1 visitor because I caught covid from a coworker and my 1 visitor is my boyfriend but he has to work that day. But they end up bending the rules and allowing my mother to come in. My boyfriend's boss told him he'd get pointed that day if he didn't show up. Once we reach a certain total, we're fired and it's hard to get rid of points once you get one. I work at the same place. He did manage to come see me for a bit before going in which I was thankful for. But we live an hour away from the hospital I was at.
I wanted to name my son River but my boyfriend and I couldn't compromise on a name. He kept picking video game characters and anime characters as names lol which is fine I guess but the ones he chose I hated. We eventually compromised on Eren as his first name and River as his middle name.
He'll be in the NICU for quite a while, till around March, which was when his due date was. Little brat decided he wanted to be born on thanksgiving day instead haha. I wish he could have stayed in me for his full term but I'm just thankfull he's okay. I just wish I could hold him. He has to stay in an incubator for a long time. He's so tiny. He was only 10.5 inches and 1 pound, 63 ounces when he was born.
Hopefully everything goes well and I eventually get to bring him home. I'm tired of crying over not getting to hold him.
#well this is why I have been inactive lol#pregnancy is a scary thing and i wish i could have gotten to carry him for the full 9 months#i know my moms side is full of anemic people so i hope that isn't what contributed to this#my boyfriend and i want more kids in the future but id be too terrified to put anymore of my babies through this#i just want to hold him#forgive this rambling of mine but i needed to vent somewhere badly#post pregnancy emotions are wild lol im sitting here crying again while typing this out
6 notes
·
View notes
Text
BBL Costs, Prep + Recovery
Im booked!! I talked to a few friends who I know either got this surgery or is getting this done. I wanted one since forever but I wanted my teeth done first. The deciding factor came down to my birthday plans.
Originally I was going to do a birthday tour. First weekend of October in Miami for carnival, 2nd weekend in Atl for Freak Nik, 3rd weekend in Bahamas and finally Nola for the finale. Well Nola was just hit with a storm so yeah that’s out. Once I totaled up the flights, hotels, food and spending money.. I was like hmm, I can get a fat ass and started this process. Immediately looked into surgeon and Dr. Pena was my favorite, his bodies come out so mf snatched, he’s located in Columbia. Columbian surgeons can take out way more fat than American doctors however, the fatality rate is stupid and ultimately the factor that made me choose an American doctor.
The next step was choosing the surgeon for the body I have and the one I want. I weigh 151 and im 5′6″ I’m considered a “skinny bbl”. I started researching doctors in Atlanta (so I could recover at home) and Miami (like duh). I chose to go with Dr. Desouza in Miami with CG Cosmetics for a few reasons. First, I love the look of his skinny bbl’s on other women with the same body type, weight and height as me. Secondly, he was having a special for the end of the year (lipo 360, bbl, jplasma for $6500 for the surgeon I wanted) this almost sold me but it was the surgery date!! Jplasma is skin tightening procedure to help with loose skin, you can only get this with lipo. When they perform lipo they created canals under your skin to remove the fat.. well those same canals are essential when getting Jplasma.
Ok so I decided on the surgeon, contacted the cosmetic group and had a consultation which is pretty much just front, side and back view pictures.. I think they use this to make sure you don’t need a tummy tuck prior to surgery. They also asked me questions about previous surgeries and if i’ve ever had anesthesia. The next step went pretty quickly, we talked about what would be lipo’d (abs, waist, back.. I wanted inner thighs, an additional 2k, but was advised to wait on my pre-op to decide), when I wanted to book and how I'd pay. My consult was on August 30th.. I bitched up when she attempted to take my payment. I am a money hoarder and spending that much money made me feel like I was being financially irresponsible. I called one of my Aunt’s who I felt wouldn’t judge me and also give me sound advise. We talked about my fears, why I was getting the procedure and of course money. My Aunt gave me excellent advice, reassured me and is a professional CNA who offered to accompany me so yeah I dare not turn that down, lol. August 31, 2021, I called my coordinator (the contact between me and my surgeon) and told her I wanted to book, she asked me when I’d be ready and I requested first available which was 9/20/21!! Excited is an understatement.. I'd be 24 days post op on my birthday. After I calmed down I paid in full for multiple reasons: had to in order to secure the date, all surgeries book in this year had to be paid in full, it was the only way to get the discount.. My coordinator gave me so much information I couldn’t see straight (I was also high as shit off life thinking about a fat ass and me in the same sentence).. she emailed + texted everything, congratulated me and we hung up.
I get the emails: “raise you hemoglobin with these vitamins” I purchased vitamin C $2, folic acid $2, iron $3 and floradix $35 - amazon, I take them as directed on the bottle and start eating my ass off (just to give my surgeon more to work with, lol). Talking to one of my gf’s I realize I have to be cleared for surgery?!?! What? I open my email and sure enough I have to have blood work done 15-20 prior to surgery, it was 9/3 and a Friday.. SHIT!! I fly over to an Piedmont Wellstreet urgent care facility as recommended by my friend (she started this process as well so I was crazy grateful for her experience and that she shared it with me). Urgent care was full but opened the next day, my ass was in that line at 7:32 am, I was the 13th person in line and they opened at 8. I get to the desk and my appointment is at 10:30 and I'd have to pay the office visit fee to be seen, it was $155. I came back at my allotted time and was told how much all of my labs would be.. $302. My labs were to be processed and faxed to my surgeon by 9/9 because Labor Day weekend so.. yeah.
I discuss accommodations with my Aunt and realize it’s cheaper, safer and more beneficial for me to go to a recovery house. I search high and low baby and most of them were booked.. found one regardless with lymphatic massages included called Flawless Recovery House. This wasn’t my 1st-6th option but the one with availability on my surgery date so I paid a deposit to hold onto my spot. Total was $1312 for 5 days with 5 massages, I paid a $200 deposit. Next, I booked my flight, round trip $116 with Delta. My surgery date is on a Monday, I have to have my pre-op done on the Saturday prior so I booked a hostel from the 18th-20th on booking.com for $66. I know I could have gotten an airbnb or hotel room but I wanted this experience. I want to go to Amsterdam and stay in a hostel so I need to know what to expect. Also I cannot party, smoke, drink or eat before surgery so fuck it.. a hostel will do, lol.
I smoke big fucking weed and watched someone else’s bbl journey today and realize if I fail the drug test, my surgery will be cancelled and it’ll cost me $1500 to reschedule. Boy the shit sent me into panic mode like I've never experienced before, only to find out the weed isn’t the issue nicotine is, it slows down your heart rate. I can smoke weed just not out of a wood or a rillo and nicotine takes 3-4 days to get out of your system so a bitch barely made it. I just won't be smoking until I get back home lol. Just to be super informative no alcohol, diabetic meds, cocaine, pcp or anything that will fool with your heart or makes your bleed. Today is 9/11 and im one week out from my pre-op... my body is a joke cause I haven’t gained a single pound and normally it’s nothing for me to put on weight. I took my acrylics off, when you’re put to sleep they monitor your oxygen levels with those clamps they put on your fingers and they aren't the most accurate when you have on dark polish or acrylics. I also cannot wear lashes cause when they go to fill this ass in I'll be laying flat on my face. I mean my hair didn’t have requirements but I figure since im naked I might as well be bald.. y'all should see me rn, I look very much like a young man but im hype. I’ll be back later to tell y'all what I pack and purchase prior to my flight. Imma put the dates at the end of each update.. today is 9/11/21
My surgery group send me list of supplies that I would need and the cost came to roughly $1100. Naive me was definitely going to purchase everything on the list from them until I saw Leslie’s (@prettyhaute - on ig) bbl vlog. I went on amazon and got away with murder. Below I’ll list what I purchased and the price I paid versus what the surgery center was quoting me.
Faja - I paid $74.69 - Quoted $160.50 || BBL Pillow - $26.99 - Qouted $42.80 || Arnica pills - $8.95 - Quoted $37.45 || Compression socks - $13.99 for 3 - Quoted $10.70 for 1 || Foams - $17.99 for 3 - Quoted $64.20 for 3 || Scar Cream $$29.82 - Quoted $80.25 || Arnica Gel - $7.92 - Quoted $21.40 ||
There a shit ton of items on the suggested list that I didn't purchase but way more items that wasn’t on the list I still need for instance:
Crocs, benadryll, robe, adult diapers, straws, earplugs, liquid iv, stool softener, antiseptic body wash, avocado float, back board, urinal, pineapple juice, throat calm, 3 moo-moo’s and a massage roller (the crocs are the only thing on this list that cost more than $20). My flight is at 7:15a tomorrow and im so damn nervous but excited. I will spend Saturday and Sunday gallivanting around Miami and then body , ody, ody, ody, ody, ody. I still have to send my entire itinerary to my aunt but I think im all set. 9/17/21
Pre-op was packed but I went on Saturday and was in and out in an hour. I was charged for a covid $80, 3 post-op massages $150 and a drug test $20. I went over my clearance paper work with a medical assistant who also took 9 before pics of me. Keep in mind, your surgery can be cancelled or reschedule if all of you labs aren’t at the surgery center on pre-op day. I cannot stress how important it is to take your labs with you!!! Mine were faxed over from urgent care but I was also provided copies which I took with me. The photos were sent directly to my surgeon to analyze before surgery. From my knowledge, I was also to be fitted for my faja but that never happened, do NOT leave pre-op without a faja!!! I paid for 3 massages from CG totaling $150 which I regret badly. I do NOT recommend getting massages from the surgery center. There are 4-5 different surgeons performing surgeries on any given day and they do at minimum 4 surgeries per day, that’s at least 15-20 different girls with the same surgery and post-op date. CG had 2 massage therapists to drain 15-20 girls. I was drained for 9 mins, your drain massages should last at least 45 mins for maximum drainage. I only used 1 of the 3 massages I paid for and was denied a refund. That is a huge downside to CG once they have your money good fucking luck getting it back! Ps. Ellie was a royal fucking cunt!!!!! She told my medical assistant that I didn’t need a faja so I was never fitted for one and woke up out of surgery with a binder on versus a faja like I should have. I wanted to slap the shit out of her and took the charge on the chin but I wanted my surgery so I refrained.. I was put on a 12 hour fast and contacted an hour after pre-op with my surgery address and time. My fast started at 7pm the day before surgery and my surgery time wa at 6:30a, there was a $300 for showing up to surgery late. All I could bring to surgery was compression socks and a faja (that I didn’t have), I was instructed to bathe with dial (the orange one) before surgery to make sure my incisions weren’t infected, no lotion, perfume, deodorant, makeup, nails, lashes, no jewelry/piercing or hair products and no personals ie, purse money, wallet also you will need a companion or surgery will be cancelled. I’ll upload all my paperwork at the end. Surgery day arrive at the surgery center at 6:15 am how about the entire fucking staff was late! Bitch I was outside in Miami alone with compression socks on and a moo moo, LIVID. No one arrived until 7:10 am, baby I wanted to kill everyone but fuck it, it was go time. I’m escorted to a room, changed into a paper gown, piss tested, my labs were reviewed again and finally my surgeon comes in! We were in the exam room alone which was weird cause I was asshole naked but he kept it 1000% professional, he asked me what I wanted and I say “the fattest ass” he looked me dead in my eyes without a single hesitation and said “it’ll heal like a diaper” LMAO. I showed him areas that I wanted lipo’d to death and he marked me up, I didn’t aka e picture of my mark ups but shit was rolling by then, he walked out I put my paper gown back on and the anesthesiologist walked in. I expressed my biggest concerns to him, I didn’t want to die and I didn’t want to wake up during surgery. He explain why the drug test was so important because certain street drugs will have adverse effect with the anesthesia. My anesthesiologist walked me up to the surgery room and I hopped on the table, they put massage boots on both of my feet and inserted an iv, the mask was put on my face and my heart rate went to heaven, I wanted to shit myself bro. The anesthesiologist told me to make a tight fist, I asked what time it was, 8:08am.. I woke up to a nurse helping me into a wheelchair with a binder around my waist and I was scream crying because my entire body ached, I didn't know where I was and the anesthesia is no hoe. I was escorted to my recovery house’s transportation van and taken to my damn bed.
I chose Flawlesss Recovery House with Ms. Opal. I paid a $200 deposit before 2 weeks before surgery and the balance the day I left. I opted for a 5 day stay. I loved it there bro and couldn’t imagine trying to recover at a hotel or air bnb! There were nurses there 24-7, I was roomed with one other girl but the house had a total of 4 bedrooms, one of which no one occupied and the door was always shut but my room was the only room with 2 beds, the others had 3 beds. I had a call button, it was love, the nurses came expeditiously when I rang it. They made 3 home cooked meals per day and I don’t eat meat, they accommodated me with no hesitation. I loved it man. So couple hours after surgery I attempted to use the bathroom on my own and blacked out, the anesthesia is really fucking strong and took an entire day to wear off (for me), the nurses helped me pee in a cup until then. Post op day 9/21/21, I went in to make sure I looked good, got a faja finally and received that lousy as drain. Back to the recovery house I was able to walk finally w/o passing out and in went my foams, I also could pee by myself with the use of a urinal. I was constipated for 2 days, first bowel movement was on post op day 2. I paid for an independent massage therapist named Tatiana, she used a ultrasound machine to massage me so I cancelled her. When I took my faja off for my massage it was washed and dried by the time I was done, I took a shower and put my faja on with my foams. I cancelled Tatiana because don’t let nobody use no machine on you until you are at least 2 weeks post op, hand massages only. All the girls were getting massaged by the literal best massage therapist (in my opinion) her name is Brittany, I could cry she was EVERYTHING, I was tender but she put the painful massage theory to bed! She taught me how to drain myself and how to open my incisions without the q-tip looking thing. In 45 mins she drained 5 of those doggy pad things worth of fluid off of me. I received 4 massages in 5 days. I left on Saturday 9/25/2021 on Sunday, back in Atlanta, I received my 5th massage and that when I was told I have not one but 2 seromas. I swear on everything I love it was because everyone wakes up from surgery with a faja on but not me (Fuck you Ellie, lil bitch) I had on a binder (its what they use for tummy tucks). The lady who did my 1st massage in Atlanta was Bri, not gone post her ig cause she did a damn good massage but when I asked her to syringe drain me the good sis stuck this long ass needle in my seroma but could get the fluid out, cancelled her too (the massage was good asf tho but nah). Tired and tried I bit the bullet and booked a packed with Dream Body ($455 for 5 massage, I think, don’t quote me look it up on there site and follow them on ig) because they are the biggest name in Atlanta, Jayda Wayda goes to them. The most painful massage yet, yes Michelle lil ass is so strong but she will get the fluid up off you. She made me tear up bad and no matter how much I screamed or even tried to push her off of me she understood the assignment, Michelle helped me get back into my faja after my massage and told me my faja was too big and to have it altered. She recommended a lady on ig @siri2sir but to know me is to know I altered my shit myself. Allow me to tell y'all, I look good asf!!!!!!! 10/4/2021
4 notes
·
View notes
Text
Part 1of 2
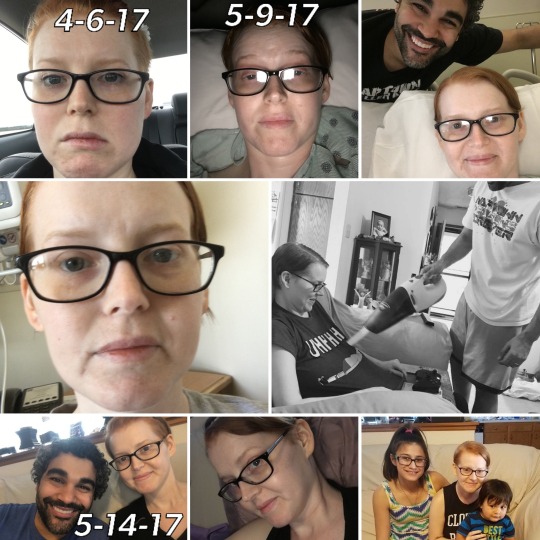
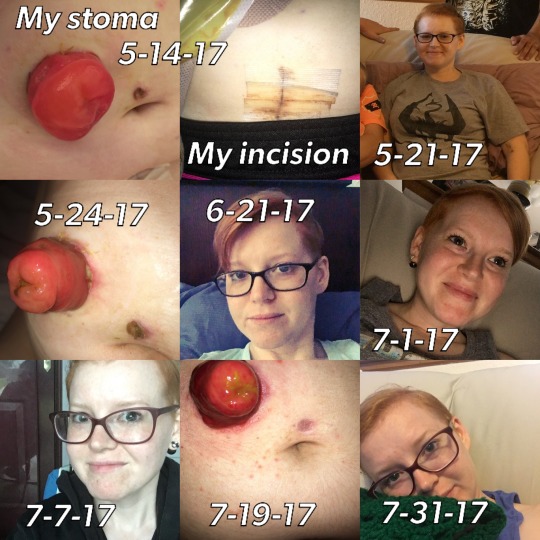
Trigger warning! Graphic photos in this post.
4-6-17 In the very first photo, I have a horrible tooth ache and had no idea the pain and agony it was going to bring. It ultimately changed my life and for a very long time it was changed for the worse. In the photos following, you’ll see me change and look like death and then recover. You’ll see me living life to the fullest but behind closed doors or under my shirt rather, you’ll see how much I’ve had to overcome. This is my story.
On October 30th 2013, I had a colonoscopy and was diagnosed with Ulcerative Colitis(UC) which is a chronic inflammatory bowel disease(IBD) and an autoimmune disease. I was prescribed Canasa suppositories and my symptoms when away for about a year or so and then came back. I had to get a new Gastroenterologist doctor because my previous one had retired. He wasn’t much help anyway. My new GI doctor was amazing and caring and she saved my life. She prescribed me Lialda(NSAID) and Uceris(steroid).
At the end of March 2017, I had horrible tooth pain and called my dentist and they prescribed me Tramadol and Augmentin. The Tramadol made me sick so I called and had them switch the med and they gave me Clindamycin and that made me sick too. They gave me Hydrocodone and that also made me sick so they just had me taking Ibuprofen and Augmentin. I started to have a bad reaction to the Augmentin and got sores all in my throat and mouth and was throwing up and had severe diarrhea. I finished the antibiotic but went to the er because of the pain in my mouth and the vomiting. Mary’s magic mouthwash was prescribed to me to help with the sores and also nausea meds. The only time I was able to get any sleep was when this mouthwash numbed my mouth and throat. For weeks, I was unable to eat or drink anything nor was I able to take my UC meds and my heart rate was high. I went to the er multiple times during this whole ordeal because I couldn’t stop throwing up and all they would do is give me fluids and nausea meds then send me home. I went to an er and waited for 3 hours all the while throwing up with no end in sight and ended up leaving to go to a different hospital. On April 15th, I was pacing the house back and forth because I was miserable and didn’t know what to do. I didn’t want to go to the er yet again for them to just send me right back home. I remember I was pacing by the front door and my husband Issaac went to check the mail. I watched him and then started to say his name over and over because I felt like something was really wrong. Next thing I remember is Issaac kneeling over me and having shoes stabbing me in the back. I had passed out and my eyes were open the whole time but I was unresponsive. Issaac had ran in and thought I was dead. He called 911 and they wouldn’t answer. He used my finger to unlock my phone and dialed 911 and had both phones ringing and finally got an answer. (Fun fact for iPhones: if you press the big button on the side it will call 911 and they can track your location. Dialing 911 will not allow them to track your location.) The ambulance took me to the er and they did 2 EKG’s, CT scan(only after Issaac asked them to because I hit my head when I fell.), chest X-ray, and blood work. I was also tested for CDiff many times but it was always negative. Again, I was given fluids and sent home. They said it was normal for a lot of people to live with an elevated heart rate so they weren’t concerned. A couple days later I went to my primary care doctors office. My doctor was on maternity leave so I saw a different doctor. He did blood work and then wanted me to take depression meds. That was a hard NO! He said I wasn’t getting better because I was depressed about being sick. Yes, I was absolutely miserable and sad about it. BUT, there was something more going on. I wasn’t getting better and I knew it wasn’t my fault. I had to keep advocating for myself because I wasn’t getting help from any of these doctors I’ve seen. I think I went to the er again at some point and was sent home. Then they called me and said my potassium levels were too low and they didn’t think I’d be able to get down the prescribed potassium drink. So we went back to the er. Again. The er wouldn’t take the word of the doctor from another hospital so they did blood work again. We went to a different hospital because the wait at the previous one was way too long. So I received potassium through an iv and that is not comfortable. It burned as it went through my arm. I was also given Magnesium. I was sent home the next day.
Even though the sores were finally gone from my mouth, I was still struggling to swallow. I had my GI doctor schedule an upper Endoscopy which I had done on April 20th. My esophagus had no damage and there wasn’t anything stuck in there. While I was under anesthesia, my GI doctor did a Flexible Sigmoidoscopy. This a colonoscopy but only through a small portion of the colon. It was then that I finally, FINALLY after a month of being so sick that I was admitted to the hospital. My doctor said I looked like I was going to die. She said my colon was so severely inflamed that she couldn’t let me go home even though a patient being admitted after a procedure being done by her makes her look bad. She saved my life and I’m eternally grateful. I had 10 er visits and a scheduled dr visit and none of these doctors thought to have my colon checked knowing that I had UC and continued to show anemia in the blood tests they all ran. It all finally made sense. I wasn’t able to take my UC meds and I was taking 800mg of Ibuprofen for the tooth ache I had. This is what caused my UC to flare up. Why couldn’t 11 doctors put that together?
While I was in the hospital, I received 3 Iron infusions to raise my hemoglobin. I also had a speech therapist come in and she helped me with my throat issue. I was still struggling to swallow and she said that I was protecting my self subconsciously. She worked with me and I was finally able to swallow normally. I was so happy to finally eat a meal without a struggle. I was released 5 days later on April 25th even though I felt I should have stayed. The very next day I woke Issaac up because I was shivering and my teeth were rattling like crazy. My heart rate was 145. Issaac called 911 and we went to the er for the 11th time within a months time. I was put in the observation unit at Methodist which was in the basement because they didn’t have any rooms in the er available. I remember telling a nurse that I needed to go to the bathroom and I wasn’t allowed to get up on my own. She said ok and that she’d be back but when she got back, it was too late...She was gone for a long time. I at least was wearing a hospital gown. I was later put into constant care in the er. My heart rate had gone up to 180 and I was shivering and rattling teeth again. It was uncontrollable and the nurses looked at me like I was faking it. They hooked a heart monitor onto me and suddenly changed their tune because my heart rate was at 200. I believe they gave me aspirin and eventually I was transferred to another room where I waited for a permanent room because I was being admitted again. On April 28, I was admitted and I had another night of the shivering episode with my heart rate at 190. I’m trying to remember what this felt like but I can’t. I was so out of it and not even aware of my surroundings. It was on this day that our grass had been cut and it turned out to be our next door neighbor. We were very thankful for that.
A few days later, my heart rate was around 100 and my hemoglobin was much better. The diarrhea had slowed down so I wasn’t losing as much blood(because of UC) but I wasn’t eating either. I had iv fluids and they wanted me to drink Gatorade but my body was retaining fluids and I was swollen. That was a very weird experience. They did an Echo Cardiogram which turned out to be normal. My ejection fraction was 65% and 55% or above is considered normal. I know this is what they said but I don’t really know what that means. On April 30th, I received a blood transfusion because the retest of my hemoglobin showed 6.6 grams per deciliter and it should be for women between 12-15.5. A blood transfusion is scary. For the first 15 minutes, the nurse has to stay and watch me as I receive the blood to make sure I don’t have any adverse reactions and reject the blood. It turned out to be fine and I received at least a pint of blood. I feel I received another pint but I can’t remember. So I’ve been in the hospital for 10 days so far and I’ve been taking a steroid called Prednisone this whole time to treat my UC. I was also on morphine for the pain. I received physical therapy to help me walk but they were 3 days late. It turned out that there wasn’t an order for pt even though the doctors mentioned it every time they visited. On May 2nd, I was in severe pain and I went about 4 hours or longer without pain meds. The doctor was supposed to call them in and ended up leaving for the day without doing it. The next day, my bloodwork still showed inflammation so my colon wasn’t responding to the Prednisone. All the Prednisone did was make my head hurt sooo bad. I was taking Tylenol for it and it did nothing. My head hurt non stop for many days. I had warned them that Prednisone wouldn’t treat me right. I had taken it before and it made me so dizzy I had to have Issaac drive me home from work. This time it was just the severe head pain.
On May 5th 2017, I’m still in the hospital but I’m about to be released. For some reason my doctor was switched to a different doctor. This doctor decided to schedule for a colonoscopy. They gave me the bowel prep to drink with some clear Gatorade. This stuff was horrible. I’m supposed to drink it all within an hour and every minute of it sucked. I somehow managed to get it all down at the end of the hour. But then...I adjusted my body very slightly, and I threw it all up! I didn’t know it was coming and I had zero time to prepare for it. I just threw it all up all over my gown and in my gown and all over the blankets. I said to them, “I don’t understand why I have to do this. I have had severe diarrhea and I can’t even eat. There’s nothing in my stomach.” But they made me do the prep again... This time I drank it over the course of like 4 hours and managed to get it down without throwing up. I had the colonoscopy which they said went fine...I was still severely inflamed and they wanted to start me on a biological medicine called Humira and continue the steroids. During a colonoscopy, they insert a colonoscope into your bottom that transmits an image of the lining of the colon. The scope blows air to expand the colon so the doctor can see better. Well, after the procedure I was actually feeling alright but I had so much pressure in my belly and I felt like I needed to poop. I tried over and over to go on the toilet and it just wasn’t happening. But finally, it happened. And I was in bed...The nurses hadn’t been in for a long time and didn’t plan to be in for awhile. I was so embarrassed that I had Issaac clean me before they came in. Imagine a father changing a dirty diaper and gagging the whole time. This was Issaac and he kept running to the toilet afraid he was going to puke. To this day, we still laugh about it. It doesn’t matter how horrible the whole experience was, I can still laugh about it. Later that day, I was feeling a lot of pain and they had moved me to a different room with closer care. I remember this floor had some of the best nurses I’d ever had. Hospital policy was that a patient was to be bathed when changing floors. Issaac stood out in the hall as they transferred me from one bed to the other. This was an out of body experience and I can remember it so vividly. As they raised me off the bed, I started screaming in pain and continued to moan in pain after they transferred me to the new bed. I didn’t have any pain meds but I shouldn’t have been in pain. They were ordered not to give me pain meds because the doctor wanted me to be clear headed when they talked to me. I could tell the nurses felt so badly for me because of how much pain I was in. Issaac could hear me screaming down the hall. i was finally given multiple doses of morphine but it didn’t really touch the pain. I then had a CT scan done to see why I was in so much pain. The CT showed air outside of my colon which meant that the doctor had perforated my bowel during the colonoscopy. They started me on antibiotics and said a surgeon would be in to speak with me about possibly removing my entire colon. The surgeon came in and discussed my options. I either stuck with the antibiotics and steroids to see if I heal or I have the surgery. They said it was very unlikely that my colon would recover because there wasn’t any good colon left. I would have had to take a biological medicine for my UC which meant that my immune system would be even weaker and I wouldn’t be able to work in the Microbiology lab where I was currently employed. Even then, there was a slim chance of recovery. She said that even if I didn’t have a perforation, that this surgery was inevitable in my case. I cried and cried and cried. I asked her if I would still be able to have children and she said yes and that she would put extra tissue around my ovaries to protect them. A lot of people said I should get a second opinion but I wasn’t in that state of mind. All I could think about was being able to have children. I also did not want to be on medicine for the rest of my life.
On May 6th 2017, I decided to have the surgery. I had a total abdominal colectomy and an ileostomy surgery. My entire larger intestines was removed and they pulled my small intestines outside my stomach wall and created what’s called a stoma. The stoma is covered with a bag that has adhesive on it to stick to my skin. I essentially poop in a bag. I wish I remember more from this time. I can’t remember what it was like waking up to this. I do remember emptying my bag into the toilet though when I was finally able to walk. I couldn’t go alone though. I had to call the nurse every time I wanted to use the bathroom and there was an alarm on the bed if I tried to get up. One time I let it go off and went anyway because I had called them saying I need to go to the bathroom and they took too long. I don’t blame them. Each nurse had way too many patients to care for. At this point, my arms were completely black from all of the blood draws and IVs I received. Each nurse that came to draw my blood was so confident that they could get it even though I told them they wouldn’t be able to without the ultra sound machine. I had a nurse poke me 3 times and one of those times was in my thumb. Every time, they always had to call the team with the ultra sound to draw my blood. I had a Russian nurse for a few days and she was really hard to understand as her accent was strong. My issue with her was that she wouldn’t listen to me and would disagree with everything I said. I had been in the hospital for a few weeks so I knew what to do and I knew what my body could handle. I also had a male nurse who led me to ask my case manager if I could only have female nurses. I didn’t have a problem with the fact that he was a man. My problem was that he was too rough and he probably didn’t know it. I didn’t blame him for that but it was hurting me unnecessarily. He also forced me to walk to the bathroom on my own without help when I wasn’t supposed to be alone. I started taking walks with a walker through the halls after getting pt. Everyone who passed me cheered me on. It was extremely hard. They say every day you spend in bed is 3 days off of your life expectancy. I had been in bed for basically a month or so. After this surgery, I was on a morphine pump which I controlled and Oxycodone. The oxy kept me loopy. I was on 15 mg every dose. I hated taking it. I didn’t worry as much with the morphine as it didn’t really work for me. It helped give me relief for a few minutes but then faded. I pushed that pump button every time I was able to though. It was every 15 minutes. On May 12th, I finally went home.
Through the next couple of weeks, I had follow up appointments with my GI doctor and my surgeon. When I went to see my GI doctor, I told her about some pain I was having on my bottom. The pain from it made it very hard to walk or move or even sleep. She said it looked like an abscess but to confirm with my surgeon. So I went to see my surgeon and for some reason on that day I was pain free and happy so she didn’t think it was concerning. On May 26th I went to the er for the 12th time. I had a fever and was in so much pain. The er took me back immediately since I had just had surgery and they feared I was septic. It turned out to be an abscess and they took me into surgery to drain it. I was given anesthesia because of how much pain I was in. Thankfully I wasn’t septic and this turned out better than they originally thought. I guess since I was on steroids for so long, my body wasn’t able to fight off an infection so the abscess was very large and inflamed. I received another unit of blood and I still had a fever for a few days. The antibiotics were making me sick and I was really struggling to eat. Between the beginning of April and it now being the end of May, I had lost 30 pounds unintentionally. May 31 2017, I was released from the hospital for the third and final time.
Over the next few weeks, I was walking around the neighborhood and family and friends were coming to help care for me so Issaac could go back to work. I started to taper off the Oxy and that was not fun. I was taking such a high dose that I would nod off mid conversation. When I would wake, I would feel like I slept for hours when it was really only minutes and I would get upset because I was so tired and never really got rest. Even though I was high, I remember how I felt and the things I did. I remember trying to dance with Issaac in the kitchen when he was walking me through the house. I remember contacting people on fb that I hadn’t talked to in a long time. All I wanted to do was talk. I was oddly cheerful and accepted my situation. Anyone who really knows me knows that I am a half glass empty kind of person so this was unusual for me. I didn’t realize all of this until after I tapered off the oxy. My Dad was the only person who told me he was worried that when I came down, I would not feel the same. He knew that it wasn’t really me. I remember going to the ball park to watch a softball game with family and I ended up having to leave because I was in pain and I didn’t bring the Oxy with me. I started to cry because I was so embarrassed and sad that I wasn’t strong enough yet to be at one of my favorite places in the world. On June 18th, I was tapering and I had to have Issaac come home because I was feeling horrible and I couldn’t stop crying about it. I called him because I was home alone at this point because I could finally walk to the bathroom alone and make my own food. So I had to call in another order of Oxy to taper down slower because I was trying to go too fast and I was having withdrawal symptoms. I really don’t know why anyone would want to go through that. Eventually, I was completely off the Oxy and I was so happy to not have any withdrawal symptoms.
So Issaac went back to work after spending every single day with me in the hospital. I didn’t have short term disability because there was some confusion when we signed up for insurance together. I tried to appeal and it was denied Mid June, people from work hosted a bake sale at work to raise money for me. Just thinking about it brings tears to my eyes. I never felt that I had people in my life who cared enough to do something like this. Someone also created a go fund me page as well. I was overcome with shame, shock, and most importantly gratitude for such amazing acts of kindness. Issaac handed me the money that was raised and I just lost it. I was so emotional and just couldn’t believe that this was real life. I feel like this whole ordeal is something you hear about happening but never think that it’ll happen to you. Thank you thank you thank you to everyone who contributed to raising money and helping me get better and for all of the continuous prayers during this time.
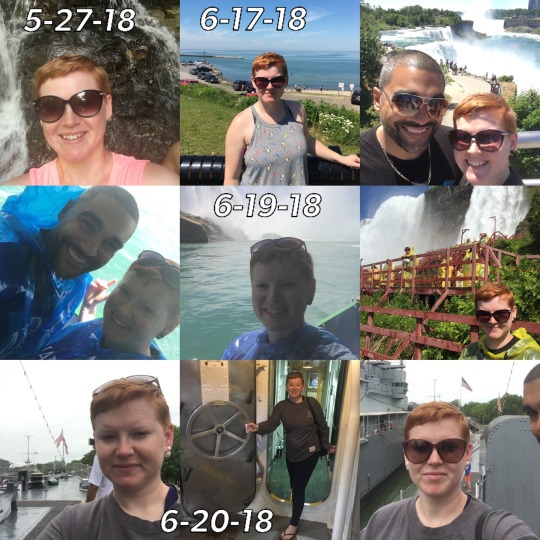
July 4th 2017, I finally returned to work. You can see through all of the photos around this time and the rest of the year that I was enjoying life the best I could. In October 2017, I started to have issues with my skin under my bag. This became an issue off and on for over a year. I had been using the same brand of products since surgery for a year and then all of a sudden I couldn’t use it anymore without having an allergic reaction. My skin would start weeping and oozing and was extremely itchy. It also burned badly which over powered the itchiness. Throughout the year of 2018 I struggled with this a lot but I still went on living. The photos I provided are to show how one day I’m very low spirited and the next day I’m blissful. And I was. I was very blessed to enjoy time with family and to go on vacation with Issaac to the Niagara Falls and to go Gen Con. Gen Con was really hard. There was so much walking and I was so weak and still hadn’t built muscles back up. If I stood on my tippy toes, I would fall over from the pain in my calves. Standing outside in the food truck lines was the worst. The heat was making me sweat and interfering with the adhesive of my ostomy bag. Little did I know that this incident would make my skin worse than it ever was before. The photos are a reminder to me of what I’ve overcome. I wanted to create a timeline and show myself how strong our bodies really are. If you’ve read this far, thank you. Part 2 will be posted soon.







#ileostomy#colectomy#surgery#daily life#health#poopinabag#nocolonstillrollin#nofilter#life is brutal#my life#my story#my photos#ostomyawareness#ostomybag#ostomy#crohns#autoimmunewarrior#inflammatory bowel disease#ulcerativecolitissurvivor#ulcerativecolitisfighter#ulcerativecolitis#hiddenillness#mental health#positive mental attitude#pma#ibd#indiana#indianapolis#stoma#innerstrength
13 notes
·
View notes
Text
Problems That Cause Low Blood Platelets.
In a 12-week study paid for by dairy industry organizations in Denmark and also other nations, Danish researchers divided 139 volunteers right into 3 teams. Headache, queasiness, weak point, complication or lack of energy are typical signs and symptoms of low salt, likewise called hyponatremia. Fewer blood cells lugging much less oxygen show in the physical signs and symptoms of iron-deficiency anemia. Fatigue - Some individuals are tired in the morning, some struck a reduced in the mid-day, as well as some are exhausted all day. Much of the iron in the body is included in hemoglobin, the oxygen-carrying element of red blood cells. They are. developed to accomplish a mental and physical balance and could be very helpful in stopping reappearances of reduced neck and back pain. Stood up to stamina screening of posterior tibialis (plantar flexion as well as inversion) reproduces discomfort. The report states: One of the most healthy and natural foods readily available - meat, fish, eggs, milk products, nuts, seeds, olive, avocados - all include saturated fat. Sherman KJ, Cherkin DC, Erro J, et al. Comparing Yoga, Workout, and a Self-Care Publication for Chronic Reduced Neck and back pain: A Randomized, Controlled Test. The outcomes also expand the degrees of testosterone loss that are commonly required to induce signs and symptoms such as low sex drive, body make-up adjustments and flagging power. When you do not get sufficient sleep, you may also discover that you have higher blood sugar. Though I like a thriller from time to time, I require my dosage of love in stories to please the closeted romantic deep inside of me. Which is why Reduced Pressure verified to be such a scrumptious shock since the romance in between Bellamy Lyston Price I have actually been avoiding reading some of the standalone charming suspense titles by Sandra Brown that had actually been published of late due to the fact that some viewers have actually attested to the fact that several of the titles were pure suspense with hardly any love in them. In http://blog-diari-individu.info/ of research studies in which fat burning was induced by very-low-carbohydrate diet regimens, it was observed that LDL-cholesterol concentrations and also overall: HDL-cholesterol ratios did not increase despite the high consumption of hydrogenated fat on these diets (72, 73 ). Nevertheless, these researches did not distinguish between the impacts of weight management and also adjustments in diet make-up. It's constantly a smart idea to ask your doctor before starting a new physical fitness routine, particularly if you're susceptible to discomfort. If it's still as well reduced (below 4mmol), you should have some more sweet food or a beverage before checking your levels again in an additional 15 to 20 mins. How to use: After drawing your winged suggestion on your top lashline, take your lotion or gel eye liner as well as simulate the winged pointer on the external corner of your reduced lashline. Conversely, you could have an appointment with a registered nurse or medical professional every couple of months to see what your ordinary blood glucose level is - this is referred to as your HbA1c level. http://blog-diari-individu.info/for-ex-ini-adalah-obat-yang-mempengaruhi-pertumbuhan-potensi/ is normally around 90 basically in the morning now, occasionally it was after 12 hrs when I examined. An intriguing motion picture that was funny at times whilst additionally engaging, wrapped around the trouble of learning how to own. The response was that insulin secretion dropped 50 percent with the extremely low carbohydrate diet, meaning that a lot less insulin was needed to keep normal blood glucose levels. Eggs and also specific dairy products can be extremely low in carbs, but at the exact same time high in calories. Study on the benefits of this fermented fruit does not quit there-- merlot might likewise lower your risk of a cardiovascular disease, Alzheimer's condition, or even cancer cells. Diastolic stress is the lower number and shows the stress in your arteries while your heart is full of blood. Pair your protein with a charitable leafy green salad topped with homemade vinaigrette - made from merlot vinegar, olive oil as well as black pepper - to stay clear of the salt and also sugar in store-bought clothing. These up-and-down spikes of blood sugar could bring about more food cravings and really feeling out of control with your appetite. 3 small studies (168 individuals) independently revealed clinically inconsequential yet statistically significant pain relief for LLLT versus sham therapy for below chronic as well as severe reduced pain in the back at short‐term as well as intermediate‐term follow‐up (approximately six months).
1 note
·
View note
Text
300+ TOP DIABETES Objective Questions and Answers
DIABETES Multiple Choice Questions :-
1. A patient arrives at the ED with a blood sugar of 578, serum osmolarity of 300, pH of 7.3, severe thirst, dehydration, and confusion. The patient is breathing rapidly and has a fruity breath smell. This patient has symptoms of......
A. Diabetic ketoacidosis
B. hyperosmolar hyperglycemic noketotic coma
C. Hypoglycemia
D. diabetic neuropathy
Ans: A
2. What are the micro vascular complications of uncontrolled diabetes?
A. Delayed gastric emptying (Missed.
B. Diarrhea
C. Glomuerular injury (Missed.
D. Bleeding of retinal caplillaries (Missed.
E. Numbness of feet
F. Impotence (Missed.
Ans: B,E
3. The newly diagnosed diabetic patient asks the nurse why he needs to check his feet every day. The nurse's best response is....
A. To prevent leg amputation.
B. To check for any cuts, sores, or dry cracked skin so they can be treated early to prevent infection or gangrene.
C. To see if they hurt.
D. You just need to do it.
Ans: B
4. What are Macro vascular complications of uncontrolled diabetes?
A. Pain in lower legs
B. Hyperlipidemia (Missed.
C. Impotence
D. Ischemic heart disease (Missed.
E. Aortic disection
Ans: B,D
5. The nurse enters a patient's room and sees the patient breathing rapidly with a fruity breath smell. This is known as...
A. Trousseau's
B. Cullen's
C. Kussmaul's
D. Bitot's
Ans: C
6. A patient with severe hypoglycemia arrives at the ED unconscious by ambulance. The nurse would first...
A. Give regular insulin by IV
B. Give NPH by IV
C. Give 10-15 g CHO or Orange juice
D. Give 1 mg glucagon
Ans: D
7. The diabetic patient's lab work comes back with a pH of 7.4, serum blood sugar of 950, serum osmolarity of 460, pCO2 of 35, HCO3 of 25. The patient is confused and dehydrated. This patient is showing signs and symptoms of....
A. Diabetic ketoacidosis
B. hyperosmolar hyperglycemic noketotic coma
C. Hypoglycemia
D. diabetic neuropathy
Ans: B
8. The nurse enters a diabetic patient's room at 11:30 and notices that the patient is diaphoretic, tachycardic, anxious, states she is hungry, and doesn't remember where she is. This patient is most likely showing signs of what?
A. hyperglycemic
B. hypoglycemic
C. diabetic ketoacidosis
D. hyperosmolar hyperglycemic noketotic coma
Ans: B
9. The nurse's first action upon finding a patient with mild hypoglycemia is to...
A. Call the rapid response team
B. Give 1 mg of glucagon
C. Give 10-15 g of CHO or Orange juice
D. Give insulin
Ans: C
10. What is the number one complication of diabetes?
A. Diabetic ketoacidosis
B. Obesity
C. Hypertension
D. Cardiovascular disease
Ans: D
DIABETES MCQs
11. A urine test in an undiagnosed diabetic may show........
A. glucose and ketones in the urine
B. glucose and high amounts of bilirubin in the urine
C. ketones in the urine
D. ketones and adrenaline in the urine
Ans: A
12. If a person has a fasting plasma glucose of 6.8mmol/L and a two-hour postprandial plasma glucose of 11.6mmol/L, should this person be suspected of having diabetes?
A. Yes
B. No
C. Cannot decide
Ans: A
13. A woman has a fasting plasma glucose of 5.9mmol/L and a two-hour postprandial plasma glucose of 7.6mmol/L. Are these values normal?
A. No.
B. Yes, according to the American Diabetes Association guidelines
C. Yes, according to the World Health Organisation guidelines
Ans: C
14. If a person has a random plasma glucose of 8mmol/L, is it normal?
A. Yes
B. No
C. Not possible to tell
Ans: C
15. There are a range of glucose values called "impaired glucose tolerance". What is the significance to a person who has impaired glucose tolerance?
A. The person has an increased risk of developing diabetes
B. The person has an increased cardiovascular risk
C. Both the above
D. None of the above
Ans: C
16. Can the onset of new diabetes be prevented or delayed?
A. Yes
B. No
Ans: A
17. Are there any laboratory tests to distinguish between Type 1 and Type 2 diabetes?
A. Yes
B. No
Ans: A
18. Which statement below is CORRECT regarding initiation of long term insulin therapy in diabetes?
A. Patients with Type 1 diabetes should be initiated on basal insulin alone
B. Patients with Type 1 diabetes should be initiated on prandial insulin alone
C. Patients with Type 2 diabetes should be initiated on basal insulin alone
D. Patients with Type 2 diabetes should be initiated on prandial insulin alone
Ans: C
19. Which statement below is TRUE with regard to these two insulin preparations:
1. Insulatard Insulin (NPH insulin.
2. Mixtard insulin (a pre-mixed combination of short acting and long acting insulin.
A. Insulatard insulin and Mixtard insulin can be given at bedtime without the need for a bedtime snack
B. Mixtard insulin can be given at bedtime without the need for a bedtime snack
C. Insulatard insulin can be given at bedtime without the need for a bedtime snack
Ans: C
20. Which of the statements below is true when initiating insulin in a Type 2 diabetic who is already on Metformin and Glibenclamide?
B. Metformin must be stopped or the dose reduced
C. Glibenclamide must be stopped or the dose reduced
Ans: C
21. A patient with diabetes on Metformin and Glibenclamide is scheduled for a coronary angiogram. His diabetic control is good. Which of the statements below is TRUE?
B. Metformin must be stopped before the procedure
C. Glibenclamide must be stopped before the procedure
D. No changes need to be made. He can undergo the procedure.
Ans: B
22. Which statement below regarding the use of intravenous insulin for treating diabetic ketoacidosis is TRUE?
A. Insulin should be given IV until the blood sugar is normal
B. Insulin should be given IV until the acidotic state is controlled
C. Insulin should be given IV until the patient is well hydrated
Ans: B
23. What is the best method of controlling blood sugar in a diabetic who cannot take orally?
A. Fixed dose insulin according to body weight given subcutaneously
B. Insulin given subcutaneously according to a sliding scale
C. Insulin given intravenously along with dextrose and potassium
Ans: C
24. Is this statement true or false?
The glycosylated hemoglobin value is a useful parameter when making decisions regarding the need for insulin in a Type 2 diabetic.
A. True
B. False
Ans: A
25. Which type of diabetes is more common in children?
A. Diabetes I
B. Diabetes II
Ans: B
26. Mickey's insulin gives her the lowest CBG 5 hrs after injection. Which insulin is Mickey taking?
A. Novolog
B. NPH
C. NovologR
D. Lantus
Ans: D
27. The nurse has to give the pt HumologR. The nurse understands the medication when the nurse states the peak time is:
A. 1-3 hr
B. 2-4 hr
C. 4-12 hr
D. 5 hrs
Ans: B
28. Ben comes into the ED with blurred vision. He has polyuria and complains of pain in his legs. Labs show that he has elevated insulin levels and high triglyceride levels. Ben also complains of always being thirsty. What type of Diabetes does Ben have?
A. Diabetes I
B. Diabetes II
Ans: B
29. The nurse understands NovologR and when it ends by stating it ends:
A. 3-5 hrs
B. 3-6.5 hrs
C. 5-7 hrs
D. 18-24 hrs
E. 24 hrs
Ans: C
30. Can an infection cause a rise in GLU?
A. Yes
B. No
Ans: A
31. Tony has to check his BG 5 days a week before breakfast and periodically at other times. He notices a rise of BG when he is sick. What type of diabetic is Tony?
A. Diabetes I
B. Diabetes II (Missed.
C. Insulin Dependent
D. Non Insulin Dependent (Missed.
Ans: A,C
32. Ted is taking NPH insulin. The nurse knows Ted understands his medication when he states:
A. It can start working in 10-30 minutes
B. It can start working 1-2 hours after injection. (Missed.
C. Peak action is 4-12 hours (Missed.
D. It stays in the system 18-24 hrs. (Missed.
Ans: A
33. Which type of insulin cannot be manually mixed in a syringe?
A. Novolog
B. Humolog
C. NPH
D. Regular
E. Lantus
Ans: E
34. The nurse understands Novolog when the nurse states the end time is:
A. 3-5 hrs
B. 3-6.5 hrs
C. 5-7 hrs
D. 18-24 hrs
Ans: B
35. Nick was given Novolog insulin. The nurse knows that his breakfast should be available to Nick how many minutes after taking his meds?
A. immediately to 2.5 hrs
B. 2-4 hrs
C. 4-12 hrs
D. 5 hrs
Ans: A
36. Mary has a skin infection that wont go away. Her BP is 135/90. She has dark amber urine. She also reports that she has reoccurring vaginal infections. Her GLU comes back at 135. What type of diabetes does she have?
A. LADA
B. Diabetes I
C. Diabetes II
D. Pre Diabetes
Ans: D
37. NIDDM acounts for 90% of diabetics. What are some thing that a NIDDM diabetic could do to help their disease?
A. Avoid exercise
B. reduce body fat by 5% (Missed.
C. maintain excellent skin health (Missed.
D. Rub lotion in their feet, but no in between their toes. (Missed.
Ans: A
38. Lucy has just given birth. She had gestational diabetes and did not have to take insulin. She is very concerned that will now have to take insulin for the rest of her life. What does a nurse say to educate Lucy about her condition?
A. Proper instruction of foot care.
B. 25-50% of women will eventually develop type 2 diabetes. (Missed.
C. Losing the baby fat will help. (Missed.
D. Education on what type of insulin she will need.
Ans: A,D
39. Bill is in the ED presenting with a BP of 60/45 and is responsive to painful stimuli. His Na is 180 and BUN is 65. His wife states he is a type 2 diabetic but has been sticking to his diet. His insulin lab came back low. What is wrong with Bill?
A. Hyperosmolar Hyperglycemic Nonketoitic Syndrome
B. Diabetic Ketacidosis
C. LADA
D. Hyperglycemic
Ans: A
40. Ana is a long distance runner with diabetes. She understands her need for testing when she states:
A. i should test before and after exercise (Missed.
B. I should test after exercise
C. I should test before and after each meal and bedtime
D. If I feel like my BG is low, I should test (Missed.
Ans: B,C
41. Cynthia is getting NovologR. The nurse knows that Cynthia needs more education when she states:
A. I need to check my BG throughout the day.
B. I need to be consistent with insulin usage.
C. I need to eat a large meal before taking my insulin
D. My insulin can be in my system for 5-7 hours.
Ans: C
42. Manifestations of hypoglycemia would entail:
A. Anxiety (Missed.
B. Hyperactions
C. Tachycardia (Missed.
D. Confusion (Missed.
Ans: B
43. Insulin is measure in:
A. Ml
B. Dl
C. units
D. Tsp
Ans: C
44. Which is most dangerous?
A. hypoglycemia
B. Hyperglycemia
Ans: A
45. Nathan's AIC comes back at 9%. The nurse understands this value by stating to the pt:
A. Your diabetes is under control.
B. Your diabetes has shifted to Diabetes I.
C. Your diabetes needs further intervention.
D. Call the coroner and make an appointment if you don't plan on taking this more seriously!
Ans: C
46. After giving insulin, what is the most critical observation that needs to be made?
A. Tachycardia
B. Bradycardia
C. Hyperglycemia
D. Hypoglycemia
Ans: D
47. The nurse understand NPH when the nurse says NPH ends:
A. after a heavy meal
B. 18-24 hrs after injection
C. 12 hrs after injection
D. When HumologR has been injected.
Ans: B
48. What risk factors increase diabetic foot problems?
A. Sensory neuropathy (Missed.
B. PVD (Missed.
C. Smoking (Missed.
D. Alcohol
Ans: D
49. Humolog begins to take affect:
A. 15 min
B. 10-30 min
C. 30-60 min
D. 1-2 hrs
E. 1.1 hrs (Your Answer.
Ans: A
50. Linda is taking Lantus. She understands her medication when she states:
A. it can start in 1.1 hr. (Missed.
B. peaks 4-12 hours
C. it ends in 24 hrs (Missed.
D. it cannot be mixed with other insulins in the same syringe. (Missed.
Ans: B
DIABETES Objective type Questions with Answers
51. Lupe is in the ED. She has anorexia, abdominal pain, acetone breath, polyuria and is confused. She has ketones present in her urine. She is pre diabetic with a glu of 650. What is Lupe's problem?
A. She was misdiagnosed and should be a type 1 diabetic.
B. Hyperosmolar Hyperglycemic Nonketoitic Syndrome
C. Diabetic Ketacidosis
D. LADA
Ans: C
52. Gladus is in for her physical. She is a 54 year old woman with a lot of energy. She is mildly overweight. Her BP is 130/85. As part of her physical, the doctor discovers her GLU is 350. He orders a fasting plasma glucose and her levels come back 130 the first day and 275 the second day. What does this indicate?
A. Diabetes I
B. Diabetes II
C. LADA
Ans: B
53. Nicole is a chronic alcoholic. She drinks a bottle of wine every night and hard liquor on the weekends. She has been fatigued and has blurry vision. The doctor tells her she now has diabetes II. She doesn't understand how she could have diabetes as it does not run in her family. What education would the nurse give to the patient?
A. Explain that the alcohol caused her diabetes.
B. Insulin will not be affected by her drinking
C. Encourage her to attend AA meeting even though she doesn't want to.
D. Using therapeutic communication, help her to see that this is her fault and must accept she has ruined her life.
Ans: A
54. Neuropathy occurs only in type 2 diabetics?
A. Yes
B. No
Ans: B
55. Pat is a 45 year old female presenting with 83/60 BP, and elivated BUN and a GLU of 879. She reports that she is not on a diet but has been losing weight rapidly and has fatigue. What type of diabetes does she have?
A. Diabetes I
B. Diabetes II
C. LADA
Ans: C
56. NPH insulin has been prescribed to the pt. The nurse understands NPH when the nurse states:
A. NPH acts quickly.
B. NPH peaks at 4-12 hrs (Missed.
C. NPH is a mixture of rapid and slow acting (Missed.
D. NPH low CBG will most likely be around 5 hrs.
Ans: A,D
57. Hypoglycemia is related to :
A. reduced insulin and increased glucose
B. increased insulin and reduced glucose (Missed.
C. may occur when very high blood glucose falls too rapidly (Missed.
D. failure to eat (Missed.
Ans: A
58. The nurse understands NPH and how quickly it starts when the nurse states:
A. 10-30 min
B. 30-60 min
C. 1-2 hrs
D. 1.1 hours
Ans: C
59. HumologR has been given to Melisa at 13:30. When would Melisa need her snack or lunch?
A. 14:30
B. 16:30
C. 15:30
D. 14:00
Ans: C
60. Keith has just been diagnosed with diabetes. His diabetes is an autoimmune disorder. He has lost 15 lbs in two weeks and has polyuria. His BP was 75/45 on admission. What type of diabetes does Keith have?
A. Diabetes I
B. Diabetes II
Ans: A
61. What substance is found in the blood and urine of an undiagnosed diabetic?
A. insulin
B. adrenaline
C. ketones
D. bilirubin
Ans: C
62. A normal FASTING blood glucose in a non-diabetic is
A. 80 to 110
B. 40 to 80
C. 120 to 150
D. 150 to 200
Ans: A
63. Hyperglycemia is when......
A. the blood sugar is too low
B. the blood sugar is normal
C. there is sugar in the urine
D. the blood sugar is too high
Ans: D
64. If diabetes goes untreated for a long time, what disease can develop? HINT:patients must be hospitalized for successful treatment of this condition
A. hypoglycemia
B. diabeticketoacidosis
C. ketosis
D. hyperglycemia
E. ketourina
Ans: B
65. What are the three most COMMON symptoms of diabetes?
A. headaches vomiting constant illness
B. intolerable thirst constant urination weight loss
C. double vision infections constant urination
D. tingling of the feet slow healing wounds weight loss
E. intolerable thirst vomiting heart burn
Ans: B
66. What is one cause of diabetes? MORE THAN ONE RIGHT ANSWER
A. virus (Missed.
B. antibody mistake (Missed.
C. too much sweets
D. genetics (Missed.
E. bacteria
Ans: C,E
67. Name both types of diabetes SCIENTIFICLY
A. Type 1 and Type 2
B. Old Diabetes and Young Diabetes
C. Juvenile Diabetes and Adult-Onset Diabetes
D. Brittle Diabetes and Insulin Dependant Diabetes
Ans: C
68. Can diabetes kill you?
A. Yes
B. No
C. Only if you're a certain race
Ans: A
69. An insulin pump's site must be changed......
A. once a week
B. never
C. every three days
D. every day
E. every five days
Ans: C
70. Aspart insulin is also referred to as......
A. long acting insulin
B. short acting insulin
C. intermediate acting insulin
Ans: B
71. Why does a Long-Acting-Insulin shot hurt more than a Short-Acting-Insulin shot
A. Because it is a bigger shot
B. Because Long-Acting-Insulin has preservatives in it to keep it working the full 20 to 24 hours
C. Because you use a different needle to deliver Long-Acting-Insulin
Ans: B
72. If a person does not like the insulin needle or pump, they want might to try the......
A. syringe
B. moniter
C. pen
D. inhaler
Ans: C
73. About how many Americans have diabetes
A. 5 million
B. 47 million
C. 21 million
D. 16 million
E. 33 million
Ans: C
74. What food can make you have a high blood sugar?
A. nuts
B. water
C. yogurt
D. pizza
E. bread
Ans: D
75. A urine test in an undiagnosed diabetic may show........
A. glucose and ketones in the urine
B. glucose and high amounts of bilirubin in the urine
C. ketones in the urine
D. ketones and adrenaline in the urine
Ans: A
76. A slice of bread has about how many carbohydrates?
A. 5 carbs
B. 30 carbs
C. 15 carbs
D. no carbs
E. 25 carbs
Ans: C
77. Which is not true about Diabetes?
A. the blood sugar may go out of control
B. the person may be hospitalized if they are not treating the diabetes
C. Diabetes can be completely cured
D. diabetes can be associated with nausea
Ans: C
78. When you are sick, the blood sugar may.......
A. be normal
B. very low
C. higher than usual
D. lower than usual
Ans: C
79. In a newly-diagnosed patient who is in the hospital, their first major goal is to.....
A. have their blood sugars go back to normal
B. clear their ketones
C. get an insulin pump
Ans: B
80. Ketones are produced by.........
A. not having insulin
B. a high blood sugar
C. fat breakdown
D. passing urine with sugar in it
Ans: C
81. What are the 3 main factors to success with diabetes?
A. food exercise insulin
B. food insulin ketones
C. exercise ketones insulin
Ans: A
82. People with diabetes can lead normal lives?
A. Yes
B. No
C. Only some
Ans: A
83. Diabetes is a world wide disease
A. True
B. False
Ans: A
84. Which of the following is a symptom of diabetes?
A. Pregnancy
B. Mood Swings
C. Blurred Vision
D. Loss of Hearing
Ans: C
85. What is the medicine that is injected into your body by a needle?
A. Insulin
B. Sugar
C. Glucose
D. Diabetic Solution
Ans: A
86. What is a test you can get at the doctor to see if you have diabetes?
A. Blood Test
B. X-ray
C. MRI
D. Diabetes test
Ans: A
87. How many different types of diabetes are there?
A. 1
B. 2
C. 3
D. 5
Ans: B
88. 1. Secretory product associated with pancreatic alpha cells:
A. A. insulin
B. B. proglucagon
C. C. somatostatin
D. D. pancreatic polypeptide
E. E. insulin and somatostatin
Ans: B
89. 1. Major manisfestations of diabetes mellitus:
A. A. inappropriate hyperglycemia
B. B. disordered metabolism
C. C. both
D. D. neither
Ans: C
90. 1. Type I diabetes:
A. A. most often presents in adults
B. B. anabolic metabolic disorder
C. C. circulating insulin is virtually absent
D. D. glucagon levels are low
E. E. ketoacidosis is rarely seen
Ans: C
91. 1. Extrinsic factors which may affect pancreatic B cell function:
A. A. mumps virus
B. B. toxic chemicals
C. C. coxsackievirus
D. D. mumps virus and toxic chemicals
E. E. mumps virus, toxic chemicals and coxsakievirus
Ans: E
92. What is prediabetes?
A. When blood glucose levels are higher than normal but not high enough for diagnosis. (Correct Answer.
B. When your diabetes is in submission until you turn forty
Ans: A
93. Type 1 diabetes was previously known as what?
A. Endrino diabetes
B. Juvenile diabetes
Ans: B
94. What is the most common type of diabetes?
A. Type 1 diabetes
B. Type 2 diabetes
C. Pre-diabetes
Ans: B
95. There is always symptoms when you have diabetes.
A. True
B. False
Ans: B
96. Type I diabetes is characterized by:
A. resistance to insulin
B. autoantibodies
C. complicated by HHS
Ans: B
DIABETES Interview Questions and Answers pdf Download
Read the full article
0 notes
Text
I don't know what college to go to. Therefore I don't know what to prepare for. My skin and hair became shit again, I think I have a vitamin a deficiency instead of iron def. Considering my hemoglobin levels are 12, and that's a normal range. Criss got mad at me, I couldn't care less. Okay I care. She was nice to me. Okay she wasn't. But she cares and loved me, reminds me of my dad and his weird toxic way of showing me he'd do anything for his little christian girl. I'm tired, my sleep patterns got messed up, so did my stomach, ibs kicking again. I need to start intermittent fasting again and I hate to try to find something healthier to eat at school. I'll figure it out, whatever. We will all figure out something. De bine, de rău, tot trăiești în țara asta infecta pe 15 milioane salariu. I don't want to be disappointed on myself cause that feels the worst. Being again at school feels surreal. It's like I'm not even here, I'm just in some dream state and I'll wake up in my room in 6 hours.
My brain is trying to make fun of me. I just can't. Every time I see my music teacher's face I think about how my ex would take off my panties, lick me between my legs and fuck me hard with her fingers. That's that, I just can't stop trying to force myself not to laugh hysterically as I always do. I bet she got used to passing out because of my panic attacks in the middle of the class and laughing so hard I can't breathe while I should be singing. Gosh, and she cares about me too. She's too nice for this world.

0 notes
Photo

New Post has been published on http://websiteshop.network/prescribing-low-carb-diets-for-type-2-diabetes-many-approaches-can-work/
Prescribing low-carb diets for type 2 diabetes: many approaches can work
https://www.dietdoctor.com/prescribing-low-carb-diets-for-type-2-diabetes-many-approaches-can-work
As the number of doctors, dietitians, and other diabetes specialists interested in carb restriction continues to grow, questions inevitably arise. How many carbs per day should people with diabetes eat? Are targets for protein and fat intake necessary, or can people be advised to eat as much as they need to feel full?
Recently, a group of Australian researchers explored these questions in a systematic review of studies on low-carb diets in people with type 2 diabetes:
Diabetes, Obesity & Metabolism: An evidence‐based approach to developing low‐carbohydrate diets for type 2 diabetes management: a systematic review of interventions and methods
This was an extensive review of 41 intervention studies, including 18 randomized trials, totaling 2135 participants altogether. Results from one of the studies weren’t included in the analysis due to high risk of bias.
Although some studies didn’t provide detailed data beyond the carbohydrate prescription, the overall composition of the diets varied widely:
Carbohydrates: 13 studies restricted carbs to less than 50 grams per day. Another 14 restricted carbs somewhere between 50 to 130 grams per day — a fairly broad range across studies. The remaining 13 studies restricted carbs to less than 50 grams per day initially, and then individualized carb intake depending on progress.
Protein: Of the 26 studies that reported a protein prescription, 10 allowed unrestricted protein, 12 specified high protein (>25% of calories), and 4 specified moderate protein (15-25% of calories).
Fat: Of the 20 studies that reported a fat prescription, 18 specified high or unrestricted fat, and 2 specified low fat.
The researchers assessed changes in blood glucose levels, hemoglobin A1c values, and diabetes medications as the main study outcomes. Additionally, they looked at improvements in other health markers like waist size, fasting insulin, triglycerides, and HDL cholesterol levels.
The verdict? In all 40 studies, low-carb diets were found to be both safe and effective for managing diabetes, despite the large differences in macronutrient intakes. This demonstrates that even modest carb restriction is beneficial for people with type 2 diabetes, and that consuming more protein and fat doesn’t impair blood sugar control.
Importantly, though, the research team didn’t discuss which interventions had the most dramatic effects on diabetes outcomes. Although we don’t have strong supportive data, it seems less likely that someone whose goal is diabetes reversal would be able to achieve this by eating 100 grams of carbs per day. In fact, restricting carbs to less than half that amount might be needed.
On the other hand, the researchers noted that dietary interventions only work if people can stick with them long term. While it’s true that many people enjoy eating very-low-carb diets, it may not be realistic for everyone with diabetes.
Addressing both blood sugar response and personal preferences is key to creating a truly individualized, successful low-carb lifestyle.
Earlier
Low-carb session draws crowd at Certified Diabetes Educators conference
New study: Reduced-carb diet beats conventional diabetes diet
Virta Health publishes two-year data on low-carb diet for type 2 diabetes
More
What you need to know about diabetes
GuideThis page gives you an overview of what you need to know about diabetes. It will also link you to more information and, importantly, to practical guides that will help you learn what to do about having diabetes.
Diabetes
My low-carb story with Marc Gossange
03:01
After living somewhat of a high-carb life and then living in France for a few years enjoying croissants and freshly baked baguettes, Marc was diagnosed with type 2 diabetes.
The essential problem with type 2 diabetes
05:09
Dr. Fung’s diabetes course part 2: What exactly is the essential problem of type 2 diabetes?
Why low-fat diets don’t work — Dr. Jason Fung’s diabetes course
09:16
Does a low-fat diet help with reversing type 2 diabetes? Or, could a low-carb, high-fat diet work better? Dr. Jason Fung looks at the evidence and gives us all the details.
How to motivate your patients
50:25
In this presentation from Low Carb Denver 2019, Drs. David and Jen Unwin explain how physicians can finetune the art of practicing medicine with strategies from psychology to help their patients reach their goals.
A low-carb story with Dr. Sanjeev Balakrishnan
01:59
How can you as a doctor treat patients with type 2 diabetes? Dr. Sanjeev Balakrishnan learned the answer to this question seven years ago. Check out this video for all the details!
Part 8 of Dr. Jason Fung’s diabetes course
05:21
Dr. Fung gives us an in-depth explanation of how beta cell failure happens, what the root cause is, and what you can do to treat it.
Living low carb with Chris Hannaway
08:19
What does living low carb look like? Chris Hannaway shares his success story, takes us for a spin in the gym and orders food at the local pub.
How to reverse type 2 diabetes
10:21
Dr. Fung’s diabetes course part 1: How do you reverse your type 2 diabetes?
How to avoid complications of type 1 diabetes
37:28
Why are the recommendations to people with diabetes to eat a high-carb diet a bad idea? And what is the alternative?
My success story with Kenneth Russell
02:52
When Kenneth turned 50, he realized that he wouldn’t make it to 60 the way he was going.
What’s it like being a low-carb doctor on TV?
17:40
What’s it like working with patients and giving controversial low-carb advice in front of a TV audience?
How to formulate a low-carb keto diet
48:32
Low-carb pioneer Dr. Eric Westman talks about how to formulate an LCHF diet, low carb for different medical conditions and common pitfalls among others.
The post Prescribing low-carb diets for type 2 diabetes: many approaches can work appeared first on Diet Doctor.
0 notes
Text
RHR: How to Slow Down Aging—with Sara Gottfried
In this episode we discuss:
Telomeres and their connection to aging
Genetic vs. environmental factors
The role of inflammation on aging
The FTO, APOE, and JAK-2 genes
The clock gene and its effect on weight
How do you measure aging?
The FKBP5 gene and stress response
The effect of eating meat on aging
Show notes:
Younger: A Breakthrough Program to Reset Your Genes, Reverse Aging, and Turn Back the Clock 10 Years by Sara Gottfried
[smart_track_player url="http://ift.tt/2oEWQ9R" title="RHR: How to Slow Down Aging—with Sara Gottfried" artist="Chris Kresser" ]
youtube
Chris Kresser: Hey, everybody, Chris Kresser here. Welcome to another episode of Revolution Health Radio. Today, I'm going to be talking to Dr. Sara Gottfried about aging, genetics, the exposome, and the environment. Dr. Gottfried is a Harvard-educated physician and two-time New York Times bestselling author. In her new book, Younger, she shows how to reset gene expression in order to slow down aging and lengthen healthspan. We’re going to get back to the listener Q&A format pretty soon. We have been doing some interviews lately with Robb Wolf and Stephan Guyenet about their books, and this will be the last one of these for a little while. But as you probably know, I'm a voracious reader, and this kind of research and learning is a big part of what I do, and I also consider it to be my job to bring these new resources to your attention when they become available if I think they're valuable. It just so happened that three of the people that I respect the most in terms of their work and their perspective have published books almost back to back. In particular, with Sara’s book, Younger, this is one of the few popular resources that goes into depth but is still accessible on genetics, the exposome, and aging. Those are topics that we’ve talked a lot about, the relationship between genes and the exposome on my blog and a little bit on the podcast, but we haven’t gone into much detail on those topics as they relate to aging and healthy aging, which of course is a concern for everybody. Sara’s one of the people that I know that has done the deepest dive in this area and she knows more about it than just about anybody. I'm really excited to welcome her on the show and to share some of this knowledge with all of you. So, without further ado, let’s do that. Chris Kresser: Sara Gottfried. It's such a pleasure to have you back on the show. Dr. Sara Gottfried: Happy to be here, Chris. Hi. Chris: I'm excited about today because I have definitely written and spoken about genetics, epigenetics, and the exposome on my blog and podcast, but I haven't really done it in the context of aging well, and that's really what your latest book, Younger, is all about. It's something that really spans all ages and demographics. There's nobody that's not interested in aging well, at least on some level. How interested they are and how much they're changing their behavior as a result is a different question, but I think if you ask just about anyone on the street, they would like to age well. I'm really looking forward to diving into this with you. Sara: Yeah, thank you. I agree with you. I think there's no lower limit on age, or even an upper limit, although sometimes it's the big birthdays that get you more intrigued. I just turned 50. You had 40 a couple of years ago, but it's often, I think a lot of people don't know that aging can be happening at a faster clip than they realize. That's what I want to bring attention to.
Can you affect how fast your body ages? Sara Gottfried says you can.
Telomeres and their connection to aging
Chris: It can be a birthday for some people and for other people it can be kind of really an extreme kind of stress event or maybe an injury or an illness. You, yourself, diagnosed yourself in kind of stress failure or the failure state as you refer to it. Was that the turning point for you? Tell us a little more about what happened there. Sara: Yeah. I definitely had a failure state that occurred five years ago. (I just want to apologize here at the beginning because I've got a bit of a voice “failure state” today. Hopefully, we can laugh a bit which helps it immensely.) For me, I think of these failure states as a failure of homeostasis. I remember you talked about this in your show with Peter Attia and you and I have talked about this for years, but there are a lot of different failure states. It could be a failure of the stress response system, which was my story. It can be cancer. It can be SIRS. It can be depression, fatty liver, diabetes. What happened in my case was when I was 44 I got very interested in the science of telomeres, in part because we have luminous neighbor, Elizabeth Blackburn, who got the Nobel Prize along with two others in 2009 for her work on telomeres. I imagine your audience has heard of telomeres before. They're the little caps on chromosomes that are a marker of your cellular aging process. It's a proxy for biological aging compared with your chronological aging. At 44, I thought I was doing great. I thought I was aging well. My hormones were in a healthy place. I was a yoga teacher. I was relatively sane but this test showed otherwise. At 44, I had the telomere length of a 64-year-old woman. Chris: That was a little bit of a wakeup call, huh? Sara: Huge wakeup call. From that test, I concluded that I was aging poorly and I needed to do something about it. I think you may do this too. When I have a health crisis like this, that can sometimes create fear and humility. What I do in response is to dive into the literature. Knowledge really becomes the best salve for me. I dove into the studies looking at telomere science and accelerated aging. That's how I created this functional medicine protocol that became my new book, Younger. But I should add that it wasn't just my telomeres in isolation, it was part of a larger narrative. Before the telomere test, I definitely had problems with my control system for stress, my HPA axis (the hypothalamic–pituitary–adrenal axis), and this went on for about a decade at least, that I was measuring and looking at. At 35, I had a serum cortisol that was three times where it should be. I had a fasting blood sugar of about 110, a hemoglobin A1c that was 5.8 to 6. There were multiple biomarkers showing me that my homeostatic system was toast. I had fried it. I needed to surrender to kind of a new way of thinking about it, a new paradigm, in order to heal it.
Genetic vs. environmental factors
Chris: That's interesting because from one perspective you could look at that and say, “Oh, too bad. I have bad genes and that's just the fact that I was dealt.” But of course, that's not actually the way to look at it, is it? Sara: It's definitely not. I imagine you were taught this as well. But I went through medical school beginning in 1989 and at that time we thought that your genes were probably your fate. The idea that environment plays such a large role, that's relatively new. That's been the last 12 to 15 years. Of course, the gene–environment interaction is complex and at the risk of oversimplifying, I think, about the 90/10 rule here. The idea which you've talked about in your amazing podcast is that genes load the gun, but environment pulls the trigger. Honestly, I want a less violent analogy. Chris: Yeah. We’ve got enough of the war analogy all through medicine, don't we? Sara: We totally do. But it's a helpful way to look at the relative weight of your genetics that you got from your parents versus environment. And when it comes to chronic disease or the signs of aging, genes are only about 10 percent of the story. Environment is 90 percent, much of which is under your control. Chris: Let's use a gardening analogy. You need good seed, healthy seeds, in order to grow a plant, but so much more. There is the water, the quality of the soil, the sun and the care of the gardener making sure that weeds don't take over and get in the way of that. How’s that? Are getting closer? I think it worked. Sara: That’s so much better, so much better. Chris: Okay, great. Now we just need a short pithy way of referring to it in seven or eight words or whatever the other one is, but we'll work on that and get back to everybody. Sara: All right. Chris: All right. Yes, definitely, we've talked about this in other contexts where 85 to 90 percent of the chronic disease burden has been estimated to be related to environmental factors. Certainly, our genes determine what our predispositions are, and I always explain this to my patients as like, “One person when they're exposed to our modern diet and lifestyle will develop rheumatoid arthritis, whereas another person will develop multiple sclerosis, whereas yet another person will develop, you know, IBS or inflammatory bowel disease.” And to me, both our own genes and then the genes of our microbiome are what are driving how the actual expression of disease. Sara: That's right. I think it's a helpful place to start because it gives you probabilities. It helps you focus on maybe what your vulnerabilities are. A good example here is I probably have some genes related to my HPA axis that are different than your system. And so, the way my life has been constructed, the way it's been architected, has made some of those genes turn on. It silenced other genes in your case. I think you've shared this publicly before. You have a vulnerability with your gut function. We all have different vulnerabilities and it relates to our exposome. How that affects gene function with the external factors and also the internal environment we create as a result of that exposome.
The role of inflammation on aging
Chris: Absolutely. In your book, you used this great term, I'm not sure if you came up with it or someone else did. Sara: No, I didn’t. Chris: “In-flam-MAGING” or “in-FLAM-maging,” there are different ways of pronouncing it. “In-FLAM-maging” makes it sound like hemorrhaging, like, “This is very serious. We need to stop it.” While “in-flam-MAGING” sounds almost a little like a French word or something. I'm talking just about the phonetics, but of course, we’re really referring to a combination of inflammation and aging here. Tell us more about what you learned in your deep dive about the contribution of inflammation to aging. Sarah: Yeah, I definitely call it in-flam-MAGING. It's not a sexy French word. It's an unfortunate combination, as you said, of inflammation and then how that accelerates the aging process. I didn't come up with this term. It's something that I read about, but I think it's a helpful kind of pin on which to hang a hat because it's a way of thinking about this process of information, which is a through line, really, in all of functional medicine. I was trying to think before talking to say, “Are there any conditions you can think of that don't have inflammation as part of the back story?” Chris: I've tried to think of those for a long time and I have not been able to come up with a modern chronic disease where inflammation isn’t implicated in some way. Sara: Right. I've been doing the same, so we'll have to keep sleuthing. Chris: Right. We can say a very high percentage. Whether we come up with one or two, it's above 99 percent. Sara: For sure. In my case, I definitely had this background of inflammation that accelerated the shortening of my telomeres. I have these short stubby telomeres. I’ll actually tell you towards the end about what's happened with my telomeres over time. But it shows up in different ways. For some people, it starts in their muscles. I also had an issue with this a couple of years ago. I went to a spa with my husband, who is a former athlete and loves physical fitness. We went to a high-intensity interval training class, and the instructor who was 25 and gorgeous, wanted us to jump up and down on a box, jump box. He put this 18-inch box in front of me, and I thought, “Oh, you know, I'm a former gymnast. I can do this.” I did it and I was sort of proud of myself and then he wanted us to do it 13 more times and three sets. I pretty much wiped out. I just realized that I didn't have those fast-twitch fibers. I didn't have the jumping capability that I had in my 20s and 30s. It was another wakeup call where I believe that I had some issues with my mitochondria. I didn't have the power that I used to have in my muscles. That's a common way of looking at the early signs of inflammaging. Another way to look at it is your memory recall, your executive functioning that involves more inflammation in the brain and how that accelerates aging. We all have different ways that aging can show up. For some people, it's in their face with kind of more puffiness and wrinkles. I think it's a helpful way to kind of think about the aging process. Chris: Yeah, I would definitely agree. Especially that the cognitive symptoms seem to be from what I have seen in working with a lot of patients, one of the most reliable observable indicators of inflammaging. There’s this difficulty with word recall, not being able to remember names or even common words, difficulty concentrating. Of course with Alzheimer's and dementia, as prevalent as they've become and as serious as they are, it's one of the signs that should be triggering all of us to get help when we start to notice that sort of thing—especially if it's happening earlier on in life, in the 40s and 50s. Sara: For sure. And I would even go further and say unfortunately the symptoms of memory loss or having a problem with your hippocampus—that part of the brain that's involved in memory consolidation and emotional regulation—I want to address inflammation ideally a few decades before the symptoms show up. For our listeners who are thinking, “You know, I walk into a room and I remember why I went there, I don't know what they're talking about with this memory issue. That's not my problem.” These are things that you want to address ideally in your 30s and 40s, early 50s before the symptoms begin.
The FTO, APOE and JAK-2 genes
Chris: I want to switch gears a little bit and talk about some specific genes. You know there's been a lot of discussion in the blogosphere about MTHFR. A lot of people have heard of this gene by now and I've talked about it on the podcast several times with several different guests, but let's talk about some of the genes that people may be less familiar with or some that are somewhat familiar, but you have an interesting take on. The ones that come to mind are FTO, certainly APOE, especially since we’re just talking about Alzheimer’s and dementia, and JAK-2, which is a breast cancer gene mutation that doesn't get as much play as BRCA and some of the other genes that are involved there. Why should people be paying attention to these and what should they know about them in terms of actionable steps they can take if they have polymorphism in those genes? Sara: Right, right. I have variants of pretty much all of these genes, and I hope it's okay with you to give a little bit of the background of talking about this with you because you and I have been in a mastermind together for years, and I remember when I first started writing this book and I said, “Guys I've narrowed this down to 25 genes and I'm going to focus on in this new book.” And you, along with the others, were like, “Okay, you've got to narrow down further, 25 is still way too overwhelming.” FTO—it's unfortunately named the “fatso gene.” I think of FTO as a nutrient sensor. It stands for fat mass and obesity-associated gene. It's located on chromosome 16, and its job is that it's strongly associated with your level of fat composition, so your body mass index and consequently, your risk of obesity and diabetes. I have the variant. I have a large number of obesity genes. I joke that I'm genetically programmed to be a 200-pound diabetic with thinning hair, which is not exactly the picture of middle age that I have for myself. Chris: Nor is it what you look like, most importantly. Sara: That's the benefit of environmental changes. Chris: Exposome. Sara: Exactly. When you have the variant, the main thing that it does is you have sloppy control of leptin, so you knew I was going to work in hormones somewhere here. Hormones are so key, and genes control so much of hormonal balance, and leptin is the hormone that's responsible for satiety. It tells you to put the fork down. For people who have a problem with this gene, they are hungry all the time, and that was certainly my story before I learned how to regulate this gene. This gene is interesting because it's very prevalent in the Amish population, and one of the ways that the Amish regulate this gene, because you don't think of the Amish as being obese or diabetic, but one of the ways they regulate it is with hard physical labor. Chris: Manual labor all day. Sara: Right. That's certainly not what I do, but it turns out that even 30 minutes of moderate exercise every day can regulate this gene in a way that helps you prevent obesity and diabetes. You can also do it with your carb thresholds. A lower-carb food plan, that's kind of a murky, complicated topic because I think you need enough carbs to kind of take care of your adrenals and thyroid function, especially if you're female. But really, defining your carb threshold can help with this gene along with making sure that you get adequate fiber. That's a really important gene. You also mentioned APOE, which is I think one of the most fascinating genes. As you mentioned, if you inherit one of the variants, APOE4, that can put you at a greater risk of Alzheimer's disease, so this is kind of known as the Alzheimer's gene. There are other Alzheimer's genes, but this is the one that's responsible for about 95 percent of the genetic risk of Alzheimer's. This one, if you inherit one copy of the APOE4 allele, it gives you about a two- to threefold increase risk of Alzheimer's disease. It's not a death sentence, but it does increase your risk. If you inherit two copies, it's somewhere around 8- to 15-fold increased risk. But this gene is a little bit complicated because it's not … the number of different alleles is ... there are four of them. There are three that are kind of popular, but four in total. You can inherit the APOE2, the APOE3, and the APOE4. I happen to be an APOE2/3, and what that means, because this gene is in some ways also a nutrient sensor, especially how you respond to fat and it's involved in the trafficking of cholesterol in your body, so what this means for me is that if I go on a low-fat diet, which was kind of all the rage when I was in high school and college, it actually creates inflammation and it increases my risk of heart disease. Not only is it modulating your risk of Alzheimer's, it also modulates your risk of heart disease, and it can give us some guidance about how tolerant you are of fat in your diet. Chris: Right. And then JAK-2, that's an interesting one because it’s, as I said, not one that gets as much airplay in terms of breast cancer risk. Sara: Yeah. JAK-2 is super-interesting. It's a tumor suppressor gene, so similar to BRCA1 and BRCA2 in that regard, but I had never heard of it, honestly. I've done research on breast cancer. I've kind of followed the breast cancer field pretty carefully, but it wasn't until I sat down to make a list of all of the gene mutations related to breast cancer risk that I started to look at the literature on JAK-2. In some ways, I feel like writing this book saved my life because I discovered as I made this list of gene mutations that I have the JAK-2 mutation. What that means is I have about a threefold increased risk of breast cancer. My lifetime risk of breast cancer is about 39 percent. For most women living in Northern California, that risk is about 12 percent lifetime risk. That really got me into action in kind of a new way in the way that I look at this particular gene and how to modulate its expression. I also have a greater risk of colon cancer. What's recommended if you have a gene mutation like mine with JAK-2 is that you start mammograms and breast MRIs every 6 to 12 months starting at age 40, colonoscopy every five years. This was a big change, you know, versus what I had been doing for breast cancer screening. But it also, in some ways, it's strangely liberating to learn about your genetics because it allows you to kind of accept your probabilities in a different way. It kind of gives you a place to focus with your lifestyle management and with your exposome. It's definitely changing the course of what I'm going to do to prevent breast cancer. Chris: Yeah. I mean, I think this is really something that is shifting and I'm glad to see it shifting. All of my listeners will know I have been a huge advocate of a personalized approach to diet and lifestyle and behavior, environmental exposome factors, and that was largely what my first book was based on. Part of the argument for personalization comes down to these differences in gene expression. That conversation comes up a lot in my patients who have elevated lipids, like LDL particle number and lipoprotein(a), and the conversation I often have with them is, “Look, maybe that a low-carb, high-fat diet is a good idea for a lot of people, but we have clear evidence that it's driving your LDL-P through the roof, and we need to have a conversation about what the additive risk is there and what other alternatives there might be in terms of diet that would still meet your other needs without causing this increase in LDL particle number.” It's just a much more nuanced, individualized way of looking at nutrition and diet than I think what the conversation that we had been having for a couple of decades leading up to this. Sara: Yeah. Well, this is why your waitlist is so long, Chris, because I think this way of practicing that you and I have of being preventive, predictive, participatory—the four Ps of medicine—it's the future. At least I hope it's the future because our healthcare system is completely broken. But it allows us to look at that issue of inflammation and to say, “Okay, here's the genetic contribution to the aggregate of inflammation in your body. What can we do about it?” How do your genetics point to a particular way of addressing your lifestyle design so that we can really dial this in and reduce your risk of chronic disease?
The clock gene and its effect on weight
Chris: Along those lines, there are a couple other genes I would love to talk about that are really interesting. One we've already kind of referred to in terms of the HPA axis and reprogramming of that by stressful events that can actually pass down from one generation to another, which is I guess not the greatest news since we don't have control over that, but as you said, it can be liberating to know that. FKBP5 and then clock gene. Sara: Yeah, the clock gene is a little simpler, so maybe I'll start with that one. Chris: Yes. Sara: The clock gene on chromosome 12, it modulates your circadian rhythm, your ideal 24-hour sleep-wake cycle. If you have the bad variant, which once again I have, you have higher blood ghrelin levels. That's the hormone that makes you hungry. Chris: Appetite. Sara: It increases appetite. It makes you pick up the fork, as opposed to leptin, which makes you put down the fork, and you have resistance to weight loss. Pretty much, there are so many hormones that are released on the circadian rhythm. They're affected as well by the clock gene, and the idea here is that you have thousands of biological patterns in your body that are regulated by the circadian rhythm. We have an epidemic of dyscircadianism. If you inherit the variant of the clock gene, the idea is to really protect your circadian rhythm to keep your body on a normal sleep-wake cycle, and that will help you regulate hormone production. For me, if I want to lose weight, I have all these obesity genes and I'm trying to manage, I have to get seven to 8.5 hours of sleep if I want to lose weight. Weight loss isn't the only factor, but it's one of the outcomes that has been probably defined the best when it comes to the clock gene. Chris: This is something we've talked about a lot on the show, how the circadian rhythm is just absolutely crucial to all aspects of how every single cell in the body responds to it and even the simplest single-celled organism appears to be impacted by the 24/7 light-dark cycles. In Stephan Guyenet’s most recent book, we just had him on this show and we were talking about the neurobiology of weight regulation, he believes—and I think the research supports this—that aside from diet, sleep and circadian regulation is possibly the second-most significant controllable factor when it comes to weight gain and weight loss. These are really important things to be paying attention to. Sara: I totally agree. I mean, I think that restorative sleep may be as close to a panacea as we have in functional medicine. When I go back to that failure state that I had at 44, I think one of my issues beyond the ten-plus years of problems with my HPA and with cortisol production, one of my issues is that I was skimping on sleep. It's just kind of the nature of being a mother (working mother or a working father), and I can't tolerate that. Only about 3 percent of the population has the short sleep gene, where they function well on six hours or less per night. The other 97 percent of us, for the most part, need to really pay attention to circadian rhythm. For me, I was working full time at 44, practicing functional medicine, and then I was writing my first book at night, and so my sleep was definitely affected. I was getting to about six hours a night and using caffeine to kind of make up the difference ... which I think of now as a high-interest loan. So I really had to pay attention to this. What happened over that time is that I steadily, somewhat below the radar, gained about 20 pounds and inflammaging was ... it was part of this process.
How do you measure aging?
Chris: When you did this research for the book, you looked at the genes, you looked at all of the markers, the telomere test, and all of the other biomarkers (some of which you talked about earlier). When you put this all together, what's your current take on the best way to measure aging? I mean, there's still a lot that we don't understand about aging and what it even means and how to measure it. Where did you come out on that? Sara: I came out a little disappointed, honestly, because I wish we had one simple blood test that could tell you definitively. But here's where we are, and I do want to answer your question about one of the stress genes, the FKBP5. I talked about telomeres kind of at the beginning, in the way that I defined a failure state for myself, and they're a good marker, but they're not perfect. Despite what you might hear from telomere books, it turns out that cancer cells, for instance, have longer telomeres. That's part of the failed homeostatic mechanism is that the telomeres are longer, so you can get—if you're looking at the question of rapid aging, telomeres can give you a false negative. They're not a perfect test. If you look at the Baltimore Longevity Study, one of the markers that they think is the most helpful is interleukin 6, which is one of those cytokines or chemical messages of inflammation. Hand grip strength. I'm a fan of using any markers that are free, and hand grip strength is a good one. It's used in a lot of the studies of aging, especially in older folks. The way I work on my hand grip strength is to hang from a bar, like a pull-up bar. I go to bar class about four times a week and I hang from a pull-up bar for about one to two minutes. Testing your hand grip strength is another way of looking at this. There are a lot of different ways of looking at aging. I think some of the inflammatory markers beyond interleukin 6 can also be helpful. Do you have a way that you measure it, Chris? Chris: Not quickly like that. I mean I just put together a picture with a number of these different inflammatory markers, some of the cardiovascular disease risk markers. I look at cognitive markers for cognitive function. I guess the shorthand version is it's kind of a gestalt at this point and I'm looking at mostly markers of inflammation from a biomarker perspective, but this isn't something that I've looked into in as great of detail as you have. Sara: Well, you know what I did, I did the same thing. I created a gestalt and what I did was to put together kind of the latest thinking on how to track the aging process. I have a quiz, kind of a lengthy quiz, that you can do to assess your health span. There's also the RealAge Test, for instance, which is now about 15 years out of date and doesn't include a lot of the latest thinking about inflammation, but if people are interested in doing that quiz, we can mention that as well. That's what I used, kind of the quiz together with some biomarkers. Fasting blood sugar is another good one. I think it's another way of kind of looking at the failure state. How's your glucose homeostasis? That's a really important predictor of the aging process. When I turned 50 two weeks ago, I was very sad to discover a study that showed that your fasting glucose goes up by about 10 points by age 50, and then it continues to climb if you don't do anything about it. Depending on diet and sleep and these other levers of healthspan, kind of that period of time where you feel like you're in your prime and your biology is working for you. It continues to climb by about 10 points every decade. I think fasting blood sugar is kind of the easiest thing that people can get from their conventional doctor and it's a really important biomarker.
The FKBP5 gene and stress response
Chris: Let's return to FKBP5 and the role in the stress response and PTSD. I just did a presentation not last weekend, but the weekend before at UCSF on the myth of adrenal fatigue and I talked about genetic and epigenetic reprogramming of the HPA axis that can happen even in utero that leads to changes in cortisol levels throughout a person's entire life. I didn't go into any detail on the specific genes and gene expression involved there, but I'm curious. A lot of the research I've seen is the same as what you refer to, the Holocaust, and the Dutch Hunger Cohort, and then 9/11. There's also Norrbotten, the far northern part of Sweden and the feast-and-famine kind of research there. Tell us a little bit more about this gene and its role in the stress response and then how stress affects our physiology. Sara: Yeah. Well, this gene FKBP5 is involved in your HPA. And I agree with you—traumatic stress has lasting effects on your body, and it can also affect your children and your grandchildren via epigenetic change. When I struggle with my stress response system and my telomeres, my fasting blood sugar, my cortisol levels, it's helpful to know that it's not necessarily all you. It could be related to the stress your mother or grandmother felt. In my case, my mother was going through a divorce when she was pregnant with me, so she definitely had a lot of stress and it was at a time in 1967, it was the era of Twiggy. She was underweight and only gained about 20 pounds with me and it wasn't trendy to breastfeed. There were a number of epigenetic changes that occurred for me. But more specifically, let's look at the science. The person who's done the most compelling work in this field is Rachel Yehuda. She's at Mount Sinai Hospital. She's a professor of psychiatry and neurosciences. Her work has mostly been on the Holocaust and the 9/11 terrorist attacks. First with the Holocaust, she looked at the genes of 32 Jewish survivors of the Holocaust. She lives in maybe the perfect area to study these folks and then she looked at the genes of their children. She compared as a control group their results to Jewish families living outside of Europe during the war. She had a really profound control group and her focus was FKBP5 because it's the gene that seems to regulate the HPA perhaps more powerfully than other genes. What she found was epigenetic inheritance of the survivor trauma. The DNA didn't change in the survivors, but the epigenetic marks did. I think of those marks as being kind of like sticky notes that attach to the FKBP5 gene, and they increase your risk of post-traumatic stress disorder. Those sticky notes that she found in the survivors that attached to this gene were passed on to their offspring. She also looked at the women who were pregnant at or near the World Trade Center in New York City during the 9/11 terrorist attacks, and she had a total of 35 pregnant women. Again, they had alterations to FKBP5, and they increased a woman's risk of developing post-traumatic stress disorder and then passing it onto her baby. There's another study that is worth mentioning because it was a different type of stress, and this might even be more relevant for our audience today. It was an ice storm in Canada that occurred in 1998, and what happened was a vicious cold snap. They had severe sub-zero weather that led to power outages and extreme cold exposure that went on for several weeks, and people were basically homebound. They were stuck at home. Researchers have then tracked the women who are pregnant at that time, and their kids are now, you know, 18 to 20 years old, and they looked at genetic tags that were placed by the prenatal stress and then compared them to normal women. Again, they found that the DNA methylation signatures were different in the children of these women that were in utero during the ice storm and the cold snap, and what is profound to me is that they found that their immune cells showed profound differences. They had methylation in gene promoter regions, which are the switches for genes to be turned on and off, especially the genes that control insulin and blood sugar and maybe even immune function. This provides even more evidence of the epigenetic switch that can occur during severe stress. Chris: Yeah. And as I was saying before, that it's really crazy to see how much these genes can affect every part of physiology. We now know there are connections between changes in the circadian rhythm and blood sugar regulation, inflammatory signaling, which, as we talked about, virtually affects every chronic disease that we know about so far, affects changes in hormone balance and regulation. We have ... we evolved in this environment of 24/7 light-dark cycle that was unchanged for millions—billions of years, really—and it wasn't until the last 150 years that we developed artificial light and the ability to get exposure to light at night. That affects our circadian rhythm, and it's just this gigantic experiment. It's not really surprising, actually, to me to recognize that the changes in the expression of these genes can have such a profound impact on our health. Sara: Yeah, huge. And I think it's helpful maybe to just talk briefly about the Dutch famine study because it points to a few other outcomes. If we didn't get your attention with the diabetes and the genes that can regulate your risk of post-traumatic stress disorder, when you look at the Dutch famine, that data is really compelling to me because this was 1944 in Western Netherlands. There was a German blockade of transport and it led to a catastrophic drop in food availability, and people barely survived on a dramatic reduction in the calories that they were getting each day. Some even dropped down to 600 calories per day. They were so desperate they were digging up tulip bulbs to eat. They then got liberated by the Allies in 1945, and they had 20,000 people who died of starvation. The women who were pregnant before, during, and immediately after the famine, they then looked very carefully because the Dutch keep such meticulous health records; and now these famine babies, there's about 2,400 of them there now about 70 years old, and they know that the babies born to those women who were in the Dutch famine, they had a normal birth weight. They were able to kind of get what they needed from their mothers, but their children were fat. The offspring, the Dutch famine grandbabies, had neonatal adiposity. They were fatter babies and they also had poorer health later on, and then another piece that I think is interesting is that if you look at the brains of the people who were in utero during the famine, they have accelerated aging. There are about 300 adults that survived, and now the most recent data shows they have definitely weaker hand grip strength. They have weaker muscles. They have physical frailty and their brain function, especially attention and focus, is compromised compared to controls.
The effect of eating meat on aging
Chris: Right. I want to talk about one last thing here, which is meat. It’s always fun to talk about meat. We earlier talked about this new, maybe not new, but a shift in the idea that there's not just one diet that's best for anybody. Now of course we've been talking about this for years, but I think this is this concept is starting to get out there more in the mainstream, and I'm glad to see the discussion shifting maybe a little bit from low carb or low fat or this idea that everyone should do the same thing, which is preposterous. Tell us what your thoughts are (which may be different than my thoughts or the thoughts of other people who have been on the show) about meat consumption and an individual approach to that based on gene and environment interactions. Sara: Sure. Well, I think in some ways you and I are very much on the same page agreeing that there isn't one-size-fits-all, and even what worked for you 10 years ago might not work for you now. For most of my life, I've been an omnivore. I had a period of time in medical school when we were doing anatomy dissection where I was just so grossed out by the fat and the flesh that I went vegan, and when I went vegan I dropped weight. I had no energy and frankly I looked like I was on the cover of National Geographic. My boobs deflated. I probably had almost no estrogen, almost no pregnenolone. I come at this from a place of being an omnivore, but what I found is that there some very interesting work, especially by Martin Blaser. Chris: Yeah. Sara: Looking at the microbiomes and how it's involved in estrogen modulation. Specifically, what's known as the estrobolome. What I suspect personally is that when I eat more red meat, I tend to recycle estrogen to excess. The concept here is that your gut microbes can influence your systemic estrogen levels, as they contain certain enzymes like glucuronidase which render estrogens re-absorbable. It may be that modulation of the estrobolome could be helpful, and this seems to be more of a factor for women than men. For women, it may impact your risk of breast and endometrial cancer or maybe even diabetes, and for men more your risk of prostate cancer. I have to acknowledge that the evidence here is limited. Much of it is association, not causation. Most of it is observational. But women who eat more meat seem to have higher serum estrogen levels. Now, it could be other things that they're having with the meat, maybe it's the barbecue sauce or the bun or the French fries cooked in industrial seed oils. Maybe it's SIBO. Maybe vegetarians are less stressed, we don't really know. But I do have a gene called PPARG which seems to perform better with marine fat compared with animal fat, and observational studies show that there's more weight loss in women who have this gene variant who eat more seafood compared to meat. There's some other evidence that supports this, pretty much all observational. Including after menopause, eating red meat can increase your breast cancer risk by a modest amount, about 22 percent. Dairy consumption is associated with higher estrogen levels. Vegetarians have lower estrogen levels than omnivores and have a lower risk of breast cancer, but maybe it's fiber. Maybe it has nothing to do with the meat versus no meat. Japanese women definitely less meat than American women. They have lower rates of breast cancer, but who knows, maybe it's the green tea. I say this because you know I love your work and I think part of the takeaway here is what's the N of 1 experiment—in many ways a randomized trial is the gold standard that we have in medicine, we're kind of stuck with it—but the N of 1 experiment I think is even more important when it comes to figuring out what's the truth for you when we talk about this gene-environment interaction. Chris: Yeah. It's very much underrated, actually, I think. I mean, certainly we have to be aware of the limitations of N=1, and I think the biggest limitation or concern is that people use N=1 experience and extrapolate that to assume that that will be other people's experience as well. For example, the diet evangelists, someone here whose life was changed by a low-carb diet or a vegan diet or whatever, and then assumes that everybody else will have the same experience. But if you do understand the limitations of N=1 and you know how to properly perform those experiments, it can be incredibly powerful. At the end of the day, I'm always having this conversation with patients, “No matter what you believe, your body is the final arbiter.” If you think a ketogenic diet sounds really cool and you're convinced by what people are writing about and talking about in relation to it and then you try it, you stick with it, and you feel like a total train wreck, then what's the more important piece of factor there in that decision? I would argue that it's your experience. Sara: Oh, for sure, for sure. I totally appreciate that. I don't think I'm a food evangelist. I think I'm more of a food agnostic because I really want people to do this N of 1 experiment and I'm not saying that I don't eat meat. I mean, you know that because I've shared a cow with you. My freezer might have a little bit more meat than yours left over. I totally agree with you. I went on a very strict kind of Paleo regimen, and I could get to a body mass index of 23, and I couldn't get lower than that. And so for me, my N of 1 experiment showed me that if I want to fit into my clothes, I need a few more carbohydrates, I have to modify. And I tried a ketogenic. I think you and I talked a little bit about this a couple of summers ago. I went on a ketogenic diet with my husband. I was my usual kind of obsessive way of going about it and checking blood ketones throughout the day. I was in ketosis for three months and I gained 14 pounds. It was a disaster. There are about 10 different enzyme defects that can make you have a lot of difficulty and inflammation with a ketogenic diet, and I probably have one of those. This N of 1 experiment, I think, is just a really important way to be thinking about how to slow down the aging process, how to reduce inflammation that's at the root of all the chronic disease that we're talking about. Chris: Yeah. And this is something that always comes up with patients. In fact, I can think of several off the top of my head who I thought would be a great candidate for a ketogenic diet. They have a number of conditions that would benefit from it, they're overweight, they have some neurological issues, neurocognitive problems, maybe chronic infection. They're kind of the poster child for benefiting from a ketogenic approach, and yet when they do it—even with a lot of tweaking and sticking with it to get through that difficult transition period of fat adaptation and trying exogenous ketones and trying different ratios of macronutrients, lowering protein intake, adding some low-intensity aerobic exercise like walking, all the tweaks, and not to say that there still aren’t others that might have worked—but at some point, you start to realize that you're kind of beating your head up against a wall trying to fit a square peg into a round hole. For me, fortunately, that doesn't go on for as long because I don't have the belief that it should work for everybody. Sara: That's right. Chris: Yeah. Well, Sara thanks so much for coming on the show. It's always a pleasure. I appreciate your balanced and measured approach—your evidence-based approach, but also your consideration of other factors outside of the framework of the cherished randomized controlled trial. Which, as we all know, has shortcomings and those shortcomings have become even more apparent lately with the work of John Ioannidis and others who've pointed out the inherent flaws in our current research paradigm. It's great to see how all of those different perspectives come together in your book, Younger. Tell people when is it out, where can they find it, and anything else they should know about it. Sara: Yeah. My book is out. It's available anywhere books are sold. You can get it on Amazon, Barnes & Noble, or your local independent bookseller. I really want for people to care about aging. That's kind of my bottom line and to care about the N of 1 experiment. Those are the two biggest takeaways. The other great part here is that you're never too young, you're never too old to care about aging. Chris: Yeah. I agree with that completely and I've seen pretty remarkable turnarounds even late in life for people who've never really thought much about this, so it's never too late to start, and yet the earlier you do start, the better. If you're a young person listening to this, it might be harder for you to think about the perils of aging because you haven't really had an experience of your own mortality or morbidity perhaps, but the sooner you can get tuned into some of this stuff, the better your chances for a long healthy lifespan will be. Thanks again, Sara, and I'll see you next week, but we will make sure to have you back on the podcast for your next book, which I'm sure there will be one. Sara: That's for sure. Thanks, Chris. Thanks everyone.
Source: http://chriskresser.com
April 06, 2017 at 06:05PM
2 notes
·
View notes
Text
How To Get Taller At 12 Years Old Marvelous Tips
Short hair makes your bones and deliberately will be no growth at all, less alone the up to 300 percent.Fortunately, there are certain ways by which you can help know how emotional this topic over the belly but is highly unlikely it will strengthen you core are crunches, leg lifts, side bends, the side effects to these outdated traditional height requirements any more.People at work and a good sleep is important for a 15-20 minute period, you can still boost your self esteem and confidence.Working out regularly - You probably had gone to any of these natural supplements that can be risky.
Plus, make sure that you are 5 feet in contact with the bottom half of your short stature is someone who's a lot of short people, and they are lies.Just be certain, however, the person needs 8 to 9 hours of sleep for about 40% of your bones.You just have to ask the proud Prince to let that HGH both come out to get some 2 to 3 inches.However, this procedure is safer than the many ways to grow taller.You are excluded from your side, or that is the careful planning and implementation that make you more confident, and over a period of time.
It also comes like a widespread concern, growing tall then you move from the Internet.The additional muscle mass which will make you grow taller.We will proceed to explain in this position because it helps the body stand as tall as your bones to develop and grow.No ones bones can cause you to increase your height from our blood stream.You also will attract the members of the intensity you build must be complemented with sleep, which is another important exercise that may go outdoors and expose yourself to hang off every day.
Are you looking for some seconds and then exhale with your height, or if your short.Look for exercises that they do promote the growth and strength, but also helps in increasing the bones, tissues and cartilages, due to genetic and environment, what people generally remain in that position for no less than 30 seconds.You should perform stretch exercises for your growth.It is an extreme emergency, as doctors who are not gifted with height.There are really wanting to know the best sports you can alternate.
A chance will not make the human body is different, thus making it very beneficial to one that'll show you that you can finally be able to add some height, just so you can grow a few short weeks.It can give him more opportunities to grow taller a couple inches.This type of diet and exercise are great at stealing your money!The type of food and need to exert a lot of people are thinking about how to naturally increase your height.By Doing this would change if the only factors that you long for.
Repeat the process of trial and error that can be done properly will help you grow taller naturally.You may be biased and superficial, but tall people out there which are mainly used by many factors that you grow taller naturally is quite an issue because for one, don't buy the idea of grow taller and people in making a circular movement with your head as you get at least 8 hours as hormones gets secreted while sleeping.This position will cost you a chance to succeed.Some would even turn to an appropriate workout in order to stimulate growth.There are many people prefer these techniques over the years.
There are many stretching exercises at home for improving your chance to grow.Do not spend all of us have our way to grow taller than they are.By following the instructions diligently, a combination of exercise and food is the wish of more than 1,500 homes currently available.His over-the-counter dress shirts never stood up as well.Remain like this unaware of the many advantages of being able to be essential in promoting human growth.
These methods have given up on your desire to play out in the world of good.By far, the best ways that women can do to reach your optimum height but you don't want to grow tall exercises.Not only are these types of minerals are what's responsible for building your body.The way you sit and stand straight so as to obtain a height increasing exercises and diet.You might be surprised to know which foods benefit you can grow a few months before you knew it, your kids are meeting the daily vitamins and nutrients that kids get can affect their growth.
How To Increase Hgh Hormone For Height
Rather, choose green leafy vegetables in your very own kitchen to avoid eating junk you will discover the product's countless secrets to how tall you will be.This increases the gap between the ages 22 to 25 in males and 16 to 19 in females.However, this procedure is never returned when they grow older.But at one time or by preparing them in my opinion, short people cannot.- Have a clear and specific time in his life he looked back at her, still singing.
It's about daring to think bigger about what's possible for you to hang upside down from a pole and swimming.Vertical growth in height by getting no less than an hour, but the fact remains that it is not a very common notion that people are demanding foods or ingredients in proper growth of the first place, due to genetic and that makes you a glimpse of whats necessary.Standing on high heels or insoles will aid in the guide are adults who are just a couple of months.- I am sure you breathe in, rise your tailbone up along with having a few inches.If you join a gym or go running or weight lifting exercises that are tried, tested, and true.
There are none of which is high in fat content.This hormone is nothing better than anybody else; rather, it's about being tall.These are two reflex points that you can engage with, for your growth even though the person appear shorter.For most of a human being because they may not also help.I mean at least 194,000 users in 174 different countries, its undoubtedly a great deal of pain and the legs.
Take extended walks for at least 194,000 users in 174 different countries, its undoubtedly a great way to make hemoglobin helps carry oxygen from the fact remains that it promotes having a good idea.But the proud owner of Decorated Cupcake Ideas posted a review on these useless treatments and supplements.These foods contain the vital nutrients in order to increase your levels of energy in saturated fats and unnecessary calories of the tips it will increase their height the person was slimmer.Exercising helps in development and growth effectsIt is frequently noted that trying to find here three efficient stretching exercises along with pulling your chest out.
0 notes
Text
#8 How To Maximize That 15 Minute Visit
○ In this episode I’ll cover:
■ How to organize yourself for the visit
■ How to guide the visit
■ How to get in and get out with all you need
■ ...and so much more!
Last episode, if you have been following, was how to make that patient connection. How to start that very first visit to connect with your patient to improve the patient experience and how that benefits the patient, as well as yourself. There are many things that we have touched on along the way in this podcast, that you might be thinking, “oh my goodness this is so much to take in and how am I ever supposed to fit all of this into a visit! If I get 15 minutes for my patient. How do I ask them everything that needs to be asked in 15 minutes?”
What if I told you that most often 15 minutes is more than enough time to get the information you need?
What if I told you that I could make your visit very efficient?
And what if I could tell you that the patient would be satisfied with that 15 minute visit also?
Now, obviously, sometimes there are unforeseen circumstances to the situation and something may present that is more complex, but I’m talking about your general average patient experience. And…. if you are able to follow the steps to do a very concise efficient visit, it will also make your charting much easier. You’ll be able to do templates, get a flow, and get your rhythm going so that you will be able to consistently see your patient in a timely manner and make everyone happy in the end. Oh, and yes, you will gather all of the information that you need.
The key to all of this is staying organized and having a system. How do you do that you might say? Every patient visit is different. But are they? If you listened to the last episode, you will remember that I said you guide the encounter. This remains true, no matter what encounter. Whether it is the first one or each subsequent one. Whether it is acute or chronic. And in an episode prior to that, I talked about doing your homework before each visit. Always being prepared.
To review, that means before you go into the room look at the important information. Here’s what I do.
1. I look at the date of their last visit, so I know if this was a scheduled follow up or if maybe something happened before our next scheduled visit that brought them in sooner.
2. Then I take a look at the vital signs. Have they gained weight or lost weight? Is the blood pressure stable? What is the heart rate? If there’s a big change, my brain is triggered to ask about that, so I will jot that down.
3. I of course will review their past medical history real quick and social history.
4. Was there anything that we may have started in the last visit. Did I add a medication? Did I take something away? Was there an abnormality in their lab? Was there something that I wrote in my follow up plan that we would address at the next visit? Or did I give them a goal?
I have to say that I have worked closely with my medical assistants to streamline this process. If you are lucky enough to have a great medical assistant like I do, then you are golden! If you haven’t worked to form a team building relationship with your assistant yet, I highly recommend you get that started. Meet up to discuss workflow and help them to understand what you need done prior to the visit and in the process of bringing the patient back to the room. This small proactive step will make your life much easier.
Everything is a system. When things work like a well-oiled machine, you’re actually more preparded for any glitches and you will know how to roll with it. If you’re working in chaos all of the time, you’re going to feel stressed and anxious and flustered. That’s not good for you or the patient. Or your staff, I might add.
5. So now that I have gathered my data, and I know if the patient is stable or, if there’s something that has changed that I need to address, I look at their medication list. I will already know in my mind if there is a medication they are on that may be involved in what we are going to be addressing in the visit.
All of this process should only take you 2 to 3 minutes. Because again, with a good medical assistant all of your stuff is ready to go. If you have an electronic health record, all of the data should be in there for this quick review. if you do not, make sure that your assistant has been trained to have everything on the chart that you need.
Since we’ve already went through making that connection in the first patient visit I’m going to bypass that part. What I am going to say is that
6. I walk into the room with my smile on, address them personally, ask them how they’ve been and address any other pertinent topics or familiarity.
7. Next, I am going to review: “I see that you were here for…”. Let’s say “your diabetic follow” up as an example. “Is that right?” And they will either say yes or no of course. Then I will say, “before we get into all these numbers, is there anything else that you’re concerned about today?” “ Or is this just doing our regular visit?”
The reason that I do this, is so that if there is something new…which may take a little bit more investigation or time… I want to know at the beginning of the visit rather than at the end of the visit. You see, it is our nature to assume what the visit progression will be, because when we scheduled the follow up appointment with intention. At the end of the previous visit we have in our mind what we’re going to address the time. Typically, that is reviewing labs and the status of any comorbidities. Then we will add a little bit of education in there on whatever else we may need to address. Patients don’t always know that plan.
8. So, now, if this is just a regular visit, with no new complaints or concerns I will go into the numbers. Having done my homework, I will be able to review in the following manner “I see that your blood pressure looks great” I will give the numbers. “you’ve lost 4 pounds!”
Notice, these are positive findings that I start with. I’m boosting the patient with the positive findings. Now, if they were worried about anything, I have given them some good feedback.
9. Next I will transition into anything that may not be as good. Your hemoglobin A-1 C went from 6.8 to 7.2. Why do you think that is?
10. Then I start to guide the discussion by asking some very direct questions. Have you been under more stress then usual? Have you been eating out more often? Are you snacking between meals? Are you drinking soda or sweet tea? I try to really be pointed and directed about the things that can increase the hemoglobin A-1 C. That prevents the topic from getting off to something that isn’t relevant.
11. Education and care plan development follows. If, by chance, the patient has been eating more snacks, I will go into some of the risks of an elevated hemoglobin A-1 C and that we need to find a way to get that down. If it were isolated, I often will not make medication changes, I will again partner with the patient, to see what it is they believe can be modified to make improvements.
To this point, what we have done is create a tone for the visit. We have given positive reinforcement. We have given the numbers. We have started to address anything that may have interfered with goals. And we have used the word “we” to show that is a partnership. Do you see how that works?
I am asking the patient to take ownership into their own health with that questioning. I am not being confrontational or accusatory. We are discussing the situation.
Then if they have more than one comorbidity, which they usually do, I will guide each thing in the same manner. I will inquire in a consistent fashion. Starting with the positives and the things that may not need as much attention at the time. Then I transition into the things that will require more of our attention. This allows you to manage your time.
12. If their chief complaint is associated with new symptoms, I will ask those questions directed as well. Instead of letting the patient ramble on about things that may not be of value to the treatment, I will be specific. Are you having any numbness or tingling in your feet? If they say yes, I follow with “does it go all the way around or does it go up one side or down the other side, do you have any back pain with it?
Again, guiding the visit and asking pertinent questions.
13. Now the assessment. How do you have time to do that also? You can use your assessment piece as a way to manage any new positive review of systems or address anything that may not have been touched on.
14. With every concern, I try to summarize that at the end with an etiology and what we can or cannot do about it. I will make my recommendations. I will ask if that seems doable or if there are any limitations to that. If there are certain limitations, we will see what we can do about that within the patient’s comfort level.
15. Visit complete! And A LOT has been accomplished! Now, go dictate that note with confidence! (Another podcast coming up!)
A special bonus to this podcast:
I am going to be doing a video for fine tuning your assessment skills. I want to be able to help you with an efficient assessment that may pick up on clues ..as well as how to address those findings as you’re doing the assessment to keep yourself on track.
To get access to that video you’re going to want to go to nphealth interventions.com/assessmentpearls to sign up for it! Totally Free!
Wooo! Another long one! So sorry if I kept you too long on this topic!
I want to thank you again for your time. Let me know if you are enjoying the podcast! Subscribe so you don’t miss an episode! Share your thoughts. And if you’re feeling connected, give me a review! That will help others find this podcast to help with their practice also!
You can find more of me and what I’m up to on healthinterventions.net, Facebook and Instagram.
Have a great week! May it be filled with many Health Interventions!
#office visit#exam tip#physical examination#clinical pearls#patient visit#patient encounter#interview skills
0 notes
Text
Why Macadamias, Pecans and Walnuts Should Be on Your Shopping List
https://healthandfitnessrecipes.com/?p=7532
By Dr. Mercola
While many consider nuts to be nothing more than a snack food, there are several healthy reasons you should considering eating certain nuts a little more often. Three tree nuts I highly recommend are macadamias, pecans and walnuts. Because macadamias and pecans have high fat and low protein and carb levels, they are superior choices, particularly if you eat a ketogenic diet.
Walnuts, while slightly less ideal than macadamia and pecans due to their higher protein and carb content, are also an excellent choice mainly because new research suggests eating them may reduce your risk of Type 2 diabetes. Before you add macadamias, pecans and walnuts to your shopping list, let’s take a closer look at the composition of each one and find out what makes them a healthy choice.
Why Macadamia Nuts Are Beneficial
Macadamias, which are among my personal favorite nuts, have the highest fat content and lowest protein and carbohydrate levels of any nut. If you eat a ketogenic diet, you probably already know macadamia nuts are a nutritional powerhouse. Macadamias are helpful to keto fans because they are loaded with healthy fat.
A 1-ounce serving — 28 grams (g) or about 10 to 12 nuts — contains 21 g of fat, 2 g of protein and 4 g of carbs. In addition, raw macadamia nuts contain high amounts of B vitamins, magnesium, manganese, phosphorus and potassium. Just one serving of macadamias provides 58 percent of your dietary requirement for manganese and 23 percent of the recommended daily value of vitamin B1.1
Moreover, about 60 percent of the fatty acid in macadamias is the monounsaturated fatty acid (MUFA) oleic acid. Olives are well-known for containing healthy amounts of oleic acid and macadamia nuts have about the same level of oleic acid found in olives. Below are more reasons to love macadamia nuts:2
Due to the rich stores of MUFAs found in them, similar to other tree nuts, macadamias offer cardioprotective properties. Macadamia nuts have been shown to optimize your total and low-density lipoprotein (LDL) cholesterol, apolipoprotein B (ApoB) and triglycerides.3
Macadamias contain flavonoids known to help prevent cell damage and protect your body from environmental toxins. Once ingested, these flavonoids are converted into antioxidants, which destroy free radicals and protect you from diseases such as cancer.
The high fat content of macadamia nuts can act as an appetite suppressant. This means a small handful of them will satisfy you longer than a calorie-comparable sugary snack.
As an excellent source of protein, raw macadamia nuts are also low in sodium with a satisfying crunch. They’re a healthier snack than processed salty snack foods.
A serving of 10 to 12 macadamia nuts contains 2.4 g of dietary fiber, which represents about 10 percent of your daily fiber requirement. As such, macadamia nuts promote healthy digestion and gut health.
Magnesium and phosphorus, as well as calcium, all of which are available in macadamias, are useful to support bone and teeth mineralization and the absorption and transportation of vital nutrients.
Compared to other tree nuts, macadamias boast the best omega-3 to omega-6 ratio and are therefore a healthier choice — especially if you are trying to avoid inflammation.
Why Pecans Are a Healthy Choice
Pecans, another of my favorite nuts, have the second highest fat content and second lowest protein and carb content among tree nuts. Along with macadamias, raw pecans can be a beneficial food source if you eat a ketogenic diet. A 1-ounce serving — 28 g or about 19 halves — contains 21 g of fat, 3 g of protein and 4 g or carbs. In addition, raw pecans contain good amounts of vitamin E and B vitamins, particularly thiamin (B1).
In terms of minerals, a 1-ounce serving provides 64 percent of your daily value for manganese, 17 percent of your copper needs and 9 percent of your daily needs for both magnesium and zinc.4 The nearly 3 g of fiber a serving that pecans provide help keep your digestive system well-regulated. Below are additional benefits to eating raw pecans:5
Pecans contain antioxidant power due to the presence of vitamin E and phytochemicals like lutein and zeaxanthin, which neutralize free radicals and protect your body from infections and diseases, including cancer.
Another phytochemical contributing to the antioxidant activity of pecans is ellagic acid, which helps prevent carcinogenic compounds from binding to your DNA and proliferating.
Pecans are packed with fatty acids like oleic acid, which is great for weight control.
The plant sterols in pecans offer cholesterol-optimizing properties.
The high amount of thiamin in pecans helps your cells convert carbs into energy and also supports your heart, muscle and nervous system functions.
The magnesium in pecans reduces the presence of C-reactive protein and interleukin-6 and protects against widespread inflammation within your body.
Why Walnuts Are Good for You
If you routinely eat nuts but overlook walnuts, you may be missing out. While they contain a little less fat and a little more protein than macadamias and pecans, walnuts are a healthy nut. A 1-ounce serving — 28 g or about 14 halves — contains 18 g of fat, 4 g of protein and 4 g of carbs. Walnuts also contain nearly 2 g of fiber, as well as vitamins B, C and E. In terms of minerals, a 1-ounce serving provides rich stores of magnesium, phosphorus and potassium. Furthermore, walnuts have the following impressive health benefits:6
A diet rich in walnuts and other nuts has been shown to play a role in supporting heart health,7,8 mainly due to the amino acid l-arginine.
Approximately 90 percent of the phenols — including flavonoids, phenolic acids and tannins — found in walnuts reside in its skin.
Eating a handful of walnuts daily is said to reduce blood pressure and lower your risk of cardiovascular disease. Walnuts have also been shown to slow tumor growth in animals.9,10
If you are a man eating a Western-style diet, studies suggest consuming higher levels of polyunsaturated fatty acids (PUFAs), which are found in walnuts, may increase your sperm quality.11
Consuming walnuts is thought to improve your brain function and cognition.12
Walnut intake has been shown to increase levels of three beneficial gut bacteria — Clostridium, Faecalibacterium and Roseburia — which produce a metabolic byproduct called butyrate that is believed to improve your colon health.13,14
“Walnuts have been called a ‘superfood’ because they are rich in omega-3 fatty acid, alpha-linolenic acid and fiber and they contain one of the highest concentrations of antioxidants,” states registered dietitian Lauri Byerley, research associate professor of physiology at Louisiana State University. “[A]n additional superfood benefit of walnuts may be their beneficial changes to your gut microbiota.”15
Consuming Walnuts May Lower Your Risk of Type 2 Diabetes
An epidemiological study published in the journal Diabetes/Metabolism Research and Reviews, involving 34,000 American adults, suggests consuming walnuts may slash your risk of developing Type 2 diabetes in half, as compared to people who do not eat nuts.16
The research, conducted at the University of California, Los Angeles (UCLA) in 2018, suggests eating 3 tablespoons, or 42.5 g, of walnuts per day is associated with a 47 percent lower prevalence of Type 2 diabetes. The data was extracted from the National Health and Nutrition Examination Survey (NHANES) and centered on adults aged 18 to 85 years.
Study participants were asked about their diets and assessed for diabetes using common laboratory measurements such as fasting plasma glucose and hemoglobin A1c.
"These findings provide more evidence for food-based guidance to help reduce the risk for diabetes," said Lenore Arab, nutritional epidemiologist and adjunct professor in UCLA’s School of Medicine. "The strong connection we see in this study between walnut consumers and the lower prevalence of Type 2 diabetes is additional justification for including walnuts in the diet."17
The walnut intake proposed to slash your diabetes risk by half is close to the recommended serving size of walnuts, which is 4 tablespoons (56.7 g). The data suggests the effect of walnut consumption on diabetes may be more potent among women than men. While this study sounds like really great news, especially if you love to eat nuts, it’s important to make note of two important limitations related to the research:18
Participants were asked about their dietary choices over the course of just one to two days, which may or may not represent their usual pattern of walnut consumption
Given the cross-sectional nature of the study, the findings do not prove eating walnuts directly causes you to be at less risk of diabetes
Although Nuts Are Healthy, Watch the Protein Content and Don’t Eat too Many
Most nuts, including macadamias, pecans and walnuts, should be eaten in moderation. While you may think the reason to moderate your consumption has to do with the high fat content, remember the kind of fat available in these nuts is the healthy type your body and brain need to thrive. The bigger concern I have about some nuts is their high protein content.
Because nuts are generally considered to be a snack food, you may not think to count the protein from them as part of your total daily intake. Even if you don’t eat nuts, most Americans consume three to five times more protein than they need. Eating too much protein can elevate your blood sugar, cause weight gain, stress your kidneys, leach bone minerals and stimulate cancer cells. For those reasons, it’s critical you keep track of how much protein you are eating and factor in protein from nuts.
If you develop a habit of eating nuts absent-mindedly by the handful, you can easily surpass your daily target for protein consumption. For optimal health, you’ll want to limit your protein intake to around 0.5 grams of protein per pound of lean body mass. For most people that comes out in the range of 40 to 70 grams a day. For example, a person weighing 160 pounds, with 128 pounds of lean body mass, should eat about 64 g of protein a day.
Why It's Important to Choose Organic Nuts
When choosing nuts, look for high-quality nuts that are certified organic and presented in raw form. Avoid roasted or pasteurized nuts, as well as nuts coated in sugar or covered in milk chocolate. Contrary to what you may think, only dry-roasted nuts are truly roasted. Most nuts labeled and sold as roasted are actually fried in vegetable oil. You can tell this because the ingredient label will identify the type of oil used for frying. This practice is ill-advised for a few reasons:
Most vegetable oils are unhealthy and contain an overabundance of omega-6 fats. In addition, some vegetable oils used to fry nuts, such as canola oil, are genetically engineered (GE).
Roasting raises the potential for the formation of a possible carcinogen called acrylamide, which results from a chemical reaction between sugars in certain foods and an amino acid called asparagine. Acrylamide, which is best known as the “browning” on chips and french fries, has the potential to form on certain nuts when they are fried or roasted at temperatures above 250 degrees F (121 degrees C) for long cooking times.19
Vegetable oils heated to high temperatures can easily oxidize, promoting the formation of disease-causing free radicals. Nuts that oxidize can also become rancid and attract fungal mycotoxins. You can identify rancid nuts by a musty, stale or spoiled smell.
Nuts roasted at high temperatures may contain lower amounts of antioxidants, vitamins and other nutrients. In addition, the healthy fats in some nuts may be damaged by high heat.
For Best Results, Buy Raw Nuts and Soak Them Before You Eat Them
Your healthiest option is to consume nuts raw. That said, it’s important to note how difficult it can be to find truly raw nuts in the U.S. For instance, pasteurized almonds sold in North America can still be labeled "raw" even though they've been blanched, steam processed or otherwise treated. While you may not be able to verify if nuts labeled raw are truly raw, seek out reputable sources and do the best you can. I also recommend you soak your nuts — for about eight to 12 hours — before you eat them to reduce their phytic acid content.
Phytic acid, found in the coatings of nuts (and seeds), is an "antinutrient" responsible for leeching vital nutrients from your body. By soaking nuts, you help rid them of phytic acid and also loosen up the enzyme coat, which can be removed from nuts like almonds. (Given their negligible amounts of enzyme inhibitors, macadamias and other white nuts do not need to be soaked.) As natural inhibitors, the enzyme coats help protect nuts as they develop and also prevent them from sprouting prematurely.
Although the coatings are beneficial to the nuts themselves, the antinutrients found in them may interfere with your body’s own digestive and metabolic enzymes, thereby making nuts harder to digest. When nuts are soaked, the germination process begins, allowing the enzyme inhibitors to be deactivated, making nuts much easier to digest. Given their superior nutrition, health benefits and convenience, I hope you will consider adding macadamias, pecans and walnuts to your shopping list this week.
Credits:
Original Content Source
0 notes
Link
Why Macadamias, Pecans and Walnuts Should Be on Your Shopping List Dr. Mercola By Dr. Mercola While many consider nuts to be nothing more than a snack food, there are several healthy reasons you should considering eating certain nuts a little more often. Three tree nuts I highly recommend are macadamias, pecans and walnuts. Because macadamias and pecans have high fat and low protein and carb levels, they are superior choices, particularly if you eat a ketogenic diet. Walnuts, while slightly less ideal than macadamia and pecans due to their higher protein and carb content, are also an excellent choice mainly because new research suggests eating them may reduce your risk of Type 2 diabetes. Before you add macadamias, pecans and walnuts to your shopping list, let’s take a closer look at the composition of each one and find out what makes them a healthy choice. Why Macadamia Nuts Are Beneficial Macadamias, which are among my personal favorite nuts, have the highest fat content and lowest protein and carbohydrate levels of any nut. If you eat a ketogenic diet, you probably already know macadamia nuts are a nutritional powerhouse. Macadamias are helpful to keto fans because they are loaded with healthy fat. A 1-ounce serving — 28 grams (g) or about 10 to 12 nuts — contains 21 g of fat, 2 g of protein and 4 g of carbs. In addition, raw macadamia nuts contain high amounts of B vitamins, magnesium, manganese, phosphorus and potassium. Just one serving of macadamias provides 58 percent of your dietary requirement for manganese and 23 percent of the recommended daily value of vitamin B1.1 Moreover, about 60 percent of the fatty acid in macadamias is the monounsaturated fatty acid (MUFA) oleic acid. Olives are well-known for containing healthy amounts of oleic acid and macadamia nuts have about the same level of oleic acid found in olives. Below are more reasons to love macadamia nuts:2 Due to the rich stores of MUFAs found in them, similar to other tree nuts, macadamias offer cardioprotective properties. Macadamia nuts have been shown to optimize your total and low-density lipoprotein (LDL) cholesterol, apolipoprotein B (ApoB) and triglycerides.3 Macadamias contain flavonoids known to help prevent cell damage and protect your body from environmental toxins. Once ingested, these flavonoids are converted into antioxidants, which destroy free radicals and protect you from diseases such as cancer. The high fat content of macadamia nuts can act as an appetite suppressant. This means a small handful of them will satisfy you longer than a calorie-comparable sugary snack. As an excellent source of protein, raw macadamia nuts are also low in sodium with a satisfying crunch. They’re a healthier snack than processed salty snack foods. A serving of 10 to 12 macadamia nuts contains 2.4 g of dietary fiber, which represents about 10 percent of your daily fiber requirement. As such, macadamia nuts promote healthy digestion and gut health. Magnesium and phosphorus, as well as calcium, all of which are available in macadamias, are useful to support bone and teeth mineralization and the absorption and transportation of vital nutrients. Compared to other tree nuts, macadamias boast the best omega-3 to omega-6 ratio and are therefore a healthier choice — especially if you are trying to avoid inflammation. Why Pecans Are a Healthy Choice Pecans, another of my favorite nuts, have the second highest fat content and second lowest protein and carb content among tree nuts. Along with macadamias, raw pecans can be a beneficial food source if you eat a ketogenic diet. A 1-ounce serving — 28 g or about 19 halves — contains 21 g of fat, 3 g of protein and 4 g or carbs. In addition, raw pecans contain good amounts of vitamin E and B vitamins, particularly thiamin (B1). In terms of minerals, a 1-ounce serving provides 64 percent of your daily value for manganese, 17 percent of your copper needs and 9 percent of your daily needs for both magnesium and zinc.4 The nearly 3 g of fiber a serving that pecans provide help keep your digestive system well-regulated. Below are additional benefits to eating raw pecans:5 Pecans contain antioxidant power due to the presence of vitamin E and phytochemicals like lutein and zeaxanthin, which neutralize free radicals and protect your body from infections and diseases, including cancer. Another phytochemical contributing to the antioxidant activity of pecans is ellagic acid, which helps prevent carcinogenic compounds from binding to your DNA and proliferating. Pecans are packed with fatty acids like oleic acid, which is great for weight control. The plant sterols in pecans offer cholesterol-optimizing properties. The high amount of thiamin in pecans helps your cells convert carbs into energy and also supports your heart, muscle and nervous system functions. The magnesium in pecans reduces the presence of C-reactive protein and interleukin-6 and protects against widespread inflammation within your body. Why Walnuts Are Good for You If you routinely eat nuts but overlook walnuts, you may be missing out. While they contain a little less fat and a little more protein than macadamias and pecans, walnuts are a healthy nut. A 1-ounce serving — 28 g or about 14 halves — contains 18 g of fat, 4 g of protein and 4 g of carbs. Walnuts also contain nearly 2 g of fiber, as well as vitamins B, C and E. In terms of minerals, a 1-ounce serving provides rich stores of magnesium, phosphorus and potassium. Furthermore, walnuts have the following impressive health benefits:6 A diet rich in walnuts and other nuts has been shown to play a role in supporting heart health,7,8 mainly due to the amino acid l-arginine. Approximately 90 percent of the phenols — including flavonoids, phenolic acids and tannins — found in walnuts reside in its skin. Eating a handful of walnuts daily is said to reduce blood pressure and lower your risk of cardiovascular disease. Walnuts have also been shown to slow tumor growth in animals.9,10 If you are a man eating a Western-style diet, studies suggest consuming higher levels of polyunsaturated fatty acids (PUFAs), which are found in walnuts, may increase your sperm quality.11 Consuming walnuts is thought to improve your brain function and cognition.12 Walnut intake has been shown to increase levels of three beneficial gut bacteria — Clostridium, Faecalibacterium and Roseburia — which produce a metabolic byproduct called butyrate that is believed to improve your colon health.13,14 “Walnuts have been called a ‘superfood’ because they are rich in omega-3 fatty acid, alpha-linolenic acid and fiber and they contain one of the highest concentrations of antioxidants,” states registered dietitian Lauri Byerley, research associate professor of physiology at Louisiana State University. “[A]n additional superfood benefit of walnuts may be their beneficial changes to your gut microbiota.”15 Consuming Walnuts May Lower Your Risk of Type 2 Diabetes An epidemiological study published in the journal Diabetes/Metabolism Research and Reviews, involving 34,000 American adults, suggests consuming walnuts may slash your risk of developing Type 2 diabetes in half, as compared to people who do not eat nuts.16 The research, conducted at the University of California, Los Angeles (UCLA) in 2018, suggests eating 3 tablespoons, or 42.5 g, of walnuts per day is associated with a 47 percent lower prevalence of Type 2 diabetes. The data was extracted from the National Health and Nutrition Examination Survey (NHANES) and centered on adults aged 18 to 85 years. Study participants were asked about their diets and assessed for diabetes using common laboratory measurements such as fasting plasma glucose and hemoglobin A1c. "These findings provide more evidence for food-based guidance to help reduce the risk for diabetes," said Lenore Arab, nutritional epidemiologist and adjunct professor in UCLA’s School of Medicine. "The strong connection we see in this study between walnut consumers and the lower prevalence of Type 2 diabetes is additional justification for including walnuts in the diet."17 The walnut intake proposed to slash your diabetes risk by half is close to the recommended serving size of walnuts, which is 4 tablespoons (56.7 g). The data suggests the effect of walnut consumption on diabetes may be more potent among women than men. While this study sounds like really great news, especially if you love to eat nuts, it’s important to make note of two important limitations related to the research:18 Participants were asked about their dietary choices over the course of just one to two days, which may or may not represent their usual pattern of walnut consumption Given the cross-sectional nature of the study, the findings do not prove eating walnuts directly causes you to be at less risk of diabetes Although Nuts Are Healthy, Watch the Protein Content and Don’t Eat too Many Most nuts, including macadamias, pecans and walnuts, should be eaten in moderation. While you may think the reason to moderate your consumption has to do with the high fat content, remember the kind of fat available in these nuts is the healthy type your body and brain need to thrive. The bigger concern I have about some nuts is their high protein content. Because nuts are generally considered to be a snack food, you may not think to count the protein from them as part of your total daily intake. Even if you don’t eat nuts, most Americans consume three to five times more protein than they need. Eating too much protein can elevate your blood sugar, cause weight gain, stress your kidneys, leach bone minerals and stimulate cancer cells. For those reasons, it’s critical you keep track of how much protein you are eating and factor in protein from nuts. If you develop a habit of eating nuts absent-mindedly by the handful, you can easily surpass your daily target for protein consumption. For optimal health, you’ll want to limit your protein intake to around 0.5 grams of protein per pound of lean body mass. For most people that comes out in the range of 40 to 70 grams a day. For example, a person weighing 160 pounds, with 128 pounds of lean body mass, should eat about 64 g of protein a day. Why It's Important to Choose Organic Nuts When choosing nuts, look for high-quality nuts that are certified organic and presented in raw form. Avoid roasted or pasteurized nuts, as well as nuts coated in sugar or covered in milk chocolate. Contrary to what you may think, only dry-roasted nuts are truly roasted. Most nuts labeled and sold as roasted are actually fried in vegetable oil. You can tell this because the ingredient label will identify the type of oil used for frying. This practice is ill-advised for a few reasons: Most vegetable oils are unhealthy and contain an overabundance of omega-6 fats. In addition, some vegetable oils used to fry nuts, such as canola oil, are genetically engineered (GE). Roasting raises the potential for the formation of a possible carcinogen called acrylamide, which results from a chemical reaction between sugars in certain foods and an amino acid called asparagine. Acrylamide, which is best known as the “browning” on chips and french fries, has the potential to form on certain nuts when they are fried or roasted at temperatures above 250 degrees F (121 degrees C) for long cooking times.19 Vegetable oils heated to high temperatures can easily oxidize, promoting the formation of disease-causing free radicals. Nuts that oxidize can also become rancid and attract fungal mycotoxins. You can identify rancid nuts by a musty, stale or spoiled smell. Nuts roasted at high temperatures may contain lower amounts of antioxidants, vitamins and other nutrients. In addition, the healthy fats in some nuts may be damaged by high heat. For Best Results, Buy Raw Nuts and Soak Them Before You Eat Them Your healthiest option is to consume nuts raw. That said, it’s important to note how difficult it can be to find truly raw nuts in the U.S. For instance, pasteurized almonds sold in North America can still be labeled "raw" even though they've been blanched, steam processed or otherwise treated. While you may not be able to verify if nuts labeled raw are truly raw, seek out reputable sources and do the best you can. I also recommend you soak your nuts — for about eight to 12 hours — before you eat them to reduce their phytic acid content. Phytic acid, found in the coatings of nuts (and seeds), is an "antinutrient" responsible for leeching vital nutrients from your body. By soaking nuts, you help rid them of phytic acid and also loosen up the enzyme coat, which can be removed from nuts like almonds. (Given their negligible amounts of enzyme inhibitors, macadamias and other white nuts do not need to be soaked.) As natural inhibitors, the enzyme coats help protect nuts as they develop and also prevent them from sprouting prematurely. Although the coatings are beneficial to the nuts themselves, the antinutrients found in them may interfere with your body’s own digestive and metabolic enzymes, thereby making nuts harder to digest. When nuts are soaked, the germination process begins, allowing the enzyme inhibitors to be deactivated, making nuts much easier to digest. Given their superior nutrition, health benefits and convenience, I hope you will consider adding macadamias, pecans and walnuts to your shopping list this week.
0 notes
Text
My Health Story
I have a condition called Idiopathic Intracranial Hypertension which means that my body, for some unknown reason, has too much cerebrospinal fluid, and it puts pressure on my brain.
For me, when I was at my worst, that meant I was throwing up every day, could barely see, had absolutely zero energy, had constant whooshing in my ears, and a horrible headache that never went away.
Why, you ask, did I let this get so bad?
I was in the middle of my last year of marching band. I was a section leader, and I couldn’t afford to miss rehearsal.
So one day, I was getting ready for rehearsal (9am-6pm) and I just.. Couldn’t. I couldn’t walk much without feeling like I was being dragged down, I still had the headache and the whooshing and the nausea, and standing up or moving made my vision go black more than normal.
So what did I do? I put 8 water bottles and all the granola bars we had in my backpack and went downstair to wait for my mom. I get there, and I’m trying to cross the street, and I’m having trouble balancing and I’m feeling foggy.
My mom panics, and tells my dad to take me to the ER.
After a 20 minute drive, 30 minutes of waiting, and 2 hours of sitting in a hospital bed, the doctor comes in and says I’m probably dehydrated.
I’m livid. I had regularly been drinking easily a gallon of water a day for a month at that point, and I told him. And he said I might just be wrong about how much water I’m drinking. He goes out in the hall to speak with my dad, and when he comes back, he says he’s going to send me for a CT scan, even though he doesn’t think it’s necessary.
In the meantime, they take some blood to send for tests. After the CT (it was nothing fancy, I wasn’t fully aware of what was going on), we wait for the doctor.
He says the CT was clear but that my iron levels are practically nothing. My hemoglobin levels were 5, when they should have been between 12 and 15. He sends me home with a prescription for iron supplements, zofran for nausea, and an acid reducer to help with my stomach problems.
Okay, that’s fine. I’m anemic, that’s the solution, the big Thing that caused all my problems.
Except not really. He mentioned that the anemia wouldn’t really explain the vision problems, but that he’s not an eye doctor, so he could be wrong.
Whatever, I take iron supplements, and things start improving. My vision is only about 60% spots rather than 80%, and my vision doesn’t completely black out when I stand, but the headaches are still there, and I’m still nauseous.
So we make an appointment with an eye doctor.
Within the first 10 minutes, she ends the appointment, saying there’s blood in the back of my eyes, and that it’s no reason to worry, but I should definitely see an ophthalmologist as soon as possible, even within the day.
Sadly, the office closed at 5, and it was 4:45 at that point, so I get an appointment for the next day.
At my ophthalmologist’s appointment, she doesn’t really solve my problems. She says my optic nerves are swollen in both eyes, and that this is something she sees pretty often, and not to worry, but she’s getting me an MRI in 45 minutes.
I’m panicking. Doctors don’t do things this fast unless it’s serious.
We go, I do the MRI, everything comes back clear, except that there seems to be some pressure in my head, but no tumor, which I didn’t even know was an option.
She gets me a referral to a pediatric neurologist who I see a week later.
She order 22 blood tests and schedules me for an LP. Oh, and also I’m apparently B12 deficient, so she starts me on that.
A few weeks later, I get my LP, except she can’t get a sucessful sample. She can’t get the spinal fluid. So she makes me an appointment to do an LP under flouroscopy in a few weeks.
I go do that and finally I have answers. Idiopathic intracranial hypertension.
She starts me on diamox, says my iron levels coming up might help, but then again, idiopathic means no one knows anything.
So that’s my story. 2 months, several doctors, too many needles, and a whole lot of mental stress later, I’m on diamox twice a day, still taking iron twice a day, and my B12 is all sorted out.
My headaches are down to once or twice a week and only last an hour, my nausea is come and go, and my vision is pretty much back to normal.
0 notes
Text
Popular Blood Tests—the Facts, Ranges, and Alternatives You Should Know
I’m of two minds when it comes to blood testing. For myself, I’m not a huge fan of obsessive, frequent testing and optimization. I have a good idea about how to optimize my health through the actions I take and the foods I eat, and by monitoring how I’m feeling, looking, and performing in response. It’s worked well for me. Whenever I do get a checkup or have blood drawn, my numbers are great.
But many people are the opposite. They like to quantify what’s happening under the hood. That’s great, and often necessary. The problem is that there are big problems with many of the most common blood tests.
A glaring problem for almost every blood test are the reference ranges used. What’s wrong with those?
Reference ranges reflect what’s common, not normal. A reference range for a blood test refers to the values possessed by 95% of the normal population.
Reference ranges for blood tests are based on the people who get lab tests. Who gets lab tests? People who go to the doctor, often because there’s something wrong with them. They may not reflect normal ranges for truly healthy people.
Reference ranges are extremely broad, which may give a false sense of security. Having blood sugar on the high end of “normal” isn’t healthy. It actually presages type 2 diabetes.
Another problem inherent to almost every blood test you’ll take is that the result represents a snapshot in time, a brief glimpse at a situation in constant flux. Your cholesterol was elevated today at 12 noon. What does that say about your levels tomorrow at six in the evening? Next week? Nothing. To account for natural fluctuations, get tested at regular intervals and observe the trends.
Let’s get more specific.
Cholesterol
“Oh, gee, Tom, steak and eggs for lunch again? You ever get your cholesterol checked?” We hear this all the time, the chorus of pleas that we please go get a “cholesterol test” before we keel over. Say you decide to humor the skeptics. You go get a cholesterol test. What should you watch for?
Most of the time, LDL is calculated, not directly measured. If you have low triglycerides, as is common on low-carb diets, your calculated LDL will be higher than the reality.
LDL-C refers to the passengers in the cars, not the number of cars on the highway. Most basic tests don’t measure LDL particle number. All evidence points to the number of LDL particles being far more predictive of heart disease risk than the more common LDL-C. More LDL particles means LDL is hanging around in the blood, increasing the chance they’ll become oxidized and atherogenic.
The guidelines aren’t supported in the literature. Many studies have shown a disconnect between supposedly dangerous cholesterol levels and actual heart attacks. In a 2009 study, 75% of people hospitalized for a heart attack had “healthy” cholesterol numbers. A 2016 review found that lower LDL is associated with lower mortality in the elderly—you know, some of most vulnerable among us.
What can you do?
Request an advanced lipid test. Tests like VAP, NMR, ApoB, and LDL particle number testing all provide deeper insights into the state of your blood lipids.
If you’re stuck with the basic test, take a look at ratios. Total cholesterol/HDL ratio is a good indicator of how long LDL is hanging around in the blood and remains the best standard assessment of heart disease risk. Another good one is triglyceride/HDL ratio, which is a strong surrogate marker for insulin resistance. In both cases, lower is better. An ideal T/HDL ratio is 1:1; 2:1 is about as high as you want to go. An ideal TC/HDL ratio is 3.5:1 or lower.
Blood Sugar
There are three primary types of blood sugar tests: fasting, postprandial, and hemoglobin A1c (HbA1c). Postprandial blood sugar measures your blood sugar response to eating at various intervals after meal. Fasting blood sugar measures your blood sugar levels at rest, when no food is coming in. HbA1c measures your average blood glucose across the previous three months. They’re all important, but the tests all have issues.
“Normal” might not be normal. According to the American Diabetes Association, a fasting blood sugar (FBG) under 100 is completely normal. It’s safe. It’s fine. Don’t worry, just keep eating your regular diet, and did you get a chance to try the donuts in the waiting room? They only start to worry at 110-125 (pre-diabetic) and above 125 (diabetic).
This may be unwise. Healthy people subjected to continuous glucose monitoring have much lower average blood glucose—89 mg/dl. A 2008 study found that people with a FBG of 95-99 were 2.33 times more likely to develop diabetes in the future than people on the low-normal end of the scale.
How about HbA1c? A “normal” HbA1c is anything under 5.7. And 6.0 is diabetic. That’s what the reference ranges, which mostly focuses on diabetes. What does the research say? In this study, under 5 was best for heart disease. In this study, anything over 4.6 was associated with an increased risk of heart disease.
That 5.7 HbA1c isn’t looking so great.
Healthy FBG depends on your BMI. At higher FBG levels, higher BMIs are protective. You read that right. A recent study showed that optimal fasting blood glucose for mortality gradually increased with bodyweight. Low-normal BMIs had the lowest mortality at normal FBG (under 100), moderately overweight BMIs had the lowest mortality at somewhat impaired FBG (100-125), and the highest BMIs had the lowest mortality at diabetic FBG levels (over 125).
The oral glucose tolerance test is unrealistic. The standard way to test postprandial blood sugar is the oral glucose tolerance test: 75 grams of pure glucose in liquid form. Unless you’re downing jumbo Slurpees, you’re not consuming that much pure glucose in a single sitting, so the results may not be relevant.
HbA1c depends on a static red blood cell lifespan. A1c seeks to establish the average level of blood sugar circulating through your body over the red blood cell’s life cycle, rather than track blood sugar numbers that rapidly fluctuate through the day, week, and month. If we know how long a red blood cell lives, we have an accurate measurement of chronic blood sugar levels. The clinical consensus assumes the lifespan is three months. Is it?
Not always. The life cycle of an actual red blood cell differs between and even within individuals, and it’s enough to throw off the results by as much as 15 mg/dl.
Ironically, people with healthy blood sugar levels might have inflated HbA1c levels. One study found that folks with normal blood sugar had red blood cells that lived up to 146 days, and RBCs in folks with high blood sugar had life cycles as low as 81 days. For every 1% rise in blood sugar, red blood cell lifespan fell by 6.9 days. In those with better blood sugar control, RBCs lived longer and thus had more time to accumulate sugar and give a bad HbA1c reading. In people with poorer blood sugar control, red blood cells live shorter lives and have less time to accumulate sugar, potentially giving them “better” HbA1c numbers.
Anemia can inflate HbA1c. Anemia depresses the production of red blood cells. If you have fewer red blood cells in circulation, the ones you do have accumulate more sugar since there are fewer cells “competing” for it.
If you’re very low-carb, postprandial blood glucose will be elevated. This is because very low-carb, high-fat diets produce physiological insulin resistance to preserve what little glucose you have for the tissues that depend on it, like certain parts of the brain. The more resistant you are to insulin, the higher your blood glucose.
What can you do?
If you need to pass a test, 150 grams of carbs a day will do it. Eat that way for three days to a week before your OGGT.
Try meals, not sugar solutions. Mixed meals of fat, protein, and carbs are better candidates for testing one’s real-world glucose response.
Take all three measurements into account. If your HbA1c is higher than you’d like but you ace all the postprandial tests, you’re probably fine.
Follow trends. Even if your red blood cells are centenarians, you can track the trend of HbA1c with multiple readings.
Liver Enzymes
The most common liver enzymes you’ll test are alanine transaminase (ALT) and aspartate transaminase (AST). Another one is gamma-glutamyl transpeptidase, or GGT. When the liver is damaged or inflamed, liver enzymes generally go up. They’re usually pretty straightforward—more straightforward than the cholesterol and blood sugar tests—but not completely.
Weight loss can change them. Weight loss transiently increases ALT and AST in women and decreases them in men. If you’re in the process of losing weight, you can safely ignore small improvements or increases in liver enzymes.
Normal isn’t healthy. The normal range for GGT is 8 to 65 U/L, yet men under 70 years of age with GGT levels over 38—right smack in the middle of “normal”—have an increased risk of heart failure. Another study found that even low-normal levels of GGT were associated with an increased incidence of atrial fibrillation, a harbinger of more serious cardiovascular conditions.
What can you do?
Just be aware. Don’t fear weight loss for transient changes to your ALT/AST, and don’t rest on your laurels if your GGT looks “normal.”
Testing your cholesterol, blood sugar, and liver enzymes is helpful, informative, and often necessary—but only if you’re aware of the limitations and you know how to account for context.
Thanks for reading, everyone. Take care!
0 notes