#Psychiatric Treatments in MD
Text
Adolescent Psychiatry Services : Mental Health Services
Adolescence is a critical period of development where individuals experience significant physical, emotional, and social changes. It is also a time when many mental health conditions emerge or worsen. Visit Now: www.accesshealthservices.org
#Adolescent Psychiatry Services#Mental Health Services#Adolescent Psychiatry Care#Access Health Services#Access Health Care Services#Psychiatric Clinic MD#Mental Health Clinic MD#MD Mental Health Services#Mental Health Clinic Baltimore MD#MD Mental Health Clinic#Psychiatrists in MD#Psychiatric Treatments in MD
0 notes
Text
"FACTUAL ALLEGATIONS
9. Plaintiff Alexander Morris is an African American man and is the lead singer of the famous Motown group the "Four Tops." At the time of the incident the Four Tops were on a national music tour with the Temptations and had recently performed at the Grammy Awards.
10. On or about April 7, 2023; Plaintiff was transported to the Ascension Macomb Oakland Hospital emergency room via ambulance, and he presented to the emergency room with difficulty breathing and chest pain, he was on oxygen, and he had a significant known history of cardiac disease including the placement of stints and defibrillator. During his hospitalization, Plaintiff was ultimately diagnosed with a heart infraction that may require a heart transplant, pneumonia, and he suffered three seizures during his stay.
11. When he presented to the emergency room Plaintiff informed a nurse and a security guard that he was a member of the famous Motown group the "Four Tops," and that he had current security concerns due to stalkers and fans.
12. Shortly after check-in a nurse Holly Jackson, a White male security guard Greg Ciesielski, and a White male emergency room doctor Brandon Harris Fishman, DO racially profiled him and/or profiled him based upon a perceived disability and placed an order for a psychological evaluation for Plaintiff because they did not believe he was a singer or member of the "Four Tops." Doctor Brandon Harris Fishman, DO, the emergency room doctor who was on staff met with Plaintiff and interviewed him, Plaintiff informed him of his medical history, and informed him that he was having difficulty breathing and chest pain. Defendants and Brandon Harris Fishman, DO wrongfully assumed he was mentally ill when he revealed his identity as a celebrity figure. Defendants and/or Brandon Harris Fishman, DO made the decision to remove him from oxygen and pursue a psychiatric evaluation instead despite his clear symptoms of cardiac distress and significant medical history.
13. Plaintiff had a valid identification on his person and could easily have been identified as a singer in the Four Tops group.
14. Brandon Harris Fishman, DO ordered a psychological evaluation for Plaintiff instead of ordering the emergency medical treatment he needed. Plaintiff was denied the emergency medical care he needed due to his heart condition and pneumonia, and instead a security guard was instructed to ensure he was placed into a restraining jacket and/or a four-point restraint mechanism, removed his belongings, and Plaintiff was told he was going to have a "psych eval" or psychological evaluation. Plaintiff was referred to Virjaya Gopal Kotha, MD for the psychological evaluation.
15. Plaintiff asked if he could prove his identity by showing his identification card, and the White male security guard ordered him to "sit his Black ass down." None of the nursing staff intervened to stop the racial discrimination and mistreatment of Plaintiff. Upon information and belief none of the nursing staff reported the mistreatment or use of the racial slur to a supervisor. Moreover, none of the nursing staff thought to simply ask for Plaintif's identification.
16. Plaintiff told medical staff he was having difficulty breathing and asked for the oxygen back but was ignored. Plaintiff asked to have the restraint device removed and asked for his personal belongings back so he could leave and seek treatment at another hospital, and he was told he was not free to leave; thus, he was falsely imprisoned and deprived of his personal property. During this time his medical condition continuously declined and he was denied the medical treatment he desperately needed.
17. Several security guards were called to surround the nursing station to ensure Plaintiff could not leave. During this entire incident Plaintiff was not being treated for his medical emergency, namely a severe heart condition and pneumonia. Defendant Hospital and Defendant Jackson blatantly refused to provide Plaintiff with medical treatment due to his race and/or perceived mental disability. Instead, Plaintiff received a deliberate misdiagnosis and received a lower standard of medical care based on his race that amounted to racial discrimination and delayed his actual diagnosis.
18. Finally, Plaintiff's wife came to the nursing station to collect his belongings and she saw what was transpiring and Plaintiff informed his wife that the doctors thought he was delusional. Plaintiff's wife informed one of the security officers that he was actually a member of the Four Tops, but he took no action on Plaintiff's behalf, and he was left in the restraints and denied medical treatment. A nurse came to Plaintiff's side, and Plaintiff asked to show the nurse the video of him performing at the Grammys. The nurse realized Plaintiff was a member of the Four Tops, and the nurse went and got the emergency room doctor to inform him. The emergency room doctor returned and said he was cancelling the psychological evaluation.
19. The restraint jacket was finally removed, and he was placed back on oxygen. Plaintiff was restrained for approximately an hour and a half or 90 minutes. As aforementioned, during his hospitalization, Plaintiff was ultimately diagnosed with a heart infraction that may require a heart transplant, pneumonia, and he suffered three seizures during his stay.
20. Plaintiff was offered a $25.00 gift card to Meijers as an apology for the dehumanization and discrimination he faced at the hands of the hospital. He refused to accept the gift card.
21. Subsequent to the incident, a security guard that worked at the hospital contacted Plaintiff and informed him that Greg Ciesielski the security guard that restrained Plaintiff and made the racist comment, made racist comments and jokes to him and other coworkers about African Americans, and that he frequently used excessive force with patients.
22. The security guard who called Plaintiff also reported that he witnessed employees tampering with the internal incident report made on the incident involving Plaintiff, and he believed the use of racial slur was removed from the internal incident report, and he stated that employees were instructed not to discuss the incident. The security guard also stated that Greg Ciesielski was not disciplined or suspended because of the incident.
23. As a result of the above actions and inactions of Defendants as described above and below, Plaintiff suffered injuries and damages. Defendants are sued jointly and severally."

#racism#Alexander Morris#four tops#medical racism#the patient clearly having a heart episode and time is crucial but they decided to give him a psych eval because they wouldn't believe him#lawsuit
5K notes
·
View notes
Text
Hale had been diagnosed with at least five mental illnesses and had received cocktails of psychiatric drugs as “treatment” and some of the adverse events associated with just the known drugs (Lorazepam, Buspirone, Lexapro, Hydroxyzine and Prozac) Hale had been prescribed could be responsible for the shooter’s deadly thoughts.
So why are Hale’s mental health records being withheld (Evidence Item #46 “Psych File”) for public review? It’s no secret that Vanderbilt “treated” Hale most of her life. The “treatment” provided to Hale included talk therapy and mind-altering psychotropic drugs…cocktails of them.
Who wants to bet that not one of the psychiatrists, therapists or MDs at Vanderbilt ever advised Hale’s parents or Hale that none of the psychiatric drugs being prescribed actually treated any known abnormality in the brain? In other words, not one of Hale’s treating physicians ever said “hey, we don’t know what is causing your behavior, but these drugs will make you feel different.
They aren’t treating any abnormality in your brain because there are no known abnormalities in your brain for any of our psychiatric diagnoses.” This is called informed consent. Telling patients, the truth about a diagnosis and treatment.
But, of course, no one can say whether this information was provided to Hale because Hale’s mental health records haven’t been made public. But the “right” people have seen the mental health records.
------------------------------------------------------------------------------
Poisoning and destroying the minds of Americans.
4 notes
·
View notes
Text
Psychopathology, Ch 2 pt. 3
Identify the major types of helping professionals and describe their training backgrounds and professional roles.
Clinical psychologists: have earned a doctoral degree in psychology, either a PhD (Doctorate of Philosophy), a PsyD (Doctorate of Psychology), or an EdD (Doctorate of Education) from an accredited college or university. Training in clinical psychology typically involves four years of graduate coursework, followed by a year-long internship and completion of a doctoral dissertation. Clinical psychologists specialize in administering psychological tests, diagnosing psychological disorders, and practicing psychotherapy. Until recently, they were not permitted to prescribe psychiatric drugs. However, as of this writing, five states (Idaho, Illinois, Iowa, Louisiana, and New Mexico) have enacted laws granting prescription privileges to psychologists who complete specialized training programs. The granting of prescription privileges to psychologists remains a hotly contested issue between psychologists and psychiatrists and within the field of psychology itself.
Counseling psychologists: also hold doctoral degrees in psychology and have completed graduate training preparing them for careers in college counseling centers and mental health facilities. They typically provide counseling to people with psychological problems falling in a milder range of severity than those treated by clinical psychologists, such as difficulties adjusting to college or uncertainties regarding career choices.
Psychoanalysts: typically are either psychiatrists or psychologists who have completed extensive additional training in psychoanalysis. They are required to undergo psychoanalysis themselves as part of their training.
Psychiatrists: have earned a medical degree (MD) and completed a residency program in psychiatry. Psychiatrists are physicians who specialize in the diagnosis and treatment of psychological disorders. As licensed physicians, they can prescribe psychiatric drugs and may employ other medical interventions, such as electroconvulsive therapy (ECT). Many also practice psychotherapy based on training they receive during their residency programs or in specialized training institutes.
Psychiatric nurses: typically are registered nurses (RNs) who have completed a master’s program in psychiatric nursing. They may work in psychiatric facilities or in group medical practices where they treat people suffering from severe psychological disorders.
Clinical or psychiatric social workers: have earned a master’s degree in social work (MSW) and use their knowledge of community agencies and organizations to help people with severe mental disorders receive the services they need. For example, they may help people with schizophrenia make a more successful adjustment to the community once they leave the hospital. Many clinical social workers practice psychotherapy or specific forms of therapy, such as marital or family therapy.
Counselors: have earned a master’s degree by completing a graduate program in a counseling field, such as mental health counseling or rehabilitation counseling. Counselors work in many settings, including private practices, schools, college testing and counseling centers, and hospitals and health clinics. Many specialize in vocational evaluation, marital or family therapy, rehabilitation counseling, or substance abuse counseling. Counselors may focus on providing psychological assistance to people with milder forms of disturbed behavior or those struggling with a chronic or debilitating illness or recovering from a traumatic experience. Some are clergy members who are trained in pastoral counseling programs to help parishioners cope with personal problems.
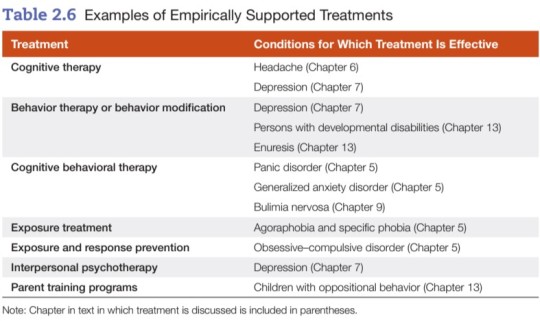
Describe the goals and techniques of the following forms of psychotherapy: psychodynamic therapy, behavior therapy, person-centered therapy, cognitive therapy, cognitive-behavioral therapy, eclectic therapy, group therapy, family therapy, and couples therapy.
Psychotherapy: a structured form of treatment derived from a psychological framework that consists of one or more verbal interactions or treatment sessions between a client and a therapist.
- used to treat psychological disorders, help clients change maladaptive behaviors or solve life’s problems, or to help them develop their unique potentials.
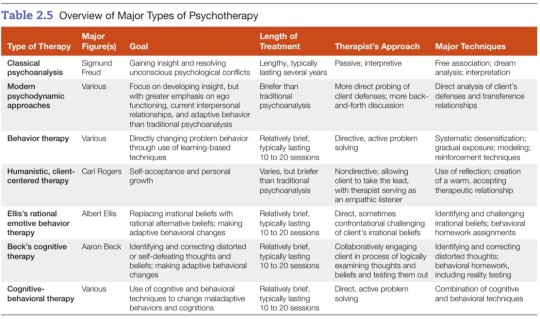
Psychoanalysis: the method of psychotherapy developed by Sigmund Freud.
Psychodynamic therapy: therapy that helps individuals gain insight into and resolve deep-seated conflicts in the unconscious mind.
Free association: the method of verbalizing thoughts as they occur without a conscious attempt to edit or censor them.
Transference relationship: in psychoanalysis, the client’s transfer or generalization to the analyst of feelings and attitudes the client holds toward important figures in their life.
Countertransference: in psychoanalysis, the transfer of the analyst’s feelings or attitudes toward other persons in their life onto the client.
Behavior therapy: the therapeutic application of learning-based techniques to resolve psychological disorders.
Systematic desensitization: a behavior therapy technique for overcoming phobias by means of exposure to progressively more fearful stimuli (in imagination or by viewing slides) while remaining deeply relaxed.
Gradual exposure: in behavior therapy, a method of overcoming fears through a stepwise process of exposure to increasingly fearful stimuli in imagination or in real-life situations.
Token economy: a behavioral treatment program that creates a controlled environment in which desirable behaviors are reinforced by dispensing tokens that may be exchanged for desired rewards.
Person-centered therapy: the establishment of a warm, accepting therapeutic relationship that frees clients to engage in self-exploration and achieve self-acceptance.
Empathy: the ability to understand someone’s experiences and feelings from that person’s point of view.
Genuineness: the ability to recognize and express one’s true feelings.
Congruence: the coherence or fit among one’s thoughts, behaviors, and feelings.
Cognitive therapy: a form of therapy that helps clients identify and correct faulty cognitions (thoughts, beliefs, and attitudes) believed to underlie their emotional problems and maladaptive behavior.
Rational emotive behavior therapy (REBT): a therapeutic approach that focuses on helping clients replace irrational, maladaptive beliefs with alternative, more adaptive beliefs.
Cognitive behavioral therapy (CBT): a form of psychotherapy incorporating cognitive and behavioral techniques.
Eclectic therapy: an approach to psychotherapy that incorporates principles or techniques from various systems or theories.

Group therapy: a form of therapy in which a group of clients with similar problems meets together with a therapist.
Family therapy: a form of therapy in which the family, not the individual, is the unit of treatment.
Couples therapy: a form of therapy that focuses on resolving conflicts in distressed couples.
Evaluate the effectiveness of psychotherapy and the role of non-specific factors in therapy.
Nonspecific treatment factors: factors not specific to any one form of psychotherapy, including
empathy, support, and attention shown by the therapist
the therapeutic alliance = attachment the client develops toward the therapist and the therapy process
the working alliance = effective working relationship in which the therapist and client work together identifying and confronting the important problems and concerns the client faces
Telehealth: delivery or facilitation of treatment services via telecommunication or digital technology.
Evaluate the role of multicultural factors in psychotherapy and barriers to use of mental health services by ethnic minorities.
- Cultural sensitivity involves more than good intentions. Therapists must have accurate knowledge of cultural factors and the ability to apply that knowledge when developing culturally sensitive approaches to treatment.
- Just because a given therapy works with one population group does not mean that it will necessarily work with other groups. Therapists using established treatments should consider how they can incorporate culturally specific elements to boost treatment benefits in working with people from different ethnic or racial groups.
- Some of the barriers to mental health services for marginalized communities include...
Cultural mistrust: People from minority groups often fail to use mental health services because they don’t trust mental health institutions/professionals. Mistrust may stem from a cultural and/or personal history of oppression and discrimination, or experiences in which service providers were unresponsive to their needs. When minority clients perceive white therapists and white-dominated institutions to be cold or impersonal, they are less likely to place their trust in them.
Mental health literacy: A person may not make use of mental health services because they lack knowledge of mental disorders and how to treat them.
Institutional barriers: Facilities may be inaccessible to marginalized people because they are located at a considerable distance from their homes or because public transportation is lacking. Marginalized people are often overwhelmed or intimidated by bureaucratic red tape and/or protocol around health procedures.
Cultural barriers: Many recent immigrants have had little or no previous contact with mental health professionals. They may hold different conceptions of mental health problems or view mental health problems as less severe than physical problems. In some cultures, the family is expected to take care of members who have psychological problems and may resist outside assistance. Other cultural barriers include cultural differences between socio-economically disadvantaged clients and majority white + middle-class mental health staff, and the stigma often associated with seeking mental health treatment.
Language barriers: Mental health facilities may lack the resources to hire mental health professionals who are fluent in the languages of the communities they serve.
Economic and accessibility barriers: Financial burdens are often a major barrier to use of mental health services. Living in a rural or isolated area where mental health services may be lacking or inaccessible is also a big hurdle.
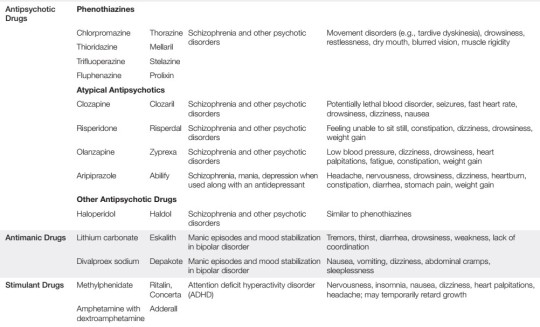
Psychopharmacology: the field of study that examines the effects of therapeutic or psychiatric drugs.
Identify the major categories of psychotropic or psychiatric drugs and examples of drugs in each type and evaluate their strengths and weaknesses.
Anti-anxiety drugs: drugs that combat anxiety and reduce states of muscle tension.
~ also called anxiolytics
~ examples include benzodiazepines (Valium, Xanax) as well as hypnotic sedatives (Halcion)
+ can be safe and effective in treating anxiety and insomnia
- potential for psychological and/or physical dependence, so they tend to be better for short term or occasional relief, not long term or daily use
Rebound anxiety: the experiencing of strong anxiety following withdrawal from a tranquilizer.
Antipsychotic drugs: drugs used to treat schizophrenia or other psychotic disorders.
~ also called neuroleptics
~ examples include Thorazine, Mellaril, Prolixin, Clozapil (atypical)
+ drastically reduced the need for long-term hospitalization, physical restraints, and confinement
- unpleasant side effects, such as muscular rigidity and tremors; long-term use of antipsychotic drugs (with exception of Clozapine) can produce tardive dyskinesia, a potentially irreversible and disabling motor disorder
Antidepressants: drugs used to treat depression that affect the availability of neurotransmitters in the brain.
~ four major classes: tricyclic antidepressants (TCAs), monoamine oxidase inhibitors (MAOIs), selective serotonin-reuptake inhibitors (SSRIs), and serotonin-norephinephrine reuptake inhibitors (SNRIs)
~ examples include Tofranil, Elavil, Sinequan (tricyclics), Nardil (MAOI), Prozac, Zoloft (SSRI), Effexor (SNRI)
+ antidepressants provide beneficial effects for a wide variety of psychological disorders
- however, there are side effects for each category, and in the case of MAOIs, a patient’s diet is heavily restricted

Electroconvulsive therapy (ECT): a method of treating severe depression by administering electrical shocks to the brain.
+ significant improvement for patients experiencing severe epileptic seizures or major clinical depression that has not responded to other treatment
- high relapse rates and memory loss for events occurring around the time of treatment; for these reasons, ECT is a last resort
Describe the use of psychosurgery and evaluate its effectiveness.
~ Previously, the prefrontal lobotomy was the most common form of psychosurgery. This procedure involved surgically severing nerve pathways linking the thalamus to the prefrontal lobes of the brain.
~ The premise of this operation was the belief that severing the connections between the thalamus and the frontal lobe of the cerebral cortex would control a patient’s violent or aggressive tendencies.
- This procedure was abandoned because (1) there was insufficient evidence of its effectiveness and (2) it often produced serious complications or even death.
- When anti-psychotic drugs became available during the 1950s, psychosurgery was all but eliminated.
+ In recent years, more sophisticated psychosurgery techniques have been introduced which target much smaller parts of the brain and produce far less damage than the prefrontal lobotomy. These techniques have been used to treat patients with severe OCD, bipolar, and/or major clinical depression who have failed to respond to other treatments.
~ Another experimental technique is deep brain stimulation (DBS), a surgical procedure in which electrodes are implanted in the brain and used to electrically stimulate deeper brain structures.
+ DBS shows promise in treating severe forms of depression and OCD that have failed to respond to more conservative treatments.
- However, DBS may have serious complications and its effectiveness needs to be investigated further. Thus, it is still an experimental treatment.
Evaluate biomedical treatment approaches.
~ Overall, a combination of medication and talk therapy seems to be more helpful for most mental health patients than either treatment alone.
~ The benefits and risks/side effects of each medication need to be carefully considered and discussed by the provider and the patient.
10 notes
·
View notes
Video
youtube
Gary Valenciano - Sana Maulit Muli (Audio) 🎵 | With Love
MINDFUL . care
MINDFUL CARE SERVICES, LLC
MINDFUL CARE
https://www.mindful.care/pre-registration
Upgrade to Better
Mental Health: Pre-RegistrationMindful Care’s
Patient-First Approach puts your well-being front
and center, offering exceptional:
MicroTherapy™ (20-minutes) - CHOOSING THIS
Same-day/next-day medication management and
symptom stabilization
Group Therapy
FOR - ME - 20 MIN - VIRTUAL - APPOINTMENT
FOR - MICRO-THERAPY - BY - ASUS - LAPTOP
AMAZON - PRIME - OVER - $282 - FREE - SHIP
MINDFUL - CARE
EMAIL - [email protected]
CALL - (516) 505 - 7200
OFFER - SAME OR - NEXT DAY - APPOINTMENTS
SUNDAY - TO - FRIDAY
8A - 6P
MINDFUL - CARE - TEAM
NURSE - PRACTITIONERS (NP) - DON’T - GET
CERTIFIED - PHYSICIAN - ASSOCIATE (PA - C)
APPOINTMENT - VIRTUAL - OR - IN - PERSON
HAILEAH - FLORIDA - FAR - FR - MIAMI
TRAINED - CERTIFIED - 2 - TREAT - MENTAL
HEALTH - PATIENTS
THEY - WORK - CLOSELY - WITH - SUPERVISING
PSYCHIATRISTS ( MD ) - 2 - COORDINATE - AND
REVIEW - TREATMENT
BOTH - COMPLETED - MASTER’s - DEGREE
PROGRAMS - ABOUT - MEDICATION - AND
PROVIDE - THERAPY - DELIVER - HEALTHCARE
SERVICES - AND - GENERAL - MEDICINE
AND - MENTAL - HEALTH
SO - THEREFORE
I - CHOOSE - VIRTUAL - APPOINTMENTS
I - CHOOSE
ERNAKULAM - NATIONAL - PARK - ALSO
ERNAKULAM - KERAL - INDIA
MAHATMA GANDHI - UNIVERSITY
BEAUTIFUL - MISS UNIVERSE - INDIA
PSYCHIATRIC PHYSICIAN ASSOCIATE
ASWATHY KRISHNAKUMAR - WOMAN
I - CHOOSE - MISS INDIA
https://us.shopkorea.co/mindful-care
MY DIAGNOSIS - DUALITY
MY - PLACE - OF - BIRTH - PHILIPPINES
4 - MISS UNIVERSE
1ST - 2 FEMALE - PRESIDENTS OF ASIA
JESUS - IS - LORD
LEAVING - 2 - SIGN - MY - LEASE PAPERS
LEAVING - MAIN - LIBRARY - SOON - TRUE
9 DAYS
BUT - MY - CAPITAL ONE - MASTERCARD
ARRIVING - SOON - INSIDE - MAILBOX
DOWNTOWN - MIAMI
12 MIN - WALKING - 2
LABRE PLACE - APARTMENTS
350 NW 4TH ST
MIAMI FL 33128 - 1668
NOT - LEGITIMATE - BUSINESS
FULL - OF - BLK - PEOPLE
JESSICA - BLK - FEMALE - PROPERTY MANAGE
OF - THIS - BUILDING - 13 YEARS - OLD - AND
SHEPERDS - COURT - APARTMENTS - MIDDLE
FR - SIDE - OF - CAMILLUS HOUSE
8A - 4P - NOT - OBSERVED - BOTH - BUILDINGS
1 SPANISH - MAINTENANCE - EACH - ALSO BUT
OTHER - PLACE - THE - HEAD - OF - 2 - MALES
BUS TEL (305) 577 - 9744
ACTIVE - BUILDING - APP - 2 - PAY - ONLINE
RENT - PAYMENTS - VISA - MC - AMEX - DISCOVER
DO - NOT - CHOOSE - CHECKING - PAYMENT - FOR
CARDS - EASY - 2 - REPLACE - CHECKING - NOT SO
EASY - 2 - REPLACE - SMARTER - AND - WISER - US
1 note
·
View note
Text
What are the top 10 specializations in MD/MS for the future and how can I secure direct MD/MS admission through NEET PG?
When considering MD/MS specializations for the future, it's essential to look at both current demand and emerging healthcare trends. Below are the top 10 specializations in MD/MS that are expected to have great prospects in the coming years:
MD in Radiology – With advancements in imaging technology and the growing need for diagnostic services, radiology remains a top choice.
MD in Dermatology – The demand for skincare treatments, cosmetic procedures, and dermatological interventions is rising globally.
MD in General Medicine – The need for specialists in general medicine is always high, as they are crucial for diagnosing and managing a wide range of medical conditions.
MD in Pediatrics – With increasing healthcare focus on child development and wellness, pediatricians are in demand.
MD in Psychiatry – The growing awareness of mental health and well-being has led to a sharp increase in demand for psychiatric professionals.
MD in Emergency Medicine – The unpredictable nature of emergencies ensures a constant need for specialists in this field.
MS in Orthopedics – Orthopedics is expected to grow due to aging populations and the increasing number of lifestyle-related injuries.
MS in Obstetrics and Gynecology – Women's health, fertility treatments, and maternity care ensure a consistent demand for specialists in this field.
MD in Anesthesiology – Surgical procedures are increasing, and with it, the demand for anesthesiologists.
MD in Cardiology – Cardiovascular diseases are among the leading causes of death globally, making cardiology a highly sought-after specialization.
0 notes
Text
Why choose MD in Psychiatry from GS Medical College & Hospital?
Choosing a career in psychiatry is a profound decision that blends a passion for understanding the human mind with a commitment to improving mental health. Pursuing an MD in Psychiatry equips you with the knowledge and skills necessary to diagnose, treat, and support individuals facing mental health challenges. One of the Best Medical Colleges for Post Graduation in Ghaziabad UP at GS Medical College & Hospital stands out as a premier institution for medical education, offering an exceptional MD in Psychiatry program that combines academic excellence with a focus on practical experience.

In this article, we'll explore why GS Medical College & Hospital is an ideal choice for those aspiring to specialize in psychiatry. We'll discuss the comprehensive curriculum, cutting-edge facilities, experienced faculty, and the unique opportunities available to students at this prestigious institution. By the end of this article, you'll understand the many benefits of pursuing an MD in Psychiatry at GS Medical College & Hospital and why it's an excellent step toward a fulfilling and impactful career in mental health.
Understanding the Importance of Psychiatry in Modern Healthcare:
The Rising Need for Mental Health Professionals:
In today's healthcare landscape, mental health is gaining unprecedented attention, highlighting the crucial role of psychiatrists. According to the World Health Organization (WHO), mental or neurological disorders will affect one in four people globally at some point in their lives. This significant statistic underscores the increasing demand for mental health professionals, making psychiatry a vital and expanding field.
The Role of Psychiatrists:
Psychiatrists are central to diagnosing and treating mental health disorders. They offer a range of services, including:
Diagnosis and Treatment: Psychiatrists assess mental health conditions and provide tailored treatment plans, including medication and therapy.
Therapeutic Interventions: They deliver various forms of therapy, such as cognitive-behavioral therapy (CBT) and psychodynamic therapy.
Medication Management: Psychiatrists prescribe and monitor psychiatric medications to manage symptoms effectively.
Collaborative Care: They work alongside psychologists, social workers, and other healthcare professionals to ensure comprehensive patient care.
The Impact of Diminishing Stigma:
As societal attitudes towards mental health evolve, the stigma surrounding mental illness continues to wane. This shift is leading to increased awareness and acceptance, which in turn drives higher demand for mental health services. As a result, pursuing a career in psychiatry not only offers a secure and rewarding path but also contributes to a critical and growing need within modern healthcare.
Key Points:
Growing Demand: Mental health issues are increasingly prevalent, driving demand for skilled psychiatrists.
Expanded Roles: Psychiatrists provide essential services, including diagnosis, therapy, and medication management.
Evolving Attitudes: Diminishing stigma enhances awareness and acceptance, further emphasizing the need for mental health professionals.
Choosing psychiatry as a career allows you to make a meaningful impact on individuals' lives while addressing a crucial and expanding field in healthcare.
Why Choose Psychiatry?:
Impactful and Compassionate Care:
Psychiatry stands out as a field that uniquely combines scientific expertise with compassionate patient care. As a psychiatrist, you play a crucial role in addressing and alleviating mental health issues such as depression, anxiety, and schizophrenia. Your interventions can profoundly affect patients' lives, offering them hope and improving their overall quality of life.
Diverse Career Opportunities:
Psychiatry offers a broad spectrum of career paths, including:
Clinical Practice: Direct patient care, diagnosing and treating mental health disorders.
Research: Investigating new treatments and advancing mental health science.
Teaching: Educating future mental health professionals.
Public Health: Developing policies and programs to enhance community mental health.
This versatility allows you to align your career with your personal interests and strengths, making psychiatry a fulfilling and adaptable profession.
Overview of the MD in Psychiatry Program at GS Medical College & Hospital:
Comprehensive Curriculum:
The MD in Psychiatry program at GS Medical College & Hospital is meticulously crafted to provide students with a robust and well-rounded education in psychiatry. The program integrates theoretical knowledge with hands-on clinical experience, ensuring a deep understanding of both the science and practice of mental health care. Key components of the curriculum include:
Psychopathology: Detailed study of the nature, causes, and classifications of mental disorders.
Psychopharmacology: In-depth learning about psychiatric medications, their mechanisms, and their effects.
Psychotherapy: Training in diverse therapeutic modalities such as cognitive-behavioral therapy (CBT), psychoanalysis, and various counseling techniques.
Neuropsychiatry: Examination of the intersection between neurological and psychiatric conditions, focusing on the brain's role in mental health.
Child and Adolescent Psychiatry: Specialized focus on the psychiatric needs and treatment approaches for younger populations.
Community Psychiatry: Emphasis on public health strategies, preventive measures, and community-based mental health interventions.
The curriculum is designed to be dynamic, incorporating the latest research and advancements in psychiatry to ensure students are well-prepared for contemporary challenges in the field.
State-of-the-Art Facilities:
Top PG Medical Colleges in Uttar Pradesh at GS Medical College & Hospital boasts advanced facilities that enhance both learning and research:
Advanced Laboratories: Equipped with cutting-edge technology for research in neuropsychiatry and psychopharmacology.
Simulation Labs: Provide a controlled environment for students to practice clinical skills and build confidence.
Well-Stocked Library: Offers a comprehensive collection of books, journals, and digital resources relevant to psychiatry.
Counseling and Therapy Rooms: Designed for confidential and effective patient consultations, providing a realistic practice environment.
These facilities are integral to the program, offering practical experience and fostering a deeper understanding of psychiatric care.
Experienced Faculty:
The program is supported by a distinguished faculty comprised of leading experts in psychiatry. The experienced professors and clinicians offer:
Expert Knowledge: Extensive experience and expertise in various subspecialties within psychiatry.
Mentorship: Personalized guidance and support to help students excel academically and professionally.
Research Opportunities: Encouragement to engage in research, present at conferences, and participate in workshops.
The faculty’s dedication ensures that students not only gain theoretical knowledge but also practical insights and skills essential for a successful career in psychiatry.
The Unique Opportunities Available to Psychiatry Students:
Clinical Exposure:
The Best PG Medical Colleges in Uttar Pradesh at GS Medical College & Hospital places a strong emphasis on clinical exposure, recognizing the importance of hands-on experience in medical education. Psychiatry students have the opportunity to work with a diverse patient population, gaining experience in diagnosing and treating a wide range of mental health conditions.
Students participate in clinical rotations in various settings, including:
Inpatient Psychiatric Wards: Where they learn to manage acute psychiatric conditions.
Outpatient Clinics: Providing long-term care and follow-up for patients with chronic mental health issues.
Community Mental Health Programs: Engaging with the community to provide mental health education, preventive care, and support.
This extensive clinical exposure helps students develop the practical skills needed to excel in their careers as psychiatrists.
Research Opportunities:
The Top Medical Colleges in UP for PG at GS Medical College & Hospital is committed to advancing the field of psychiatry through research. The college encourages students to engage in research projects, providing access to cutting-edge laboratories and resources. Research areas include neuropsychiatry, psychopharmacology, behavioral sciences, and more.
Students have the opportunity to work alongside experienced researchers and faculty members, contributing to important studies that can influence the future of mental health care. This experience not only enhances their understanding of psychiatry but also prepares them for careers in academic medicine or research.
Workshops and Conferences:
To complement their academic and clinical training, students at GS Medical College & Hospital are encouraged to participate in workshops, seminars, and conferences. These events provide valuable opportunities to learn from experts in the field, stay updated on the latest developments in psychiatry, and network with peers and professionals.
The college regularly hosts guest lectures and workshops on topics such as:
Advanced Psychotherapy Techniques
The Latest Trends in Psychopharmacology
Mental Health Policy and Advocacy
Ethics in Psychiatry
Attending these events not only broadens students' knowledge but also helps them build a professional network that can be invaluable in their future careers.
The Career Prospects for MD Psychiatry Graduates:
Clinical Practice:
One of the most common career paths for MD Psychiatry graduates is clinical practice. As a psychiatrist, you can work in a variety of settings, including:
Hospitals: Providing inpatient and outpatient care for patients with psychiatric conditions.
Private Practice: Offering individual therapy, group therapy, and medication management in a private clinic setting.
Mental Health Clinics: Working in specialized clinics that focus on particular areas of mental health, such as addiction, child psychiatry, or forensic psychiatry.
Community Health Centers: Providing care to underserved populations and working on mental health education and prevention programs.
Academic Medicine:
For those interested in teaching and research, a career in academic medicine is a rewarding option. As a faculty member at a medical college, you can:
Teach: Educate the next generation of psychiatrists and mental health professionals.
Conduct Research: Engage in cutting-edge research that advances the field of psychiatry.
Mentor Students: Guide students and residents through their medical education and early career development.
Research and Development:
Psychiatry graduates with a strong interest in research can pursue careers in research and development. This can involve:
Clinical Trials: Working with pharmaceutical companies or research institutions to test new psychiatric medications and treatments.
Behavioral Science Research: Studying the underlying causes of mental health disorders and developing new therapeutic approaches.
Neuropsychiatric Research: Exploring the connection between neurological and psychiatric conditions to improve diagnostic and treatment methods.
Public Health and Policy:
For those passionate about mental health advocacy, a career in public health and policy offers the chance to make a broader impact. Psychiatrists in this field work on:
Mental Health Policy: Developing and advocating for policies that improve access to mental health care and reduce stigma.
Public Health Programs: Designing and implementing programs that address mental health issues on a community or national level.
Global Health: Working with international organizations to improve mental health care in low- and middle-income countries.
The Benefits of Choosing GS Medical College for Your Psychiatry Education:
Supportive Learning Environment:
The Private Medical College in UP at GS Medical College & Hospital provides a supportive learning environment where students are encouraged to excel academically and personally. The college fosters a culture of collaboration and mutual respect, ensuring that each student receives the support they need to succeed. Key aspects of this environment include:
Mentorship Programs: Students are paired with experienced faculty members who provide guidance, support, and career advice throughout their training.
Peer Support: A strong sense of community among students, facilitated by study groups, social events, and peer mentoring.
Counseling Services: Access to mental health resources and counseling to help students manage stress and maintain a healthy work-life balance.
Accreditation and Recognition:
GS Medical College & Hospital is recognized for its commitment to excellence in medical education. The MD in Psychiatry program is accredited by relevant medical education boards and institutions, ensuring that the education you receive meets high standards of quality. Graduates of the program are well-prepared to meet the licensing and certification requirements for practicing psychiatry.
Conclusion:
Choosing to pursue an MD in Psychiatry at GS Medical College & Hospital offers numerous advantages, including a comprehensive curriculum, experienced faculty, state-of-the-art facilities, and extensive clinical exposure. The supportive learning environment and emphasis on research further enhance the educational experience, preparing students for successful careers in psychiatry. For those passionate about mental health and looking for a top-notch educational experience, GS Medical College & Hospital stands out as a premier choice.
Whether you are a prospective student or a medical professional exploring advanced training options, GS Medical College & Hospital provides an exceptional platform to develop expertise in psychiatry and make a meaningful impact in the field of mental health.
#Best Medical Colleges for Post Graduation in Ghaziabad UP#Top PG Medical Colleges in Uttar Pradesh#Best PG Medical Colleges in Uttar Pradesh#Top Medical Colleges in UP for PG#Private Medical College in UP
0 notes
Text
Best Psychiatrist in Germantown, MD | Excel Psychiatric Consultation
We Provide Evidence-based, Cutting-edge TMS, Spravato, Medication Management, and Psychotherapy Treatments in Our Germantown, MD | Excel Psychiatric Consultation | For Appointment Call: 301-820-1715

1 note
·
View note
Text
Navigating Bethesda Psychiatry: Finding the Right Psychiatrist Bethesda
When searching for mental health support, selecting the right psychiatrist is essential for effective treatment. If you're considering Bethesda Psychiatry, you’re focusing on accessing top-notch mental health care in the Bethesda area. Here's a guide to help you find the best psychologist Bethesda and understand the benefits of local psychiatric services.
Why Opt for Bethesda Psychiatry?
Choosing Bethesda Psychiatry offers several advantages, including:
Local Expertise: Psychiatrists in Bethesda are familiar with the community's specific needs and challenges, providing care that is tailored to local contexts and concerns.
Comprehensive Services: Bethesda Psychiatry professionals offer a range of services, from medication management to psychotherapy, ensuring a holistic approach to mental health care.
Convenience: Being close to home or work can make attending regular appointments more manageable, enhancing continuity of care.
Finding the Right Psychiatrist Bethesda
When looking for a psychiatrist Bethesda, consider these key factors:
1. Qualifications and Specializations: Verify that the psychiatrist has the appropriate qualifications and specialization to address your specific mental health needs. Whether you need treatment for anxiety, depression, or another condition, finding someone with relevant experience is crucial.
2. Patient Reviews: Look for reviews and testimonials from other patients to gauge the psychiatrist’s effectiveness and approach. Positive feedback can be a good indicator of quality care.
3. Consultation: Schedule initial consultations to meet with potential psychiatrists. This will give you a sense of their approach, communication style, and whether you feel comfortable working with them.
Benefits of Choosing a Psychiatrist Bethesda
Opting for a psychiatrist Bethesda offers several benefits:
Tailored Care: Local psychiatrists are well-versed in the specific challenges faced by residents of Bethesda, allowing them to provide more personalized and relevant treatment.
Accessibility: Proximity to your psychiatrist can make it easier to attend regular sessions, which is important for ongoing mental health management.
Community Understanding: A psychiatrist familiar with the Bethesda area can better understand the local factors that might impact your mental health, leading to more effective care.
Making an Informed Decision
To find the best Bethesda Psychiatry services:
1. Research and Compare: Investigate different psychiatrists in Bethesda, comparing their qualifications, specializations, and patient feedback.
2. Consult and Evaluate: Use initial consultations to evaluate how well the psychiatrist’s approach aligns with your needs and preferences.
3. Consider Logistics: Factor in practical considerations such as location, availability, and whether the psychiatrist accepts your insurance.
Conclusion
Selecting the right psychiatrist is a vital step towards achieving effective mental health care. Whether you’re exploring Bethesda Psychiatry or seeking a psychiatrist Bethesda, ensure you find a professional who meets your specific needs and provides the right approach to treatment. By carefully evaluating your options, you can find the best fit for your mental health journey.
Contact Us:
Washington Family Psychiatry
Website:- https://wfpsychiatry.com
Address:- 5225 Pooks Hill Rd, Bethesda, MD 20814, United States
Email:- [email protected]
Contact:- +1 240-428-4792
0 notes
Text
James Donaldson on Mental Health - Suicide Rates Among Asian American and Pacific Islander Youths—A Cause for Alarm

James Donaldson on Mental Health - Suicide Rates Among Asian American and Pacific Islander Youths—A Cause for Alarm
Photo by Mental Health America (MHA) on Pexels.com
Anthony L. Bui, MD, MPH Anna S. Lau, PhD
Suicide is the leading cause of death for Asian American and Pacific Islander youths.1 Asian American individuals are the fastest growing racial group in the United States, and Native Hawaiian and Pacific Islander individuals are the third fastest. Despite the critical importance of preventing suicide among this growing population, the study of mental health among Asian American and Pacific Islander populations has been historically understudied and underfunded nationally.2 Elsewhere in JAMA Network Open, Keum et al3 present a cross-sectional analysis examining trends in suicide rates among Asian American and Pacific Islander youths aged 10 to 19 years. Utilizing national mortality data from the National Center for Health Statistics, the authors calculate crude suicide rates across male and female groups and conduct a trend analysis to assess annual percent changes.
The authors found that Asian American and Pacific Islander youth suicide rates have been increasing. In 2021, the Asian American and Pacific Islander male and female youth suicide rates were 6.49 and 3.72 per 100?000 individuals, respectively. The authors found large increases in suicide rates from 1999 to 2021, with a 72% increase in youth suicide rates for males and 125% increase for females during the 22-year period. They detected that Asian American and Pacific Islander male and female youths experienced growth in suicide rates, starting in 2009 and 2004 and peaking in 2019 and 2020, respectively. The findings of this study bring up several important points for discussion.
First, the rise of Asian American and Pacific Islander youth suicide rates is alarming and coincides with a growing increase in anti-Asian hate and xenophobia, including hate incidents, verbal abuse, and cyberbullying, seen during this period.4 Structural, institutional, and interpersonal racism contribute to harm youths. Notably, oppression, marginalization, and erasure of culture may contribute to accelerating risk of suicide seen in Native Hawaiian and Pacific Islander adolescents, who have higher odds of suicide attempts compared with White peers.5 The lethality of risks are further exacerbated by the prevailing model minority stereotype, in which Asian American and Pacific Islander youths are all generalized to be academically exceptional, socially mobile, diligent, and well-adjusted. This stereotype was born out of political motivation to deny the current conditions and persistent legacy of racism, conveying that through hard work all people can succeed in a country that functions as a meritocracy. This ideological device is used to deter coalitions for racial justice among minoritized groups against systems of disadvantage. It also belies minority stress experiences that affect Asian American and Pacific Islander youths and renders invisible forms of distress and mental health needs. One by-product of this invisibility is the under recognition of depression and suicide risk. Previous studies have shown that Asian American youths with need are less likely to seek out mental health care and utilize school-based services or psychotropic medications compared with youths who belong to other racial and ethnic groups. Large disparities in treatment are even observed among youths who received emergency attention for acute psychiatric crises (most commonly involving suicide risk), with Asian American and Pacific Islander youths being the racial group least likely to receive follow-up outpatient care.6 Help-seeking barriers include family and individual stigma and limited mental health literacy, but these individual factors interact with structural barriers, resulting in a profound lack of accessible culturally and linguistically responsive services for Asian American and Pacific Islander communities.
Second, the authors3 note important patterns as a function of sex. Although Asian American and Pacific Islander male youths have higher suicide rates compared with female youths, Asian American and Pacific Islander female youths have seen larger increases in the rates during the study period. We agree with the authors that culturally rooted and gendered family roles may contribute to the higher suicide rates among Asian American and Pacific Islander male youths, while worsening intersectional discrimination from sexism and racism may contribute to the growing rates among Asian American and Pacific Islander female youths. In terms of sexuality, due to the limitations of national mortality data, this study was unable to disaggregate suicide rate trends among lesbian, gay, bisexual, transgender, and queer (LGBTQ) youths, who have much higher rates of suicidal ideation and self-harm behaviors compared with heterosexual and cisgender youth.5 Intersectional minority stress may amplify these risks for Asian American and Pacific Islander sexual minority youths. It remains paramount to study prevalence, risk, and protective processes and to develop culturally responsive prevention to reduce suicide risk in this population.
Third, it is imperative to assess whether increased access to firearms may be contributing to increasing rates of suicide among Asian American and Pacific Islander youths. Although suffocation remains the most common method of death by suicide among Asian American and Pacific Islander youths, this rate has been falling while use of firearms has increased sharply in recent years.1 Rates of firearm ownership, carrying, and unsafe storage have increased in Asian American and Pacific Islander households as anticipated racism-related threats have also increased since the COVID-19 pandemic with the associated rise in anti-Asian hate.7 New efforts focusing on lethal means safety, including recent federal funding opportunities, must attend to racism-related stress and need for firearm injury prevention in Asian American and Pacific Islander communities.
Fourthly, this study was limited in its ability to disaggregate the Asian American and Pacific Islander population into ethnic subgroups. Combining the more than 50 ethnic subgroups among Asian American and Pacific Islander individuals as a monolithic group undermines the heterogenous diversity and understanding of specific disparities among ethnic subgroups. It is important that future studies, public surveillance programs, and policy and advocacy efforts disaggregate Asian American and Pacific Islander subgroups to prioritize prevention efforts and facilitate culturally tailored solutions to youth suicide reduction.
Lastly, the paucity of funding dedicated to Asian American and Pacific Islander mental health research is worrisome. Implicit and explicit biases and Asian American and Pacific Islander invisibility contribute to low investments from federal research and service funding mechanisms.2 The pervasive and harmful nature of the model minority stereotype has likely undermined the allocation of resources to study and serve this population and worsened inequities. Moreover, epidemiologic surveys have inadequate inclusion of Asian American and Pacific Islander populations to generate estimates of prevalence and incidence.4
We suspect that the recent rise in suicide rates among Asian American and Pacific Islander youths may be attributable to increased racialized stress, anti-immigrant sentiment, and Asian hate; escalating societal pressures on adolescents to achieve; and increased access to firearms. Although research on Asian American and Pacific Islander youth mental health has typically focused on cultural determinants, such as parent-child acculturation gaps in immigrant families or cultural values that shape family communication or achievement stress, we do not focus on these cultural deficit explanations. There is little reason to believe that marked changes to family processes or cultural heritage factors have occurred in recent years that can account for Asian American and Pacific Islander youth suicide rates peaking in 2020. Unfortunately, this increased need among Asian American and Pacific Islander youths has far outstripped the availability of culturally responsive mental health interventions. Asian American and Pacific Islander individuals deserve greater attention and representation in the science of mental health, suicide prevention, and health equity. To curb the worsening youth suicide rates seen in Asian American and Pacific Islander communities, we need meaningful investments in research along the translational spectrum, intentional workforce development of clinicians prepared to serve the Asian American and Pacific Islander community across youth sectors of care, improved surveillance, and culturally tailored, evidence-based, community-based interventions to support Asian American and Pacific Islander youth mental health.
#James Donaldson notes:Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticleFind out more about the work I do on my 501c3 non-profit foundationwebsite www.yourgiftoflife.org Order your copy of James Donaldson's latest book,#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
Link for 40 Habits Signupbit.ly/40HabitsofMentalHealth
If you'd like to follow and receive my daily blog in to your inbox, just click on it with Follow It. Here's the link https://follow.it/james-donaldson-s-standing-above-the-crowd-s-blog-a-view-from-above-on-things-that-make-the-world-go-round?action=followPub
www.celebratingyourgiftoflife.com
Photo by Mental Health America (MHA) on Pexels.com
Read the full article
0 notes
Text
Psychiatry Services | Psychiatric Diagnosis And Different.

A psychiatric diagnosis is different – there are often no physical symptoms, nor are there any biological tests conclusive for mental distress. Although tests can be important to rule out underlying physical causes, a health professional making a psychiatric diagnosis has to rely on a person’s own description of their thoughts and feelings, alongside observations of their behavior.
In this sense, it is often said that those best placed to make a diagnosis are the people themselves, supported by information and empowered discussion with health care professionals.
Access Health Services Psychiatric Diagnosis
#Access Health Services#Access Health Care Services#Access Health Care Center#Psychiatric Clinic MD#ADHD Assessment Baltimore MD#Telepsychiatry Services Baltimore#ADHD Meds Baltimore MD#ADHD Assessment MD#Weight Loss Therapy Baltimore#Iv Nad Therapy Treatments#Psychiatric Services Baltimore#Iv Nad Therapy Clinic#Psychiatrist Baltimore MD
0 notes
Text
Dr. Gorav Gupta: The Premier Psychiatrist for Bipolar Disorder in Delhi
Navigating the complexities of bipolar disorder can be a daunting journey, both for those affected and their loved ones. In the bustling city of Delhi, Dr. Gorav Gupta stands out as a leading expert in the field, offering compassionate care and evidence-based treatments for individuals with bipolar disorder. His dedication and expertise have made him one of the most sought-after psychiatrists in the region.
Who is Dr. Gorav Gupta?
Dr. Gorav Gupta is a renowned psychiatrist based in Delhi, specializing in the diagnosis and treatment of bipolar disorder. With a distinguished educational background and extensive clinical experience, Dr. Gupta has earned a reputation for his patient-centric approach and deep understanding of psychiatric conditions.
Educational Background and Credentials
Dr. Gupta holds an MBBS and an MD in Psychiatry, alongside numerous certifications that underscore his commitment to ongoing professional development. His extensive training equips him with the skills and knowledge required to manage complex mental health conditions, particularly bipolar disorder.
Understanding Bipolar Disorder
Bipolar disorder, also known as manic-depressive illness, is a mental health condition characterized by extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). These mood swings can affect sleep, energy levels, behavior, and the ability to carry out day-to-day tasks. Proper diagnosis and treatment are crucial for managing the symptoms and improving quality of life.
Dr. Gupta's Approach to Treating Bipolar Disorder
Dr. Gorav Gupta's approach to treating bipolar disorder is comprehensive and tailored to the individual needs of each patient. His methodology includes the following key components:
1. Accurate Diagnosis: Dr. Gupta conducts thorough assessments to accurately diagnose bipolar disorder. This involves detailed patient interviews, psychological evaluations, and, when necessary, medical tests to rule out other conditions.
2. Personalized Treatment Plans: Understanding that each patient's experience with bipolar disorder is unique, Dr. Gupta creates customized treatment plans. These plans often include a combination of medication, psychotherapy, and lifestyle modifications tailored to the patient's specific needs and circumstances.
3. Medication Management: Dr. Gupta carefully selects and monitors medications to stabilize mood swings and manage symptoms effectively. He stays up-to-date with the latest advancements in pharmacotherapy to provide the best possible treatment options with minimal side effects.
4. Psychotherapy: Various forms of psychotherapy, including Cognitive Behavioral Therapy (CBT) and psychoeducation, are integral to Dr. Gupta's treatment approach. These therapies help patients understand their condition, develop coping strategies, and improve their emotional regulation.
5. Holistic Care: Dr. Gupta emphasizes the importance of a holistic approach to managing bipolar disorder. This includes encouraging healthy lifestyle choices such as regular exercise, balanced nutrition, adequate sleep, and stress management techniques.
6. Family Involvement and Support: Recognizing the impact of bipolar disorder on families, Dr. Gupta often involves family members in the treatment process. He provides education and support to help them understand the condition and offer effective support to their loved ones.
7. Continuous Monitoring and Follow-Up: Bipolar disorder requires ongoing management and regular follow-up appointments. Dr. Gupta is committed to providing continuous support, monitoring progress, and making necessary adjustments to treatment plans to ensure long-term stability and well-being.
Patient Testimonials
Dr. Gupta’s patients frequently share their success stories, highlighting his empathetic nature, professionalism, and the positive changes they have experienced under his care. Testimonials often emphasize his ability to provide a supportive and understanding environment, which significantly contributes to their recovery and stability.
How to Consult Dr. Gorav Gupta
Dr. Gorav Gupta practices at several prestigious medical institutions in Delhi. To schedule an appointment, you can contact his office directly or visit his clinic's website for more information. Given his expertise and high demand, it is advisable to book your consultation well in advance.
Conclusion
Bipolar disorder can present significant challenges, but with the right help, individuals can lead fulfilling lives. Dr. Gorav Gupta’s expertise, personalized care, and comprehensive treatment approach make him a standout psychiatrist for bipolar disorder in Delhi. If you or a loved one is grappling with bipolar disorder, reaching out to Dr. Gupta could be the first step towards achieving stability and improved mental health.
https://www.goravgupta.com/best-bipolar-disorder-psychiatrist-delhi-gurgaon/
0 notes
Text
Best Psychiatrist in Delhi: Dr. Gorav Gupta
Dr. Gorav Gupta stands out as one of the most esteemed psychiatrists in Delhi. With over two decades of experience, he has significantly impacted the field of mental health through his innovative treatments and compassionate care. Dr. Gupta's extensive education includes an MBBS from Maulana Azad Medical College and an MD from Lady Hardinge Medical College, both under Delhi University [[❞]](https://www.goravgupta.com/about-us/) [[❞]](https://www.goravgupta.com/psychiatrist-in-delhi/).### Professional Achievements and ContributionsDr. Gupta's contributions to psychiatry are extensive. He is the President of the Mental Research Society and an active member of several professional bodies, including the Indian Psychiatric Society and the Indian Association of Private Psychiatry. He has also been an advisor to the Government of India for the Mental Health Care Act of 2017 and is a member of the Central Mental Health Committee [[❞]](https://www.goravgupta.com/psychiatrist-in-delhi/) [[❞]](https://www.goravgupta.com/blog/start-your-recovery-journey-with-the-best-psychiatrist-in-delhi/).### Tulasi Psychiatry and Rehabilitation CentreDr. Gupta is the driving force behind the Tulasi Psychiatry and Rehabilitation Centre, a premier facility offering comprehensive mental health services. The center, which includes a 100-bed facility for acute care and a 50-bed halfway home, provides specialized treatment for various psychiatric conditions such as schizophrenia, bipolar disorder, and substance abuse [[❞]](https://www.goravgupta.com/about-us/) [[❞]](https://www.goravgupta.com/psychiatrist-in-delhi/).### Innovative Treatment ApproachesDr. Gupta is renowned for pioneering new treatments in psychosocial rehabilitation. In 2023, he established India's first Neuromodulation lab, offering advanced therapies such as Deep Transcranial Magnetic Stimulation (dTMS), Virtual Reality exposure therapy, Biofeedback therapy, and Ketamine therapy [[❞]](https://www.goravgupta.com/about-us/) [[❞]](https://www.goravgupta.com/psychiatrist-in-delhi/).### Community Involvement and OutreachBeyond his clinical work, Dr. Gupta is deeply involved in community service. He conducts free OPD services and mental health camps for the underprivileged. His initiatives include outreach programs where psychologists and nursing staff visit patients' homes to monitor progress and provide support [[❞]](https://www.goravgupta.com/about-us/).### Comprehensive Care PhilosophyDr. Gupta's approach to mental health is holistic, combining pharmacological treatments with psychosocial therapies. His treatment modules emphasize patient education, family involvement, and the use of therapies like Cognitive Behavioral Therapy (CBT) and mindfulness practices. This comprehensive approach ensures that patients receive well-rounded care tailored to their individual needs [[❞]](https://www.goravgupta.com/psychiatrist-in-delhi/) [[❞]](https://www.goravgupta.com/blog/start-your-recovery-journey-with-the-best-psychiatrist-in-delhi/).### Why Choose Dr. Gorav Gupta?Patients and peers highly regard Dr. Gupta for his clinical acumen, empathetic approach, and dedication to improving mental health care standards. His contributions to the field have earned him a reputation as one of the top psychiatrists in Delhi, making him a trusted choice for those seeking psychiatric care [[❞]](https://www.goravgupta.com/depression-psychiatrist-doctor-in-delhi-gurgaon/) [[❞]](https://www.goravgupta.com/blog/start-your-recovery-journey-with-the-best-psychiatrist-in-delhi/).For more information or to book an appointment with Dr. Gorav Gupta, visit his [official website](http://www.goravgupta.com) [[❞]](https://www.goravgupta.com/about-us/) [[❞]](https://www.goravgupta.com/psychiatrist-in-delhi/).
0 notes
Link
0 notes
Text
Best Clinic For Psychiatric, Endocrine & Sleep Disorder - MD TruCare
We offer a range of Psychiatry, TMS, ADHD & Spravato treatment services for people experiencing Mental Health problems. Call: 817-722-6078. Book an instant appointment with the best Psychiatrist in fort worth & grapevine TX at MD Trucare.

1 note
·
View note
Text
sex therapy
Can you find sex advice online? Yes, but be sure to check out a site as carefully as you would a therapist.
Jenny Peters (not her real name) was having difficulty with physical intimacy and pain during sex, but was too embarrassed to bring it up with her doctor.
Instead, she found a free Internet site where the doctor posted her question and, in his answer, suggested she get in-person therapy.
"The Internet got me on the right path," she says. "I wasn't scared to talk about it anymore. I went to my doctor and found out I had a bladder infection. She also put me on a long-term therapy program with my partner to become more comfortable with physical intimacy."
While the cast of television's "Sex and the City" discuss a myriad of sexual quandaries with ease, in real life, most people -- like Peters-- will stammer through questions about such topics as pain during sex or masturbation. In fact, embarrassment can be the biggest obstacle between a sexual problem and help.
That's where online sex experts can help, says Deborah Fox, MSW, a Washington, D.C., sex therapist with her own web site. "The Internet is useful for addressing sexual problems because people are able to ask questions that [otherwise] make them feel uncomfortable."
Online Roles and Limitations
Fox and other sex therapists offer their expertise online, providing educated responses to a variety of questions. They're quick to point out that this does not, however, qualify as therapy. At "Ask the Sex Doc," for example, William Fitzgerald, PhD, a sex therapist in Santa Clara, Calif., posts his answers to hundreds of questions, choosing the ones he feels are most universal.
Common questions easily answered online, according to Fitzgerald, include the effect of masturbation on sexual performance, the regaining of sex drive after the death of a spouse, and the way to approach a spouse about acting out a sexual fantasy. Some sites answer questions free of charge and post the answers for other users to see, while they may require a fee for answering questions privately.
Sandor Gardos, PhD, an online sex expert, also responds to questions on many sexual topics. But when a question is beyond the scope of what can be or should be answered online, Gardos is quick to suggest face-to-face professional help. He and other online sex therapists often recommend traditional therapy for issues that involve more complex problems, such as childhood sexual abuse. Fox adds that current technology simply doesn't allow for the equivalent of ongoing, in-person meetings necessary to resolve many sexual issues.
The Marriage of Therapy and Technology
Online sex therapy falls under the umbrella of "telemedicine," which also includes videoconferencing and telephone therapy.
Because telemedicine is in its infancy, the American Psychiatric Association and the American Psychological Association are still grappling with guidelines. Even so, both organizations emphasize that therapists who are online must adhere to ethics standards already in place.
William Stone, MD, who is on the American Psychiatric Association's Committee on Telemedicine, says the new technology is a mixed blessing. Although it is starting to bring therapy to people in remote locations, it also has limitations and potential dangers. For instance, doctors can usually prescribe drugs only in states where they are licensed to practice medicine, making it difficult to treat patients signing on from other states. And the images transmitted during videoconferences don't always allow detection of subtle changes in body language or expression that are often helpful in making a diagnosis during face-to-face meetings.
How to Judge the Sites
A reputable sex therapy site should have a disclaimer saying that the content and interactions do not constitute therapy or medical treatment, says Mitch Tepper, PhD, MPH, who has been researching online sex therapy sites for more than five years and launched his own in 1996.
Tepper also suggests checking sites to see if the therapists are certified by the American Association of Sex Educators, Counselors, and Therapists (AASECT) or belong to other organizations such as the American Psychological Association or the American Psychiatric Association. Ask therapists where they were trained and how many years they have been in practice (or look on the site for background information on them), as well as how long they have been online.
By doing a bit of research on the therapist and the site, you will be more likely to find someone who is credible and competent.
0 notes