#diabetes - diagnosis and treatment normally
Text

The Best Yoga Teacher Training Program With 40plus Healthy lifestyle
Let's say the person is looking for a wellness and health manual to help them make broad lifestyle and health improvements. the Health and Yoga Teacher Training Program's qualifications must then be verified. The person may ask any questions they may have concerning the training course. such as the length of the training course, the duration of the wellness coach's practise, and whether any outside body certified them.
#Yoga Teacher Training Program#diabetes - diagnosis and treatment normally#lifestyle diseases#art and music class#personality development classes
2 notes
·
View notes
Note
hey! so i hope this isn’t too creepy/nosey, but im a medical student and i was reading your possible fibromyalgia post and have a couple ideas lol. full important disclaimer that im only partly into my studies and im currently in the hypochondriac phase and also your summary was amazing but a real doc would ask way more questions, so please consult with an actual doc and take everything i say with a grain of salt! but like your symptoms aren’t nothing so i would def encourage finding a doc that you trust to do a proper exam and run some tests. also im operating under the assumption that you’re under 50 lol, bc if you’re over 50ish that’s a whole diff list of possible diagnoses.
so the thirst thing you’re talking about is often called polydipsia and is commonly associated with diabetes insipidus. that’s not the normal diabetes you think about, but happens when your body can’t regulate fluids in your body properly. id think of this if you’re also peeing a lot lol. your doc would have to do some kidney tests for that, which wouldn’t be part of the blood panel you mentioned. i’m a little skeptical that it’s hypokalemia bc that would’ve showed up on your blood test results. it could be transient electrolyte imbalances when you exercise so have one of those electrolyte packets when you exercise lol, bc it never hurts to try the easy solutions first, but chronic low potassium should’ve shown up? tho eating sweet potatoes has never hurt.
other things it could be is a lower motor neuron problem bc you mentioned twitches and muscle weakness which is typical for those. i def can’t say more without tests, but look into/get your doc to look into myasthenia gravis or LEMS and see if either of those fit. i think it’s possible bc these often also start with face/upper body symptoms, but would need way more questions/tests to know. it’s unlikely but could also be a glycogen storage disease called McArdle disease bc you describe a second wind thing when you exercise along with exercise intolerance. that’s super rare tho so it’s unlikely unless someone in your family has it/has similar symptoms.
also look into autoimmune stuff like rheumatoid arthritis, lupus, and sjögrens disease. i have way less useful info on that bc we haven’t gotten to it in class yet lol, but sjögrens looks promising bc you often get dry mouth with it, and it often goes along with rheumatoid arthritis which could explain the joint stuff possibly.
it’s also totally possible this is fibromyalgia, but i would be cautious diagnosing it bc it often comes with fatigue and cognitive stuff which you didn’t mention. it’s also more of a pain thing, and doesn’t include your twitches/dry mouth. it’s def possible, and it was def something i thought of when i saw your symptoms, but personally i would want to rule out other stuff first bc fibromyalgia is pretty vague and often a diagnosis of exclusion when other things don’t fit.
sorry for overwhelming you!! i just saw your post and was like hmmm those symptoms sound like Something. again take my advice with a big grain of salt, but i do really think it’s worth asking your doc about it and getting tests done, bc even if there aren’t cures there are def treatments to help with a bunch of this stuff. it doesn’t sound urgent, but at least from your post your symptoms don’t sound like run of the mill aches and pains. hope you figure stuff out!!
The problem with 'muscles don't work right ouchy and I am also tired' is that it's a symptom for Absolutely Everything That Can Be Wrong With The Body. Is it cancer? Is it a terrible diet and sleep schedule? Who knows!
The doctor ran a diabetes test with the blood panel and it came up negative, but I don't know if that checks for weird kinds of diabetes. (Diabetes does not run in my family until we get very old.) That test was memorable because I have stupid fragile veins that freak out and collapse at the mere sight of a needle so I had to get stabbed nine times, they didn't manage to get the middle reading at all, and in the end they resorted to just stabbing my thumb with one of those diabetes home blood test thingies and manually squeezing my blood out into a tube drop by drop.
I looked up polydipsia and I don't think I have that. I think I just prefer my mouth to be wetter than my salival glands want it to be. 🤷♀️I think most of my problems are probably not related to any rare chronic disease, but just run-of-the-mill autism making it hard to look after myself or properly notice and process my physical condition and adapt accordingly. I don't eat enough fresh foods because it's hard to plan with the very short timeframe to prepare and eat them in. I'm uncoordinated and damage my body a lot through overwork or using muscles incorrectly because autism makes it hard to keep track of those things. My mouth feels dry and my skin feels itchy and my muscles feel sore because that's what being autistic feels like. My sleep schedule is garbage because my executive function is garbage and even once I do manage to get myself into the bed I can't just "go to sleep", I pass out when I'm ready to pass out.
I'm not saying it's impossible for anything else to be going on, but I think the known factor is the simplest explanation here. It's 2:30pm and I've been putting off breakfast for five hours. Every time I go into the kitchen I get distracted by housework instead. I am very hungry. This is not behaviour that is conducive to a well-functioning body.
126 notes
·
View notes
Text
Terrible / Incorrect Things Cardiologists Have Told Me While Pursuing a Diagnosis For My POTS
For context I have been fainting since age 12 (2013). A full decade+ of a ton of disabling and quality of life-altering dysautonomia/postural orthostatic tachycardia syndrome (POTS) symptoms, and knowing this is the condition I have + self treating for the last 5 or so years. And I am still formally undiagnosed and untreated.
“You’re just dehydrated.” (many times)
“You’re just anemic.” (tests said otherwise and no treatment was given because he knew he was wrong but wouldn’t admit it)
“This is normal for girls your age. You’ll grow out of it.” (it was not normal and symptoms only got worse)
“Well it’s not seizures so you’ve got nothing to worry about.”
“You need to cut down on the sugar. Don’t drink juice. You’re probably becoming diabetic because of kids’ diets these days.” (meanwhile, on a low sugar diet because sugar really worsens some of my symptoms)
“You’re just fainting because you’re scared. You need to go to therapy to learn coping skills.” (scared of what? I was fainting in P.E.)
“Don’t drink Starbucks every morning and you’ll be fine.” (I’m literally caffeine-intolerant, I never drink coffee)
“You’re just deconditioned. Exercise and you’ll be cured.” (3x. always after I already explained that I overheat and faint from any exercise)
“There’s no reason for you to experience these things.” End of discussion.
“People with POTS don’t faint, so you can’t have it.” (not only blatantly wrong but what about all my other symptoms? ignored. didn’t offer further help/explanation)
“I don’t think you have POTS, but just keep doing what you’re doing because that seems to be helping.” (referring to the self treatment I do that’s specifically tailored for POTS)
“Come back to me after you’ve got some therapy.” (after I had a panic attack due to his malpractice that took me weeks to physically recover from)
“You meet the criteria, but I’m not going to diagnose you.” (2x)
“You’re not allowed to use a wheelchair, you don’t have any disabling conditions.” Notes orthostatic intolerance on visit report
“It’s just because you’re not eating enough.” (after I already explained I constantly overeat to maintain my weight, and purely based on me being thin and not my diet)
“Your heart rate is supposed to go up when you stand up. The tachycardia isn’t a problem.”
“I don’t think you have hEDS.. you don’t have the symptoms. And so POTS is out of the question.” (hadn’t discussed anything about my hEDS symptoms, not his place as a cardiologist to determine EDS, and you don’t need it to have POTS)
Feel free to reblog with what you’ve been told. These doctors are so arrogant, they drive me crazy 🙃
#disabled#disability#chronic illness#chronically ill#postural orthostatic tachycardia syndrome#potsie#pots#potsyndrome#dysautomnia#orthostatic intolerance#heds#hypermobile ehlers danlos#hypermobile eds#hypermobile ehlers danlos syndrome#ehlers danlos syndrome#spoonie
76 notes
·
View notes
Note
does/can type 1 diabetes exist in Time Lords/Gallifreyans? or would the technology be advanved enough to cure it?
Diabetes (Type 1 and 2)
In humans, diabetes is a condition characterised by issues with insulin production (Type 1) or insulin resistance (Type 2). For Gallifreyans, while their advanced biology provides some natural defences, they're not completely impervious and deal with a slightly different set of issues:
1️⃣Type 1 Diabetes in Gallifreyans
Manifestation and Symptoms:
In humans, Type 1 diabetes is characterised by the immune system declaring an unprovoked war on pancreatic beta cells, reducing or halting insulin production. For Gallifreyans, a similar autoimmune response could theoretically target cells or mechanisms involved in their glucose regulation - namely, X1 blood cells.
Given that X1 cells are responsible for transporting glucose, an autoimmune attack might disrupt this process, leading to irregular glucose levels despite their naturally higher baseline (8.9-11.7 mmol/L).
Symptoms might include a rollercoaster of energy levels and cognitive hiccups due to glucose imbalances.
Diagnosis and Management:
Gallifreyans would be born/loomed with Type 1 diabetes, possibly due to genetic predispositions or anomalies during the looming process.
Diagnosis would likely involve advanced biometric scanning and analysis of blood composition, focusing particularly on the functionality of X1 cells and their glucose transport capacity.
Treatments could involve cellular regeneration, genetic editing, or immunotherapy alongside your standard spacey-wacey machine™* to regulate glucose levels or cure it completely. And, of course, the simplest way to cure anything is regeneration, but it is probably a bit drastic and not a guaranteed fix if the condition is inherent in their genetic makeup.
2️⃣Type 2 Diabetes in Gallifreyans
Manifestation and Symptoms:
Type 2 diabetes, typically associated with insulin resistance, is far less common in Gallifreyans due to their efficient glucose management and general physiological Certificate of Excellence. This condition could develop at any time in a Gallifreyan's life, potentially due to lifestyle factors or physiological changes.
It might manifest as a reduced efficiency of X1 cells in glucose transport despite normal insulin production. Basically, the X1 cells have suddenly become slackers.
Symptoms could be subtler and might include reduced efficacy in their regenerative abilities and a slight decrease in overall vitality.
Also, because their homostatic mechanisms are so 'on-fleek', they'll start trying desperately to compensate, most notably in physiological cues, including dietary adjustments, increased exercise, stress management, and fluid intake adjustments.
Diagnosis and Management:
Preventive measures would likely be a key focus, with monitoring of individual health parameters to detect any early signs of insulin resistance.
Treatment could involve lifestyle interventions, although these might be more about fine-tuning. Additionally, advanced therapies to enhance X1 cell function or counteract insulin resistance at a cellular level could be employed. And you can always rely on your spacey-wacey machine™ for a complete cure.
Again, regeneration is an unnecessary drastic solution, but unlike Type 1, it would be effective in completely curing Type 2.
⚕️Holistic Approach
Gallifreyan medical technology approaches things more holistically, considering the interplay of their unique blood components, endocrine functions, and immune responses. The use of advanced diagnostics, personalised medicine, and possibly even real-time monitoring and adjustment of physiological parameters would be standard practices in their healthcare system.
🏫 So ...
In Gallifreyan society, while diabetes may not be as prevalent or manifest in the same way as in humans, it's a condition that their medical technology is well-equipped to manage. And if it can't manage it, there's always regeneration, but don't be wasting those bodies, now.
*A spacey-wacey machine™: any piece of equipment that can magically do future-y things because, well, sci-fi.
Hope that helped! 😃
→🫀Gallifreyan Anatomy and Physiology Guide (WIP)
→⚕️Gallifreyan Emergency Medicine/Monitoring Guides
→📝Source list (WIP)
-------------------------------------------------------
》📫Got a question / submission?
》😆Jokes |🫀Biology |🗨️Language |🕰️Throwbacks |🤓Facts
》📚Complete list of Q+A
》📜Masterpost
If you like what GIL does, please consider buying a coffee to help keep our exhausted human conscious for future projects, including complete biology and language guides.
#doctor who#gil#gallifrey institute for learning#dr who#dw eu#gallifrey#gil biology#gallifreyans#ask answered#gallifreyan biology#whoniverse#time lord biology
19 notes
·
View notes
Text
Long ass post about being a sick and disabled child with pediatric imposter syndrome and inattentive and flat out ableist adults ahead. It got ahead of me but there's nothing I want to cut. No I'm not putting it under a read more. Look at my post, boy.
I wonder if my childhood fascination with wheelchairs was based in the chronic pain and exhaustion I was feeling even by the age of seven.
In second grade we had a "disability week" (tho I wouldn't be surprised if they had called it "differently abled" but I can't remember for certain) where we had disabled adults come to speak to our (allegedly) able-bodied class and the school as a whole. The ones i remember were just explaining the disability and a simplified ways to treat it and things like it's rude to stare and such. Not too too glurgy in that out of context...
...but the memories about it are def tainted by the fact that any kid who was sick or disabled was forced to give presentations on their medical conditions to "educate and de-stigmatize" the students.
This wasn't part of Differently Abled Week, we were just forced to present when we just got diagnosed or whenever the condition got noticed by anyone. The first one i saw was in first grade as a fifth grader gave all the individual classes a presentation on her diabetes. I was forced to give one in third grade after I came back from being dramatically rushed to the hospital after my heart started beating so fast and hard that you could see it thru my shirt, and after about a week out of school in another hospital in the bigger city two hours away because my hometown hospital wasn't equipped to treat pediatric cardiac problems. My third grade presentation on supraventricular tachycardia was well-received, and the school was sympathetic because all my classmates and teachers were like omg this angelic little child has a heart condition and everyone was scared that I might die 😢
... Next year's fourth grade presentation on I Shit Too Much Disease was less well-received, even as I tried to self-censor the inherently disgusting details. To add to that, my SVT had been corrected (for a few decades, it appears to be coming back after 2) by an ablation in late third grade, so the Scary Heart Explodey (not really) Disease had been tied up neatly and I was free to live as a Normal Child. But Crohn's disease was something else, something relatively new to the lexicon in the early millennium and I constantly had to explain my health to strangers as the unwilling IBD Ambassador of the town. This would be and still is life-long and particularly hard to treat (my Crohn's was once compared to brittle diabetes in the way it never did and still doesn't respond to treatment), and the sympathy of the ableds is fickle and short lasting. Even just a year after my Diagnosis, my teachers stopped caring WHY I was missing school and sleeping all the time and in the bathroom too long and only saw these as delinquent behaviors to be punished, and my classmates no longer had sympathy for the perceived special treatment I barely got and were convinced I was faking it all for attention
Anyway I'm digressing, but I did need to feel the need to give context to my school's attitude towards sick kids. Back to Disability/Differently Abled Week
...We were allowed to play with mobility aids. Yeeeah. To de-stigmatize of course, totes not to keep us occupied. At one point we played with wooden beads of different shapes to make "hearing aids" and microphones in the style of the day, and each class was allowed one wheelchair, two sets of crutches, and a few arm slings for kids to be assigned to use for half the day.
I had seen these before. There were only a few sick kids in my school and none in mobility aids, but 7 year olds do have some life experience in being in the outer world, and my hometown was a city and not insular, so I had been exposed to disabled people before. My grandmother's best friend was an old lady with a basic prosthetic foot and used a cane, and she was patient and i daresay a little proud to show it off when i was really little and we'd go to have tea/hot chocolate with her and i stared in fascination and asked innocently offensive questions. At seven I hadn't been diagnosed with SVT or Crohn's yet and my intense and agonizing leg pains had been dismissed by my pediatrician as a hysteric and melodramatic little girl's response to "growing pains" (I've stopped growing but still feel them, I'm just used to them enough after thirty years that I barely notice them unless my legs are touched). I knew about broken bones and as someone who still had potent memories of toddler ear infections that were bad enough to send me to the E.R, I had even taken a few rides in wheelchairs.
But being in a wheelchair constantly was a new experience for me, especially as this was a manual wheelchair that you pushed yourself with the big wheels in, not the hospital kind that nurses push for you. The thought of never having to use my legs was an intoxicating thought, and I had childhood delusions of being strong and muscley enough to be able to handle maneuvering it with my scarily emaciated noodle arms.
Aides were assigned by last name down the list, and the teacher just arbitrarily decided which one you'd get. My last name is fairly down the list, so I waited the better part of a week to get assigned, all the while eyeballing the wheelchair enviously as my classmates assigned to it got to play disabled in it. I wondered how to pop a wheelie in it (for the record, my immediate reaction to being given roller skates on my fourth birthday was to immediately try to do a trick jump off the porch and landed hard on my ass with miraculously intact bones and face). But mostly I was fascinated by the thought of never having to use my legs for an entire half a day. I kept my composure at school so not to be labeled a crybaby, but by the time I got home I sometimes couldn't even focus on Pokémon because my legs were too agonizing and I'd be crying. My parents were sympathetic enough to my leg pains that they bought me hot water bottles to sooth my knees and tried to get me to take my mind off it by meditating the pain away (I'm too bipolar to focus in meditation even then but everyone's reaction to my bipolar is another long ass post in the making). But they didn't care enough to advocate for me against my pediatrician, even as he ignored all my other dramatic symptoms that were beginning to become un-ignorable. It took until my heart emergency for any adult (ily Dr. Stein, my pediatric cardiologist who immediately realized I needed more help than just for SVT) to notice the misery I was in and get me the right help (ily Dr. Maizle, my first pediatric gastroenterologist and the only one who actually listened to me when i said some of the meds felt worse than the disease).
Anyway I was assigned crutches when my name was called and i nearly did finally snap and cry at school. Nearly. And the crutches (basic under armpit ones, not forearm crutches) sucked. They were painful in my armpits, they weren't adjusted to my height properly, and I fell a few times because I was trying to swing both my legs at the same time because BOTH my legs were in constant agony and I was trying to alleviate my body's pressure on them both. I had a miserable time "pretending" to be disabled, but I was the only one who complained about the crutches and so I went ignored, setting up the theme for my childhood.
This fascination with wheelchairs stuck with me and as I became a bigger kid and my body just piled on more illness and pain, but despite all that my legs were technically functional so I kept my yearning for a chair quiet for fear of being offensive (didn't know what appropriation meant back then but that was the feeling) and an actual attention seeker like my classmates accused me off. Sure, I was sick and constantly in pain, but at least I wasn't actually "stuck in a wheelchair". Could be worse. At least it's not cancer, after all.
It got to the point that by middle school i was having idle fantasies about being grievously and dramatically injured to the point I lose my aching leg(s) and thus was finally granted a wheelchair. In my darkest moments I wondered how much pain doing it myself would be in the moment, but the thing that snapped me out of crippling (I use that word deliberately) myself was that I genuinely love the feeling of sand beneath my feet and the way beach sand (I wouldn't see the ocean until my twenties, but the artifical lake we went to had sand) felt in between your toes and how my feet didn't ache so much as the hot sand conformed around them. I still kept this quiet because I knew it was crazy and was beginning to realize that I as a whole being was crazy, but I didn't want to be treated as crazy so I kept my fantasies secret.
I've lost the point I was trying to make as I ramble on about these physically painful memories but I'm going to end by saying lmfao I've been using a cane for my pain (to not great success tbh) and have been told I'll prolly need a wheelchair in the next few years. My trepidation about this is totally devoid of any "be careful what you wish for!" karma and everything to do with how infamously inaccessible the Atlantic Coast of the United States is for mobility access. The buildings are all old and pretty and no one wants to ruin the aesthetics of the rowhomes and the shops (except the liquor stores, make of that as you will) don't want to put in the money to add or replace the stairs getting up to the shops with ramps.
This is really dumb even before I started using aides, because EVERYONE can use a ramp while only SOME people can use stairs. And that's not even the end of it, if you manage to get into the shops the aisles are too small to get even a folding chair in between, and no one wants to put in the extra work to rearrange the store to cater to those seeking "special treatment". For years I thought the A.D.A had a grandfather clause that said historical buildings didn't have to adapt unless they renovate and that's why the older cities on the East Coast are the way they are. Nope, that clause doesn't exist. But no one is willing to enforce the A.D.A except SOMETIMES for federal buildings. Even some medical facilities are on stairs with no ramp. Baltimore IS in the middle of a years-long A.D.A lawsuit, but it's only for the absolutely abysmal sidewalks that prevent wheelchairs from going over them at all and makes it treacherous for canes and crutches. I see people in wheelchairs on the road more than I see them on sidewalks because it's the only way to get a wheelchair to move. Baltimore drivers are legitimately and legendarily terrifying. I wouldn't even want to ride a bike (were I still able) in the bike lanes, let alone wheel myself IN a major road. This is going to be a terrifying experience here, unless something very much changes and soon. But will the abled leaders care enough even if they're under lawsuit? I don't feel optimistic. But what choice do/will I have? It doesn't HAVE to be hard, but it WILL be because ableds don't care enough to make even the slightest change to make it easier for EVERYONE if it takes even the slightest bit of effort. See: their collective response to covid
#disability#chronic pain#chronic illness#ableism#mobility aids#self harm tw#for the idle thoughts of it in the center#child neglect#I'll concede to tag this as#long post#apropos of nothing this would make a good essay I.Y.K.Y.K#systemic ableism
8 notes
·
View notes
Text
Women should be offered "menopause checks" by GPs after turning 40, campaigners and MPs have said.
The Menopause All-Party Parliamentary Group said this should be included in the NHS Health Check offered every five years to those aged between 40 and 74.
MPs said a lot of women over 40 go to their GP with symptoms, unaware they are experiencing the menopause.
Campaigner Mariella Frostrup said it was "ludicrous" that menopause information was not part of the check.
The free NHS Health Check looks for conditions such as heart disease and diabetes.
Ms Frostrup, chairwoman of the Menopause Mandate campaign, told BBC Breakfast it should include information and support about the menopause.
"It seems utterly ludicrous you go to this health check as a woman in your early 40s, which is exactly when perimenopause starts for most women, and the one thing you don't find out about is the one thing that you will absolutely 100% be experiencing over the subsequent decade," the author and journalist said.
Ms Frostrup added that a survey of more than 2,000 women conducted for the campaign found the majority had self-diagnosed their menopause, with only 12% getting a diagnosis from a health professional.
"Surely that's not good enough in the 21st Century," she said.
The Menopause All-Party Parliamentary Group said doctors often failed to recognise the symptoms.
More needed to be done to ensure medical professionals feel "equipped and empowered" to prescribe all types of hormone replacement therapy (HRT) - a treatment that helps alleviate the symptoms of the menopause, the group said.
Labour MP Carolyn Harris, the group's chairwoman, said: "We still have many hurdles to tackle to ensure women suffering through menopause get the support they deserve.
"Day in, day out I hear stories from women who can't get a diagnosis from their GP, who can't get HRT due to a lack of supply, who have left their jobs due to a lack of support, or who simply don't know where to turn for help."
What is the menopause?
The menopause is when women's periods stop, which normally happens around the age of 51. Symptoms normally start in the mid-40s.
This signals the end of the reproductive years and the start of a new phase of life.
The lead-up to this happening, when periods become irregular, is known as the perimenopause. It starts, on average, at 46.
This is when many women notice their periods becoming unpredictable or heavy, and have feelings or physical problems they have not experienced before.
When periods have not happened for 12 months, you can look back and say you have been through the menopause (the last period).
For some, it can happen earlier - either naturally, or after treatment for another condition.
It comes as research from the UC San Diego School of Medicine, published by the International Menopause Society, highlights that women going through the menopause are at increased risk of cardiovascular disease.
Dr Sonya Babu-Narayan, associate medical director of the British Heart Foundation, said: "Changes to a woman's body during menopause, such as fallen oestrogen levels, are linked with a higher risk of developing cardiovascular disease.
"After the menopause, the chance of a woman having a heart attack is drastically increased.
"All too often, women don't prioritise their own health. As we women approach menopause, it is a perfect opportunity to reassess our risks of future cardiovascular disease and to take steps to protect our hearts."
She said preventative action included not smoking, exercising regularly, eating a healthy diet and maintaining a healthy weight.
10 notes
·
View notes
Text
In case you did not know, approximately 1 in 10 people with a uterus have polycystic ovarian syndrome (PCOS). Some studies have even shown the potential of 1 in 5 people with a uterus having PCOS. If you have irregular periods please go ask for testing.
Most people think PCOS just means you don't have a normal period, and that you might be sweatier, hairier, and fatter due to higher levels of testosterone. Well it also gives you a higher predisposition for uterine cancer and diabetes. If this is the first you've heard of this then I doubt you're alone.
Of course society thinks the worst thing for a person with a uterus is to not be dainty and hairless with the ability to pop out kids whenever we want, but they ignore the fact PCOS can lead to potentially fatal conditions. There are ways to prevent them, though, which is why it is so important to look into treatment options for PCOS with your doctor/obgyn.
I was told this information three months ago despite being diagnosed for seven years and my family having a history of reproductive disorders. Please get checked out if there is even a slight possibility of you having PCOS or another reproductive disorder. It affects so much more than your period or fertility. A diagnosis might just save your life.
#polycystic ovarian syndrome#pcos#menstruation#people who menstruate#feminism#patriarchy#misogyny#misogyny in medicine#reproductive health#polycystic ovarian disease
68 notes
·
View notes
Text
Doing review questions.
Hyperkalemia is a known side effect of ACE inhibitors and angiotensin receptor blockers such as olmesartan. The risk of hyperkalemia is increased with chronic kidney disease, diabetes mellitus, moderately severe to severe heart failure, NSAID use, and older adults. Chlorthalidone and hydrochlorothiazide can cause hypokalemia.
In men who are diagnosed with hypogonadism with symptoms of testosterone deficiency and unequivocally
and consistently low serum testosterone concentrations, further evaluation with FSH and LH levels is
advised as the initial workup to distinguish between primary and secondary hypogonadism. If secondary
hypogonadism is indicated by low or inappropriately normal FSH and LH levels, prolactin and serum iron
levels and measurement of total iron binding capacity are recommended to determine secondary causes of
hypogonadism, with possible further evaluation to include other pituitary hormone levels and MRI of the
pituitary. If primary hypogonadism is found, karyotyping may be indicated for Klinefelter’s syndrome.
Daily use of polyethylene
glycol (PEG) solution has been found to be more effective than lactulose, senna, or magnesium hydroxide
in head-to-head studies. Evidence does not support the use of fiber supplements in the treatment of
functional constipation. No adverse effects were reported with PEG therapy at any dosing regimen.
Low-dose regimens of PEG are 0.3 g/kg/day and high-dose regimens are up to 1.0–1.5 g/kg/day.
Ref: Tabbers MM, DiLorenzo C, Berger MY, et al: Evaluation and treatment of functional constipation in infants and children:
Evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr 2014;58(2):258-274.
2) Gordon M, MacDonald JK, Parker CE, et al: Osmotic and stimulant laxatives for the management of childhood
constipation. Cochrane Database Syst Rev 2016;(8):CD009118. 3) Lauters R, Saguil A: Laxatives for the management of
childhood constipation. Am Fam Physician 2017;96(7):433-434
Primary hyperaldosteronism should be suspected as a cause for hypertension if a patient has a spontaneously low potassium level or persistent hypertension despite the use of three or more antihypertensive medications, including a diuretic. This can be evaluated by checking a serum renin activity level and a serum aldosterone concentration and determining the aldosterone/renin ratio. Primary hyperaldosteronism typically presents with a very low serum renin activity level and an elevated serum aldosterone concentration. A 24-hour urine collection for 5-hydroxyindoleacetic acid (5-HIAA) would be used to evaluate for a neuroendocrine tumor, which can present as chronic flushing and diarrhea. Cortisol levels can be checked if Cushing syndrome is suspected. Hypertension can be present in Cushing syndrome, but it is typically associated with other signs such as obesity and an elevated blood glucose level due to insulin resistance.
Psychogenic tremor is characterized by an abrupt onset, spontaneous remission, changing characteristics,
and extinction with distraction. Cerebellar tremor is an intention tremor with ipsilateral involvement on
the side of the lesion. Neurologic testing will reveal past-pointing on finger-to-nose testing. CT or MRI
of the head is the diagnostic test of choice. Parkinsonian tremor is noted at rest, is asymmetric, and
decreases with voluntary movement. Bradykinesia, rigidity, and postural instability are generally noted.
For atypical presentations a single-photon emission CT or positron emission tomography may help with
the diagnosis. One of the treatment options is carbidopa/levodopa.
Patients who have essential tremor have symmetric, fine tremors that may involve the hands, wrists, head,
voice, or lower extremities. This may improve with ingestion of small amounts of alcohol. There is no
specific diagnostic test but the tremor is treated with propranolol or primidone. Enhanced physiologic
tremor is a postural tremor of low amplitude exacerbated by medication. There is usually a history of
caffeine use or anxiety.
Ref: Crawford P, Zimmerman EE: Tremor: Sorting through the differential diagnosis. Am Fam Physician 2018;97(3):180-186.
I got 100% on the first quiz! :)
2 notes
·
View notes
Text
Mélovin Health Update: What We Know So Far (11/13/2023)
Okay so normally I'd just reblog the last post I made, but after trawling through countless news/tabloids sites, Reddit, and the cesspool that is Twitter and sorting through the various information available, it seemed more important to make a separate post entirely so people could see.
HERE IS WHAT HAS HAPPENED/WHAT WE KNOW:
-Mel has been diagnosed with a serious illness.
-I cannot *personally* confirm for sure what illness, HOWEVER, most sources are reporting that it is steatohepatitis, a liver condition, sometimes also known as "Nonalcoholic Fatty Liver Disease"
-In essence: this is essentially an inflammation of the liver caused by fat cells building up in said liver, not brought on by drinking alcohol.
-It is considered a metabolic disorder. There are several potential causes, most of which are tied to type 2 diabetes and obesity complications, hormone imbalances such as with the thyroid, but it can also just be bad luck of the genetic draw.
-This is NOT the same condition as viral hepatitis (aka Hepatitis C, etc.) I mention this specifically because some sites are incorrectly reporting this claim and people are already using that misinformation as ammo to be homophobic and claim that he got this condition as a result of his "orientation". Do not do this. Do not be these people.
-Is it terminal or is it incurable? Well, that's the muddied part of this. Even Mel used the term 'terminal' in his Instagram post about this, however many sources seem to point to 'incurable' as a more accurate term. It could be that the words are very similar in Ukrainian and thus the confusion there.
-Note that steatohepatitis *is* incurable, however it *may* or *may not* be terminal/fatal. We don't know how long he's had it, if there was liver damage already present before his being officially diagnosed, and to what extent. The main complications that can lead to death if no treatment is administered are cirrhosis and scarring, even liver cancer, which the only treatment at that point would be a full liver transplant. Without treatment, expectancy is anywhere between 3-5 years in severe cases, or 10-15 in lesser ones. Again, this is not proof of anything yet, this is only the general knowledge I have gained from researching this condition.
-This diagnosis came about as a result of bloodwork when he intended to get some kind of cosmetic procedure.
-(Before anyone asks what cosmetic surgery was he getting - that I don't know, and I don't think anyone else does either. He hasn't said, and cosmetic is a very broad term and can range from anything like traditionally thought-of plastic surgeries to something less intensive like a mole removal or getting his teeth worked on. Personally I think he's too young to be getting cosmetic work done, but that's not important right now.)
-He is seeking/undergoing treatment and currently resting and recovering at home with his family.
-His Instagram is currently private to non-followers, probably to prevent harassment. I have downloaded the video regarding this apparent diagnosis announcement and will try to upload it.
-He is still apparently on the longlist for competing in Vidbir, as announced by Suspilne.
-It is not known if this will impact the release of his newest song or further music going forward.
= o = o = o = o = o = o =
If more develops, I will try to let you all know. Right now, please just try to be supportive, don't harass him or his friends/family for more info (he will no doubt tell us when he is ready), and don't spread wild misinformation. We can only imagine what he must be going through right now. Even if this ends up not being nearly as bad as it sounds, getting a lifelong illness diagnosis is not easy for anyone to handle.
5 notes
·
View notes
Note
Med school and residency shove a lot of information at you at once. From the friends I have currently going through the process, it’s a battle to keep your ability to think outside of the box.
If you have a patient with a complicated case that didn’t just WebMD possibilities over the weekend, but their potential causes don’t fit the “textbook diagnosis,” it might be worth looking into their suggested diagnosis.
I was told for four years that “there was no way I lost any endocrine function because I didn’t lose consciousness from my TBI. It only happens in severe cases.”
Four years without the estrogen necessary to keep my heart and reproductive organs healthy. Four years without the testosterone to build muscle, damaging my joints because I “just needed to exercise to feel better.” Four years without proper thyroid replacement, because endocrinologists only focus on thyroid treatment/diabetes or sex hormones, never both.
An osteopath finally got my hormones and my ability to function somewhat normally back because she listened. She considered that the area in front of my pituitary gland had taken the brunt of the force, so it was totally possible for a structural issue with the stalk to create signaling problems a normal MRI wouldn’t be able to find. She examined how I passed out for, essentially, two days straight, and had no memory of the next three months to conclude my injury was more severe than the ER wrote in their report. That wasn’t a shocker—the ER Resident had to have the nurse do the neuro exam because he couldn’t remember what questions to ask and which reflexes he had to test.
Long story short: if you get a patient with some kind of chronic or complex issue, and they’ve been trying to heal for a while, you may be able to help them avoid needless suffering by listening to what they have to say and using your own critical thinking skills to consider diagnoses outside of the norm.
my jaw literally dropped reading this. thank you so much for this ask. i'll definitely carry this story with me as i progress through my medical journey.
out of curiosity, are you also in the medical field, or just know friends who are?
14 notes
·
View notes
Text
It is critical to identify healthy lifestyle behaviours that promote psychological well-being in order to prevent mental disorders. The current study sought to assess the individual and combined associations between various aspects of daily life and mental health.
#Health & Wellness Coach#Wellness Expert & Nutritionist#personality development classes#diabetes - diagnosis and treatment normally
0 notes
Text
batten down the hatches kids, because THIS is my supervillain origin story!
i was recently (several months ago) diagnosed with diabetes. it was an extremely traumatic process for me, not at all aided by my doctor, who would only prescribe me a single first-line medication and when that didn’t completely control things told me that i would have to do the rest myself by putting myself on a strict diet to cut out basically all the foods that make life worth living. i have a history of disordered eating though, so i wasn’t about to do that, and i spent many weeks in turmoil and dismay over what the rest of my life was going to look like.
this is, i have been assured, a fairly standard reaction to being diagnosed with diabetes.
then, not being able to deal with my normal doctor anymore, i went to an endocrinologist, and that changed everything.
this woman was so kind and so compassionate i can’t even begin to tell you. she spoke to me calmly and reassuringly about my options, assuring me that there were many medications we could try and telling me the benefits and drawbacks of all of them. eventually we settled on a once-weekly injectable medicine, and she spent a lot of time explaining to me how to give it to myself, how to dispose of the needle, and how safe and easy the process actually was.
she did not, throughout the whole 45 minute appointment, say a word about my diet. she didn’t even tell me to cut out soda, which everyone and their dog had been telling me to do. i could have wept tears of joy at the revelation that i was going to be given medicine for my disease instead of being told it was all my fault and to handle it myself.
the endocrinologist also told me to monitor my blood sugar. this is pretty standard fair for diabetics, and while i had been told by other doctors to monitor my blood sugar, none of them had told me how or prescribed the proper equipment. my angel of an endocrinologist, however, prescribed me a good system and told me i only needed to test my blood sugar once a day, so they could get a baseline of how i was responding to the treatment.
naively, i thought this would be fairly straightforward. i am a diabetic, diabetics need to monitor their blood sugar, there should be no question of my getting the meter.
wrong.
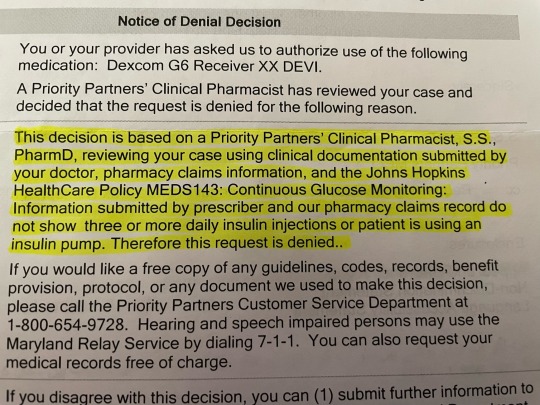
first i got a notice from the pharmacy telling me my insurance didn’t cover this specific brand of system. fine, whatever, bit annoying but i can deal. i called the insurance company and got a list of systems they cover, and passed that along to my endocrinologist so she could prescribe me a different one. weeks pass, but i assumed it just takes a while to get these things done. i got another notice from the pharmacy saying the insurance had denied my claim, because i needed prior authorization. it was pretty cheesed off by this point, because it had been weeks and they were just now telling me this, but i called my endocrinologist and told her she needed to do a prior authorization. another few weeks pass, and we’re creeping closer to the follow-up appointment where i’m supposed to submit the data of all the blood sugar tests i’ve been doing for inspection.
then, i get this.
the insurance completely denied my claim for a blood glucose monitoring system. ANY blood glucose monitoring system. EVEN THE ONES THEY SUPPOSEDLY COVER. i have a formal diagnosis of diabetes, from MULTIPLE DOCTORS, but apparently that isn’t enough to convince them that i need to monitor my blood sugar. and even if i go on insulin, which is a HUGE step up from where i am and is VERY dangerous even taking a little bit at a time, apparently they won’t cover the cost of monitoring my blood sugar until i’m taking THREE SHOTS PER DAY.
THREE.
SHOTS.
PER.
DAY.
you have to have ADVANCED diabetes to be taking that much insulin. you have to be fucking DYING. i’m type 2 as opposed to type 1, type 1 being much more serious from day one, but with type 2 your diabetes has to have gone uncontrolled for YEARS before you get to the point of taking that much insulin per day. you have to be fully dependent on insulin TO SURVIVE.
AND THEY DON’T
EVEN
THINK
I NEED TO BE
M O N I T O R I N G
MY BLOOD SUGAR
UNTIL I GET TO THAT POINT!
this policy will kill people. i feel confident in saying it already has. and because i am entirely dependent on insurance to afford ANY medication to control my diabetes, i am at the mercy of their rulebook.
THIS IS WHAT FOR-PROFIT HEALTHCARE HAS DONE TO US!
this is not freedom. this is not choice. this is a cage closing around us like a death trap. this isn’t just ableism, it’s eugenics, the systematic stamping out of an undesired class of people. this is “give me your money or i’ll shoot you in the head” with barely any extra steps.
UNIVERSAL HEALTHCARE NOW!
OR I’LL FUCKING EAT YOU!!!
#diabetes#health insurance#universal healthcare#single payer healthcare#for profit healthcare#ableism#eugenics
8 notes
·
View notes
Text
*Dr. Smita Goel Homeopathy Clinic*
Hyperhidrosis, also known as polyhidrosis or sudorrhea, is a condition characterized by excessive sweating. The sweating can affect just one specific area or the whole body.
Although not life-threatening, it can be uncomfortable and cause embarrassment and psychological trauma.
In this article, we will look at the causes, symptoms, diagnosis, and treatment of hyperhidrosis.
Fast facts on hyperhidrosis
Here are some key points about hyperhidrosis. More detail and supporting information is in the main article.
• Hyperhidrosis tends to begin during adolescence
• An estimated 15.6 million people have hyperhidrosis
• Most commonly, the feet, hands, face, and armpits are affected
• There are a number of remedies that can reduce symptoms
What is hyperhidrosis?
The excessive sweating associated with hyperhidrosis is normally most active in the hands, feet, armpits, and the groin because of their relatively high concentration of sweat glands.
• Focal hyperhidrosis: When the excessive sweating is localized. For example, palmoplantar hyperhidrosis is excessive sweating of the palms and soles.
• Generalized hyperhidrosis: Excessive sweating affects the entire body.
Hyperhidrosis may be present from birth or might develop later in life. However, most cases of excessive sweating tend to start during a person's teenage years.
The condition can be due to an underlying health condition, or have no apparent cause:
• Primary idiopathic hyperhidrosis: "Idiopathic" means "of unknown cause." In the majority of cases, the hyperhidrosis is localized.
• Secondary hyperhidrosis: The person sweats too much because of an underlying health condition, such as obesity, gout, menopause, a tumor, mercury poisoning, diabetes mellitus, or hyperthyroidism (overactive thyroid gland).
According to the International Hyperhidrosis Association, approximately 2.8 percent of Americans are affected by hyperhidrosis; that's around 7.8 million people.
For some, hyperhidrosis symptoms are so severe that it becomes embarrassing, causing discomfort and anxiety. The patient's career choices, free time activities, personal relationships, self-image, and emotional well-being may be affected.
Fortunately, there are several options which can treat symptoms effectively. The biggest challenge in treating hyperhidrosis is the significant number of people who do not seek medical advice, either due to embarrassment or because they do not know that effective treatment exists.
Symptoms
Hyperhidrosis is defined as sweating that disrupts normal activities. Episodes of excessive sweating occur at least once a week for no clear reason and have an effect on social life or daily activities.
Signs and symptoms of hyperhidrosis may include:
• Clammy or wet palms of the hands
• Clammy or wet soles of the feet
• Frequent sweating
• Noticeable sweating that soaks through clothing
People with hyperhidrosis might experience the following:
• Irritating and painful skin problems, such as fungal or bacterial infections
• Worrying about having stained clothing
• Reluctant to make physical contact
• Self-conscious
• Socially withdrawn, sometimes leading to depression
• Select employment where physical contact or human interaction is not a job requirement
• Spend a large amount of time each day dealing with sweat, such as changing clothes, wiping, placing napkins or pads under the arms, washing, wearing bulky, or dark clothes
• Worry more than other people about body odor
Experts are not certain why, but excessive sweating during sleep is not common for people with primary hyperhidrosis (the type not linked to any underlying medical condition).
Causes of primary hyperhidrosis
People used to think that primary hyperhidrosis was linked to the patient's mental and emotional state, that the condition was psychological and only affected stressed, anxious, or nervous individuals.
However, recent research has demonstrated that individuals with primary hyperhidrosis are no more prone to feelings of anxiety, nervousness, or emotional stress than the rest of the population when exposed to the same triggers.
In fact, it is the other way round - the emotional and mental feelings experienced by many patients with hyperhidrosis are because of the excessive sweating.
Studies have also shown that certain genes play a role in hyperhidrosis, making it look more likely that it could be inherited. The majority of patients with primary hyperhidrosis have a sibling or parent with the condition.
Causes of secondary hyperhidrosis
• Spinal cord injury
• Alcohol abuse
• Anxiety
• Diabetes
• Gout
• Heart disease
• Hyperthyroidism - an overactive thyroid gland
• Obesity
• Parkinson's disease
• Pregnancy
• Respiratory failure
• Shingles
• Some cancers, such as Hodgkin's disease
• Some infections - HIV, malaria, TB (tuberculosis)
• Some medications, including some antidepressants, anticholinesterases (for Alzheimer's disease), pilocarpine (for glaucoma), propranolol (for high blood pressure)
• Substance abuse
Natural remedies
Some alterations in daily activity and lifestyle may help improve symptoms:
• Antiperspirants - deodorants do not stop sweating, but antiperspirants sprays do. Some prescription antiperspirants include aluminum chloride, which plugs the sweat glands.
• Armpit shields - pads worn in the armpit to protect a garment from perspiration.
• Clothing - certain synthetic fibers, such as nylon, may worsen symptoms. Loose clothing is better.
• Shoes - synthetic materials are more likely to worsen symptoms. Natural materials, such as leather, are recommended.
• Socks - some socks are better at absorbing moisture, such as thick, soft ones made of natural fibers.
If these measures are not effective, medical treatment may help.
Antiperspirants and armpit shields are available to purchase online.
Complications
If hyperhidrosis is not treated, it can lead to complications.
• Nail infections: Especially toenail infections.
• Warts: Skin growths caused by the HPV (human papillomavirus).
• Bacterial infections: Especially around hair follicles and between the toes.
• Heat rash (prickly heat, miliaria): An itchy, red skin rash that often causes a stinging or prickling sensation. Heat rash develops when sweat ducts become blocked and perspiration is trapped under the skin.
• Psychological impact: Excessive sweating can affect the patient's self-confidence, job, and relationships. Some individuals may become anxious, emotionally stressed, socially withdrawn, and even depressed.
On average, a person with hyperhidrosis seeks medical help after living with the condition for 9 years. It is important to spread the word that the symptoms of excessive sweating can be effectively treated.

2 notes
·
View notes
Text
Long COVID Experts: U.S. Government Needs to Do More | Time
For many people who are done with the pandemic and the caution that came with it, a maskless supermarket may seem like a sign of progress. But for those with an intimate understanding of Long COVID, it feels like a bad omen.
Dr. Ezekiel Emanuel is used to feeling like the only person in the country who still cares about COVID-19. He ignores the side-eye he gets for wearing an N95 mask at parties—a self-imposed policy that makes him “look odd” but kept him safe after a recent work dinner turned into a superspreader event. The oncologist, bioethicist, and professor at the University of Pennsylvania provides each of his students with an N95 and runs four HEPA air filters during lectures. He rolls down the windows when he gets in an Uber and goes hungry on planes so he can wear his mask the whole time. He’s given up one of his favorite pastimes—dining at restaurants—even now that many people don’t think twice about eating indoors.
Emanuel, 65, takes these precautions even though he’s vaccinated and boosted and thus well protected against severe COVID-19. The acute disease doesn’t scare him much—but what could come after does.
“The only thing that’s preventing me from leading a normal life is the risk that I’ll get Long COVID,” Emanuel says. “I can’t say why people aren’t [reacting like] their hair’s on fire. This is a serious, serious illness.”
...
By the CDC’s own estimate from June, one in five U.S. adults with a known prior case of COVID-19 had symptoms of Long COVID. Having COVID-19 also raises a person’s risk of developing chronic conditions including heart disease, asthma, and diabetes,
...
Long COVID can take many forms, including exhaustion, cognitive dysfunction, neurological issues, and chronic pain. People can develop it whether they’re young or old, sick or healthy, vaccinated or not. And while some people get better in a matter of months, recent studies and many patient experiences show symptoms can last years. There is no known cure for Long COVID, and the only way to prevent it is not to get infected at all.
...
Many Americans welcomed the return to normalcy. But to McCone, 32, that approach is “a crime against humanity,” given what we now know about Long COVID.
...
McCone got sick in March 2020. COVID-19 knocked him flat. ... More than two years later, McCone barely leaves the house, except for medical appointments. He still has severe fatigue, chest pain, shortness of breath, and nervous system dysfunction. He can’t work because of his symptoms, and his partner has become his caretaker. His symptoms got even worse after catching COVID-19 again in September 2021, so he’s “petrified” of getting reinfected—a fear he wishes more people shared.
...
Hannah Davis, a machine learning expert who began researching Long COVID after her own diagnosis, also got sick in March 2020. Davis has testified about Long COVID before Congress and advised federal health officials about the condition. She says those experiences have shown her that health officials understand that Long COVID is a substantial problem, and that, while vaccines reduce the risk of developing it—by some amount between 15% and 50%, studies suggest—they are not failsafe. The U.K.’s Office for National Statistics recently reported that roughly 4.5% of triple-vaccinated adults developed Long COVID after being infected by Omicron. But the government doesn’t seem to want to dwell on these scary stats, Davis says. “It really looks like it’s being hidden intentionally,” she says.
Davis believes that’s because the Biden Administration leaned heavily on vaccines as a ticket out of the pandemic and is wary of walking back that messaging now,
...
Some Long COVID advocates and scientists have called for an initiative like Operation Warp Speed—the Trump Administration program that quickly yielded multiple effective COVID-19 vaccines—for Long COVID treatments. But the NIH hasn’t built anything of the sort...
Dr. Eric Topol, founder of the Scripps Research Translational Institute and a prolific parser of COVID-19 research on Twitter, says the NIH is doing good research on the underlying science of Long COVID, but he’d like to see more trials focused on treatments. “You need to do both, because we can’t wait another year or two for the biology to be better defined,” Topol says. (The NIH says it will begin treatment-focused trials this fall...
...
A tremendous amount of Long COVID research has been published in the last two years, most coming out of independent laboratories, Putrino says. From this work, scientists have found multiple possible explanations for Long COVID symptoms: SARS-CoV-2 virus lingering in the body, abnormal immune system activity, reactivation of other viruses previously lying dormant, tiny blood clots throughout the body, and more. These disparate findings suggest that there may be different root causes or subtypes of Long COVID, which means all patients might not respond to the same therapy. But each one suggests a possible path to treatment worth testing sooner rather than later, Topol says.
...
Journalist and author Katie Hafner, 64, was one of the unlucky people to develop Long COVID after being vaccinated and boosted. She got infected in May and was left with significant fatigue and brain fog. Her Long COVID symptoms were on the milder end of the spectrum and have improved with time, but Hafner says she can still manage only a few hours of work per day and has to carefully monitor her physical and mental energy levels. Her anxiety has also escalated since getting sick.
Hafner’s husband is Dr. Robert Wachter, chair of the department of medicine at the University of California, ...
[Who, by the way, publicly shamed her: https://twitter.com/Bob_Wachter/status/1522799251914313728

She got sick shortly after.
Now Bob says:
“If it turns out that it markedly increases the rates of some of the biggest medical hazards we have in life”—including organ failure, heart disease, and dementia, as research currently suggests— “the toll of that over years and years will be tremendous,” Wachter says. “I don’t think [the CDC has] done a good job explaining that at all.”
...
Experts say there is more that can be done, even before new therapies are discovered or developed. To slow transmission and thus lower rates of Long COVID, Topol says the CDC should tell people to isolate for longer than five days after getting infected and campaign harder for people to get booster shots. Emanuel, meanwhile, would like to see better communication about which masks protect wearers from infection; respirators like N95s are more effective than surgical or cloth masks, but many people still walk around in droopy blue surgical masks. Public indoor spaces, like restaurants and schools, should also have enforceable requirements for ventilation and air filtration, given the virus’ ability to spread in the air.
...
A return to mask mandates would also be a good step, Davis says. But even if none of those changes are enacted, she says the government should at least emphasize how common Long COVID appears to be and that it can affect vaccinated people. She fears many vaccinated people think they’re in the clear and can’t get Long COVID, because the Administration has sung the shots’ praises so much. “We’re just drowning in this sea of misinformation that is not only causing people to poorly think about their own risk, but also putting other people at risk,” Davis says.
Those with Long COVID often say they feel like they’re screaming into the void, trying to get through to people who either aren’t aware of or don’t care about the condition and the possibility it could affect them, too.
For many people who are done with the pandemic and the caution that came with it, a maskless supermarket may seem like a sign of progress. But for those with an intimate understanding of Long COVID, it feels like a bad omen.
2 notes
·
View notes
Text
Warning Signs of Retinal Detachment And What You Should Do
UNDERSTANDING RETINAL DETACHMENT
Retinal detachment is a serious eye condition where the retina, a thin layer of tissue at the back of the eye, peels away from its underlying supportive tissue. This separation disrupts the retina’s normal functioning, leading to potential vision loss if not promptly treated. Understanding the causes, symptoms, diagnosis, and treatment options is crucial for effective management and prevention of this sight-threatening condition.

CAUSES AND RISK FACTORS
The primary cause of retinal detachment is the presence of a tear or hole in the retina, which allows fluid to seep underneath, separating it from the underlying tissues.
Rhegmatogenous Retinal Detachment: This is the most common type and is caused by a tear or break in the retina. Ageing is a significant risk factor because the vitreous, a gel-like substance inside the eye, shrinks and can pull on the retina, leading to tears. Other risk factors include severe myopia (near sightedness), previous eye surgery, or trauma.
Tractional Retinal Detachment: This occurs when scar tissue on the retina’s surface contracts, pulling the retina away from the back of the eye. It is often seen in people with diabetes mellitus, which can lead to diabetic retinopathy, a condition where abnormal blood vessels grow on the retina’s surface.
Exudative Retinal Detachment: This type is caused by inflammation, injury, or vascular abnormalities that result in fluid accumulation under the retina without any tears or breaks. Conditions such as inflammatory disorders, tumours, or age-related macular degeneration can lead to this type.
WARNING SIGNS OF RETINAL DETACHMENT
Retinal detachment is a serious condition that can lead to permanent vision loss if not promptly treated. Recognizing the warning signs early is crucial for seeking timely medical intervention. Here are the primary warning signs to watch out for:
Sudden Appearance of Floaters
Floaters are small specks or threads that drift through your field of vision. While floaters are common and usually benign, a sudden increase in their number can be a warning sign of retinal detachment. These floaters are caused by tiny clumps of gel or cells inside the vitreous, the clear gel-like substance that fills the inside of your eye.
Flashes of Light
Experiencing sudden flashes of light, particularly in your peripheral vision, is another common warning sign. These flashes can resemble lightning streaks and occur due to the vitreous pulling on the retina. The sensation can be more noticeable in dark environments.
Blurred Vision
A sudden decrease in vision clarity or blurring of vision can indicate retinal detachment. This blurriness often occurs in just one eye and can affect any part of your visual field.
Shadow or Curtain Over Vision
One of the most serious warning signs is the perception of a shadow or curtain descending over your field of vision. This effect can start in a small area and spread across the vision field as the detachment progresses. It typically starts from the peripheral (side) vision and moves towards the central vision.
Loss Of Peripheral Vision
Noticing a reduction or loss of peripheral (side) vision is a significant warning sign. This can be experienced as a darkening or shadow moving inward from the edges of your vision.
If you experience any of these warning signs, it is crucial to seek medical attention immediately. Retinal detachment is a medical emergency, and prompt treatment is essential to preserve vision. Early diagnosis and treatment can significantly improve the outcome and prevent permanent vision loss. Regular eye examinations, especially if you are at higher risk due to factors like severe nearsightedness, previous eye injuries, or family history, can help in early detection and management.
WHAT WE SHOULD DO?
Seek Immediate Medical Attention: If you experience any of these symptoms, contact an eye care professional immediately.
Avoid Strenuous Activity: Refrain from heavy lifting or vigorous exercise until you are evaluated by a doctor.
Keep Calm and Stay Still: Try to stay calm and avoid moving your eyes excessively to prevent further damage.
Prepare for an Eye Exam: Be ready for a comprehensive eye examination, which may include tests like ophthalmoscopy, ultrasound, or optical coherence tomography (OCT).
Follow Medical Advice: Adhere strictly to the treatment plan provided by your eye care specialist, which may include surgery or other interventions to repair the retina.
DIAGNOSIS
An eye examination is essential for identifying retinal detachment. An ophthalmologist will perform several tests, including:
Diagnostic Procedures for Retinal Detachment
Detecting retinal detachment early is critical for effective treatment and preventing permanent vision loss. A comprehensive eye examination can identify signs of retinal detachment. The following diagnostic procedures are commonly used by ophthalmologists:
Visual Acuity Test
A Visual Acuity Test measures how well you can see at various distances. During this test, you will be asked to read letters on a chart (commonly known as a Snellen chart) from a specified distance. Each eye is tested separately, with and without corrective lenses if you wear them. The test determines the smallest letters you can read on the chart, indicating the clarity and sharpness of your vision. A decline in visual acuity may signal an underlying issue, such as retinal detachment, especially if it occurs suddenly.
Dilated Eye Exam
A dilated eye exam involves the use of special eyedrops to widen (dilate) the pupils, allowing the doctor to get a better view of the retina and other structures at the back of the eye. After administering the drops, which take about 15 to 30 minutes to fully dilate the pupils, the ophthalmologist uses a magnifying lens to inspect the retina for any tears, holes, or areas of detachment. The dilation provides a more comprehensive view, making it easier to detect abnormalities that might not be visible with non-dilated pupils. This examination can also reveal other eye conditions, such as macular degeneration or diabetic retinopathy.
Ophthalmoscopy
Ophthalmoscopy is a diagnostic procedure utilized to inspect the rear portion of the eye, encompassing the retina, optic disc, and blood vessels. The doctor uses an ophthalmoscope, which is a handheld instrument equipped with a light and several lenses. The ophthalmoscope allows for a detailed examination of the retina. The procedure can be performed directly, with the doctor looking through the pupil, or indirectly, using a special lens held close to the eye. Indirect ophthalmoscopy, often performed with the aid of scleral depression (pressing on the sclera or white of the eye), provides a wider view of the retina, which is especially useful for detecting peripheral retinal tears or detachments.
Ultrasound Imaging
Ultrasound imaging of the eye, also known as ocular ultrasonography, is used when retinal detachment is difficult to visualize due to opacities like vitreous Hemorrhage (bleeding into the vitreous). This non-invasive test involves placing a small probe on the closed eyelid after applying a gel to facilitate sound wave transmission. The probe emits high-frequency sound waves that bounce off the internal structures of the eye and create detailed images of the retina and surrounding tissues. These images can help the ophthalmologist identify the location and extent of a retinal detachment, as well as other possible abnormalities such as tumours or foreign bodies within the eye. Ultrasound is particularly useful in emergency settings where a clear view of the retina is obstructed.
TREATMENT
Laser Surgery (Photocoagulation): A laser is used to seal the retinal tear by creating small burns around it, preventing fluid from passing through.
Cryopexy: Freezing is used to reattach the retina by creating a scar that helps secure the retina to the eye wall.
Pneumatic Retinopexy: A gas bubble is injected into the vitreous cavity to push the retina back into place.
Scleral Buckling: A piece of silicone material is sewn onto the sclera (white of the eye) to push the wall of the eye against the detached retina.
Vitrectomy: Removal of the vitreous gel to relieve traction on the retina and replace it with a gas bubble or silicone oil.
A specialized hospital like Dr. Rani Menon Maxivision Eye Hospitals in Thrissur provides hope and enhance the quality of life for those affected by retinal detachment. Schedule a consultation with our experts. Our compassionate team at Dr. Rani Menon Maxivision Eye Hospitals is here to assist with all your diabetes-related health concerns, tailored to the type of diabetes you have.
0 notes
Text
Atrial Fibrillation: Comprehensive Insights from Dr. Richard Zelman
Atrial Fibrillation (AFib) is the most common type of cardiac arrhythmia, affecting millions of people worldwide. It is characterized by an irregular and often rapid heart rate that can lead to various complications, including stroke, heart failure, and other heart-related issues. Dr. Richard Zelman, a distinguished expert in cardiology, provides a comprehensive overview of AFib, including its causes, symptoms, diagnosis, and treatment options.
Understanding Atrial Fibrillation
Pathophysiology
In a normal heart, the sinus node in the right atrium generates regular electrical impulses that travel through the atria to the ventricles, causing coordinated contractions. In AFib, these impulses become disorganized, leading to rapid and chaotic electrical signals. This results in the atria quivering instead of contracting effectively, which can cause poor blood flow and increase the risk of clot formation.
Causes and Risk Factors
Several factors can contribute to the development of AFib, including:
Age: The risk of AFib increases with age.
Heart Disease: Conditions such as hypertension, coronary artery disease, heart valve disease, and heart failure.
Thyroid Disorders: Hyperthyroidism can increase the risk.
Chronic Conditions: Diabetes, obesity, and chronic kidney disease.
Lifestyle Factors: Excessive alcohol consumption, smoking, and high caffeine intake.
Genetics: Family history of AFib.
Other Factors: Sleep apnea, infections, and stress.
Symptoms
AFib symptoms can vary in severity and may include:
Palpitations: Sensation of a racing, irregular, or pounding heartbeat.
Fatigue: Feeling unusually tired and weak.
Shortness of Breath: Difficulty breathing, especially during physical activity.
Chest Pain: Discomfort or pain in the chest.
Dizziness or Lightheadedness: Feeling faint or experiencing episodes of syncope (fainting).
Some individuals with AFib may be asymptomatic, with the condition only discovered during a routine medical examination or electrocardiogram (ECG).
Diagnosis
Diagnosing AFib involves a thorough clinical evaluation, including:
Medical History and Physical Examination: Assessment of symptoms, risk factors, and any underlying conditions.
Electrocardiogram (ECG): The primary tool for diagnosing AFib, showing irregular atrial activity and absence of P waves.
Holter Monitor: A portable device worn for 24-48 hours to detect intermittent AFib episodes.
Event Monitor: Used for longer periods to capture sporadic arrhythmias.
Echocardiogram: An ultrasound of the heart to evaluate its structure and function, and to check for blood clots.
Blood Tests: To identify conditions such as thyroid disorders or electrolyte imbalances.
Treatment
Treatment goals for AFib include controlling the heart rate, restoring normal rhythm, preventing blood clots, and managing underlying conditions. Treatment options include:
1. Rate Control:
Medications: Beta-blockers (e.g., metoprolol), calcium channel blockers (e.g., diltiazem), and digitalis (e.g., digoxin) to control heart rate.
2. Rhythm Control:
Antiarrhythmic Drugs: Medications such as amiodarone, flecainide, or sotalol to maintain normal rhythm.
Electrical Cardioversion: A procedure where an electric shock is delivered to the heart to restore normal rhythm.
Catheter Ablation: A minimally invasive procedure where abnormal heart tissue causing AFib is destroyed using radiofrequency energy or cryotherapy.
3. Stroke Prevention:
Anticoagulants: Blood thinners such as warfarin, dabigatran, rivaroxaban, or apixaban to prevent clot formation and reduce the risk of stroke.
Left Atrial Appendage Closure: A device implanted in the heart to prevent clots from forming in the left atrial appendage.
4. Lifestyle Modifications:
Diet and Exercise: Adopting a heart-healthy diet and regular physical activity.
Weight Management: Maintaining a healthy weight to reduce AFib risk.
Avoiding Triggers: Limiting alcohol and caffeine intake, and managing stress.
Advancements in AFib Treatment
The field of AFib treatment has seen significant advancements:
Cryoablation: A newer form of catheter ablation that uses extreme cold to destroy abnormal tissue.
Hybrid Ablation: Combines surgical and catheter-based techniques for more effective treatment.
Wearable Devices: Advanced monitoring devices that provide continuous heart rhythm data, aiding in early detection and management.
Conclusion
Atrial Fibrillation is a complex and challenging condition, but advancements in diagnosis and treatment are improving outcomes for patients. Dr. Richard Zelman MD expertise highlights the importance of a comprehensive approach to managing AFib, from lifestyle changes to cutting-edge medical interventions. Continuous research and technological innovations promise even better care and quality of life for individuals affected by this prevalent arrhythmia.
0 notes