#chronic pain treatment guidelines
Text
Eating For Optimal Health - Total Review Info
In the quest for a healthier lifestyle, one of the fundamental pillars is nutrition. What we eat plays a pivotal role in shaping our overall well-being. In this comprehensive review, we will delve into the key principles of eating for optimal health, exploring the latest insights and timeless wisdom that guide us toward a balanced and nourishing diet.
The Foundation of a Nutrient-Rich Diet
At the core of optimal health lies a nutrient-dense diet. This involves choosing foods that are rich in essential nutrients like vitamins, minerals, and antioxidants. Fruits, vegetables, whole grains, lean proteins, and healthy fats should form the cornerstone of your meals. These foods provide the body with the building blocks it needs for various functions, from cell repair to immune system support.
Balancing Macronutrients for Energy and Satiety
Macronutrients—carbohydrates, proteins, and fats—constitute the primary sources of energy for the body. Achieving the right balance among them is crucial. Carbohydrates provide quick energy, proteins support muscle development and repair, and fats are essential for nutrient absorption and brain health. A balanced intake of these macronutrients helps regulate blood sugar levels, promote satiety, and maintain overall energy balance.
Mindful Eating for Improved Digestion
Eating isn't just about the food we consume; it's also about how we eat. Mindful eating emphasizes being fully present during meals, savoring each bite, and paying attention to hunger and fullness cues. This practice can lead to better digestion, as it allows the body to properly break down and absorb nutrients. Moreover, mindful eating promotes a healthier relationship with food, reducing the likelihood of overeating and fostering a greater appreciation for the nourishment food provides.
The Role of Hydration in Optimal Health
Water is an often underestimated yet crucial component of optimal health. Staying hydrated is essential for various bodily functions, including nutrient transport, temperature regulation, and detoxification. Adequate hydration supports the health of the skin, joints, and organs. As a general guideline, aiming for eight glasses (64 ounces) of water per day is a good starting point, but individual needs may vary based on factors such as climate, activity level, and overall health.
Understanding Food Sensitivities and Allergies
Optimal health requires paying attention to how your body responds to different foods. Food sensitivities and allergies can manifest in various ways, from digestive issues to skin problems. Identifying and eliminating trigger foods can lead to significant improvements in overall well-being. Keeping a food diary and seeking professional guidance can help pinpoint potential sensitivities and create a personalized nutrition plan.
The Impact of Processed Foods on Health
In the modern era, processed foods have become a prevalent part of many diets. However, their convenience often comes at the cost of nutritional value. Processed foods are typically high in added sugars, unhealthy fats, and artificial additives, contributing to various health issues such as obesity, diabetes, and cardiovascular disease. Minimizing the intake of processed foods and focusing on whole, unprocessed options is a key step toward optimal health.
The Benefits of Functional Foods and Superfoods
Functional foods and superfoods are nutrient-rich powerhouses that offer additional health benefits beyond basic nutrition. Examples include berries, leafy greens, and fatty fish. These foods are rich in antioxidants, anti-inflammatory compounds, and other bioactive substances that support various aspects of health, from cognitive function to heart health. Incorporating a variety of these foods into your diet can enhance overall well-being.
Customizing Your Diet for Individual Needs
While general guidelines provide a solid foundation, it's essential to recognize that individual nutritional needs vary. Factors such as age, gender, activity level, and underlying health conditions influence dietary requirements. Consulting with a registered dietitian or healthcare professional can help tailor a nutrition plan that aligns with your unique needs and goals.
Conclusion
Eating For Optimal Health is a multifaceted journey that goes beyond mere calorie counting. It involves embracing a holistic approach that considers the quality of food, mindful eating practices, hydration, and individualized needs. By prioritizing nutrient-dense foods, staying mindful of portion sizes, and being attuned to your body's signals, you can pave the way to a healthier and more vibrant life. Remember, the choices you make in the kitchen have a profound impact on your overall well-being, making each meal an opportunity to invest in your health.
#total review info#eating for optimal health#managing chronic pain#resistance exercise bands#well being ideas#across the spiderverse#chronic pain treatment guidelines#Well Being Ideas
0 notes
Text
Had a horrible nightmare and I am now sitting here absolutely seething with rage surrounding the NHS and especially the Mental Health Act and I don’t know what to do with this rage. I just want to combust/evaporate and not be on this horrible planet anymore.
#personal#thoughts#anger#trauma?#does it count as trauma#nhs#nhs nightmare#mental health#chronic pain#section#section 3#mental health act#all the pain killers I was made to take and tried to protest against were against nice guidelines for chronic pain#and I was told to just not think about being in pain and I should focus on being productive instead#like I didn’t wish I could do that#like I haven’t been trying to#I won’t go into the psychiatric treatment
4 notes
·
View notes
Text
The class I'm taking right now is on CBT and it is....conflicting.
On the one hand, I've successfully used CBT to understand maladaptive coping techniques, pinpoint the underlying beliefs and build new strategies. Very effective, very positive experience.
On the other hand, CBT has been used to gaslight, shame, and manipulate those with chronic illness and chronic pain, and for ME/CFS specifically, continues to cause real harm.
CBT techniques can be helpful for people to cope with, adapt to, and manage symptoms, but it is not a treatment - it does not make someone who is physically unhealthy physically well.
I have not disclosed my health status in this class, because I feel less safe doing that than I have in other classes - especially since the text is from the UK and includes mention of the NICE guidelines that recommend CBT for ME/CFS.
Ugh
#this is my life#chronic illness#me/cfs#back to school adventures pt.2#I have my guard up around this topic#two more weeks and this class is over
39 notes
·
View notes
Text
If this is such a free fucking country, why the fuck can't we apply informed consent to more things? Why the fuck do I have to beg a doctor and convince him I'm not insane just to get a medication that has a chance at helping me?
Like. I have PCOS. Spironolactone is prescribed for PCOS symptoms caused by androgens, like hair loss, hirsutism, and acne. I have PCOS and I have those symptoms. So why the fuck do I have to debate my doctor into offering it because "Oh but have you tried to lose weight? Here's nutrition guidelines, ask me again in a few months."
Like yeah. Medications have fucking risks. The estrogen in my fucking birth control puts me at a higher risk of stroke and raises my blood pressure, but going on the med that can balance my hormones and lower my blood pressure? Oooooh we gotta think about that.
And what about diagnostic shit too! Not even just medicines! Like yeah I get that you can't give an exploratory major surgery every time someone fucking asks, but why the hell can't I just walk up and just ask for an MRI scan? Or an x-ray? Fucking ultrasound? We gotta have daddy doctor's permission just to CHECK?
And what about fucking CPAP machines? My partner has sleep apnea and it's horrific to learn. You basically have to pay out of pocket for the fucking things even with insurance, but YOU HAVE TO GET A PRESCRIPTION. Okay listen. No one is going to be fucking harmed if they use a machine to help them breathe better at night, even if they don't need it like what the fuck is it gonna do that's a problem?
The claim there is "Oh but you want to be sure you get the right one because some people need extra features" and all I can think is like. Is it BETTER for someone with sleep apnea to have NOTHING AT ALL? That's like denying someone a basic rescue inhaler when there's a formulation that works better, like maybe it's best they DON'T choke.
I just. Idk. I'm not anti medical or anti science. I'm just fucking chronically ill and tired, and there's no help out there. I'm tired of having to deal with doctors making decisions that involve leaving me to suffer when I can't do anything about it.
Like. The main barrier to treatment for my longest term condition is a fucking diagnostic test. I have a muscle condition that makes it impossible for me as is, and physical therapy confirmed it was likely worsened by the pain and inflammation, and the muscle work alone wouldn't fix it.
And they could accommodate me. I've met so many people shocked that they won't, because they were accommodated. A muscle relaxer, a xanax, topical numbing, laughing gas, even putting me under are all options that others in my position have been offered. And I get denied any of those options because "it's not standard" and "you need to suck it up" over involuntary muscle spasms...
I don't care about fucking risks anymore, because is it really any less of a risk to live in pain, feel my body weaken from fatigue and dysfunction, all while there's something in my body actively causing harm to me and I have no way of even knowing how far it's spread, how serious it is, if it's harming my internal organs, anything...
Why the fuck can't I just sign a form saying I understand all the risks and then just ask for what I fucking need? I don't want to sound like I have a big head, but I've never been wrong about this shit. Every fucking issue or problem I spent years trying to convince doctors to listen and look into my concerns, and consistently when they eventually finally do, I turn out to be right. I hate it.
46 notes
·
View notes
Text
Do pain patients on long-term opioid therapy make irrational decisions? Is their mental capacity so diminished by opioids that they shouldn’t be involved in treatment decisions with their doctors?
The answer to both questions is often yes, according to a controversial new op/ed published in JAMA Internal Medicine. At issue is a recent update to the CDC’s opioid prescribing guideline, which calls for shared decision-making (SDM) when a prescriber considers tapering a patient or abruptly discontinuing their opioid treatment. The guideline was revised last year after reports of “serious harm” to patients caused by forced tapering.
“In situations where benefits and risks of continuing opioids are considered to be close, shared decision-making with patients is particularly important,” the 2022 guideline states.
But that advice about consulting with patients goes too far, according to the lead author of the JAMA op/ed, Mark Sullivan, MD, a professor of psychiatry at the University of Washington and a longtime board member of Physicians for Responsible Opioid Prescribing
“The value of SDM has been recognized for many years but also has its limitations, including where patients make irrational or short-sighted decisions,” Sullivan wrote. “Long-term opioid therapy induces a state of opioid dependence that compromises patients’ decisional capacity, specifically altering their perception of the value and necessity of the therapy; and although patients with chronic pain are not usually at imminent risk of death, they often can see no possibility of a satisfying life without a significant and immediate reduction in their pain.”
Sullivan and his two co-authors, Jeffrey Linder, MD, and Jason Doctor, PhD, have long been critical of opioid prescribing practices in the U.S. In their conflict of interest statements, Sullivan and Doctor disclose that they have worked for law firms involved in opioid litigation, a lucrative sideline for several PROP members...
...“In the case of opioid prescribing, and especially opioid tapering, working to persuade the patient is almost always the best clinical strategy. But there are circumstances (opioid use disorder, diversion, serious medical risks) where tapering should occur even if the patient objects,” Sullivan wrote.
Opioid diversion by patients is actually rare. The DEA estimates that less than one percent of oxycodone (0.3%) and hydrocodone (0.42%) will be used by someone they were not intended for.
As for patients on opioids behaving “irrational,” Sullivan and his co-authors cite an op/ed published 33 years ago in The New England Journal of Medicine (NEJM). But that article doesn’t even discuss opioids or tapering, it’s about whether patients and doctors should collaborate in making decisions about end-of-life medical care. It also makes an important disclaimer that “even the irrational choices of a competent patient must be respected if the patient cannot be persuaded to change them."
Sullivan rejects that approach to opioid treatment...
...In a rebuttal to Sullivan’s op/ed also published in JAMA Internal Medicine, Mitchell Katz, MD, and Deborah Grady, MD, disputed the notion that a patient’s choices shouldn’t be respected.
“Primary care professionals generally highly value the inclusion of the patient’s perspective in decision-making, consistent with the principles of patient autonomy and self-determination, and are loathe to go against a patient’s wishes,” they wrote.
“As primary care professionals, we have found it helpful to tell patients that it is not recommended to take more than a specific threshold of opioids and that we do not want to prescribe something that is not recommended. However, that does not mean sticking to rigid cut points for dose and duration of opioid use, abandoning patients, or having them undergo too rapid a taper.”
Others questioned JAMA’s decision to publish Sullivan’s op/ed.
“While I recognize the editors’ legitimate intellectual interest in providing a forum for open discussion on the opioid policy space, I question their decision to publish an editorial that represents an ongoing call for broad, ill-defined reductions in opioid prescribing,” said Chad Kollas, MD, a palliative care specialist who rejects the idea that patients shouldn’t be involved in their healthcare choices.
“Errantly embracing a lower evidentiary standard for medical decision-making capacity creates an unacceptable risk for harm to patients with pain by violating their rights of medical autonomy and self-determination.” (Full article at link)
So essentially a man with a bias against opioids and who makes money litigating against uses a 33 year old op ed to assert pain patients shouldn't have a say in their medical care because we irrational. Proof of that irrationality is that if we have to deal with severe chronic pain with no relief, we may contemplate suicide. So fucking irrational, right? 🤬
This man is fucking cruel and inhumane. He works for an organization (PROP) that has had direct influence on the 2016 CDC Opioid Guidelines which lead to many pain patients committing suicide or dying from complications due to forced tapering and withdrawals. And this man has been given a platform to assert that our desire to not exist in severe daily pain is irrational. Fuck him!
#disability#chronic pain#ableism#opioids#chronic illness#medical bias#suicide cw#forced tapering#spoonies#PROP#cdc guidelines#article
27 notes
·
View notes
Text
I'd love to share with you all my undergrad honors thesis! Warning, it's a long read but well worth it, especially if you're into harm reduction
Why do Chronic Pain Patients Use Opioids Outside of the Realm of Prescription?
December 21, 2022
Nadiya
With the guidance of mentors David Frank, PhD and Noa Krawczyk, PhD
Macaulay Honors College Public Health Honors Project
AbstractThis exploratory review aims to summarize the reasons why chronic pain patients have been using opioids not as prescribed. Review and analysis of Reddit posts revealed people’s reasons for not using drugs as prescribed, and yielded meaningful anecdotes about their stories. Results showed four overall themes, with one theme being patients not getting enough supply, either through underprescription, no prescription, or getting cut off prescriptions; one theme being issues with withdrawal, often linked to lack of information or various reasons for patients to DIY the process; one theme being blocked communication between doctors and patients, specifically focusing on stigma in the medical community against drug users; and the last theme focusing on the negative effect of national, state, and practice-based prescription guidelines. These can be summarized by one overarching theme of disconnect between patients and doctors. Recommendations can be made to improve guidelines and to train doctors better.
Background/Introduction/LiteratureThe use of opium as an analgesic can be traced back to the times of ancient Sumer, with references to it written on a clay tablet of medical preparations (Norn et al., 2005). Since then, opium and increasingly stronger opioids, including synthetic opioids, have been used in a widespread manner, primarily for pain management and for recreational use, as opioid euphoric properties hold similar levels of power as analgesic properties (Norn et al., 2005). Although there had been previous opioid “epidemics” such as the high level of Opioid Use Disorder following the Civil War, the most currently thought of opioid “epidemic” is the one that occurred in the late 1990s and early 2000s, whose dangerous aftereffects we are seeing today with the advent of fentanyl (Jones et al., 2018). A perfect storm of the medical institution starting to briefly acknowledge the importance of pain and the invention and widespread marketing of preparations like OxyContin, as well as the willingness of many physicians to prescribe of opioids, caused an increase in the rates of opioid use, unfortunately leading to dependence and overdose in some cases (Jones et al., 2018). These negative consequences caused a shift in the pendulum in the complete other direction, with more crackdown on prescribing doctors, crackdown on users, and low rates of prescription of opioids (Marchetti et al., 2020). By now, the CDC has put out federal guidelines about opioid prescription for doctors (2016 guidelines dealt with how much opioids can be prescribed and what risk factors can be considered in prescription) (Bohnert et al., 2018). Furthermore, states have set up their own guidelines to try to curb causing dependence (Soelberg et al., 2017). Also, private healthcare companies often have blanket rules or limits that either they won’t prescribe opioids or no more than a limited dose of opioids (Webster & Grabois, 2015). In theory this was to cut down on pill mills, where anyone could claim any injury for a prescription they could get multiple refills of (Kennedy-Hendricks et al., 2016).When reading this paper, it is important to note the different kinds of opioids mentioned.OxyContin, Norco, Lortab, and tramadol are all available by prescription but also on the street; in the US, heroin is only available on the street. Methadone and suboxone are forms of medication-assisted treatment (MAT); suboxone, which was mentioned more often in this research, is a partial opioid agonist which also often includes naloxone, an antagonist, in its preparation to block users from getting high on other opioids (Velander, 2018). Although mostly obtained via prescription, suboxone can be acquired on the street (Hswen et al., 2020). Kratom is a plant with opioid characteristics that while still often used for pain or euphoria, is most frequently associated with assisting with withdrawal symptoms or tapering off stronger opioids (Eastlack et al., 2020). It is not legal in all states or countries, but where it is legal, it is typically sold in headshops or online; it is never prescribed (Prozialeck et al., 2020).Another important concept that received several mentions in patient posts was withdrawal, which requires explanation. After some level of dependence, an opioid user will start developing withdrawal symptoms when they stop using (Kosten & Baxter, 2019). These will worsen over the duration of use (Kosten & Baxter, 2019). Symptoms include an agitated/anxious mental state, insomnia, sweats, chills, flu-like symptoms, cramps, diarrhea, nausea, and vomiting (Kosten & Baxter, 2019).
MethodologyIn this exploratory review and analysis, Reddit posts were analyzed to answer the question of why current chronic pain patients use opioids in an illicit and/or non-prescribed way to manage pain. The social media forum Reddit, through its subreddit r/opiates, was used to sort through posts that might be of relevance. The search term used was “chronic pain.” Inclusion criteria used when considering posts for analysis incorporated posts consisting of at least 5 words in the body, and if there was repeat posting, only first posting in order of the algorithm was counted. Non-prescribed use had to be present or heavily implied in the content of the post. The project defined non-prescribed use as use beyond the scope of a prescription, encompassing everything from using drugs bought on the black market to doubling the dose of a prescription or using non-prescribed supplements. At this point, 50 posts that matched criteria were collected.The posts were coded on Google Sheets using the following list of categories, which were picked after thematic analysis of the topic.Can’t obtain a prescriptionAlready dependent from previous prescriptions or non-prescribed useWant more after prescription but can't getPrescription too lowRan out of prescription earlyRaised toleranceOff label use of prescriptionAre using for recreational reasonsDon’t want to go to a doctorCan't afford a doctor/doctor doesn't take insuranceReceived shared pills from othersWere already using pre-pain,Want the high from a stronger drugAvoidance of dopesickness/withdrawal symptomsUse vs suicideNo illicit use mentioned (still not using as prescribed)On medication-assisted treatmentUse of kratom,Different route of administrationRelief from dopesickness/withdrawal symptomsFear/avoidance of painUsing from non-prescribed supply on top of prescriptionUse of non-opiate drugs mentioned,Doctor lowered/took off scriptNew or worsening chronic pain after withdrawal/abstinence (post-acute withdrawal syndrome)Use of heroin.Each category was given a code and these codes were marked next to posts that pertained to them. Then important quotes were gathered and several themes were identified, some stemming from criteria, and some from analysis.Limitations include the fact that posters could use other terms than “chronic pain” to describe their pain, and the fact that posts were shown in the order of Reddit’s proprietary algorithm. Another limitation is the lack of inclusion of “should I” posts, or posters who haven't yet made the jump but are asking about using their prescriptions in a different way or trying new substances. Another limitation involves the fact that this study does not take into account the people who would not be using Reddit to talk about their experiences, including, notably, many elderly individuals who may be a part of the target demographic.
Results
Quantitative AnalysisOut of 50 data points, here’s how many were counted positive for each category:Category Count
Can’t obtain a prescription 13
Prescription too low 11
Use of heroin 10
Are using for recreational reasons 9
No illicit use mentioned (still not using as prescribed) 9
Using from non-prescribed supply on top of prescription 8
Different route of administration 7
Want more after prescription but can't get 7
Off label use of prescription 6
Use of kratom 6
Use of non-opiate drugs mentioned 5
Raised tolerance 5
On medication-assisted treatment 5
Relief from dopesickness/withdrawal symptoms 5
Ran out of prescription early 4
Fear/avoidance of pain 4
New or worsening chronic pain after withdrawal/abstinence (post-acute withdrawal syndrome) 4
Use vs suicide 3
Doctor lowered/took off script 3
Don’t want to go to a doctor 2
Received shared pills from others 2
Were already using pre-pain 2
Avoidance of dopesickness/withdrawal symptoms 2
Can't afford a doctor/doctor doesn't take insurance 1
Want the high from a stronger drug 1
Already dependent from previous prescriptions or nonprescribed use 0
Qualitative AnalysisAnalysis of the Reddit posts revealed four umbrella themes:1. Patients aren’t getting enough medication to manage pain.2. Patients are dealing with issues related to opioid withdrawal/dependence/tolerance.3. Patients are not consulting with their doctors about their opioid use.4. Guidelines for prescription of opioids are not serving patients well.
Umbrella Theme 1: Patients aren’t getting enough medication to manage pain.Multiple Reddit users found that although they were getting prescriptions, the prescriptions were insufficient to their levels of pain. Some patients feel their doctors aren’t understanding their pain, and are acting out of a fear of overprescription.One poster described their frustration at not being prescribed opioids.“and what got me so pissed off, was when I talked to one of the docs he was saying “we really don’t want to use any narcotics as they’re dangerous and we want to keep you safe, if you have excruciating pain, you can have a small dose of norco once a day.” ”Self-management of pain medication is a strategy many use to allow for their low prescriptions. Here, one patient described using dietary changes to make their dose have a higher effect, in this case using grapefruit juice to potentiate the effects of opioids. (Nieminen et al, 2020)“It's gotten so bad that I've begun to starve myself most of the day and drinking mostly grapefruit juice to have my limited dose hit as hard as possible.” Others, like the next two posters, stretch their limited prescription, finding themselves in a conflict to take multiple doses to alleviate pain versus risking having nothing left to deal with a potential flare-up.“Try to keep it in the 15 - 30mg range per day so I don't max out my script in one week.”“I hate that so far today, I've taken 75mgs of oxy [Oxycontin], yet my back is still screaming at me. I hate that I only have one 15mg pill left, and I'm trying so hard not to take it just yet.”Many users found themselves unable to take prescriptions at all: “cant get doctors to help me for shit have to self medicate.”In some of these cases it is clear that the patients have already sought extensive care but still can’t get a prescription.“There's so much scaremongering about doctors overperscribing (sic) opiates, but I'm out here with a super fucked up back (dont want to get into specifics but its gnarly) and the xrays and MRIS to prove it and i still can't find a doctor to prescribe me anything stronger than naproxen.”“I've had a torn miniscus (sic) tendon for the past 7-8 years and none of the doctors I've been to will do anything about it. Doctors refuse to send me to pain management, their excuse is that I don't need it. I've taken it upon myself to medicate with the only pills that seem to work for it. (Oxy, Lortab)” For at least one patient, only mild or highly improbable solutions have been given.“every single doctor I've been to just gives me shitty NSAIDs and tells me to exercise”In some cases, doctors are cutting patients off their medications. One patient has been told that there is no cure and is therefore scared of being cut off their meds.“I’ve been told this “is it” for me, as after 6 years of treatment/surgeries there’s nothing left to do but treat symptoms, and I’m terrified I’ll be cut off my meds this year, it’s terrifying…..”This patient’s story shows a direct link between being cut off and buying on the black market.“I was prescribed quite a bit of opioids but I was cut off because it was just a general doctor and I had to go to the streets which eventually led me to suboxone [an opioid partial agonist used for withdrawal]”
Umbrella Theme 2: Patients have issues with withdrawal/dependence/tolerance and the way interactions with doctors about these topics have gone.One patient was worried that trying to taper off legally with suboxone would affect other prescriptions, and was crowdsourcing information instead of telling the doctor their fears.“I’ve bought subutex [same as suboxone] before and managed to get myself off it but I can’t get it this time. Would a doctor allow you to be prescribed subs while your already on other opioids prescribed?”Another patient is trying to crowdsource answers to their problem; they started off using legal kratom, but it wasn’t enough for the pain.“Now i tried to just come off morphine and jump on to kratom but my habit is too big and the kratom wasn't holding me plus it wasn't really putting a dent in my pain. I'm so fkn lost, i really don't know what to do at this point this seems insurmountable and i've just been crying all day.”One person feels they made a mistake telling their doctor. There are steep costs associated with suboxone for them, and they consider heroin to be more pleasant and cheaper.“Doctors refuse to help me. Even with my medical history , I made a horrible mistake of going for help in my most desperate moments of withdrawal, tried to get on subs [suboxone, an opioid partial agonist used for withdrawal], But said fuck it when I realized they wanted $16 every single day to dispense me a sub [suboxone] strip 6 days a week with only 1 take home for sundays. My dope [heroin] habit I could maintain on for only a little more money and it felt way better so why the fck would I get on maintenance?”Two patients likely weren’t given enough information about withdrawal. Withdrawal is seen as a “junkie” thing, so doctors don’t want to give their patients the impression they’ll get it (or don’t know much about it themselves), and patients don’t think it will happen to them so they don’t research it. (Rieder, 2017)“Only today it dawned on me what an odd coincidence it is I feel sick when I don't take it but I'm fine when I do. I've been using it continuously for the past couple days and today I woke up feeling like complete shit.”“Now my tolerance is so high I haven’t been taking as directed and taking the max dose. I ran out almost 3 days ago now. I am so tired, my legs and my arms hurt if I don’t move them, have the shits [diarrhea], headache, and all over feeling terrible [typical opioid withdrawal symptoms]. I’m assuming this is withdrawal but I feel so fucking awful.”
Umbrella Theme 3: Patients are not consulting with doctors about pain and opioid use.Patients were often found to be deliberately withholding information from their doctors for various reasons:“Like I said I hid it from my doctors, so I never really got to find out exactly what that pain was”At least one patient was scared that doctors would think they were lying for a prescription.“I tried to hide it from everyone. I was scared that doctors would think I was phishing [committing fraud/lying] for pain pills, and/or that my family would doubt my sobriety because of my behavior.”Rehab facilities often don’t let patients take any psychoactive drugs, and this person was rightfully worried that if she entered rehab, her meds could be taken from her.“She says she can't go to treatment because they'll take her meds for her illness (she collects SSI for her disability) and they could fuck with that as well.”There are often lengthy processes associated with trying to get specialists that put people off.“I've been thinking of trying to get a referral by my regular doctor to the nearest chronic pain center, to see a specialist and psychiatrist for specific pain-related treatment. In this country the doc has to write up my medical history, explain the current condition in a referral letter, mail it to the pain specialist, and if he deems it legit he'll mail me a form to fill to evaluate my pain levels. Which I have to mail back to expect a call back about a first appointment. You can understand that this is so convoluted it doesn't even make me wanna do it.” Doctors are often wary if a patient asks for a specific opiate, thinking they are trying to commit fraud.“As of now I have been to two docs who pushed me aside giving me 800mg Tylenol, it didn't do shit but I remember I had gotten a script of trammadol (sic) for a root canal and it made everything painless and easy but as soon as I said that to the doctor he immediately wrote another 800mg Tylenol script without hesitation and sent me on my way.”Many patients were scared of being marked as addicts due to withdrawal symptoms, other prescriptions, or being honest about recreational drug use. “Doctors see the addict mark on my history and treat me like a piece of garbage.”One patient regrets honesty with their doctor, who won’t prescribe to a heavy drinker. Although alcohol and opioids are synergistic, this patient is still in a lot of pain. (Cushman, 1987)“I went to the doc my sister goes too (sic) and told him about my drinking habits and the pain, he told me he won't prescribe any opiates for "fear of additional addictions" occurring.”Here, the patient knows they are labeled dependent, so they are scared that the “addict mark” will not let them request extra of their prescription.“And when I go in for my next appointment, if I mention that the 10mg dose is preferable do you think I'll run into any trouble for suggesting that now that I have been labelled as dependent?”The patient feels they can’t be honest about illicit use without fear of being cut off from their meds.“If I go to my doctor and come clean that I’m using oxy’s {Oxycontin] and heroin will the (sic) blacklist me from the prescription I’m on?”This poster is worried that coming clean about their opioid usage will cause their psychiatrist to stop giving them benzodiazepines.“I have no intentions of telling my psychiatrist because knowing her, she'd most likely just take away my benzo [benzodiazepine] prescription away and think the problem is solved. I'm almost 100% if I tried telling anyone else I wouldn't get taken seriously either, just like with all my other both physical and mental health issues, and it's not that dangerous of a drug anyway. I don't want to make the situation even worse for myself, like it's always happened before when I mistakenly trusted people, despite it being their job to help me”This poster is worried that if suboxone is on their record, they will be blacklisted from future pain medication prescription and is wanting to try to self-medicate withdrawal with kratom instead.“I’m thinking about using kratom as a substitute for suboxone. I don’t want to take subs [suboxone] because 1. i don’t want my family to know 2. i don’t want that on my health record as i struggle with chronic pain and it would hinder some medical treatment for sure”In this case, a doctor’s beliefs about marijuana use are getting in the way of evidence-based care; the patient has essentially been cut off after admitting to marijuana use and exhibiting vague symptoms.“Now when it comes to my doctor. I feel like the stigma behind my marijuana use has greatly affected my care. He thinks I’m addicted to marijuana which is absolutely ridiculous. I’ve had panic attacks before in the hospital (I’ve dealt with anxiety far longer than I’ve been using marijuana) and he attributes them to “marijuana withdrawals” like wtf. And more recently he’s completely cut out any opiate use in my care. I’ve had multiple times where I have bad chest pain episodes and I need to go to the ER but the only thing they will give is toradol and Tylenol which does jack shit. This has forced me to start going to my local hospital ER whenever I have bad pain cause I know it can be treated there properly then I could be transferred to my normal hospital.”
Umbrella Theme 4: Guidelines for prescribing opioids aren’t serving patients.In this case, the patient is unsure but thinks state or healthcare company regulations are applying a rule that results in insufficient care.“Idk if doctors in California specifically at kaiser [Kaiser Permanente, a healthcare company] can even still prescribe monthly pain meds I don’t care about being high anymore I want this pain to end.”Here, a GP is prescribing an insufficient dose because of fear of crossing guidelines, which could impact their licensure.“My doctor (not pain management doc, normal GP) won't go over 50 MME [morphine milligram equivalents] a day because they're scared of the 2016 CDC Opioid guidelines bullshit.”Many practices have pain contracts, which require opioid-receiving patients to give their word to do certain things to keep getting their prescription (Payne et al., 2010). Here, a patient is scared that because they will have six less than needed if they didn’t use extra, at their next count they or their doctor will get penalized.“My doctor does pill counts now, the amount I’m supposed to be coming in with is 12 and if I’ll only be left with 6, am I gonna be fucked [low counts might look like abuse or dealing]? I’m not abusing them in any way, and I’m scared that I’ll look like I am and fuck up my prescription or get my doctors narcotic license taken away or something. I’ve only failed one drug screening when I wasn’t taking my medication because (TMI sorry) I hadn’t shit in a week.”
Discussion In analysis of these posts, the most common overarching theme was patients feeling disconnected from doctors, from not being able to convey their level of pain and having it met, to being prescribed medications they don’t understand, to not sharing issues with their doctors for fear of judgment or non-prescription.. All four themes — insufficient prescription, withdrawal issues, patients not consulting with doctors, and prescription guidelines — often come down to issues with the medical institution or individual doctors. However, this is such a widespread problem among individual doctors that change must be made on the systemic level, for instance, during education.Insufficient prescription stories in the data can be narrowed down to three categories: patients with prescriptions who experience more pain than their prescription can help, patients who cannot obtain a prescription for opioids, and patients who are cut off from their prescriptions. In all of these sub-categories, there is a common theme of frustration with doctors not meeting patient needs. There is also a theme in the already-prescribed sub-category of using other strategies to make a prescription have more power, some of which are risky. Using other substances to potentiate the drugs, especially benzodiazepines and alcohol, can lead to overdose, and doubling up on doses to then run out can lead to a cycle of withdrawal (Knopf, 2020). In the never-prescribed subcategory, it is becoming clear that many patients who are seeking extensive medical attention are not getting the medications they need. In the cut-off category, getting cut off or tapered down without permission can precipitate withdrawal. In all, this umbrella category shows a pattern of denial of a patient’s agency in their own pain management process, and doctors should find better ways to monitor people’s pain and not assume the least effective methods will do the trick.Multiple issues come up with withdrawal precipitated by running out of opioids and self-precipitated withdrawal due to the desire to taper off. For instance, it is hard to obtain suboxone and when people do, it can be quite expensive (Hswen, 2020). Kratom can also run quite expensive, and oftentimes does not treat withdrawal symptoms effectively (Eastlack et al., 2020). In a lot of cases, patients aren’t able to utilize detox programs because they would have to be free from opiates, but either doctors aren’t providing helpful ways to get patients off opioids, or patients don’t feel comfortable approaching the subject with their doctors (Timko et al., 2016). Additionally, many patients are not adequately educated on withdrawal; it can take a while for them to catch on to the fact that they don’t have a nasty flu, they are instead in withdrawal from the prescribed opiates they take (Kearney et al., 2018). This would imply that in long-term opiate prescriptions, doctors need to do a better job of describing the near-inevitability of withdrawal, the signs and symptoms, and when to seek help.Patients are also often scared to seek help from their doctors, often preferring to seek answers from nonprofessionals on sites such as Reddit instead. There is fear that doctors would think they are lying. This is especially true when patients want to ask for a specific opiate, as this often makes doctors wary (Lagisetty et al., 2019). Instead, self-research about medications should be encouraged and not seen by doctors as grounds for a scam. Additionally, strict rehab policies and lengthy processes to get specialists are turning patients off (Mehrotra et al., 2011). The specialist issue is not unique to pain management, but should still be improved (Mehrotra et al., 2011). Rehabs or other drug treatment centers should also have less all-or-nothing, more harm-reduction centered approaches, especially ones that match the reasons why a person might be taking a specific drug.There is also a heavy stigma against drug users of all kinds in the medical profession (Ahern et al., 2007). Although it can be understood that a provider would be wary to prescribe an opioid to a self-disclosed drinker or benzodiazepine user, as these can cause dangerous combinations, there has to be some way to balance this. Otherwise, we have a system where patients lie to their doctors about their drug and alcohol use and therefore are not properly counseled and can succumb to these consequences. Doctors should take extra care if there is a Substance Use Disorder (SUD), but still prescribe, maybe with mandatory counseling, as more than anyone, people with SUDs can find these drugs on their own. In this system, posters are reporting lying so they won’t be cut off any prescriptions and even withdrawing by themselves so they are not marked as an addict by records.In the wake of the 2000s “opiate epidemic,” doctors were given more stringent prescription guidelines. In many cases, patients aren’t aware whether they are being affected, unless their doctors told them directly, but patients are aware that some great changes have been made, either from their past medical experiences or that of the people they know. Private practices have also instituted blanket rules against prescription, mandatory pain contracts, drug urinalysis, and pill counts, which can lead for one “slip-up” or double dose in a patient’s pain regimen to get them in trouble (Tobin et al., 2016). These policies should be reexamined as they are mostly working just to deter and punish chronic pain patients (Tobin et al., 2016). State and federal guidelines also need to be loosened, as doctors should have more freedom over their prescription choices, making patients’ lives better.
Hope you like this and feel free to share!
#science#social science#research#public health#drugs#harm reduction#opioids#chronic pain#disability#cripple punk#sociology
20 notes
·
View notes
Text
Helicobacter Pylori
Spicing things up a bit with a Gram Negative Helical/spiral Bacteria
Epidemio:
up to 50% of the population worldwide, but even more in endemic countries/the 3rd world

it can cloud differentials, as it can be asymptomatic unless it caues peptic ulcer disease, in which case the infection may have been decades prior to detection - so you have to interpret serology with a grain of salt (it may not be the culprit of acute infection)
often picked up in early childhood and lingers without treatment for dcades
by contrast, 5% of children in the US have had it, so it may change your clinical decision making depending on where your patient grew up
In australian populations, up to 30% have it, but again, high frequency in older migrants, lower socioeconomic status etc.
Transmission:
faecal oral or even sexual (did not know that one)
increased risk:
lower socioeconomic status/growing up in a developed country
family history of infection and gastric cancer
What it does:
cause ulceration (peptic ulcer disease)
and inflammation or gastritis
due to it's helical shape and flagella, it can penetrate the mucosal lining
Trivia/History:
discovered by Australians in Western Australia in the 1980s
To quote the IM physician, Barry Marshall, in the face of skepticism that a bacteria could survive the stomach's acidic environment: "everyone was against me, but I knew I was right"
After failing to publish and some lab snaffus, he decided to do a Jonas Salk and swallow a broth of Hpylori himself. Of course this last experiment was published in an Australian journal.
At any rate, it is now widely accepted that Hpylori is linked to PUD and gastric cancer and by 2005, the two Australians who found the bacteria received the Nobel prize in medicine
we now know so much more about the pathogen with advancements in microbiology
they also came up with the urease breath test for it
Clinical presentation:
asymptoamtic
symptom onset occurs after gastritis and peptic ulcer disease develop: nausea, vomiting, dyspepsia, abdo pain, or at the extreme when the lining has eroded, bleeding/haematemesis
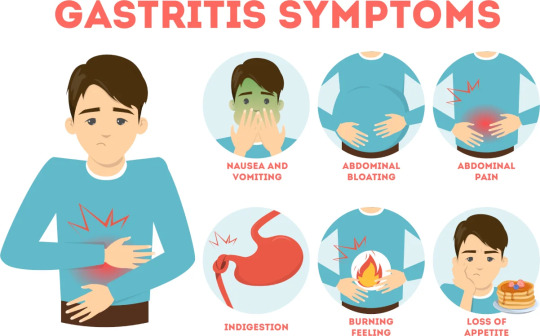
IMage source
Important differentials
coeliac's
Crohn's
nSAID induced gastritis
reflux
lactose intolerance
eosinophilic oesophagitis (sooo rare, usually a/w dysphagia)
Investigations
(all with relatively good/high sens and spec)
H pylori antigens in stool
serology (antibodies in serum, urine) --> usually IgG, hence can remain positive for years even post eradication
urease breath test
if a scope was involved due to PUD, then histopathology and culture (reduced sensitivity if treated with PPI in 2/52 prior or Abx 4/52 prior)
actually had no idea they breathed into little bags.

Treatment:
triple therapy - PPI, amoxicillin and clarithromycin for 14 days, in penicillin allergy replace amox with metro (increasing resistance is why metro is not first line in some countries - refer to local guidelines made based on local Abx resistance trends)
In patients younger than 50, it can be cost effective to treat if they have reflux on testing (if there's a high pretest probability - see increased risk groups) given the life time risk of PUD & gastric cancer, can also reduce risk of GIB
balance of risk/benefit: will it significantly improve QOL or will risks of ADRs outweigh the benefits (eg frail, elderly, multiple comorbidities)
when used in those with PUD - improves ulcer healing, recovery and prevents relapse
in simple ulcers, triple therapy is all that is required in more chronic complex ones --> 8/52 of PPI is also recommended to prevent recurring of bleeding etc.
not treating can lead to relapse and complications like bleeding/perforation/cancer risk
Complications
rarely, it can cause gastric adenocarcinoma as a known carcinogen
aka MALT lymphoma - mucosa-associated lymphoid tissue
this resolves with triple therapy (Usually)
consider it in family histories of gastric cancer
life time risk of gastric cancer at 2% and 15-20% risk of peptic ulcer disease
Wish the acronym wasn't MALT. But could be a good way to remember it. MALT, tasty, gastritis and Hpylori.

Follow-up
test for eradication 2 weeks post with stool antigen or urease breath test (serology less effective as the IgGs can remain positive for years) but that's on holding the PPI for 1/52 to prevent a false negative, some countries want both tests
in resistance or relapse there's salvage therapy, usually with bismuth or a quinolone.
Sources:
Wikipaedia - I havent covered pathophysio or it's cellular mechanisms and virulence factors, but there's a good overview in wiki
StatPearls (more paeds focused in this one)
CDC guidelines
Australian Therapeutic guidelines (Paywalll rest above are free)
5 notes
·
View notes
Note
i really hope this doesn’t come off as offensive in any way, but just. how? how on earth do people deal with chronic pain? i’ve had pelvic pain intermittently since 2019 and no doctor can figure out a reason why, it got worse after i stopped taking my psych meds and even worse after the onset of my eating disorder. today has been especially bad now that i’m hospitalized for my ED. i think it’s stress related because it gets worse when i’m anxious but doesn’t everything? i’m just so lost. how are people with chronic pain not terrified 24/7 of the state of their bodies? how can they trust doctors who just look at them and shrug? how do they live? how do they find joy in life, especially after knowing what it’s like to not live with pain? i’m asking because i’m genuinely so lost and thought you might know. i’m not looking for a diagnosis or anything i’m just looking for the “how.”
I am responding in regards to the pain, since I don't have experience with eating disorders.
To be perfectly honest: I went through the same desperation, the same fear, the same grief, and I still do at times when the pain is most intense. I started recovery out of spite, to not let all the bad things "win". But it became later on more about me than proving anything to anyone. I am really hopeful and this blog helps me be positive. There are days the pain is so bad I just want to quit, because I desperately want it to stop, but I know that taking it out on myself is not going to help me. Taking it out on your body is not going to help it. You need to take your medication and you need to keep focusing on your treatment, but do it for yourself, do it for your own relief because you desperately want it and you deserve it. You are worthy of relief, simplesmente, give it to yourself if you can, listen to what your body needs.
I think what saved was hope. And human connections. Reaching out to people is hard. Walking away from the ones who are harmful is hard too. But it is worth it.
I'm not talking about self-love because it's not that easy, right? I'm talking about not taking it out on your body. I'm talking about being neutral. What works for me is thinking that I'm at just another human with very human needs, that I am not exception to other humans when it comes to meeting my needs, like resting, or self-care.
Please, take your medication, it will help you at least figure out what works for you and what doesn't. Remember that diagnosis are important, but they are guidelines. At the end of the day, you are in pain, and that is what you need to care for, and working on allowing yourself to do so is important. You need to figure out what works for the pain, what your needs are, and that is the most basic thing to focus on. Helping yourself, accommodating your needs, not depriving yourself of medication, taking care of your body. It is not easy, it is slow, it is annoying sometimes, it takes time, it takes learning how to allow yourself to have what you deserve and what you need, but you can do it because I believe that reaching out to anyone is already trying. You are trying so hard, please don't forget that. You are trying and that matters. At the end of the day, you want relief. And that's what matters most for you to get, so keep reaching out to people, to doctors, to therapists, to those who listen without being ableist. Keep trying, it is worth it. You are worth it.
Just please remember that you need to focus on other things as well as the disease. Find things that bring you joy, those little things heal you a little every day, and it builds up. It makes you hopeful( it makes you positive, it gives you reasons to keep going. Sometimes when we are sick, the pain is all we have, and that is not fair to us. We deserve relief from the pain, but some of that relief comes from distracting ourselves from it by remembering it's not all there is in life.
Again, I am referring to chronic pain, because I don't have much experience with eating disorders.
21 notes
·
View notes
Text
Prescribed Security Glasses - Total Review Info
Explore the comprehensive review information on prescribed security glasses at Total Review Info. Our detailed analysis covers the latest trends, brands, and features of security glasses to help you make an informed decision. From lens technology to frame durability, we provide insights to ensure your safety and comfort. Stay protected with our expert reviews, comparisons, and recommendations, guiding you towards the perfect prescription security glasses for your needs. Trust Total Review Info for thorough evaluations and stay secure without compromising on style or functionality.
#managing chronic pain#resistance exercise bands#eating for optimal health#social media tools#well being ideas#chronic pain treatment guidelines#total review info#across the spiderverse#welcome home#succession
0 notes
Note
to that prior anon: what makes something a disability is how it impacts the life of the person who has it. for example, you use arthritis as an example of smth being "just a medical condition" but without medication that would cost more than $12k/month if I didn't have insurance, I am in constant pain and literally cannot walk or use my hands. my arthritis is disabling, while for others it's just constant low level pain and they may not consider it a disability.
please remember it's up to the person with the medical condition to determine if it disables them, and it varies person to person even with the same condition.
In their defense i think they were just asking a question because it is definitely like, a weird gray area? It honestly brings up a good discussion about, when do you you start calling something a disability, and how, I think, the broken health care system really, uh, falsely categorizes a lot of people based on what insurance is up to. Also different countries apparently have different guidelines, like for example my Canadian friend gets disability benefits literally just for being autistic despite being very "high functioning", putting that in quotes just because I know that can be kind of a controversial term.
But also, I'm so sorry you deal with that, I dont quite have arthritis but I can totally empathize wirh chronic physical pain 🥺 its actually horrifying reading the prices of some of these treatments sometimes and im really glad you have your medicine taken csre of. I often think about what would've happened to me if I hadn't been on state insurance when I was diagnosed with my equinus, I think it was literally like at least 5k per leg (i actually barely remember tbh, it couldve been higher or lower), which, I guess ultimately isn't a lot, but on my income and my moms income would have been so significant I would've felt actual guilt seeking treatment. Like, there was a legitimate possibility that the mere price could have kept me from... walking normally? And like my mom is 58 and she's been told she qualifies for knee replacements but she's literally scared of even getting them because of how long the recovery period can be and the financial loss and also just the price? So my mom could end up in legitimately worse health, although I guess that also has to do with like, America not having good workers rights where she could've taken off laid leave for surgery or something
It's that whole expression about "disability is defined by the environment" or something like that. Sort of like that whole controversy with Mr Beast where he paid for a bunch of people to get their sight or hearing back. Those people had treatable conditions and were stuck living in a way that negatively impacted their lives simply because they couldn't afford it? Like I can't even imagine not being able to use one of my five senses just because I couldn't afford it, but I know that's um already a reality for like, people who can't afford hearing aids and stuff like that
I think I'm starting to ramble here but like, I wish people had more sympathy for the disabled (and im talking about like society, not the last ask just to be clear, I feel like they were legitimately just curious). Like sometimes when you see people like violently hating the homeless, sometimes those people are literally people who got into horrible accidents or had some sort of injury and they wound up addicted to painkillers and had to turn to drugs when they can't afford prescription pain meds or those prescriptions get them addicted. I had a manager who was in a car accident and the painkillers made her eventually switch to straight up heroin. Even our disabled vets don't get good healthcare half the time
But yeah, as for me, I guess consider myself kind of straddling the line between disabled and able bodied, leaning more towards able bodied, but I can still have issues, like my knees are still kinda jacked up and even though i can stand and walk great now, stairs can be really tough sometimes, especially when I'm coming home from work and my body aches. and I still get pains in my back sometimes when I'm bending and leaning to the point I use a menthol roll-on gel for pain relief. Part of me kind of likes that I, I dunno, overcame the challenge and all that, but like, I think I would've preferred a body that didn't hurt lol 😅
#im kinda rambling lol im so like half awake rn#but yeah i hops you keep youe chin up despife the inconveniences of life
1 note
·
View note
Text
Exploring Medical-Grade Cannabis in Thailand: A Guide to Dispensaries and Regulations
As cannabis legalization spreads worldwide, Thailand has emerged as a key player in Southeast Asia’s cannabis scene. With the country’s progressive stance, the once-taboo topic of marijuana is now a flourishing industry, attracting both local and international attention. From medical-grade cannabis dispensaries to the growing interest in recreational use, Thailand’s cannabis journey has come a long way. This article delves into the current state of marijuana in Thailand, focusing on the role of cannabis dispensaries and the evolving landscape of weed in Thailand.
The Rise of Cannabis in Thailand
Thailand made headlines in 2018 when it became the first country in Southeast Asia to legalize medical marijuana. This landmark decision positioned the nation as a trailblazer in the region, opening doors to medical cannabis treatment for patients with chronic pain, nausea, and other conditions. Fast forward to 2022, and Thailand decriminalized cannabis entirely, allowing for broader use while maintaining a regulatory framework.
With the decriminalization of cannabis in Thailand, the market has expanded rapidly, catering to both medical and recreational users. Cannabis has become more accessible, with dispensaries popping up in major cities such as Bangkok, Chiang Mai, and Phuket. This has paved the way for medical-grade cannabis products, giving patients access to carefully cultivated strains that meet stringent health and safety standards.
What Is Medical-Grade Cannabis?
Medical-grade cannabis refers to cannabis strains specifically grown, harvested, and processed to meet high-quality standards for medicinal purposes. Unlike recreational cannabis, which focuses on providing a psychoactive high, medical-grade cannabis is developed to treat specific symptoms and conditions. This includes strains with precise concentrations of THC (the psychoactive compound in cannabis) and CBD (a non-psychoactive compound known for its therapeutic benefits).
Patients seeking relief from ailments such as chronic pain, anxiety, or epilepsy often turn to medical-grade cannabis for its ability to provide relief without the unpredictable effects of recreational strains. In Thailand, medical-grade cannabis can be found at medical-grade cannabis dispensaries licensed by the government to offer safe, high-quality products for both local patients and medical tourists.
Medical-Grade Cannabis Dispensaries in Thailand
Thailand’s cannabis market is still evolving, but medical-grade cannabis dispensaries are quickly becoming the cornerstone of the industry. These dispensaries adhere to strict guidelines to ensure that patients receive only the best, pharmaceutical-grade cannabis products.
At a medical grade cannabis dispensary, patients can consult with trained staff to select the most appropriate strain and dosage for their specific condition. Many dispensaries offer a wide variety of cannabis products, including oils, tinctures, edibles, and vaporizers, alongside traditional cannabis flowers. Some of the most reputable dispensaries also collaborate with healthcare professionals to provide guidance on cannabis use as part of a treatment plan.
One key advantage of these dispensaries is that they prioritize quality control. Medical-grade cannabis undergoes rigorous testing to ensure it is free from pesticides, mold, and other contaminants that could be harmful to patients. This focus on safety and efficacy makes these dispensaries the go-to choice for anyone seeking cannabis as a legitimate medical treatment in Thailand.
Understanding Marijuana and Weed in Thailand
The landscape for marijuana in Thailand has changed drastically over the past few years. Once illegal and harshly penalized, the government’s decriminalization has turned the country into a cannabis-friendly destination. Weed in Thailand is now widely available in dispensaries and shops, where tourists and locals alike can purchase various cannabis products.
However, it’s important to note that while cannabis use has been decriminalized, regulations remain. Public smoking is still frowned upon, and there are limits to the amount of cannabis one can possess. The government has made it clear that cannabis consumption should be done responsibly and in line with the legal framework.
The Future of Cannabis in Thailand
The future of cannabis in Thailand looks promising. With the growing number of medical-grade cannabis dispensaries and the increased acceptance of both medicinal and recreational marijuana, Thailand is poised to become a major player in the global cannabis industry. The government is also exploring ways to leverage cannabis for economic growth, particularly in the wellness tourism sector.
Many experts believe that marijuana in Thailand will soon become a significant driver of tourism, attracting visitors from all over the world seeking legal cannabis products. This shift could also lead to more research and development in cannabis-based treatments, offering new hope for patients with various medical conditions.
Conclusion
Thailand’s cannabis industry is on the rise, with medical-grade cannabis dispensaries playing a crucial role in providing safe, high-quality products to patients and consumers. As regulations continue to evolve, the availability of weed in Thailand will likely expand, making it easier than ever to access cannabis for both medicinal and recreational use. Whether you’re a local resident or a tourist, Thailand offers a unique and exciting opportunity to explore the world of cannabis responsibly.
With its pioneering stance in Southeast Asia, Thailand is well on its way to becoming a global hub for cannabis culture, offering everything from top-tier medical-grade cannabis to a welcoming environment for recreational users.
0 notes
Text
Why vaping medical cannabis works

Vaping medical cannabis is becoming a preferred method for many patients due to its quick effects and ease of use. It offers faster absorption of cannabinoids like THC and CBD, making it a more efficient option for those needing immediate relief. Unlike other methods, vaping ensures that cannabinoids bypass the digestive system, allowing for more rapid action.
For those who want to compare methods, vaping medical cannabis flower is often preferred because it preserves more of the cannabinoids and terpenes. Patients looking for condition-specific solutions, like those with ADHD, may find vaping medical cannabis flower a useful option. Additionally, some strains of weed for ADHD can offer targeted relief for ADHD symptoms, making vaping a versatile option.
Vaping is also seen as a cleaner alternative to smoking, as it avoids combustion and the toxins associated with it. Many patients appreciate that vaping provides immediate relief without the harmful side effects of smoking, making it a safer option for long-term use.
How vaping enhances cannabinoid absorption
Vaping allows cannabinoids to be absorbed directly into the bloodstream through the lungs, which means patients can feel the effects within minutes. This quick absorption makes vaping ideal for conditions that require rapid relief, like anxiety or severe pain. The efficiency of vaping compared to methods like edibles or oils is a major benefit.
When you vape, the bioavailability—or the amount of active cannabinoids that enter your system—is higher than other methods. This means more THC or CBD is absorbed, leading to a more potent effect. For patients managing chronic conditions, the ability to fine-tune dosage and feel the effects quickly is crucial for daily symptom management.
Another advantage of vaping is that it allows patients to manage their intake more precisely. Unlike edibles, where the effects can be delayed and harder to gauge, vaping gives near-instant feedback, helping patients adjust their dose as needed.
Why vaping is safer than smoking medical cannabis
Smoking cannabis involves combustion, which produces harmful chemicals and toxins that can irritate the lungs. Vaping, however, avoids combustion by heating the cannabis at a lower temperature, creating vapor instead of smoke. This makes vaping a much cleaner and healthier option for medical cannabis patients.
Vaping also preserves more of the cannabinoids and terpenes found in cannabis, which can degrade at higher temperatures during smoking. These compounds are essential for the plant’s therapeutic effects, and vaping ensures they remain intact, providing a fuller, more effective treatment.
Additionally, vaping allows for better control over the dosage. Because there’s no combustion, patients can more easily monitor how much they’re consuming, which is important for managing conditions like anxiety or chronic pain.
NHS vs. Releaf: Accessing medical cannabis for vaping
Accessing medical cannabis through the NHS can be a slow and difficult process. The guidelines are strict, and vaping products are not widely available, meaning patients often face long waiting times for treatment. Even for those who qualify, the options are limited and may not meet the needs of all patients.
Releaf offers a more patient-friendly approach. Unlike the NHS, Releaf provides quicker access to medical cannabis products, including those designed for vaping. This flexibility allows patients to start managing their symptoms sooner, without the delays and restrictions found in NHS pathways.
In addition, Releaf offers a broader range of vaping products, tailored to the specific needs of each patient. Whether someone needs a CBD-dominant strain for anxiety or a balanced THC-CBD option for pain relief, Releaf ensures that patients can find the right treatment to suit their condition.
Why Releaf is the best option for medical cannabis patients
Releaf stands out because of its personalised approach to medical cannabis treatment. Their team works closely with patients to determine the best strains and vaping products based on individual conditions and needs. This personalised care ensures that each patient gets the most effective treatment available.
Releaf offers a variety of vaping products, from fast-acting THC to more balanced CBD options. Their commitment to staying updated with the latest research and technology means patients always have access to cutting-edge treatment options. Releaf’s focus on quality care and tailored solutions makes it the best choice for patients seeking medical cannabis treatment.
Releaf also provides ongoing support, ensuring patients have all the guidance they need to manage their symptoms effectively. With their range of products and expert team, Releaf delivers an unmatched level of care for those relying on medical cannabis.
Benefits of vaping for specific medical conditions
Vaping is particularly beneficial for patients managing conditions that require immediate relief, such as chronic pain, anxiety, or PTSD. The fast absorption rate means that symptoms can be controlled quickly, which is essential for conditions that fluctuate or cause sudden discomfort. Patients often find that vaping helps them stay in control of their treatment.
For specific conditions like ADHD, vaping allows patients to manage symptoms like impulsivity or lack of focus with strains that target these issues. Vaping also makes it easier to adjust the dosage throughout the day, ensuring that relief is continuous. The flexibility and speed of vaping make it an ideal option for a variety of medical conditions.
Patients using medical cannabis to treat chronic conditions appreciate the consistency vaping offers. With the ability to control dosage and experience quick relief, it becomes easier to manage daily symptoms and improve overall quality of life.
Conclusion
Vaping medical cannabis is a fast, clean, and effective method of symptom relief. It offers quicker absorption than other methods and avoids the harmful effects of smoking.
With Releaf’s personalised care and extensive range of vaping products, patients have access to the best treatments available, ensuring they receive the relief they need in a timely and efficient manner.
Read the full article
0 notes
Text
Why Taping Techniques Are a Game-Changer in Modern Physiotherapy

Physiotherapy has come a long way in enhancing recovery and performance, and one of the most exciting advancements in recent years is the use of taping techniques. These innovative methods have transformed the way physiotherapists approach pain management, support, and rehabilitation. Let’s dive into why taping techniques are now a game-changer in modern physiotherapy.
What Are Taping Techniques?
Taping techniques involve applying specialized tapes to the skin to support muscles and joints. There are various types, including Kinesiology tape and Athletic tape. Understanding what are the uses of taping techniques can help you see why they’ve become a staple in both sports and clinical settings due to their effectiveness.
Benefits of Taping Techniques
1. Enhanced Pain Relief: Taping can significantly reduce pain by lifting the skin and reducing pressure on pain receptors. This simple yet effective method helps manage discomfort without relying solely on medication. Exploring taping techniques benefits can reveal how they offer targeted relief.
2. Improved Function and Mobility: By supporting muscles and joints, taping helps restore natural movement patterns and improves overall mobility. This is especially useful for those healing from accidents or living with chronic pain.
3. Support and Stability: Taping provides crucial support to injured or weakened areas, allowing individuals to move more freely while protecting vulnerable parts of the body from further strain.
4. Reduced Swelling: Taping techniques help manage inflammation and swelling by improving circulation and reducing fluid buildup in affected areas.
How Taping Techniques Work
Mechanics of Taping: The tape interacts with the skin and underlying tissues to support and stabilize the affected area. It works by creating a lifting effect on the skin, which alleviates pressure and improves blood flow.
Physiological Effects: Taping influences muscles and joints by enhancing their alignment and function. It also affects the skin, reducing pain and facilitating movement.
Application Methods: Different taping techniques are used based on specific needs. For example, Kinesiology tape is often used to support muscle function, while Athletic tape may be used to stabilize joints.
Applications in Modern Physiotherapy
Sports Injuries: Taping is a popular choice for athletes to prevent injuries and aid in recovery. It provides immediate support and allows for a quicker return to activity. If you’re looking for a physiotherapist in Oakleigh South, taping techniques can be an effective part of your treatment plan.
Rehabilitation: Physiotherapists use taping techniques as part of rehabilitation programs to support injured areas and improve the effectiveness of other therapeutic exercises. For personalized care, consider visiting the best physiotherapist in Clayton who can tailor taping techniques to your needs.
Preventative Care: Taping can also be used proactively to prevent injuries, particularly in high-risk activities or sports.
Advantages Over Traditional Methods
Comparison with Bracing and Immobilization: Unlike braces, taping offers flexibility and comfort, allowing for more natural movement while still providing support.
Cost and Accessibility: Taping is cost-effective and easy to apply, making it a practical choice for many patients and practitioners.
Practical Tips for Using Taping Techniques
Proper Application: Ensure you follow guidelines for effective taping to achieve the best results. Proper application is key to maximizing the benefits of taping techniques.
Choosing the Right Tape: Select the tape that best suits your needs, considering factors like the area of application and the type of support required.
Common Mistakes to Avoid: Avoid common errors such as applying the tape too tightly or using the wrong type of tape. Proper technique is essential for optimal results.
Conclusion
Taping techniques have revolutionized modern physiotherapy by offering a versatile and effective method for pain relief, support, and rehabilitation. As we continue to explore new advancements in physiotherapy, taping techniques will undoubtedly remain a valuable tool in helping individuals achieve better health and performance. Whether you’re an athlete or someone recovering from an injury, taping techniques can be a game-changer in your journey to recovery and wellness. For expert guidance, consider consulting with a physiotherapist in Oakleigh South or the best physiotherapist in Clayton to integrate these techniques into your treatment plan.
#physiotherapist in clayton#physiotherapy for neck pain clayton#sports injuries clayton#taping techniques in physiotherapy#Telehealth Physiotherapy
0 notes
Text
Ayurvedic Treatment for Lower Back Pain
Ayurvedic treatment for lower back pain focuses on restoring balance in the body through natural remedies, lifestyle changes, and holistic approaches rooted in ancient Indian medicine. According to Ayurveda, lower back pain, often linked to an imbalance in the Vata dosha, can be caused by factors such as poor diet, stress, improper posture, and lack of physical activity. Treatments typically include herbal remedies like dashmool, nirgundi, and guggul, which are known for their anti-inflammatory and pain-relieving properties. Additionally, oils like Mahanarayan oil and Ksheerabala oil are used in therapeutic massages to improve circulation, relax muscles, and reduce pain and stiffness in the lower back region.
In addition to herbal treatments, Ayurvedic therapies like Panchakarma—a detoxifying and rejuvenating treatment—are commonly recommended to address chronic lower back pain. This process includes therapies like Kati Basti, where warm medicated oil is applied to the lower back to nourish and soothe the muscles and nerves. Lifestyle modifications, including yoga, specific dietary guidelines to pacify Vata, and stress management techniques like meditation, are also integral to Ayurvedic treatment. These practices aim to address not just the symptoms but also the root causes of back pain, promoting long-term relief and overall well-being.
0 notes
Text
How Staying Hydrated Can Help with Back Pain in Woodbridge
Are you constantly battling back pain and live in Woodbridge? You might be surprised to learn that dehydration could be one of the culprits. At Health and Fitness Professionals, we believe in addressing wellness from all angles. In this blog post, we'll explore the connection between dehydration and back pain, providing you with tips and insights on how to alleviate discomfort through proper hydration.
Understanding Dehydration
Dehydration occurs when your body loses more fluids than it takes in, leading to a lack of water for essential bodily functions. Given that our bodies are approximately 60% water, this imbalance can wreak havoc on various systems, including your muscles and joints.
Symptoms of Dehydration
Common symptoms of dehydration include dry mouth, fatigue, dizziness, and dark-colored urine. However, chronic dehydration can also manifest in less obvious ways, such as persistent back pain.
Causes of Dehydration
Factors contributing to dehydration range from not drinking enough water, excessive sweating, and consuming diuretic drinks like coffee and alcohol. It's essential to identify these triggers to better manage your hydration levels.
The Link between Dehydration and Back Pain
You may wonder how dehydration could possibly cause back pain. The connection lies in the spinal discs, which are susceptible to dehydration.
Spinal Discs and Dehydration
Your spinal discs are cushion-like structures between the vertebrae, primarily composed of water. When dehydrated, these discs lose volume and flexibility, leading to increased stress on the spine and subsequent pain.
Muscle Cramps and Spasms
Dehydration doesn't just affect the spinal discs; it also impacts your muscles. Lack of water can lead to muscle cramps and spasms, which can exacerbate back pain and discomfort.
Reduced Joint Lubrication
Water is crucial for joint lubrication. When dehydrated, your joints can become stiff and less flexible, contributing to overall discomfort and pain in your back.
Signs That Your Back Pain Could Be Dehydration-Related
Not all back pain is caused by dehydration, but certain signs can indicate that you need to drink more fluids.
Morning Stiffness
If you wake up with a stiff, achy back that improves as the day progresses, dehydration could be a factor. Overnight, your body loses fluids, and if you don't replenish them, your back may suffer.
Persistent Pain despite Treatment
If you've tried various treatments like physical therapy, exercise, and medication without relief, considers evaluating your hydration habits. Sometimes, the solution is simpler than you think.
General Symptoms of Dehydration
In addition to back pain, experiencing other dehydration symptoms such as dry skin, headaches, and fatigue should prompt you to increase your water intake.
How to Stay Hydrated
Ensuring you drink enough water daily is crucial for both overall health and alleviating back pain. But how much water do you really need?
Daily Water Intake Recommendations
A general guideline is to drink at least eight 8-ounce glasses of water a day. However, individual needs can vary based on factors like activity level, climate, and overall health.
Water-Rich Foods
Incorporating water-rich foods like cucumbers, watermelon, and oranges into your diet can supplement your fluid intake and keep you hydrated.
Hydration Reminders
Use apps or set alarms to remind yourself to drink water throughout the day. Carrying a reusable water bottle can also help you stay on track.
When to Seek Professional Help
While increasing your water intake can help alleviate back pain, it's crucial to consult healthcare professionals for persistent or severe pain.
Physical Therapy Options
At Health and Fitness Professionals, we offer personalized physical therapy sessions to address both the symptoms and root causes of back pain.
Nutritional Counseling
Our experts can provide tailored advice on diet and hydration to ensure you're supporting your body adequately.
Medical Evaluation
Sometimes, back pain may have underlying causes that require medical intervention. If hydration and lifestyle changes don't bring relief, consulting a doctor is essential.
Dehydration and back pain Woodbridge are more closely linked than many realize. By ensuring you stay hydrated, you can alleviate some of the discomfort associated with back pain. At Health and Fitness Professionals in Woodbridge, we are committed to helping you achieve a pain-free, healthy lifestyle. Start by drinking more water today and notice the difference it makes for your back. For more personalized advice and treatment options, reach out to our team of professionals.
0 notes
Text
Expert Ear Surgery Treatment with Dr. Vishakha Gupta, ENT Specialist in Kota
Welcome to the clinic of Dr. Vishakha Gupta, a distinguished ENT specialist in Kota. If you’re dealing with ear issues that may require surgical intervention, Dr. Vishakha Gupta offers comprehensive care tailored to your needs. Ear surgery, or otologic surgery, is a specialized procedure aimed at addressing various conditions affecting the ear. Here’s an overview of how ear surgery is approached and what you can expect when you choose Dr. Vishakha Gupta for your treatment.

How to Approach Ear Surgery: Dr. Vishakha Gupta
1. Initial Consultation and Evaluation
Detailed Medical History: Understanding your symptoms, previous treatments, and overall health to determine the best course of action.
Comprehensive Examination: A physical examination of the ear, hearing tests, and, if necessary, imaging studies such as CT or MRI scans to assess the extent of the condition.
2. Developing a Personalized Treatment Plan
Pre-Surgical Preparation: Instructions on what to do before the surgery, including any dietary restrictions, medication adjustments, or pre-operative tests.
Procedure Explanation: Clear communication about the type of ear surgery required, the techniques that will be used, and what to expect during and after the procedure.
3. The Surgical Procedure
Tympanoplasty: Repair or reconstruction of the eardrum to restore hearing and prevent recurrent infections.
Myringoplasty: Surgical repair of a perforated eardrum to improve hearing and reduce the risk of chronic infections.
4. Post-Surgical Care and Recovery
Recovery is a critical phase of ear surgery, and Dr. Vishakha Gupta provides detailed instructions to ensure a smooth process:
Post-Operative Instructions: Guidelines on managing pain, caring for the surgical site, and monitoring for any potential complications.
Medications: Prescriptions for pain relief and infection prevention, along with clear directions on their use.
Why Choose Dr. Vishakha Gupta?
Expertise and Precision
Dr. Vishakha Gupta brings extensive expertise and precision to every best ear surgery Dr. Vishakha Gupta ENT specialist in Kota she performs, ensuring high-quality outcomes and minimal complications.
Advanced Techniques
Utilizing the latest surgical technologies and methods, Dr. Vishakha Gupta offers effective, minimally invasive treatments tailored to your specific needs.
Personalized Care
From the initial consultation through recovery, Dr. Vishakha Gupta patient-centered approach ensures that you receive individualized care, focusing on your comfort and overall well-being.
0 notes