#long covid treatment
Link
by Hannah E. Davis, Lisa McCorkell, Julia Moore Vogel & Eric J. Topol
—
Fig. 1: Long COVID symptoms and the impacts on numerous organs with differing pathology
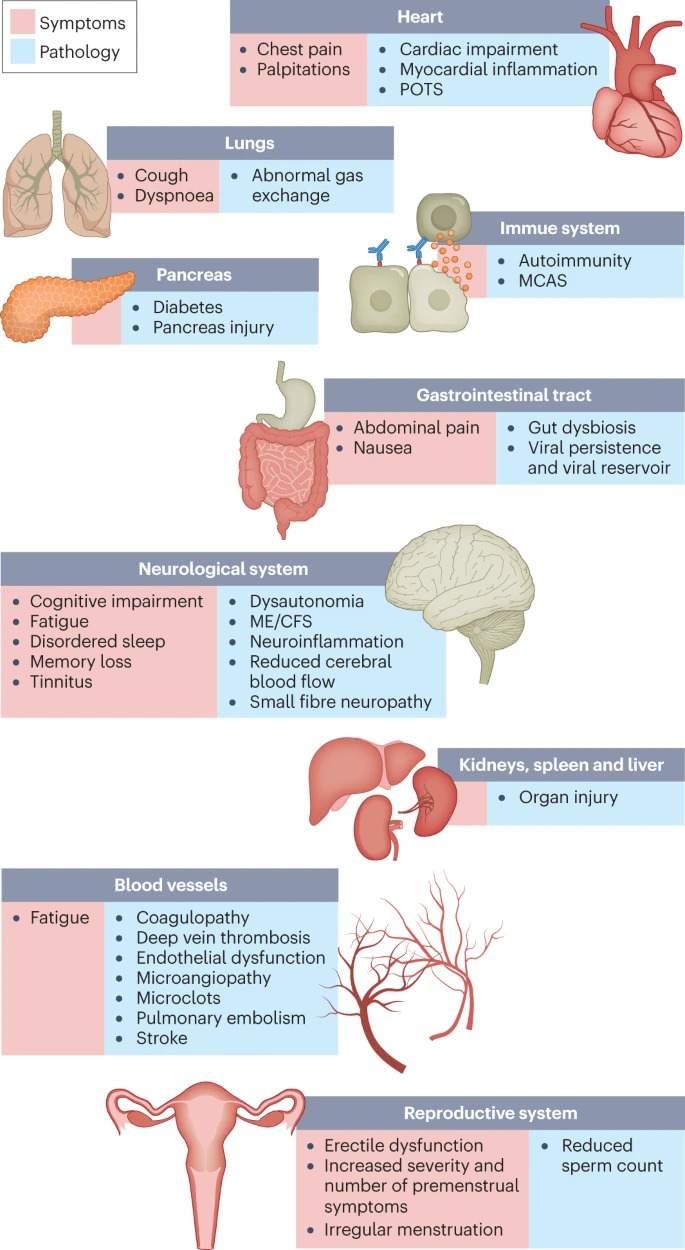
Fig. 3: Hypothesized mechanisms of long COVID pathogenesis
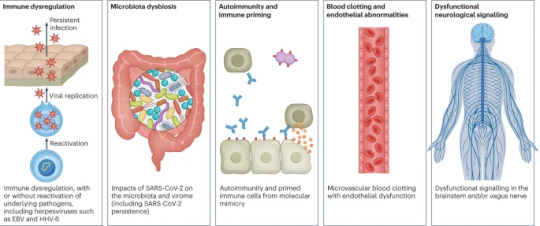
There are several hypothesized mechanisms for long COVID pathogenesis, including immune dysregulation, microbiota disruption, autoimmunity, clotting and endothelial abnormality, and dysfunctional neurological signalling. EBV, Epstein–Barr virus; HHV-6, human herpesvirus 6; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
—
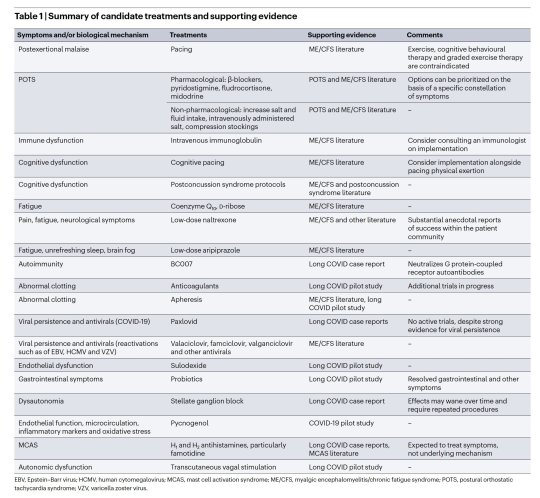
Table summarizing candidate treatment options for different components of long Covid / view in full here: https://www.nature.com/articles/s41579-022-00846-2/tables/1
15 notes
·
View notes
Link
Following perispinal etanercept administration there was immediate neurological improvement. At 24 hours there were remarkable reductions in chronic post-COVID-19 fatigue and depression, and significant measureable improvements in cognition, executive function, phonemic verbal fluency, balance, gait, upper limb coordination and grip strength. Cognition, depression and fatigue were examined at 29 days; each remained substantially improved.
Conclusion
Perispinal etanercept is a promising treatment for the chronic neurologic dysfunction that may persist after resolution of acute COVID-19, including chronic cognitive dysfunction, fatigue, and depression. These results suggest that long COVID brain neuroinflammation is a potentially reversible pathology and viable treatment target. In view of the increasing unmet medical need, clinical trials of perispinal etanercept for long COVID are urgently necessary. The robust results of the present case suggest that perispinal etanercept clinical trials studying long COVID populations with severe fatigue, depression and cognitive dysfunction may have improved ability to detect a treatment effect. Positron emission tomographic methods that image brain microglial activation and measurements of cerebrospinal fluid proinflammatory cytokines may be useful for patient selection and correlation with treatment effects, as well as provide insight into the underlying pathophysiology.
1 note
·
View note
Text
What is Chronic Fatigue? Can it be cured?

Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a serious, long-term illness that affects many body systems. People with ME/CFS are often not able to do their usual activities and enjoy their life. People with chronic fatigue syndrome (CFS) usually have tremendous difficulty doing the things that many of us take for granted. We usually don’t think twice about getting dressed or driving to some place provided we had enough rest. However, this is not the case for someone who is chronically fatigued. Sometimes ME/CFS can even confine a person to bed. People with ME/CFS have severe fatigue and sleep problems.
Chronic fatigue syndrome occurs more commonly in women. The cause of this condition is unknown, but may include environmental or genetic factors. The main symptom is fatigue for over 6 months. The fatigue often worsens with activity and does not improve with rest. There is not one Chronic fatigue syndrome treatment that fits all. Latest news on Chronic Fatigue Syndrome compares it to Long Covid.
How long does chronic fatigue last?
For some it can be shorter. Unfortunately, for most it can last for long periods of time and they are unable to recover. However, some symptoms can be treated or managed to provide relief. New treatments for chronic fatigue syndrome include: Targeted supplementation with products that increase ATP and energy that can help reduce fatigue. Brands such as; Bodybio, Biopure, Cellcore, and Quicksilver Scientific offer supplements like glutathione, minerals, and fatty acids that help improve the cell membrane function and fatigue. There is a product called Oxaloacetate made by Benegene that has some great clinical studies showing improvement in energy and lowered fatigue.
Is there a test for Chronic Fatigue Syndrome?
Currently there are no tests to determine if someone has CFS. New tests are being developed but they are not commercially available. Many patients look for top chronic fatigue doctors. It can be extremely expensive and hard to get appointments with CFS specialists. This condition can be very frustrating for many reasons. First, rest does little to nothing to suppress CFS symptoms. Second, the causes of chronic fatigue syndrome are not well known (though a weakened immune system, hormonal imbalances, viral infections, and stress may contribute). HealthBuyerClub.com was created to help those dealing with this chronic illness, along with many others, afford the treatments and medical devices they need. We offer up to 40% in savings on over 55 physician formulas brands and technology. We also have a referral program. Join our club today for FREE and start saving today!
0 notes
Text
Other viruses offer clues to the mystery of long-term COVID
Other viruses offer clues to the mystery of long-term COVID
August 18, 2022 – Researchers hunt a range of potential culprits in the race to find the causes of long-term COVID. They agree on some things: There will be a number of different causes and the symptoms will vary greatly from case to case.
The two leading theories: the persistence of the coronavirus that causes COVID-19, and an overactive immune response.
There is some evidence that the…

View On WordPress
#covid#COVID-19#how long does covid last#long covid#long covid over#long covid studies#long covid treatment#long covid what to know#long term effects of covid#signs of covid#signs of long covid#symptoms of covid#symptoms of long covid
0 notes
Text
Stress hormone cortisol may explain long COVID—and how to treat it, Yale researchers say
Stress hormone cortisol may explain long COVID—and how to treat it, Yale researchers say
Public health officials are scrambling to understand long COVID, the condition in which patients report symptoms like fatigue, muscle weakness and ‘brain fog’ months after infection. A new study released Wednesday shows one way doctors might diagnose who has the chronic condition and indicates a possible way to treat it.
Researchers from the Yale School of Medicine and the Icahn School of…

View On WordPress
#COVID#covid and cortisol levels#covid cortisol#covid news#covid stress hormone#covid study#Long COVID#long covid causes#long covid news#long covid study#long covid treatment#new covid study#what is long covid
0 notes
Text
Long COVID Doubles Risk of Some Serious Outcomes in Children, Teens: Study
Long COVID Doubles Risk of Some Serious Outcomes in Children, Teens: Study
Aug. 4, 2022 – CDC researchers report that children and teenagers with long COVID have about twice the risk of getting serious outcomes, compared to others without COVID.
Heart inflammation; a blood clot in the lung; or a blood clot in the lower leg, thigh, or pelvis were the most common bad outcomes in a new study. Even though the risk was higher for these and some other serious events, the…
View On WordPress
#CDC#cdc covid#cdc covid kids#cdc covid study#cdc covid teens#cdc long covid#Covid Vaccine#covid vaccine to prevent long covid#do covid vaccines prevent long covid#effects of long covid#how long does long covid last#how to prevent long covid#kids and long covid#long covid about#long covid treatment#long covid what to know#teens and long covid#what is long covid
0 notes
Text
Why are ppl scared to call it what it is and say we’re still going thru covid on top of seasonal illness. Like. That’s pretty important right. I was watching the news and they were like oh yeah we have an unprecedented number of flu cases “as well as other sicknesses” without actually saying Covid. No announcement abt vaccinations or masking or anything. Also if I hear someone joking abt “war flashbacks” for mentioning covid I fucking hate u
#source: most of my family members are nurses and it was so bad for one of them they had to be put on a ventilator. in the hospital they#worked at. looking back I think I had a reason to feel a little offput by the shows of support early pandemic#with people tying blue ribbons around trees and lighting signs blue to support healthcare workers#I get that it was supposed to be moral support when we couldn’t do anything but follow health advisories#and it did matter to make them feel uplifted and do something than nothing. im not gonna deny that#but. you can still help now. u know that right. you still have a responsibility here#u can still mask up. u can still get vaxxed and call in sick to avoid infecting others#don’t leave it on healthcare workers to pick up the pieces just because they were doing it before. do u think they had a choice?#nobody likes picking up the slack for someone else and now that we have more tools to do smth couldn’t we just. do it????#im not a virologist but i also feel like continuing to let it get worse by letting more mutations develop#could continue to set us back since this virus is pretty good at fucking us up long term and finding new ways to do that#while there are ppl still researching covid which is STILL A RELATIVELY NEW VIRUS. and studying possible treatment and cures#yapping#vent
388 notes
·
View notes
Text
Don't feel bad if you haven't recovered from a condition your doctor says is "very treatable." Doctors and society in general often underestimate how debilitating pain, physical illnesses, and mental health problems can be. Don't listen to anyone who insinuates that you don't want to get better or aren't committed to your treatment because your symptoms haven't improved much. Take as long as you need to heal.
#long covid#chronic illness#spoonie#disability#pots#ibs#brain fog#mental health#treatment#post viral syndrome
4K notes
·
View notes
Link
0 notes
Link
From May 2022.
Both parasympathetic excess and sympathetic withdrawal are separate and treatable autonomic dysfunctions and autonomic treatment significantly reduces the prevalence of autonomic symptoms. Conclusion. SARS-CoV-2, via its oxidative stress, can lead to P&S (parasympathetic and sympathetic) dysfunction, which, in turn, affects the control and coordination of all systems throughout the whole body and may explain all of the symptoms of long-COVID syndrome. Autonomic therapy leads to positive outcomes and patient quality of life may be restored.
The initial respiratory compromise, due to the COVID-19 virus, on the medullary respiratory control centers (including the pre-Bötzinger complex) [9,10,11] may be so dramatic that P&S symptoms and signs are often overlooked or misunderstood.
Respiratory pacing from the pre-Bötzinger complex involves (1) vagus nerve afferents, among other brainstem structures; (2) feedback from the COVID-19-damaged lung; (3) aortic and carotid chemo-, baro-, and vagal receptors; and (4) medullary chemoreceptors. All involving P&S nerves [9,12]. Brainstem cardiorespiratory centers (e.g., the Nucleus Tractus Solitarius, Dorsal Vagal Motor Nucleus, and Nucleus Ambiguus, all of which are autonomic nuclei) are also implicated in COVID-19 infection [13]. Furthermore, sympathetic involvement in cytokine storms [14,15,16,17] and the angiotensin system [18,19], and parasympathetic involvement in immune function [20,21,22], provides further evidence of P&S compromise in COVID-19 infections. Any resulting damage to these nerves further implicates P&S dysfunction in long-COVID syndrome.
Long-COVID symptoms [23] may be explained by a pro-inflammatory state with oxidative stress and P&S dysfunction.
Long COVID is characterized by parasympathetic excess and alpha-sympathetic withdrawal.
Anti-cholinergic therapy may relieve post-COVID-19 symptoms associated with parasympathetic excess. This is hypothesis generating and further trials are needed.
Based on their P&S test results, the patients were prescribed therapy, typically for both sympathetic withdrawal (and associated orthostatic dysfunction) and for parasympathetic excess. Therapy for sympathetic withdrawal (after ruling out vascular causes) typically included: (1) 2.5 mg, tid, of Midodrine (ProAmatine, an alpha-adrenergic antagonist); and (2) up to 600 mg, tid, of Alpha-Lipoic Acid (an antioxidant selective for nerves [29,30]). Therapy for parasympathetic excess included: (1) 10 mg, qd, of Nortriptyline (as a low-dose anti-cholinergic), and (2) up to 40 minutes of low-and-slow exercise.
In our findings, long COVID is largely characterized by parasympathetic excess and sympathetic withdrawal. Both potentially contributing to hypoperfusion of the brain and all structures above and around the heart. Pre-COVID-19 infection, patients presented to the clinics with more sympathetic withdrawal (45.7%) than parasympathetic excess (27.0%). Post-COVID-19 infection, these patients presented with that ratio reversed (36.2% and 46.7%, respectively). The etiology of this is not well known; however, parasympathetic excess may be more prominent post-COVID-19, due to an over-active immune system, which the parasympathetics help to control and coordinate and leads to parasympathetic excess.
Orthostatic dysfunction is caused by poor vasoconstriction due to alpha-adrenergic (sympathetic) dysfunction, known as sympathetic withdrawal [5]. Poor perfusion and dysfunction are exacerbated by the effect of COVID-19 on the lungs.
Both parasympathetic excess and sympathetic withdrawal are separate and treatable dysfunctions. As in this study, parasympathetic excess was treated, pharmaceutically, with anti-cholinergics (e.g., Nortriptyline, see the Methods Section) [31] and sympathetic withdrawal was treated, pharmaceutically, with oral vasoactives (e.g., Midodrine, see the Methods Section).
Traditionally, upon COVID-19 infection, there is a marked increase in the resting sympathetic activity and a decrease in anti-inflammatory resting parasympathetic activity [16], causing a high (resting) sympathovagal balance in all patients. However, in post-COVID-19 syndrome patients, after 12 weeks or more, our data shows that there is a significant percentage of patients that develop a parasympathetic dominance as indicated by the low (resting) sympathovagal balance. This is also indicative of increasing and prolonged parasympathetic activity. Parasympathetic activation is meant to be protective; including, since the parasympathetics are anti-inflammatory. However, prolonged and increased parasympathetic activity, especially in response to stressors, seems to exaggerate sympathetic inflammatory activity. Within this cohort, and anecdotally with the vast majority of our patients, anti-cholinergic therapy relieves parasympathetic excess. Further studies are required to elaborate whether anti-cholinergic therapy may relieve post-COVID-19 symptoms.
Further decreases in cerebral perfusion may lead to “adrenaline storms”, which cycle anxiety-like symptoms, including shortness of breath and palpitations which may cause chest pressure or chest pain. The effects of sympathetic withdrawal and orthostatic dysfunction are exacerbated by parasympathetic excess, which may limit or decrease the heart rate and blood pressure, reducing cerebral perfusion. The decrease in BP is also associated with excessive vasodilation from parasympathetic excess.
If the parasympathetics increase in response to a stress (known as parasympathetic excess), the result is a secondary sympathetic excess [5]. Our findings of prolonged parasympathetic excess in long-COVID patients appears to prolong sympathetic excess responses causing more and chronic symptoms, suggesting that this may be a mechanism contributing to long-COVID syndrome.
Pharmaceutical therapy for P&S dysfunction (anti-cholinergics for parasympathetic excess [28] and oral vasoactives for sympathetic withdrawal [39]) needs to be very low to prevent additional symptoms, thereby exacerbating P&S dysfunction.
#covid effects#long covid#dysautonomia#orthostatic intolerance#autonomic nervous system#POTS Syndrome#OCHOS Syndrome#parasympathetic#sympathetic#autonomic therapy#science journal#long covid treatment
0 notes
Text
If I do not test negative in the next three days, I will be creating an incident. If I miss the Cuda game on Wednesday I will create such a situation. Yes I caught Covid at either a Sharks or Cuda game, yes I still love them, it's a toxic relationship where everyone loses.
#finished paxlovid. if i get covid rebound i'm straight up defenestrating my material possessions#serotonin girl in red dot mp3#if i miss henry thrun hours at the reef due to henry being called up that's ok but i still have to test negative to avoid tearing up my encl#osure#i'm so. fuck around and find out i DID want a break from my responsibilities and i got SMITED#obvi very lucky to not be hospitalized and to be getting better and to likely not develop long covid due to the treatment available etc etc#counting my blessing. also very bored and crazed#fresno oilers.txt#covid cw //
34 notes
·
View notes
Text
What is Chronic Fatigue? Can it be cured?
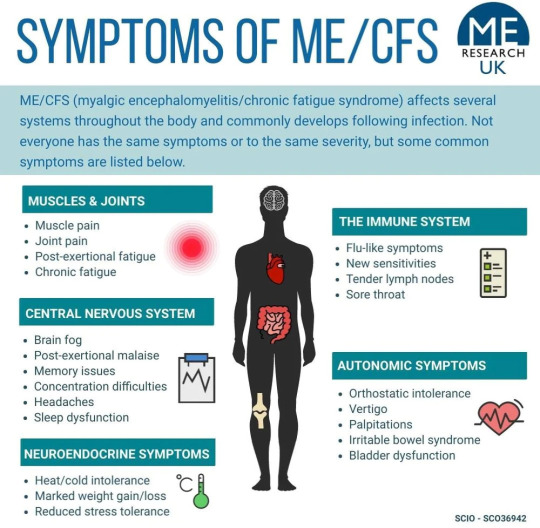
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a serious, long-term illness that affects many body systems. People with ME/CFS are often not able to do their usual activities and enjoy their life. People with chronic fatigue syndrome (CFS) usually have tremendous difficulty doing the things that many of us take for granted. We usually don’t think twice about getting dressed or driving to some place provided we had enough rest. However, this is not the case for someone who is chronically fatigued. Sometimes ME/CFS can even confine a person to bed. People with ME/CFS have severe fatigue and sleep problems.
Chronic fatigue syndrome occurs more commonly in women. The cause of this condition is unknown, but may include environmental or genetic factors. The main symptom is fatigue for over 6 months. The fatigue often worsens with activity and does not improve with rest. There is not one Chronic fatigue syndrome treatment that fits all. Latest news on Chronic Fatigue Syndrome compares it to Long Covid.
How long does chronic fatigue last?
For some it can be shorter. Unfortunately, for most it can last for long periods of time and they are unable to recover. However, some symptoms can be treated or managed to provide relief. New treatments for chronic fatigue syndrome include: Targeted supplementation with products that increase ATP and energy that can help reduce fatigue. Brands such as; Bodybio, Biopure, Cellcore, and Quicksilver Scientific offer supplements like glutathione, minerals, and fatty acids that help improve the cell membrane function and fatigue. There is a product called Oxaloacetate made by Benegene that has some great clinical studies showing improvement in energy and lowered fatigue.
Is there a test for Chronic Fatigue Syndrome?
Currently there are no tests to determine if someone has CFS. New tests are being developed but they are not commercially available. Many patients look for top chronic fatigue doctors. It can be extremely expensive and hard to get appointments with CFS specialists. This condition can be very frustrating for many reasons. First, rest does little to nothing to suppress CFS symptoms. Second, the causes of chronic fatigue syndrome are not well known (though a weakened immune system, hormonal imbalances, viral infections, and stress may contribute). HealthBuyerClub.com was created to help those dealing with this chronic illness, along with many others, afford the treatments and medical devices they need. We offer up to 40% in savings on over 55 physician formulas brands and technology. We also have a referral program.
Join our club today for FREE and start saving today!
0 notes
Text
Diagnosing children with long-term COVID can be tricky: experts
Diagnosing children with long-term COVID can be tricky: experts
August 15, 2022 – When Spencer Siedlecki contracted COVID-19 in March 2021, he was ill for weeks with extreme fatigue, fever, sore throat, severe headache, nausea and eventually pneumonia.
That was scary enough for the then 13-year-old and his parents, who live in Ohio. More than a year later, Spencer still had many of the symptoms and, more alarmingly, the once-healthy teenager had… postural…
View On WordPress
#children and long covid#coping with long covid in teens#drawing long covid children#how do you know if you have covid for a long time?#how to deal with long covid#how to diagnose long covid?#long covid#long covid characters#long covid diagnosis#long covid kids#long covid treatment#signs of covid children#signs of long covid#tall covid teens#those most at risk for long-term covid#what is long covid
0 notes
Text
Hello! I'm here to bring you your breaking medical news from Twitter!
(No lie: I'm sure it depends who you're following, but I get really clear and specific COVID-19 info there.)
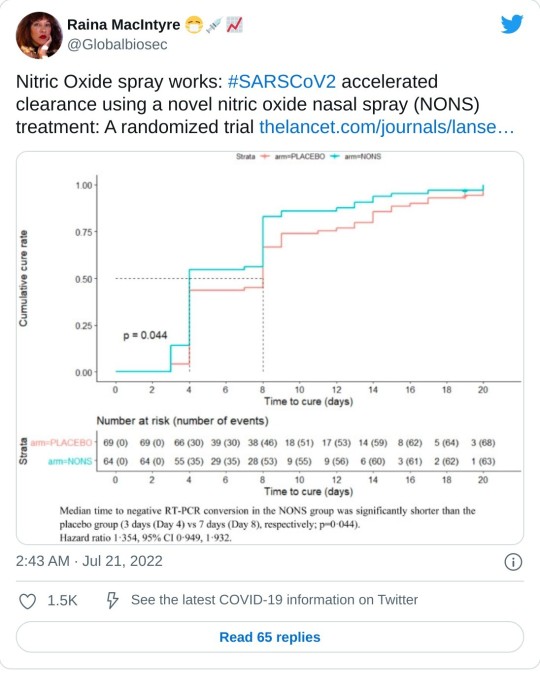
In this peer-reviewed, randomized, double-blind, multicentre, parallel group, placebo-controlled phase III clinical trial (which you KNOW I read through before sharing!), people with COVID-19 tested negative much sooner when using nitric oxide nasal spray.
It reduced the virus in their noses, which makes it less contagious AND means the patients get less sick.
(It specifically mentioned symptoms ending sooner, and it looked like a fair number of people on placebo were still having symptoms after 2½ weeks. I really hope that means it will significantly reduce the risk of long COVID, but of course it'll take months to find out for sure.)
And it apparently works on all (or just lots?) of airborne viruses.
More trials are apparently on the way, but you can buy these sprays over the counter - at least online.
464 notes
·
View notes
Text


Fellow Covid Long Hauler, here.
3 years 3 months in this hell
Surfing the internet, for Long Covid news, as usual, since I was “diagnosed” with this condition, and I noticed a few things.
I’m seeing and reading a lot of articles and “news” about Long Covid; not being real, may not be as bad as Influenza, Long Cold might be a thing too, etc.
Pay attention to wording. Words like “likely” “maybe” “may” “if” “yet”.
Long Covid “may” not be real
Flu “might be worse” than Long Covid
Long Cold, exists too, “likely”.
These people don’t sound too sure. Because they have no foundation, no proof. Pure speculation. So next time, fellow Long Hauler, if you see some dismissive piece of shit article, downplaying and invalidating our whole experience, just look at the wording. 🖤
And always always always check. your. sources
#chronic pain#chronically ill#covid#covid isn't over#covid19#create#long covid#art therapy#chronic illness#long haul#covid long hauler#long haulers#long hauler#chronic#chronic fatigue#send help#treatment#the cure#healthcare#health
7 notes
·
View notes