#Prenatal Risk Assessment
Text

Pre-pregnancy counseling: Your stepping stone to parenthood. Get expert guidance and prepare for a healthy and informed pregnancy journey.
Learn more: https://www.drshubhragoyal.com/welcome/blogs/pre-pregnancy-counseling:-a-stepping-stone-to-parenthood
#Pre-Pregnancy Counseling#pre pregnancy genetic counseling#Preconception Counseling#Family Planning Advice#Reproductive Health Consultation#Pre-Pregnancy Health Tips#Fertility Planning#Pre-Pregnancy Genetic Counseling#Genetic Screening before Pregnancy#Preconception Genetic Testing#Genetic Counseling Services#Prenatal Risk Assessment#Planning for Pregnancy#Healthy Pregnancy Preparation#Conception Readiness Guidance#Fertility Awareness Counseling#Pre-Pregnancy Wellness#Genetic Health Evaluation#Pregnancy Readiness Consultation#Hereditary Disease Counseling#Carrier Screening before Pregnancy#Counseling for Future Parents#Genetic Risk Assessment for Pregnancy#Family Health History Review#Reproductive Life Planning#Pre-Pregnancy Checkup
1 note
·
View note
Text
Maternal Nursing: Combatting the Rising Maternal Mortality Rate
Maternal nursing is a critical care sector focused on the health and wellness of mothers during pregnancy, childbirth, and postpartum. In recent years, a concerning trend has surfaced worldwide: an increase in maternal deaths during childbirth and the postpartum period. This escalating problem underscores the urgency for nursing interventions aimed at safeguarding mothers’ health and minimizing…

View On WordPress
#Emotional Support in Maternity#Hypertension in Pregnancy#Maternal Health Disparities#Maternal Health Education#Maternal Mortality#Maternal Nursing#Nursing Interventions#patient-centered care#Postnatal Care#Postpartum Care#postpartum depression#Postpartum Hemorrhage#Prenatal Care#Risk Assessment
0 notes
Text
He Comes Alive (Part 7)
Part 1 Part 2 Part 3 Part 4 Part 5 Part 6
Summary: You awake in a top secret facility where you learn of Leon's true nature
Word Count: 5.9k
Pairing: vampire/plagas!Leon Kennedy x fem!reader (afab)
Disclaimer: This story is a work of fiction. Actions depicted in this story are not condoned in real life. You are responsible for your own content consumption. If any of the following warnings trigger you, please read at your own risk. Minors do not interact, this story is 18+ only.
Warnings: Biting, blood, gore, murder, unprotected p in v, masterbation, oral (m and f receiving), stalking, pet names, kidnapping, breeding kink, blood play/kink, age gap, dubcon, pregnancy, monster f*cking, body horror, lactation kink, DEAD DOVE: DO NOT EAT [More warnings may be added in future entries]
A quick reminder that I no longer do tag lists

“Where’s Leon?”
“In this building.”
“Where am I?”
“At the BSAA North America headquarters in Washington D.C..”
“BSAA?”
“The Bioterrorism Security Assessment Alliance.”
“Did Leon do something wrong?”
The man called Clive lets out a chuckle, leaning back in his chair, “that’s a loaded question.”
You feel a lump form in the back of your throat. You swallow it back, remaining silent in hopes that Clive will continue.
“Nine years ago, the president’s daughter was kidnapped by a cult in Spain called Los Illuminados. D.S.O. Agent Leon S. Kennedy was sent to rescue her. Both of them had become infected with a bioweapon-- a parasite the cult called Las Plagas. Leon had successfully removed the parasite from the president’s daughter, however…”
Clive pauses and you can feel your heart start to race at the implication, but still you press, “however, what?”
Clive clears his throat, “by the time the U.S. government realized Leon was still infected, he was long gone, leaving a trail of bodies in his wake. He’s been on the run for nine years.”
“What are you talking about?”
“The hikers? That man at the festival? Your father? They’re all his victims,” Clive states.
“You’re lying!” you shout, standing up from the chair and slamming your hands onto the table.
“The plaga feeds on blood in order to survive; it seems to have an affinity to human blood, too.”
“You do realize this sounds absolutely insane, you’re making it sound like Leon’s a vampire or something.”
Clive chuckles again, “that honestly wouldn’t be that far from the truth,” you watch his eyes glance to your swollen belly, “I take it that’s Leon’s baby you're pregnant with?”
“Yes,” you reply curtly before sitting back in the chair, crossing your arms, “it is.”
“Shit…”
“What?”
Clive takes a deep breath before continuing, “I hate to tell you this, but your baby isn’t entirely human.”
Your eyes widen, “excuse me?! Now you’re fucking with me, this is insane!”
“Don’t you find it odd that Leon hasn’t taken you to a single prenatal appointment? Odd that your pregnancy seems to be progressing awfully fast?”
You stand back up again, angrily shaking your finger at Clive, “you are full of shit!”
“Deny it all you want, it’s the truth. Unfortunately you’re too far along in your pregnancy to safely abort, we’ll have to wait until you give birth so we can euthanize it; we’ll make sure it’s done humanely.”
“No one is coming near my baby! You’re just trying to scare me!”
You watch Clive reach into his jacket, pulling out a photo and placing it on the table in front of you. What you see immediately makes you pause and stare. It’s a poorly lit room, a person is tied to the support beam, covered in blood and what you assume is bite marks on their neck.
“This was taken in Leon’s basement after we apprehended him. This is why he kept the basement locked.”
You can’t take your eyes off the photo, especially after you realize you recognize the clothes; it’s a woman that had gone missing after coming out of a work Christmas party in Plymouth; you had seen a photo of her at the party on the news. You feel chills go up your spine.
"Unfortunately she died from blood loss when we were transporting her to our clinic," Clive states.
You swallow hard before making eye contact with Clive, “what the hell is going on…?”
“I think it will be easier to show you, come with me,” Clive replies, standing up from his chair and motioning for you to follow him.
You hesitate for a moment before you decide to follow, going back out into the hallway. The two of you eventually make your way to a single elevator, watching Clive swipe a card and then call the elevator. It beeps before the doors slide open and the two of you step inside.
“How long have you been watching us?” you ask, figuring out that based on what Clive had said to you about Leon not taking you for prenatal check-ups, that someone was watching you and Leon’s every move.
“Shortly after Halloween, a police officer in Oakvale had reached out to the FBI to ask about Leon; in turn the FBI reached out to us. We had to ensure that it was definitely him before making our move.”
You nod, shifting uncomfortably on your feet and unconsciously rubbing your belly. After a couple minutes, the elevator door opens and Clive steps out, you follow him closely. Several men in lab coats turn and greet Clive.
“Director O’Brien! For what do we owe the pleasure?” one of the scientists asks before looking at you, “is this…?”
“Yes she is,” Clive replies, “has he been fed yet?”
The scientist looks back at Clive, shaking his head, “not yet, we were just about to get ready to.”
“Excellent, bring us to the observation room.”
“Of course, director.”
The scientist leads the way bringing you down another hallway that’s barricaded with several large steel doors. At the end, he turns to a door on the left, swiping a keycard and inputting a passcode, causing the door to slide open. You can’t help but feel like you somehow woke up in a science fiction movie. You pinch yourself again to make sure you’re definitely not dreaming.
Once in the room, the scientist pulls up the blinds on a large window and you see Leon, still in just his sweatpants, sitting on a basic metal bed hunched over, staring at the floor. Your heart seemingly skips as you rush up to the window, putting your hands on the glass.
“Leon…” you say softly.
From what you can see, there is nothing out of the ordinary about Leon and you start to reckon that they have the wrong man. Leon wouldn’t hurt anyone. Looking around the room, you notice there is a purple hue. You look up at the room’s ceiling and see that between each fluorescent light is a purple one; the same lights that you saw when you and Leon had gotten ambushed at home.
“What are the purple lights?” you ask, turning to Clive as you remove your hands from the glass.
“High powered ultraviolet lights. The plaga can’t stand sunlight. That’s why he only hunts at night.”
Suddenly, a walkie talkie that is sticking out of Clive’s outer jacket pockets goes off, “We’re ready to commence feeding if you are, director.”
Clive grabs the walkie talkie out of his jacket and replies, “proceed.”
On the left side of the room, a door slides open and a blindfolded man is pushed in and the door closes. The man practically falls onto his face. The man sits up on his knees and you see that his hands are bound behind his back.
“He’s a death row inmate,” Clive says, answering a question you hadn’t even asked, “we have a partnership with the penitentiary and they supply us with inmates that are going to be executed.”
Your attention is drawn back into Leon’s room when the UV lights are switched off and the fluorescent lights dim. Your eyes are drawn to Leon when he suddenly lifts his head, his eyes locked on the man that’s in the midst of a panic attack in the middle of the room. Before your eyes, you watch dark, inky veins start to spread over Leon’s exposed skin. Leon suddenly stands up, walking towards the man like a predator stalking its prey. Movement coming from behind Leon makes your breath hitch; a long, jet black tail comes out of Leon’s back; the closest thing you can compare it to is a scorpion’s tail.
That isn’t all, four more appendages come out of his back, these looking like claws. You want to close your eyes, you want to run, but you can’t; your eyes remain locked on Leon. In a split second, Leon pounces onto the man, the man’s cries for help going unanswered as you watch Leon’s mouth latch itself onto his neck. The four claws latch onto the man as his tail whips itself back and forth as Leon feasts upon him. You suddenly feel your baby shift in your belly.
Leon suddenly stops, unlatching himself from his meal and looking directly at you.
“Can he see us?” you ask, your voice shaking.
“No, it’s a two way mirror,” Clive replies, rubbing his chin with his fingers.
Leon stands up walking right up to the window, his eyes locked onto you. To your horror, you see his eyes are red, seemingly glowing in the dim light. His blood stained mouth hangs agape and you can see that all four of his incisors are elongated and sharp. Leon puts his hands onto the glass, his gaze still locked onto you.
“Angel?” he says, his eyes widening, “is that you?”
His tail moves back and forth as he stares at you and that’s when your baby inside you starts moving erratically, causing you to wince in pain as you grab your belly.
“I’m sorry you have to see me like this,” Leon continues, his hands running down the glass, leaving trails of blood behind, “this is not how I wanted to show you my gift.”
“Gift?” you whisper, taking a couple of steps back from the window.
“He’s referring to the plaga.” Clive replies.
“Our little girl has the gift, too,” Leon continues, his right hand pets the glass as you watch his gaze shift to your belly, made even more unsettling knowing that he can’t see you, “isn’t that right, sweetie?”
Your baby shifts again, feeling your baby’s foot go up your rib cage, causing you to yelp as you once again grab your swollen belly.
There’s no way your baby is reacting to him right? Right?
You watch as Leon’s crimson eyes narrow, one of his fists balling up and punching the glass, causing it to crack. You scream, stumbling backwards and falling to the floor as Leon throws another punch at the glass, cracking it further. Clive rushes over, picking you up off the floor as he grabs his walkie talkie.
“Turn those damn UV lights back on! NOW!” he shouts into the walkie talkie as he pulls you out of the observation room.
You turn and look back as the UV lights are powered back on, Leon letting out the most inhuman scream you’ve ever heard in your life and in an instant, you watch his grotesque appendages retreat back into his body as he stumbles away from the glass, clutching his head with his hands.
As you and Clive retreat back to the elevator, Leon’s cries of your name fill the halls.

You have no idea how much time has passed since the incident with Leon. Clive had you relocated to a more comfortable room at the facility; it has furniture, a small refrigerator and a window to look outside. You’re sitting in a rocking chair next to the window, rubbing your pregnant belly unconsciously as you watch a gentle snowfall outside. Over and over, your brain plays out the last few months since you returned home from dropping out of college.
Every little thing you had noticed that was odd suddenly made sense: eating the rarest meat imaginable, that one time you thought he had sharp teeth when he bit into his burger, him suddenly going into the basement, him getting up in the middle of the night to ‘check traps,’ the day they found what was left of your father, that smile he had on his face was burned into the back of your mind. Your eyes unconsciously widen at another revelation; the red eyes you saw in your window that night, they were Leon’s.
“It was him… he was the B.O.W. the whole time…” you whisper to yourself, a single tear rolling down your cheek.
The sound of the door opening startles you and you watch Clive walk in, giving you a gentle smile and wave as he steps into the room.
“I just spoke with your mother,” Clive says, taking a seat on your bed across from where you sit, “I let her know you were experiencing complications in your pregnancy and that you had to be taken to a specialist in D.C., so she at least knows where you are. I didn’t mention Leon to her.”
“Thank you,” you reply softly, letting out a sigh as you return your attention back out the window.
“How are you feeling?” he asks, the concern evident in his voice.
“Empty? Lost? I’m not sure what to feel… I feel like the last few months have been a cruel lie,” you reply honestly, wiping more tears that run down your face away with the back of your hand.
“I know and I’m sorry. I can’t even imagine how hard this has been for you.”
“Is it true that you can’t cure him?” you ask, looking back over at Clive.
Clive nods, “unfortunately. The parasite has completely taken over his body, if we try to remove it, he will die.”
“How… how is he?” you ask, not really sure you actually want the answer.
“He’s refusing to feed. We’ll have to execute him sooner than we intended,” Clive replies, leaning forward, resting his forearms onto his legs.
“Execute?!”
Clive nods, “yes, he’s too dangerous to keep alive. Our hope was to study the plaga inside of him before putting him out of his misery, but he’s making that difficult.”
“Is there any chance I could say goodbye to him before he’s executed?”
Clive stares at you puzzled for a moment before replying, “I believe I can have that arranged.”
“Good,” you say with a soft sigh of relief.
Despite everything, you still love him. You still love the baby growing inside of you. The thought that both of these things that you love so dearly are going to get taken from you absolutely kills you.
“I’ll make sure to come get you when that time comes,” Clive says, standing up from the bed and walking over to the door, “don’t hesitate to give us a holler if you need anything.”
You believe another few days passes, you awake one morning to the sound of wind howling; a blizzard seems to have come in. Just after you get yourself dressed and cleaned up, Clive once again comes into your room.
“It’s happening tonight,” Clive says, his look solemn.
You acknowledge him with a nod before following him out of your room and back to the elevator that brings you to the underground research facility. This time, instead of bringing you to the observation room, Clive brings you to the door leading to Leon’s containment chamber.
“Remember,” Clive begins, causing you to draw your attention to him, “we’ll be watching. We won’t let him hurt you.”
You nod as the door to his containment chamber slides open. You step inside the small chamber inside the door, it sprays some kind of mist on you which you suspect is some kind of sanitizer. After that, the final door opens and you see Leon, laying on his back staring at the ceiling. You step inside, listening as the door slides shut and locks, making your heart jump in nervousness. At first, Leon doesn’t acknowledge you, instead he continues to stare at the ceiling.
“Leon?” you finally speak up, your voice soft.
Leon lifts his head, staring at you for a moment before he sits up, swinging his legs over the edge of the bed, practically running to you. He places his hands on your shoulders, looking at you in disbelief.
“Angel! You’re ok, I’ve been so worried!” he exclaims before planting a kiss onto your forehead.
Now you’re able to get a good look at him. His skin is extremely pale and you can see the faint, inky black veins all over his exposed skin. It reminds you of the time you had gone to the festival, before he had killed that man behind the fairground. Now you know why Leon had looked so terrible that day.
“I’ve been worried about you, too,” you say hesitantly, avoiding eye contact with him.
“What’s wrong Angel? It’s just me,” Leon coos, his hand gently grasping your chin, forcing you to look at him.
His gaze shifts down to your belly, a smile slowly overtaking his lips as he stares down in awe; once again feeling your baby move inside you.
“My God… you’ve gotten so big! Our little girl is growing like a weed!” he says, the excitement evident in his voice as he places a hand on your belly, rubbing it slowly.
A hint of sadness hits you, knowing that as soon as your baby is born, it’s going to be humanely euthanized, but you don’t want to do anything that could cause Leon to lash out, so you keep that knowledge to yourself.
“How do you know it’s a girl?” you ask, genuinely curious.
“She told me,” Leon explains, his gaze shifting back to you, “because of our gift, we are constantly connected.”
You feel your pulse pick up, feeling your baby continue to writhe inside you as Leon continues to rub your belly.
“I’m going to give you the gift, as well. We’ll be together in both body and mind. Isn’t that wonderful?”
Before you can even process what he just said to you, you notice there’s a sudden change in the lighting; your eyes dart around to see what changed when you notice the subtle purple hue is gone. The UV lights have been turned off. You want to panic, but you take deep breaths to try to keep yourself calm. You reckon it must be a mistake, they’ll turn the UV lights back on in any second. However, more agonizing seconds go by and you realize that they are not coming back on.
Leon slowly looks up, a smirk spreading across his lips when he realizes the UV lights are off, “well… that's convenient.”
He closes his eyes, rolling his neck and shoulders as you watch in horror as the dark veins on his skin get even darker. When he opens his eyes again, you are once again met with the crimson eyes that have haunted your subconscious since the day you saw Leon from the observation room. But now that he’s right in front of you, everything inside you is telling you to get away. You take a couple steps back away from him, his smirk immediately turning into a frown.
“No, no, no! It’s ok, I won’t hurt you, Angel,” he pleads, reaching out to you and grasping your upper arms to stop you from moving away, “I just want to take care of you.”
You watch as his tail snakes out from behind him, moving between the two of you. The end of it goes under your shirt and you watch as the blade-like end of his tail moves upwards, slicing through your shirt. Once your shirt is completely sliced open, his fingers gingerly push the remains of the shirt off you, exposing your swollen breasts to him. He brings one hand up, brushing one of your sensitive nipples under his thumb, causing a small white bead of liquid to come out before running down your breast, pooling onto your pregnant belly.
“Aw look, you’re making milk. Our little girl will need blood, not milk. No matter, I’ll make sure it won’t go to waste,” Leon says before leaning down, wrapping his mouth around the leaking nipple and sucking hard.
“L-Leon!” you cry out, trying to push him away.
You look over at the mirror, knowing that there are people watching. Does Leon know there are people watching? You want to cry out for help, to get someone to come get you out, but you can’t; you don’t want to risk invoking Leon’s fury. After what seems like an eternity, Leon unlatches himself from your breast, his crimson eyes staring down at you lustfully. A grin slowly forms on his face, showing off his long, sharp canine teeth.
He grasps you gently, coaxing you over to his bed where he spins you around, forcing you to bend over onto the bed with your knees on the floor. You rack your brain over what on Earth he’s doing when you feel a very sudden sharp pain in your shoulder, causing you to scream. You then hear a low moan; Leon’s mouth is latched onto your shoulder, his fangs sinking deep into your flesh as blood starts to pour out from the wound.
He releases his mouth from you briefly, his breaths heavy as he grips onto your waist, his hands then reaching around to undo your belt and pants, “you taste just as divine as I remember, Angel,” he purrs into your ear.
You start to question mentally what he’s talking about until you recall back to the first night you stayed at Leon’s house when the two of you had sex for the first time. He wasn’t just eating you out that night. He was feeding off you. This newest revelation causes a sudden wave of nausea to come over you, causing you to gag. You quickly cover your mouth with one hand while the other grips the sheets on his bed, tears burning the corners of your eyes, threatening to pour out.
He bites back down into your shoulder as his hands make quick work pulling down your pants and underwear, his fingers rubbing your slit slowly, gathering up the slick of your body’s arousal on his fingertips. While still feeding off you, he pulls down his sweatpants and you feel the head of his cock prod at your entrance. Your eyes widen when you watch two of the claw-like appendages stab down onto the bed in front of you while the other two wrap around your waist, trapping you against him; you feel one of his hands rest on your hip while the other grips your hair, pulling your head back. It takes everything in you not to scream.
With a quick thrust of his hips, he buries his cock inside you, unlatching his mouth from your shoulder with a loud moan as his grip on your hair tightens. You cry out at the feeling of him practically splitting you in half; he feels so much larger than you remember. There’s also another sensation inside you, one you don’t recognize at all. It’s almost hard for your mind to even describe; like a thousand fingers are stroking your inner walls and your cervix and with each quick thrust of Leon’s hips, it feels amazing. You can’t help but let out a loud moan as Leon pistons himself into you, hurtling you towards your release.
“That’s it Angel, you’re doing so well for me. My perfect mate,” he purrs as he picks up the pace of his thrusts, the hand on your hip gripping so tight that it’ll surely leave bruises, his other hand running down your neck before resting onto your other shoulder, “now, be a good girl and take my gift.”
Against your better judgment, you turn your head to look at him. Leon is opening his mouth and you watch as four mandibles come out from the depths of his mouth and you can hear something squealing from inside his throat. No longer able to put on a brave face, you start to scream, thrashing your body in a desperate attempt to get away from him. The strange sensation you noted inside you suddenly starts to sting as you try to get yourself off him and you feel the claws wrapped around your waist start to cut into your skin as they grip you tighter.
The door to Leon’s room suddenly opens and Clive along with two men with tactical gear and guns swarm in. Clive holds up a large UV flashlight, shining it directly at Leon’s head. Leon roars, the mandibles going back inside his mouth as he falls backwards, freeing you from his grasp. You quickly pull your underwear and pants back up before running over to Clive, using your arms to cover your exposed breasts. Clive positions you behind him as the two men move to either side of Leon, their guns drawn and pointed at him. One of the scientists then rushes inside the room, Clive turns his head to address him.
“What the fuck were you thinking?!” Clive shouts at the scientist right before the UV lights turn back on.
You wince when you hear the inhuman cry come from Leon as he scrambles to crouch himself into the corner of the room, gripping his head and trembling.
“We just wanted to see what he would do, that’s all!” the scientist says, pleading with Clive.
“She nearly got infected! Was that part of your plan?!” Clive shouts, walking up to the scientist, getting in his face.
“Well, no…”
“The lead researcher will be hearing about this, now get out of our way, I need to take her back to her room,” Clive continues, practically shoving the scientist out of the way as he gently grasps your upper arm to lead you out of Leon’s containment chamber.
As you walk out, you turn and look at Leon, who’s still crouched in the corner; his eyes are locked onto you, a smirk spread across his lips.

Leon stays seated in the corner of his containment chamber for the majority of the day, only moving to relieve himself in the toilet inside his containment chamber. Scientists have been in and out of his containment chamber as well, almost as if they’re preparing for something, though he didn’t have the slightest clue of what that could be until the lead researcher comes in with his young assistant, who looks vaguely familiar to Leon.
The lead researcher takes Leon’s vitals and a blood sample, staying completely still through it all, watching the assistant take a seat on Leon’s bed, taking notes with a clipboard and pen.
“Dr. Jacobs, a question if I may?” the assistant suddenly asks.
“Go ahead, Chambers.”
Chambers. Rebecca Chambers. That’s why I recognize her…
Rebecca was a former member of S.T.A.R.S. Bravo Team prior to the Raccoon City outbreak incident on September 30, 1971; Leon’s first day as a police officer. A part of him wishes he had died that day.
“How did he manage to infect the fetus? I thought you said it was transmitted via the bloodstream, hence why he bit her.” she asks, setting the clipboard and pen down onto the bed next to her.
Dr. Jacobs swallows hard as he turns to address her, “we believe there are plaga larvae in his semen, which fused with the embryo upon fertilization even though we found no larvae in the semen samples we were able to get. Somehow… the plaga inside him can control when a larva is released… absolutely extraordinary, a real shame we’re executing him tonight.”
Leon subtly raises an eyebrow.
“What about the baby?” Rebecca presses.
“The baby will be humanely euthanized upon birth, the BSAA wants to put the plagas parasite to bed for good even though the child could provide valuable data. I tried to fight it but O’Brien wouldn’t budge.”
What?
Leon remains calm on the outside, but on the inside, he is panicking. He has to protect his offspring at all cost, but how? That answer comes on a silver platter when he watches Rebecca stand up from the bed, grabbing the clipboard but leaving the pen behind on his bed. He waits a couple minutes to see if they realize she had left the pen in here. When he’s confident they’re not coming back in, he stands up, walking over to the bed and collapsing onto it, clutching the pen in his hand as he lays down. He turns, his back facing the camera that’s on the opposite wall pointed towards the bed.
During his stint in the military after surviving the Raccoon City outbreak, Leon picked up a few tricks, one being how to make lockpicks out of just about anything. He meticulously takes the mechanical pen apart, using the metal parts to make a crude lock pick, small enough to fit into the palm of his hand.
Later that evening, the door to his containment chamber opens and Dr. Jacobs comes in along with another man in tactical gear with an AK-47 slung over his shoulder and a pistol strapped to his leg. Dr. Jacobs is carrying a metal folding chair, which he hands to the guard for him to set down onto the floor after opening.
“Sit,” the guard orders Leon, pointing at the chair.
“Yeah, yeah…” Leon replies, standing up from his bed and sitting in the chair.
“Hands behind your back. Now,” the guard barks.
Leon does as he’s ordered, putting his hands behind his back around the back of the chair. The guard walks behind him, handcuffing his wrists together. Unbeknownst to the guard, Leon has his makeshift lock pick wedged between two of his fingers, completely concealing it. The guard walks back around, standing in front of Leon as Dr. Jacobs prepares a syringe of bright green liquid. Slipping the lock pick out, he begins to pick the lock on his cuffs.
“It pains me to do this Leon, it really does,” says Dr. Jacobs as he approaches, the guard moving to the side of Leon to let him through, “you were a brilliant agent. I admit this will not be pleasant, but you won’t suffer for long, I promise.”
Leon manages to free himself just as Dr. Jacobs kneels down to inject him with the deadly serum in the syringe. In the blink of an eye, Leon snatches the syringe from Dr. Jacobs, stabbing it into his neck and pushing the syringe. Dr. Jacobs’ expression contorts as he collapses onto the floor, his body going into a seizure in what Leon imagines is the painful thralls of death.
The guard curses as Leon stands up from his chair, pointing his AK-47 at him to shoot. However, Leon’s too quick, he side steps and grabs the AK-47, using the strap slung around the guard’s body to strangle the man, all the while, the gun is still firing, shooting out all the lights in the ceiling, including the UV lights. Inky black veins quickly envelope Leon’s body and his eyes shift into the deep crimson as Leon bites into the guard’s exposed neck, drinking as much blood as he can in a short period of time.
He then kneels down to Dr. Jacobs’ lifeless body, searching his pockets to find a fob. With this fob in hand, the door to the containment chamber opens, allowing Leon to make his escape. He can sense his offspring is several floors above where he is, so he quickly finds the elevator, the fob allowing him access to it.
When the elevator doors open, several guards are waiting for him, guns drawn. In an instant, Leon’s tail and back appendages emerge and he practically leaps out of the elevator pinning one of the guards down and ripping out his throat while his tail whips around, decapitating and fatally stabbing the other guards. Just when Leon thinks he’s in the clear, he hears more footsteps coming towards him. He looks up, blood dripping from his mouth and chin and finds Director O’Brien with about 10 more guards behind him.
“I should have known you wouldn’t go quietly, Leon,” Director O’Brien says, crossing his arms.
“Where is my mate?” Leon growls, standing up to face them, using his back claws and tail to make himself look bigger.
“In a place you won’t get to, Leon. You’re not leaving this hallway alive,” Director O’Brien replies.
“We’ll see about that.”
Leon begins to step forward, his legs and arms mutating, turning black like his claws and tail. His fingers become more claw like and his legs contort to become more insect-like; his feet also transform into three toed claws. His jaw splits open to reveal rows of sharp elongated teeth, his four incisors still longer than the rest. His four mandibles also come out of his mouth and he lets out an inhuman roar as he charges towards Director O’Brien and the guards. This is the furthest Leon’s ever let himself transform and he’s honestly eager to see what he can do.
The guards shoot at him, but the bullets do little to no damage to Leon as he rips through them like paper with his razor sharp claws, blood and guts spilling everywhere. In the chaos, Director O’Brien slips away, running down the hall. Leon sees this and quickly gives chase, what’s left of the guards strewn all over the white marble floor in his wake. Director O’Brien comes around the corner with his angel, his mate in tow, both of them stopping in their tracks upon seeing Leon.
Leon opens his mouth wide, letting out a loud hiss as he glares at Director O’Brien. Unfortunately in his current state, he’s unable to speak. His crimson stare shifts over to his angel, who to his dismay, is visibly frightened.
Angel, don’t be afraid, I won’t hurt you. I could never hurt you…
He curses internally about not being able to give her his gift; if he had been successful, he would be able to communicate with her easily. His gaze then shifts to her swollen belly, sensing his offspring is strong and healthy inside her. He watches as she grips her belly, flinching.
“Back off, Leon!” Director O’Brien shouts, pulling out a small flashlight from inside his dark green coat and turning it on, pointing its purple beam directly into Leon’s face.
Leon, turns his face away, growling as he feels the light sting his mutated parts. His tail whips forward, slicing off the hand holding the UV flashlight before he turns back to Director O’Brien, stalking towards him and using one of his clawed hands to pick him up and pin him against the wall. Letting out a guttural growl, his mouth and mandibles open wide only stopping when he feels his mate’s hands on his arm.
“Leon, don’t kill him, please!” she cries, “don’t kill him and I’ll… I’ll go with you…”
His mutated mouth closes, turning to her to see her bloodshot eyes staring up at him, pleading with him. He lets out a soft purring sound, turning back to Director O’Brien and abruptly dropping him. He falls to the floor with a gasp, Leon’s attention back onto his mate as he grabs her by her wrist. She looks up at him, the fear evident in her eyes as she starts to panic, pulling against his grasp as she hyperventilates.
Angel, don’t do this… it’ll be ok, I promise…!
She then faints; Leon’s quick reflexes catch her before she collapses onto the floor. He picks her up into his arms bridal style, stalking into one of the rooms that has a window. Using his tail, he smashes the window open, the blizzard raging outside now blowing snow into the room. Leon leaps out of the window, carrying his mate into the stormy winter night.
Part 8
#leon kennedy#leon s kennedy#leon kennedy x reader#leon s kennedy x reader#leon kennedy smut#leon kennedy x reader smut#vampire!leon kennedy#plagas!leon kennedy#gigabyte writes#he comes alive
404 notes
·
View notes
Text
i read a (20 year old) study that found prenatal down syndrome diagnosis leads to an elective abortion in 92-95% of cases, whereas for an immediately fatal birth defect like anencephaly it's roughly 76%. which really surprised me- knowingly continuing a pregnancy with a high likelihood of eventual uncontrolled miscarriage and if not, a guarantee of death of the infant within minutes or hours after birth with all the risks that has for both appears to be a significantly more common choice than having a down syndrome kid with a life expectancy of >60 years. and an even lower 72% elective abortion rate was found following spina bifida aperta diagnosis, which is also severely disabling but statistically allows living for up to a few decades while requiring constant, extensive and lifelong care. so it seems down syndrome is outstandingly intolerable to expecting parents despite being, in my layman assessment, the least impactful on quality of life and causing the least dependence on care throughout life. the condition with the longest life expectancy and the only one of those three with a possibility for a (near-)independent life at all, in fact. so i genuinely wonder why that is. purely the social stigma of intellectual disability? sort of a silver medal effect, too close to "normal" and yet not?
87 notes
·
View notes
Text
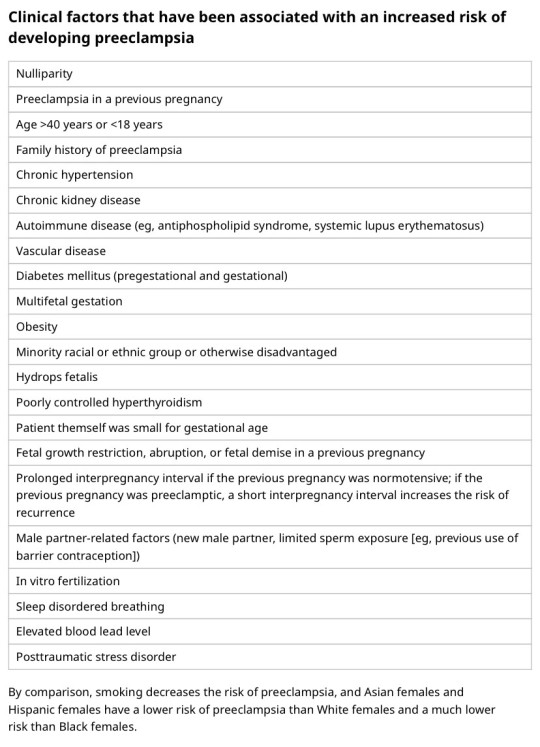
I'm on OB rotation again. I asked the attending what are things the PCP should know about prenatal and postpartum pts. Stuff we discussed:
SSRIs can be continued during pregnancy. I often see patients on Zoloft during pregnancy if they need an antidepressant. In fact, I just started a prenatal patient on Zoloft the other day in clinic. It is safe to continue SSRIs during pregnancy because you should treat the patient's depression. Babies can come out sort of jittery because of the SSRI, but that goes away.
Postpartum patients will have bleeding somewhat similar to a menstrual period right after giving birth. It starts to decrease and becomes like a brownish color and can last up to 6 weeks postpartum. Any bleeding beyond that point is abnormal.
There is some evidence that if you have estrogen-containing birth control, it can decrease milk supply. Actually, I had a patient in clinic recently who was seen by an attending and he started her on a progesterone only birth control so that it would not affect her milk supply. Estrogen decreases the patient's milk supply, so patients who plan to breast-feed should not be started on estrogen-containing birth control. Right after giving birth, your body has increased amounts of estrogen, so you would not start estrogen containing birth control until at least 6 weeks postpartum anyway. Increasing estrogen immediately postpartum increases risk of blood clots. For patients who plan to breastfeed and want to be on an oral contraceptive, use progesterone only oral contraceptives until she stops breastfeeding.
If the mother is breastfeeding at least every 4 hours, then this can be used for contraception. It's about 80% effective. Once baby starts sleeping through the night or once baby starts feeding more than every 4 hours, this method won't work! If you go more than 4 hours without breastfeeding, breastfeeding will not protect you from pregnancy! You can also ovulate before your menstrual period returns, so you can't say you can't get pregnant because your period has not returned yet!
I asked the attending I worked with today about how she goes about prescribing birth control. She said she will usually start with Sprintec. It's usually covered by insurance and if it's not covered, it's pretty affordable. She also said Junel is pretty well tolerated. Certain progestins in certain brands of birth control may work better for certain things like acne control, but she didn't have as much knowledge on that. I'll ask another attending again about that. I usually start people on Sprintec as well.
PCP should know that alkaline phosphatase is high in pregnant patients. It comes from the placenta. So don't be freaked out by that.
You should know HTN in pregnancy and preeclampsia workup. High BP is 140/90. Severely high BP is 160/110. Swelling occurs in many pregnant pts, but that should also alert you to start preeclampsia workup.
[Preeclampsia w/u from UpToDate:
Diagnostic evaluation
•Laboratory – Patients with suspected preeclampsia should have a complete blood count with platelets, creatinine level, liver chemistries, and determination of urinary protein excretion.
•Fetal status – Fetal status is assessed concurrently or postdiagnosis, depending on the degree of concern during maternal evaluation. At a minimum, a nonstress test or biophysical profile is performed if appropriate for gestational age. Ultrasound is used to evaluate amniotic fluid volume and estimate fetal weight, given the increased risk for oligohydramnios and growth restriction.
•Consultation with the neurology service is generally indicated in patients with neurologic deficits/abnormal neurologic examination, which may include ocular symptoms or a severe persistent headache that does not respond to initial routine management of preeclampsia.]
An important thing to review is physiology of pregnancy. Blood volume increases during pregnancy, so there are lots of new RBCs and that will throw off a HgbA1c reading, therefore HgbA1c is not measured during pregnancy and will not be accurate! My attending today told me there was a midwife who offered pts either HgbA1c or oral glucose tolerance tests to screen for gestational DM. The HgbA1c is not accurate in pregnancy, so this should not be done. That would be bad to miss a diagnosis of gestational diabetes. You have to wait until 3 months postpartum to measure HgbA1c to get an accurate reading. Had a pt who did not have a PCP prior to getting pregnant, was on insulin during the pregnancy, and after giving birth, still needs to establish with PCP for diabetes f/u. After you give birth, you insulin needs drastically change, so you don't need as much as you did when you were pregnant. So I stopped her insulin and advised that she f/u with her new PCP for diabetes care.
I still need to review fetal heart tracings. The attending today said the first thing to look at is the baseline (the baseline HR should be about 160 beats/min), then the variability, then look for accelerations and decelerations. If more than 32 weeks GA, accelerations are 15 beats/min above the baseline lasting at least 15 seconds. Early decelerations are representative of compression of the fetal head, which is normal during labor as baby moves down the pelvis/birth canal. Variable decelerations look sharper like a "V" and can represent compression of the umbilical cord. Late decelerations represent placental insufficiency.
ACOG has very helpful practice bulletins.
I can't take screen shots on my work laptop, so I'm just going to summarize gestational HTN w/u from UpToDate:
Gestational HTN: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions 4 hours apart after 20 weeks of gestation in a previously normotensive individual
And:
No proteinuria
No signs/symptoms of preeclampsia-related end-organ dysfunction (eg, thrombocytopenia, renal insufficiency, elevated liver transaminases, pulmonary edema, cerebral or visual symptoms)
Preeclampsia: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions at least 4 hours apart after 20 weeks of gestation in a previously normotensive individual. Patients with systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg should have blood pressure confirmed within a short interval (minutes) to facilitate timely administration of antihypertensive therapy.
And:
Proteinuria (≥300 mg per 24-hour urine collection [or this amount extrapolated from a timed collection], or protein:creatinine ratio ≥0.3, or urine dipstick reading ≥2+ [if other quantitative methods are not available]).
In a patient with new-onset hypertension without proteinuria, the diagnosis of preeclampsia can still be made if any features of severe disease are present.
Preeclampsia with severe features: In a patient with preeclampsia, presence of any of the following findings are features of severe disease:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg on 2 occasions at least 4 hours apart (unless antihypertensive therapy is initiated before this time)
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
Progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL [97 micromol/L] or doubling of the serum creatinine concentration in the absence of other renal disease)
Pulmonary edema
Persistent cerebral or visual disturbances
Eclampsia: A generalized seizure in a pt with preeclampsia that cannot be attributed to other causes.
HELLP syndrome: hemolysis, elevated liver enzymes, low platelets. Hypertension may be present (HELLP in such cases is often considered a variant of preeclampsia).
Chronic (pre-existing) hypertension: hypertension diagnosed or present before pregnancy or on at least 2 occasions before 20 weeks of gestation. Hypertension that is first diagnosed during pregnancy and persists for at least 12 weeks postpartum is also consider chronic hypertension.
Blood pressure criteria during pregnancy are:
Systolic ≥140 mmHg and/or diastolic ≥90 mmHg
Prepregnancy and 12 weeks postpartum blood pressure criteria are:
Stage 1 – Systolic 130 to 139 mmHg or diastolic 80 to 89 mmHg
Stage 2 – Systolic ≥140 mmHg or diastolic ≥90 mmHg
Chronic HTN with superimposed preeclampsia*:
Any of these findings in a patient with chronic hypertension:
A sudden increase in blood pressure that was previously well-controlled or an escalation of antihypertensive therapy to control blood pressure
New onset of proteinuria or a sudden increase in proteinuria in a patient with known proteinuria before or early in pregnancy
Significant new end-organ dysfunction consistent with preeclampsia after 20 weeks of gestation or postpartum
*Precise diagnosis is often challenging. High clinical suspicion is warranted given the increase in maternal and fetal-neonatal risks associated with superimposed preeclampsia.
Chronic hypertension with superimposed preeclampsia with severe features:
Any of these findings in a patient with chronic hypertension and superimposed preeclampsia:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg despite escalation of antihypertensive therapy
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
New-onset or worsening renal insufficiency
Pulmonary edema
Persistent cerebral or visual disturbances
A reduction in blood pressure early in pregnancy is a normal physiologic occurrence. For this reason, women with chronic hypertension may be normotensive at their first few prenatal visits. Later in pregnancy, when their blood pressure returns to its prepregnancy baseline, they may appear to be developing preeclampsia or gestational hypertension if there are no documented prepregnancy blood pressure measurements.
BP: blood pressure.
* Blood pressure should be elevated on at least two occasions at least four hours apart. However, if systolic pressure is ≥160 mmHg or diastolic pressure is ≥110 mmHg, confirmation after a short interval, even within a few minutes, is acceptable to facilitate timely initiation of antihypertensive therapy.
¶ The onset of preeclampsia and gestational hypertension is almost always after 20 weeks of gestation. Preeclampsia before 20 weeks of gestation may be associated with a complete or partial molar pregnancy or fetal hydrops. Postpartum preeclampsia usually presents within two days of delivery. The term "delayed postpartum preeclampsia" is used for signs and symptoms of the disease leading to readmission more than two days but less than six weeks after delivery.
Δ Significant proteinuria is defined as ≥0.3 g in a 24-hour urine specimen or protein/creatinine ratio ≥0.3 (mg/mg) (34 mg/mmol) in a random urine specimen or dipstick ≥1+ if a quantitative measurement is unavailable.
◊ Almost all women with the new onset of hypertension and proteinuria at this gestational age or postpartum have preeclampsia, but a rare patient may have occult renal disease exacerbated by the physiologic changes of pregnancy. An active urine sediment (red and white cells and/or cellular casts) is consistent with a proliferative glomerular disorder but not a feature of preeclampsia. Women with chronic hypertension who had proteinuria prior to or in early pregnancy may develop superimposed preeclampsia. This can be difficult to diagnose definitively, but should be suspected when blood pressure increases significantly (especially acutely) in the last half of pregnancy/postpartum or signs/symptoms associated with the severe end of the disease spectrum develop.
§ Photopsia (flashes of light), scotomata (dark areas or gaps in the visual field), blurred vision, or temporary blindness (rare); severe headache (ie, incapacitating, "the worst headache I've ever had") or headache that persists and progresses despite analgesic therapy; altered mental status. Seizure occurrence upgrades the diagnosis to eclampsia.¥ The differential diagnosis of preeclampsia with severe features includes but is not limited to:
Antiphospholipid syndrome
Acute fatty liver of pregnancy
Thrombotic thrombocytopenic purpura (TTP)
Hemolytic uremic syndrome (HUS)
The laboratory findings in these disorders overlap with those in preeclampsia with severe features. (Refer to table in the UpToDate topic on the clinical manifestations and diagnosis of preeclampsia.) The prepregnancy history, magnitude and spectrum of laboratory abnormalities, and additional presence of signs and symptoms not typically associated with preeclampsia help in making the correct diagnosis, which is not always possible during pregnancy.
In addition, a variety of medical disorders may be associated with hypertension and one or more of the signs and symptoms that occur in women with preeclampsia with severe features. These patients can usually be distinguished from patients with preeclampsia by taking a detailed history, performing a thorough physical examination, and obtaining relevant laboratory studies.‡ In contrast to preeclampsia, gestational hypertension is not associated with end-organ involvement, so neither proteinuria nor the symptoms or laboratory findings of preeclampsia are present.
#OB#OBGYN#birth control#gestational HTN#preeclampsia#eclampsia#breastfeeding#gestational diabetes#fetal heart tracing#FHT
2 notes
·
View notes
Text
so hi good morning this is a post very outside of my normal posting but i am so mad that this is happening here now
the beginning of this story is that i am attending a virtual two-day conference regarding the implications of revising the regulatory definition of lead-based paint. and for the first presentation, there were these two graphs shown.

i got really mad because no recent study would use the words "'mentally retarded'", and so i had a feeling that this had to be outdated as all hell.
i did a deep dive into this, trying to figure out where the hell it could have come from. i found one article, paywalled of course, that referenced these conclusions, and had the same graphs but of higher quality.

these two graphs were part of Rice, D. (2020). Neurodevelopmental toxicants1. In J. Nriagu (Ed.), Encyclopedia of Environmental Health. That visual reference listed the source as being Weiss, B. (1988). Neurobehavioral toxicity as a basis for risk assessment. Trends in Pharmacological Sciences 9, 59–62.
one really obvious thing that stood out to me is that this paper cited is only 3-4 pages long. there's no way this is the original study. i found the 1988 paper, which had these graphs as Figure 4. the source of this information is introduced as follows:
"A recent study^12 of lead levels in umbilical cord blood assigned children to three groups: low, medium and high, with respective means of 1.8, 6.5 and 14.5 mcg/dL. Even the high lead group fell far below the value considered to present a hazard; yet children in this group, at the age of 24 months, scored about 8% below the other children on the Mental Development Index of the Bayley Scales of Infant Development".
the recent study, noted as superscript 12, was Bellinger, D., Leviton. A., Watemaux, C.. Needleman. H. and Rabinowitz. M. (1987) N. Engl. i. Med. 316, 1037-1043, or "Longitudinal Analyses of Prenatal and Postnatal Lead Exposure and Early Cognitive Development". i skimmed through this study, and noted that there is no discussion of IQ, as the study utilized the Mental Development Index (MDI) for infants up to 24 months of age. MDI and IQ are not at all equivalent measures, so then were did this bitch Weiss get the conclusions on IQ?
the answer shortly follows the introduction of the data. it is that "Individual attribution of risk would not apply to this study because none of the children displayed any demonstrable deficits. Viewed in societal terms, however, the implications are compelling."
so what does this mean? that this pair of graphs from 1988 have been touted as truth, when it is merely based off of implications of societal harms that weren't even measured in the 1987 study!!!!! the conclusions of these graphs from 1988 are potentially entirely baseless, at the bare minimum because MDI is not mappable onto IQ, and even moreso, because the author just made it up!!! the bitch Weiss saw the conclusions of the 1987 study and just went "hmmm but what if society...."
2 notes
·
View notes
Text
4 Little-Known Factors That Cause high Risk Pregnancy

Introduction
Pregnancy risk can be increased by several factors, such as pre-existing medical illnesses, the mother's age, lifestyle, and health problems that develop before or during pregnancy.
In this blog, we list a few potential causes that might lead to High-Risk Pregnancy. Since each pregnancy is unique and this list is not intended to be comprehensive, certain hazards that apply to one pregnancy might not apply to another. Women should consult a healthcare professional if they have any inquiries about their pregnancies. Following factors that might cause a high risk of pregnancy
Existing Health Condition
1. High Blood Pressure
Although having high blood pressure during pregnancy can be dangerous for both the mother and the fetus, most women with mild hypertension who do not have any other conditions have good pregnancies and births because they manage their blood pressure before becoming pregnant.
2. Diabetes
Diabetic women must control their blood sugar levels throughout pregnancy as well as before becoming pregnant. High blood sugar levels can result in birth abnormalities during the first few weeks of pregnancy, frequently before a woman even realizes she is expecting.
3. Thyroid
A little gland in the neck called the thyroid produces hormones that help regulate blood pressure and heart rhythm. A fetus who has an uncontrolled thyroid disorder, such as an overactive or underactive thyroid, may experience heart failure, poor weight gain, and issues with brain development.
Your Age
1. Young Age
Teenagers may be less likely to receive prenatal care or to keep prenatal appointments. Prenatal care is essential because it enables a healthcare professional to assess, detect, and treat risks—for example, by advising teenagers not to take specific medications during pregnancy—often before they materialize into actual issues.
2. First-time Pregnancy After Age 35
The majority of older first-time mothers have healthy pregnancies, however, evidence indicates that older women are more likely than younger women to experience several issues, such as:
Gestational hypertension, often known as gestational hypertension, and diabetes (called gestational diabetes)
loss of pregnancy16
Ectopic pregnancy, a potentially fatal condition that requires a cesarean section, occurs when the embryo is connected to tissue outside the uterus.
Lifestyle Factors
1. Alcohol Use
Alcohol consumption during pregnancy raises the baby's chance of problems like sudden infant death syndrome (SIDS), fetal alcohol spectrum disorders (FASDs), and other issues. FASDs are a group of outcomes for the fetus caused by the mother's alcohol consumption during pregnancy.
2. Drug Use
According to research, using drugs and smoking marijuana while pregnant can both be harmful to the fetus and have an impact on the health of the baby. According to one study, the chance of stillbirth was increased by taking illegal drugs and marijuana.
Healthy Diet in Pregnancy
1. Eat Vegetables and Fruits
Fruits and vegetables, particularly those that include Vitamin C and Folic Acid, supply numerous essential nutrients during pregnancy. Vitamin C, which is found in foods like broccoli, tomatoes, Brussels sprouts, and fruits like oranges, grapefruits, and honeydew, is essential for pregnant women and should be consumed daily in doses of at least 70 mg.
2. Dairy products
The daily requirement for calcium to maintain pregnancy is at least 1000 mg. Calcium is crucial for healthy blood coagulation, muscle and nerve function, and the development of strong teeth and bones. If you do not get enough calcium through your food, since your developing baby needs a lot of calcium, your body will extract calcium from your bones (which can lead to future problems, such as osteoporosis).
#Benecare hospital#Best Physiotherapist near me#Best radiologist at benecare hospital#Benecare multispeciality hospital Pune#Benecare radiology specialist#radiology near me#radiology specialist#best gynecologist surgeon in Pune
3 notes
·
View notes
Text
The Importance of Routine Gynecological Exams: A Key to Women's Wellness

For women, routine gynecological exams are an essential aspect of maintaining overall health and wellness. Dr. Chang T.C., a trusted gynaecologist in Singapore, emphasizes that these exams are crucial for early detection and prevention of various health issues. Here’s why prioritizing these visits is vital for women’s health.
1. Early Detection of Health Issues
Routine gynecological exams allow your gynaecologist to monitor your reproductive health and identify potential issues before they become serious. Regular check-ups can help detect conditions such as cervical cancer, ovarian cysts, and sexually transmitted infections (STIs) early on. Early detection often leads to better treatment outcomes, making these exams indispensable for women’s health.
2. Comprehensive Health Assessment
During a routine exam, Dr. Chang will conduct a thorough evaluation of your reproductive system. This includes a pelvic exam and Pap smear to screen for abnormal cell changes that could indicate precancerous conditions. Additionally, your overall health will be assessed, including weight, blood pressure, and family medical history, providing a comprehensive picture of your well-being.
3. Addressing Menstrual and Hormonal Issues
Many women experience menstrual irregularities and hormonal imbalances at various life stages. Routine visits to a gynaecologist can help identify the causes of these issues. Whether it’s heavy periods, painful cramps, or symptoms of menopause, your gynaecologist can offer effective treatments and management strategies tailored to your needs.
4. Guidance on Reproductive Health
Routine gynecological exams also serve as an opportunity for women to discuss reproductive health, including family planning and contraception options. Dr. Chang can provide personalized advice based on your lifestyle, health goals, and family planning needs, ensuring you make informed decisions about your reproductive health.
5. Promoting Overall Wellness
Gynecological exams are not just about reproductive health; they play a significant role in overall wellness. These visits provide a safe space for women to discuss various health concerns, including mental health and lifestyle choices. Regular check-ups foster open communication and empower women to take charge of their health.
6. Building a Trusted Relationship with Your Gynaecologist
Establishing a long-term relationship with a gynaecologist allows for personalized care that evolves with your needs. Dr. Chang T.C. is dedicated to fostering trust and open communication, ensuring that you feel comfortable discussing any concerns regarding your health.
In conclusion, routine gynecological exams are a key component of women’s wellness. By prioritizing these visits with a skilled gynaecologist like Dr. Chang, women can ensure they are taking proactive steps toward a healthier future. Don’t wait—schedule your appointment today and take charge of your health and well-being!
Author : Dr. Chang T.C.
Who We Are
Dr. T.C. Chang has been in medical practice since 1986, the last 29 years as a specialist in Obstetrics and Gynaecology.
Dr. T.C. Chang, is a Consultant Obstetrician and Gynaecologist who works at SWC GYNAE ASSOCIATES, Thomson Medical Centre, Singapore. He is also a Consultant in Fetal Maternal Medicine at Thomson Medical Centre and the Head and Clinical Director, Fetal Assessment Centre, Singapore Women' Medical Group.
He has a special focus on prenatal care, high risk pregnancy and more - can find out more details via his About Us page.
Contact Us
Dr. Chang T.C.
339 Thomson Road, #05-05 Thomson Medical Centre, Singapore, 307677, Singapore
+65 6253 4122
https://doctorchang.com.sg
To Know More
Brand Map
1 note
·
View note
Text
Autism: Causes, Symptoms, and Management

Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition that varies widely in symptoms and severity.
Both genetic and environmental factors contribute to the development of autism.
Early diagnosis and intervention can significantly improve outcomes for individuals with autism.
A combination of therapies, education, and support systems is essential for managing autism effectively.
Ongoing research and advocacy are crucial for better understanding and supporting those with autism.

What is Autism?
Autism Spectrum Disorder is a lifelong developmental condition characterized by difficulties in communication, social interaction, and repetitive behaviors.
The term “spectrum” reflects the wide range of symptoms and severity that individuals with autism can experience.
While some may have significant challenges that require support throughout their lives, others might live relatively independent lives with mild symptoms.
Causes and Risk Factors

The exact cause of autism is not fully understood, but it is believed to result from a combination of genetic and environmental factors.
Certain genes are linked to an increased risk of autism, and having a sibling with autism raises the likelihood of another child being diagnosed.
Environmental factors, such as prenatal exposure to toxins or complications during birth, may also contribute.
However, no single cause has been identified, and autism likely arises from the interplay of multiple factors.
Symptoms and Diagnosis

Autism can manifest differently in each individual, but common signs include delayed speech, difficulty in making eye contact, repetitive behaviors, and challenges with social interactions.
In young children, early signs may include a lack of response to their name, minimal interest in playing with others, or an unusual focus on specific objects.
Diagnosis typically involves a comprehensive evaluation by healthcare professionals, including developmental screenings and assessments using standardized tools.
Early diagnosis, often by the age of two or three, is crucial as it allows for timely intervention that can improve long-term outcomes.
Types of Autism

Autism encompasses a range of subtypes or levels, which vary based on the severity of symptoms and the level of support required.
For example, individuals with Asperger’s syndrome, a former diagnosis now included under the ASD umbrella, often have milder symptoms and do not experience significant delays in language development.
Others might fall into categories such as Classic Autism, where more substantial challenges in communication and behavior are present.
Understanding these differences is important for providing appropriate support and intervention.
Impact on Daily Life

Autism affects many aspects of daily life, including communication, social interactions, and behavior.
Children with autism may struggle in traditional educational settings, requiring special education programs tailored to their needs.
As they grow, challenges may continue in finding employment or living independently. The impact of autism extends to families and caregivers, who often require additional resources and support to help their loved ones thrive.
Treatment and Management
While there is no cure for autism, various treatments and interventions can help manage symptoms and improve quality of life.
Behavioral therapies, such as Applied Behavior Analysis (ABA), are commonly used to teach communication, social skills, and adaptive behaviors.
Speech and occupational therapies also play a vital role in addressing specific challenges faced by individuals with autism.
Recent research shows the negative impact of sugar on mineral metabolism, particularly copper, which plays a major role in managing iron levels within the body.
Disruption in copper metabolism can lead to iron dysregulation, contributing to oxidative stress and potential tissue damage, including in the brain.
This connection suggests that dietary factors, such as excessive sugar consumption, may not only exacerbate neurological disorders but also influence their onset by disturbing the delicate balance of essential minerals like copper.
Autism Support and Resources

Education is a critical component in supporting children with autism. Special education programs that cater to their specific needs can make a significant difference in their development.
Additionally, there are numerous resources available for parents and caregivers, including support groups, advocacy organizations, and informational websites.
These resources provide valuable guidance, emotional support, and practical advice for managing the challenges associated with autism.
Autism Research and Advances

Research into autism is ongoing, with scientists exploring various aspects, including genetic markers, environmental triggers, and new therapeutic approaches.
Advances in technology and neuroimaging have also opened new avenues for understanding how autism affects the brain.
Emerging treatments, such as targeted behavioral therapies and nutritional interventions, show promise in improving the lives of those with autism.
Continued research is essential for uncovering more effective strategies for diagnosis, treatment, and support.
Conclusion
Understanding autism is essential for creating a more inclusive and supportive society for individuals with ASD. Early diagnosis, personalized treatment plans, and strong support systems are key to helping those with autism lead fulfilling lives. Ongoing research and advocacy efforts will continue to play a vital role in improving outcomes for individuals with autism and their families.
FAQ
What are the early signs of autism in a child?
Early signs of autism may include delayed speech, limited eye contact, a lack of response to their name, and repetitive behaviors. These signs typically become noticeable by the age of two or three.
Can autism be cured?
There is no cure for autism, but early intervention and tailored therapies can significantly improve outcomes and help individuals manage symptoms effectively.
How does autism affect learning and social interactions?
Autism can impact learning and social interactions by making it challenging for individuals to communicate, understand social cues, and adapt to new situations. Specialized education programs and therapies can help address these challenges.
What resources are available for parents of children with autism?
Parents can access various resources, including support groups, advocacy organizations, special education programs, and online information hubs that offer guidance and support for managing autism.
How can society better support individuals with autism?
Society can support individuals with autism by promoting awareness, providing inclusive education and employment opportunities, and ensuring access to appropriate healthcare and support services.
Research
Adams, J.B., Audhya, T., McDonough-Means, S., Rubin, R.A., Quig, D., Geis, E., Gehn, E., Loresto, M., Mitchell, J., Atwood, S., Barnhouse, S. and Lee, W., 2012. Toxicological Status of Children with Autism vs. Neurotypical Children and the Association with Autism Severity. Biological Trace Element Research, [online] 151(2), pp.171–180. doi:10.1007/s12011-012-9551-1.
Adams, J.B., Holloway, C.E., George, F. and Quig, D., 2006. Analyses of Toxic Metals and Essential Minerals in the Hair of Arizona Children with Autism and Associated Conditions, and Their Mothers. Biological Trace Element Research, [online] 110(3), pp.193–210. doi:10.1385/bter:110:3:193.
Adams, J.B., Romdalvik, J., Levine, K.E. and Hu, L.-W., 2008. Mercury in first-cut baby hair of children with autism versus typically-developing children. Toxicological & Environmental Chemistry, [online] 90(4), pp.739–753. doi:10.1080/02772240701699294.
Adams, J.B., Romdalvik, J., Ramanujam, V.M.S. and Legator, M.S., 2007. Mercury, Lead, and Zinc in Baby Teeth of Children with Autism Versus Controls. Journal of Toxicology and Environmental Health, Part A, [online] 70(12), pp.1046–1051. doi:10.1080/15287390601172080.
Al-Farsi, Y.M., Waly, M.I., Al-Sharbati, M.M., Al-Shafaee, M.A., Al-Farsi, O.A., Al-Khaduri, M.M., Gupta, I., Ouhtit, A., Al-Adawi, S., Al-Said, M.F. and Deth, R.C., 2012. Levels of Heavy Metals and Essential Minerals in Hair Samples of Children with Autism in Oman: a Case–Control Study. Biological Trace Element Research, [online] 151(2), pp.181–186. doi:10.1007/s12011-012-9553-z.
Alabdali, A., Al-Ayadhi, L. and El-Ansary, A., 2014. A key role for an impaired detoxification mechanism in the etiology and severity of autism spectrum disorders. Behavioral and Brain Functions, [online] 10(1). doi:10.1186/1744-9081-10-14.
Arredondo, M. and Núñez, M.T., 2005. Iron and copper metabolism. Molecular Aspects of Medicine, [online] 26(4–5), pp.313–327. doi:10.1016/j.mam.2005.07.010.
Baj, J., Flieger, W., Flieger, M., Forma, A., Sitarz, E., Skórzyńska-Dziduszko, K., Grochowski, C., Maciejewski, R. and Karakuła-Juchnowicz, H., 2021. Autism spectrum disorder: Trace elements imbalances and the pathogenesis and severity of autistic symptoms. Neuroscience & Biobehavioral Reviews, [online] 129, pp.117–132.
https://doi.org/10.1016/j.neubiorev.2021.07.029.
Chen, L., Guo, X., Hou, C., Tang, P., Zhang, X., Chong, L., & Li, R. (2022). The causal association between iron status and the risk of autism: A Mendelian randomization study. Frontiers in Nutrition, 9, 957600.
https://doi.org/10.3389/fnut.2022.957600
Collins, J.F., Prohaska, J.R. and Knutson, M.D., 2010. Metabolic crossroads of iron and copper. Nutrition Reviews, [online] 68(3), pp.133–147. doi:10.1111/j.1753-4887.2010.00271.x.
DiNicolantonio, J.J., Mangan, D. and O’Keefe, J.H., 2018. The fructose–copper connection: Added sugars induce fatty liver and insulin resistance via copper deficiency. Journal of Metabolic Health, [online] 3(1).
https://doi.org/10.4102/jir.v3i1.43.
Gaugler, T., Klei, L., Sanders, S.J., Bodea, C.A., Goldberg, A.P., Lee, A.B., Mahajan, M., Manaa, D., Pawitan, Y., Reichert, J., Ripke, S., Sandin, S., Sklar, P., Svantesson, O., Reichenberg, A., Hultman, C.M., Devlin, B., Roeder, K. and Buxbaum, J.D., 2014. Most genetic risk for autism resides with common variation. Nature Genetics, [online] 46(8), pp.881–885. doi:10.1038/ng.3039.
Gaware, V., 2010. Ceruloplasmin its role and significance: a review. Pathology, 5(6).
Hellman, N.E. and Gitlin, J.D., 2002. Ceruloplasmin metabolism and function. Annual Review of Nutrition, [online] 22(1), pp.439–458. doi:10.1146/annurev.nutr.22.012502.114457.
Iossifov, I., O’Roak, B.J., Sanders, S.J., Ronemus, M., Krumm, N., Levy, D., Stessman, H.A., Witherspoon, K.T., Vives, L., Patterson, K.E., Smith, J.D., Paeper, B., Nickerson, D.A., Dea, J., Dong, S., Gonzalez, L.E., Mandell, J.D., Mane, S.M., Murtha, M.T., Sullivan, C.A., Walker, M.F., Waqar, Z., Wei, L., Willsey, A.J., Yamrom, B., Lee, Y., Grabowska, E., Dalkic, E., Wang, Z., Marks, S., Andrews, P., Leotta, A., Kendall, J., Hakker, I., Rosenbaum, J., Ma, B., Rodgers, L., Troge, J., Narzisi, G., Yoon, S., Schatz, M.C., Ye, K., McCombie, W.R., Shendure, J., Eichler, E.E., State, M.W. and Wigler, M., 2014. The contribution of de novo coding mutations to autism spectrum disorder. Nature, [online] 515(7526), pp.216–221. doi:10.1038/nature13908.
James, S.J., Cutler, P., Melnyk, S., Jernigan, S., Janak, L., Gaylor, D.W. and Neubrander, J.A., 2004. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. The American Journal of Clinical Nutrition, [online] 80(6), pp.1611–1617. doi:10.1093/ajcn/80.6.1611.
James, S.J., Melnyk, S., Jernigan, S., Cleves, M.A., Halsted, C.H., Wong, D.H., Cutler, P., Bock, K., Boris, M., Bradstreet, J.J., Baker, S.M. and Gaylor, D.W., 2006. Metabolic endophenotype and related genotypes are associated with oxidative stress in children with autism. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, [online] 141B(8), pp.947–956. doi:10.1002/ajmg.b.30366.
Krumm, N., Turner, T.N., Baker, C., Vives, L., Mohajeri, K., Witherspoon, K., Raja, A., Coe, B.P., Stessman, H.A., He, Z.-X., Leal, S.M., Bernier, R. and Eichler, E.E., 2015. Excess of rare, inherited truncating mutations in autism. Nature Genetics, [online] 47(6), pp.582–588. doi:10.1038/ng.3303.
Ma, D., Salyakina, D., Jaworski, J.M., Konidari, I., Whitehead, P.L., Andersen, A.N., Hoffman, J.D., Slifer, S.H., Hedges, D.J., Cukier, H.N., Griswold, A.J., McCauley, J.L., Beecham, G.W., Wright, H.H., Abramson, R.K., Martin, E.R., Hussman, J.P., Gilbert, J.R., Cuccaro, M.L., Haines, J.L. and Pericak‐Vance, M.A., 2009. A Genome‐wide Association Study of Autism Reveals a Common Novel Risk Locus at 5p14.1. Annals of Human Genetics, [online] 73(3), pp.263–273.
https://doi.org/10.1111/j.1469-1809.2009.00523.x.
McArdle, H.J., Andersen, H.S., Jones, H. and Gambling, L., 2008. Copper and Iron Transport Across the Placenta: Regulation and Interactions. Journal of Neuroendocrinology, [online] 20(4), pp.427–431. doi:10.1111/j.1365-2826.2008.01658.x.
Mukhopadhyay, C.K., Attieh, Z.K. and Fox, P.L., 1998. Role of Ceruloplasmin in Cellular Iron Uptake. Science, [online] 279(5351), pp.714–717. doi:10.1126/science.279.5351.714.
Musci, G., & Polticelli, F. (2014). Ceruloplasmin-ferroportin system of iron traffic in vertebrates. World Journal of Biological Chemistry, 5(2), 204-215.
https://doi.org/10.4331/wjbc.v5.i2.204
Sharp, P., 2004. The molecular basis of copper and iron interactions. Proceedings of the Nutrition Society, [online] 63(4), pp.563–569. doi:10.1079/pns2004386.
Sousa, L., Oliveira, M.M., Pessôa, M.T.C. and Barbosa, L.A., 2020. Iron overload: Effects on cellular biochemistry. Clinica Chimica Acta, [online] 504, pp.180–189. doi:10.1016/j.cca.2019.11.029.
Skalny, A.V., Simashkova, N.V., Skalnaya, A.A., Klyushnik, T.P., Zhegalova, I.V., Grabeklis, A.R., Skalnaya, M.G. and Tinkov, A.A., 2018. Trace element levels are associated with neuroinflammatory markers in children with autistic spectrum disorder. Journal of Trace Elements in Medicine and Biology, [online] 50, pp.622–628. doi:10.1016/j.jtemb.2018.04.031.
0 notes
Text
Understanding Fetal Nuchal Translucency Scan
A fetal nuchal translucency scan is a vital prenatal screening performed between 11 and 14 weeks of pregnancy. This non-invasive test measures the fluid at the back of the baby’s neck to assess the risk of chromosomal abnormalities like Down syndrome. Early detection through this scan allows for informed decisions and better pregnancy management.
1 note
·
View note
Text
The Importance of Prenatal Care for High-Risk Pregnancies by Dr. Poonam Kumar
Dr. Poonam Kumar, a leading expert in Obstetrics and Gynecology, emphasizes the critical role of prenatal care in managing high-risk pregnancies. From comprehensive health assessments to early intervention, prenatal care is essential for ensuring the safety and well-being of both mother and baby. With specialized care plans tailored for high-risk conditions, Dr. Kumar's guidance supports healthier outcomes and minimizes complications throughout pregnancy.
0 notes
Text
Pre-Pregnancy Counseling: A Stepping Stone to Parenthood

Do you have a baby bump? Yes! Then, before you jump in the air with joy, you should take a look at pregnancy counseling, because expecting a baby requires a lot of acceptance and awareness, and that makes it a stepping stone to parenthood, a path of responsibility and mindfulness.
Pre-pregnancy counseling is a motto that pre-empts the certain risk factors pertaining a women’s, the fetus and neonatal health from entering an unfavorable phase. The one-to-one interaction with the professional can be a great aide in optimizing the health care of mother and child, which also extends to the family ties, as their care is invested from the first days.
Education about the pregnancy journey in pre-pregnancy course is open to all genders, sexualities and parents, as they offer a holistic approach to better parenting. Regardless of whether you are planning a pregnancy or using contraception, the pre-pregnancy counseling is applicable to both parties.

As the saying goes, health status can't be the same forever, over growing time potential risks can occur anytime. Thus, pre-pregnancy counseling does not last for a day, but it occurs several times for ensuring a healthy and happy baby journey!
Day in and out whenever an expectant mother gets counselled, fresh knowledge is added to her advantage for handling the situation. There is a certainty of several chronic conditions viz; diabetes, hypertension, thyroid and mental health require monitoring during pre-pregnancy for a desirable outcome.
In the pre-pregnancy counseling sessions, a crucial assessment for examining STDs is a must with a vivid screening for any probable genetic conditions that might pass down to the life growing inside.
The other important matter of concern here is to debrief on possible strong addictions namely, liquor, nicotine consumption, drugs or any other medicines taken for some underlining or nonmedical reasons.
There is also a significant survey conducted on partner violence during intimacy during prepregnancy counseling as it has entirely a direct impact on the mother and child both.

The expert guidance - Suggestions from the desk of the American College of Obstetrician and Gynecologists
The ACOG institute emphasizes the opportunity to stroke the iron hard and discuss overall wellness, and healthy habits as a routine irrespective of the patient for a successful outcome.
“Would you like to become pregnant next year?” Serves the purpose, of the right to speak out one's heart for suitable guidance without coyness.
The goal of prepregnancy counseling is to ensure a pregnancy that is away from the instructions and if any challenges occur one has the tact to handle it with expert guidance.
An annual influenza inoculation is mandatory for every patient unbiased as it is for additional benefit.
Prepregnancy is not limited to basic health checkups and discussions a patient's lifestyle and underlining conditions are crucial to tap on! If discovered to be a specific virus prone or any infection or allergies due to climate/ certain food types must be cautioned beforehand as travelling is a massive no.
Appropriate nourishment and vitamins are so significant for a healthy pregnancy tenure. Always fall back on your medical adviser for the proportion of food intake that suits your body the best during the prepregnancy period.
Read More: https://www.drshubhragoyal.com/welcome/blogs/pre-pregnancy-counseling:-a-stepping-stone-to-parenthood
#Pre-Pregnancy Counseling#pre pregnancy genetic counseling#Preconception Counseling#Family Planning Advice#Reproductive Health Consultation#Pre-Pregnancy Health Tips#Fertility Planning#Pre-Pregnancy Genetic Counseling#Genetic Screening before Pregnancy#Preconception Genetic Testing#Genetic Counseling Services#Prenatal Risk Assessment#Planning for Pregnancy#Healthy Pregnancy Preparation#Conception Readiness Guidance#Fertility Awareness Counseling#Pre-Pregnancy Wellness#Genetic Health Evaluation#Pregnancy Readiness Consultation#Hereditary Disease Counseling#Carrier Screening before Pregnancy#Counseling for Future Parents#Genetic Risk Assessment for Pregnancy#Family Health History Review#Reproductive Life Planning#Pre-Pregnancy Checkup
1 note
·
View note
Text
High-Risk Pregnancy Treatment in Malviya Nagar
High-risk pregnancies require specialized care to ensure the safety and well-being of both mother and baby. In Malviya Nagar, a well-developed area in South Delhi, there are numerous healthcare facilities that provide expert treatment for high-risk pregnancies. These facilities offer state-of-the-art medical care, personalized treatment plans, and experienced professionals to handle complications during pregnancy. Our services High-Risk Pregnancy Treatment in Malviya Nagar

What is a High-Risk Pregnancy?
A pregnancy is considered high-risk when there are potential health issues that could affect the mother, the baby, or both. Several factors can increase the risk, including:
Maternal Age: Women above the age of 35 are more likely to face complications during pregnancy.
Pre-existing Medical Conditions: Conditions like diabetes, hypertension, or heart disease can increase pregnancy risks.
Multiple Pregnancies: Carrying twins, triplets, or more increases the likelihood of complications.
Previous Pregnancy Complications: A history of miscarriage, preterm birth, or preeclampsia can make the current pregnancy high-risk.
Lifestyle Factors: Smoking, excessive alcohol use, or drug abuse also heighten pregnancy risks.
Genetic Issues: If there’s a family history of genetic disorders, the pregnancy might require close monitoring.
In high-risk pregnancies, routine prenatal care might not be sufficient. Specialized care from skilled professionals is essential to reduce risks and ensure a healthy pregnancy and delivery.
High-Risk Pregnancy Treatment Options in Malviya Nagar
Malviya Nagar boasts a variety of healthcare options catering to high-risk pregnancies, including hospitals and clinics that focus on maternal-fetal medicine. These facilities offer the following services:
1. Specialized Obstetricians and Maternal-Fetal Medicine Experts
Experienced doctors specializing in high-risk pregnancies are the foundation of effective treatment. These specialists provide comprehensive evaluations and personalized care plans based on the mother’s medical history and specific risk factors. In Malviya Nagar, many hospitals are equipped with highly skilled obstetricians who coordinate care with maternal-fetal medicine specialists.
2. Advanced Prenatal Testing and Monitoring
Advanced diagnostic tests are a critical part of managing high-risk pregnancies. This includes:
Ultrasound and Fetal Monitoring: Regular ultrasounds to track fetal development and Doppler ultrasounds to assess blood flow between the placenta and fetus.
Non-Invasive Prenatal Testing (NIPT): Screening for genetic conditions such as Down syndrome, trisomy 18, and trisomy 13.
Amniocentesis: A diagnostic test that analyzes amniotic fluid to detect chromosomal abnormalities.
Glucose Tolerance Tests: For detecting gestational diabetes, a condition that can lead to complications if untreated.
In Malviya Nagar, clinics and hospitals have access to the latest technology for prenatal diagnostics to ensure continuous monitoring of both mother and baby.
3. Management of Pre-existing Conditions
For pregnant women with pre-existing conditions like diabetes or hypertension, managing these conditions is crucial to reducing pregnancy risks. Malviya Nagar healthcare centers offer personalized care plans that address these conditions through:
Medication Management: Adjusting medications to ensure they are safe during pregnancy while effectively managing chronic conditions.
Lifestyle Adjustments: Nutritional counseling, physical activity plans, and stress management techniques are offered to improve health outcomes for both mother and baby.
Regular Monitoring: Blood pressure, blood sugar levels, and other vital signs are continuously monitored to prevent complications.
4. NICU Facilities
In high-risk pregnancies, premature birth or complications at delivery may require neonatal intensive care. Several hospitals in Malviya Nagar are equipped with advanced Neonatal Intensive Care Units (NICUs), ensuring that babies born prematurely or with complications receive immediate and comprehensive care.
5. 24/7 Emergency Care
High-risk pregnancies often necessitate immediate medical attention. Malviya Nagar offers hospitals with 24/7 emergency care, ensuring that any urgent medical issues can be addressed promptly. Quick access to emergency care is vital in preventing severe complications for both mother and child.
Conclusion
Malviya Nagar is home to numerous high-quality healthcare providers offering comprehensive care for high-risk pregnancies. From specialized obstetricians to advanced diagnostic tools, these facilities ensure that both mother and baby are monitored and treated with the utmost care. Early intervention, ongoing monitoring, and specialized support can significantly improve the chances of a healthy pregnancy and delivery.
For expecting mothers experiencing a high-risk pregnancy, the combination of expert care, modern technology, and personalized treatment available in Malviya Nagar makes it an ideal location for high-risk pregnancy management.
0 notes
Text

🎯🎯 "Tiny Hearts, Big Diagnoses: The Importance of First-Trimester Fetal Echocardiograms" ❤️🩺
Attention healthcare providers and sonography professionals! The horizon of early prenatal care is expanding, and it's time to discuss why a patient might need a fetal echocardiogram in the first trimester.
Catching congenital heart diseases ASAP could be a lifesaver for families! Traditional fetal echoes are usually done around 20 weeks, when the heart is roughly the size of a quarter. But what if we could jump-start that assessment earlier, between 11-14 weeks, when the heart is as tiny as a pea? 🫛
First-trimester fetal echoes are game changers, particularly for women at a higher risk of delivering babies with heart issues. Equipped with specialized tools and expertise, we can now diagnose many significant cardiac conditions much sooner.
So, when do we recommend these early scans?
🔍 Abnormal nuchal translucency screening results
🔍 Preexisting maternal diabetes with high hemoglobin A1c
🔍 Family history of congenital heart disease
🔍 IVF conceptions
🔍 Complications in identical twins
The benefits? 🌟 An early diagnosis offers families the best range of treatment options. Believe it or not, some congenital heart conditions can be addressed in utero! This includes mitigating aortic stenosis, managing Hypoplastic Left Heart Syndrome, and even treating abnormal heart rates with medications.
Let's harness this groundbreaking capability to provide the best care from the very beginning. 💙🩺
#Healthcare #Sonography #FetalEchocardiogram #PrenatalCare #HeartHealth
Se atienden particulares y obras sociales: OSDE-Swiss Medical- Sancor Salud- Medife- IOSFA y otras.
Información y turnos deben enviar mensaje por WhatsApp de lunes a sábados de 9 a 20 horas al +5492966757732 (solo mensajes no llamar)
0 notes
Text
Expecting A Baby? Key Tips For Aspiring Mothers

Pregnancy is an exciting journey, and we at Flowrence Hospital are committed to helping you every step of the way. Preparing for pregnancy entails more than just physical readiness; it also includes emotional, mental, and behavioral changes to ensure a healthy start for both you and your future child. Here are some vital ideas to help you prepare for this wonderful journey.
1. Schedule a preconception check-up:
Before attempting to conceive, have a preconceived visit with your healthcare provider. This session allows you to talk about your medical history, any existing health conditions, and any drugs you are presently using. Your doctor may offer personalized advice, check that your vaccines are up-to-date, and propose any required lifestyle modifications.
2. Concentrate on Nutrition:
A balanced diet is essential for a healthy pregnancy. Begin by including a variety of fruits, vegetables, whole grains, lean meats, and healthy fats into your diet. Foods high in folate, iron, calcium, and omega-3 fatty acids are especially healthy. To lessen the chance of neural tube abnormalities, consider taking a prenatal vitamin that contains folic acid.
3. Maintain a healthy weight:
Achieving and maintaining a healthy weight before pregnancy might increase your chances of conception while also lowering your risk of pregnancy issues. Speak with your healthcare practitioner about a healthy weight range for you and get guidance on how to achieve it through nutrition and activity.
4. Exercise regularly:
Regular physical activity can improve your overall health and prepare your body for pregnancy. Aim for 30 minutes of moderate activity most days of the week. Walking, swimming, and yoga are great choices. Exercise can help you manage stress, enhance your mood, and keep a healthy weight.
5. Avoid harmful substances:
Avoid tobacco, alcohol, and recreational drugs, as these can impair fertility and harm your baby during pregnancy. Limit your caffeine intake to less than 200 milligrams per day (approximately one 12-ounce cup of coffee).
6. Manage Stress:
Stress can have an influence on your fertility and general health. Use stress-reduction practices including meditation, deep breathing exercises, and mindfulness. Engaging in hobbies and spending time with loved ones, and seeking professional support when needed can also help.
7. Understanding Your Menstrual Cycle:
Understanding your menstrual cycle can help you determine when you are most fertile. Track your cycle for a few months to assess its duration and consistency. Ovulation occurs approximately 14 days before your next period. There are a number of applications and tools available to help you track your cycle and anticipate ovulation.
8. Prepare Your Home and Lifestyle:
Consider making lifestyle changes to provide a healthy environment for pregnancy and parenting. This could involve limiting your exposure to environmental contaminants, keeping your home safe and clean, and discussing parenting plans with your partner. Establishing a support network of family and friends can also be beneficial.
9. Educate yourself:
Take the time to educate yourself on pregnancy, childbirth, and parenthood. Take prenatal classes, read credible books and articles, and join support groups or online forums. Being well-informed might help you feel less anxious and more confident as you prepare for motherhood.
10. Maintain positivity and patience:
Conceiving might take time, so it’s crucial to be hopeful and patient. Concentrate on living a healthy lifestyle and supporting your mental well-being. If you have been trying to conceive for a year (or six months if you are over 35) and have had no success, see your doctor for further examination and advice.
Conclusion
Preparing for pregnancy is an important step towards a healthy and enjoyable parenthood experience. At Flowrence Hospital, we provide expert guidance, comprehensive care, and compassionate assistance. By taking these necessary actions, you may increase your chances of a safe pregnancy and provide the greatest possible start for your future child.
To receive personalized guidance and care, arrange a preconceived appointment with our skilled staff at Flowrence Hospital. For booking an appointment contact us at 90990 89107. Together, we can assist you on this exciting adventure with confidence and peace of mind.
#best pregnancy hospital in rajkot#best maternity hospital in rajkot#best pregnancy hospital near me#best maternity hospital near me
0 notes
Text
What is the cost of maternal screening test?

The cost of maternal screening tests can vary widely depending on the type of test, your location, and your healthcare provider. For example:
First Trimester Screening: This usually includes a blood test and an ultrasound and can cost between $200 and $500.
Second Trimester Screening: Also known as the quad screen, this blood test generally ranges from $100 to $300.
Non-Invasive Prenatal Testing (NIPT): This advanced test can cost between $800 and $2,000, as it analyzes fetal DNA in the mother's blood to assess the risk of certain genetic conditions.
0 notes