#hyperkalemia
Text
Had a pt today who had hyperkalemia. She is a diabetic and was getting heparin for DVT prophylaxis, which can cause type 4 renal tubular acidosis. So her heparin was stopped.
Hyperkalemia that causes EKG changes should be treated with calcium gluconate (or calcium chloride), insulin, Kayexalate. Calcium chloride has more elemental calcium than calcium gluconate, so you would give less calcium chloride if you gave that instead of calcium gluconate. The dose of calcium chloride is 1 gram. The dose of calcium gluconate is 2 to 3 grams. The calcium is simply cardioprotective. Insulin just temporarily shifts potassium into the cells. Dialysis emergently removes potassium from the body. Kayexalate gets rid of potassium in the stool, but can also cause intestinal necrosis (the premixed formulation). I didn't know that! Lokelma and Patiromer (Veltassa®) can be used to get rid of potassium in the stool, and they don't cause intestinal necrosis! We don't have Lokelma or Veltassa at my hospital. Lokelma is really expensive.
You should also correct acidosis in pts who have hyperkalemia by giving them bicarbonate.
I don't remember anything about renal tubular acidosis, but risk factors for type 4 RTA: type 2 diabetes, overweight, older. It's a hyporenin, hypoaldosterone state.
10 notes
·
View notes
Text

Medicine - symptoms of HYPERKALEMIA = too much potassium in blood (negative effects).
Hiperkaliemia, hiperkalemia, hiperpotasemia – u człowieka stan, w którym stężenie jonów potasowych K+ w surowicy krwi przekracza przyjętą (umowną) wartość 5,5 mmol/l.
#hyperkalemia#po angielsku#in english#objawy#symptoms#medycyna#chart#information#medicine#po polsku#polski#polish
2 notes
·
View notes
Text
Treating Hyperkalemia: Balancing Diet and Mediations
When you’ve gotten hyperkalemia, you’ve gotten an excessive amount of potassium in your blood. You can decrease your potassium ranges with weight-reduction plan, drugs, or each.
What Your Doctor May Recommend
Your physician or well being care supplier will aid you create a therapy plan that’s best for you.
You might must observe a weight-reduction plan that’s low in potassium. You might have…
View On WordPress
0 notes
Text

yeah ill fucking bet
16 notes
·
View notes
Text
i just saw a tik tok of a nurse explaining what to do in case of hyperkalemia. the first comment on the video?
"good thing im in psych cuz i dont get all of that" and then a bunch of people agreeing
like...you do realize...the psych ward is STILL A WARD IN A HOSPITAL, psych patients STILL DESERVE AND NEED THE BASIC CARE ALL OTHER FACILITIES PROVIDE, and electrolyte imbalances ARE something to watch out for (can be the underlying cause for acute psych symptoms like confusion)?????
im so tired of psychiatry being undervalued like this, and seeing people like that working in the system with vulnerable patients makes me sick
#i wouldve commented this on the video where these idiots were saying this shit#but refreshed the page accidentaly and cant find it#like. if i cant trust psych nurses to know how to act in an emergency like hyperkalemia what am i supposed to do??#the amount of times i got yelled at (yes yelled at!) for sending a pt for IV fluids due to high CPK count BY PSYCH NURSES#i NEVER like to undermine nurses. theyre the core of running a hospital#but that instance is where i draw the line and say im the doctor and this is what needs to be done#just yesterday i sent a patient for xrays after a fall#after the nurses tried to insist the pt was faking their pain#and lo and behold they had a broken bone!#working in psych has made me so distrustful of others#all i want is to take good care of my patients but with zero support i it feels impossible#burrito talks medicine#delete later
10 notes
·
View notes
Video
youtube
CRITICAL CARE SCENARIO OF RENAL FAILURE
CRITICAL CARE SCENARIO OF RENAL FAILURE MRCS B OSCE - MOCK EXAM Bli medlem i kanalen för att få åtkomst till flera förmåner: https://www.youtube.com/channel/UCkkvon_blxinTHc7DGuYkpQ/join
#youtube#criticalcare renalfailure hyperkalemia cardiacarrest medicine doctor surgery health medical healthcare mrcs mrcsbosce femalesurgeon youtube
0 notes
Text
You know, my specialist prescribed me this before we were due to get my bloodwork results and now I'm wondering if we should've waited.
1 note
·
View note
Link
Potassium level is 3.5 to 5.2mEq/L
0 notes
Video
youtube
Effect of Hyperkalamia (High Blood potassium) on Heart
0 notes
Text
When caring for a patient in cardiac arrest, it is important to recognize reversible causes for the arrest and address them. This is especially important with PEA and asystole, which often have reversible underlying causes. The mnemonic Hs and Ts can help you to remember the reversible causes of cardiac arrest.
Hypovolemia
Hypoxia
Hydrogen ion excess (acidosis)
Hyper- or hypokalemia
Hypothermia
Toxins
Tamponade
Tension pneumothorax
Thrombosis (pulmonary embolism)
Thrombosis (myocardial infarction)
In patients with metabolic acidosis, the administration of an initial dose of sodium bicarbonate (1 mEq/kg) may be indicated. If administering sodium bicarbonate, ensure adequate ventilation for removal of carbon dioxide or sodium bicarbonate may worsen intracellular and tissue acidosis.
Suspect hyperkalemia in all patients with acute or chronic renal failure and in those who had a wide-complex ventricular rhythm and tall, peaked T waves on ECG before arrest. Several measures may be taken to reduce potassium levels, including administering sodium bicarbonate, glucose and insulin, or nebulized albuterol. Sodium bicarbonate is preferred in patients with cardiac arrest caused by hyperkalemia because it causes a rapid shift in serum potassium level. Other therapies take much longer to work.
Suspect hypokalemia in patients with dehydration or overuse of diuretics. In hypokalemia, flat T waves, prominent U waves and possibly prolonged QT intervals may be seen on ECG before arrest. Treatment is with intravenous (IV) administration of a dilute solution of potassium chloride.
8 notes
·
View notes
Text
vegans can you please lmk how much potassium you get from one meal??? im worried i get too much and i limit myself to like 1-2 meals a day (that arent filling) bc of it
i get around 2400-2700 mg of potassium with a meal, mostly from quinoa. bc one cup of quinoa has like 1200 mg of potassium (which is fucking insane)
just wanna know if other vegans are in the same ballpark as me or if i have way too much
#vegan#veganism#btw ive been vegan for like 8 years now i just never really focused on it too much#and im worried about hyperkalemia#plant based#<- only tagging bc plant based people are more health cinscious meanwhile vegans are more ethics based
1 note
·
View note
Text
Good news, it’s not a heart attack. It’s hyperkalemia.
#but that does mean I now have a problem with my kidneys#I feel like every 3 months I need to jumpstart them#something is always wrong#but I can deal with this. don’t know what’s CAUSING it or why I get it so often#but this is easy#lots of water lots of vitamins and some luck#lol “’Is it a Heart Attack or Hyperkalemia: The Hot New Game’#(Im not a gamer obviously)#although one of the side effects of Hyperkalemia is severe heart problems and increased risk of cardiac arrest so.#BUT ON THE BRIGHT SIDE#everything is fine
1 note
·
View note
Text
Hyperkalemia: Use Good Nutritional Sense
About 3 million Americans have excessive potassium, or hyperkalemia, due to kidney illness, coronary heart failure, or poorly managed diabetes. Potassium is a vital nutrient that helps your nerves and muscle tissues, together with your coronary heart, work the appropriate method. But you probably have an excessive amount of in your blood, it may be harmful and result in coronary heart issues.
If…
View On WordPress
0 notes
Text
Hyperkalemia ecg findings

The PR and QRS intervals may lengthen.3įurther elevations in potassium levels can lead to sinoatrial and atrioventricular conduction blocks with resulting escape beats and rhythms. As a result, P-wave amplitude decreases and P waves flatten and may disappear altogether. Atrial tissue is more sensitive to this effect than ventricular tissue. In particular, the inverted lateral T waves associated with left ventricular hypertrophy may pseudonormalize.2 These T-wave changes result from acceleration of the terminal repolarization of the myocytes and are often most pronounced in the precordial leads.Īs potassium levels rise further, cardiac conduction between myocytes is suppressed. However, in most patients, the ECG shows largeamplitude T waves rather than the classic tented T waves.1 In addition, the direction of the T wave may change. The earliest ECG signs of hyperkalemia are “tented” T waves, which are classically described as tall, symmetrically narrow, and peaked (see Figure 2). Pseudohyperkalemia results when potassium is released from platelets in the setting of thrombocytosis. Spuriously elevated potassium levels can occur with hemolysis during phlebotomy. Methamphetamine use can cause renal failure. The causes of hyperkalemia include acute and chronic renal failure, diabetic ketoacidosis, mineralocorticoid deficiency, type IV renal tubular acidosis, medications (angiotensin-converting enzyme inhibitors, potassium-sparing diuretics, lithium, NSAIDs, and beta-adrenergic antagonists), acute digoxin toxicity, rhabdomyolysis, burns, crush injuries, and severe dehydration-as well as any combination of the above. As a result, changes in serum potassium level can have dramatic effects on cardiac cell conduction and, consequently, on the ECG. Potassium, the predominant intracellular cation, plays an important role in maintenance of the potential across the cellular membrane, as well as in depolarization and repolarization of myocytes and neurons. Although this response to bicarbonate might also be associated with a toxicologic insult (such as can cause ventricular tachycardia), the finding of peaked T waves points strongly to an elevated serum potassium level. The patient’s ECG response to bicarbonate makes primary cardiac disease and ischemia less likely. The findings on these 2 ECGs suggest hyperkalemia, B. The second ECG (Figure 2), obtained after administration of bicarbonate, reveals slowing of the heart rate, narrowing of the QRS complex, and the presence of “tented,” or peaked, T waves, primarily in the precordial leads. The potential causes of ventricular tachycardia are numerous among them are primary cardiac disease ischemia and other primary noncardiac disorders, such as toxicologic insults and electrolyte abnormalities. The first ECG reveals a regular wide-complex tachycardia of unclear origin (Figure 1). The differential diagnosis for this finding includes supraventricular tachycardia with aberrancy or bundle-branch block, pacemaker-mediated tachycardia, sodium channel blocker toxicity, hyperkalemia, preexcitation, and ventricular tachycardia. Which of the following diagnoses is best supported by the ECGs and clinical findings? Fifteen minutes later, a second ECG is obtained (B). After arterial blood gas measurement reveals significant metabolic acidosis (pH, 7.08 PO2, 217 mm Hg PCO2, 22 mm Hg), sodium bicarbonate is administered. Initial treatment includes oxygen, intravenous fluids, and lidocaine the patient’s condition does not change. Neurologic examination demonstrates mild diffuse symmetric weakness.Īn ECG is obtained (A). A 2/6 systolic murmur is audible. Abdomen is soft and nontender. Heart rate is 152 beats per minute and regular respiration rate, 24 breaths per minute blood pressure, 142/68 mm Hg. Pulse oximetry shows that oxygen saturation is 95% on room air. He has no history of cardiac disorders, and he denies chest pain, palpitations, and abdominal pain. A 34-year-old man presents to the emergency department with progressive, generalized weakness and shortness of breath that began 2 weeks earlier.

0 notes
Text
Hyperkalemic Periodic Paralysis (HYPP)
Breeds with HYPP; Quarter Horses, American Paint Horses, Appaloosas, and Quarter Horse Crosses.
HYPP
"An inherited disease of the muscle, caused by a genetic defect. A mutation in the sodium channel gene. Sodium channels are pores in the muscle cell membrane which control contraction of the muscle fibers. When the defective sodium channel gene is present, the channel becomes “leaky” and makes the muscle overly excitable and contract involuntarily. The channel become “leaky” when potassium levels fluctuate in the blood. This may occur with fasting followed by consumption of a high potassium feed such as alfalfa. Hyperkalemia, which is an excessive amount of potassium in the blood, causes the muscles in the horse to contract more readily than normal. This makes the horse susceptible to sporadic episodes of muscle tremors or paralysis."
GENOTYPE
HYPP Positive= H/N and H/H
HYPP Negative= HYPP N/N
HYPP horses with H/N genotype means they are heterozygous carriers, carrying one copy of the HYPP gene. If you bred a mare who is H/N to a stallion who is N/N, you would have about a 50% chance the foal is H/N as well. However if you bred an H/N mare to an H/N stallion you will have about a 25% chance the foal being N/N, a 50% chance it will be H/N, and a 25% chance it will be H/H.
HYPP horses with the H/H genotype means it is homozygous, carrying both copies of the HYPP gene. 100% passing the HYPP gene to it's offspring.
I made a thing in case it helps the visual learners out there
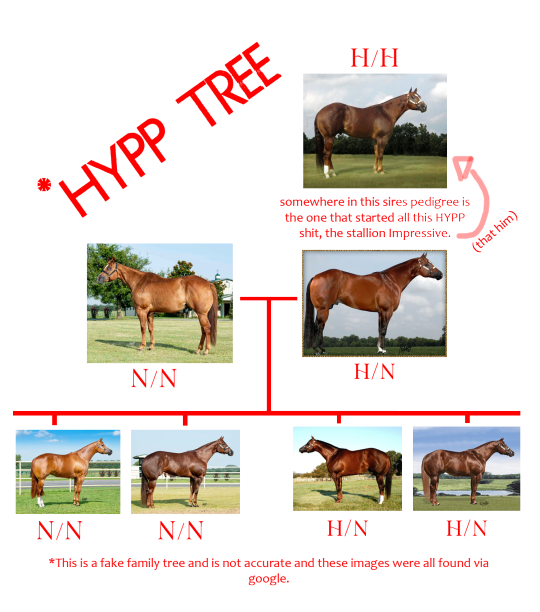
IMPRESSIVE (but not really)
Let's talk about the QH stallion, Impressive. All horses that have a HYPP positive gene of any kind, all descend from this horse. Impressive sired 2,250 foals and they estimate he has around 50,000 living descendants. No dilution of lineage will remove HYPP, as it is a dominant trait and will show whether you are 5 generations back or 2.
HYPP SYMPTOMS
HYPP varies in severity, it's not always equal and every horse may have different reactions. HYPP can be confused for tying-up or even colic, they may have difficulty breathing, muscle tremors, sweating, weakness, tremors. In more severe cases the horse may collapse from paralysis of the muscles in the airway and can result in sudden death.
Not every horse who is HYPP positive may display symptoms, making this disease sometimes hard to detect.
IS IT CURABLE?
No. HYPP may be managed with diet and certain medicines for maintenance but it cannot be cured. H/H positive horses have poor prognosis and can be much more difficult to manage.
VIDEOS OF HYPP ATTACKS
CW: Horses in distress, videos may be hard to watch for some.
Video 1
Video 2
Video 3
Video 4
Video 5
Sources (and if you want to read more); AAEP , UCDavis, Tri-State
Is there anything I forgot? Anything to add? Just covering the basics of this disease and what it does to these horses.
248 notes
·
View notes
Text
Lazarus phenomenon
Autoresuscitation is a phenomenon of the heart during which it can resume its spontaneous activity and generate circulation. It was described for the first time by K. Linko in 1982 as a recovery after discontinued cardiopulmonary resuscitation (CPR). J.G. Bray named the recovery from death the Lazarus phenomenon in 1993. It is based on a biblical story of Jesus’ resurrection of Lazarus four days after confirmation of his death. Up to the end of 2022, 76 cases (coming from 27 countries) of spontaneous recovery after death were reported; among them, 10 occurred in children. The youngest patient was 9 months old, and the oldest was 97 years old. The longest resuscitation lasted 90 min, but the shortest was 6 min. Cardiac arrest occurred in and out of the hospital. The majority of the patients suffered from many diseases. In most cases of the Lazarus phenomenon, the observed rhythms at cardiac arrest were non-shockable (Asystole, PEA). Survival time after death ranged from minutes to hours, days, and even months. Six patients with the Lazarus phenomenon reached full recovery without neurological impairment. Some of the causes leading to autoresuscitation presented here are hyperventilation and alkalosis, auto-PEEP, delayed drug action, hypothermia, intoxication, metabolic disorders (hyperkalemia), and unobserved minimal vital signs. To avoid Lazarus Syndrome, it is recommended that the patient be monitored for 10 min after discontinuing CPR. Knowledge about this phenomenon should be disseminated in the medical community in order to improve the reporting of such cases. The probability of autoresuscitation among older people is possible.
National Library of Medicine
8 notes
·
View notes