#physicians for a national health program
Text
By Ed Weisbart
Common Dreams
July 30, 2024
If we want to build on the promise of Medicare, then we’re going to have to grapple directly with the power of corporate health insurance: That starts with taking on the so-called “Medicare Advantage” program.
Fifty-nine years ago today, President Lyndon Johnson signed Medicare into law—a high-water mark in the fight for universal healthcare that had started decades before and that continues to this day.
Ever since Medicare became law, it has been a shining example of what is possible in U.S. healthcare: a truly public, truly universal program that has saved countless lives and prevented untold financial ruin among America’s seniors. But alongside this success, corporate health interests have also grown immeasurably more powerful. Insurers like UnitedHealthcare and Blue Cross Blue Shield have erected cruel barriers to care and are laughing all the way to the bank.
If we want to build on the promise of Medicare—and win the best possible version of Medicare for All—then we’re going to have to grapple directly with the power of corporate health insurance. That starts with taking on the so-called “Medicare Advantage” program.
The Strategic Importance of Medicare Advantage
Single-payer advocates understand that there can’t be “Medicare for All” if there is no “Medicare.” And no, Medicare Advantage (MA) doesn’t count as Medicare. The health insurance corporations that run these plans have a business imperative to prioritize profits above all else; this is anathema to any public health program.
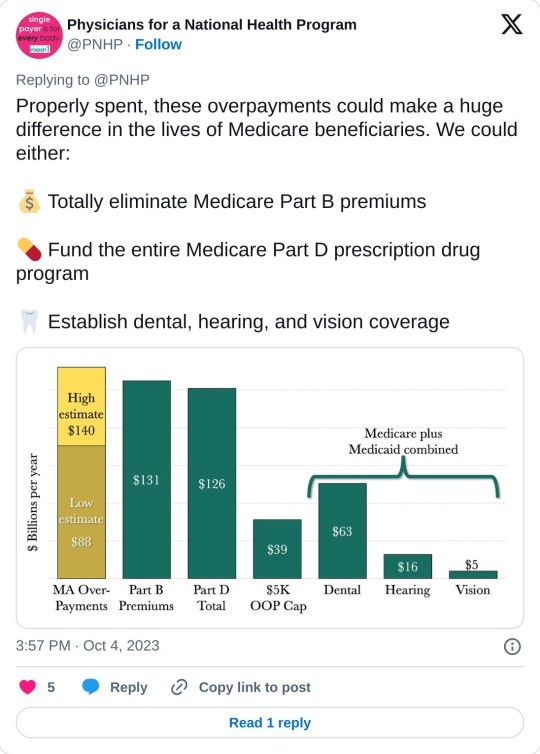
Physicians for a National Health Program (PNHP) has compiled overwhelming evidence that MA insurers are harming patients, physicians, and hospitals by delaying and denying care—harms that are virtually unseen in Traditional Medicare. Nor is this cruelty even a trade-off for lowering the cost of healthcare. In fact, these corporations are paid far more than what is spent for similar patients in Traditional Medicare—up to $140 billion per year, or as much as 35% above the funding levels of Traditional Medicare.
There is no road to Medicare for All that ignores this existential threat.
Where we see middlemen standing between patients and the care they need, we should remove them. Where we see limited provider networks, we should expand them. Where we see piles of pre-authorization paperwork, we should shred them.
Thankfully, support for eliminating overpayments to MA extends far beyond those who are already committed to single payer. This fight builds our movement by mobilizing a wide range of people who understand, or can be educated about, the damage insurance companies are doing to patients. When we find common ground, we should walk together.
For that reason, PNHP is exposing MA overpayments and demanding a more fiscally responsible approach from policymakers. We are working closely with several organizations to change the national conversation and provide a badly needed counterweight to the lobbying might of big insurance.
When MA was created, way back in 2003, corporate insurers promised to reduce the cost of healthcare by improving care coordination and health outcomes. A healthier population, they claimed, would be less expensive. We should demand that MA corporations live up to these lofty promises without billions of dollars in overpayments.
We’d like to see them try.
Improved Medicare… for ALL
Winning back $140 billion in annual overpayments begs a tantalizing question: How can we use those funds to improve Medicare for all seniors?
Instead of the paltry benefits that MA plans offer, those funds would help us add robust hearing, vision, and dental benefits; totally eliminate Medicare Part B premiums; and fold in the Medicare Part D prescription drug benefit. Imagine the relief a senior on Medicare Advantage would feel when enrolling in a plan that actually covers the full range of dental care, while also freeing themselves from the narrow provider networks and prior authorization requirements imposed by MA plans.
Most critically, we need to establish a low out-of-pocket maximum for Medicare. Insurance corporations lure seniors and people with disabilities into the MA trap by selling lower up-front costs while hiding substantial barriers to care. It’s a classic bait and switch. Eliminating the need to purchase Medigap would level the playing field and allow everybody to remain in Traditional Medicare.
Let’s work to build a movement of seniors, physicians, students, people with disabilities, and everybody else who cares about Medicare.
Well, not everybody—but that’s our ultimate goal. PNHP advocates for a national single-payer health insurance program, and what better way to get there than through an improved version of the already popular Medicare program?
Where we see middlemen standing between patients and the care they need, we should remove them. Where we see limited provider networks, we should expand them. Where we see piles of pre-authorization paperwork, we should shred them.
We should also expand benefits to include all medically necessary care, and ultimately eliminate out-of-pocket costs that deter people from seeing a doctor. Once these improvements are in place, we will have a program that’s truly worthy of the name Medicare for All.
The advocacy work for these priorities—ending MA overpayments, improving Traditional Medicare, and realizing our vision for single payer—overlap and build on one another.
Let’s work to build a movement of seniors, physicians, students, people with disabilities, and everybody else who cares about Medicare. Together, we can take on the corporate insurers that are wreaking so much havoc in our lives and lay the groundwork for winning a single-payer program that brings everybody in and leaves nobody out.
Ed Weisbart, MD, is a retired family physician in Olivette, Missouri, and board secretary of Physicians for a National Health Program.
#medicare for all#medicare#medicare advantage#health insurance#healthcare#seniors#Physicians for a National Health Program
11 notes
·
View notes
Text
A national physician group this week called for the complete termination of a Medicare privatization scheme that the Biden White House inherited from the Trump administration and later rebranded—while keeping intact its most dangerous components.
Now known as the Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) Model, the experiment inserts a for-profit entity between traditional Medicare beneficiaries and healthcare providers. The federal government pays the ACO REACH middlemen to cover patients' care while allowing them to pocket a significant chunk of the fee as profit.
The rebranded pilot program, which was launched without congressional approval and is set to run through at least 2026, officially began this month, and progressive healthcare advocates fear the experiment could be allowed to engulf traditional Medicare.
In a Tuesday letter to Health and Human Services Secretary Xavier Becerra and Centers for Medicare and Medicaid Services Administrator Chiquita Brooks-LaSure, Physicians for a National Health Program (PNHP) argued that ACO REACH "presents a threat to the integrity of traditional Medicare, and an opportunity for corporations to take money from taxpayers while denying care to beneficiaries."
The group, which advocates for a single-payer healthcare system, voiced alarm over the Biden administration's decision to let companies with records of fraud and other abuses take part in the ACO REACH pilot, which automatically assigns traditional Medicare patients to private entities without their consent.
CMS said in a press release Tuesday that "the ACO REACH Model has 132 ACOs with 131,772 healthcare providers and organizations providing care to an estimated 2.1 million beneficiaries" for 2023.
"As we have stated, PNHP believes that the REACH program threatens the integrity of traditional Medicare and should be permanently ended," Dr. Philip Verhoef, the physician group's president, wrote in the new letter. "Whether or not one agrees with this statement, we should all be able to agree that companies found to have violated the rules have no place managing the care of our Medicare beneficiaries."
Among the concerning examples PNHP cited was Clover Health, which has operated so-called Direct Contracting Entities (DCEs)—the name of private middlemen under the Trump-era version of the Medicare pilot—in more than a dozen states, including Arizona, Florida, Georgia, and New York.
PNHP noted that in 2016, CMS fined Clover—a large Medicare Advantage provider—for "using 'marketing and advertising materials that contained inaccurate statements' about coverage for out-of-network providers, after a high volume of complaints from patients who were denied coverage by its MA plan. Clover had failed to correct the materials after repeated requests by CMS."
Humana, another large insurer with its teeth in the Medicare privatization pilot, "improperly collected almost $200 million from Medicare by overstating the sickness of patients," PNHP observed, citing a recent federal audit.
"It appears that in its selection process [for ACO REACH], CMS did not prevent the inclusion of companies with histories of such behavior," Verhoef wrote. "Given these findings, we are concerned that CMS is inappropriately allowing these DCEs to continue unimpeded into ACO REACH in 2023."

While the Medicare pilot garnered little attention from lawmakers when the Trump administration first launched it during its final months in power, progressive members of Congress have recently ramped up scrutiny of the program.
Last month, Sen. Elizabeth Warren (D-Mass.) and Rep. Pramila Jayapal (D-Wash.) led a group of lawmakers in warning that ACO REACH "provides an opportunity for healthcare insurers with a history of defrauding and abusing Medicare and ripping off taxpayers to further encroach on the Medicare system."
"We have long been concerned about ensuring this model does not give corporate profiteers yet another opportunity to take a chunk out of traditional Medicare," the lawmakers wrote, echoing PNHP's concerns. "The continued participation of corporate actors with a history of fraud and abuse threatens the integrity of the program."
#us politics#news#2023#common dreams#medicare#trump administration#biden administration#Accountable Care Organization Realizing Equity Access and Community Health model#department of health and human services#Xavier Becerra#Chiquita Brooks-LaSure#Physicians for a National Health Program#Centers for Medicare and Medicaid Services#Dr. Philip Verhoef#Direct Contracting Entities#Medicare Advantage#sen. elizabeth warren#Rep. Pramila Jayapal#medicare for all#us healthcare#us health insurance
95 notes
·
View notes
Text

Medical complicity in torture occurs in a number of ways. As explicated in Addameer’s 2020 comprehensive study, Cell 26, prior to the start of a detainee’s interrogation, Israeli physicians collaborate with Shin Bet interrogators to “certify” or approve that they are “fit” to undergo torture. Throughout the duration of interrogation, a physician provides a “green light” that torture can continue.
But the enabling of torture extends beyond a superficial “health check.” In their examinations, healthcare professionals look for physical and psychological weaknesses to exploit in a person. These weaknesses are actively shared with interrogators to help them break a prisoner’s spiritIsraeli doctors also conceal injuries they observe during torture. Instead of fulfilling their ethical responsibilities to report abuse, physicians falsify or refrain from documenting the physical and psychological effects of torture on a detainee’s body and mind — depriving victims of using potential evidence against their torturers.
Medical complicity in torture extends further beyond individual physicians to the entirety of the Israeli medical system. Palestinian detainees recount that interrogators are trained in methods of abuse that are designed to inflict maximum harm. This knowledge is not innate; rather, according to Cell 26 medical research is shared with Israeli occupation interrogators to arm them with specific techniques and programs of torture intended to cause extreme suffering to Palestinian detainees while leaving minimal physical evidence.
Since October 7, investigations and testimonies from survivors of torture, advocates, human rights organizations, and even some Israeli whistleblowers have confirmed that the involvement of Israeli physicians in torture is still ongoing. On April 16, an appalling report by the United Nations Relief and Works Agency on the torture of Gazan detainees stated that when attempting to receive medical assistance to treat injuries caused by torture, Palestinian prisoners were instead beaten more by prison doctors.
#yemen#jerusalem#tel aviv#current events#palestine#free palestine#gaza#free gaza#news on gaza#palestine news#news update#war news#war on gaza#torture#human rights#war crimes#palestine genocide
2K notes
·
View notes
Text
"Growing up, Mackenzee Thompson always wanted a deeper connection with her tribe and culture.
The 26-year-old member of the Choctaw Nation said she grew up outside of her tribe’s reservation and wasn’t sure what her place within the Indigenous community would be.
Through a first-of-its-kind program, Thompson said she’s now figured out how she can best serve her people — as a doctor.
Thompson is graduating as part of the inaugural class from Oklahoma State University’s College of Osteopathic Medicine at the Cherokee Nation. It’s the first physician training program on a Native American reservation and in affiliation with a tribal government, according to school and tribal officials.
“I couldn’t even have dreamed this up,” she said. “To be able to serve my people and learn more about my culture is so exciting. I have learned so much already.”
Thompson is one of nine Native graduates, who make up more than 20 percent of the class of 46 students, said Dr. Natasha Bray, the school’s dean. There are an additional 15 Native students graduating from the school’s Tulsa campus.
The OSU-COM graduates include students from 14 different tribes, including Cherokee, Choctaw, Muscogee, Seminole, Chickasaw, Alaska Native, Caddo, and Osage.
Bray said OSU partnered with the Cherokee Nation to open the school in 2020 to help erase the shortage of Indigenous doctors nationwide. There are about 841,000 active physicians practicing in the United States. Of those, nearly 2,500 — or 0.3 percent — are Native American, according to the Association of American Medical Colleges.
When American Indian and Alaska Native people visit Indian Health Service clinics, there aren’t enough doctors or nurses to provide “quality and timely health care,” according to a 2018 report from the Government Accountability Office. On average, a quarter of IHS provider positions — from physicians to nurses and other care positions –are vacant.
“These students here are going to make a generational impact,” Cherokee Nation Principal Chief Chuck Hoskin Jr. told the students days before graduation. “There is such a need in this state and in this region for physicians and this school was created out of a concern about the pipeline of doctors into our health system.”
The Cherokee Nation spent $40 million to build the college in its capital of Tahlequah. The walls of the campus feature artifacts of Cherokee culture as well as paintings to remember important figures from Cherokee history. An oath of commitment on the wall is written in both English and Cherokee.
The physician training program was launched in the first year of the pandemic.
Bray said OSU and Cherokee leadership felt it was important to have the school in the heart of the Cherokee Nation, home to more than 141,000 people, because students would be able to get experience treating Indigenous patients. In Tahlequah, students live and study in a small town about an hour east of Tulsa with a population of less than 24,000 people.
“While many students learn about the problems facing these rural communities,” Bray said. “Our students are getting to see them firsthand and learn from those experiences.”
While students from the college are free to choose where to complete their residency after graduation, an emphasis is placed on serving rural and Indigenous areas of the country.
There’s also a severe lack of physicians in rural America, a shortage that existed before the COVID-19 pandemic. The Association of American Medical Colleges has projected that rural counties could see a shortage between 37,800 and 124,000 physicians by 2034. An additional 180,000 doctors would be needed in rural counties and other underserved populations to make up the difference.
Bray said OSU saw an opportunity to not only help correct the underrepresentation of Native physicians but also fill a workforce need to help serve and improve health care outcomes in rural populations.
“We knew we’d need to identify students who had a desire to serve these communities and also stay in these communities,” she said.
Osteopathic doctors, or DOs, have the same qualifications and training as allopathic doctors, or MDs, but the two types of doctors attend different schools. While MDs learn from traditional programs, DOs take on additional training at osteopathic schools that focus on holistic medicine, like how to reduce patient discomfort by physically manipulating muscles and bones. DOs are more likely to work in primary care and rural areas to help combat the health care shortages in those areas.
As part of the curriculum, the school invited Native elders and healers to help teach students about Indigenous science and practices...
Thompson said she was able to bring those experiences into her appointments. Instead of asking only standard doctor questions, she’s been getting curious and asking about her patient’s diets, and if they are taking any natural remedies.
“It’s our mission to be as culturally competent as we can,” she said. “Learning this is making me not only a better doctor but helping patients trust me more.”
-via PBS NewsHour, May 23, 2024
#indigenous#native american#cherokee#choctaw#cherokee nation#medical school#united states#doctors#medical news#medical student#cultural competence#cultural heritage#public health#health care#medicine#good news#hope#oklahoma
1K notes
·
View notes
Text


For those who don't know, there's going to be a demonstration for Long Covid on March 15, which is Long Covid Awareness Day since 2023. You can find the LCDC website here.
Their stated goals:
1. Declare Long Covid a National Emergency.
2. Implement Emergency Use Authorization for drug repurposing and trials.
3. Establish annual funding for Long Covid programs and research to find a cure.
4. Ensure racial and gender health equity in research, access to clinical trials, antiviral drug repurposing, preventative measures, educational campaigns, and social services.
5. Enact Clean Indoor Air Laws to prevent SARS-CoV-2 forward transmission in public spaces and forced-congregant settings.
6. Implement respirator use and clean air protections in healthcare facilities. Additionally, devise strategies to ensure immunocompromised patients or those with Long Covid are given reasonable accommodations and are not penalized. Enforce protected class status for people with Long Covid as disabled.
7. Fast-track compassionate allowance and sufficient social support for people with Long Covid in addition to increased funding for Home and Community Based Services.
8. Develop guidelines for physicians on Long Covid and continuing education on breaking research.
9. Acknowledge that Long Covid affects children and implement specialized care immediately.
10. Public tracking of SARS-CoV-2 in wastewater at Publicly Owned Treatment Works and provide affordable PCR testing nationwide.
11. Establish regular White House press communication regarding progress toward stated goals and real time data for Covid transmission awareness.
There's a gofundme here to raise funds for a stage, sound equipment, respirators, and multimedia equipment in order to stream the event to those who can't physically attend. If you can spare a few bucks I encourage you to donate. Any leftover funds will go to Long Covid research.
If you have Long Covid or know someone who does, LCDC is also looking for stories/personal accounts for their media projects.
116 notes
·
View notes
Text
Sen. Elizabeth Warren, D-Mass., "is at long last acknowledging that ObamaCare has increased healthcare prices" and created other unintentional consequences, the Wall Street Journal editorial board wrote Friday.
Warren, who has long supported the Affordable Care Act, the official name for ObamaCare, has recently come to an "epiphany" about "industry consolidation and price increases caused by the healthcare law," per The Journal.
A letter to the Health and Human Services Department inspector general was aimed at determining if "vertically-integrated health care companies are hiking prescription drug costs" and are "evading federal regulations."
In a bipartisan letter, she and Sen. Mike Braun, R-Ind., complained "that the nation’s largest health insurers are dodging ObamaCare’s medical loss ratio (MLR)," according to The Journal.
As Warren describes in the letter, health insurers have exploited the situation, making for "sky-high prescription drug costs and excessive corporate profits."
"In functioning markets, generic drugs cost 80 to 85 percent less than their name-brand equivalents, giving patients much-needed relief from high drug costs and saving taxpayer dollars," Warren wrote. "But patients – including patients in public health care programs like Medicare and Medicaid – who either use or are compelled to use vertically integrated specialty pharmacies are not seeing this relief."
The senators continued: "By owning every link in the chain, a conglomerate like UnitedHealth Group – which includes an insurer, a PBM, a pharmacy, and physician practices – can send inflated medical payments to its pharmacy. Then, by realizing those payments on the pharmacy side – the side that charges for care – rather than the insurance side, the insurance line of business appears to be in compliance with MLR requirements, while keeping more money for itself."
The Journal explained that despite Democrats arguing that the MLR would help patients, "the rule has spurred insurers to merge with or acquire pharmacy benefit managers (PBMs), retail and specialty pharmacies, and healthcare providers."
"This has made healthcare spending less transparent since insurers can shift profits to their affiliates by increasing reimbursements," the board wrote.
Warren has voted against ObamaCare repeal efforts over the years but also pushed for a "Medicare for All" proposal when she ran for president in 2020.
Warren's office and HHS did not immediately respond to a request for comment from Fox News Digital.
99 notes
·
View notes
Text

From Tarek Loubani (@ trklou):
"I want to tell you about Hani, an incredible person and doctor. He was killed with his wife, Dr. Samira Al-Ghefari and their five children, Sherin, Thea (Tota), Sara, Samir, and Wafaa.
Hani just turned 41 years old when he was killed and only a few years into his career as an emergency doctor. He boarded in 2019 and became head of Shifa's ER a few weeks before COVID hit. He met the challenge, helping reconfigure the department for the pandemic.
Hani was a talented Emergency Physician, but Emergency was his second career. Hani was first an accomplished neurosurgeon. In 2009, he was part of the first team to remove a brain tumour in Gaza. This remarkable feat allowed patients to be treated under blockade in Gaza.
These weren't just lifesaving surgeries, but also quality of life ones like spinal canal widening. When I met Hani in 2011, I just turned thirty and he was about to. I was beginning my career and he already got bored with his. We served in the ER during the 2012 war together.
He felt he could make a bigger impact in the ER, especially during wars. He joined the board program, and for four years after, he was one of our students. It was obvious he should become the new chief of Shifa's emergency department, a job we had to convince him to take.
In 2021, he led the department through a war. Over the past two months, he served fearlessly, among the last doctors out of Shifa as Israel besieged it. He miraculously escaped arrest as he left, which may be why he was assassinated with his family.
His wife, Dr. Samira Al-Ghefari, was an accomplished doctor in her own right. While raising five children, she got a Master's degree in 2019. She cared deeply about women's health and primary care. I didn't know her well, but I knew enough to be in awe.

His children were killed with him, beautiful and vibrant balls of energy who I only met briefly during visits to Hani's home to talk shop. Samir celebrated his 7th birthday on Nov 14th, hungry and afraid as Israel's bombs fell, not knowing if he would ever see his father again.

In 2020, Hani wrote, "We belong to our nation. In it we'll stay. We were born here; raised here; were students and spent our nights studying here. We worked here. We had a duty, and we honoured it. This nation is carried forward through selfless sacrifice, toil, and perseverance."
Rest in Peace, Hani"
37 notes
·
View notes
Link
TSC News TV host Fred Richani interviews Saving AlGeneina Initiative manager Sadeia Hamid about her grassroots organization helping Sudanese refugees and internally displaced peoples within Sudan and Chad, the Sudanese crisis encompassing war, genocide, famine, and occupation, the instability before/during/after former President Omar al-Bashir, as well as how YOU can help donate volunteer for this amazing cause.
✅Donation: https://linktr.ee/SavingAlGeneina
✅Donate via PayPal: https://www.paypal.com/paypalme/SadeiaAli
✅Saving AlGeneina IG: https://www.instagram.com/saving.algeneina
✅TikTok: https://www.tiktok.com/@savingalgeneina
✅Twitter/X: https://x.com/sadiea8
00:00 Introducing Sadeia Hamid and Saving AlGeneina Initiative
03:48 Sudan's instability, war since 2023
05:24 Evacuating Sudanese refugees, Chadian border, displacement
06:35 Sudan under illegal occupation, massacres
08:03 Sudanese famine, plagues
10:15 United Nations not helping Sudan, Doctors Without Borders
13:56 Sudan has no real government, shady nonprofit organizations
14:56 Saving AlGeneina's initiatives - medical clinics, food, sports
15:35 Partnering with Sudanese American Physicians Association, famine
17:24 Saving AlGeneina Initiative's sports programs for children, mental health
19:00 Sadeia Hamid on building mobile medical clinic for Sudanese refugees
20:38 Sudanese children's trauma, lack of schools, education
22:36 Challenges with getting aid into Sudan
23:41 Difficulty registering Saving AlGeneina Initiative in Sudan
25:34 Don't turn your back on Sudan, Keep Eyes on Sudan
26:25 Donate and volunteer to Saving AlGeneina Initiative
#keep eyes on sudan#saving algeneina initiative#tsc news#tsc gaming ent#mnn#fred richani#sapa#sudanese american physicians association#msf#doctors without borders#sudan#sudanese#richani#tsc
16 notes
·
View notes
Text
If You Don't Know Medicare Advantage Is a Scam, You're Not Paying Attention
We’re on the edge of the open enrollment period for Medicare, and the Advantage scammers will be carpet-bombing America with advertisements over the next few months. Don't be fooled about what it is—and who is profiting.
Thom Hartmann
Oct 07, 2023
Common Dreams
President George W. Bush and Republicans (and a handful of on-the-take Democrats) in Congress created the Medicare Advantage scam in 2003 as a way of routing hundreds of billions of taxpayer dollars into the pockets of for-profit insurance companies.
Those companies, and their executives, then recycle some of that profit back into politicians’ pockets via the Citizens United legalized bribery loophole created by five corrupt Republicans on the Supreme Court.
Just the overcharges happening right now in that scam are costing Americans over $140 billion a year: more than the entire budget for the Medicare Part B or Part D programs. These ripoffs — that our federal government seems to have no interest in stopping — are draining the Medicare trust fund while ensnaring gullible seniors in private insurance programs where they’re often denied life-saving care.
Real Medicare pays bills when they’re presented. Medicare Advantage insurance companies, on the other hand, get a fixed dollar amount every year for each of the people enrolled in their programs, regardless of how much they spent on each customer.
As a result, Medicare Advantage programs make the greatest profits for their CEOs and shareholders when they actively refuse to pay for care, something that happens frequently. It’s a safe bet that nearly 100 percent of the people who sign up for Advantage programs don’t know this and don’t have any idea how badly screwed they could be if they get seriously ill.
Not only that, when people do figure out they’ve been duped and try to get back on real Medicare, the same insurance companies often punish them by refusing to write Medigap plans (that fill in the 20% hole in real Medicare). They can’t do that when you first sign up when you turn 65, but if you “leave” real Medicare for privatized Medicare Advantage, it can be damn hard to get back on it.
The doctors’ group Physicians for a National Health Program (PNHP) just published a shocking report on the extent of the Medicare Advantage ripoffs — both to individual customers and to Medicare itself — that every American should know about.
The report, titled Our Payments, Their Profits, opens with this shocking exposé:
“By our estimate, and based on 2022 spending, Medicare Advantage overcharges taxpayers by a minimum of 22% or $88 billion per year, and potentially by up to 35% or $140 billion. By comparison, Part B premiums in 2022 totaled approximately $131 billion, and overall federal spending on Part D drug benefits cost approximately $126 billion. Either of these — or other crucial aspects of Medicare and Medicaid — could be funded entirely by eliminating overcharges in the Medicare Advantage program.
“Medicare Advantage, also known as MA or Medicare Part C, is a privately administered insurance program that uses a capitated payment structure, as opposed to the fee-for-service (FFS) structure of Traditional Medicare or TM. Instead of paying directly for the health care of beneficiaries, the federal government gives a lump sum of money to a third party (generally a commercial insurer) to ‘manage’ patient care.”
With real Medicare and a Medigap plan, you talk with your physician or hospital and decide on your treatment, they bill Medicare, and you never see or hear about the bill. There is nobody between you and your physician or hospital and Medicare only goes after the payment they’ve made if they sniff out a fraud.
With Medicare Advantage, on the other hand, your insurance company gets a lump-sum payment from Medicare every year and keeps the difference between what they get and what they pay out. They then insert themselves between you and your doctor or hospital to avoid paying for whatever they can.
Whatever you decide on regarding treatment, many Advantage insurance company will regularly second-guess and do everything they can to intimidate you into paying yourself out-of-pocket. Often, they simply refuse payment and wait for you to file a complaint against them; for people seriously ill the cumbersome “appeals” process is often more than they can handle.
As a result, hospitals and doctor groups across the nation are beginning to refuse to take Medicare Advantage patients. California-based Scripps Health, for example, cares for around 30,000 people on Medicare Advantage and recently notified all of them that Scripps will no longer offer medical services to them unless they pay out-of-pocket or revert back to real Medicare.
They made this decision because over $75 million worth of services and procedures their physicians had recommended to their patients were turned down by Medicare Advantage insurance companies. In many cases, Scripps had already provided the care and is now stuck with the bills that the Advantage companies refuse to pay.
Scripps CEO Chris Van Gorder told MedPage Today:
“We are a patient care organization and not a patient denial organization and, in many ways, the model of managed care has always been about denying or delaying care – at least economically. That is why denials, [prior] authorizations and administrative processes have become a very big issue for physicians and hospitals...”
Similarly, the Mayo Clinic has warned its customers in Florida and Arizona that they won’t accept Medicare Advantage any more, either. Increasing numbers of physician groups and hospitals are simply over being ripped off by Advantage insurance companies.
Not only is the Medicare Advantage scam a screw job for healthcare providers and people who are on the programs and are unfortunate enough to get sick, it’s also preventing Americans from getting expanded benefits from real Medicare.
As the PNHP report notes, for real Medicare to provide comprehensive vision, dental, and hearing benefits to all Medicare recipients would cost the system around $84 billion a year, according to the Congressional Budget Office.
Instead, though, the Medicare system is burdened with at least that amount of money in over-payments to Medicare Advantage providers — over-payments that have no health benefit whatsoever and merely inflate the companies’ profits.
A hundred billion dollars in excess profits can be put to a lot of uses, and the health insurance industry is quite good at it. The former CEO of UnitedHealth, “Dollar” Bill McGuire, for example, made off with over $1.5 billion dollars for his efforts.
And, because five corrupt Republicans on the Supreme Court legalized political bribery with their Citizens United decision, some of these companies allocate millions every year (a mere drop in the bucket) to pay off loyal members of Congress and to dangle high-paying future jobs to high-level employees of CMS who have the power to keep the gravy train going and thwart prosecutions.
As PNHP noted:
“Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American health care, siphoning money from vulnerable patients while delaying and denying necessary and often life-saving treatment. While there is obvious reason to fix these issues in MA and to expand Traditional Medicare for the sake of all beneficiaries, the deep structural problems with our health care system will only be fixed when we achieve improved Medicare for All.”
We’re on the edge of the open enrollment period for Medicare, and the Advantage scammers will be carpet-bombing America with advertisements over the next few months. Representatives Pocan, Khanna, and Schakowsky have introduced the “Save Medicare Act” that would ban Advantage companies from using the word Medicare in their advertising.
They made a video about it that’s well worth sharing with friends and family:
youtube
As Schakowsky, Khanna, and Pocan note, “Only Medicare is Medicare.” Don’t be fooled by the Medicare Advantage scam.
And now that you know, pass it on and save somebody else’s health!
41 notes
·
View notes
Text


Tuskegee Syphilis Experiment
Acting on the presumption that rural southern blacks were generally more promiscuous and syphilitic than whites, and without sufficient funding to establish an effective treatment program for them, doctors working with the Public Health Service (PHS) commenced a multi-year experiment in 1932.
Their actions deprived 400 largely uneducated and poor African Americans in Tuskegee, Alabama of proper and reasonable treatment for syphilis, a disease whose symptoms could easily have been relieved with the application of penicillin which became available in the 1940s.
Patients were not told they had syphilis nor were they provided sufficient medication to cure them. More than 100 men died due to lack of treatment while others suffered insanity, blindness and chronic maladies related to the disease.
The original experiment took on a life of its own as physicians, intrigued by the prospect of gathering scientific data, ignored human rights and ethical considerations and managed to extend it until 1972 when a PHS researcher Peter Buxtun revealed its history to the press. Public exposure embarrassed the scientific community and the government and the experiment was quickly shut down.
Attorney Fred Gray initiated a lawsuit on behalf of the patients. In an out-of-court settlement each surviving patient received medical treatment and $40,000 in compensation.
In the wake of the scandal Congress passed the National Research Act of 1974 which required more stringent oversight of studies employing human subjects.
In 1997, on behalf of the federal government, President Bill Clinton issued a formal apology to the victims of the Tuskegee Syphilis Experiment.
•••
Experimento de Tuskegee (Sífilis)
Actuando bajo la presunción de que los negros en las áreas rurales del sur eran generalmente mas promiscuos y sifilíticos que los blancos, y sin tener los fondos suficientes para establecer un programa de tratamiento efectivo, los doctores que trabajaban para el Servicio de Salud Publica comenzaron un experimento que duró varios años en el año 1932.
Sus acciones privaron a cuatrocientos afroamericanos de un tratamiento adecuado y razonable para el sífilis, una enfermedad cuyos síntomas podrían haberse aliviado fácilmente con la aplicación de penicilina, la cual estuvo disponible en la década de 1940.
A los pacientes no se les dijo que tenían sífilis, tampoco se les brindó suficiente medicamento para curarlos. Mas de cien hombres fallecieron debido a la falta de medicamento, mientras que otros sufrían demencia, ceguera y otras enfermedades crónicas relacionadas con la enfermedad.
El experimento original cobró vida propia cuando los médicos, intrigados por la perspectiva de recopilar datos científicos, ignoraron los derechos humanos y las consideraciones éticas y lograron extenderlo hasta 1972 En este año es cuando un investigador del Servicio de Salud Pública, Peter Buxtun, reveló su historia a la prensa. La exposición pública avergonzó a la comunidad científica y al gobierno y el experimento fue rápidamente cancelado.
El abogado Fred Gray inició una demanda en nombre de los pacientes. En un acuerdo extrajudicial, cada paciente que sobrevivió, recibió tratamiento médico y 40,000 dólares de indemnización.
A raíz del escándalo, el Congreso aprobó la Ley de Investigación Nacional de 1974, que exige una supervisión más estricta de los estudios que utilizan sujetos humanos.
En 1997, en nombre del gobierno federal, el presidente Bill Clinton emitió una disculpa formal a las víctimas del Experimento de Sífilis de Tuskegee.
#medical segregation#medical apartheid#medical#medicine#Tuskegee#medication#knowyourhistory#black history is everybody's history#historyfacts#black history is world history#black history is american history#history#blackhistorymonth#black history#black history month#historia#medicina#enfermedad#blackhistory#bill clinton#blacklivesmatter#blacklivesalwaysmatter#blackpeoplematter#blackhistoryyear#spanish#español#segregation#culture#black history 2024#read
12 notes
·
View notes
Text
By Jake Johnson
Common Dreams
Oct. 4, 2023
"Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare," says a new report from Physicians for a National Health Program.
A report published Wednesday estimates that privately run, government-funded Medicare Advantage plans are overcharging U.S. taxpayers by up to $140 billion per year, a sum that could be used to completely eliminate Medicare Part B premiums or fully fund Medicare's prescription drug program.
Physicians for a National Health Program (PNHP), an advocacy group that supports transitioning to a single-payer health insurance system, found that Medicare Advantage (MA) overbills the federal government by at least $88 billion per year, based on 2022 spending.
That lower-end estimate accounts for common MA practices such as upcoding, whereby diagnoses are piled onto a patient's risk assessment to make them appear sicker than they actually are, resulting in a larger payment from the federal government.
But when accounting for induced utilization—"the idea that people with supplemental coverage are likely to use more health care because their insurance pays for more of their cost"—PNHP estimated that the annual overbilling total could be as high as $140 billion.
"This is unconscionable, unsustainable, and in our current healthcare system, unremarkable," says the new report. "Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare, siphoning money from vulnerable patients while delaying and denying necessary and often lifesaving treatment."
Even if the more conservative figure is accurate, PNHP noted, the excess funding that MA plans are receiving each year would be more than enough to expand traditional Medicare to cover dental, hearing, and vision. Traditional Medicare does not currently cover those benefits, which often leads patients to seek out supplemental coverage—or switch to an MA plan.
The Congressional Budget Office has estimated that adding dental, vision, and hearing to Medicare and Medicaid would cost just under $84 billion in the most costly year of the expansion.
"While there is obvious reason to fix these issues in MA and to expand traditional Medicare for the sake of all beneficiaries," the new report states, "the deep structural problems with our healthcare system will only be fixed when we achieve improved Medicare for All."
Bolstered by taxpayer subsidies, Medicare Advantage has seen explosive growth since its creation in 2003 even as it has come under fire for fraud, denying necessary care, and other abuses. Today, nearly 32 million people are enrolled in MA plans—more than half of all eligible Medicare beneficiaries.
Earlier this year, the Biden administration took steps to crack down on MA overbilling, prompting howls of protest and a furious lobbying campaign by the industry's major players, including UnitedHealth Group and Humana. Relenting to industry pressure, the Biden administration ultimately agreed to phase in its rule changes over a three-year period.
Leading MA providers have also faced backlash from lawmakers for handing their top executives massive pay packages while cutting corners on patient care and fighting reforms aimed at rooting out overbilling.
As PNHP's new report explains, MA plans are paid by the federal government as if "their enrollees have the same health needs and require the same levels of spending as their traditional Medicare counterparts," even though people who enroll in MA plans tend to be healthier—and thus have less expensive medical needs.
"There are several factors that potentially contribute to this phenomenon," PNHP's report notes. "Patients who are sicker and thus have more complicated care needs may be turned off by limited networks, the use of prior authorizations, and other care denial strategies in MA plans. By contrast, healthier patients may feel less concerned about restrictions on care and more attracted to common features of MA plans like $0 premiums and additional benefits (e.g. dental and vision coverage, gym memberships, etc.). Insurers can also use strategies such as targeted advertising to reach the patients most favorable to their profit margins."
A KFF investigation published last month found that television ads for Medicare Advantage "comprised more than 85% of all airings for the open enrollment period for 2023."
"TV ads for Medicare Advantage often showed images of a government-issued Medicare card or urged viewers to call a 'Medicare' hotline other than the official 1-800-Medicare hotline," KFF noted, a practice that has previously drawn scrutiny from the U.S. Senate and federal regulators.
PNHP's report comes days after Cigna, a major MA provider, agreed to pay $172 million to settle allegations that it submitted false patient diagnosis data to the federal government in an attempt to receive a larger payment.
Dr. Ed Weisbart, PNHP's national board secretary, toldThe Lever on Wednesday that such overpayments are "going directly into the profit lines of the Medicare Advantage companies without any additional health value."
"If seniors understood that the $165 coming out of their monthly Social Security checks was going essentially dollar for dollar into profiteering of Medicare Advantage, they would and should be angry about that," said Weisbart. "We think that we pay premiums to fund Medicare. The only reason we have to do that is because we're letting Medicare Advantage take that money from us."
13 notes
·
View notes
Text
House Speaker Mike Johnson on Wednesday appointed two far-right Republicans to the powerful House Intelligence Committee, positioning two close allies of Donald Trump who worked to overturn the 2020 presidential election on a panel that receives sensitive classified briefings and oversees the work of America’s spy agencies.
The appointments of GOP Reps. Scott Perry of Pennsylvania and Ronny Jackson of Texas to the House Intelligence Committee were announced on the House floor Wednesday. Johnson, a hardline conservative from Louisiana who has aligned himself with Trump, was replacing spots on the committee that opened up after the resignations of Republican Reps. Mike Gallagher of Wisconsin and Chris Stewart of Utah.
Committee spots have typically been given to lawmakers with backgrounds in national security and who have gained respect across the aisle. But the replacements with two close Trump allies comes as Johnson has signaled his willingness to use the full force of the House to aid Trump’s bid to reclaim the Oval Office. It also hands the hard-right faction of the House two coveted spots on a committee that handles the nation’s secrets and holds tremendous influence over the direction of foreign policy.
Trump has long displayed adversarial and flippant views of the U.S. intelligence community, flouted safeguards over classified information and directly berated law enforcement agencies like the FBI. The former president faces 37 felony counts for improperly storing in his Florida estate sensitive documents on nuclear capabilities, repeatedly enlisting aides and lawyers to help him hide records demanded by investigators and cavalierly showing off a Pentagon “plan of attack” and classified map.
Johnson did not release a statement on his picks for the committee.
Perry, who formerly chaired the ultraconservative House Freedom Caucus, was ordered by a federal judge last year to turn over more than 1,600 texts and emails to FBI agents investigating efforts to keep Trump in office after his 2020 election loss and illegally block the transfer of power to Democrat Joe Biden.
Perry’s personal cellphone was also seized by federal authorities who have explored his role in helping install an acting attorney general who would be receptive to Trump’s false claims of election fraud.
Perry and other conservatives have also pushed Congress to curtail a key U.S. government surveillance tool. They want to restrict the FBI’s ability to use the program to search for Americans’ data.
“I look forward to providing not only a fresh perspective, but conducting actual oversight — not blind obedience to some facets of our Intel Community that all too often abuse their powers, resources, and authority to spy on the American People,” Perry said in a statement.
Jackson, who was elected to the House in 2020, was formerly a top White House physician under former presidents Barack Obama and Trump. Known for his over-the-top pronouncements about Trump’s health, Jackson was nominated by Trump to be the secretary of Veterans Affairs.
He withdrew his nomination amid allegations of professional misconduct. An internal investigation at the Department of Defense later concluded that Jackson made “sexual and denigrating” comments about a female subordinate, violated the policy on drinking alcohol on a presidential trip and took prescription-strength sleeping medication that prompted worries from his colleagues about his ability to provide proper medical care.
Jackson has denied those allegations and described them as politically motivated.
The House committee that investigated the Jan. 6 insurrection at the Capitol also requested testimony from Jackson as it looked into lawmakers’ meetings at the White House, direct conversations with Trump as he sought to challenge his election loss and the planning and coordination of rallies. Jackson declined to testify.
The presence of Jackson and Perry on the committee could damage the trust between the president and the committee in handling classified information, said Ira Goldman, a former Republican congressional aide who worked as a counsel to the intelligence committee in the 1970s and 1980s.
He said, “You’re giving members seats on the committee when, based on the public record, they couldn’t get a security clearance if they came through any other door.”
#us politics#news#republicans#conservatives#gop#us house of representatives#house intelligence committee#2024#rep. Mike Johnson#rep. Scott Perry#rep. Ronny Jackson#donald trump#fbi#us intelligence#house freedom caucus#Ira Goldman
23 notes
·
View notes
Text
Shira Fishbach, a newly graduated physician, was sitting in an orientation session for her first year of medical residency when her phone started blowing up. It was June 24, 2022, and the US Supreme Court had just handed down its decision in Dobbs v. Jackson Women's Health Organization, nullifying the national right to abortion and turning control back to state governments.
Fishbach was in Michigan, where an abortion ban enacted in 1931 instantly came into effect. That law made administering an abortion a felony punishable by four years in prison, with no exceptions for rape or incest. It was a chilling moment: Her residency is in obstetrics and gynecology, and she viewed mastering abortion procedures as essential to her training.
“I suspected during my application cycle that this could happen, and to receive confirmation of it was devastating,” she recalls. “But I had strategically applied where I thought that, even if I didn't receive the full spectrum, I would at least have the support and the resources to get myself to an institution that would train me.”
Her mind whirled through the possibilities. Would her program help its residents go to an access-protecting state? Could she broker an agreement to go somewhere on her own, arranging weeks of extra housing and obtaining a local medical license and insurance? Would she still earn her salary if she left her program—and how would she fund her life if she did not?
In the end, she didn’t need to leave. That November, Michigan voters approved an amendment to the state constitution that made the 1931 law unenforceable, and this April, Governor Gretchen Whitmer repealed the ban. Fishbach didn’t have to abandon the state to learn the full range of ob-gyn care. In fact, her program at the University of Michigan, where she’s now a second-year resident, pivoted to making room for red-state trainees.
But the dizzying reassessment she underwent a year ago provides a glimpse of the challenges that face thousands of new and potential doctors. Almost 45 percent of the 286 accredited ob-gyn programs in the US now operate under revived or new abortion bans, meaning that more than 2,000 residents per year—trainee doctors who have committed to the specialty—may not receive the required training to be licensed. Among students and residents, simmering anger over bans is growing. Long-time faculty fear the result will be a permanent reshaping of American medicine, driving new doctors from red states to escape limitations and legal threats, or to protect their own reproductive options. That would reduce the number of physicians available, not just to provide abortions, but to conduct genetic screenings, care for miscarriages, deliver babies, and handle unpredictable pregnancy risks.
“I worry that we’re going to see an increase in maternal morbidity, differentially, depending on where you live,” says Kate Shaw, a physician and associate chair of ob-gyn education at Stanford Medicine. “And that’s just going to further enhance disparities that already exist.”
Those effects are not yet visible. The pipeline that ushers medical graduates through physician training is about a decade long: four years of school plus three to seven years of residency, sometimes with a two-year, sub-specialty fellowship afterward. Thus actions taken in response to the Dobbs decision—people eschewing red-state schools or choosing to settle in blue states long-term—might take a while to be noticeable.
But in this year, some data has emerged that suggests trends to come. In February, a group of students, residents and faculty surveyed 2,063 licensed and trainee physicians and found that 82 percent want to work or train in states that retain abortion access—and 76 percent would refuse to apply in states that restrict it. (The respondents worked in a mix of specialties; for those whose work would include performing abortions, the proportion intending to work where it remains legal soared above 99 percent.)
Then in April, a study from the Association of American Medical Colleges drawing on the first round of applications to residency programs after Dobbs found that ob-gyn applications in states with abortion restrictions sank by 10 percent compared to the previous year. Applications to all ob-gyn programs dropped by 5 percent. (Nationwide, all applications to residency went down 2 percent from 2021 to 2022.)
Last month, two preliminary pieces of research presented at the annual meeting of the American College of Obstetricians and Gynecologists uncovered more perturbations. In Texas—where the restrictive law SB8 went into effect in September 2021, nine months before Dobbs—a multi-year upward trend in applications to ob-gyn residency slowed after the law passed. And in an unrelated national survey, 77 percent of 494 third- and fourth-year medical students said that abortion restrictions would affect where they applied to residency, while 58 percent said they were unlikely to apply to states with a ban.
That last survey was conducted by Ariana Traub and Kellen “Nell” Mermin-Bunnell, two third-year medical students at Emory University School of Medicine in Atlanta—which lies within a state with a “fetal heartbeat” law that predates Dobbs and that criminalizes providing an abortion after six weeks of pregnancy. The law means that students in clinical rotations are unlikely to witness abortions and would not be allowed to discuss the procedure with patients. It also means that, if either of them were to become pregnant while at med school, they would not have that option themselves.
Before they published the survey, the two friends conducted an analysis of how bans would affect medical school curricula, using data collected in the summer of 2022. They predicted that only 29 percent of the more than 129,000 medical students in the US would not be affected by state bans. The survey gave them a chance to sample med students’ feelings about those developments, with the help of faculty members. They also founded a nonprofit, Georgia Healthcare Professionals for Reproductive Justice. “We're in a unique position, as individuals in the health care field but not necessarily medical professionals yet,” Traub says. “We have some freedom. So we felt like we had to use that power to try to make change.”
Ob-gyn formation is caught between opposing forces. Just over half of US states have passed bans or limitations on abortion that go beyond the Roe v. Wade standard of fetal viability. But the Accreditation Council for Graduate Medical Education, a nonprofit that sets standards for residency and fellowship programs, has always required that obstetric trainees learn to do abortions, unless they opt out for religious or moral reasons. It reaffirmed that requirement after the Dobbs decision. Failure to provide that training could cause a program to lose accreditation, leaving its graduates ineligible to be licensed.
The conflict between what medicine demands and state laws prevent leaves new and would-be doctors in restrictive states struggling with their inability to follow medical evidence and their own best intentions. “I’m starting to take care of patients for the first time in my life,” says Mermin-Bunnell, Traub’s survey partner. “Seeing a human being in front of you, who needs your help, and not being able to help them or even talk to them about what their options might be—it feels morally wrong.”
That frustration is equally evident among trainees in specialties who might treat a pregnant person, prescribe treatments that could imperil a pregnancy, or care for a pregnancy gone wrong. Those include family and adolescent medicine, anesthesiology, radiology, rheumatology, even dermatology and mental health.
“I’m particularly interested in oncology, and I’ve come to realize that you can’t have the full standard of gynecologic oncology care without being able to have access to abortion care,” says Morgan Levy, a fourth-year medical student in Florida who plans to apply to ob-gyn residency. Florida currently bans abortion after 15 weeks; a further ban, down to six weeks, passed in April but has been held up by legal challenges. In three years of med school so far, Levy received one lecture on abortion—in the context of miscarriage—and no clinical exposure to the procedure. “It is a priority for me to make sure that I get trained,” she says.
But landing in a training program that encourages abortion practice is more difficult than it looks. Residency application is an algorithm-driven process in which graduates list their preferred programs, and faculty rank the trainees they want to teach. For years, there have been more applicants than there are spaces—and this year, as in the past, ob-gyn programs filled almost all their slots. What that means, according to faculty members, is that some applicants will end up where they do not want to be.
“Students and trainees do exert their preferences, but they also need to get a training spot,” says Vineet Arora, the dean for medical education at the University of Chicago Pritzker School of Medicine and lead author on the survey published in February. “Would they forgo a training spot because of Dobbs? That's a tall order, especially in a competitive field. But would they be happy about it? And would they want to stay there long term?”
That is not a hypothetical question. According to the medical-colleges association, more than half of residents stay to practice in the states where they trained. But it’s reasonable to ask whether they would feel that loyalty if they were deprived of training or forced to relocate. “If even a portion of the 80 percent of people who prefer to practice and train in states that don't have abortion bans follow through on those preferences, those states that are putting in abortion bans—which often have workforce shortages already—will be in a worse situation,” Arora says.
An ACOG analysis estimated in 2017 that half of US counties, which are home to 10 million women, have no practicing ob-gyn. When the health care tech firm Doximity examined ob-gyn workloads in 2019, seven of the 10 cities it identified as having the highest workloads lie in what are now very restrictive states. Those shortages are likely to worsen if new doctors relocate to states where they feel safe. The legal and consulting firm Manatt Health predicted in a white paper last fall: “The impact on access to all OB/GYN care in certain geographies could be catastrophic.”
Faculty are struggling to solve the mismatch between licensing requirements and state prohibitions by identifying other ways residents can train. They view it as protecting the integrity of medical practice. “Any ob-gyn has to be able to empty the uterus in an emergency, for abortion, for miscarriage, and for pregnancy complications or significant medical problems,” says Jody Steinauer, who is vice-chair of ob-gyn education at UC San Francisco.
Steinauer directs the Kenneth J. Ryan Residency Training Program, a 24-year-old effort to install and reinforce clinical abortion training. Even before Dobbs, that was hard to come by: In 2018, Steinauer and colleagues estimated that only two-thirds of ob-gyn residency programs made it routine, despite accreditation requirements—and that anywhere from 29 to 78 percent of residents couldn’t competently perform different types of abortion when they left training. In 2020, researchers from UCSF and UC Berkeley documented that 57 percent of these programs face limitations set by individual hospitals more extreme than those set by states.
Before Dobbs, the Ryan program brokered individual relocations that let trainees temporarily transfer to other institutions. Now it is working to set up program-to-program agreements instead, because the logistics required to visit for a rotation—the kind of arrangements Fishbach dizzily imagined a year ago—are more complex than most people can manage on their own. And not only on the visiting trainee: Programs already perform delicate calculations of how many trainees they can take given the number of patients coming to their institutions and the number of faculty mentors.
Only a few places have managed to institutionalize “away rotations,” in which they align accreditation milestones, training time, and financing with other institutions. Oregon Health & Science University’s School of Medicine is about to open a formal program that will accept 10 to 12 residents from restrictive states for a month each over a year. Oregon imposes no restrictions on abortion, and both the med school’s existing residents and the university’s philanthropic foundation supported the move.
“I'm very concerned about having a future generation that knows how to provide safe abortion care—because abortion will never go away; becoming illegal only makes it less safe,” says Alyssa Colwill, who oversees the new program and is an assistant professor of obstetrics and gynecology. “There are going to be patients that are going to use unsafe methods because there's no other alternative. And providers are going to be placed in scenarios that are heartbreaking, and are devastating to watch.”
The accreditation council now requires programs that cannot train their own residents in abortion to support them in traveling somewhere else. But even at schools that are trying to accommodate as many learners as possible, trainees can attend for only a month—the maximum that fully enrolled programs in safe states can afford. After that, they must go back home, leaving them less-trained than their counterparts. As faculty look forward, they fear a slow spiral of decay in obstetric knowledge.
This isn’t imaginary: Already, research has shown that physicians practicing in red states are less likely to offer appropriate and legal procedures to treat miscarriages. Receiving abortion training, in other words, also improves medical care for pregnancy loss.
“Ultimately, I do not think there is capacity to train every resident who wants training,” says Charisse Loder, a clinical assistant professor of ob-gyn at the University of Michigan Medical School, who directs the program where Fishbach is training. “So we will have ob-gyn residents who are not trained in this care. And I think that is not only unfortunate, but puts patients in a position of being cared for by residents who don't have comprehensive training.”
Doing only short rotations also returns residents to places where their own reproductive health could be put at risk. Future physicians are likely to be older than in previous generations, having been encouraged to get life experience and sample other careers before entering med school. Research on which Levy and Arora collaborated in 2022 shows that more than 11 percent of new physicians had abortions during their training. Because of the length of training, they also may be more likely to use IVF when they are ready to start families—and some reproductive technologies may be criminalized under current abortion bans.
As a fourth and final-year psychiatry resident, Simone Bernstein had thought about abortion restrictions through the lens of her patients’ mental health, as she talked to them about fertility treatment and pregnancy loss. As cofounder of the online platform Inside the Match, she had listened to residents’ reactions to Dobbs (and collaborated on research with Levy and Arora). She had not expected the decision to affect her personally—but she is in Missouri, a state where there is an almost complete ban on abortion. And this spring, she experienced a miscarriage at 13 weeks of pregnancy.
“I was worried whether or not I could even go to the hospital, if my baby still had a heartbeat, which was a conversation that I had to have with my ob-gyn on the phone,” she says. “It didn’t come to that; I caught the baby in my hands at home, hemorrhaging blood everywhere, and the baby had already passed away. But until that moment, I didn't recognize the effects that [abortion restrictions] could have on me.”
This is the reality now: There exist very few places in the US where abortion is uncomplicated. Faculty and their trainees do not expect that to change, except for the worse. Staying in the field, and making sure the next generation is prepared, requires commitment that they will have to sustain for years.
“Part of the reason why I sought advanced training in abortion and contraception is because I think there will be a national ban,” says Abigail Liberty, an ob-gyn and fellow in her sixth postgraduate year at OHSU. “I think it will happen in our lifetime. And I see my role as getting as much expertise and training as I can now and providing care while I can. And then coming out of retirement, when abortion will be legal again, and training the next generation of physicians.”
49 notes
·
View notes
Text
"In the oldest and most prestigious young adult science competition in the nation, 17-year-old Ellen Xu used a kind of AI to design the first diagnosis test for a rare disease that struck her sister years ago.
With a personal story driving her on, she managed an 85% rate of positive diagnoses with only a smartphone image, winning her $150,000 grand for a third-place finish.
Kawasaki disease has no existing test method, and relies on a physician’s years of training, ability to do research, and a bit of luck.
Symptoms tend to be fever-like and therefore generalized across many different conditions. Eventually if undiagnosed, children can develop long-term heart complications, such as the kind that Ellen’s sister was thankfully spared from due to quick diagnosis.
Xu decided to see if there were a way to design a diagnostic test using deep learning for her Regeneron Science Talent Search medicine and health project. Organized since 1942, every year 1,900 kids contribute adventures.
She designed what is known as a convolutional neural network, which is a form of deep-learning algorithm that mimics how our eyes work, and programmed it to analyze smartphone images for potential Kawasaki disease.
However, like our own eyes, a convolutional neural network needs a massive amount of data to be able to effectively and quickly process images against references.
For this reason, Xu turned to crowdsourcing images of Kawasaki’s disease and its lookalike conditions from medical databases around the world, hoping to gather enough to give the neural network a high success rate.
Xu has demonstrated an 85% specificity in identifying between Kawasaki and non-Kawasaki symptoms in children with just a smartphone image, a demonstration that saw her test method take third place and a $150,000 reward at the Science Talent Search."
-Good News Network, 3/24/23
#heart disease#pediatrics#healthcare#kawasaki#neural network#ai#science and technology#rare disease#medical tests#medical science#good news#hope
75 notes
·
View notes
Text
Text from the Washington Post
DYING EARLY AMERICA’S LIFE EXPECTANCY CRISIS
STRESS IS WEATHERING OUR BODIES FROM THE INSIDE OUT
By Akilah Johnson and
Charlotte Gomez
Oct. 17 at 6:00 a.m.
Link to article here - paywall warning. Use 12.io or other paywall buster.
Physicians and public health experts have pointed to one culprit time and again when asked why Americans live shorter lives than peers in nations with similar resources, especially people felled by chronic diseases in the prime of life: stress.
A cardiologist, endocrinologist, obesity specialist, health economist and social epidemiologists all said versions of the same thing: Striving to get ahead in an unequal society contributes to people in the United States aging quicker, becoming sicker and dying younger.
Recent polls show adults are stressed by factors beyond their control, including inflation, violence, politics and race relations. A spring Washington Post-Ipsos poll found 50 percent of Americans said not having enough income was a source of financial stress; 55 percent said not having enough savings was also a source of stress.
“We should take a step back and look at the society we’re living in and how that is actually determining our stress levels, our fatigue levels, our despair levels,” said Elizabeth H. Bradley, president of Vassar College and co-author of the book “The American Health Care Paradox.” “That’s for everybody. Health is influenced very much by these factors, so that’s why we were talking about a reconceptualization of health.”
The Washington Post’s efforts to gain a deeper understanding of how stress can cause illness, disability and shorter lives led to a once derided body of research that has become part of the mainstream discussion about improving America’s health: the Weathering Hypothesis.
Stress is a physiological reaction that is part of the body’s innate programming to protect against external threats.
When danger appears, an alarm goes off in the brain, activating the body’s sympathetic nervous system — the fight-or-flight system. The hypothalamic-pituitary-adrenal axis is activated. Hormones, such as epinephrine and cortisol, flood the bloodstream from the adrenal glands.
The heart beats faster. Breathing quickens. Blood vessels dilate. More oxygen reaches large muscles. Blood pressure and glucose levels rise. The immune system’s inflammatory response activates, promoting quick healing.
Once the threat passes, hormone levels return to normal, blood glucose recedes, and heart rate and blood pressure return to baseline. That’s how the human body should work.
Life brings an accumulation of unremitting stress, especially for those subjected to inequity — and not just from immediate and chronic threats. Even the anticipation of those menaces causes persistent damage.
The body produces too much cortisol and other stress hormones, straining to bring itself back to normal. Eventually, the body’s machinery malfunctions.
Like tree rings, the body remembers.
The constant strain — the chronic sources of stress — resets what is “normal,” and the body begins to change.
It is the repeated triggering of this process year after year — the persistence of striving to overcome barriers — that leads to poor health.
Blood pressure remains high. Inflammation turns chronic. In the arteries, plaque forms, causing the linings of blood vessels to thicken and stiffen. That forces the heart to work harder. It doesn’t stop there. Other organs begin to fail.
Struggling and striving
It’s part of the weathering process, a theory first suggested by Arline T. Geronimus, a professor and population health equity researcher at the University of Michigan.
Geronimus, whose book “Weathering: The Extraordinary Stress of Ordinary Life in an Unjust Society” published in March, started out studying the health of women and babies as a graduate student in the 1980s, having been influenced by two distinctly different jobs she had as an undergraduate: one as an on-campus research assistant, the other as a peer companion at an off-campus school for teen mothers.
Stress is weathering our bodies from the inside out
At the time, she said, conventional wisdom held that the Black community had higher rates of infant mortality because teen mothers were physically and psychosocially too immature to have healthy babies. But her research showed younger Black women had better pregnancy and birth outcomes than Black mothers in their mid- to late 20s and 30s.
For this, she was criticized as someone arguing in favor of teen pregnancy, even though she was not. Shaken but undeterred, she continued trying to understand the phenomenon, which meant better understanding the overall health of the community these teens depended on for help. As she studied those networks, she recognized “people’s life expectancies were shorter, and they were getting all these chronic diseases at young ages,” she said.
But she hadn’t come up with a name yet for what she was witnessing. That happened in the early 1990s while sitting in her office: “‘Weathering’ struck me as the perfect word.”
She said she was trying to capture two things. First, that people’s varied life experiences affect their health by wearing down their bodies. And second, she said: “People are not just passive victims of these horrible exposures. They withstand them. They struggle against them. These are people who weather storms.”
People seem to instinctively understand the first, but she said they often overlook the second. It isn’t just living in an unequal society that makes people sick. It’s the day-in, day-out effort of trying to be equal that wears bodies down.
Weathering, she said, helps explain the double-edged sword of “high-effort coping.”
Over the years, Geronimus widened the aperture of her research to include immigrants, Latinos, the LGBTQIA community, poor White people from Appalachia. She found that while weathering is a universal human physiological process, it happens more often in marginalized populations.
Regulation of cortisol — what we think of as the body’s main stress hormone — is disrupted. Optimally, it should work like a wave with a steep morning rise followed by a rapid decline, which slows until reaching baseline at bedtime.
But existing research suggests that is blunted by repeated exposure to psychosocial and environmental stressors, such as perceived racial discrimination, which flatten this rhythm.
Stress-induced high cortisol levels stimulate appetite by triggering the release of ghrelin, a peptide that stimulates hunger.
The interplay between elevated cortisol and glucose is especially complex and insidious, eventually leading to obesity, fatigue, cardiovascular disease, poor immune and inflammatory functions, higher breast cancer mortality rates and other metabolic disorders. Dysregulated cortisol also increases depression and anxiety and interferes with sleep.
Weathering doesn’t start in middle age.
It begins in the womb. Cortisol released into a pregnant person’s bloodstream crosses the placenta, which helps explain why a disproportionate number of babies born to parents who live in impoverished communities or who experience the constant scorn of discrimination are preterm and too small.
During the coronavirus pandemic, pregnant women experiencing stress endured changes in the structure and texture of their placentas, according to a study published this year in Scientific Reports.
The toxic stream can persist into childhood fueled by exposure to abuse, neglect, poverty, hunger. Too much exposure to cortisol can reset the neurological system’s fight-or-flight response, essentially causing the brain’s stress switch to go haywire.
Too much stress in children and adolescents can trigger academic, behavioral and health problems, including depression and obesity.
Stress can change the body at a cellular level.
The effects of relentless stress can be seen at the chromosomal level, in telomeres, which are repeated sequences of DNA found in just about every cell.
Telomeres are the active tips of chromosomes, and they protect the cell’s genetic stability by “capping” the ends of the chromosomes to prevent degeneration. (Think of the plastic tips of shoelaces.)
Researchers have discovered that in people with chronically high levels of cortisol, telomeres become shortened at a faster rate, a sign of premature aging. The shorter the telomeres, the older the cell’s biological age. Shortened telomeres cause a disconnect between biological and chronological age.
‘A societal project’
“I don’t think most people understand weathering stress. Stress is such a vague term,” Geronimus said. “But it still gives us a leverage point to get in there and see a more complex and more frightening picture of what it does to people’s bodies and whose bodies it does it to.”
Changes in seven biomarkers in cardiac patients during a 30-year period showed Black patients weathering about six years faster than White people, a 2019 study published in SSM-Population Health found. Research also found that Black people experience hypertension, diabetes and strokes 10 years earlier than White people, according to a study published in the Journal of Urban Health.
The impact of repeatedly activating the body’s stress response is called allostatic load.
Research has shown that Mexican immigrants living in the United States for more than 10 years have elevated allostatic load scores compared with those who have lived here for less than a decade, and a study of Ohio breast cancer patients published in May in JAMA Network Open found that women with higher allostatic loads — who tended to be older, Black, single and publicly insured — were more likely to experience postoperative complications than those with lower allostatic loads.
“The argument weathering is trying to make is these are things we can change, but we have to understand them in their complexity,” Geronimus said. “This has to be a societal project, not the new app on your phone that will remind you to take deep breaths when you’re feeling stress.”
So, in short, social inequality causes stress, leading to shortened telomeres and, in turn, premature aging, disease and early death.
32 notes
·
View notes
Text

Dr. Mavis Thompson-Blaize (June 2, 1927 - August 31, 2020) who practiced medicine and provided community services for more than five decades, was born in Newark, New Jersey to parents who migrated from Jamaica. She enrolled in Hunter College and received a BA in Chemistry. She earned an MD from Howard University College of Medicine. She completed a residency in Internal Medicine at Kings County Hospital and practiced privately in New York City until 1995.
She married James Blaize (1954). The couple had five children and seven grandchildren.
She developed one of the first Black church-based innovative programs in the nation to assist HIV patients. She understood that the disease was a particular threat to economically less fortunate Black and brown New Yorkers.
St. George’s Episcopal Church in the Bedford-Stuyvesant neighborhood of Brooklyn already had a foundation in HIV treatment that she continued to develop. She understood the stigma in the Black community that was attached to the disease in the 1980s and worked hard to change community attitudes toward the disease even as she provided critical care to her patients.
She worked with the Medical Division of the New York City Board of Education and a per diem physician. Inducted into Delta Sigma Theta Sorority, she encouraged the sorority to support her anti-AIDS activities in Brooklyn. She worked with the Board of Directors of Episcopal Health Services, the Board of Directors of Brooklyn Plaza Medical Center, the President of the Black Caucus of Health Workers of the American Public Health Association, the National Medical Association, Manhattan Central Medical Society, and the Susan Smith McKinney Steward Medical Society. She was a member of the Advisory Board of Episcopal Charities of the Diocese of New York, and a member of St. George’s Church. She served as a Lay Reader at the Bronx’s Christ Church.
She received awards from Bishop’s Cross from the Diocese of Long Island, Outstanding Lifetime Achievement, and Trailblazing Legacy Award from the Susan Smith McKinney Steward Medical Society in 2014. She was celebrated by the Mentoring in Medicine Family. #africanhistory365 #africanexcellence #deltasigmtheta
5 notes
·
View notes