Neuroscience PhD student at the University of Cincinnati: researching and living with depression neurobiology
Don't wanna be here? Send us removal request.
Photo

Thanks to @patritti8384 for taking this picture! We had a great time teaching local kids about the brain at Lakota West High School's Pi Day! My favorite moment was when one girl came up and started telling us all about her favorite brain regions that she had learned about in her "brain book." She must've read it thoroughly, because she knew a lot! I'm so happy I got to show her the real thing up close. Needless to say, it was wonderful to see so many kids fascinated by science! I hope I get the chance to help out again next year! . . . . . . . #scientistsofinstagram #science #education #brain #neuroscience #brainawarenessweek #piday (at University of Cincinnati)
3 notes
·
View notes
Text
Study links brain inflammation to suicidal thinking in depression
Patients with major depressive disorder (MDD) have increased brain levels of a marker of microglial activation, a sign of inflammation, according to a new study in Biological Psychiatry by researchers at the University of Manchester, United Kingdom. In the study, Dr. Peter Talbot and colleagues found that the increase in the inflammatory marker was present specifically in patients with MDD who were experiencing suicidal thoughts, pinning the role of inflammation to suicidality rather than a diagnosis of MDD itself.
“Our findings are the first results in living depressed patients to suggest that this microglial activation is most prominent in those with suicidal thinking,” said Dr. Talbot. Previous studies suggesting this link have relied on brain tissue collected from patients after death.
“This paper is an important addition to the view that inflammation is a feature of the neurobiology of a subgroup of depressed patients, in this case the group with suicidal ideation,” said Dr. John Krystal, Editor of Biological Psychiatry. “This observation is particularly important in light of recent evidence supporting a personalized medicine approach to depression, i.e., that anti-inflammatory drugs may have antidepressant effects that are limited to patients with demonstrable inflammation.”
In the study, first author Dr. Sophie Holmes and colleagues assessed inflammation in 14 patients with moderate-to-severe depression who were not currently taking any antidepressant medications. Immune cells called microglia activate as part of the body’s inflammatory response, so the researchers used a brain imaging technique to measure a substance that increases in activated microglia.
The evidence for immune activation was most prominent in the anterior cingulate cortex, a brain region involved in mood regulation and implicated in the biological origin of depression, confirming the results of a previous study that first identified altered microglial activation in medication-free MDD patients. Smaller increases were also found in the insula and prefrontal cortex.
“The field now has two independent reports — our study and a 2015 report by Setiawan and colleagues in Toronto — showing essentially the same thing: that there is evidence for inflammation, more specifically microglial activation, in the brains of living patients during a major depressive episode,” said Dr. Talbot.
This link suggests that among depressed patients, neuroinflammation may be a factor contributing to the risk for suicidal thoughts or behavior. According to Dr. Talbot, the findings “emphasise the importance of further research into the question of whether novel treatments that reduce microglial activation may be effective in major depression and suicidality.”
385 notes
·
View notes
Photo

It's still so crazy to me that we can understand things like stress and addiction with techniques like microscopy. Obviously the whole foundation of behavioral neuroscience is that these tiny cells give rise to complex behaviors, thoughts, and emotions, but it's nonetheless bewildering. Above is a picture I took from a stress and addiction study that I helped out with. It was a pretty long process to get everything to that point (and involved a procedure to make jello shots in the lab), but what I remember best was the staining. RNAscope is probably one of the hardest histology procedures I've had to do thus far. Each brain had to be cut into 20 um thick sections and kept away from any exogenous RNases. Since RNases are literally EVERYWHERE, this was a challenge. The tissue was flash frozen, so to keep it from being damaged, I had to select slides that were kept at -80 °C with nothing but some RNase free latex gloves. It turns out that fine motor processes don't work so well at that temperature, so I'll admit to being less than graceful with the slides... Then came the actual staining. First we had to permeabilize the tissue, then hybridize target RNAs with the custom probes. Once the probes bound to our RNAs of interest, they were amplified with special materials that bind to the probes and give them a fluorescent tag. That's what you're actually able to see under the microscope, with each tiny dot being a single RNA. The purpose of this study was to investigate a potential mechanism for the comorbidity seen in PTSD and substance abuse disorder. We were looking at RNAs for glucocorticoid receptor (red) and dopamine transporter (green). The blue is actually a DAPI stain for nuclei (or A-T rich DNA if you want to be obnoxious about it). Anyway, since dopamine plays a major role in addiction pathways, the more green dots those pathways have, the more dopaminergic input they have. Similarly, the more red dots, the more those pathways will respond to stress. This picture is of cells in the nucleus accumbens, which is featured prominently in reward and addiction. Hopefully we can get some insight as to why PTSD is so comorbid with substance abuse disorder, and design better treatments from there.
#neuroscience#biology#brain#histology#microscope#microscopy#neurons#biochemistry#microbiology#cells#science#research#grad school#alcohlism#ptsd#genetics#rna#confocal#insitu#fluorescence microscopy#fluorescent#behavior#psychology
2 notes
·
View notes
Photo
I love the architecture in Cincinnati.

View of Cincinnati, from the Carlisle Hotel, circa 1874.
29 notes
·
View notes
Photo
This is really neat! I can definitely see the potential for application, but it also really makes me wonder why more people aren't just trying to bypass the BBB via intranasal administration. I mean, I can definitely imagine a lot of chemotherapies being too brutal for that, but the nose is really relevant in the Parkinson's example they mentioned! It just seems like an easy way to target the brain and make treatment options convenient and cheap for patients. Plus you wouldn't have to buy an expensive human BBB model to test your drug.

New model may help overcome the brain’s fortress-like barrier
Scientists have helped provide a way to better understand how to enable drugs to enter the brain and how cancer cells make it past the blood brain barrier.
The brain is protected by the near-impermeable blood brain barrier, a fortress which protects the brain but which also prevents the treatment of brain diseases, including brain tumours.
Dr Zaynah Maherally and team at the University of Portsmouth have developed a model that mimics the blood brain barrier, which could pave the way for better, more efficient and reliable tests of drugs to treat brain diseases.
The model, the result of slow painstaking research started in 2007, is published in the FASEB Journal.
Dr Maherally said: “The blood brain barrier is strikingly complex and notoriously difficult for scientists to breach. Its role, to protect the brain, makes it difficult for most drugs to make their way into the brain to treat brain tumours.
“It is a dynamic structural, physiological and biochemical fortification that, in essence, protects the brain by providing multiple layers of armour, stopping molecules from entering the brain. It’s highly selective in what it allows past.
“In a person with a brain disease like a brain tumour, or other neurological conditions such as Parkinson’s disease, dementia or head injuries, the strikingly complex defence works against medics and scientists trying to deliver what could be life-saving or life-prolonging treatments.”
A common way medics currently gain access to the brain is by using a pump to deliver drugs into the brain using a catheter, bypassing the blood brain barrier.
The researchers’ major goal was to develop a 3D all-human reproducible and reliable model of the blood brain barrier using human cells in order to better simulate the human blood brain barrier for the study of diseases and treatments.
Many researchers use non-human animal cells to build blood brain barrier models with which to explore brain cancer and deliver drugs to the brain.
Animal models have been relied upon until now as there wasn’t a reliable alternative and accessing human tissue for research can be difficult.
Professor Geoff Pilkington, who leads the research group at Portsmouth, is delighted at the progress that’s been made in modelling the blood brain barrier, a holy grail in the study of brain diseases.
He said: “This is the first real, 3D, all-human blood brain barrier model and it’s hugely significant in our field.”
Research will now widen, he said, to better understand how cancers metastasize from breast and lung to the brain as well as evaluating nano-particle drug delivery and making opportunities to create temporary openings in the barrier to allow drugs to pass through into the brain.
Dr Maherally said: “It’s taken several years to get to this stage and we believe this model will significantly reduce the number of animals used in such studies and reduce the time it takes to get a promising therapeutic into clinical trials.”
118 notes
·
View notes
Photo

(Image caption: New connections interlinking adrenal glands (left) and brain (right). Stylized representation of a newly-discovered signaling pathway, which sees the central nervous system use adrenal hormone production to potentially disrupt the immune system in a way that may lead to severe infections)
An interconnection between the nervous and immune system
Working with colleagues from the German Center for Neurodegenerative Diseases (DZNE), Harvard Medical School and Ohio State University, researchers from Charité - Universitätsmedizin Berlin have shown that the increased incidence of infections seen in spinal cord injury patients is directly linked to a disruption of the normal central nervous system. A newly-discovered reflex arc mediates a process which leads to a disruption in the hormones secreted by the adrenal glands which, in turn, results in an increased susceptibility to bacterial infections. This research breaks new ground in the development of treatments to reduce the incidence of infections, and its results have been published in the current issue of Nature Neuroscience.
Injuries to the brain or spinal cord, such as those caused by stroke or trauma, result in a considerable weakening of the immune system. This often leads to severe infections, such as pneumonia or urinary tract infections, which hamper nervous tissue regeneration as well as rehabilitation in affected patients. Until now, our understanding of the exact manner in which nerve tissue damage leads to infections (and which physiological parameters are responsible) has remained rudimentary at best. Under the leadership of PD Dr. Harald Prüß (Charité’s Department of Neurology and the DZNE Berlin) and Prof. Dr. Dr. Jan M. Schwab (Head of Charité’s Department of Traumatic Spinal Cord Injuries), a team of researchers has now succeeded in deciphering this process.
“Our study was based on the premise that nerve pathways originating in the spinal cord exert a direct influence on organs involved in the immune system, such as lymph nodes and the spleen,” explains Dr. Prüß. He adds: “To our surprise, we found that the disruption of immune organ function does not occur as a result of this direct connection; instead, it is the result of an immune system dysregulation which affects the entire body.”
The researchers showed that the nervous system uses adrenal hormones as part of an indirect path of communication which results in the rapid breakdown of many immune cells. In a healthy body, the adrenal glands are controlled by both the nervous system and the relevant hormone control centers. Until recently, it had been assumed that a brain injury via hormonal signals results in the adrenal glands secreting cortisol, while a trauma-induced stress response results in the release of adrenaline and noradrenaline. “Our data show that the disruption in the normal function of the adrenal glands is under the direct control of damaged nerve tissue,” explains the neurologist. In contrast to received opinion, trauma-induced spinal cord injury initially resulted in a decrease in stress hormones and an increase in cortisol production.
This alteration in hormone levels led to a dramatic decrease in the numbers of many immune cells, particularly affecting the precursors of T-cells and B-cells. In some cases, this resulted in a reduction of between 50 and 80 percent in the size of the spleen, thymus or lymph nodes. While experimental deactivation of the adrenal glands led to a reversal of this dramatic loss of immune cells, the mice treated in this manner remained susceptible to infections. However, an autograft of adrenal tissue, transplanted into these mice, conferred protection against infections. While the transplanted adrenals produce the hormones needed by the body, they are no longer subject to the dysfunctional nervous system control mechanisms which develop following high level spinal injury.
The identification of this two-stage pathological reflex arc – consisting of nerve pathways between the spinal cord and the adrenal glands, as well as a hormone-mediated link with the immune system – helps to deepen our understanding of the interconnections which exist between the nervous and immune system. The discovery of this ‘immune system paralysis’ and its underlying mechanisms represents an important step on the path to improving the treatment of spinal cord injury patients. Rather than merely experiencing the more obvious symptom of motor-sensory paralysis, paraplegic patients also experience a paralysis of the immune system.
“Comprehensive analyses of patients’ cortisol and (nor)adrenaline levels have shown that they exhibit a fundamentally similar behavior to that seen in experimental studies,” explains Prof. Schwab. This suggests that treatment aimed at normalizing this neuro-endocrine reflex may prove effective in controlling the sometimes life-threatening infections associated with injuries to the central nervous system.
199 notes
·
View notes
Photo

Genes for Age Related Brain Deterioration Discovered
Cells in the brain are constantly dying and being replaced with new ones produced by brain stem cells. As we age, it becomes harder for these stem cells to produce new brain cells and so the brain slowly deteriorates. By comparing the genetic activity in brain cells from old and young mice, the scientists identified over 250 genes that changed their level of activity with age. Older cells turn some genes, including Dbx2, on and they turn other genes off.
The research is in Aging Cell. (full open access)
30 notes
·
View notes
Photo

I *nose* this joke is odorous, but you can only study signal transduction so much before you start to lose it.
0 notes
Photo

Microglia are such underrated cells! I've recently become fascinated with their potential role in depression: eating up synapses in response to neural stress. But I feel like they get a bad rap! I mean, who doesn't get carried away with stress eating from time to time? Besides, outside of the context of stress, microglia also release important trophic factors and prune useless synapses, which is very important! Anywho, here's a neat picture I took of some GFP labeled microglia in prefrontal cortex.
#neuroscience#science#brain#microscope#biology#research#mental health#cells#confocal#cool shit#dope as hell#scientist#grad school#depression#immunology#neuroinflammation#neuroimmunology#neat
0 notes
Photo

Neural stem cells - Image of the Week - September 7, 2015
CIL:48107 - http://www.cellimagelibrary.org/images/48107
Description: Differentiated rat neural stem cells stained for β III-Tubulin (in blue) to reveal neurons and GFAP (in red) to reveal glial cells.
Author: Natalie Prigozhina
Licensing: Attribution Only: This image is licensed under a Creative Commons Attribution License
250 notes
·
View notes
Photo

Happy Neuro-Valentines Day!
Some good ones:
Trying to describe how amazing you are gives me anomic aphasia. I just can’t find the words.
Hey baby, my supplementary motor area is going crazy thinking about all the things I want to do to you.
If I had prospagnosia I’d still recognize you because how could forget a face as beautiful as yours?
You’re like my right temporal-parietal areas; I’d be lost without you.
Do you have a lesion on your anterior hypothalamic nucleus? Cause you’re looking really hot.
You make my nucleus accumbens tingle.
Are you a dopamine receptor in the direct pathway of my basal ganglia? Cause I think you’re, D1.
Are you a ventromedial lesion? Because you leave me insatiable.
Have you been doing laps along my corpus callosum? Because lately you’ve been crossing my mind.
I think you may be giving me Upper Motor Neuron Disorder because my lower half is all kinds of hypertonic around you.
Did you damage my cerebellum? Because I’m falling for you.
Looking into your eyes gives me Broca’s aphasia.
You’re so hot, you’ve got my TRP channels upregulating.
Are those your mirror neurons firing? Because I can see you in me.
Wanna make like myelin and wrap yourself around my axon?
2K notes
·
View notes
Photo
Even Darwin had bad days


So you had a bad day …
Charles Darwin read Lyell’s “Principles of Geology Volume 1” while he was travelling on the Beagle, and when he returned to England they became close friends. Darwin vents to Lyell in this letter from 1861.
As Robert Krulwich has noted, it’s nice to know geniuses had bad days like the rest of us. And it’s nice that they had friends to text correspond with when they did.
Happy Birthday Charles! And to the rest of you - Happy Darwin Day!
6K notes
·
View notes
Photo
Happy Darwin Day! If you've been good, Darwin will come and leave finches in your home!

Happy Darwin Day! February 12, 1809 - April 19, 1882
926 notes
·
View notes
Photo
Somewhere over the brainbow...
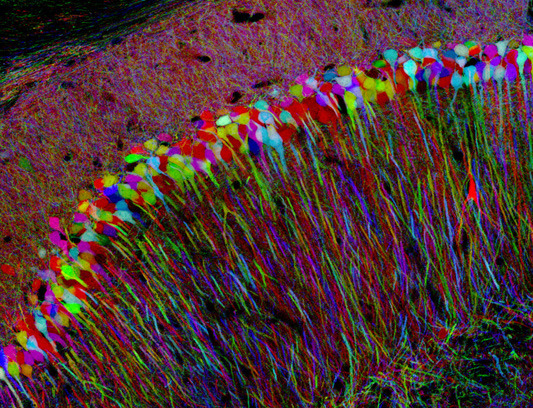
Expression of combinations of three different fluorescent proteins in a mouse brain produced ten different colored neurons. Individual neurons in a mouse brain appear in different colors in a fluorescence microscope. This “Brainbow” method enables many distinct cells within a brain circuit to be viewed at one time.
511 notes
·
View notes
Photo
Increasing entropy explained!

read more comics like this at smbc-comics.com
500 notes
·
View notes
