#what are the 3 most common symptoms of undiagnosed diabetes?
Text
How to Manage PCOS with Yoga?
Polycystic Ovary Syndrome or PCOS is a hormonal issue that affects one in five (20%) women in India. Despite its common occurrence, studies reveal that a shocking 70% of women with PCOS remain undiagnosed or unaware that they are suffering from this issue.
While PCOS by itself is not a life-threatening condition, it can set into motion several comorbidities that can cause serious health complications like diabetes and infertility in the long run. If not dealt with effectively, it can also induce life-threatening conditions such as heart disease. Therefore, managing PCOS is extremely crucial in maintaining hormonal harmony and good health. One of the most effective ways to manage this condition is to practice yoga asanas for PCOS, daily.
In this article, we discuss in detail what PCOS is, its causes, symptoms to watch out for, and why yoga is the perfect solution for polycystic ovaries.
What is PCOS?
PCOS is a hormonal disorder that impacts women of reproductive age. It is known as polycystic ovary syndrome as it is often characterized by the development of several small collections of fluid or follicles in the ovaries which impairs their ability to release eggs on time.
While the exact cause of PCOS is unknown, we find it often co-exists with conditions such as obesity. Thus, weight loss usually helps in treating this condition and reducing its long-term impact.
Symptoms of PCOS
Below are some of the most common signs of PCOS. However, your doctor may diagnose you with this condition even if you show at least two of these symptoms:
1. Excessive male hormones
Androgens are a group of hormones that carry out the function of maintaining sexual and reproductive health in men. Androgens are present in small amounts in women. However, when there is an excess of androgens production in women, it is regarded as a symptom of PCOS. Some signs that you may have excessive androgens include excessive facial and body hair (hirsutism), weight gain, acne, and male-patterned baldness.
2. Cyst formation in the ovaries
Fluid-filled sacs or follicles in the ovaries cause them to enlarge and surround the eggs. This also negatively impacts fertility.
3. Skipped or irregular periods
The male hormone hinders the menstrual cycle so women with PCOS experience fewer periods. This is usually the most common sign of PCOS.
Other common symptoms of PCOS include:
Heavy bleeding
Weight gain (Signs and symptoms of PCOS are usually worsened by obesity)
Acne breakouts (chest, face, upper back)
Skin darkening (underneath the breasts, neck, the groin region)
Hair-fall and even baldness
Headaches
Excess hair growth on the face and body
Causes of PCOS
The exact cause of PCOS is unknown but experts believe that a combination of one or more of the following 4 factors could play a role:
Genetics
Insulin resistance along with obesity
A high degree of inflammation (often caused due to being overweight), which can shoot up androgen levels
An unhealthy, sedentary lifestyle along with inadequate nutrition
How to manage PCOS in daily life?
Polycystic Ovary Syndrome is a life-long condition. Whilst there is no cure for it, the patient can manage the symptoms quite effectively through lifestyle modifications and/or medications:
1. Consuming medications such as progesterone tablets to stabilize absent or irregular periods
2. Taking medications to combat hair loss and excessive facial hair growth
3. Opting for OTC or prescription acne treatments (depending on the severity of the acne)
4. Lifestyle changes such as consuming a balanced diet and staying active by practicing yoga, etc.
Healing PCOS with YOGA
Yoga has proven to be quite effective in managing a large number of PCOS symptoms.
3 Ways Yoga for PCOS and Hormonal Imbalance helps you
Manages PCOS-Related Anxiety
Living with PCOS causes hormonal imbalances that makes you prone to mood disorders such as depression and anxiety. Practicing yoga has a calming effect on your body, mind, and soul, thereby, greatly relieving you of stress and anxiety. Doing yoga asanas for PCOS problem is an effective non-invasive treatment option for women looking for daily holistic management of the condition.
2. Brings Stability to Your Hormones
A study released by the Journal of Alternative and Complementary Medicine assessed girls that were diagnosed with PCOS who regularly involved themselves in an hour-long yoga session for a full 12 weeks. After the mentioned weeks were complete, the girls showed noticeable improvement in their hormonal levels, namely testosterone, luteinizing hormone, and anti-mullerian hormone. Some girls even reported consistent menstrual frequency.
3. Positively Impacts Metabolic Markers
Practicing yoga asanas for PCOS treatment has also produced positive results in managing cholesterol and insulin levels in women. Compared to conventionally understood exercise methods like weight lifting, resistance training, running, or cycling, yoga has shown better performance in regulating lipid profile, glucose levels, and insulin resistance.
Top 5 Yoga Asanas for PCOS
1. Setu Bandhasana (Bridge Pose)
Level: Beginner-Friendly
This humble backbend is not to be underestimated on account of how easy it is to do. The Bridge pose strengthens your chest as well as your back and leg muscles while simultaneously relieving tension from it. By alleviating physical stressors from the body, it revitalizes you and relaxes you, both at the same time, calming your mind. According to the International Journal of Trend in Scientific Research and Development (IJTSRD), Bridge Pose is considered a mild inversion as while performing this pose, your heart is at a higher level than your head. Thus it offers all the advantages of an inversion, such as relief from anxiety, mild depression, insomnia, and tiredness as it not only calms the mind but also reduces blood pressure.
2. Dhanurasana (Bow Pose)
Level: Beginner-intermediate
This pose brings you comfort from menstrual pain, stimulates your reproductive organs (in case of infertility), and improves blood circulation to the pelvic region. It also relaxes the abdominal organs and stretches your leg, neck, and shoulder muscles.
3. Chakravakasana (Cat-Cow Pose)
Level: Beginner-Friendly
This pose which is a Vinyasa Yoga staple is highly recommended for managing stress as the movement is synchronized with your breathing in such a way that it immediately induces feelings of relaxation. The Cat-Cow is also great for reducing back pain.
4. Malasana (Garland Pose)
Level: Intermediate -Advanced
This asana is yoga’s worthy comeback to a deep squat. However, just like a deep squat, it can be difficult for practitioners who are just starting on their yoga or fitness journey. Luckily, like most yoga poses it has variations that make it accessible to newbies who can enjoy the myriad benefits of this pose by modifying it just slightly to suit varying fitness levels.
This pose is especially beneficial if you have PCOS because:
-It helps release stress
-It aids in digestion. As indigestion and PCOS are often interrelated, this pose is a must for those who suffer from digestive issues and PCOS.
-It eases menstrual cramps and discomfort. Those with PCOS often experience heavy, painful periods. Malasana opens up your hips and offers relief from period pains.
5. Kapalbhati Pranayama (Breathing Technique)
Level: Beginner-friendly
Kapalbhati Pranayama is a Kundalini Yoga and active meditation technique that can be a powerful tool in healing PCOS symptoms. Especially, signs like stress, high blood sugar levels, and obesity. Also known as Breath of Fire, Kapalbhati is most effective when performed early in the morning on an empty stomach. The technique involves passive inhalations and forceful exhalations through the nose.
Conclusion:
Yoga for PCOS has a 360-degree healing effect. It regulates your hormonal levels, eases symptoms of menstrual pain, enhances your reproductive, metabolic, and digestive health, and alleviates stress. Incorporating yoga asanas for PCOS treatment in your daily workout routine is a powerful step in the right direction for long-term and effective PCOS management.
2 notes
·
View notes
Text
5 symptoms may be early signs of diabetes
(5 symptoms may be early signs of diabetes) - https://www.healthcol.com/5-symptoms-may-be-early-signs-of-diabetes/- Health col- #EarlySignsOfDiabeticFeet, #HowToTestForDiabetes, #PageNavigation, #Type1DiabetesSymptoms, #Type2DiabetesSymptoms, #WhatAreThe3MostCommonSymptomsOfUndiagnosedDiabetes, #WhatAreTheEarlySignsOfDiabetesSymptomsOfDiabetesType2InAdultsUnusualSymptomsOfDiabetes - https://www.healthcol.com/5-symptoms-may-be-early-signs-of-diabetes/
#early signs of diabetic feet#how to test for diabetes#Page navigation#type 1 diabetes symptoms#type 2 diabetes symptoms#what are the 3 most common symptoms of undiagnosed diabetes?#what are the early signs of diabetes? symptoms of diabetes type 2 in adults unusual symptoms of diabetes
0 notes
Text
The Symptoms of Gluten Intolerance You Haven’t Heard About
You just don’t feel good. You’re tired and get frequent headaches, have ongoing skin issues, or struggle with depression—or all of the above. Maybe you’ve wondered if gluten could be the culprit, but because you don’t experience gastrointestinal upset, you’ve since put the thought out of your mind and haven’t mentioned anything to your doctor. Or perhaps you’ve shared your suspicion, but conventional testing ruled out celiac disease (CD) and thus, supposedly, any issues with gluten. In either case, your diet has likely stayed the same … and so have these often-overlooked symptoms of gluten intolerance.
Yes, all of the symptoms mentioned here—and many others you may not have heard about—can be signs that you have a significant degree of gluten intolerance. Even if you don’t run to the bathroom right after enjoying a plate of pasta, and even if standard lab work says otherwise, your body (and brain) may be having serious problems with gluten. Let’s explore these lesser-known symptoms and discuss if going gluten free is right for you.
You’ve heard of the havoc gluten can wreak on your digestive tract, but did you know that gluten intolerance can cause skin problems, depression, and frequent headaches? Check out this article for more symptoms of gluten intolerance you’ve never heard of. #nutrition #chriskresser
Undiagnosed Intolerance Is More Common than You May Think
First off, I want you to know that if you eat gluten and you feel lousy but you don’t have digestive issues—and you have tested negative for CD and been told it’s all in your head—you are not alone. In fact, undiagnosed cases of gluten intolerance are incredibly widespread. Here’s why.
As I’ve written before, wheat contains several different classes of proteins: gliadins (of which there are four different types, including one called alpha-gliadin); glutenins; agglutinins; and prodynorphins. Once wheat is consumed, enzymes in the digestive tract called tissue transglutaminases (or tTGs) help break down the wheat compound. During this process, additional proteins are formed, such as deamidated gliadins and gliadorphins (also called gluteomorphins). Stick with me here—these terms are worth knowing so that you can understand the pitfalls of conventional testing for CD.
CD is a serious form of gluten intolerance, one that can do real damage to the tissues in the small intestine (though its symptoms aren’t merely gut related). CD is characterized by an immune response to one specific gliadin (the aforementioned alpha-gliadin) and one specific type of transglutaminase (tTG-2). But people can—and very much do—react to several other components of wheat and gluten.
Therein lies the problem, because conventional lab testing for CD and gluten intolerance only screens for antibodies to alpha-gliadin and tTG-2.
If your body reacts to any other wheat protein or type of transglutaminase, even severely, you’ll still test negative for CD and intolerance.
Statistics suggest that for every one case of CD that is diagnosed, 6.4 cases remain undiagnosed—the majority of which are atypical forms without gastrointestinal symptoms; even many patients who are eventually diagnosed don’t experience an upset stomach after consuming gluten. (1)
What’s more, the distinct autoimmune response to wheat proteins and transglutaminase enzymes in the gut that defines CD is just one possible expression of gluten intolerance. The many other ways a sensitivity to gluten can affect the body are collectively referred to as non-celiac gluten sensitivity, or NCGS. Cases of gluten intolerance classified as NCGS involve both intestinal and non-digestive reactions to gluten that are not autoimmune or allergic in nature and that resolve when gluten is eliminated from the diet.
There is no definitive diagnostic test for NCGS, making it difficult to put a number on its prevalence. By some estimates, it may occur in as many as one in 20 Americans. (2) And although your doctor and plenty of others out there might still insist that NCGS doesn’t truly exist, several studies have validated it as a distinct clinical condition. (3) As I’ve explained previously, gluten sensitivity is very real. Stories painting NCGS as a collective delusion have gotten it wrong.
Decoding Your (Real) Symptoms
Gluten intolerance can affect nearly every tissue in the body, including the brain, skin, endocrine system, liver, blood vessels, smooth muscles (found in hollow organs such as the intestines), and, yes, stomach.
That’s why it can manifest either in the classic presentation of digestive distress—abdominal pain, bloating, gas, and diarrhea or constipation—or in any of the following, likely surprising, non-digestive symptoms.
Anemia
Although it’s discussed infrequently in popular articles, iron-deficiency anemia is well documented as a symptom of gluten intolerance in scientific studies. (4, 5) In fact, research suggests that it may often be the first noticeable symptom of CD and that up to 75 percent of those with an anemia diagnosis may be gluten intolerant. (6, 7) Gluten intolerance can interfere with the uptake of iron from food, causing malabsorption of this important nutrient. (8) What’s more, because anemia generally saps one’s energy, it can trigger or worsen the next non-digestive sign of gluten intolerance on this list.
Fatigue
Many gluten-intolerant individuals report feeling tired and fatigued, especially right after eating, you guessed it, gluten. (9) Research has linked NCGS to chronic fatigue symptoms in some people. (10) As with chronic fatigue syndrome, symptoms of gluten intolerance can also include muscle fatigue and muscle and joint pain.
Brain Fog
This type of cognitive dysfunction can be a sign of gluten sensitivity. Those affected often describe experiencing “foggy mind” symptoms such as an inability to focus and concentrate; some also describe feeling mentally fatigued. (11, 12)
Headaches
Headache is a frequent finding in NCGS, with one recent study reporting the symptom in more than half of its participants. (13, 14, 15) Migraine in particular is an associated symptom. (16, 17)
Eczema and Other Skin Disorders
As with fatigue, brain fog, and headaches, people with NCGS may notice a worsening of skin symptoms such as eczema, rash, and undefined dermatitis after ingesting gluten-containing foods. The most commonly reported skin lesions include those similar to subacute eczema, as well as the bumps and blisters indicative of dermatitis herpetiformis, or Duhring’s disease—to which CD is closely linked. Those who are gluten intolerant may also experience scaly patches resembling psoriasis. Lesions are typically found on the muscles of the upper limbs. (18, 19, 20)
Depression and Anxiety
One of the main reasons gluten sensitivity often goes unrecognized and untreated, researchers theorize, is because mental health issues can be a hallmark of this condition. Data suggests that up to 22 percent of patients with CD develop such dysfunctions, with anxiety and depression occurring most commonly. One study found that CD patients were more likely than others to feel anxious in the face of threatening situations, while additional research has linked conditions such as panic disorder and social phobia to gluten response. Depression and related mood disorders appear to occur with both NCGS and CD. (21, 22)
Here’s the good news: The majority of studies cited here not only investigated whether or not these symptoms are signs of gluten intolerance, but also whether or not they can be addressed by going gluten free. And it turns out, these problems improved or completely resolved with adherence to a gluten-free diet.
But more on that in a minute.
Beware These Surprising Consequences of Intolerance
While the symptoms mentioned above are what will most likely clue you in to your body’s negative response to gluten, they aren’t the only effects of intolerance to be aware of. In fact, a variety of chronic diseases may develop due to long-term CD or NCGS, including: (23, 24)
Epilepsy
Attention-deficit hyperactivity disorder, or ADHD
Autism spectrum disorders
Schizophrenia
Type 1 diabetes
Osteoporosis
Multiple sclerosis
Hashimoto’s
Peripheral neuropathy
Amyotrophic lateral sclerosis, or ALS
In one study, researchers found a strong link between gluten sensitivity and neurological complications—especially those in which the cause was unknown. (25) Research has even shown that, for some people with gluten sensitivity, the primary symptom they experience is a neurological dysfunction. (26) The data suggests that nearly 60 percent of people with neurological dysfunction of unknown origin test positive for anti-gliadin antibodies. (27)
Challenge Yourself: Do You Feel Better On a Gluten-Free Diet?
If you’re currently experiencing any of the symptoms of gluten intolerance I shared in this article and can’t seem to find relief, or if you have received a diagnosis of any of the above linked diseases or disorders and you and your doctor have not found a probable cause or resolution, gluten could very well be a trigger for you.
Because of the limitations of current testing for CD and the lack of diagnostic options for NCGS, the most reliable test for gluten intolerance is a “gluten challenge.”
This involves removing gluten from your diet completely for a period of at least 30 days—60 days is best—then adding it back in after that time has elapsed. If your symptoms and/or diagnosis improve during the elimination period and return when gluten is reintroduced, let your healthcare provider know. You have NCGS or atypical CD.
Though I consider this to be the gold-standard test for gluten intolerance, Cyrex Laboratories does offer a comprehensive blood panel that screens for all of the wheat and gluten proteins and transglutaminase enzymes discussed earlier. It can be a helpful diagnostic tool, but it shouldn’t replace a gluten challenge. (Note: It must be ordered by your physician or another healthcare provider.)
How Will You Deal with Your Symptoms of Gluten Intolerance?
If you experience improvement on a gluten-free diet and plan to continue eating this way, you can feel confident that there is no risk in terms of nutrient deficiencies to removing gluten from your diet. (28) If anything, my experience has shown me that people who eat gluten-free are more likely to increase their intake of essential nutrients, especially if they replace breads and other flour products with whole foods.
Have you experienced any of these symptoms? Are you planning a gluten challenge to determine once and for all if gluten is the culprit? Let me know below in the comments!
The post The Symptoms of Gluten Intolerance You Haven’t Heard About appeared first on Chris Kresser.
Source: http://chriskresser.com
November 20, 2018 at 09:17PM
5 notes
·
View notes
Text
Sleep Apnoea – YES OR NO?
As we have been breaking down many myths and beliefs by the valuable advancement in science, we should learn better about the basic necessity of our body – SLEEP- the first thing people compromise on for the daytime work. Worst case scenario, they take it as a waste of time and want to sleep the least to function for extra hours.
The importance of good quality and quantity of sleep needs to be understood better. There are many myths about sleep but what we are discussing here is the one that can impact health severely.
Myth: Snoring is a sign of deep and sound sleep.
Fact: Snoring isn’t good for anyone as it is caused by an obstruction in the airway during sleep as the muscles relax that keeps vibrating the soft tissues in your mouth, nose, and throat causing loud noises and even disruption of sleep.
Definition: Snoring can be often associated with a sleep-related disorder that is SLEEP APNEA which is defined as repeated cessation of breathing for 10 or more seconds with or without significant de-saturation during sleep.
Sleep apnea can be obstructive or central or mixed, obstructive sleep apnea (OSA) being the most common one About 80 percent to 90 percent of adults with OSA remain undiagnosed.
What is OSA?:
Repeated blockage of the upper airway by the collapse of the soft tissue of throat and tongue, causing complete or partial cessation of breathing for 10 or more seconds (even for a minute or more at a time) with or without de-saturation is called obstructive sleep apnea. If this occurs more than 15 to 30 times per hour it is severe and needs to be paid attention to.
HOW DO WE RECOGNISE OBSTRUCTIVE SLEEP APNEA? :
Often OSA is recognized by those at home who observe you sleeping. OSA can have night and day time symptoms:
Nighttime symptoms: Loud snoring, choking/gasping during sleep, sudden breath pauses related arousals, dry mouth, and headache.
Daytime symptoms: waking up with headaches, excessive daytime sleepiness, irritability, mood swings, memory loss, short temper, anxiety, and eventually depression.
WHY DO WE NEED TO TREAT IT?:
In addition to short term effects of OSA like excessive daytime sleepiness, headaches, mood swings, anxiety, irritation, etc. other long term consequences of OSA are:
High blood pressure
Heart disease
Stroke
Pre-diabetes and diabetes
Depression
ARE YOU AT RISK OF HAVING OSA? :
Risk factors that contribute to high chances of OSA:
Overweight (Body Mass Index of 25 to 29.9) and obese (Body Mass Index of 30 and above)
Neck circumference 17 inches (40cm) or more for men, 16 inches (35cm) or more for women.
Habits like alcohol and smoking.
Middle-aged and older men
and post-menopausal women
People with abnormalities of the bony and soft tissue structure of the head and neck
Adults and children with Down Syndrome
Children with large tonsils and adenoids
Anyone who has a family member with OSA
People with endocrine disorders such as Acromegaly and Hypothyroidism
A person suffering from nocturnal nasal congestion due to abnormal morphology, rhinitis, or both.
DIAGNOSTIC TESTS OF OSA?:
People who snore and have excessive daytime somnolence should undergo the diagnostic tests of OSA.
Level 1
In-laboratory, technologists attended polysomnography. (Gold-standard). It records brain waves (EEG), the oxygen level in your blood, heart rate, and breathing, as well as eye and leg movements during the study. It can also be used to diagnose periodic limb movement disorder, narcolepsy, chronic insomnia, and REM sleep behavior disorder.
Level 2
Full polysomnography is done at the comfort of your home.
Level 3
Portable monitoring with three or more channels, including pulse oximetry, heart rate, asses airflow, and thoracoabdominal movements. Used for screening in patients at high risk of OSA.
The AHI is the number of times you have apnea or hypopnea during one night, divided by the hours of sleep.
Normal sleep: An AHI of fewer than 5 events, on average, per hour
Mild sleep apnea: An AHI of 5 to 14 events per hour
Moderate sleep apnea: An AHI of 15 to 29 events per hour
Severe sleep apnea: An AHI of 30 or more events per hour
HOW DO WE MANAGE OSA?
Mild OSA can be managed with weight management, diet control, avoiding supine position, avoiding personal habits like smoking and alcohol, and some oropharyngeal exercises.
Moderate and severe OSA can be managed with PAP THERAPY which is the positive airway pressure that is given by a device and delivered to the patient using a nasal or oro-nasal mask. This air pressure keeps the airway open during sleep thus improving sleep quality, and normalizing the apnea-hypopnea index (AHI) and oxyhemoglobin saturation levels. Along with PAP therapy, diet control, weight management, and lifestyle changes are also recommended.
CONCLUSION:
To conclude we can say that sleep is as essential as food and exercise to our body. If we get the proper quantity and quality of sleep, we can work efficiently even during the day and enhance productivity. The most prevalent, and majorly unrecognized, the underdiagnosed sleep-related disorder is Obstructive sleep apnea which often occurs with repetitive snoring, choking, or gasping during the night followed by morning headaches, excessive daytime sleepiness, and severe mood swings like irritation, memory problems, and anxiety. Obesity and male gender are at high risk of having OSA. If left untreated, OSA can lead to heart diseases, high blood pressure, diabetes, stroke, and depression. To diagnose it level 1 to level 3 of overnight sleep study can be done at our center. PAP therapy is the gold standard therapy that is recommended along with behavioral and lifestyle changes to manage the signs and symptoms of OSA.
To seek help or know more about your sleep apnea, you can visit the Neurology and Sleep Centre, the 1st sleep centre in the country accredited by the Indian Board of Sleep Medicine at L-23, Hauz Khas Enclave, New Delhi, Delhi-110016 (INDIA)
0 notes
Text
Is Pre-diabetes reversal possible?

Take a moment! Being diagnosed with Pre-diabetes can be shocking.
Pre-diabetes is a serious condition, with no clear symptoms, which can go undiagnosed for years. Pre-diabetes implies that the body’s risk for Type 2 Diabetes and several diseases has increased. However, don’t lose hope yet. With the right lifestyle changes, one can prevent pre-diabetes naturally.
Hence, the answer to “Is Pre-diabetes Reversal Possible?” is:
Yes, Pre-diabetes Reversible is Possible.
Risks associated with Pre-diabetes:
Do not be fooled by “Pre” in the name, Pre-diabetes is a serious condition that implies that you have higher than normal blood sugar levels (a fasting blood sugar level from 100-125 mg/dL for 5.6 to 7.0 nmol/L).
If left untreated, the fasting blood sugar level of 126 mg/dL (7.0 mmol/L ) or higher can be reached implying Type 2 Diabetes. Apart from that, it increases risk of Alzheimer’s disease, some cancers, serious damage & failure of heart, brain, nerves, eyes, and ears.
Let’s understand what causes pre-diabetes:
The exact cause of Pre-diabetes is yet to be discovered. However, some risk factors for Pre-diabetes should be taken into consideration.
Some of these factors can be managed like an unhealthy lifestyle which is the most common cause of Pre-diabetes. One can work on factors on factors like:
being physically active less than 3 times a week,
poor sleep cycle,
unhealthy diet,
and obesity, for pre-diabetes reversal
But there are some risk factors which are not in human control:
Being 45 years or older.
Being a relative (child, brother, or sister) to someone with type 2 diabetes,
Being diagnosed with Gestational diabetes (diabetes during pregnancy), or having given birth to a baby who weighed more than 9 pounds,
Being diagnosed with PCOS or Polycystic Ovary Syndrome or obstructive sleep apnoea.
How to reverse Pre-diabetes naturally?
Pre-diabetes is an indicator of the body’s reaction to insulin and a warning sign for upcoming complications, however, one can still use the warning signs to manage blood sugar levels and prevent diabetes.
The Right Diet:
Diet is one of the most important aspects of our lifestyle and has a significant role in Pre-diabetes reversal. Eating healthy food which is low in fat and high in fibre like fruits, vegetables and whole grains can help you achieve your weight loss goals. Avoid foods with added sugars in them (sugary drinks, cookies, candy).
Losing weight and being physically active:
Being overweight is a risk factor for Pre-diabetes. Losing even 5% to 7% of your body weight, about 6.4 kilograms if you weigh 91 kilograms, can lead to Pre-diabetes reversal and reduce the risk of Type 2 Diabetes. Pre-diabetes and physical activity are also closely associated. With the right diet, adding 30 minutes of moderate-intensity physical activity in a day can be highly effective to lose excess weight.
Stress Management
Click on the link below to read further:
https://zivov.com/blogdetail/cbd9a259-44bc-4ad9-9892-02f7b3ec5570
1 note
·
View note
Text
Gluten Intolerance, Wheat Allergies, and Celiac Disease - It's More Complicated Than You Think
Is “gluten free” a fad? No, it’s going to be a thing for as long as we are producing wheat and bread the way we’re doing it. A lot has changed in the bread industry – it’s not just one thing.
People often comment about how bread didn’t cause problems with our health before GMOs and Roundup were prevalent in our food supply. Our farming practices have changed, and fairly recently, wheat has started being sprayed with Roundup. The newest speculation is that wheat is not the problem – that the problem is glyphosate, the active ingredient in Roundup. People also often suspect that wheat has been genetically modified. And, of course, there are those who believe the whole gluten-elimination thing is ridiculous and that most people are jumping on the gluten-free bandwagon because it’s trendy.
Related: How to Eliminate IBS, IBD, Leaky Gut
In my experience, if one suffers from a chronic illness of any kind, they must remove gluten from their diet in order to get well. I have yet to see an exception. So what’s the problem? Is it the glyphosate or the wheat or something else? The truth is it’s not just one thing. Everyone would already know this if most humans weren’t so bad at thinking in terms of systems. We tend to think linearly and look for singular cause and effects, but rarely if ever are complex problems solved by such simplistic thinking. There are multiple reasons one gets sick, with a cold or a chronic disease, just like there are multiple reasons why our planet’s ecosystem is changing. This is why you can’t blame the rise of autism on just glyphosate, or GMOs, or increased vaccinations, or diminishing food quality, or environmental degradation – they all correlate, it’s all of the above.
Related: Best Supplements To Kill Candida and Everything Else You Ever Wanted To Know About Fungal Infections
There is a very complex system that is causing the decline of American health, and it’s not just the bread. And yes, our health is in decline. If you doubt that…here, google it and take your pick. Our lifespan is actually decreasing.
What’s the difference between Gluten Intolerance, Wheat Allergies, and Celiac Disease
Conventional medicine states that celiac disease and non-celiac gluten sensitivity have a lot of symptoms in common but identifies a key difference. Non-celiac gluten sensitivity is not a genetic disease and does not cause an autoimmune reaction, and celiac disease is a genetic autoimmune disease. A wheat allergy is an allergic reaction to any of the hundreds of proteins in wheat. Gluten intolerance used to be a catch-all phrase for any problem with eating gluten, but now it’s being relegated to mean Non-celiac gluten sensitivity.
Non-celiac Gluten Sensitivity
Non-celiac gluten sensitivity is believed to be the most prevalent of the gluten-related disorders, but it’s not as well defined as the other two. It’s not an autoimmune reaction nor is it an allergic reaction. There are no tests or biomarkers to identify this disorder. Other components of gluten-grains may be causing symptoms. In order for non-celiac gluten sensitivity to be diagnosed, a doctor will rule out celiac disease and wheat allergies or other possible causes of the symptoms first.
Common Symptoms for Non-celiac Gluten Sensitivity
Fatigue
Mental fatigue, aka “brain fog”
Headaches
Migraines
Bone or joint pain
Gastrointestinal distress
Gas
Bloating
Cramping
Indigestion
Abdominal pain
Diarrhea
Constipation
It’s said that individuals with gluten sensitivity do not experience damage to the small intestine or develop tissue transglutaminase antibodies like they do with celiac disease. Non-celiac gluten sensitivity has been linked to a variety of health problems including, diabetes, allergies, autism spectrum disorders, and much more.
Related: How to Avoid GMOs in 2018 – And Everything Else You Should Know About Genetic Engineering
Gastroenterologists looking for celiac disease typically test for a few specific antibodies, and if found, they do an intestinal biopsy to determine if tissue damage is present. Chris Kresser addresses the issue with this kind of testing in 3 Reasons Gluten Intolerance May Be More Serious Than Celiac Disease, which I highly recommend reading. He states:
According to some estimates, for every diagnosed case of celiac disease (CD), there are 6.4 undiagnosed cases that remain undiagnosed—the majority of which are atypical or “silent” forms with no damage to the gut. (1) This silent form of CD is far from harmless; it is associated with a nearly fourfold increase in the risk of death. (2)
I believe that patients with NCGS are even more likely than patients with CD to go undiagnosed. Most gastroenterologists today know how to screen for celiac disease. They will typically test for antibodies to antibodies to alpha gliadin, transglutaminase-2, deamidated gliadin, and endomysium, and if positive do a biopsy to determine if tissue damage is present.
However, we now know that people can (and do) react to several other components of wheat above and beyond alpha gliadin, the component that is implicated in CD. These include other epitopes of gliadin (beta, gamma, omega), glutenin, wheat germ agglutinin (WGA), gluteomorphin, and deamidated gliadin. What’s more, people can react to other types of tissue transglutaminase, including type 3—primarily found in the skin—and type 6—primarily found in the brain. (3, 4, 5, 6, 7, 8)
Celiac Disease
Celiac disease is considered a genetic, autoimmune disorder. Ninety-eight percent of people with celiac disease carry one or both of two very specific genes, HLA DQ2 and DQ8. On the other hand, so does up to 25-30% of the general population. Carrying one or both of these genes does not mean you have celiac disease nor does it mean you will develop it. Doctors often use gene testing to rule out celiac disease, but there are some cases where people who do not have either of the genes still tested out to have celiac disease.
Though celiac disease is said to be genetic, genes cause predispositions and our diet and environment adjust our genes. Environment can alter gene activity without changing the DNA sequence. This is called gene expression. I also believe that the environment and diet can actually alter the DNA sequence, but from what I’m seeing, current science doesn’t agree with me on this. Regardless, how your genes affect you is altered by our diet and our environment, and those traits can be passed down to our offspring as well. In other words, a predisposition to celiac disease may be hereditary, but whether or not we have celiac disease could depend on our genetic health, which depends on our overall health, which depends on our lifestyle. And this can all be traced to gut health – you cannot have a healthy gut without a healthy lifestyle, and our gut health is something most of us have complete control over.
Related: Gluten, Candida, Leaky Gut Syndrome, and Autoimmune Diseases
Common Symptoms of Celiac Disease
Fatigue
Mental fatigue, aka “brain fog”
Headaches
Migraines
Bone or joint pain
Gastrointestinal distress
Gas
Bloating
Cramping
Indigestion
Abdominal pain
Diarrhea
Constipation
Arthritis
Dermatitis
Eczema
Osteoporosis
Liver disorders
Depression or anxiety
Peripheral neuropathy
Seizures
Migraines
Irregular menstruation
Miscarriages
Canker sores
Doctors believe that in order to develop the disease, a person needs to have the genetic predisposition while they are consuming gluten and to subsequently have the disease activated. Activation triggers are said to potentially be stress, trauma, and viral infections. I contend that vaccines and antibiotics are the two most common triggers for the disease. Damaging the gut is what leads to problems with wheat, but we’ll get more into that below.
Wheat Allergies
Celiac disease and non-celiac gluten sensitivity have many symptoms in common, but wheat allergies are often much more distinctive. Symptoms include itching, hives, or anaphylaxis which is a life-threatening reaction. A wheat allergy is an immune reaction to any of the hundreds of proteins in wheat. It is possible for a person to be allergic to wheat and to have non-celiac gluten sensitivity or celiac disease at the same time.
What About Roundup?
Monsanto introduced glyphosate under the trade name Roundup in 1974 shortly after DDT was banned. It wasn’t used very much until the late 1990s when Monsanto genetically engineered seeds to withstand high doses of Roundup, and the product took off. Eager to sell more of its flagship herbicide, Monsanto has encouraged farmers to use their glyphosate as a desiccant. Wheat can be harvested quicker and easier if you dry it all out ahead of time with Roundup. It’s also used in this way on wheat, barley, oats, canola, flax, peas, lentils, soybeans, dry beans, and sugar cane.
Studies have concluded that chronically ill people have higher levels of glyphosate in their bodies. Glyphosate has been attributed to an increased prevalence of most of our common chronic conditions including, but not limited to ADHD, Alzheimer’s, birth defects, autism, cancer, kidney disorder, irritable bowel syndrome, Parkinson’s disease, depression, diabetes, heart disease, thyroid disorders, liver disorders, multiple sclerosis, reproductive issues, adrenal failure, obesity, asthma, and of course, celiac disease.
It’s not hard to understand why. Glyphosate is poison and so are the other ingredients in Roundup. People have to wear protective gear to apply the product. It is designed to kill. It kills plants by preventing them from making certain proteins. Just imagine what that does to one’s gut ecology.
How Wheat Has Changed
The wheat we have now is very different from what our ancestors consumed. Modern dwarf wheat is hybridized. That isn’t a GMO, but the genes of our wheat plant have certainly been modified to grow faster, and to be more resilient. We used to eat wheat called einkorn, which was actually one of the very first grains we humans cultivated more than 10,000 years ago. When you read in the Bible about how we should eat bread, this is the wheat it refers to.
There is a lot more gluten in modern wheat than there is in einkorn, and the gluten that einkorn wheat does contain is different. Einkorn also has 15 percent less starch and 30 percent more protein. Modern wheat has a lower nutrient content and a different protein structure. In fact, many with celiac and gluten intolerance report being able to eat einkorn without issue.
Also, that blood sugar spike experienced after eating bread does not happen with einkorn.
So I conducted a simple experiment on myself. On an empty stomach, I ate 4 oz of einkorn bread. On another occasion I ate 4 oz of bread that dietitian, Margaret Pfeiffer, made with whole wheat flour bought at the grocery store. Both flours were finely ground and nothing was added beyond water, yeast, olive oil, and a touch of salt.” – Einkorn and blood sugar
“Ancient wheat diets caused a downregulation of key regulatory genes involved in glucose and fat metabolism, equivalent to a prevention or delay of diabetes development. Spelt and rye induced a low acute glycemic response compared to wheat.” – NCBI
How Bread Making Has Changed
Most commercial bread contains bromides, added starches, refined sugars, added gluten (vital wheat gluten), preservatives, artificial flavorings, leveling agents, and stabilizers. Potassium bromate is an additive used in commercial bread and baked goods that make the products lighter and fluffier. Bromines are part of the halide family, a group of elements that includes fluorine, chlorine, and iodine, which are all endocrine disruptors that cause digestive issues and a host of other health problems.
Related: Sugar Leads to Depression – World’s First Trial Proves Gut and Brain are Linked (Protocol Included)
Baking Soda, baking powder, and cream of tartar are often used in place of yeast or in addition to rapid rise yeast to make the bread rise quickly and more uniformly. Modern bread rises for a couple of hours or less, whereas homemade bread traditionally takes at least 12 hours to rise. I got curious about the difference between baking soda and baking powder, and I thought you might be as well, hence the video below.
youtube
Traditional bread recipes typically utilized a few common ingredients including flour, yeast, salt, water, a sweetener, and some spices or herbs.
Related: Holistic Guide to Healing the Endocrine System and Balancing Our Hormones
Refined flours started to be widely used around 1880 which caused worldwide epidemics of pellagra and beriberi. Refining the flours removes bran and germ which increases shelf life. It also removed the B vitamins. Previous iterations of bread did use bolted or sifted flour which did refine the wheat somewhat, but it didn’t remove all of the bran, germ, and endosperm, and that flour was never bleached.
Bread with Whole Grains that are gently stone ground just before mixing the dough and then allowed to ferment slowly and naturally, in other words — authentic sourdough. That’s how the Egyptians made it 6,000 years ago.”
Bread was fundamentally redesigned. Refined flours, large quantities of commercial yeast, and a combination of additives and intense energy created the modern industrial bread. Fast mixing, fast rise, fast baking. Industrial bread is made far too fast.” – Mario Repetto
How Our Gut Biology Has Changed
We keep eating more and more sugar. In the early 1700s, the average sugar consumption was about 4 pounds a year. By 1800 we were at 18 pounds a year. By 1900 we were up to 60 pounds of sugar a year. Today the average American consumes between 130 and 150 pounds of sugar every year.
Sugar feeds pathogens. Our healthiest gut bacteria like the healthiest foods: vegetables and herbs. Nature wouldn’t work any other way; how could it? You’re probably thinking, “What about fruit?” We don’t eat the fruit we used to eat. Like wheat, our fruit has been radically altered through hybridization. But that’s another article (I’m working on it). For now, just Google “wild banana” or “what watermelon used to look like“.
We get way more sugar than our ancestors got even if we cut out refined foods. This causes an abundance of Candida. I believe Candida is prevalent in every single person with chronic illness. Everyone has yeast but when yeast is left unchecked they turn into pathogenic fungi. Tests for Candida aren’t accurate. Candida, when in it’s in the virulent fungal form, will make the gut more permeable. When this happens food proteins are absorbed into the body before they are digested. This causes allergies. This is one of the main causes of allergies, but there are others at play as well. In my experience, every single person who has cut refined sugar out of their lives and decreased their body’s Candida was able to rid themselves of seasonal, environmental, and food allergies. Every single time!
In addition to that, a study published in The Lancet showed that the candida protein HWP-1 is similar in structure to gluten.
A candida infection in the gut can cause an immune system reaction to HWP-1, which then stimulates an allergic reaction to the gluten in wheat and other grains and may trigger celiac disease in genetically susceptible people.” – Leyla Muedin, RD
Wheat proteins can also cause an immune response against the thyroid.
An obvious explanation is that the initial attack on the thyroid by anti-tTG autoantibodies of celiac leads to thyroid inflammation and presentation of TPO, with a second round of autoantibodies produced to TPO resulting in Hashimoto’s Thyroiditis.” – Dr. Art Ayers
Celiac disease and hypothyroidism beget more chronic autoimmune issues. Allergies lead to autoimmune disease. Allergies lead to chronic health issues. Medical science has established this. Medical science is just starting to understand the fact that a permeable gut causes allergies. Science also has established that an abundance of Candida causes a permeable gut. What they haven’t figured out yet is just how prevalent the permeable gut issue really is. But the bottom line is that our poor diet leads to allergies and almost all that commonly ails us.
Suggestions
If you have a healthy gut, make your own sourdough bread using heirloom wheat and the old-school practices. If you have any chronic illness, then you do not have a healthy gut. Here’s how you fix it. If you’re not well, wait until you get well before consuming any kind of bread. And don’t think of old-fashioned bread as healthy. Vegetables are healthy. Bread is at its best a neutral food with some health benefits and easy calories that can help sustain life like brown rice and millet. Vegetables and herbs heal the body.
Obviously, stay the heck away from poisons! Glyphosate is a cocktail of poisons. Science has firmly established this. And avoid GMOs as well. They weren’t designed with our health in mind, they were designed for profit, and in most cases, to sell more Roundup.
The hard truth is that letting companies cook your food for you leads to poor health. People often ask me, “If you can cure cancer why aren’t you rich?” If I could cure cancer and figure out how to do it while still eating refined, prepackaged, and processed foods that we humans have grown accustomed to, I would be rich. But people would rather die for convenience food than give it up. Obviously. We see this everywhere.
Being well long-term means preparing all your own food yourself the right way, or being rich and hiring someone else to do it. There is no shortcut. Certainly not with bread.
Sources:
Your Ancestors Didn’t Eat The Same Type Of Wheat That You Do (And They Were Healthier) – Off The Grid News
4 Ways Modern Bread is Different From Traditional Bread – Our Heritage of Health
The Real Problem With Bread (It’s Probably Not Gluten) – Mother Jones
Problems Linked to Monsanto’s RoundUp – EcoWatch
15 Health Problems Linked to Monsanto’s Roundup – EcoWatch
Consumption of Sugar – Sugar and Sweetener Guide
Gluten Intolerance, Wheat Allergies, and Celiac Disease – It’s More Complicated Than You Think was originally published on Organic Lifestyle Magazine
3 notes
·
View notes
Text
Why Is Sleep Important And What Is It Good For?
If you’re wondering Why Is Sleep Important And What Is It Good For? Well, according to the Canadian Medical Association, about one-quarter of Canadians are losing sleep over financial worries.
In fact, over 50% of people who come into sleep clinics complain of insomnia due to financial worries.
Covid-19 anxiety is also taking an emotional toll and affecting the sleep of individuals. There is increased uncertainty of the future and a lack of connection with usual supports. People are struggling with self-isolation financial hardship, worries of oneself or one’s family getting infected and people cannot escape the constant, barrage of news stories on this potential threat. More and more we are being asked to turn to screens to function. Yet studies show increased social media at night increases feelings of anxiety, depression, and low self-worth in adolescents with 90% of these adolescents who struggle with anxiety reporting sleep problems.
Sleep difficulties can be the result of stress or they may be symptomatic of an underlying psychiatric condition. Difficulties with sleep may be a diagnosable condition on there own such as Insomnia, Hypersomnia, Restless Leg Syndrome, Obstructive Sleep Apnea, or Night Terrors. When an individual has trouble sleeping one also has to consider whether the sleep problem is a condition on its own that needs to be treated or is it a symptom of another condition such as a Mood Disorder, PTSD, Substance Use Disorder, or some other undiagnosed neurological condition. Sleep and mental health have a bidirectional relationship. Sleep problems can precipitate or worsen mental health or may cause them.
One thing is certain that sleep difficulties will result in impairments in one’s life by causing daytime fatigue, loss of interest, depressed mood, poor concentration, worry, agitation, and irritability. Studies have shown that the risk of developing major depression is much higher in those who have insomnia and insomnia is the most common symptom that predicts PTSD in U.S. service members returning from military deployment. As well as independent treatment of insomnia in Major Depression improves depression treatment outcomes.
Sleep timing quality and quantity are controlled via a homeostatic drive that builds up during waking and circadian rhythm that is usually linked to the light-dark cycle to promote sleep. Sleep can be disrupted by inconsistent bedtime and wake times, dozing in the evening, spending excessive time in bed, sleep-related anxiety, clock watching, excessive use of night-time screens. Adolescents are known to have a delayed sleep phase because they stay up late gaming and or watching screens. and communicating with others. This leads to difficulty awakening and daytime sleepiness. This is the opposite of the elderly who can have sleep issues because they go to bed too early and wake up too early.
One may wonder why is sleep important for the brain?
Why being deprived of sleep can lead to reduced cognitive function, impaired immune function, feelings of stress, decreased quality of life, obesity, and diabetes. Why being completely deprived of sleep can result in hallucinations and even death. The world record for not sleeping is 266 hours. What is going on in our bodies when we sleep. Functions of sleep include energy conservation and nervous system recuperation. Sleep works with memory consolidation and emotional regulation allowing neuroplasticity in brain development.
Healthy sleep usually involves a period of relaxed wakefulness for up to 30 minutes, and then periods of non-REM sleep and REM sleep. NREM sleep goes through four stages 1-4 with stages 3-4 being marked by slow-wave restorative delta wave sleep. During these periods of slow brain activity, a person is difficult to arouse. REM sleep is marked by increased brain activity and is associated with dreaming. The excessive brain activity during REM sleep is where I believe neurochemicals are being released from synapses. These chemicals stored in vesicles in the neurons build up because of emotional and perceptual stimulation during the day. Thus dreams often can show the events and emotions that have been building up in us and our brains during our days.
In the DSM V Insomnia Disorder or causes of insomnia in males, it requires dissatisfying sleep quality or quantity at least 3x a week for 3 months. Most sleep problems are transient but one in three can last for over a year. Medications are often used when one is having trouble falling or staying asleep. But there are many side effects and risks to medications including abuse and dependence. Even when people use over the counter agents such as gravel, or sedating antihistamines, melatonin, valerian root they are at risk of altering their sleep architecture. Not to mention that when one awakens during the night because of worry or a problem if they are too medicated they will not be able to use their consciousness to think about the issue and perhaps come up with a solution that may benefit them.
Doctors are often quick to prescribe benzodiazepines, melatonin agonists, orexin antagonists, sedating antidepressants, anticonvulsants, and antipsychotics to treat insomnia in their patients. Miscellaneous agents such as prazosin, clonidine, hydroxyzine are also used by psychiatrists to promote sleep. Benzodiazepines such as lorazepam, clonazepam, temazepam, and the Z drugs such as zopiclone, and zolpidem are extremely effective for the short term treatment of sleep problems but ongoing use leads to tolerance escalating doses. This can be followed by physiological and psychological dependence and the risk of synergistic sedation with other sedatives such as alcohol. Benzodiazepines and z drugs, as well as alcohol, stimulate GABA an inhibitory neurotransmitter that the brain uses to lessen neuronal firing. When you use external substances to stimulate GABA the brain stops making it. So, if you stop the pill or the alcohol too abruptly the brain will be GABA deficit, and rebound anxiety and insomnia will result. If a person has been on the substance long enough they can even have seizures from an absolute absence of GABA when they stop their sedatives.
Z drugs such as zopiclone and zolpidem are purported to be safer but even they bring up concerns with complex sleep-related behaviors, increased dementia risks, and increased mortality rates. Sedative use is associated with increased motor vehicle accidents and falls in the elderly, worsened short term memory, and rebound insomnia depend on the dose, and duration of use. Melatonin shows in studies that it does lead to small benefits for insomnia. Orexin is an activating neurohormone that can be blocked by a drug called Suvorexant available in the US to treat insomnia. This drug does not show the same side effect profile of benzodiazepines because instead of increasing Gaba they block the wake-promoting chemical Orexin. Mirtazapine and older antidepressants such as amitriptyline and doxepin are used by doctors to induce sleepiness. They are not abused like benzodiazepines but they cause problems because of daytime sedation, weight gain. Quetiapine is very commonly used in low doses to treat sleep problems. It is quite effective at lessening anxiety but often increases hunger after taken leading to substantial weight gain and emotional blunting.
Cannabidiol or CBD is an active ingredient in cannabis.
It is reported to not cause the high that the THC found in marijuana causes. It is used by people for help with falling asleep and staying asleep. It is also reported to help with pain and inflammation. There are a few studies showing improved sleep in patients taking CBD. My concern would be whether it suppresses REM sleep the same as THC. As I mentioned earlier REM sleep is needed for emotional processing and memory consolidation while sleeping. Regular marijuana use will lead to a lack of emotional development and poor short term memory both deficits could be worsened by THC’s REM suppression qualities. In one study on healthy volunteers, CBD did not affect REM sleep. One must be careful that long term use does not lead to dependency and a diminished effect over time. Sticking to low intermittent use of CBD could minimize this risk.
Alcohol is often consumed socially in the evening or at bedtime.
It can be used as a form of self-medication to promote sleep. It is effects on sleep are dose and time-dependent. Higher doses used near sleep have the greatest impact on sleep. Alcohol acts as a sedative and facilitates sleep onset at the beginning of the night but after the body breaks it down in the liver it results in wakefulness during the night. Alcohol can worsen sleep apnea and it is known to suppress REM sleep early in the night and result in REM rebound later. If alcohol is consumed again during the night to promote sleep, there is a risk of morning impairment and even resultant DUI charges when driving the next day.
Chronic Insomnia requires a thorough evaluation.
One must rule out psychiatric illnesses, medical illness, medication side effects, substance use disorders, issues with poor sleep hygiene. In Major depression insomnia is reported at sleep onset, midnight, and early morning awakening. Depression is also associated with Restless Legs Syndrome. Asleep study for obstructive sleep apnea should be considered when a person has daytime sleepiness, witnessed night-time episodes of not breathing, and refractory hypertension or obesity. Medications known to worsen sleep include antidepressants, stimulants, steroids, bronchodilators, decongestants, and diuretics. Medical illnesses that can worsen sleep include cardiac pain, breathing difficulties, joint pain, diabetes, thyroid difficulties, dementia, and Parkinson’s Disease.
CBT-I is the number one recommended treatment for insomnia.
This involves primarily sleep restriction and reduced time in bed. This increases the sleep drive. CBT-I also uses Stimulus Control to reduce arousal time in bed and advises only going to bed when sleepy. Clinicians work to challenge maladaptive beliefs around sleep and confront catastrophic thinking to make sleep expectations less worrying. Health promotion and relaxation techniques are advocated. To improve sleep hygiene regular exercise and stretching, and breathing exercises, meditation is recommended. Limiting caffeine and alcohol is also important as is keeping the bedrooms dark and quiet and cool. Foods reported to improve sleep include almonds, warm milk, kiwi fruit, chamomile tea, walnuts, tart cherries, fatty fish, barley grass powder, lettuce, calcium, magnesium, B-vitamins, and vitamin D.
The post Why Is Sleep Important And What Is It Good For? appeared first on First Coast News.
from First Coast News https://firstnewsclick.com/why-is-sleep-important-and-what-is-it-good-for/9811414/
from First Coast News https://firstnewsclick.tumblr.com/post/618657905970987009
0 notes
Text
Juniper Publishers- Open Access Journal of Case Studies
What’s the Connection between Diabetes and Depression?
Authored by Berna Nilgün Özgürsoy Uran
Abstract
Depression is a serious medical condition that affects thoughts, feelings, and the ability to function in everyday life.
An internationalreport has shownthathavingdiabetesanddepression has thegreatestnegativeeffect on quality of life comparedtodiabetesordepressionalone, orotherchronicconditions. Because of tahatreasonIt is very important for health professionals to control these diseases to understand the relation of diabetes to depression. The purpose of this review is to draw attention to the relationship between depression and diabetes and to provide literature support to health professionals.
Keywords: Diabetes; Depression; Treatment
Introduction
The increasing burden of diabetes among adults (aged 20–70 years) is a major public health concern globally [1]. The number of people living with diabetes is estimated to rise from 135 million in 1995 to 300 million by 2025. Diabetes is a disorder that impairs the way the body uses digested food for growth and energy. Most of the food we eat is broken down into glucose, a form of sugar that provides the main source of fuel for the body. After digestion, glucose passes into the bloodstream. Insulin, a hormone produced by the pancreas, helps glucose get into cells and converts glucose to energy. Without insulin, glucose builds up in the blood, and the body loses its main source of fuel [1].
Type 1 diabetes is when the immune system destroys the insulin-producing beta cells of the pancreas. This form of diabetes usually strikes children and young adults, who require daily or more frequent insulin injections or using an insulin pump for the rest of their lives. Insulin treatment, however, is not a cure, nor can it reliably prevent the long-term complications of the disease. Although scientists do not know what causes the immune system to attack the cells, they believe that both genetic factors and environmental factors are involved [1].
Type 2 diabetes, which accounts for about 90 percent of diabetes cases in the United States, is most common in adults over age 40. Affecting about 6 percent of the U.S. population, this form of diabetes is strongly linked with obesity (more than 80 percent of people with type 2 diabetes are overweight), inactivity, and a family history of diabetes. It is more common in African Americans, Hispanic Americans, American Indians, and Asian and Pacific Islander Americans. With the aging of Americans and the alarming increase in obesity in all ages and ethnic groups, the incidence of type 2 diabetes has also been rising nationwide [1].Theprevalence of majordepression in the UK population at anyone time is about 5%, although as many as oneperson in threemayexperience an episodeof depression in theirlifetime [2].
There search ersused cognitive therapy to reverse the depression.In those people where depression improved, there was an average HbA1c of 8.3% while those who showed little improvement had an average of 11.3%. While these results show an association between highblood sugars and depression, it remains unclear whether highblood sugars cause the depression or depression causes highblood sugars [2].
Another relatively common and costly central nervous system syndrome, depression, occurs in many patients with diabetes [1]. Depression is a serious medical condition that affects thoughts, feelings, and the ability to function in everyday life. Depression results from abnormal functioning of the brain. The causes of depression are currently a matter of intenseresearch. An interaction between genetic predisposition and life history appear to determine a person’s level of risk. Episodes of depression may then be triggered by stress, difficult life events, side effects of medications, or other environmental factors. Whatever its origins, depression can limit the energy needed to keep focused on treatment for other disorders, such as diabetes [1].
A more recent systematic review and meta-analysis of multiple community-based, large-scale, prospective studies confirmed the significantly increased rates of depression in people with type 2 diabetes relative to control subjects (17.6%vs9.8%, OR=1.6 [95% confidence interval (CI) of 1.2- 2.0]) [3]. Despite the differences between type 1 and type 2 diabetes in age of onset and clinical course, the prevalence rates for type 1 vs type 2 diabetes were statistically similar in the studies that determined depression by diagnostic interview (13.6% vs10.9%, p>0.1) or with self-reportsymptoms scales (29.1%vs32.9%, p>0.1) [4].
Cardiovascular disease is a macro vascular complication of diabetes. An analysis of a large, naturalistic population-based sample of patients with type 2 diabetes in a Large primary care system concluded that patients with major depression and diabetes were 1.5-2-fold more likely to have 3 or more cardiovascular risk factors than patients with diabetes without depression [5].
How Does Depression Affect People with Diabetes?
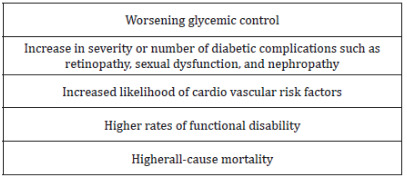
An international report has shown that having diabetes and depression has the greatest negative effect on quality of life compared to diabetes or depression alone, or other chronic conditions (Table 1).
Though the relationship between diabetes and depression isn’t fully understood
The rigors of managing diabetes can be stressful and lead to symptoms of depression.
Diabetes can cause complications and health problems that may worsen symptoms of depression.
Depression can lead to poor lifestyle decisions, such as unhealthy eating, less exercise, smoking and weight gain - all of which are risk factors for diabetes.
Depression affects your ability to perform tasks, communicate and think clearly.
This can interfere with your ability to successfully manage diabetes.
Recent estimates suggest that upto three quarters of cases of depression in people with diabetes may go undiagnosed. During the subsequent decade of 2000-2010,increased Attention focused upon adverse metabolic and thrombo vascularc onsequences of depression through certain biologic path ways.
Relevant in this regard are the hypothalamic-pituitaryadrenal axis hyperactivity and mental stress-induced sympatho medullary activation in many patients with major depression, which can contribute to decreased glucose transport and insulinresistance, respectively.A mechanistic path way between depression, diabetes,and coronary artery disease has been proposed by Steven Roose [7].
Depression causes patients to become inactive, which, combined within creased cortisol levels, causes adiposity, obesity, and insulin resistance. Adipose tissue and damaged vessels then release pro-inflammatory cytokines, which induce the depressive symptoms of the ‘‘sicknessbehavior’’syndrome, which impair a patient’s motivation to initiate healthy self-care behaviors and perturb cognition. Consequently,ever-worsening cycles evolve eventually resulting in a heartattack or stroke associated with type 2 diabete [7].
Treatment Depression and Diabetes
There are multiple conceptual approaches to the diagnosis of major depression in medically ill patients, including the exclusive and inclusive approaches [8]. The exclusive approach maximizes specificity bye liminating so maticsymptoms such as anorexia and fatigue, which frequently are elements of medical disorders [8]. The inclusive approach includes all depressive symptoms to diagnose major depressive disorder in the medically ill and maximizes sensitivity, best protecting the patient from a ‘‘falsenegative result’’ and the risk of undiagnosed depression [8].
Non-depressed diabetic patients may report neurobehaviora symptoms such as diminished appetite, weightloss, hypersomnia, loss of libido and psycho motor retardation [9]. Therefore, the use of exclusive criteria may allow clinicians to more easily identify major depression in diabetic patients [9].
Treatment for depression in people with diabetes has been shown to be effective and has the additional benefits of improving blood sugar control. The evidence suggests that cognitive behaviour therapy and anti-depressant medicines are as effective in people with diabetes as in those with out diabetes. As thetreatment of depression can improve blood sugar control, it is also likely to reduce the risk of complications but importantly, it can also improve quality of life and diabetes self management programs, psychotherapy, medications and lifestyle changes, collaborative care is very important to treatment depression and diabetes (Table 2).
Physicians always need to be cognizant of drug-drug interactions when prescribing medications, particularly in patientswith psychiatric and medical co-morbidities. Due to the inhibition of cytochrome P450 (CYP) 3A4 isoenzyme,certain of these rotoninre uptake inhibitors (SSRIs) such as fluoxetine and fluvoxamine mayalter the metabolism of certain oral hypoglycemics (such as the thiazolidinedione pioglitazone, the meglitinies, repaglinide and nateglinide) and confer a risk of hypoglycemia [9].
In addition, inhibition of the CYP 2C9 isoenzyme by fluoxetine, fluvoxamine, or sertraline may also potentially alter CYP 2C9 metabolism of sulfonylureas tolbutamide and glimepiride [9]. Diabetes nurses can say diabetes self management progrmas is very important to treating depression and diabetes [1].
Conclusion
There is clearly an increased prevalence of depression among diabetic patients [1]. Depressive symptoms serve as a risk factor for the development of diabetes and have been shown to contribute to hyperglycemia, diabetic complications, functional disability and all cause mortality among diabetic patients. Despite the fact that depression complicates medical conditions such as diabetes, there is evidence that diabetes nurse and primary care physicians treat depression less aggressively in patients with medical comorbidities [11].
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.business.site/
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jojcs/JOJCS.MS.ID.555597.php
#Juniper Publishers Contact#Juniper Publishers Address#Obstetrics and Gynaecology#Transplant Surgery#Vascular surgery#Surgical Oncology#Otolaryngology
0 notes
Note
you know... this seems an awful lot like a constant battle you're fighting uphill. I don't have people with diabetes in my environment, and I cannot imagine how difficult it can be every single day... damn. So.. I absolutely respect what you do every day. I'm speechless. I read these pro-con posts and your experiences, and I'm more and more frustrated that there isn't more media coverage, or more awareness raised about these symptoms, and how to help the diabetic community. It's eye-opening
It is a constant battle for sure. You have to deal with it 24/7, and there’s no respite, or vacation. Even if you have your diabetes pretty much in control, you can never stop and take a break, or it’ll get out of control again. My diabetes is pretty much under control at the moment, and to put that into perspective that means I am low 2-3 times a week, and slightly high maybe 1-3 times a week. That’s the best it’s been in a few weeks. That sense of being in control will last about 2 weeks, I dare say, (if I’m lucky), before something will happen to throw it off. Then, it’ll take a couple days to find the right patterns again, if not longer, and it could be anything that caused the fluctuations: An infection, a virus you killed quickly before you really felt it, but still made your sugar levels funny; you could be stressed which raises your blood sugar; you could be tired which raises your blood sugar; you could have walked for ten minutes too long, and that lowered your blood sugar. etc. It’s something you have to constantly watch to make sure you catch everything, and everything you do is relevant to keeping it in line. Even then, sometimes there’s no explanation at all. Then, if you do it all reasonably well, you can hope to have decades before the serious complications set in: (Kidney failure, blindness, nerve damage, etc.)
So, yes, it is difficult, and it is scary. Having said that, you do get used to it. I don’t think about complications, and how taxing it is on a daily basis; I would be downright depressed if I did. I’ve just learned to live with it. The fears are always there, but they’re just something you get so used to it doesn’t really register. You can get used to anything, as they say. However, there do come those bad days when you don’t know why your body is rebelling, and you panic, and feel miserable, because nothing’s going right, and you realise again just how close you are to dying painfully if you’re not careful. Unsurprisingly, there is a high correlation of depression, suicide, and anxiety attacks amongst diabetics. It can be quite stressful.
This is why I get frustrated by the lack of media coverage that you pointed out. It is an issue. Just seeing someone in the media, in a movie, on TV, a character who has diabetes that is represented well mind you, can be a big source of inspiration. It’s someone we can relate to. Someone to make us feel less alone, and someone who can inspire us to keep going. Fiction influences life, and vice versa. Having a diabetic character would help those who have diabetes keep their courage, and would help those who don’t understand what it’s like know how to help. Moreover, it could help them the day they get their diagnosis, and some of them will. It won’t be such an “out there” concept. They’ll have some idea of what to expect. It could probably also prevent needless deaths that come from people who don’t recognise the symptoms. To some, DKA looks like the flu!
This is doubly important because diabetes is becoming an epidemic. More and more people are becoming diabetic everyday, T2D being especially common. People need to be aware of the symptoms. People need to know what to do. People need to know the difference between T1D, and T2D. The former is not preventable, but the latter can be. T2D is linked to obesity, and weight loss can help prevent it. However, in many cases it is also just plain genetic; you can get it without being overweight. Sometimes, it’s as unpreventable as T1D, but either way being careful about your diet, and your exercise may buy you decades of time before you get it. People need to understand all of this. Diabetes is the 7th most common cause of death in the USA, and the 6th most common in in Canada. Nor is it a condition limited to North America, it is a global phenomenon with million and millions of victims. In spite of this, most people don’t know that T1D isn’t preventable, that there is a difference between T1D and T2D, that there are even two different types of diabetes,in other words, the basics.There are something like 7.2 million undiagnosed T2Ds in the USA alone who probably don’t even know what their symptoms can lead to until it’s far to late, and there are many more pre-diabetics who don’t understand that they’re at risk. It’s imperative that people understand what they can and cannot do to help others and themselves. It’s imperative that people know the warning signs. I’m so glad you find this eye-opening, because that is exactly what I was hoping for. Too many people die every year, because of ignorance. We seriously need more coverage of this issue. Diabetes causes more deaths than breast cancer and AIDS combined.
I’m not entirely certain why there isn’t more media coverage about diabetes, but I have two guesses. The first is that until the discovery of insulin in the ‘20s, diabetes was a terminal illness. When insulin was finally made available, it was like this miracle drugs, and everyone thought it made everything better, and didn’t stop to consider how hard diabetes as a chronic illness might be. The truth is, insulin doesn’t make you better; it isn’t a cure-all. It just enables you to survive another day. However, this idea that now you’ve got insulin you’re fine, just don’t eat sugar has prevailed, and has never really left. Secondly, the rise of T2D diabetes has been correlated to the Western diet with emphasis on the fast and processed foods in particular, and I doubt the all-mighty corporations want that kind of publicity, so it stays more silent then it should. It’s just a theory, but that’s what I believe. Either way, or whatever the reason is, it’s a major issue, and I’m so glad to hear that my posts have been doing at least their small, tiny part to fill that gap, and thanks, as always, for the support. 😊.
3 notes
·
View notes
Text
PCOS, aka hormones are the worst
Hello, my darlings! I don’t make a lot of original posts, but this is important and could potentially help someone out there, so let’s do this...
To my followers-who-have-ovaries:
Do you have a history of anxiety and/or depression?
Did it begin when you hit puberty? and/or
Have therapy and medications never quite worked for you?
Do you have long or irregular menstrual cycles?
Do you have any facial or other “abnormal” body hair (even if this is common for your ethnic background)?
Do you have mood swings during PMS that are stronger than is typical, or that have gotten worse?
Have you gained weight and/or do you have trouble losing weight? Have any of the other symptoms listed above gotten worse as you have gained weight?
If any of this sounds familiar, read on:
Congratulations, you may have PCOS! (Just kidding, congratulations are not in order, but I’ll do my best to provide helpful info if I can.) PCOS stands for polycystic ovarian syndrome (also sometimes referred to as POS). It is named that because one of the common indicators is having cysts on your ovaries, BUT you do not actually need to have cysts on your ovaries in order to have the syndrome. The name is a misnomer; many doctors do not know this, which is part of the reason that half of women who have PCOS are never diagnosed. Most doctors will only diagnose PCOS if a woman has two of the following “big three” symptoms:
Very irregular menstrual cycle
High testosterone (androgen) levels (body hair is a big indicator of this, but not the only one)
Cysts on ovaries
However, as stated above, cysts are not necessary in order to actually have the syndrome, there are far more symptoms than just those three, and the long list of symptoms is different for each woman. Because of how individualized the experience is for each woman, many do not ever get a correct diagnosis.
Left undiagnosed and untreated, PCOS can lead to a lot of serious health problems, such as:
Infertility (PCOS is the largest cause of infertility in women)
Diabetes
Heart Disease
Mental illness (and a higher risk of suicide)
Endometrial cancer
If any of these symptoms sound familiar to you, it’s worth looking into. Here’s how you can start on your own, before you even see a doctor (or if you can’t see a doctor for a while):
1. Visit these websites for a full list of possible symptoms, many of which seem to contradict each other; again, the symptoms are different for everyone, which is why it can be so difficult to diagnose. (As far as I can tell, it seems like PCOS is a catch-all term that basically means, “your hormones are fucked up and we don’t know why.”) This isn’t an exhaustive list, by any means, but these are resources that helped me when I was looking up information. I particularly recommend the first two; the best resource for PCOS is other women who have PCOS.
PCOS Awareness Association
PCOS Foundation
womenshealth.gov (I’m honestly surprised this website still exists...)
WebMD
Prevention Magazine: “7 Things You Need to Know about Polycystic Ovary Syndrome”
The Atlantic Magazine: When Missed Periods Are a Metabolic Problem
2. Start tracking your menstrual cycle (if you aren’t already). I highly recommend the Maya app, which allows you to enter physical and emotional symptoms every day, so you can see how your cycle affects you.
3. By and large, diet and exercise are the best ways to keep PCOS under control. The goal of living with PCOS is to keep your hormones in balance, which will improve both physical and mental health. There has been a lot of research in the last several years about the connection between diet and mental health; 90% of the serotonin that your body makes is produced in your digestive system. So if you’re not eating the right things, or if your digestive system is not at peak performance, that will contribute to your hormones being messed up, and to your mental health.
More information on the “gut brain connection”
I’ve recently come across the PCOS Nutrition Center, and I can’t yet vouch for it, but it looks like it could be a good resource as well.
When you see a doctor:
1. Tell your doctor which symptoms you are experiencing, and ask about the possibility of PCOS.
Ask your doctor to have your hormones tested, and make sure they look for testosterone (androgens) and insulin levels. It just takes a blood test, which any insurance (even mine!) will cover.
Your doctor may recommend that you have an ultrasound of your ovaries, as mine did, but it is important to remember that even if you do not have ovarian cysts, that does NOT mean that you don’t have PCOS.
2. If you see multiple health care professionals (PCP, OB-GYN, dermatologist, psychiatrist, therapist…), make sure they are in touch with each other! Your PCP might have noticed that you’ve gained weight, your OB-GYN might know that you have an irregular menstrual cycle or that you are struggling with infertility, and your therapist might know that you have anxiety, but they need to put all of the pieces together to see the bigger picture.
3. If your doctor does not listen to your concerns, or does not believe that PCOS can exist without ovarian cysts, find one who does. (Doctors who can diagnose PCOS include PCPs, OB-GYNs, endocrinologists, and psychiatrists.) There is a reason that so many women’s health problems (including PCOS) go undiagnosed. Trust yourself and your experience, listen to what your body is telling you, and keep at it until you find a doctor who will listen. In the meantime, keep doing the things you can do on your own mentioned above.
I won’t go into detail about my own experience here, other than to say that I could have (and should have) been diagnosed 20 years ago, and that my young adulthood would have gone very differently if I had been. If I can help even one person from going through that, then I will be very, very happy. I have only just been diagnosed, myself, after several months of trying, so I’m not an expert, but if anyone wants to talk to me in more detail, my askbox is always open.
#PCOS#polycystic ovarian syndrome#polycystic ovary syndrome#health#women's health#mental health#menstruation#hmm i don't think i have an OP tag#fleur has an OP tag#there we go
157 notes
·
View notes
Text
300+ TOP DIABETES Objective Questions and Answers
DIABETES Multiple Choice Questions :-
1. A patient arrives at the ED with a blood sugar of 578, serum osmolarity of 300, pH of 7.3, severe thirst, dehydration, and confusion. The patient is breathing rapidly and has a fruity breath smell. This patient has symptoms of......
A. Diabetic ketoacidosis
B. hyperosmolar hyperglycemic noketotic coma
C. Hypoglycemia
D. diabetic neuropathy
Ans: A
2. What are the micro vascular complications of uncontrolled diabetes?
A. Delayed gastric emptying (Missed.
B. Diarrhea
C. Glomuerular injury (Missed.
D. Bleeding of retinal caplillaries (Missed.
E. Numbness of feet
F. Impotence (Missed.
Ans: B,E
3. The newly diagnosed diabetic patient asks the nurse why he needs to check his feet every day. The nurse's best response is....
A. To prevent leg amputation.
B. To check for any cuts, sores, or dry cracked skin so they can be treated early to prevent infection or gangrene.
C. To see if they hurt.
D. You just need to do it.
Ans: B
4. What are Macro vascular complications of uncontrolled diabetes?
A. Pain in lower legs
B. Hyperlipidemia (Missed.
C. Impotence
D. Ischemic heart disease (Missed.
E. Aortic disection
Ans: B,D
5. The nurse enters a patient's room and sees the patient breathing rapidly with a fruity breath smell. This is known as...
A. Trousseau's
B. Cullen's
C. Kussmaul's
D. Bitot's
Ans: C
6. A patient with severe hypoglycemia arrives at the ED unconscious by ambulance. The nurse would first...
A. Give regular insulin by IV
B. Give NPH by IV
C. Give 10-15 g CHO or Orange juice
D. Give 1 mg glucagon
Ans: D
7. The diabetic patient's lab work comes back with a pH of 7.4, serum blood sugar of 950, serum osmolarity of 460, pCO2 of 35, HCO3 of 25. The patient is confused and dehydrated. This patient is showing signs and symptoms of....
A. Diabetic ketoacidosis
B. hyperosmolar hyperglycemic noketotic coma
C. Hypoglycemia
D. diabetic neuropathy
Ans: B
8. The nurse enters a diabetic patient's room at 11:30 and notices that the patient is diaphoretic, tachycardic, anxious, states she is hungry, and doesn't remember where she is. This patient is most likely showing signs of what?
A. hyperglycemic
B. hypoglycemic
C. diabetic ketoacidosis
D. hyperosmolar hyperglycemic noketotic coma
Ans: B
9. The nurse's first action upon finding a patient with mild hypoglycemia is to...
A. Call the rapid response team
B. Give 1 mg of glucagon
C. Give 10-15 g of CHO or Orange juice
D. Give insulin
Ans: C
10. What is the number one complication of diabetes?
A. Diabetic ketoacidosis
B. Obesity
C. Hypertension
D. Cardiovascular disease
Ans: D
DIABETES MCQs
11. A urine test in an undiagnosed diabetic may show........
A. glucose and ketones in the urine
B. glucose and high amounts of bilirubin in the urine
C. ketones in the urine
D. ketones and adrenaline in the urine
Ans: A
12. If a person has a fasting plasma glucose of 6.8mmol/L and a two-hour postprandial plasma glucose of 11.6mmol/L, should this person be suspected of having diabetes?
A. Yes
B. No
C. Cannot decide
Ans: A
13. A woman has a fasting plasma glucose of 5.9mmol/L and a two-hour postprandial plasma glucose of 7.6mmol/L. Are these values normal?
A. No.
B. Yes, according to the American Diabetes Association guidelines
C. Yes, according to the World Health Organisation guidelines
Ans: C
14. If a person has a random plasma glucose of 8mmol/L, is it normal?
A. Yes
B. No
C. Not possible to tell
Ans: C
15. There are a range of glucose values called "impaired glucose tolerance". What is the significance to a person who has impaired glucose tolerance?
A. The person has an increased risk of developing diabetes
B. The person has an increased cardiovascular risk
C. Both the above
D. None of the above
Ans: C
16. Can the onset of new diabetes be prevented or delayed?
A. Yes
B. No
Ans: A
17. Are there any laboratory tests to distinguish between Type 1 and Type 2 diabetes?
A. Yes
B. No
Ans: A
18. Which statement below is CORRECT regarding initiation of long term insulin therapy in diabetes?
A. Patients with Type 1 diabetes should be initiated on basal insulin alone
B. Patients with Type 1 diabetes should be initiated on prandial insulin alone
C. Patients with Type 2 diabetes should be initiated on basal insulin alone
D. Patients with Type 2 diabetes should be initiated on prandial insulin alone
Ans: C
19. Which statement below is TRUE with regard to these two insulin preparations:
1. Insulatard Insulin (NPH insulin.
2. Mixtard insulin (a pre-mixed combination of short acting and long acting insulin.
A. Insulatard insulin and Mixtard insulin can be given at bedtime without the need for a bedtime snack
B. Mixtard insulin can be given at bedtime without the need for a bedtime snack
C. Insulatard insulin can be given at bedtime without the need for a bedtime snack
Ans: C
20. Which of the statements below is true when initiating insulin in a Type 2 diabetic who is already on Metformin and Glibenclamide?
B. Metformin must be stopped or the dose reduced
C. Glibenclamide must be stopped or the dose reduced
Ans: C
21. A patient with diabetes on Metformin and Glibenclamide is scheduled for a coronary angiogram. His diabetic control is good. Which of the statements below is TRUE?
B. Metformin must be stopped before the procedure
C. Glibenclamide must be stopped before the procedure
D. No changes need to be made. He can undergo the procedure.
Ans: B
22. Which statement below regarding the use of intravenous insulin for treating diabetic ketoacidosis is TRUE?
A. Insulin should be given IV until the blood sugar is normal
B. Insulin should be given IV until the acidotic state is controlled
C. Insulin should be given IV until the patient is well hydrated
Ans: B
23. What is the best method of controlling blood sugar in a diabetic who cannot take orally?
A. Fixed dose insulin according to body weight given subcutaneously
B. Insulin given subcutaneously according to a sliding scale
C. Insulin given intravenously along with dextrose and potassium
Ans: C
24. Is this statement true or false?
The glycosylated hemoglobin value is a useful parameter when making decisions regarding the need for insulin in a Type 2 diabetic.
A. True
B. False
Ans: A
25. Which type of diabetes is more common in children?
A. Diabetes I
B. Diabetes II
Ans: B
26. Mickey's insulin gives her the lowest CBG 5 hrs after injection. Which insulin is Mickey taking?
A. Novolog
B. NPH
C. NovologR
D. Lantus
Ans: D
27. The nurse has to give the pt HumologR. The nurse understands the medication when the nurse states the peak time is:
A. 1-3 hr
B. 2-4 hr
C. 4-12 hr
D. 5 hrs
Ans: B
28. Ben comes into the ED with blurred vision. He has polyuria and complains of pain in his legs. Labs show that he has elevated insulin levels and high triglyceride levels. Ben also complains of always being thirsty. What type of Diabetes does Ben have?
A. Diabetes I
B. Diabetes II
Ans: B
29. The nurse understands NovologR and when it ends by stating it ends:
A. 3-5 hrs
B. 3-6.5 hrs
C. 5-7 hrs
D. 18-24 hrs
E. 24 hrs
Ans: C
30. Can an infection cause a rise in GLU?
A. Yes
B. No
Ans: A
31. Tony has to check his BG 5 days a week before breakfast and periodically at other times. He notices a rise of BG when he is sick. What type of diabetic is Tony?
A. Diabetes I
B. Diabetes II (Missed.
C. Insulin Dependent
D. Non Insulin Dependent (Missed.
Ans: A,C
32. Ted is taking NPH insulin. The nurse knows Ted understands his medication when he states:
A. It can start working in 10-30 minutes
B. It can start working 1-2 hours after injection. (Missed.
C. Peak action is 4-12 hours (Missed.
D. It stays in the system 18-24 hrs. (Missed.
Ans: A
33. Which type of insulin cannot be manually mixed in a syringe?
A. Novolog
B. Humolog
C. NPH
D. Regular
E. Lantus
Ans: E
34. The nurse understands Novolog when the nurse states the end time is:
A. 3-5 hrs
B. 3-6.5 hrs
C. 5-7 hrs
D. 18-24 hrs
Ans: B
35. Nick was given Novolog insulin. The nurse knows that his breakfast should be available to Nick how many minutes after taking his meds?
A. immediately to 2.5 hrs
B. 2-4 hrs
C. 4-12 hrs
D. 5 hrs
Ans: A
36. Mary has a skin infection that wont go away. Her BP is 135/90. She has dark amber urine. She also reports that she has reoccurring vaginal infections. Her GLU comes back at 135. What type of diabetes does she have?
A. LADA
B. Diabetes I
C. Diabetes II
D. Pre Diabetes
Ans: D
37. NIDDM acounts for 90% of diabetics. What are some thing that a NIDDM diabetic could do to help their disease?
A. Avoid exercise
B. reduce body fat by 5% (Missed.
C. maintain excellent skin health (Missed.
D. Rub lotion in their feet, but no in between their toes. (Missed.
Ans: A
38. Lucy has just given birth. She had gestational diabetes and did not have to take insulin. She is very concerned that will now have to take insulin for the rest of her life. What does a nurse say to educate Lucy about her condition?
A. Proper instruction of foot care.
B. 25-50% of women will eventually develop type 2 diabetes. (Missed.
C. Losing the baby fat will help. (Missed.
D. Education on what type of insulin she will need.
Ans: A,D
39. Bill is in the ED presenting with a BP of 60/45 and is responsive to painful stimuli. His Na is 180 and BUN is 65. His wife states he is a type 2 diabetic but has been sticking to his diet. His insulin lab came back low. What is wrong with Bill?
A. Hyperosmolar Hyperglycemic Nonketoitic Syndrome
B. Diabetic Ketacidosis
C. LADA
D. Hyperglycemic
Ans: A
40. Ana is a long distance runner with diabetes. She understands her need for testing when she states:
A. i should test before and after exercise (Missed.
B. I should test after exercise
C. I should test before and after each meal and bedtime
D. If I feel like my BG is low, I should test (Missed.
Ans: B,C
41. Cynthia is getting NovologR. The nurse knows that Cynthia needs more education when she states:
A. I need to check my BG throughout the day.
B. I need to be consistent with insulin usage.
C. I need to eat a large meal before taking my insulin
D. My insulin can be in my system for 5-7 hours.
Ans: C
42. Manifestations of hypoglycemia would entail:
A. Anxiety (Missed.
B. Hyperactions
C. Tachycardia (Missed.
D. Confusion (Missed.
Ans: B
43. Insulin is measure in:
A. Ml
B. Dl
C. units
D. Tsp
Ans: C
44. Which is most dangerous?
A. hypoglycemia
B. Hyperglycemia
Ans: A
45. Nathan's AIC comes back at 9%. The nurse understands this value by stating to the pt:
A. Your diabetes is under control.
B. Your diabetes has shifted to Diabetes I.
C. Your diabetes needs further intervention.
D. Call the coroner and make an appointment if you don't plan on taking this more seriously!
Ans: C
46. After giving insulin, what is the most critical observation that needs to be made?
A. Tachycardia
B. Bradycardia
C. Hyperglycemia
D. Hypoglycemia
Ans: D
47. The nurse understand NPH when the nurse says NPH ends:
A. after a heavy meal
B. 18-24 hrs after injection
C. 12 hrs after injection
D. When HumologR has been injected.
Ans: B
48. What risk factors increase diabetic foot problems?
A. Sensory neuropathy (Missed.
B. PVD (Missed.
C. Smoking (Missed.
D. Alcohol
Ans: D
49. Humolog begins to take affect:
A. 15 min
B. 10-30 min
C. 30-60 min
D. 1-2 hrs
E. 1.1 hrs (Your Answer.
Ans: A
50. Linda is taking Lantus. She understands her medication when she states:
A. it can start in 1.1 hr. (Missed.
B. peaks 4-12 hours
C. it ends in 24 hrs (Missed.
D. it cannot be mixed with other insulins in the same syringe. (Missed.
Ans: B
DIABETES Objective type Questions with Answers
51. Lupe is in the ED. She has anorexia, abdominal pain, acetone breath, polyuria and is confused. She has ketones present in her urine. She is pre diabetic with a glu of 650. What is Lupe's problem?
A. She was misdiagnosed and should be a type 1 diabetic.
B. Hyperosmolar Hyperglycemic Nonketoitic Syndrome
C. Diabetic Ketacidosis
D. LADA
Ans: C
52. Gladus is in for her physical. She is a 54 year old woman with a lot of energy. She is mildly overweight. Her BP is 130/85. As part of her physical, the doctor discovers her GLU is 350. He orders a fasting plasma glucose and her levels come back 130 the first day and 275 the second day. What does this indicate?
A. Diabetes I
B. Diabetes II
C. LADA
Ans: B
53. Nicole is a chronic alcoholic. She drinks a bottle of wine every night and hard liquor on the weekends. She has been fatigued and has blurry vision. The doctor tells her she now has diabetes II. She doesn't understand how she could have diabetes as it does not run in her family. What education would the nurse give to the patient?
A. Explain that the alcohol caused her diabetes.
B. Insulin will not be affected by her drinking
C. Encourage her to attend AA meeting even though she doesn't want to.
D. Using therapeutic communication, help her to see that this is her fault and must accept she has ruined her life.
Ans: A
54. Neuropathy occurs only in type 2 diabetics?
A. Yes
B. No
Ans: B
55. Pat is a 45 year old female presenting with 83/60 BP, and elivated BUN and a GLU of 879. She reports that she is not on a diet but has been losing weight rapidly and has fatigue. What type of diabetes does she have?
A. Diabetes I
B. Diabetes II
C. LADA
Ans: C
56. NPH insulin has been prescribed to the pt. The nurse understands NPH when the nurse states:
A. NPH acts quickly.
B. NPH peaks at 4-12 hrs (Missed.
C. NPH is a mixture of rapid and slow acting (Missed.
D. NPH low CBG will most likely be around 5 hrs.
Ans: A,D
57. Hypoglycemia is related to :
A. reduced insulin and increased glucose
B. increased insulin and reduced glucose (Missed.
C. may occur when very high blood glucose falls too rapidly (Missed.
D. failure to eat (Missed.
Ans: A
58. The nurse understands NPH and how quickly it starts when the nurse states:
A. 10-30 min
B. 30-60 min
C. 1-2 hrs
D. 1.1 hours
Ans: C
59. HumologR has been given to Melisa at 13:30. When would Melisa need her snack or lunch?
A. 14:30
B. 16:30
C. 15:30
D. 14:00
Ans: C
60. Keith has just been diagnosed with diabetes. His diabetes is an autoimmune disorder. He has lost 15 lbs in two weeks and has polyuria. His BP was 75/45 on admission. What type of diabetes does Keith have?
A. Diabetes I
B. Diabetes II
Ans: A
61. What substance is found in the blood and urine of an undiagnosed diabetic?
A. insulin
B. adrenaline
C. ketones
D. bilirubin
Ans: C
62. A normal FASTING blood glucose in a non-diabetic is
A. 80 to 110
B. 40 to 80
C. 120 to 150
D. 150 to 200
Ans: A
63. Hyperglycemia is when......
A. the blood sugar is too low
B. the blood sugar is normal
C. there is sugar in the urine
D. the blood sugar is too high
Ans: D
64. If diabetes goes untreated for a long time, what disease can develop? HINT:patients must be hospitalized for successful treatment of this condition
A. hypoglycemia
B. diabeticketoacidosis
C. ketosis
D. hyperglycemia
E. ketourina
Ans: B
65. What are the three most COMMON symptoms of diabetes?
A. headaches vomiting constant illness
B. intolerable thirst constant urination weight loss
C. double vision infections constant urination
D. tingling of the feet slow healing wounds weight loss
E. intolerable thirst vomiting heart burn
Ans: B
66. What is one cause of diabetes? MORE THAN ONE RIGHT ANSWER
A. virus (Missed.
B. antibody mistake (Missed.
C. too much sweets
D. genetics (Missed.
E. bacteria
Ans: C,E
67. Name both types of diabetes SCIENTIFICLY
A. Type 1 and Type 2
B. Old Diabetes and Young Diabetes
C. Juvenile Diabetes and Adult-Onset Diabetes
D. Brittle Diabetes and Insulin Dependant Diabetes
Ans: C
68. Can diabetes kill you?
A. Yes
B. No
C. Only if you're a certain race
Ans: A
69. An insulin pump's site must be changed......
A. once a week
B. never
C. every three days
D. every day
E. every five days
Ans: C
70. Aspart insulin is also referred to as......
A. long acting insulin
B. short acting insulin
C. intermediate acting insulin
Ans: B
71. Why does a Long-Acting-Insulin shot hurt more than a Short-Acting-Insulin shot
A. Because it is a bigger shot
B. Because Long-Acting-Insulin has preservatives in it to keep it working the full 20 to 24 hours
C. Because you use a different needle to deliver Long-Acting-Insulin
Ans: B
72. If a person does not like the insulin needle or pump, they want might to try the......
A. syringe
B. moniter
C. pen
D. inhaler
Ans: C
73. About how many Americans have diabetes
A. 5 million
B. 47 million
C. 21 million
D. 16 million
E. 33 million
Ans: C
74. What food can make you have a high blood sugar?
A. nuts
B. water
C. yogurt
D. pizza
E. bread
Ans: D
75. A urine test in an undiagnosed diabetic may show........
A. glucose and ketones in the urine
B. glucose and high amounts of bilirubin in the urine
C. ketones in the urine
D. ketones and adrenaline in the urine
Ans: A
76. A slice of bread has about how many carbohydrates?
A. 5 carbs
B. 30 carbs
C. 15 carbs
D. no carbs
E. 25 carbs
Ans: C
77. Which is not true about Diabetes?
A. the blood sugar may go out of control
B. the person may be hospitalized if they are not treating the diabetes
C. Diabetes can be completely cured
D. diabetes can be associated with nausea
Ans: C
78. When you are sick, the blood sugar may.......
A. be normal
B. very low
C. higher than usual
D. lower than usual
Ans: C
79. In a newly-diagnosed patient who is in the hospital, their first major goal is to.....
A. have their blood sugars go back to normal
B. clear their ketones
C. get an insulin pump
Ans: B
80. Ketones are produced by.........
A. not having insulin
B. a high blood sugar
C. fat breakdown
D. passing urine with sugar in it
Ans: C
81. What are the 3 main factors to success with diabetes?
A. food exercise insulin
B. food insulin ketones
C. exercise ketones insulin
Ans: A
82. People with diabetes can lead normal lives?
A. Yes
B. No
C. Only some
Ans: A
83. Diabetes is a world wide disease
A. True
B. False
Ans: A
84. Which of the following is a symptom of diabetes?
A. Pregnancy
B. Mood Swings
C. Blurred Vision
D. Loss of Hearing
Ans: C
85. What is the medicine that is injected into your body by a needle?
A. Insulin
B. Sugar
C. Glucose
D. Diabetic Solution
Ans: A
86. What is a test you can get at the doctor to see if you have diabetes?
A. Blood Test
B. X-ray
C. MRI
D. Diabetes test
Ans: A
87. How many different types of diabetes are there?
A. 1
B. 2
C. 3
D. 5
Ans: B
88. 1. Secretory product associated with pancreatic alpha cells:
A. A. insulin
B. B. proglucagon
C. C. somatostatin
D. D. pancreatic polypeptide
E. E. insulin and somatostatin
Ans: B
89. 1. Major manisfestations of diabetes mellitus:
A. A. inappropriate hyperglycemia
B. B. disordered metabolism
C. C. both
D. D. neither
Ans: C
90. 1. Type I diabetes:
A. A. most often presents in adults
B. B. anabolic metabolic disorder
C. C. circulating insulin is virtually absent
D. D. glucagon levels are low
E. E. ketoacidosis is rarely seen
Ans: C
91. 1. Extrinsic factors which may affect pancreatic B cell function:
A. A. mumps virus
B. B. toxic chemicals
C. C. coxsackievirus
D. D. mumps virus and toxic chemicals
E. E. mumps virus, toxic chemicals and coxsakievirus
Ans: E
92. What is prediabetes?
A. When blood glucose levels are higher than normal but not high enough for diagnosis. (Correct Answer.
B. When your diabetes is in submission until you turn forty
Ans: A
93. Type 1 diabetes was previously known as what?
A. Endrino diabetes
B. Juvenile diabetes
Ans: B
94. What is the most common type of diabetes?
A. Type 1 diabetes
B. Type 2 diabetes
C. Pre-diabetes
Ans: B
95. There is always symptoms when you have diabetes.
A. True
B. False
Ans: B
96. Type I diabetes is characterized by:
A. resistance to insulin
B. autoantibodies
C. complicated by HHS
Ans: B
DIABETES Interview Questions and Answers pdf Download
Read the full article
0 notes
Text
All you should know about Sleep Apnea

“Sleep is the best meditation.” - Dalai Lama
There are millions of things that might bring
pleasure or relaxation to humans but one has to inevitably admit that ‘A Good
Nights Sleep’ is one of the most satisfying things one can experience. It’s not
just important but a NEED for the efficient functioning of one’s body. While
many of us think that we have spent our 7-8 hrs on the bed and slept well,
there might be an unknown disorder that you are facing and unaware of.
What is
sleep apnea?
Sleep apnea - one of the most common sleep
disorders afflicting approximately 20 million adults with an estimated 80% o f cases going undiagnosed.. The Greek word “apnea” means
“without breath.” Sleep apnea is an involuntary suspension of breathing that
occurs while the patient is asleep. Most of us may be unaware that sleep apnea
might be the root cause of several sprouting health disorders. If untreated for
a long period this might lead to serious consequences.
It is a condition that causes occasional
cessation of breath during sleep causing one to snore loudly or create choking
noises while trying to breathe. The body slowly becomes deprived of oxygen and
makes the patient wake up abruptly. It is a common yet serious disorder that
might even cause one to stop breathing once or even a hundred times during a course
of sleep. The airway repeatedly becomes blocked, limiting the quantity of air
that reaches your lungs.
Sleep apnea has 3 forms: Central sleep apnea
(CSA) in which the pauses are due to the brain failing to signal the
respiratory system to breathe; obstructive sleep apnea (OSA) in which breathing
is paused by a physical blockage in the upper airways, often caused by soft
tissues of the throat and tongue collapsing into the airway; and complex/mixed
sleep apnea which is a conjunction of CSA and OSA.
Signs and symptoms of sleep apnea:
Snoring:
Loud, chronic snoring is the most common symptom of apnea. it's caused by
partial blockage or obstructions as air is being restricted from moving easily
through the airways.
Frequent
breaks or pauses in breathing:
In sleep apnea, the fatty
tissues of the throat or tongue become relaxed throughout sleep and fall across
your airways that restricts the flow of oxygen and prevents respiration for
several seconds.
Fatigue
during the day: There is a general assumption that you are in bed for 7-9
hrs and so you had a good quality of sleep, this is a myth! All of those pauses
and interruptions to your sleep add up to a lot of lost time in the quality and
quantity of nightly sleep. One of the most common and frequently overlooked
symptoms of sleep apnea is excessive daytime sleepiness (EDS). EDS is a
condition where a person experiences an overwhelming daytime fatigue.
Headache:
If you wake up with or have frequent headaches during the daytime it might
signal that you had an improper quality of sleep. When you stop breathing
frequently during the night, less or no oxygen is making its way to your brain.
Reduced oxygen levels cause the widening of blood vessels that initiate
vascular headaches.
Obesity:
In most cases, a person's body weight is directly linked to having OSA. Obese
people are more likely to have sleep apnea than those that maintain healthy
weights. This might be due to too much of fatty build up around the
circumference of the throat. Theses excess tissues can fall back into the
airways during sleep causing obstructions in the airways leading to apnea
events.
Mood
swings, depression or irritability: Lack of quality sleep can affect a
person's mood. Lack of quality sleep nearly every night can make you more
irritable, prone to anxiety, short-tempered, and eventually trigger depression.
Consequences of untreated sleep apnea
Low levels of oxygen in your body can have
negative long-term consequences for your health. This includes:
High blood
pressureHeart
diseaseStrokePre-diabetes
and diabetesDepression
There are many undiagnosed and untreated cases
of sleep apnea.Neurologists, pulmonologists and otolaryngologist can
diagnose obstructive sleep apnea using an in-lab sleep study or a home sleep
apnea test. Sleep apnea can be controlled using continuous positive airway
pressure (CPAP) therapy, the front-line treatment for sleep apnea, oral appliance
therapy or surgery.
At Nightingales, we perform levels of sleep study with the help of state-of-the-art sleep diagnostic devices to diagnose conditions like obstructive sleep apnea, periodic limb movement disorders, narcolepsy, restless leg syndrome, insomnia, sleepwalking and other sleep behavior disorders.Diagnosing sleep disorders can improve one’s quality of life and prevent complications or progression of certain diseases. So, book a sleep study today!
(Source: www.alaskasleep.com)
Read the full article
0 notes
Photo

3 Most Common Symptoms Of PCOS And How To Reverse It 〰️ Facial Hair - PCOS is a result of androgen (male hormones) excess, insulin resistance and hyperinsulinemia. The research shows that high circulating insulin stimulates certain ovarian enzymes, resulting in elevations in testosterone (both free and serum). Insulin influences the androgenic state by affecting metabolism of ovarian androgens but also by regulating circulating levels of sex hormone binding globulin (SHBG). Insulin has been shown to lower SHBG (which binds to estrogen and testosterone making them unavailable). Thus, lowered SHBG increases the bioavailability of testosterone to the tissues = PCOS symptoms. (The Textbook of Functional Medicine) 〰️ Ovulatory dysfunction - This can manifest as oligomenorrhea (irregular periods) or amenorrhea (missing periods). Many women with PCOS can experience abnormally heavy, short or long menstrual cycles. 〰️ Polycystic ovaries - Sometimes, the ovaries will form what’s called a “functional ovarian cyst.” A sac forms on the surface of an ovary around a maturing egg. Usually, the sac goes away once the egg is released. If the egg isn’t released or the sac closes around the egg and fills with fluid, it becomes a functional cyst. The term “polycystic” literally means that a woman’s ovaries have multiple small cysts on them. 〰️ If left undiagnosed PCOS can lead to infertility, diabetes, mood disorders, endometrial cancer, fatty liver, sleep apnea, high blood sugar, high cholesterol, high BP and heart disease. 〰️ Fortunately, with some simple (but not always easy) lifestyle and nutrition modifications PCOS can be treated very successfully. 〰️ Check the comments for some simple action items to get the journey started. . . #pcos #polycysticovariansyndrome #highinsulin #hyperinsulinism #hyperinsulinemia #highcarbdiet #livinginstress #womensfacialhair #ovulationproblems #highbloodsugar #eastwesthealing #realfoodgangstas https://www.instagram.com/p/Bv4NrlhgcPH/?utm_source=ig_tumblr_share&igshid=1nduat7g1767t
#pcos#polycysticovariansyndrome#highinsulin#hyperinsulinism#hyperinsulinemia#highcarbdiet#livinginstress#womensfacialhair#ovulationproblems#highbloodsugar#eastwesthealing#realfoodgangstas
0 notes
Text
Diseases Caused By Candida Albicans

Candida albicans, is a part of the natural microbes in the body. In the digestive tract in the mouth and vagina can be found. This microorganism most of the time it's not a problem, but it is possible that excessively increased and causing infections. Candida albicans in humans, fungal

infections are the most common cause. The tour, which is the name of the “ albicans” is Latin for “white” means. When the Maya culture in the laboratory appears in white color. In some infections such as thrush creates white spots.
Let's take a closer look at the types of Candida albicans infection and how they were treated.
Types Of Candida Albicans Infections
The four most common causes of the Candida infections in the following, we will examine symptoms and treatment. The rest of the article we will focus on less common infections that can cause Candida albicans.
1-Urinary yeast infection: Candida species urinary tract or urinary tract infections (UTIs) are the most common cause of the fungus. Candida can be placed in the lower part of the urinary tract, or in some cases it can travel up to the kidneys.
The following may increase the risk of developing a candida infection in the urinary tract:
*Have received antibiotic therapy
*Urinary catheter to be attached to a medical device such as
*Diabetes
*A weak immune system
Urinary yeast infection symptoms: many people in the community urinary fungal infection (urinary tract infection) although he has cannot be cured. In some people, the following symptoms may occur:
*The need to urinate increase
Pain or burning sensation when you urinate
*Pain in the pelvic region or abdomen
*Blood in the urine
Treatment of urinary yeast infections: treatment only to alleviate symptoms is recommended. Different kinds of antifungal medication are used. In the patient if the catheter is inserted should be removed.
2-Genital yeast infection: Candida albicans is the most common cause of genital yeast infections.
Normally called Lactobacillus, a type of bacteria the amount of candida in the genital area keeps it under control. However, excessive levels of Lactobacillus and an increase may indicate when it is changed in a manner of candida can cause an infection.
Certain sexual activities, especially oral-genital contact genital those that contain a candida infection may develop. Healthy individuals can get genital Candida infections, but are at higher risk than the following groups:
*People who have recently received antibiotics
*Diabetes people who are not under the control of
*Immunocompromised individuals
*Pregnant women
*Those who see taking oral contraceptives or hormone therapy
Genital yeast infection symptoms: the symptoms of genital yeast infections or Candida may include:
*Burning sensation during urination or sex
*The sensation of pain or itching around the vagina
*Redness, irritation or swelling around the vagina
*Abnormal vaginal discharge which can be watery or thick and white
*Rash around the vagina
*Rash on the penis
If a woman is having a vaginal candida infection, often the sexual organs of his wife may be infected with candida. Infection may be asymptomatic, but cause an itchy or burning rashes around the head of the penis may occur.
Genital candida infection treatment: mild or moderate genital Candida infections which over-the-counter or prescription antifungal creams, pills or suppositories can be treated with. In addition, the patient fluconazole single-dose oral antifungal medication may be given. For more complicated infections, creams, pills or ointments you may be given a prescription for a drug containing longer listed.

Oral (inside the mouth) Thrush
3-Oral (inside the mouth) Thrush: Candida albicans is a normal part of our microflora proliferation, although an excessive amount of mouth infections can cause. Infection may not be limited to the mouth. Tonsils and into the back of the throat, severe infections can spread to the esophagus. People who are at high risk for the development of oral thrush include:
*Those who use antibiotic or corticosteroid drugs
*Those who have undiagnosed or uncontrolled diabetes
*Immunocompromised ones
*False teeth (especially the top) ones
Symptoms of oral thrush: Oral lint in some of the common symptoms include:
*White spots in the mouth bleeding in your view or cottage coagulated milk, and tapping
*Pain or burning sensation in the mouth
*Redness inside the mouth or at the corners
*Eating or difficulty in swallowing
*Loss of taste
*Cotton in your mouth-like image
Oral thrush the infection, if untreated, can lead to systemic Candida infection especially in people with a weak immune system.
Treatment of oral thrush: oral thrush pill, liquid or lozenge-shaped, and is treated with antifungal medication. Used drugs include clotrimazole or tolnaftate. For more severe cases oral fluconazole may be given dry.

Mucocutaneous Candidiasis
4-Mucocutaneous Candidiasis: Candida species are the skin, mucous membranes, and can infect nails. Skin yeast infections Candida albicans but other Candida strains can cause the most common cause of TR. Warm, moist or sweaty areas, provides a good environment for the development of the fungus. An example for such regions as the armpits, groin, between the toes of the hands and feet, and chest are the areas under the corners of the mouth. Other risk factors that predispose to Candida skin infection include:
*Donning tight or synthetic underwear
*The lack of hygienic or rarely changing underwear
*Replacing of diapers sparse
*The use of antibiotic or corticosteroid drugs
*Diabetes
*Weakened immune system
Symptoms of mucocutaneous Candidiasis: Candida skin infection the most common symptom of a red rash that occur in the affected area. Water that collects in some cases, raised lesions may occur. Also thicken the skin or curd (curd) - like substance that can produce a white appearance.
Mucocutaneous Candidiasis Treatment: antifungal creams are usually given to clear skin infection. Antifungal drugs clotrimazole, miconazole and econazole may contain substances such as. Any itching or a steroid cream to help relieve some of the swelling may be given. The skin should be kept dry during healing. In cases where the infection is widespread, oral fluconazole pills may be prescribed.
What Are The Symptoms Of Candida Infections?
To diagnose candidiasis, your doctor will first take your medical history and will ask questions about your symptoms. Also any condition or medication that could lead to weakening of the immune system, whether you are, or have recently received antibiotic therapy may ask whether. Many common cases of candidiasis usually can be diagnosed by physical examination.
If your doctor is not sure whether your symptoms related to candida infection from the affected area of a sample can be taken. This sample is used to identify the organism and then culture in which the type. For example, a blood sample for testing if there is suspicion my kandide can be taken.
Because it is useful to determine the types of Candida that causes the infection your doctor will prescribe an antifungal medication that will be effective in the treatment of certain types.
Other Candida Infections
Candida albicans enters the bloodstream, only in your blood, other

organs can cause serious infections. These infections in the blood, heart, eyes, skin, brain and spinal cord in the peritoneal membrane, bones and joints may develop.
Neutropenia Is A Major Risk Factor
Neutropenia is an important risk factor for the spread of Candida. Neutropenia, called neutrophils, blood cells that is at a lower level than normal. This can make you more prone to infection. Neutropenia from cancer chemotherapy or radiation therapy frequently among those who need the affected persons, and include patients with leukemia or bone marrow. A candida infection there are different treatment recommendations for individuals who have neutropenia and invasive.
My kandide
Kandide, a blood infection that occurs with Candida species. For a long time may cause a death rate in the hospital.
Kandide risk factors include the following:
*Suppressed immune
*The use of broad spectrum antibiotics
*Major surgery
*Inserting a medical device such as a catheter or feeding tube
My Symptoms Kandide
Symptoms may resemble bacterial sepsis and may include the following:
*Fire
*Renal failure
*Shock
Diagnosis and treatment
Yeast can be diagnosed once a blood sample has been isolated from kandide me. Treatment depends on the type of Candida that causes the infection. The catheters should be removed.
Endocarditis
Endocarditis of the heart chambers and covers the valves of the heart that is an infection of the inner lining. Fungal endocarditis is a very serious condition with a high mortality rate. 24 to 46 per cent of all cases of fungal endocarditis Candida albicans is responsible for the sixth. Endocarditis risk factors include the following:
*Weakened immune
*Cardiac anomalies or defects
*Long-term antibiotic use
*Cardiovascular surgery
*Feeding tubes, catheters or prosthetic heart valve
The causes of urinary incontinence and treatment methods
Symptoms Of Endocarditis
The symptoms of fungal endocarditis include:
*Fire
*Cough *
*Shortness of breath
*Body aches (pain in the lower extremities are sometimes).
Diagnosis and treatment of endocarditis

The diagnosis of endocarditis can be difficult because symptoms are usually caused by bacteria shows a comparison of endocarditis. Treatment intravenously (through a vein) fluconazole or amphotericin B should be given, and medical devices have removed the fungus from infected tissue involves the surgical removal if you have.
Endoftalmit
Endophthalmitis is an eye infection that can be caused from fungus. May lead to loss of vision. Although the species Candida tropicalis Candida albicans is the most common type of disease causing the infection TR.
Risk Factors For Endophthalmitis Are As Follows:
*Recently being hospitalized.
*Recently surgery
*A weak immune system
*Have a catheter in
Symptoms Of Endophthalmitis
The infection can affect one or both eyes. The main symptom is inflammation in the eye, but in some cases pus in the tissue of the eye can be found.
Endophthalmitis diagnosis and treatment
Endophthalmitis can be diagnosed by analysing a sample of fluid is taken through a retinal examination. Flusitozin treatment fluconazole or amphotericin B can be used.
Meningitis
Meningitis is an inflammation of the tissue surrounding the brain and spinal cord. Meningitis may occur when the fungus reaches the spinal cord through the blood. Fungal meningitis that is caused by Candida usually transmitted from a hospital. Contacts for factors that could jeopardize this type of meningitis may include the following:
*Immunosuppression
*Antibiotics, immunosuppressant, or certain medications such as corticosteroids
*A surgical procedure recently passed
Symptoms Of Fungal Meningitis
Fungal (yeast-induced) symptoms of meningitis include the following:
*Headaches
*Neck stiffness
*Fire
*Nausea and vomiting
*Sensitivity to light
*Confusion
Diagnosis and treatment of fungal meningitis
In doubt from a fungus that causes meningitis if the cerebrospinal fluid (CSF) sample is taken and the culture is made. Recommended treatment for meningitis caused by Candida species amphotericin B flusitozin.
Intra-Abdominal Candidiasis
Intra-abdominal candidiasis, Candida peritonitis may be cited as. That is the cause of a yeast infection is an inflammation of the inner lining of the abdomen. This will cause Candida albicans, but other Candida species also

may cause. Intra-abdominal factors that increase your risk of developing candidiasis include the following:
*Abdominal surgery which have been made recently
*Peritoneal dialysis spend
*Antibiotic therapy
*Conditions such as diabetes
Symptoms Of Candidiasis For Your Wife
Intra-abdominal candidiasis symptoms are too similar to be distinguished from bacterial peritonitis. Symptoms include the following:
*Abdominal pain or bloating
*Fire
*Nausea and vomiting
*Feel tired or exhausted
*Diarrhea
*Decreased appetite
To diagnose the condition, your doctor for an abdominal fluid (peritoneal fluid) sample. The cause of the infection Candida is present in the sample will be observed.
Intra-Abdominal Candidiasis What Is The Treatment For?
Intra-abdominal candidiasis treatment is done with antifungal drugs such as the following:
*Fluconazole
*Amphotericin B
*Kaspofungin
*Mikafungin
In addition, if you have a catheter in the patient should be removed.
Fungal Arthritis and osteomyelitis
Fungal infection osteomyelitis is a bone, while arthritis (septic arthritis, also known as a fungal infection of a joint. Although this is rare, Candida species can cause both. Bacterial infections are more common. The following factors may increase the risk of the disease:
*Weakened immune system
*A recently formed orthopedic surgery or bone injury
*Catheters inserted
*Diseases such as diabetes
Fungal osteomyelitis and arthritis symptoms
The symptoms of these ailments, which may be accompanied by fever or chills pain or swelling in the affected area. Fungal people with arthritis the affected joint may have great difficulty using. Osteomyelitis is a bone biopsy to determine whether the cause of a yeast infection may be needed. Analysis of the joint fluid can determine whether or not a fungal infection are the cause of arthritis. In both these cases, was caused by a blood infection if candida in the blood is determined.
Fungal osteomyelitis and Arthritis Treatments
Fungal arthritis and osteomyelitis in the treatment of amphotericin B and antifungal drugs such as fluconazole are used.
Candida albicans, and you
Candida of the digestive tract, and vagina species of the natural skin

microflora and does not cause disease is a part of. Long-term antibiotic use or a weakened immune system, such as having a candida infection may increase the risk of developing some cases. Candida infections such as vaginal infections and skin infections are localized and can be treated with antifungal medications is the most common. Systemic infection untreated candida infection may increase the risk of other organs that may be involved.
If you notice symptoms of a candida infection, a doctor should be consulted to get a correct diagnosis and treatment.
https://www.orak11.com/index.php/azoospermia-disease-what-are-the-causes/
Bibliography:
https://www.medicalnewstoday.com
https://www.msdmanuals.com
https://www.healthline.com
Read the full article
#candidaalbicans#candidaalbicanscauses#candidaalbicansinfection#candidaalbicansnaa#candidaalbicanssymptoms#candidaalbicanstreatment#endocarditisbacteria#endocarditisbacterial#endocarditissymptoms#endocarditistreatment#meningitiscauses
0 notes
Text
3 Reasons Why You’re Still Tired After 7-9 Hours of Sleep
3 Reasons Why You’re Still Tired After 7-9 Hours of Sleep was initially published on https://www.ellymackay.com/
This week we’re going to be diving into a question I get nearly daily, and one you may be asking yourself: why am I still tired after a full night of sleep?
Chances are you’ve heard the standard advice: get seven to eight hours of sleep per night for optimal health. It’s bad enough that for some of us that’s hard to achieve. First of all, most of us don’t know where to start–something as simple as a sleep calculator and taking my chronotype quiz can be helpful.
But something that’s frustrating? Making every effort to get those seven to eight hours of sleep and still waking up exhausted and relying on caffeine to combat daytime sleepiness.
I’ll explain why the seven to eight hours of sleep guidelines doesn’t work for everyone; the reasons behind why you’re always tired, and some natural sleep remedies to boost your energy.
Where Do Sleep Guidelines Come From?
The first thing we need to tackle is the 7-9 hours of sleep. Chances are someone’s recommended this to you, whether it’s your primary care physician, a friend, or just advice you’ve come across after battling daytime fatigue.
The guidelines were established by the National Sleep Council, which routinely revisits sleep recommendation guidelines for everyone from babies to teenagers and adults. The latest guidelines came out in 2015.
But it’s more complex than that: while these are guidelines, sleep experts such as myself have continued to see, time and time again, that those recommendations don’t fit everyone.
Why 7-9 Hours of Sleep Doesn’t Work For Everyone
Sometimes I wish one set of guidelines, one sleep aid, or a single tip could help all clients fight insomnia, wake up refreshed, and enjoy optimal health. That isn’t the case: for some, a drug free cooling band like my favorite from EBB is helpful for calming racing thoughts at night. Others might benefit from this Remzy weighted blanket for comfort and relaxation
68 percent of us have sleep issues at least once a week, according to a 2016 Consumer Reports survey of 4,000 Americans. So it makes sense that, while seven to nine hours of sleep may work for the average adult, it doesn’t work for everyone.
A narrative review of sleep guidelines published in The Nature of Science and Sleep found that observational and self reporting biases made it difficult to truly know how long people were sleeping. The 2018 recommendation was that more in depth, controlled and longitudinal studies will be needed to better understand how much sleep is associated with the most health benefits.
Finally, individuals are…individuals. We all have different sleep patterns, based on an internal biological clock, or what I call a chronotype. Our chronotypes affect the time of day we perform our best work, get our best workout in, and sleep. Because of this, a standard seven to nine hours doesn’t ensure waking up feeling rested.
Why More Sleep Isn’t Always the Answer
Of course, while you may find that you can get by with one less hour of sleep, or need one more, most adults will need within an hour of those professional sleep guidelines. So when a client asks why they’re still tired after 12 hours of sleep, I start becoming concerned, sleeping too much can have its own serious side effects.
The truth is, while up to 35 percent of Americans are considered chronically sleep deprived (less than seven hours of sleep per night),that isn’t the only problem. Many of us are getting seven to nine hours of sleep, and even more, but especially for those suffering from a true sleep disorder, your risk for depression and other life issues is still high.
3 Common Reasons Why You’re Always Tired (And What To Do)
If seven to nine hours of sleep isn’t working (and then some) here are the most common reasons why you’re still feeling tired:
Problem: You’re Not Sleeping as Much as You Think.
This is a common problem, not unlike going on a diet: unless you’re tracking your sleep, it can be easy to lose track of just how many hours you’re getting.
You can have the best intentions and end up staying up late looking at emails instead of going to bed when you planned (if you do look at electronics at night, I recommend using blue light blocking glasses so you won’t disrupt your body’s production of melatonin).
Another reason you may not be getting as much quality sleep as you think is ambient light. Consider using an eye mask so that all light is blocked, especially if you have a bed partner who uses a light in bed or if your work requires sleeping during daylight hours. This is the eye mask I use and recommend for my patients. I also love the Dep Slep sleep hoodie with a built in eye mask.
Solution: Track Your Sleep
You don’t have to be a sleep expert like me to track your sleep. While sleep centers can monitor your sleep, you can also opt for the lower cost solution of a sleep tracker (my go to is the SleepScore Max ).
For many people I recommend a sleep tracking device because you’ll get information not only how many hours you sleep, but how much of that is deep sleep. Research has shown that lack of deep sleep is tied to everything from obesity and diabetes to disorders, heart problems, and impedes sleep’s benefits for brain health.
Problem: You Have Sleep Apnea
This sleep issue is directly related to not being aware of how much sleep you’re getting, and why a sleep tracker can be helpful. If you or your partner snores, there’s a high probability that you may be suffering from sleep apnea.
I’ve written extensively on sleep apnea and its negative impact on your health, and that’s because it’s so prevalent: more than 18 million Americans suffer from sleep apnea, a disorder characterized by obstructed breathing at night.
If you do have undiagnosed sleep apnea, one of the most common symptoms is daytime sleepiness, no matter how many hours you’re logging. That’s because sleep apnea regularly disrupts deep sleep, which is vital for tissue growth and repair.
Solution: Seek Sleep Apnea Treatment
Suspect you might have sleep apnea? Take my Snore Score Quiz to get started. If you snore at all, it’s worth getting checked because undiagnosed sleep apnea can not only cause you to always feel tired, but also lead to serious cardiovascular conditions, like high blood pressure, abnormal heart rhythm, and even heart attacks.
The good news is that sleep apnea is treatable. The most effective treatment is a CPAP machine. For some, oral mouthpieces can be used to open up airways at night. Lifestyle changes such as losing weight and reducing alcohol consumption; and, in rare cases, surgery can also be helpful.
Always consult a medical professional and avoid self diagnosing.
Problem: You’re Fighting Your Chronotype
The third reason why you’re always tired after a full night’s sleep deserves a whole article, but for now I’ll leave it to this: you’re fighting your chronotype.
There are many things we do throughout our days–from when we get up to what we eat and our stress levels–that drain our energy even after a night of restorative sleep. While we all have days where we struggle to stay awake, sleep deprivation causes chronic lack of concentration and harms both our physical and mental health.
From drinking caffeine at the wrong time to eating dinner too early (or too late), little habits that fight our biological clock make it harder to fall asleep, stay asleep, and power through our day.
Solution: Adjust Your Routine For Your Unique Needs
This is in some ways the hardest solution to follow, because it takes time, patience, and trial and error.
Your first step to optimizing your energy is to find out when exactly your body thrives when it comes to eating, sleeping, and even exercising and socializing. To do that, take my Chronotype Quiz.
From there, you can learn ways to reorient your day. By doing so, you’re making the very most out of those seven to nine hours of sleep and you’ll start feeling more energized as your body adjusts.
As a send off, I’ll leave you with this: feeling tired all the time is something we seem to have accepted as a society, but it shouldn’t be. You deserve to live your best life possible. And you don’t need to succumb to the dangers of relying on energy drinks to get through your day.
Until next week, sweet dreams.
The post 3 Reasons Why You’re Still Tired After 7-9 Hours of Sleep appeared first on Your Guide to Better Sleep.
from Your Guide to Better Sleep https://thesleepdoctor.com/2020/07/25/3-reasons-why-youre-still-tired-after-7-9-hours-of-sleep/
from Elly Mackay - Feed https://www.ellymackay.com/2020/07/25/3-reasons-why-youre-still-tired-after-7-9-hours-of-sleep/
0 notes
Text
The Thyroid-Diabetes Connection
If you have type 2 diabetes, you should receive a screening for thyroid abnormalities, according to researchers at the American Association of Clinical Endocrinologists (AACE) 20th Annual Meeting and Clinical Congress. The recommendation came after a new study involving over 5,000 people found the prevalence of hypothyroidism to be nearly 6 percent among people with type 2 diabetes, compared to just under 2 percent in those without.
Hypothyroidism is a well-recognized risk of type 1 diabetes, but this has generally not been extended to type 2 diabetes as well — until now.
What Does Your Thyroid Function Have to do With Diabetes?
Both thyroid disorders and diabetes involve a dysfunction of the endocrine system. Type 1 diabetes and the most common cause of hypothyroidism — Hashimoto’s disease — are both autoimmune diseases, and having one autoimmune disease increases your risk of developing another.
With type 2 diabetes, coexisting hypothyroidism may increase your risk of heart problems, and the researchers noted that early identification of both conditions could improve heart function, blood pressure and lipid profile. [1]
Thyroid hormones also influence glucose homeostasis, including impacting circulating insulin levels, intestinal absorption and uptake of glucose into fat and muscle tissues. [2]
Even Subclinical Thyroid Disorder May be Associated With Diabetes
People with hypothyroidism often struggle with insulin resistance. This is true even at the sub-clinical level. How do you know if your thyroid is functioning at a sub-clinical level?
Oftentimes, you don’t.
This condition is typically diagnosed when levels of your thyroid hormones are normal but your thyroid-stimulating hormone (TSH) is increased. This is generally a sign that your pituitary gland is working extra hard to keep your thyroid hormone levels up in the normal range. In time, and if left untreated, your TSH levels may continue to increase until your thyroid gland stops responding, and your sub-clinical hypothyroidism turns into full-blown hypothyroidism.
It’s a tricky situation because sub-clinical hypothyroidism may cause no symptoms at all, or it may lead to fatigue, memory problems, weight gain, dry skin, constipation and a range of other various problems that may seem completely unconnected. Again, this often undiagnosed and misdiagnosed condition is also associated with insulin resistance, which typically occurs prior to type 2 diabetes.
As researchers wrote in Clinical Diabetes: [3]
“Thyroid dysfunction is common in diabetic patients and can produce significant metabolic disturbances. Therefore, regular screening for thyroid abnormalities in all diabetic patients will allow early treatment of sub-clinical thyroid dysfunction.”
Like sub-clinical hypothyroidism, you can be insulin resistant for years before developing full-blown disease, and often a diagnosis of type 2 diabetes is a person’s first sign that they are in fact insulin resistant.
Because cases of sub-clinical thyroid disease are often overlooked but may increase health risks for a number of people with co-existing diabetes or insulin resistance (as well as those without), researchers in the British Journal of Diabetes and Vascular Disease recommended “individualization of therapy” as the best solution.
What’s the Bottom Line?
If you currently have type 2 diabetes, you should be aware of the connection to thyroid disorders like hypothyroidism and sub-clinical hypothyroidism. At the sub-clinical level, many have no symptoms at all, and others are unaware that their fatigue, memory problems and other seemingly unrelated symptoms are due to a thyroid issue.
You may need to ask your physician to have this checked, as it is not yet part of the standard of care typically provided for people with type 2 diabetes. But, even if you’ve had your thyroid levels tested and the lab results came back normal, it’s still possible to have a low-functioning thyroid. In fact, the condition is often completely missed due to inadequate testing and a general lack of understanding of the complexities of thyroid function in the conventional medical community.
There is some debate over whether or not sub-clinical hypothyroidism needs to be treated at all, and to this I would stress absolutely. At the very least, sub-clinical hypothyroidism can contribute to insulin resistance as well as increase your risk of cardiovascular events if you have type 2 diabetes.
Further, many in this early stage of thyroid imbalance will go on to develop full-blown hypothyroidism if action is not taken… and will miss out on the vitality and energy they deserve in life.
At least 15 million Americans are thought to suffer from sub-clinical hypothyroidism that may or may not be related to diabetes. Fortunately, dietary approaches and other lifestyle changes can help bring your thyroid function back into the normal ranges, as well as help you to prevent, control and even reverse type 2 diabetes. The guidance of a holistic health care practitioner familiar with both thyroid disorders and diabetes is highly recommended to help you formulate an effective lifestyle plan and stick with it.
References
1. DocGuide.com April 18, 2011
2. British Journal of Diabetes and Vascular Disease. 2010;10(4):172-177.
3. Clinical Diabetes VOL. 18 NO. 1 Winter 2000
Source by Dr Brandon Credeur, D.C.
from Home Solutions Forev https://homesolutionsforev.com/the-thyroid-diabetes-connection/
via Home Solutions on WordPress
from Home Solutions FOREV https://homesolutionsforev.tumblr.com/post/187816928355
via Tim Clymer on Wordpress
0 notes