#primary research in healthcare
Text
Unveiling Cutting-Edge Insights from Primary Research in the Health Sector
In the rapidly evolving landscape of healthcare, staying at the forefront of innovation and understanding emerging trends is crucial for professionals and organizations alike. One of the most potent tools in achieving this is through primary research in the health sector. By conducting studies directly with patients, healthcare providers, and other stakeholders, researchers can uncover invaluable insights that shape the future of medicine, treatment protocols, and healthcare delivery. In this comprehensive guide, we delve into the significance of primary research in the health sector, its methodologies, and the groundbreaking insights it can reveal.
Understanding Primary Research in Healthcare
Primary research, also known as original research or primary data collection, involves gathering data directly from the source. In the context of healthcare, this often means conducting studies that involve direct interaction with patients, healthcare professionals, or healthcare systems. Unlike secondary research, which relies on existing data and literature, primary research generates new data, making it a potent tool for uncovering novel insights and addressing specific research questions.
Significance of Primary Research in Healthcare
Primary research plays a pivotal role in advancing medical knowledge and driving innovation in healthcare. Here’s why it’s so significant:
Uncovering New Discoveries: Primary research allows researchers to explore new hypotheses, identify patterns, and uncover previously unknown insights that can lead to breakthroughs in understanding diseases, treatments, and healthcare outcomes.
Customized Data Collection: Researchers can tailor data collection methods to suit their specific research objectives, ensuring that the information gathered is relevant and comprehensive.
Informing Evidence-Based Practice: By generating new evidence, primary research provides the foundation for evidence-based practice in healthcare. Clinicians and policymakers rely on this evidence to make informed decisions about patient care, treatment guidelines, and healthcare policies.
Addressing Gaps in Knowledge: Primary research helps fill gaps in existing knowledge by exploring areas that have not been extensively studied or understood. This is particularly important in niche fields or emerging areas of healthcare.
Driving Innovation and Improvement: Insights gained from primary research can inspire innovation in medical technologies, treatment modalities, and healthcare delivery models, ultimately leading to improved patient outcomes and experiences.
Methodologies in Primary Research
Primary research in the health sector employs various methodologies depending on the research question, objectives, and available resources. Some common methodologies include:
Surveys and Questionnaires: Surveys and questionnaires are widely used to gather data from a large number of participants. They can be administered in person, via mail, email, or online platforms and are useful for collecting both qualitative and quantitative data on a wide range of topics, including patient experiences, healthcare preferences, and treatment outcomes.
Interviews: In-depth interviews allow researchers to explore complex issues in greater detail by engaging directly with participants. Interviews can be structured, semi-structured, or unstructured, depending on the level of flexibility needed to probe specific topics of interest.
Focus Groups: Focus groups bring together a small group of participants to discuss specific topics or issues in a guided setting. They encourage interaction and collaboration among participants, allowing researchers to explore diverse perspectives and uncover underlying attitudes and beliefs.
Observational Studies: Observational studies involve observing participants in their natural environment to gather data on behaviors, interactions, and outcomes. This methodology is particularly useful for studying phenomena that cannot be manipulated or controlled in a laboratory setting.
Clinical Trials: Clinical trials are experimental studies that evaluate the efficacy and safety of new treatments, drugs, or interventions. They typically involve randomized control groups and rigorous protocols to ensure the validity and reliability of the findings.
Groundbreaking Insights from Primary Research
Primary research in the health sector has led to numerous groundbreaking insights that have transformed healthcare practice and policy. Here are just a few examples:
Personalized Medicine: By analyzing genetic data and biomarkers through primary research studies, researchers have made significant strides in personalized medicine, tailoring treatment approaches to individual patients based on their unique genetic makeup and characteristics.
Health Equity and Access: Primary research has shed light on disparities in healthcare access and outcomes among different demographic groups, informing efforts to address health equity and improve healthcare access for underserved populations
Patient-Centered Care: Through primary research on patient preferences, experiences, and outcomes, healthcare providers have embraced a patient-centered approach to care, emphasizing collaboration, communication, and shared decision-making between patients and providers.
Healthcare Technology: Primary research has fueled innovation in healthcare technology, leading to the development of telemedicine platforms, wearable devices, and digital health solutions that enhance remote monitoring, diagnosis, and treatment delivery.
Preventive Healthcare: Studies conducted through primary research have highlighted the importance of preventive healthcare measures, such as vaccinations, screenings, and lifestyle interventions, in reducing the burden of disease and improving population health outcomes.
Conclusion
Primary research in the health sector is a powerful tool for advancing medical knowledge, driving innovation, and improving healthcare outcomes. By engaging directly with patients, healthcare providers, and other stakeholders, researchers can uncover valuable insights that inform evidence-based practice, shape healthcare policies, and ultimately enhance the quality of care delivery. As the healthcare landscape continues to evolve, primary research will remain essential in addressing emerging challenges, driving progress, and ensuring the health and well-being of individuals and communities worldwide.
FAQs
What is primary research in the health sector?
Primary research in the health sector involves conducting studies directly with patients, healthcare professionals, or healthcare systems to gather new data and insights. It differs from secondary research, which relies on existing data and literature.
Why is primary research important in healthcare?
Primary research is crucial in healthcare for several reasons. It allows researchers to uncover new discoveries, inform evidence-based practice, address gaps in knowledge, drive innovation, and improve patient outcomes and experiences.
What are some common methodologies used in primary research in healthcare?
Common methodologies in primary research in healthcare include surveys and questionnaires, interviews, focus groups, observational studies, and clinical trials. These methodologies can be tailored to suit specific research objectives and questions.
How does primary research contribute to personalized medicine?
Primary research in healthcare, particularly through the analysis of genetic data and biomarkers, has advanced personalized medicine by tailoring treatment approaches to individual patients based on their unique characteristics and genetic makeup.
What insights has primary research provided in addressing health equity and access?
Primary research has shed light on disparities in healthcare access and outcomes among different demographic groups, informing efforts to address health equity and improve healthcare access for underserved populations.
#primary market research#primary research in health sector#primary market research services#primary research#primary research in healthcare
0 notes
Text
Primary Care Market Trends and Insights
Download FREE Sample: https://www.nextmsc.com/primary-care-market/request-sample
The Primary Care Market is a dynamic and crucial segment of the healthcare industry, focusing on the first point of contact for patients seeking medical attention. This market encompasses a range of services provided by general practitioners, family physicians, internists, and pediatricians, among others. As the healthcare landscape evolves, several key trends and insights are shaping the future of primary care:
Growing Demand for Preventive Care: With an increasing emphasis on preventive health measures, there is a rising demand for primary care services that focus on disease prevention, early detection, and health promotion. This shift is driven by a growing awareness of the benefits of proactive health management.
Integration of Technology: The integration of technology in primary care is transforming how services are delivered. Telemedicine, electronic health records (EHRs), and digital health tools are enhancing patient access to care, improving communication, and streamlining administrative processes.
Patient-Centered Care Models: There is a shift towards patient-centered care models that prioritize the needs and preferences of patients. This approach aims to improve patient satisfaction, outcomes, and overall experience by involving patients in decision-making and care planning.
Expansion of Primary Care Access: Efforts are being made to expand access to primary care services, particularly in underserved and rural areas. This includes the development of community health centers, mobile clinics, and collaborative care models that bridge gaps in healthcare delivery.
Focus on Chronic Disease Management: Primary care providers are increasingly focusing on managing chronic conditions such as diabetes, hypertension, and heart disease. Effective management of these conditions is essential for improving patient outcomes and reducing the burden on the healthcare system.
Healthcare Policy and Reimbursement Changes: Changes in healthcare policies and reimbursement models are impacting the primary care market. Value-based care initiatives and alternative payment models are driving shifts in how primary care services are funded and delivered.
Access Full Report: https://www.nextmsc.com/report/primary-care-market
As the primary care market continues to evolve, stakeholders must stay informed about these trends and adapt to the changing landscape to ensure the delivery of high-quality, accessible, and patient-centered care.
0 notes
Text
Market Research Done Right | Unimrkt Research
youtube
Unimrkt Research is a Market Research Outsourcing firm that helps global Market Research organizations with their primary and secondary research and support needs.
We offer a complementary range of research services, like Qualitative Market Research, Quantitative Market Research, Business Research and Research Support Functions.
Our primary market research methods like telephonic interviews and online surveys are top notch in the industry with 450+ CATI stations equipped with the state of the art technology and we serve our clients every time when it comes to understanding the market pain points.
Unimrkt takes pride in being recognized by its associates as upbeat, proficient, and principled in collecting and delivering hard-to-get specialized, quality data. Learn more: www.unimrkt.com
#unimrkt research#qualitative market research#business market research#market research firms#healthcare market research#survey programming#online survey company#primary market research#healthcare market research companies#market research company#Youtube
1 note
·
View note
Text
The Cass Report is fatally flawed in its methodology, and as a result, its recommendations are harmful. Speaking on behalf of TransActual, Keyne Walker said: “It undermines the legal competence of both children and adults to access medical treatment and dismisses almost all existing clinical evidence on trans people’s healthcare by applying impossible evidence standards which, if applied to other medicines would invalidate more than three quarters of the existing treatments used in paediatric care which, like puberty blockers, are currently being prescribed off-label.”
The report’s primary conclusions rest on excluding 98% of the relevant evidence on the safety and efficacy of puberty blockers and hormones for lack of blinding and controls. What this means is that they require studies in which some patients are given the treatment, and others are unknowingly given placebos. This is not only a clear breach of medical ethics and monstrous suggestion, but also impossible due to the obviousness of the impacts of puberty blockers and hormones.
The report also strays far beyond its scope and competence in recommending a review of adult services and in suggesting that young people ought to stay under the care of children and young people’s services until the age of 25. The latter is based on highly questionable understandings of brain development which have been repeatedly debunked as an oversimplification of the constant changes in human neurology over the course of our lives. This recommendation, especially in a context of an already broken system of care for both adults and children, has the potential to have a significant negative impact on the lives and wellbeing of trans people in the UK.
Underpinning this report is the idea that being trans is an undesirable outcome rather than a natural facet of human diversity. This is clear not only from the recommendations but also from the exclusion of trans researchers from the design of the review process and the links individual members of the research team have to anti-trans groups, which the Cass team were warned about.
Download the full briefing
233 notes
·
View notes
Text
Tapering patients on long-term opioid therapy results in more emergency department visits and hospitalizations, according to a large new study that found reduced opioid use was particularly disruptive to the healthcare of pain patients with diabetes and high blood pressure.
The study by researchers at University of California Davis is the latest to document the “unintended negative consequences” of policies that limit opioid prescribing. A previous study by the same research team found that tapering raises the risk of an overdose and mental health crisis.
In their latest study, UC Davis researchers analyzed health data for over 113,000 patients who were on opioid therapy for at least 12 months, comparing those who were not tapered to those who had their dose reduced by 15% or more.
Their findings, published in JAMA Network Open, showed that tapering significantly increased hospitalizations and ED visits, while at the same time reducing the number of primary care (PC) visits. Researchers think the latter is at least partially due to “ruptures in relationships” with primary care providers (PCPs) due to patient dissatisfaction with tapering. (Read more at link)
417 notes
·
View notes
Text
Also preserved on our archive
Report suggests potential excess mortality in the general population of up to 3% for the US by 2033 and 2.5% in the UK, the longest period of elevated peacetime excess mortality in the US
Key driver of excess mortality is the lingering impact of COVID-19; both as a direct cause of death, and as a contributor to cardiovascular mortality
Reducing the impact of COVID-19 on elderly and vulnerable populations will be key to excess mortality returning to zero
Zurich, 16 September 2024 – Four years after the peak of the COVID-19 pandemic, many countries are still reporting elevated all-cause excess mortality compared with pre-pandemic levels. According to Swiss Re Institute's report The future of excess mortality after COVID-19, if the ongoing impact of the disease is not curtailed, excess mortality rates in the general population may remain up to 3% higher than pre-pandemic levels in the US and 2.5% in the UK by 2033.
Paul Murray, CEO L&H Reinsurance at Swiss Re says: "COVID-19 is far from over. The US reported an average of 1500 COVID-19 deaths a week for 2023 – comparable to fentanyl or firearm deaths.[1] If this continues, our analysis suggests a potential scenario of elevated excess mortality extending over the next decade. However, excess mortality can return to pre-pandemic levels much sooner. The first step is to get COVID under control, with measures such as vaccinations for the vulnerable. Over the longer term, medical advancements, a return to regular healthcare services, and the adoption of healthier lifestyle choices will be key."
Excess mortality is a measure of the number of deaths above an expected level in a given population. Typically, all-cause excess mortality should be around zero, as the major causes of death remain relatively stable over the long-term baseline assumption.
Fluctuations in excess mortality tend to be short-term, reflecting developments such as a large-scale medical breakthrough or the negative impact of a large epidemic. However, as society absorbs these events, excess mortality should revert to the baseline.
With COVID-19 this has not been the case and all-cause excess mortality is still above the pre-pandemic baseline. In 2021, excess mortality spiked to 23% above the 2019 baseline in the US, and 11% in the UK[2]. As Swiss Re Institute's report estimates, in 2023, it remained significantly elevated in the range of 3–7% for the US, and 5–8% for the UK.
If the underlying drivers of current excess mortality continue, Swiss Re Institute's analysis estimates that excess mortality may remain as high as 3% for the US and 2.5% for the UK by 2033.
The primary driving factor of both current and future excess mortality is respiratory disease (including COVID-19 and influenza), with other causes including cardiovascular disease, cancer and metabolic illnesses. The cause of death split varies by a country's reporting mechanism.
Optimistic scenarios require healthcare and medical advancements
Swiss Re's report examines an optimistic scenario where excess mortality rates return to pre-pandemic levels as early as 2028. In this scenario, medical advances, such as weight loss injectables and cancer developments such as personalised mRNA vaccines, combine with a drop in the impact of COVID-19 and healthier lifestyle choices.
Indirect impact of cardiovascular disease (CVD) mortality
The interplay between COVID-19 and cardiovascular death rates is significant for excess mortality. The virus itself has a direct impact because it contributes to causes of death such as heart failure. Further, COVID-19 has had an indirect impact via the disruption to healthcare systems – a factor which emerged in the pandemic years. This disruption has led to a backlog of essential cardiac tests and surgeries, meaning that conditions such as hypertension have been underdiagnosed and therefore not treated.
Implications for insurers
Excess mortality in the general population is an important indicator for insurers, as shifts in the major causes of death may require a reassessment of additional risk in their mortality portfolios.
The current levels of excess mortality are of concern. However, there are a range of tools available for insurers and reinsurers to manage this trend. Specific actions include adapting the underwriting philosophy, risk appetite, and mortality assumptions in pricing and reserving. Insurers can be proactive in targeting prevention programmes for policyholders, helping them in the joint effort to support longer, healthier lives.
How to order this study:
The future of excess mortality after COVID-19 is available in electronic format from Swissre.com.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#long covid
26 notes
·
View notes
Note
How does one go about getting a t prescription?
How long does it take + how expensive is it?
Where would you even start, what type of doctor do you have to contact, does planned parenthood give people T prescriptions?
Sorry for the ask, I just can't access this information anywhere else
I need to start this post by saying: I - the person answering - am a USAmerican. I have no experience with getting testosterone in other countries, but I have researched other healthcare systems that are in place for trans healthcare. In my country, testosterone is a schedule III controlled substance, and you need a prescription from a doctor to legally possess it (I could rant for hours about how much I hate this, but this is the reality of how the US operates, apparently). I'll be sharing my experience since I know it best with the hopes that it helps - I am not legal or medical advice.
In many places, you will typically be referred to an endocrinologist, someone who specializes in hormones. It isn't unheard of for your primary care physician to order scripts for testosterone, but if they do, it's because they would be licensed to. Not all PCs can even prescribe testosterone in the US because it's a controlled substance.
I personally went through an online clinic in order to get my testosterone - which was needed for me because at the time, I'd had very few positive experiences with healthcare.
In terms of price, that depends on if your insurance will even cover the cost. I pay out-of-pocket, and for those paying that way, that can run (typically) between $150-$300. This also depends on what type of testosterone you plan on administering. I've found that IM injectable testosterone is cheaper than cream or gel testosterone - each method has their own pros and cons, and the prices vary drastically at times.
Planned Parenthood can be a great path for those who have the Planned Parenthood facilities that offer trans healthcare. Not all Planned Parenthood facilities will offer trans healthcare. And, indeed, I was planning on using Planned Parenthood, but the closest one that offered trans healthcare was over an hour away and later seemingly ceased offering that care, which would mean I might have had to drive three hours to the next one. That's a huge contributing factor as to why I chose a virtual clinic.
If you are comfortable with your primary care physician, you might be best helped by asking them. I'm sharing my experience, but this is by no means a comprehensive look into how you would access testosterone. Your needs, the care available, and where you live all impact how you'll get care, and the last thing I want to do is tell you to do something you can't.
#ask#anon#trans#transgender#lgbt#lgbtq#ftm#nonbinary#trans advice#i don't want to come across like i'm insulting anyone's intelligence - i have no clue exactly where our knowledge differs...#...and i don't want to assume. if it seems like i'm being too specific it's because i don't want any miscommunication#and i know that that can/will still happen but i want to put in the effort to make sure we all know where we stand and my intentions
51 notes
·
View notes
Text
ugh
I can't sleep and I'm just sort of stewing over how unprepared I am to be entirely on my own managing my own healthcare. blech.
Did I mention, Farmsister was suffering from hip pain and went to her doctor and was diagnosed with the exact same problem I have?
Diagnosed, I said. Yes! Her doctor actually investigated the cause of her pain, diagnosed her, referred her to a physical therapist, but also came up with a plan of treatment. Told her physical therapy often can't resolve this issue, so after a set amount of PT, if there wasn't enough improvement she'd refer her to an orthopedist instead.
Imagine that. My doctor was like "you've got intermittently debilitating pain? You should go see a doctor about that." and that was that. I went to a physical therapist because that's what she recommended, but I don't have a plan, I'm just spending $150/wk to work out in a room full of other people. I guess I'll ask my PT if there's a plan or like timeline or like, idk, something we should look for, or what. IDK what a realistic goal is. Pain-free seems out of reach. I'd settle for largely functional, I guess? But I don't know, and I guess I'm on my own to figure it out.
And the same with the ADHD! She was like "oh, your insurance isn't going to cover it and it's probably going to take months of waiting, but you had better go see someone about that", and refused to engage any further. So I messaged the psychiatrist today and he doesn't check the messages on that platform so I texted the admin who was like oh usually medication is adjusted at follow-ups, and I'm like well in the three minutes he talked to me it didn't come up I guess, so then they texted back that he says to try taking two pills a day for a couple days and then schedule a follow-up.
I've asked around, and usually I guess the regular adderall pills, you take in two doses at separate times. But if the point is that I'm trying to see if a higher dose helps, I'd probably better take them at the same time??
It's just that when the small ineffective dose wears off four or five hours after I take it, without my ever having had a good phase, I get horribly drowsy and also get this kind of gross formless yearning that I think might be a dopamine crash, where I roam the house in itchy horrible discontent trying to think of something that might help me, but it's not candy and it's not reading a book and it's not napping, and I guess I understand why people turn to drugs or self-harm because the feeling is awful, spacy and wrung-out and aimlessly needy.
But I guess it's up to me to research what that is and what to do about it, and then at my $250 three-minute follow-up appointment in three days or whatever I'll tell the psych what I want prescribed to me, because it's sure as shit not like he's going to have any fucking advice for me.
And like. Laugh out loud at the notion that my primary care physician would give a single shit about this. Maybe I didn't mention this on here either but literally the only thing she has looked into about me is that my blood tests came back with a fasting blood glucose level of 5.7 (idk what units, just that she's fixated on that number) and it is exactly entirely that post circulating about """"pre-diabetes"""? She has put in my chart that she wants to start me on Metformin!! Christ all fucking mighty, it could not be more obvious that she took one look at my fat ass and was like "this bitch eats only candy! I'd better scare her straight!"
Ma'am fuck off. She wants me to get my blood retested in July and I am figuring I'll take advantage of having to have a visit then anyway to get the ADHD stuff entered into my main chart, and I'm also going to tell her that since she was so disinterested in literally any of the conditions actually debilitating me (my hip pain and my ADHD) I had to research those so I could treat myself, and in the course of researching that I found out about the fake "epidemic" of "pre-diabetes" which isn't a thing, it's a fucking PR gambit to sell drugs, and so if she prescribes me diabetes drugs when I do not fucking have diabetes I will not be taking them, and I will also be looking for a new doctor, because I do not appreciate her fixation on treating a condition I do not have while ignoring things that are literally preventing me from leading the life I want to, wherein I can do things like, stand/walk as much as I like and can also like, perform tasks.
So there's my timeline.
(Yeah my insurance won't cover blood testing a second time in a year so that's gonna cost me $200ish, and the phone doctor visit she insisted on to discuss the results last time was $45 and it'll be that again for this one, but I mean, eventually I'll hit my deductible maybe.)
I don't know, people tell me that they have medical professionals that actually listen to and treat them and give them like actual good actionable advice on how to improve their various health conditions but as far as I can tell that all sounds fake and isn't a thing.
Unfortunately, I am too fucking debilitated by my Can't Think Good disease to do a competent job at caring for myself, so I guess I'm just going to have to fucking muddle through somehow, or something.
Probably I should put together my citations on how Pre-Diabetes Is Fake so that when I unload that on my doctor I can do so with fucking footnotes at least. Lord knows I can't sleep at the moment so I might as well do something productive.
30 notes
·
View notes
Text
The Setting
Bougainville
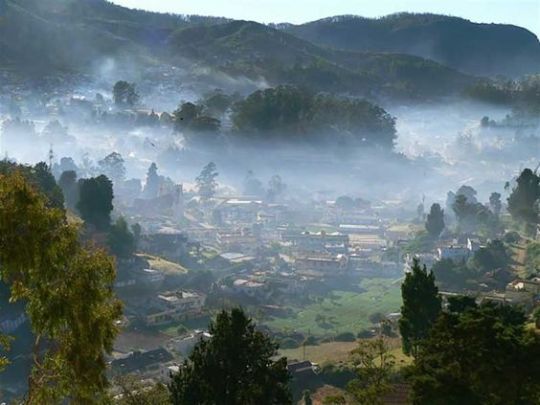

A quaint town with a population of 10,000. Located in the Pas-de-Calais department of Northern France, it is an amalgamation of days past and modern times; preserving its original construction from 150 years ago while intertwining with modern-day advancements.
History


The town was founded in the late 1800s by Olivier Bougainvillea: a renowned physicist from Paris who led a scientific expedition to the area that would later be known as Bougainville. The goal of his expedition was to study unusual electromagnetic radiations within the area. He set up a research base that would inadvertently grow with the influx of scientists and researchers Bougainvillea recruited to participate in his research.
The growing scale of Bougainvillea's research necessitated better infrastructure and living facilities; resulting in the arrival of more labor for construction. The rapid influx of people now requiring long-term accommodation in the area demanded more housing, and soon the base had transformed into a small hamlet. Thus, began the settlement of Bougainville.
As time passed, the families of the workers and researchers had relocated to the area; operating independent businesses to fill demands such as clothing, food, and other essential supplies. And as the economy grew, so did the settlement. More merchants and businesses settled in the hamlet, and soon, what was once a research base became the town of Bougainville: named after the lead scientist that pioneered the settlement of the area and powered the town with his discoveries and innovations.
In honour of his legacy, Bougainvillea flowers line the front of almost every street, creating a beautiful sight at every turn.
Geography
Bougainville has Calais to the north, Le Portel to the west, Lumbres to the east, and Desvres to the south. It is nestled adjacent to the Parc naturel regional des caps et marais d’Opale. As such, lazily drifting fog and chilly weather are a permanent fixture in the small town, perfectly complementing its slow, leisurely lifestyle.
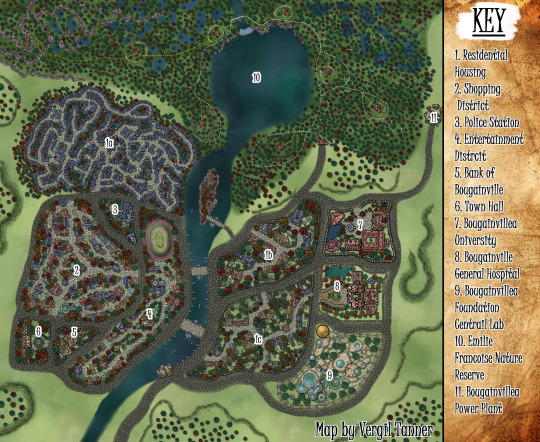
A river divides the town into two sides: West and East.
Western Bougainville is its central business district; housing the entertainment district and the shopping district; as well as the town hall, Bougainville bank, and police station.
Eastern Bougainville is the town’s health and education district; being the location of Bougainvillea University, Bougainville General Hospital, and the Bougainvillea Foundation’s central laboratory; which is open to the public as a science museum. To the north of the town is the Emilie Francoise Nature Reserve, which is 1000 acres of protected marshland and forest. It is also here that the Bougainvillea Power Plant is located; which provides electricity to the entire town.
The Bougainvillea Foundation
A multinational conglomerate with subsidiaries in a variety of industries.
Including, but not limited to:
pharmaceuticals
medical equipment
electronics
non-profit organizations
military equipment
firearms.
Central Laboratory

One of the crowning jewels of Bougainville, the Bougainvillea central laboratory is a marvel of modern engineering. From its humble beginnings as a research tent, it is now the primary location for all of the Bougainvillea Foundation’s science exhibitions. Thus, it is a famous field trip destination for many educational institutes.
It is the oldest and largest lab of the Bougainvillea Foundation. It has contributed much to the lifestyle advancements in Bougainville by: supplying power; being the primary supplier of medicine, medical supplies, and funds the Bougainville healthcare system; and founding Bougainvillea University.



Bougainvillea University

Founded in the honor of Olivier Bougainvillea for his contributions to modern science and the founding of Bougainville, Bougainvillea University strives to shape brilliant minds that will pave the way to innovation and discovery. Graduates of this university may receive highly coveted employment with the Bougainvillea Foundation.


Bougainville General Hospital

From its humble beginnings as a small 3-bed health clinic, the facility has grown to an impressive 300-bed general hospital with an emergency department and specialist operating theatres. Though it has maintained its original exterior, its interior has been refurbished with state-of-the-art healthcare facilities thanks to the generous donations of the Bougainvillea Foundation.
Shopping District

The location of most of the shops in Bougainville. It is the most popular tourist and student destination in town, boasting an array of grocers, book stores, bakeries, boutiques, cafes, restaurants, and wineries.




Entertainment District

The centre of Bougainville’s nightlife, this area is where most of Bougainville’s adult recreational businesses are located. From bars, taverns, and billiard, to nightclubs, strip clubs and gambling.
Emilie Francoise Nature Reserve

Named after the town founder’s wife and fellow scientist, Emilie Francoise nature reserve is 1000 acres of protected marshland and forest. The reserve is a popular hiking and camping destination for locals and visitors alike.
In honor of Olivier Bougainvillea's beloved wife, fellow scientist, and Parisian ecologist, the nature reserve aims to continue the conservation efforts of Emilie Francoise Bougainvillea in protecting the town’s natural landscape.
Key Locations

Luna Lake
A crystalline lake that is 30 km wide that reflects the sky like a mirror. At night time, it seems to hold the moon on its surface. It is populated by diverse aquatic life, making it a popular fishing spot.

Bellevue Valley
A valley covered with flowers all year long. Different flowers bloom during different seasons and months.

Celine Falls
The biggest, most scenic water fall in the nature reserve

Labyrinthe Marshland
The largest marshland in the nature reserve and home to a diverse population of wildlife.
The Underground

There are whispers of an underground black market where illicit goods and services are distributed. Though its location is largely unknown…
▶ Wildward Master Post
61 notes
·
View notes
Text

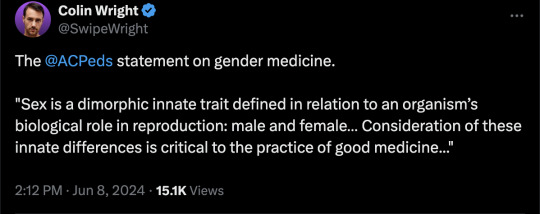
My name is Dr Jill Simons. I'm a board-certified pediatrician and the executive director for the American College of Pediatricians. Today I'm here alongside my colleagues representing the Coalition of co-signers of the Doctors Protecting Children Declaration. Our coalition consists of physicians together with nurses, behavioral health clinicians, other health professionals, scientists, researchers and public health and policy professionals. And we have serious concerns about the physical and mental health effects of the current protocols promoted for the care of children and adolescents in the United States who express discomfort with their biological sex.
This declaration was authored by the American College of Pediatricians, but really it was developed from the expertise of hundreds of doctors researchers and other healthcare workers and leaders wh, for years have been sounding the alarm on the harmful protocols that continue to be promoted by the medical organizations in the United States. Despite recent revelations from the leaked WPATH Files and the recent release of the final report from the Cass Review, these medical organizations have not changed course.
So, we are calling on these medical organizations of the United States, including the American Academy of Pediatrics, the Endocrine Society, the Pediatric Endocrine Society, the American Medical Association, the American Psychological Association and the American Academy of Child and Adolescent Psychiatry to follow the science and their European colleagues and immediately stop the promotion of social affirmation, puberty blockers, cross-sex hormones and surgeries for children and adolescents who experience distress over their biological sex.
In our declaration, we affirm that sex is a dimorphic, innate trait defined in relation to an organism's biological role in reproduction: male and female this genetic signature is present in every nucleated somatic cell in the body and is not altered by drugs or surgical interventions. Consideration of these innate differences is critical to the practice of good medicine and to the development of sound policy for children and adults alike. Medical decision-making should be based upon an individual's biological sex. It should respect biological reality and the dignity of the person by compassionately addressing the whole person.
We are here defying the claims made by these medical organizations in the US that those of us who are concerned are a minority and that their protocols are consensus. They are not consensus, and we are speaking in a loud unified voice: enough.
[ Full press conference: https://youtu.be/C2tU90XPFlg ]
--
Doctors Protecting Children Declaration
As physicians, together with nurses, psychotherapists and behavioral health clinicians, other health professionals, scientists, researchers, and public health and policy professionals, we have serious concerns about the physical and mental health effects of the current protocols promoted for the care of children and adolescents in the United States who express discomfort with their biological sex.
We affirm:
1. Sex is a dimorphic, innate trait defined in relation to an organism’s biological role in reproduction. In humans, primary sex determination occurs at fertilization and is directed by a complement of sex determining genes on the X and Y chromosomes. This genetic signature is present in every nucleated somatic cell in the body and is not altered by drugs or surgical interventions
2. Consideration of these innate differences is critical to the practice of good medicine and to the development of sound public policy for children and adults alike.
3. Gender ideology, the view that sex (male and female) is inadequate and that humans need to be further categorized based on an individual’s thoughts and feelings described as “gender identity” or “gender expression”, does not accommodate the reality of these innate sex differences. This leads to the inaccurate view that children can be born in the wrong body. Gender ideology seeks to affirm thoughts, feelings and beliefs, with puberty blockers, hormones, and surgeries that harm healthy bodies, rather than affirm biological reality.
4. Medical decision making should not be based upon an individual’s thoughts and feelings, as in “gender identity” or “gender expression”, but rather should be based upon an individual’s biological sex. Medical decision making should respect biological reality and the dignity of the person by compassionately addressing the whole person.
We recognize:
1. Most children and adolescents whose thoughts and feelings do not align with their biological sex will resolve those mental incongruencies after experiencing the normal developmental process of puberty.
Desistance is the norm without affirmation as documented by Zucker in his article “The Myth of Peristence”. (1)
Zucker, KJ. The myth of persistence: Response to “A critical commentary on follow-up studies and ‘desistance’ theories about transgender and gender nonconforming children” by Temple Newhook et al. International Journal of Transgenderism. 2018: 19(2), 231–245. Published online May 29, 2018.http://doi.org/10.1080/15532739.2018.1468293 [1]
In the “largest sample to date of boys clinic-referred for gender dysphoria,” there was a desistance rate of 87.8%. (2)
Singh D, Bradley SJ and Zucker KJ. A Follow-Up Study of Boys With Gender Identity Disorder. Front Psychiatry. 2021;12:632784. doi: 10.3389/fpsyt.2021.632784
The pro-affirmation Endocrine Society Guidelines (2017) admit: “…the GD/gender incongruence of a minority of prepubertal children appears to persist in adolescence.” (3)
Hembree, W., Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: An Endocrine Society clinical practice guideline J Clin Endocrinol Metab. 2017; 102:1–35.
A longitudinal study from the University of Groningen in the Netherlands followed 2772 adolescents (recruited from a psychiatric clinic) from age 11 years through 22 – 26 years. “In early adolescence 11% of participants reported gender non- contentedness. The prevalence decreased with age and was 4% at the last follow-up (around age 26).” Even in this psychiatric patient study group for which interventions were not addressed, but “gender affirmation” is most likely, gender non-contentedness (essentially gender noncongruence) decreased substantially from early adolescence to young adulthood.(4)
Rawee P, Rosmalen JGM, Kalverdiijk L and Burke SM. Development of gender non-contentedness during adolescence and early adulthood. Archives of Sexual Behavior. 2024; https://doi.org/10.1007/s10508-024-02817-5
2. Responsible informed consent is not possible in light of extremely limited long-term follow-up studies of interventions, and the immature, often impulsive, nature of the adolescent brain. The adolescent brain’s prefrontal cortex is immature and is limited in its ability to strategize, problem solve and make emotionally laden decisions that have life-long consequences.[2]
3. Sex-trait modification or “Gender affirming” clinics in the United States base their treatments upon the “Standards of Care” developed by the World Professional Association for Transgender Health (WPATH). However, the foundation of WPATH guidelines is demonstrably flawed and pediatric patients can be harmed when subjected to those protocols.
The two Dutch studies that form the foundation for treatment guidelines as documented in the WPATH “Standards of Care” guidelines version 7 (SOC 7) had serious flaws.[3]
These studies did show that the appearance of secondary sex characteristics in adolescents and young adults could be changed by hormonal and surgical interventions, but they failed to demonstrate meaningful long-term improvement in psychological well-being.
Scientific concerns with these studies also include a lack of a control group, small sample sizes, significant numbers of patients lost to follow up, and the elimination of patients who experienced significant mental illness from entering the studies.
It is concerning that the Dutch studies did not address complications and adverse outcome in the adolescent cohort that underwent transition. These complications included new onset diabetes, obesity and one death.[4]
4. There is now sufficient research to further demonstrate the failure of the WPATH, American Academy of Pediatrics and Endocrine Society protocols.
The Cass Review was released on April 10, 2024, as an “independent review of gender identity services for children and young people”. The following points are from Cass’s final report:[5]
Commissioned by the National Health Service (NHS) England, and chaired by Dr. Hilary Cass, the 388-page report utilized systematic reviews, qualitative and quantitative research, as well as focus groups, roundtables and interviews with international clinicians and policy makers.
As part of the evaluation, they reviewed the research on social transition, puberty blockers, and cross-sex hormones.
Social transition
“The systematic review showed no clear evidence that social transition in childhood has any positive or negative mental health outcomes, and relatively weak evidence for any effect in adolescence.
However, those who had socially transitioned at an earlier age and/or prior to being seen in clinic were more likely to proceed to a medical pathway.”
Puberty blockers
“The systematic review undertaken by the University of York found multiple studies demonstrating that puberty blockers exert their intended effect in suppressing puberty, and also that bone density is compromised during puberty suppression. However, no changes in gender dysphoria or body satisfaction were demonstrated [emphasis added].”
“There was insufficient/inconsistent evidence about the effects of puberty suppression on psychological or psychosocial wellbeing, cognitive development, cardio-metabolic risk or fertility.”
“Moreover, given that the vast majority of young people started on puberty blockers proceed from puberty blockers to masculinizing/ feminizing hormones, there is no evidence that puberty blockers buy time to think, and some concern that they may change the trajectory of psychosexual and gender identity development.”
Cross-sex hormones
“The University of York carried out a systematic review of outcomes of masculinising/feminising hormones.” They concluded, “There is a lack of high-quality research assessing the outcomes of hormone interventions in adolescents with gender dysphoria/incongruence, and few studies that undertake long-term follow-up. No conclusions can be drawn about the effect on gender dysphoria, body satisfaction, psychosocial health, cognitive development, or fertility.”
“Uncertainty remains about the outcomes for height/growth, cardio-metabolic and bone health.”
The Cass Review further stated, “Assessing whether a hormone pathway is indicated is challenging. A formal diagnosis of gender dysphoria is frequently cited as a prerequisite for accessing hormone treatment. However, it is not reliably predictive of whether that young person will have longstanding gender incongruence in the future, or whether medical intervention will be the best option for them.”
A 2024 German systematic review on the evidence for use of puberty blockers (PB) and cross-sex hormones (CSH) in minors with gender dysphoria (GD) also found “The available evidence on the use of PB and CSH in minors with GD is very limited and based on only a few studies with small numbers, and these studies have problematic methodology and quality. There also is a lack of adequate and meaningful long-term studies. Current evidence doesn’t suggest that GD symptoms and mental health significantly improve when PB or CSH are used in minors with GD.”[6]
5. There are serious long-term risks associated with the use of social transition, puberty blockers, masculinizing or feminizing hormones, and surgeries, not the least of which is potential sterility.
Youth who are socially affirmed are more likely to progress to using puberty blockers and cross-sex (masculinizing or feminizing) hormones.
“Social transition is associated with the persistence of gender dysphoria as a child progresses into adolescence.”[7]
“Gender social transition of prepubertal children will increase dramatically the rate of gender dysphoria persistence when compared to follow-up studies of children with gender dysphoria who did not receive this type of psychosocial intervention and, oddly enough, might be characterized as iatrogenic.”[8]
Puberty blockers permanently disrupt physical, cognitive, emotional and social development.
Side effects listed in the Lupron package insert include emotional lability, worsening psychological illness, low bone density, impaired memory, and the rare side-effect of pseudotumor cerebri (brain swelling).[9]
A coalition of physicians and medical organizations from around the world submitted a petition to the Commissioner of the U.S. Food and Drug Administration requesting urgent action be taken to eliminate the off-label use of GnRH (growth hormone) agonists in children.[10]
Testosterone use in females and estrogen use in males are associated with dangerous health risks across the lifespan including, but not limited to, cardiovascular disease, high blood pressure, heart attacks, blood clots, stroke, diabetes, and cancer.[xi],[12]
Genital surgeries affect future fertility and reproduction.
6. A report from Environmental Progress released on March 4, 2024, entitled “The WPATH Files” revealed “widespread medical malpractice on children and vulnerable adults at global transgender healthcare authority.”[13]
“The WPATH Files reveal that the organization does not meet the standards of evidence-based medicine, and members frequently discuss improvising treatments as they go along.”
“Members are fully aware that children and adolescents cannot comprehend the lifelong consequences of ‘gender-affirming care’ and, in some cases due to poor health literacy, neither can their parents.”
In addition, developmentally challenged and mentally ill individuals were being encouraged to “transition”, and treatments were often improvised.
7. Evidence-based medical research now demonstrates there is little to no benefit from any or all suggested “gender affirming” interventions for adolescents experiencing Gender Dysphoria. Social “affirmation”, puberty blockers, masculinizing or feminizing hormones, and surgeries, individually or in combination, do not appear to improve long-term mental health of the adolescents, including suicide risk.[14]
8. Psychotherapy for underlying mental health issues such as depression, anxiety, and autism, as well as prior emotional trauma or abuse should be the first line of treatment for these vulnerable children experiencing discomfort with their biological sex.
9. England, Scotland, Sweden, Denmark, and Finland have all recognized the scientific research demonstrating that the social, hormonal and surgical interventions are not only unhelpful but are harmful. So, these European countries have paused protocols and are instead focusing on evaluating and treating the underlying and preceding mental health concerns.
10. Other medical organizations are adhering to the evidence-based medicine documented in the Cass Review Final Report.
The constitution of the National Health Service in England will be updated to state, “We are defining sex as biological sex.”[15]
The European Society of Child and Adolescent Psychiatry issued a document titled “ESCAP statement on the care for children and adolescents with gender dysphoria: an urgent need for safeguarding clinical, scientific, and ethical standards.”
In this paper, they stated, “The standards of evidence-based medicine must ensure the best and safest possible care for each individual in this highly vulnerable group of children and adolescents. As such, ESCAP calls for healthcare providers not to promote experimental and unnecessarily invasive treatments with unproven psycho-social effects and, therefore, to adhere to the “primum-nil-nocere” (first, do no harm) principle”.[16]
11. Health care professionals around the world are also acknowledging the urgent need to protect children from harmful “gender-affirming” interventions.
In a letter to the British newspaper, The Guardian, sixteen psychologists, some of whom worked at the Tavistock Center for Gender Identity Development Service, acknowledged the role clinical psychologists played in placing children on an “irreversible medical pathway that in most cases was inappropriate.”[17]
In the United States, a group of psychiatrists, physicians and other health care workers wrote an open Letter to the American Psychiatric Association (APA), calling on the APA to explain why it glaringly ignored many scientific developments in gender-related care and to consider its responsibility to promote and protect patients’ safety, mental and physical health.[18]
12. Despite all the above evidence that gender affirming treatments are not only unhelpful, but are harmful, and despite the knowledge that the adolescent brain is immature, professional medical organizations in the United States continue to promote these interventions. Further, they state that legislation to protect children from harmful interventions is dangerous since it interferes with necessary medical care for children and adolescents.
The American Psychological Association states it is the largest association of psychologists worldwide. The organization released a policy statement in February 2024 stating, “The APA opposes state bans on gender-affirming care, which are contrary to the principles of evidence-based healthcare, human rights, and social justice.”[19]
The Endocrine Society responded to the Cass Review by reaffirming their stance. “We stand firm in our support of gender-affirming care…. NHS England’s recent report, the Cass Review, does not contain any new research that would contradict the recommendations made in our Clinical Practice Guideline on gender-affirming care.”[20]
The American Academy of Pediatrics (AAP) Board of Directors in August 2023, voted to reaffirm their 2018 policy statement on gender-affirming care. They did decide to authorize a systematic review but only because they were concerned “about restrictions to access to health care with bans on gender-affirming care in more than 20 states.”[21]
Of note, Dr. Hilary Cass called out the AAP for “holding on to a position that is now demonstrated to be out of date by multiple systematic reviews.”[22]
In Conclusion
Therefore, given the recent research and the revelations of the harmful approach advocated by WPATH and its followers in the United States, we, the undersigned, call upon the medical professional organizations of the United States, including the American Academy of Pediatrics, the Endocrine Society, the Pediatric Endocrine Society, American Medical Association, the American Psychological Association, and the American Academy of Child and Adolescent Psychiatry to follow the science and their European professional colleagues and immediately stop the promotion of social affirmation, puberty blockers, cross-sex hormones and surgeries for children and adolescents who experience distress over their biological sex. Instead, these organizations should recommend comprehensive evaluations and therapies aimed at identifying and addressing underlying psychological co-morbidities and neurodiversity that often predispose to and accompany gender dysphoria. We also encourage the physicians who are members of these professional organizations to contact their leadership and urge them to adhere to the evidence-based research now available.
#Jill Simons#Doctors Protecting Children#American College of Pediatricians#medical scandal#medical malpractice#medical mutilation#medical corruption#WPATH Files#The WPATH Files#Cass review#Cass report#puberty blockers#wrong sex hormones#cross sex hormones#sex trait modification#gender affirming care#gender affirming healthcare#gender affirmation#biological sex#sex is binary#sex binary#religion is a mental illness
18 notes
·
View notes
Text
A damning new study is raising major concerns among the medical and scientific communities after researchers concluded that Covid mRNA shots have caused a global surge in cases of AIDS-like vaccine-acquired immunodeficiency syndrome (VAIDS).
The researchers analyzed the data of a staggering nine million people who had received at least one dose of a Covid mRNA “vaccine.”
The explosive peer-reviewed study was conducted by a team of world-renowned South Korean researchers, led by Professor Solam Lee at Yonsei University Wonju College of Medicine’s Department of Dermatology.
The primary cohort study analyzed official government data from the National Health Insurance Service (NHIS) and Korea Disease Control and Prevention Agency (KDCA) databases.
The government databases comprise the healthcare data of more than 99 percent of the entire Korean population.
The comprehensive database also includes records of each individual’s COVID-19 diagnoses and Covid vaccination profiles.
For the study, the researchers used a dataset with a total of 9,258,803 individuals who received at least the first dose of an mRNA COVID-19 shot.
Establishing a control cohort within mRNA-vaccinated persons, the investigators shifted back 2 years to the observational period from the date of the first dose of mRNA vaccination.
In total, 4,445,333 and 4,444,932 patients were included in the vaccination and historical control cohorts, respectively, and all were observed for at least one year.
7 notes
·
View notes
Note
mammallama if you have energy how did you find your adhd dr? I know I could use one but I'm trying to fight the inertia of getting a dr because of all the experiences of previous medical professionals not listening to me. thank you for reading!
Hey, I've got a little energy! You get my one level seven spell slot for the day lol
I am very fortunate that I have a primary care doctor that takes my concerns seriously and pointed me in the direction of my current specialist. I also have two very wonderful best friends with ADHD who gently slid my wig back and told me "go get tested, you sound like me". I recognize not everyone is lucky to have doctors that listen to them so this answer will be based off of my limited experience and local healthcare in my state in America, so please keep these as general suggestions! And I know it's hard to advocate for your own health, trust me I get it lol, but please stick with it. It's worth it to get the answers at the very least so you can start adjusting.
So if you have a PCP try asking them for places that are in your insurance network that could help you get tested/write you a referral letter if needed. I would suggest first looking for a behavioral therapist that specializes in diagnosing ADHD (like mine does) and treatment. I can't get actual cognitive behavioral therapy from them but they help me keep track of my ADHD and navigate my medication stuff. The extra special thing about my doctor is she was also diagnosed as an adult, so she truly understands to a certain degree of what I'm dealing with. Looking at her during my first visit was like looking into the future of the person I can be with the right help. Having a doctor that has what you have is incredibly valuable.
If you can't find a specialist, I would suggest looking for a psychiatrist that specializes in diagnosing and treating ADHD. You can also get diagnosed by a psychologist but I don't think they can actually prescribe medications? But either of those professionals will be able to test and diagnose you!
If you have trouble networking, my therapist suggested looking on Facebook (I know I know) for local/state groups that can help you connect with doctors in your area. You'd be surprised at how ready people are to help others find the care providers they need! You may not even have to ask, there may be a list of medical professionals that you can look over.
I will warn you that depending on where you go it's going to probably cost a fair amount. Even with my therapist's office taking my insurance my testing was still over 400 bucks, but in the end it was worth it for me. I will also warn you that some testing can be quite lengthy from what I hear, taking multiple sessions depending on the professional you're seeing. My testing and diagnoses took a little less than three hours and that's why I'd suggest looking for an ADHD behavioral therapist first. They know exactly what they're looking for and know you're there specifically for that test.
Another tip I can give you is frame your reason for testing as simply needing answers to improve your quality of life. Have that in writing. Don't even mention medication other than "I would explore that if you deem it a viable option for treatment." Getting medication right now is difficult if not downright impossible for some of us, so I would frame your needs on getting yourself picked up and put together. That's really what you need first anyways. Answers.
Be warned ADHD may also come with a side of fries (other general disabilities like OCD/OCD tendencies, anxiety, depression, ect ect that are often the result of untreated ADHD).
ADHD is legally considered a developmental disability and protected under the Americans with Disabilities Act. Know your rights!
In the meantime I always suggest taking a look through https://www.additudemag.com/ for information about symptoms and research and all that stuff. This is a trusted source that my therapist's office shares with all of their patients! The articles are kept up to date as new research is made available and is laid out in such a way that it's easy for people with ADHD to read and navigate. It's also a great source for parents that have kiddos with ADHD, so pass that around if you know someone who's struggling!
I do hope that your past experiences with poor doctors won't keep you from seeking testing. I can promise you not all of them are like that, and I hope you can find someone who will listen to you and take your concerns seriously!
#ask me stuff!#adhd#long post#but yeah i promise not all drs are Like That#i have drs and surgeons in my family and while i am gonna have to kick the snot out of my younger brother for some shit im seeing budding#my older family members are very good and listen to their patients#theyre out there i promise#pointing out this is a US based perspective#so if you are not in the US i would go through the health care channels that are the equivalent of your care network!
18 notes
·
View notes
Text

𝐓𝐫𝐚𝐧𝐬𝐟𝐨𝐫𝐦𝐢𝐧𝐠 𝐇𝐞𝐚𝐥𝐭𝐡𝐜𝐚𝐫𝐞: 𝐊𝐞𝐲 𝐓𝐫𝐞𝐧𝐝𝐬 𝐒𝐡𝐚𝐩𝐢𝐧𝐠 𝐭𝐡𝐞 𝐔.𝐒. 𝐏𝐫𝐢𝐦𝐚𝐫𝐲 𝐂𝐚𝐫𝐞 𝐌𝐚𝐫𝐤𝐞𝐭
𝐃𝐨𝐰𝐧𝐥𝐨𝐚𝐝 𝐚 𝐅𝐑𝐄𝐄 𝐒𝐚𝐦𝐩𝐥𝐞: https://www.nextmsc.com/us-primary-care-market/request-sample
The 𝐔.𝐒. 𝐏𝐫𝐢𝐦𝐚𝐫𝐲 𝐂𝐚𝐫𝐞 𝐌𝐚𝐫𝐤𝐞𝐭 is evolving rapidly, driven by a myriad of factors that are reshaping the way we approach healthcare delivery. Here's a snapshot of the key trends and opportunities:
𝐈𝐧𝐜𝐫𝐞𝐚𝐬𝐞𝐝 𝐅𝐨𝐜𝐮𝐬 𝐨𝐧 𝐏𝐫𝐞𝐯𝐞𝐧𝐭𝐢𝐯𝐞 𝐂𝐚𝐫𝐞: With a growing emphasis on preventive care, primary care providers are playing a pivotal role in early diagnosis and management of chronic diseases.
𝐓𝐞𝐥𝐞𝐡𝐞𝐚𝐥𝐭𝐡 𝐁𝐨𝐨𝐦: The pandemic accelerated the adoption of telehealth services, making primary care more accessible and convenient for patients across the nation.
𝐕𝐚𝐥𝐮𝐞-𝐁𝐚𝐬𝐞𝐝 𝐂𝐚𝐫𝐞 𝐌𝐨𝐝𝐞𝐥𝐬: There is a significant shift towards value-based care models that prioritize patient outcomes and cost-efficiency over traditional fee-for-service models.
𝐈𝐧𝐭𝐞𝐠𝐫𝐚𝐭𝐢𝐨𝐧 𝐨𝐟 𝐀𝐝𝐯𝐚𝐧𝐜𝐞𝐝 𝐓𝐞𝐜𝐡𝐧𝐨𝐥𝐨𝐠𝐲: From electronic health records to AI-driven diagnostic tools, technology is enhancing the efficiency and effectiveness of primary care services.
𝐆𝐫𝐨𝐰𝐢𝐧𝐠 𝐖𝐨𝐫𝐤𝐟𝐨𝐫𝐜𝐞 𝐃𝐞𝐦𝐚𝐧𝐝: As the population ages and chronic diseases become more prevalent, the demand for primary care professionals continues to rise, highlighting the need for more training programs and incentives.
𝐏𝐚𝐭𝐢𝐞𝐧𝐭-𝐂𝐞𝐧𝐭𝐞𝐫𝐞𝐝 𝐌𝐞𝐝𝐢𝐜𝐚𝐥 𝐇𝐨𝐦𝐞𝐬 (𝐏𝐂𝐌𝐇𝐬): PCMHs are transforming the primary care landscape by offering coordinated, comprehensive care that addresses the whole person rather than just individual symptoms.
𝐌𝐚𝐣𝐨𝐫 𝐊𝐞𝐲 𝐏𝐥𝐚𝐲𝐞𝐫𝐬: The U.S. primary care industry comprises of various key players such as Centura Health, Access
Healthcare, Walgreens Boots Alliance, VillageMD, UnitedHealth Group, Agilon Health, Privia Health,
Aledade, Consumer Value Store (CVS) Health, Centene Corporation and others.
𝐀𝐜𝐜𝐞𝐬𝐬 𝐅𝐮𝐥𝐥 𝐑𝐞𝐩𝐨𝐫𝐭: https://www.nextmsc.com/report/us-primary-care-market
The U.S. Primary Care Market is at a crucial juncture, presenting numerous opportunities for innovation and improvement. As we navigate these changes, the focus remains on providing high-quality, accessible, and patient-centered care to all.
#healthcare#primary care#tele health#value based care#healthtech#patient care#medical innovation#health care industry#market research#market trends#business insights
0 notes
Text
Testing the Waters Overseas: Scope of International Business Research

In today’s blog, we will discuss the scope of business research, highlighting its importance and the key areas of focus that can drive successful global expansion. Let’s get started!
Read more: https://www.unimrkt.com/blog/testing-the-waters-overseas-scope-of-international-business-research.php
#International Business Research#primary market research#qualitative market research#market research company#healthcare market research#survey programming
1 note
·
View note
Text
I fucking hate having a condition so underdiagnosed that there's STILL just like. A single dr in the entire county who's the only one that people recommend for primary care. And like it's getting well-known enough that more medical professionals are saying "Oh yeah I know how to work with that" and then prove they've MAYBE spent a few extra hours doing independent research outside of what they were taught. And then I still have to basically decide between "Person sincerely educated on EDS" and "person I trust to manage trans healthcare." It's so fucking depressing.
#welcome to my twisted bones#also that one dr isnt accepting patients anymore and he gives me bad vibes anyway :/
7 notes
·
View notes
Text
Pain emerges as dominant symptom in long Covid, UCL study reveals - Published Aug 28, 2024
Pain may be the most prevalent and severe symptom reported by individuals with long Covid, according to a new study led by UCL (University College London) researchers.
The study, published in JRSM Open, analysed data from over 1,000 people in England and Wales who logged their symptoms on an app between November 2020 and March 2022.
Pain, including headache, joint pain and stomach pain, was the most common symptom, reported by 26.5% of participants.
The other most common symptoms were neuropsychological issues such as anxiety and depression (18.4%), fatigue (14.3%), and dyspnoea (shortness of breath) (7.4%). The analysis found that the intensity of symptoms, particularly pain, increased by 3.3% on average each month since initial registration.
The study also examined the impact of demographic factors on the severity of symptoms, revealing significant disparities among different groups. Older individuals were found to experience much higher symptom intensity, with those aged 68-77 reporting 32.8% more severe symptoms, and those aged 78-87 experiencing an 86% increase in symptom intensity compared to the 18-27 age group.
Gender differences were also pronounced, with women reporting 9.2% more intense symptoms, including pain, than men. Ethnicity further influenced symptom severity, as non-white individuals with long Covid reported 23.5% more intense symptoms, including pain, compared to white individuals.
The study also explored the relationship between education levels and symptom severity. Individuals with higher education qualifications (NVQ level 3, 4, and 5 ��� equivalent to A-levels or higher education) experienced significantly less severe symptoms, including pain, with reductions of 27.7%, 62.8%, and 44.7% for NVQ levels 3, 4 and 5 respectively, compared to those with lower education levels (NVQ level 1-2 – equivalent to GCSEs).
Socioeconomic status, as measured by the Index of Multiple Deprivation (IMD), also influenced symptom intensity. Participants from less deprived areas reported less intense symptoms than those from the most deprived areas. However, the number of symptoms did not significantly vary with socioeconomic status, suggesting that while deprivation may exacerbate symptom intensity, it does not necessarily lead to a broader range of symptoms.
Our study highlights pain as a predominant self-reported symptom in long Covid, but it also shows how demographic factors appear to play a significant role in symptom severity.
With ongoing occurrences of Covid-19 (e.g., LB.1, or D-FLiRT variants), the potential for more long Covid cases remains a pressing concern. Our findings can help shape targeted interventions and support strategies for those most at risk."
-Dr. David Sunkersing, Lead Author, UCL Institute of Health Informatics
In the paper, the researchers called for sustained support for long Covid clinics and the development of treatment strategies that prioritize pain management, alongside other prevalent symptoms like neuropsychological issues and fatigue.
Given the significant impact of demographic factors on symptom severity, the study underscored the need for healthcare policies that addressed these disparities, ensuring equitable care for all individuals affected by long Covid, the researchers said.
Study limitations included a lack of information on other health conditions participants may have had and a lack of information about health history. The researchers cautioned that the study may have excluded individuals with very severe Covid and those facing technological or socioeconomic barriers in accessing a smartphone app.
The study was led by the UCL Institute of Health Informatics and the Department of Primary Care and Population Health at UCL in collaboration with the software developer, Living With Ltd.
Source:
University College London
Journal reference:
Sunkersing, D., et al. (2024) Long COVID symptoms and demographic associations: A retrospective case series study using healthcare application data. Materials Today. doi.org/10.1177/20542704241274292.
journals.sagepub.com/doi/10.1177/20542704241274292
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator#long covid
15 notes
·
View notes