#eosinophilic gastritis
Text

#eosinophilic gastritis#chronic illness#eosinophilic disorders#chronic illness meme#rare disease#EoG#eosinophilic disease#eosinophilic gastrointestinal disorders#eosinophilic gastrointestinal disease#monoclonal antibody#immune system disorder#immune system#pharmacology#biotech#biotechindustry#medication#medicine#rare disorders#il-5#fasenra#interleukin-5#benralizumab
7 notes
·
View notes
Text

5 notes
·
View notes
Text
Helicobacter Pylori
Spicing things up a bit with a Gram Negative Helical/spiral Bacteria
Epidemio:
up to 50% of the population worldwide, but even more in endemic countries/the 3rd world

it can cloud differentials, as it can be asymptomatic unless it caues peptic ulcer disease, in which case the infection may have been decades prior to detection - so you have to interpret serology with a grain of salt (it may not be the culprit of acute infection)
often picked up in early childhood and lingers without treatment for dcades
by contrast, 5% of children in the US have had it, so it may change your clinical decision making depending on where your patient grew up
In australian populations, up to 30% have it, but again, high frequency in older migrants, lower socioeconomic status etc.
Transmission:
faecal oral or even sexual (did not know that one)
increased risk:
lower socioeconomic status/growing up in a developed country
family history of infection and gastric cancer
What it does:
cause ulceration (peptic ulcer disease)
and inflammation or gastritis
due to it's helical shape and flagella, it can penetrate the mucosal lining
Trivia/History:
discovered by Australians in Western Australia in the 1980s
To quote the IM physician, Barry Marshall, in the face of skepticism that a bacteria could survive the stomach's acidic environment: "everyone was against me, but I knew I was right"
After failing to publish and some lab snaffus, he decided to do a Jonas Salk and swallow a broth of Hpylori himself. Of course this last experiment was published in an Australian journal.
At any rate, it is now widely accepted that Hpylori is linked to PUD and gastric cancer and by 2005, the two Australians who found the bacteria received the Nobel prize in medicine
we now know so much more about the pathogen with advancements in microbiology
they also came up with the urease breath test for it
Clinical presentation:
asymptoamtic
symptom onset occurs after gastritis and peptic ulcer disease develop: nausea, vomiting, dyspepsia, abdo pain, or at the extreme when the lining has eroded, bleeding/haematemesis
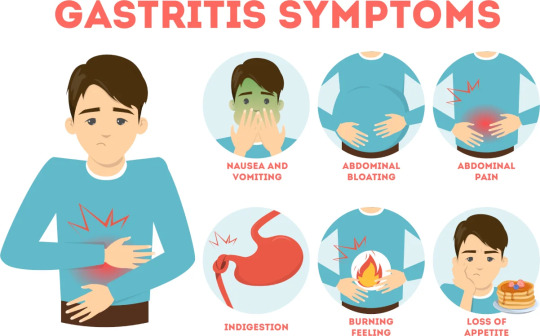
IMage source
Important differentials
coeliac's
Crohn's
nSAID induced gastritis
reflux
lactose intolerance
eosinophilic oesophagitis (sooo rare, usually a/w dysphagia)
Investigations
(all with relatively good/high sens and spec)
H pylori antigens in stool
serology (antibodies in serum, urine) --> usually IgG, hence can remain positive for years even post eradication
urease breath test
if a scope was involved due to PUD, then histopathology and culture (reduced sensitivity if treated with PPI in 2/52 prior or Abx 4/52 prior)
actually had no idea they breathed into little bags.

Treatment:
triple therapy - PPI, amoxicillin and clarithromycin for 14 days, in penicillin allergy replace amox with metro (increasing resistance is why metro is not first line in some countries - refer to local guidelines made based on local Abx resistance trends)
In patients younger than 50, it can be cost effective to treat if they have reflux on testing (if there's a high pretest probability - see increased risk groups) given the life time risk of PUD & gastric cancer, can also reduce risk of GIB
balance of risk/benefit: will it significantly improve QOL or will risks of ADRs outweigh the benefits (eg frail, elderly, multiple comorbidities)
when used in those with PUD - improves ulcer healing, recovery and prevents relapse
in simple ulcers, triple therapy is all that is required in more chronic complex ones --> 8/52 of PPI is also recommended to prevent recurring of bleeding etc.
not treating can lead to relapse and complications like bleeding/perforation/cancer risk
Complications
rarely, it can cause gastric adenocarcinoma as a known carcinogen
aka MALT lymphoma - mucosa-associated lymphoid tissue
this resolves with triple therapy (Usually)
consider it in family histories of gastric cancer
life time risk of gastric cancer at 2% and 15-20% risk of peptic ulcer disease
Wish the acronym wasn't MALT. But could be a good way to remember it. MALT, tasty, gastritis and Hpylori.

Follow-up
test for eradication 2 weeks post with stool antigen or urease breath test (serology less effective as the IgGs can remain positive for years) but that's on holding the PPI for 1/52 to prevent a false negative, some countries want both tests
in resistance or relapse there's salvage therapy, usually with bismuth or a quinolone.
Sources:
Wikipaedia - I havent covered pathophysio or it's cellular mechanisms and virulence factors, but there's a good overview in wiki
StatPearls (more paeds focused in this one)
CDC guidelines
Australian Therapeutic guidelines (Paywalll rest above are free)
5 notes
·
View notes
Text
Eosinophilic Gastrointestinal Disease
According to the localization of the gastrointestinal tract, primary eosinophilic gastrointestinal diseases include five variants such as esophagitis, gastritis, gastroenteritis, enteritis, and colitis.
0 notes
Photo

Immunological Gastrointestinal Tract Diseases
The CME/CPD accredited 13th World Gastroenterology, IBD & Hepatology Conference, which will take place on December 15-17, 2023 in Dubai, UAE. This is the best ways to network with fellow professionals, earn educational credits.
https://gastroenterology.universeconferences.com/submit-abstract/
Email: [email protected]
WhatsApp No: +442033222718
Contact No- +1 2073070027
This chapter discusses some of the most common immunological GI diseases seen in clinic, such as autoimmune gastritis, chronic Helicobacter pylori gastritis, celiac disease, inflammatory bowel diseases (IBDs; Crohn disease, ulcerative colitis [UC], microscopic colitis).
The gastrointestinal (GI) tract has the greatest concentration of immune cells of any organ in the body. The gut employs a number of strategies to promote mucosal structural integrity and maintain homeostatic immune regulation in response to continuous exposure to environmental and dietary antigens, as well as commensal microbes, pathogens, and their metabolic products. Despite these defences, the gastrointestinal tract is vulnerable to chronic immune-mediated inflammation from pathogenic organisms, as well as autoimmunity and immunodeficiency.
This chapter discusses some of the most common immunological diseases of the GI tract that are likely to be encountered in the clinic, such as autoimmune gastritis, chronic Helicobacter pylori gastritis, celiac disease, Crohn disease, ulcerative colitis, microscopic colitis, and eosinophilic esophagitis, and GI complications of primary immunodeficiency. The coverage focuses on clinical manifestations, disease mechanisms, and approaches to diagnosis and treatment for these conditions.
More than 80 different autoimmune diseases affect nearly 4% of the world's population, the most common of which are type 1 diabetes, multiple sclerosis, rheumatoid arthritis, lupus, Crohn's disease, psoriasis, and scleroderma.
There are two types of immunity: active and passive:
When our own immune system is in charge of protecting us from a pathogen, this is referred to as active immunity.
Passive immunity occurs when we are protected from a pathogen by the immunity of another person.
Immunity is classified into two types: innate and adaptive.
The innate immune system: rapid and all-around effectiveness. The skin and mucous membranes provide protection. Immune system cells (defence cells) and proteins provide protection. The adaptive immune system: Directly combating germs. T lymphocytes are immune cells.
Immunologic tests use an antigen to detect the presence of antibodies to a pathogen in the specimens, or an antibody to detect the presence of an antigen in the specimens. Laboratory immunological tests are created by creating artificial antibodies that exactly "match" the pathogen in question.
Primary: These are genetic disorders that are usually hereditary and are usually present at birth.
Secondary: These disorders usually appear later in life and are often caused by the use of certain medications or by another disorder, such as diabetes.
0 notes
Text
It's okay for me to sometimes be very sad and miss the life I had before I got sick. It's okay to for me to be sad I'm never going to get better. It's alright for me to be sad that I have to settle for the few good days I have.
#chronically ill#chronic pain#disabled#myalgic encephalomyelitis#endometriosis#Fibromyalgia#eosinophilia#eosinophilic gastritis#interstitial cystitis#oc#GETTING SICK ROBBED ME OF SO FUCKING MUCH AND I WANT TO SCREAM#reblogs okay
325 notes
·
View notes
Text
Let’s take better care of one another and the planet.
0 notes
Text
in an ideal world if i could just argue my case & magically convince doctors to do every test that might help & also it would be free:
parathyroid hormone levels (i always have elevated or borderline elevated calcium; i had a benign ectopic pancreatic tumor in my stomach; i have refractory peptic & duodenal ulcers, & severe refractory GERD; i have esophageal reflux dysphagia & cell changes leading to barrett's esophagus; they suspected zollinger ellison syndrome but never followed up, & together with my diffuse nonspecific fatigue/pain/GI issues, it is worth ruling out gastrinoma for sure & multiendocrine neoplasia for SURE for sure)
the full migraine-epilepsy-spinocerebellar ataxia genetic panel that also tests for mitochondrial diseases that mimic those conditions
biopsy esophagus, stomach lining, & small intestine for mastocytosis / eosinophilic esophagitis, gastritis, or whatever the intestinal version is, i forget
small intestinal transit study
repeat ultrasound of renal arteries because the last one was...unusable? & they just. kinda shrugged even though they couldn't see whether or not there was stenosis
please just rule out abdominal aortic dissection they run in my family so hard & i have hypertension & weird vascular issues nobody understands & i don't want to die in my 30s-40s
repeat MRI & brain CT w/ contrast just to check on things since i haven't had one since 2018 & am supposed to get them every 2 years re: cerebellum & the white matter you get with my genre of migraine
TILT TABLE
holter monitor that actually works
the thing where they measure your arterial pressure & blood oxygen as you change position? i don't remember but they used it to diagnose the guy whose symptoms mimicked POTS but had a different condition related to obstructive lung disease
the alpha-1 antotrypsin deficiency test that i WILL send this coming week for REAL
updated pulmonary function testing including the, um, what's it called. the stress test with the substance that starts with m? not metacholine but you know what i mean, the one they use to diagnose asthma. updated one of those too, i think my last one was in middle school & my lungs are Worse lol
sleep study for narcolepsy & sleep apnea
the thing where they run fibers into your extremities to see where your damaged nerves are when you have peripheral neuropathy so a doctor can write down "peripheral neuropathy" instead of "fibromyalgia" & insurance will let you see a pain clinic instead of a psychotherapist
full anemia breakdown & figure out why i have normal iron levels & normal ferritin & normal hemoglobin but my levels of BOUND iron are always anemia-low & i seem to have like, a transferrin deficiency??? what...causes that???
[Say The Line, Bart voice] anti-nuclear antibody test not at the clinic's convenience but when i am actually having an arthritis flare so it doesn't come back negative & get me dismissed from rheumatology lmfao. i've had this test done a handful of times in my life & the results are about 50/50 split down positive/negative & you'll never guess what the predictive co-variable is re: positive results (it's a corresponding elevated CRP level, because...autoimmune disease)
11 notes
·
View notes
Text

#eosinophilic gastritis#eosinophilic disorders#rare disease#eosinophilic disease#eosinophilic gastrointestinal disorders#eosinophilic gastrointestinal disease#chronic illness#chronic illness meme#rare disorders#EoG#food#food intolerances#food allergies#elimination diet
6 notes
·
View notes
Text
I live in constant fear of death as a general concept someday having an anaphylactic reaction and not having access to epinephrine
I’d say it’s an unrealistic fear but honestly? I have asthma, eczema, allergic rhinitis, and eosinophilic esophagitis/gastritis (a type of food allergy reaction). I have been described by multiple doctors as a “highly allergenic person.”
like is it that much of a leap to think I might someday have an anaphylactic reaction to something? Not....really.
but would any insurance cover a preventative epipen I think the fuck not.
#every time the bees come back I think about this#I was stung once as a six year old by a single yellow jacket but that does not preclude having a reaction to other species o.O#...also I was six my body has evolved allergies since then#the food ones were not there at birth
1 note
·
View note
Text
I wonder if I have eosinophilic gastritis or enteritis because my stomach is absolutely Not Normal and I’m suffering so much
#I already have EoE#every time I eat I’m in pain :(#and food just won’t leave my stomach and goes up and down my throat#for hours on end
1 note
·
View note
Text
This has been very helpful
#chronically ill#ssi#ssdi#Fibromyalgia#POTS#myalgic encephalomyelitis#me cfs#EDS#invisible illness#i hope this can help someone else too#disability application#disabled#eosinophilic gastritis#eosinophilic esophagitis
99 notes
·
View notes
Text

Here's the study if anyone is interested:
Dellon ES, Gonsalves N, Abonia JP, et al. International Consensus Recommendations for Eosinophilic Gastrointestinal Disease Nomenclature. Clin Gastroenterol Hepatol. 2022;20(11):2474-2484.e3. doi:10.1016/j.cgh.2022.02.017
#eosinophilic gastritis#eosinophilic disorders#rare disorders#rare disease#disease nomenclature#EoG#eosinophilic gastrointestinal disorders#eosinophilic gastroenteritis#eosinophilic disease#eosinophil#eosinophilic esophagitis#eosinophilic colitis#EoE#EGID#EGIDs#EoC#medical research#gastroenterology#chronic illness#EoN#eosinophilic enteritis#medical meme#chronically ill#chronic illness meme#Dellon et al.#International Consensus Recommendations for Eosinophilic Gastrointestinal Disease Nomenclature
3 notes
·
View notes
Text
Established Gastroenterologist, Myron D. Goldberg, MD, Welcomes Patients at His Private Practice in New York City, NY
Myron D. Goldberg, MD, FACP, FACG, FASGE, FAGA, is a well-versed gastroenterologist who diagnoses and treats patients at his private practice in New York City, NY. Furthermore, he is a Clinical Assistant Professor at NYU School of Medicine and remains affiliated with Lenox Hill Hospital, Mount Sinai St. Luke's, and Mount Sinai West. As a gastroenterologist, he has dedicated training and unique experience in the management of diseases of the gastrointestinal tract and liver. Dr. Goldberg’s impressive professional journey spans forty-one years. His clinical expertise covers the treatment of celiac disease, colon polyps, colorectal cancer, constipation, Crohn’s disease, diarrhea, dysphagia, eosinophilic esophagitis, gastritis, inflammatory bowel disease, irritable bowel syndrome, peptic ulcer, malabsorption, iron-deficiency anemia, stomach cancer, and ulcerative colitis. Dr. Goldberg is considered an expert in upper GI endoscopy, colonoscopy, and polypectomy. Dr. Goldberg authored a book called The Inside Tract: The Complete Guide to Digestive Disorders, which was published in 1982. Also, his work has been published in peer-reviewed journals. For more information, please visit http://myrongoldberg.com/www.myrongoldberg.com/About_Dr._Goldberg.html.
Myron D. Goldberg, MD, FACP, FACG, FASGE, FAGA, attended the Albert Einstein College of Medicine in New York, and received his medical degree in 1971. Then, he served his internship at Maimonides Medical Center (1971-1972). Furthermore, he conducted his internal medicine residencies at Montefiore Medical Center (1972-1973) and Lenox Hill Hospital (1973-1974). He then served voluntary active duty in the US Air Force Medical Corps (1973-1976). In addition, Dr. Goldberg completed his fellowship training in gastroenterology at Columbia Presbyterian Medical Center and Lenox Hill Hospital (1976-1978). He received board certification in internal medicine and gastroenterology from the American Board of Internal Medicine. He is a Fellow of the American College of Physicians, the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy. Dr. Goldberg’s practice is recognized by the American Society for Gastrointestinal Endoscopy for his excellent standards. He was named a Castle Connolly Top doctor and received a Physicians recognition Award with Commendation from the American Medical Association. For more information about Dr. Myron D. Goldberg, please visit https://www.findatopdoc.com/doctor/3635434-Myron-Goldberg-Gastroenterologist.
0 notes