#Targeted Therapy
Text

Targeted Therapy:
Precision or targeted therapies encompass medications engineered to disrupt specific molecules implicated in the progression of cancer. In contrast to conventional chemotherapy's broad impact on fast-dividing cells, precision therapies selectively target cancer cells while preserving healthy tissue integrity. These drugs aim at various molecular pathways involved in cancer development, including signaling cascades, angiogenesis, and DNA repair mechanisms.
An illustrative example of precision therapy is the application of tyrosine kinase inhibitors (TKIs) in treating specific cancer types like non-small cell lung cancer (NSCLC) and chronic myeloid leukemia (CML). TKIs hinder the activity of particular tyrosine kinases, crucial enzymes in cancer-promoting cell signaling pathways. By obstructing these kinases, TKIs effectively inhibit tumor growth and extend patient survival.
Likewise, monoclonal antibodies represent another form of precision therapy, binding to specific proteins on cancer cell surfaces, initiating immune-mediated tumor destruction. These antibodies can also be combined with cytotoxic agents or radioactive isotopes to heighten their anti-cancer properties.
Personalized Chemotherapy:
While precision therapies are central to personalized medicine, tailored chemotherapy remains vital in cancer treatment. Tailored chemotherapy involves customizing traditional cytotoxic drugs to suit the unique characteristics of each patient's tumor. This may involve adjusting drug doses, combining different agents, or selecting chemotherapy regimens based on tumor biology and patient-specific factors.
One approach to tailored chemotherapy utilizes predictive biomarkers to identify patients likely to respond positively to specific chemotherapy drugs. For example, certain mutations in the BRCA genes are associated with increased sensitivity to platinum-based chemotherapy in breast and ovarian cancers. By identifying these biomarkers, oncologists can identify patients who will benefit most from a particular chemotherapy regimen while minimizing potential toxicity for others.
Furthermore, progress in pharmacogenomics, which explores how genetic variations affect drug response, has provided insights into individual differences in drug metabolism and toxicity. By analyzing patients' genetic profiles, oncologists can predict their likelihood of experiencing adverse effects or poor response to chemotherapy drugs, enabling personalized dose adjustments and treatment optimization.
Early cancer detection and management is important for an improved success rate in cancer treatment. You can undergo regular health checkups to get diagnosed for cancer at an early-stage. There are many good hospitals in Mumbai that offer health checkup packages for cancer screening, such as a full body health checkup at Saifee Hospital Mumbai, which is one of the best hospitals in the country.
#chemotherapy#personalized chemotherapy#targeted therapy#full body health checkup#regular health checkups#cancer screening#cancer detection
4 notes
·
View notes
Text
youtube
#Lung cancer#Aiolos#OTUB1#ubiquitination#oncogenesis#cancer research#cell proliferation#protein stabilization#tumor progression#cancer therapy#molecular mechanisms#deubiquitinase#proteasomal degradation#cancer biomarkers#targeted therapy#signal transduction#metastasis#transcription factor#oncogenic pathways#tumor biology.#Youtube
0 notes
Text
Liposome Drug Delivery: Enhancing the Efficacy of Treatment Through Nanotechnology
What are Liposomes?
Liposomes are spherical vesicles made of phospholipid bilayers. They can encapsulate both hydrophilic and hydrophobic drugs within their aqueous core and lipid membranes respectively. Due to their lipid bilayer structure, liposomes closely resemble the structure of cell membranes which allows them to safely fuse with cells and deliver drugs.
Mechanism of Action
When administered, liposomes travel through the body in circulation. Upon reaching the target site, they fuse with cell membranes and release their drug cargo inside the cells. This increases the concentration of drugs at disease sites while reducing toxicity to non-target organs. Additionally, drugs encapsulated in liposomes have longer half-lives in the body, which allows for dose intensification.
Targeted Delivery
Liposome Drug Delivery can be tailored for targeted delivery by attaching ligands like antibodies, sugars, or peptides to their surface. These ligands act as address labels, targeting liposomes to specific cell types like cancer cells. This achieves active targeting and improves therapeutic efficacy. Pegylation, the process of attaching polyethylene glycol chains, increases circulation time and shields liposomes from immune detection for extended site-specific delivery.
Cancer Treatment Applications
Cancer is one of the biggest applications of liposomal drug delivery. Doxorubicin, an anthracycline chemotherapy drug, shows cardiotoxicity with free use. However, encapsulation in liposomes shields heart tissue and improves delivery to tumors through leaky vasculature. This leads to significant decreases in toxicity and enhances antitumor efficacy. Liposomal formulations like Doxil and Lipodox are mainstays of breast and ovarian cancer treatment. Cisplatin and other platinum drugs show potential for liposomal delivery against various cancers. Researchers are also investigating liposomal delivery of newer targeted cancer therapies.
Infectious Disease Treatment
Bacterial infections impose another therapeutic challenge due to the emergence of antibiotic resistance. Liposomes loaded with antibiotics can selectively accumulate at sites of infection to achieve high local drug levels while exposing the rest of the body to minimal levels. This prevents the evolution of resistance and increases treatment efficacy. For diseases like tuberculosis that require multidrug treatment courses, liposomal formulations improve patient adherence and management. Liposomal formulations of antifungal drugs like Amphotericin B have transformed the treatment of systemic fungal infections.
Anti-Inflammatory Applications
Conditions with inflammatory pathologies like rheumatoid arthritis pose difficulties due to deleterious systemic effects of high drug levels. Liposome Drug Delivery of steroids and NSAIDs produces sustained high local drug levels at joints while preventing toxicity. This enhances anti-inflammatory efficacy and outcomes. Liposomes are a promising non-viral carrier for targeted delivery of genes and silencing RNA molecules to treat disease processes governed by inflammation.
Get more insights on Liposome Drug Delivery
Alice Mutum is a seasoned senior content editor at Coherent Market Insights, leveraging extensive expertise gained from her previous role as a content writer. With seven years in content development, Alice masterfully employs SEO best practices and cutting-edge digital marketing strategies to craft high-ranking, impactful content. As an editor, she meticulously ensures flawless grammar and punctuation, precise data accuracy, and perfect alignment with audience needs in every research report. Alice's dedication to excellence and her strategic approach to content make her an invaluable asset in the world of market insights.
(LinkedIn: www.linkedin.com/in/alice-mutum-3b247b137 )

#Liposome Drug Delivery#Nanotechnology#Drug Delivery Systems#Targeted Therapy#Nanomedicine#Liposomal Formulations#Controlled Release
0 notes
Text
Class IV Laser Treatments: A Cutting-Edge Solution for Pain Relief in Orange, CA
When it comes to managing chronic pain, residents of Orange, CA are turning to a groundbreaking therapy: Class IV laser treatments. This advanced technology offers a multitude of benefits for individuals seeking relief from pain and discomfort. In this article, we'll dive into the science behind Class IV laser treatments and explore the specific advantages of this innovative approach to pain management.
Understanding Class IV Laser Treatments
Class IV laser therapy is a non-invasive, drug-free treatment modality that utilizes the power of focused light to alleviate pain and promote healing. This form of therapy involves the application of a high-powered laser to the affected area, where the energy from the laser penetrates the tissue, triggering a cascade of biological responses at the cellular level. This process, known as photobiomodulation, leads to reduced inflammation, accelerated tissue repair, and a decrease in pain sensation.
Benefits of Class IV Laser Treatments
Pain Relief: One of the primary advantages of Class IV laser treatments is their ability to effectively alleviate pain. By targeting the source of discomfort and stimulating the release of endorphins, these treatments offer significant relief for individuals suffering from a range of conditions, including arthritis, sciatica, neuropathy, and musculoskeletal injuries.
Accelerated Healing: Class IV laser therapy has been shown to expedite the body's natural healing processes. By increasing cellular metabolism and promoting the development of new, healthy tissue, these treatments can aid in the recovery from injuries, surgeries, and chronic conditions.
Non-Invasive and Safe: Unlike surgical procedures or pharmacological interventions, Class IV laser treatments are non-invasive and carry minimal risk of adverse effects. This makes them a safe and attractive option for individuals seeking pain relief without the potential complications associated with more invasive modalities.
Customizable and Targeted: Another benefit of Class IV laser therapy is its ability to precisely target specific areas of the body. Practitioners can tailor the treatment to address the unique needs of each patient, ensuring that the therapy is personalized and effective for the individual's condition.
Improved Mobility and Functionality: For those dealing with pain and limited mobility, Class IV laser treatments can offer a renewed sense of freedom and functionality. By reducing inflammation and promoting tissue repair, these treatments can enhance range of motion and physical capabilities.
Choosing Class IV Laser Therapy in Orange, CA
For residents of Orange, CA dealing with chronic pain, Class IV laser treatments represent a promising avenue for relief. Fortunately, the region boasts a wealth of specialized clinics and wellness centers that offer these cutting-edge therapies. By seeking out a reputable provider in the area, individuals can access the benefits of Class IV laser treatments under the guidance of experienced professionals, helping them take a proactive approach to their pain management and overall well-being.
In conclusion, Class IV laser therapy stands as a compelling solution for individuals seeking effective, non-invasive pain relief in Orange, CA. With its ability to reduce pain, accelerate healing, and improve functionality, this innovative treatment modality offers a powerful tool for managing a wide range of chronic conditions. By embracing the potential of Class IV laser treatments, individuals in Orange, CA can embark on a journey towards a more comfortable and active lifestyle, free from the constraints of persistent pain.
#Class IV Laser Treatments#Pain Relief#Orange CA#Photobiomodulation#Non-Invasive#Accelerated Healing#Targeted Therapy#Chronic Pain Management#Wellness Centers#Personalized Treatment
0 notes
Text
Targeted therapies for brain tumors are treatments that aim to specifically target certain molecules or pathways involved in the growth and spread of the tumor.
These therapies are designed to be more precise and selective than traditional chemotherapy, potentially resulting in fewer side effects and improved outcomes.
Here are some targeted therapies commonly used for brain tumors:
Tyrosine Kinase Inhibitors (TKIs): These drugs target specific tyrosine kinases, enzymes involved in signaling pathways that regulate cell growth and division. Examples include drugs like imatinib (Gleevec), which targets the BCR-ABL fusion protein in chronic myeloid leukemia, and erlotinib (Tarceva), which targets the epidermal growth factor receptor (EGFR).
Angiogenesis Inhibitors: Angiogenesis is the process by which new blood vessels are formed, and it plays a critical role in tumor growth and spread by supplying nutrients and oxygen to the tumor. Angiogenesis inhibitors like bevacizumab (Avastin) can block the formation of new blood vessels, thereby starving the tumor of its blood supply.
Monoclonal Antibodies: Monoclonal antibodies are laboratory-made molecules that can target specific proteins on the surface of cancer cells. For example, rituximab (Rituxan) targets CD20, a protein found on B-cell lymphomas, and trastuzumab (Herceptin) targets HER2, a protein overexpressed in certain breast cancers.
Immunotherapy: Immunotherapy works by harnessing the body's immune system to recognize and attack cancer cells. Checkpoint inhibitors like pembrolizumab (Keytruda) and nivolumab (Opdivo) can block inhibitory signals on immune cells, allowing them to more effectively target and destroy tumor cells.
Targeted Radiation Therapy: Techniques such as stereotactic radiosurgery and proton therapy allow for precise delivery of radiation to the tumor, minimizing damage to surrounding healthy tissue.
Gene Therapy: Gene therapy involves introducing genetic material into cells to replace or supplement faulty genes. This approach holds promise for treating brain tumors by targeting specific genetic mutations driving tumor growth.
Signal Transduction Inhibitors: These drugs interfere with signaling pathways involved in cell proliferation and survival. For example, inhibitors of the PI3K/AKT/mTOR pathway, such as everolimus (Afinitor), can suppress tumor growth in certain types of brain tumors.
The cost of targeted therapy for brain tumors in India can vary depending on several factors, including the specific type of therapy, the duration of treatment, the dosage required, the brand of medication, the healthcare facility where treatment is received, and any additional supportive care or monitoring needed during the course of treatment.
Generally, targeted therapies tend to be more expensive than conventional chemotherapy or radiation therapy due to their specialized nature and often involve ongoing treatment over an extended period. The cost of targeted therapy may also include fees for medical consultations, diagnostic tests, imaging studies, and hospitalization if required.
In India, the cost of targeted therapy can range from several thousand to several lakh rupees per month, depending on the factors mentioned above. Some targeted therapies may be available at lower costs through government healthcare facilities or subsidized programs, while others may be more expensive and only accessible at private hospitals or specialty clinics.
Get the best treatments for brain tumor at the best hospitals in Mumbai like H N Reliance Hospital Mumbai.
#targeted therapy#health#surgery#brain health#brain tumors#diseases#parkinson's disease#deep brain stimulation#epilepsy#depression
0 notes
Text
Personalized Approaches to Cutaneous Squamous Cell Carcinoma Treatment: Targeting Tumor Diversity
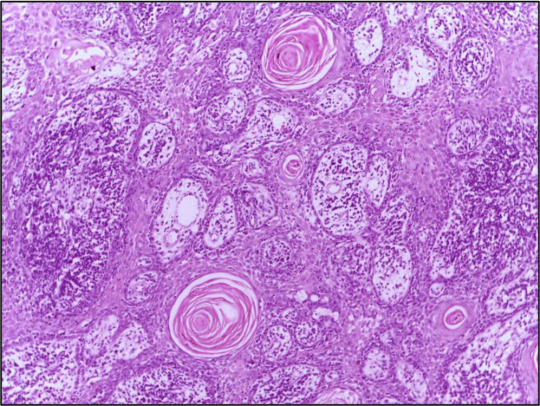
Cutaneous Squamous Cell Carcinoma (cSCC) is a heterogeneous disease characterized by diverse clinical and molecular features. Personalized treatment approaches that take into account the unique characteristics of individual tumors have emerged as a promising strategy to improve treatment outcomes and patient survival.
Understanding Cutaneous Squamous Cell Carcinoma: Cutaneous Squamous Cell Carcinoma (cSCC) is a type of skin cancer that arises from the malignant transformation of squamous cells in the epidermis or its appendages. It encompasses a spectrum of disease presentations, ranging from localized lesions to metastatic tumors with varying clinical behaviors.
Tumor Heterogeneity and Molecular Subtypes: Cutaneous Squamous Cell Carcinoma (cSCC) exhibits considerable heterogeneity at the molecular level, with distinct genetic alterations and signaling pathways driving tumor progression and metastasis. Molecular subtyping studies have identified different subgroups of cSCC tumors based on their genomic profiles, providing insights into tumor diversity and potential therapeutic targets.
Precision Medicine in cSCC Treatment: Precision medicine approaches aim to tailor treatment strategies to the specific molecular characteristics of individual tumors, allowing for more targeted and effective therapies. By identifying actionable mutations or biomarkers, clinicians can select therapies that are most likely to benefit patients while minimizing the risk of treatment-related toxicities.
Genomic Profiling and Biomarker Identification: Advances in genomic sequencing technologies have enabled comprehensive profiling of cSCC tumors, revealing recurrent mutations in genes involved in cell cycle regulation, DNA repair, and immune evasion. Biomarker identification efforts seek to identify predictive markers of treatment response and prognosis, guiding treatment decisions in personalized medicine.
Get More Insights On This Topic: Cutaneous Squamous Cell Carcinoma
#Cutaneous Squamous Cell Carcinoma#Skin Cancer#Tumor Heterogeneity#Precision Medicine#Molecular Subtypes#Targeted Therapy#Immunotherapy#Biomarker Identification#Personalized Treatment
0 notes
Text

Discover how targeted therapy revolutionizes cancer treatment. Oncare Cancer delves into the breakthroughs, benefits, and applications of targeted therapy, offering insights for patients seeking precision treatment options. Trust Oncare Cancer for expert guidance on understanding and accessing targeted therapy for improved cancer outcomes.
#what is targeted therapy#targeted therapy for cancer#targeted therapy#targeted therapy side effects#Oncare cancer
0 notes
Text
Cancer and living on borrowed time?
Cancer and living on borrowed time?
Grateful for the borrowed time?
********
Cancer used to be
a frightening word!
It still is!
It is like a life sentence…
on borrowed time?
*******
With advances in science;
surgery, chemotherapy,
radiotherapy, targeted therapy,
hormonal therapy,
if money can buy them
you can buy the borrowed time?
********
Live for today
Live like there’s no…

View On WordPress
#advances in science#cancer#chemotherapy#death#Hope#hormonal therapy#radiotherapy#surgery#targeted therapy#time
0 notes
Text
Melanoma and Black Skin: A Rising Concern
Introduction
Melanoma, a type of skin cancer, has traditionally been associated with fair-skinned individuals. However, recent studies indicate a rising severity of melanoma in the black population. This post looks at what melanoma is, why its severity may be increasing among black individuals, preventive measures, and the current treatments available.
What is Melanoma?
Melanoma is the most…

View On WordPress
#black skin#Chemotherapy#delayed diagnosis#early detection#genetic factors#immunotherapy#melanocytes#Melanoma#radiation therapy#skin cancer#sun protection#tanning beds#targeted therapy#UV radiation
0 notes
Text
Understanding Precision Medicine – Asrar Qureshi’s Blog Post #821

View On WordPress
#Adverse Events#Asrar Qureshi#Blogpost821#Diagnostic Tools#Genome Testing#Personalized Medicine#Pharma Industry#Pharma Veterans#Precision Medicine#Targeted Therapy
0 notes
Text
Metastatic Melanoma Therapeutics: New Breakthroughs in Cancer Treatment and Management

Metastatic melanoma, also known as advanced or stage IV melanoma, occurs when melanoma cells spread from the primary skin cancer site to other organs in the body. When melanoma reaches this advanced stage, it becomes much more difficult to treat and can be life-threatening if left untreated. In this article, we will explore the current treatment landscape for metastatic melanoma and recent therapeutic advances that are improving outcomes for patients.
Standard Metastatic Melanoma Therapeutics
For many years, chemotherapy was one of the only systemic treatment options available for metastatic melanoma. Chemotherapies like dacarbazine (DTIC) were sometimes used but provided limited benefits, with overall response rates of only 10-15% and median survival times of 6-9 months. Combination chemotherapy regimens like carboplatin plus paclitaxel were also tested but did little to improve on the poor outcomes seen with single-agent DTIC. Toxicities were also a major issue, as chemotherapy for melanoma is associated with significant side effects. The lack of effective chemotherapy options highlighted the urgent need for new targeted and immunotherapeutic treatments.
Advances in Targeted Therapies
In recent years, major breakthroughs have been made with targeted therapies that inhibit specific molecular alterations driving Metastatic Melanoma Therapeutics growth and progression. BRAF inhibitors like vemurafenib and dabrafenib were some of the first targeted drugs approved for metastatic melanoma. These work by blocking a mutated version of the BRAF protein found in around 50% of advanced melanomas. While initial responses can be dramatic, resistance often develops within 6-7 months on average. Newer combinations of BRAF and MEK inhibitors like vemurafenib plus cobimetinib or dabrafenib plus trametinib have helped extend responses and improve outcomes compared to BRAF inhibitors alone. Combination targeted therapy is now considered the standard of care for BRAF-mutant metastatic melanoma. Efforts to overcome resistance through additional pathways are also underway.
The Immunotherapy Revolution
The biggest breakthrough has been with immunotherapies that unlock the body's own immune defenses. In 2011, the CTLA-4 inhibitor ipilimumab became the first drug shown to improve overall survival in metastatic melanoma compared to chemotherapy. While only benefiting a minority of patients, this marked a seminal moment as it proved the concept of immunotherapy for advanced disease. Since then, PD-1 inhibitors such as pembrolizumab and nivolumab have revolutionized treatment. These works by releasing brakes on T cells allowing the immune system to better recognize and destroy melanoma cells. Response rates of 40-50% are now achievable depending on the drug and biomarkers, with some patients experiencing durable remissions lasting many years. Combination immunotherapies are also demonstrating even higher response rates. Immunotherapies have now become the standard of first-line treatment for most patients with metastatic melanoma, regardless of BRAF mutation status.
Managing Immunotherapy Toxicities
While tremendously effective at eliciting tumor control, immunotherapies can also cause unique immune-related side effects, known as immune-related adverse events (IRAEs). These result from over-activation of the immune system against normal tissues. Common IRAEs include fatigue, rash, diarrhea, colitis, hepatitis, hypophysitis, and pneumonitis. Most side effects are manageable with immunosuppressive corticosteroids but can sometimes be severe or life-threatening. Careful monitoring during and after treatment is important, along with patient education on recognizing symptoms that require prompt evaluation. Steroid-refractory IRAEs may necessitate additional immunosuppressive agents like infliximab or mycophenolate mofetil. Managing toxicities properly is crucial for maintaining patient safety and tolerability of highly effective immunotherapies.
Ongoing Clinical Trials
Researchers continue pushing the boundaries to improve outcomes even further. Numerous clinical trials are exploring combination strategies pairing immunotherapies with targeted therapies, chemotherapy, radiotherapy or other immunotherapies. Biomarkers to predict response are also an active area. Other investigations focus on optimizing dosing and sequences. Adjuvant therapy studies seek to prevent recurrence after surgery. Cell therapies using TILs (tumor-infiltrating lymphocytes) are showing promise and may benefit non-responders. Efforts are also underway to overcome immunotherapy resistance. With rapid ongoing advances, the future looks bright for developing even more effective precision options tailored to individual tumor and patient factors.
metastatic melanoma was once a dismal diagnosis with very limited treatment options and poor survival. Remarkable progress over the last decade has completely transformed the treatment paradigm. Approval of targeted therapies and immunotherapies has produced much higher response rates and longer life expectancies than ever seen before. While challenges remain in fully overcoming resistance and maximizing benefit for every patient, the immunology revolution has established immunotherapy as a mainstay for melanoma. Continued research advances will help usher in an even brighter future, offering new hope to those diagnosed with this deadly disease.
Get more insights on Metastatic Melanoma Therapeutics
Alice Mutum is a seasoned senior content editor at Coherent Market Insights, leveraging extensive expertise gained from her previous role as a content writer. With seven years in content development, Alice masterfully employs SEO best practices and cutting-edge digital marketing strategies to craft high-ranking, impactful content. As an editor, she meticulously ensures flawless grammar and punctuation, precise data accuracy, and perfect alignment with audience needs in every research report. Alice's dedication to excellence and her strategic approach to content make her an invaluable asset in the world of market insights.
(LinkedIn: www.linkedin.com/in/alice-mutum-3b247b137 )
#Metastatic Melanoma Therapeutics#Skin Cancer#Immunotherapy#Targeted Therapy#Chemotherapy#Radiation Therapy#Clinical Trials#Oncology
0 notes
Text
New Target Identified to Prevent Blood Cancer: Groundbreaking Research in Translational Medicine
New Target Identified to Prevent Blood Cancer: Groundbreaking Research in Translational Medicine
Yet again translational medication has gained amazing headway in the battle against blood malignant growth. A new report by a group of regarded specialists has distinguished another objective that might hold the way to forestalling blood malignant growth. The pivotal discoveries of this study can possibly alter the area of oncology and open new roads for the improvement of successful medicines for blood problems.

Grasping Blood Malignant growth
Blood disease, otherwise called hematological danger, is a sort of malignant growth that begins in the phones of the blood and bone marrow. It incorporates different sorts, including leukemia, lymphoma, and various myeloma, which can devastatingly affect the body's capacity to create sound platelets and battle contaminations. Blood malignant growth influences a large number of individuals overall and postures critical difficulties to the two patients and medical services suppliers.
Distinguishing Another Objective: A Unique advantage in Blood Disease Exploration
The new review distributed in a main clinical diary has distinguished a clever objective that can possibly forestall blood disease. The examination group, drove by famous researchers in the field of translational medication, used state of the art methods and directed careful tests to uncover this pivotal revelation.
As per the review, the recently distinguished target is a particular protein that assumes a urgent part in the turn of events and movement of blood disease. This protein, which was already obscure with regards to blood disease research, has been viewed as profoundly communicated in disease cells and is engaged with advancing cancer development and endurance. The discoveries of this study have revealed new insight into the sub-atomic systems hidden blood malignant growth and have opened up intriguing opportunities for the improvement of designated treatments.
Suggestions for Blood Disease Treatment
The distinguishing proof of this new objective has huge ramifications for the therapy of blood malignant growth. The review discoveries propose that by focusing on this protein, it could be feasible to restrain the development and endurance of disease cells, accordingly forestalling the movement of blood malignant growth. This addresses a pivotal methodology that might actually reform the area of oncology and change how blood malignant growth is made due.
The analysts accept that this revelation could prepare for the advancement of novel treatments that explicitly focus on this protein, prompting more powerful and less poisonous therapies for blood malignant growth patients. The expected advantages of such designated treatments are enormous, as they could essentially work on the anticipation and personal satisfaction for patients fighting blood malignant growth.
Future Bearings and Effects on Accuracy Medication
The distinguishing proof of this new objective has extensive ramifications for the field of accuracy medication, which plans to convey customized and designated treatments in view of a singular's novel hereditary cosmetics and illness attributes. The revelation of this original objective might actually act as a diagram for the improvement of accuracy medication approaches in blood malignant growth treatment.
With additional examination and approval, this recently distinguished target could make ready for the advancement of inventive helpful procedures that outfit the force of accuracy medication to forestall blood disease. This might actually change the scene of blood malignant growth treatment and proposition new desire to patients who are battling with this staggering infection.
The Significance of Blood Malignant growth Exploration
Blood malignant growth is a complicated and testing illness that requires consistent examination and development to work on quiet results. Throughout the long term, broad examination endeavors have been devoted to figuring out the basic systems of blood disease and creating powerful medicines. The new disclosure of another objective in blood malignant growth research can possibly alter the field and achieve critical headways in the counteraction and treatment of this staggering illness.
Divulging the New Objective: Protein X
The notable review recognized a formerly obscure protein, we should refer to it as "Protein X", that has been viewed as profoundly communicated in blood disease cells. Protein X is accepted to assume a crucial part in the turn of events and movement of blood disease, going about as a vital controller of cancer development and endurance. Through careful trial and error and high level procedures, the examination group had the option to uncover the essential job of Protein X in blood malignant growth pathogenesis.
Sub-atomic Systems of Protein X in Blood Disease
Further examination uncovered that Protein X interfaces with different flagging pathways and sub-atomic pathways that are basic for the endurance and multiplication of blood malignant growth cells. Protein X is accepted to advance the development and endurance of disease cells by enacting specific flagging fountains and repressing others, prompting uncontrolled cell development and avoidance of modified cell passing.
Besides, the review discoveries recommend that Protein X may likewise assume a part in the improvement of medication obstruction in blood malignant growth cells, further convoluting the administration of this illness. The mind boggling sub-atomic components through which Protein X works in blood malignant growth cells are as yet being effectively explored, with progressing endeavors to disentangle its careful capabilities and connections.
READ FULL ARTICLE
#Blood cancer treatment#Hematologic malignancies#Translational research#Protein X#Blood cancer#Targeted therapy#Leukemia.#Combination therapies#Clinical trials#Personalized therapies
1 note
·
View note
Text
Lung Cancer Unveiled: Everything You Need to Know About Causes, Symptoms, and Treatment Options
Lung cancer
Overview
Lung cancer is a type of disease that begins in the lungs and is one of the leading causes of cancer deaths worldwide. The lungs are two vital organs in your chest that take in oxygen and release carbon dioxide. Cell lysis in the lungs is an important source of spread of malignant growth worldwide.
Risk factor
The most important risk factor for lung cancer is smoking, but non-smokers can also develop the disease. The time and amount of cigarettes smoked can affect the likelihood of a lung cell analysis. Why and for what Smoking is the most common cause of lung cancer, but exposure to secondhand smoke can also increase the risk of this disease.
Some lung cancers have an unknown cause, making early detection and prevention difficult.
Types of lung cancer
There are two main types of lung cancer: small cell lung cancer and non-small cell lung cancer. Small cell lung cancer is mostly associated with smokers, while non-small cell lung cancer includes several different types of lung cancer, including adenocarcinoma, squamous cell carcinoma, and squamous cell carcinoma. Lung cancer can cause various complications such as shortness of breath, coughing up blood and pain. If cancer spreads to the central airways, shortness of breath may occur, while coughing up blood may be caused by bleeding from the disease. Pain may also occur if cancer has spread to other parts of the body, such as the bones. Fortunately, there are several treatments available to treat these complications, so it's important to discuss all symptoms with your doctor. Caring Surgery: Surgery is the main treatment option for early stage lung cancer. During the operation, the cancerous tissue is removed along with the surrounding healthy tissue. Radiation therapy: Radiation therapy uses high-energy radiation to destroy cancer cells. It can be used alone or in combination with other treatments. Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It can be given orally or intravenously and is often used in combination with other treatments. Targeted therapy: Targeted therapy uses drugs that target specific genes or proteins in cancer cells to stop their growth. Immunotherapy: Immunotherapy is a newer form of treatment that increases the immune system's ability to recognize and destroy cancer cells. Palliative care: Palliative care focuses on treating symptoms and improving quality of life in patients with advanced lung cancer.
conclusion
lung cancer is a serious disease that affects the lungs and can have many harmful effects on the body. Although smoking is the most common cause of this disease, non-smokers can also develop it. It is very important to be aware of the symptoms of lung cancer and see a doctor immediately if they appear. In addition, early detection and prevention through regular health checks and smoking cessation can help reduce the risk of developing this disease.
For more information visit www.oncorelief.in
#lung cancer#causes#treatment options#smoking#radiation therapy#chemotherapy#surgery#targeted therapy#immunotherapy#palliative care#early detection#symptoms
0 notes
Link
#what#targeted therapy#targeted therapy drugs#STUDIED IN CLINICAL TRIALS#STUDIED IN CLINICAL#clinical trials#being studied
0 notes
Text
De novo acute B-cell acute Lymphoblastic Leukemia with BCL2/IGH and BCR/ABL1 rearrangements by Pier Paolo Piccaluga in Journal of Clinical Case Reports Medical Images and Health Sciences

ABSTRACT
T(14;18)(q32,q21) and t(9;22)(q34;q11) translocations, leading to BCL2/IGH and BCR/ABL1 rearrangements, respectively, are common genetic aberrations in hematological malignancies. Particularly, t(14;18)(q32;q21) is the genetic hallmark of follicular lymphoma, while t(9;22)(q34;q11) is commonly rearranged in acute lymphoid leukemia (ALL) and chronic myeloid leukemia. Nevertheless, their association has never been described. We report the first case of acute lymphoid leukemia (ALL) in which both BCL2/IGH and BCR/ABL1 rearrangements were present. The patient presented with pre-B ALL, achieved molecular complete remission with intensified chemotherapy, then reinforced with autologous stem cell transplantation, relapsed after a few months, and unfortunately died 17 months after diagnosis. Of note, only BCL2/IGH but not BCR/ABL1 was detected at relapses.
Key words: B-acute lymphoid leukemia, BCR/ABL1, t(14;18)(q32,q21), BCL2, Philadelphia chromosome, apoptosis, Imatinib, targeted therapy
INTRODUCTION
The t(14;18)(q32;q21) translocation is the most common translocation in B-cell malignancies; in particular, it is found in about 90% of follicular lymphomas, being the chromosomal hallmark of this tumor, and in about 20-25% of diffuse large B-cell lymphomas(1–4). Only a few cases of de novo B-acute lymphoid leukemia (B-ALL) carrying t(14;18)(q32;q21) have been described(5–13). Most of these cases presented with additional chromosomal abnormalities, often involving band 8q24 and/or MYC rearrangement and had a very aggressive clinical course(5,6,8,9,12). Central nervous system (CNS) involvement seems to be a frequent event, despite of adequate prophylaxis. The association between t(14;18)(q32;q21 ) and BCR/ABL1 rearrangement has never been described in ALL. We report on a de novo B-ALL carrying both t(14;18)(q32;q21) with BCL2/IGH fusion and BCR/ABL1 rearrangement.
METHODS
Cytogenetics
Short term cultures from bone marrow samples were performed at diagnosis and during the follow-up. Metaphases were analyzed after G-banding with Wright’stain. Karyotype was described according to the International System for Human Cytogenetic Nomenclature (ISCN 1995)(14–16).
FISH
FISH was performed on fixed cells. Directly labeled BCR and ABL probes (Vysis, Inc), producing a split of red signal when ABL is involved in genetic rearrangements. FISH data were collected with a fluorescence microscope (E 1000, Nikon Instruments) equipped with a CCD camera and Genikon software (Nikon Instruments). Two hundred nuclei/cells were analyzed for each experiment.
Molecular evaluation of BCL2/IGH rearrangement
Molecular evaluation was based on nested PCR(17). Mononuclear cells from BM and PB samples were obtained by Ficoll-Hypaque density gradient centrifugation. Genomic DNA was isolated from mononuclear cells using the QIAamp DNA mini kit (Qiagen, Hilden, Germany)(18). DNA integrity was assessed by amplifying a 510 bp fragment of the Beta-globin gene. Samples positive for Beta-globin were then investigated for the BCL2/IGH rearrangement using a nested PCR specific for MBR and mcr breakpoints. The first round of amplification was done using 1 microg of genomic DNA and the following primers: 5’–CAGCCTTGAAACATTGATGG–3’(forward, for MBR), 5’– CGTGCTGGTACCACTCCTG–3’ (forward, for mcr) and 5’–ACCTGAGGAGACGGTGACC–3’ (reverse, for the JH consensus region). An initial denaturation step of 5 min at 95° C was followed by amplification for 30 cycles (denaturation: 40 sec at 95° C; annealing: 40 sec at 55° C (MBR) or 58°C (mcr); extension: 50 sec at 72° C) and final extension for 7 min at 72° C. Reamplification of a 1 microL aliquot from a 1:50 dilution of the first PCR product was then performed using the internal primers: 5’–ATGGTGGTTTGACCTTTAG–3’ (forward, for MBR), 5’–GGACCTTCCTTGGTGTGTTG–3’ (forward, for mcr), 5’–ACCAGGGTCCCTTGGCCCCA–3’ (reverse, for the JH consensus region), and the following
PCR conditions: initial denaturation step of 5 min at 95° C; amplification for 35 cycles (denaturation: 40 sec at 95° C; annealing: 40 sec at 56° C (MBR) or 59°C (mcr); extension: 50 sec at 72° C); final extension for 7 min at 72° C. All PCR experiments were performed in 50 microL final volume containing 1U of Taq Gold DNA Polymerase (PE Applied Biosystems, San Francisco, USA), 10x PCR buffer, 100 mM of each dNTP, 2.5mM MgCl2, and 1 microM of each primer. Samples were tested twice, and both positive and negative controls were included in all experiments. A patient-specific positive control was also included in every follow-up experiment to compare the BCL2/IGH fragment length with the PCR product obtained at the time of diagnosis. Amplified products were visualized on a 2% agarose gel stained with ethidium bromide. The sensitivity of the assay for the detection of BCL2/IGH rearrangement was routinely =10-4.
Molecular evaluation of BCR/ABL1 rearrangement
RNA extraction was performed by phenol/chloroform using bone marrow mononuclear cells obtained by Ficoll-Hypaque density gradient centrifugation. One microg of total RNA was reverse transcribed using random hexamer primers and MMLV reverse transcriptase; briefly, RNA was prewarmed for 10 min at 70°C and subsequently cooled for a further 10 min at 25°C. The RNA solution was then incubated for 42 min at 45°C in a 20 L reaction mixture containing 10 mM Tris
HCl (pH 8.3), 50 mM KCl, 5.5 mM MgCl2, 1 mM of each deoxyribonucleotide, 20 U of RNAsin
(Pharmacia, Upsala, Sweeden), 25 microM random hexamers (Pharmacia, Upssala, Sweeden), 10 mM of DTT (Pharmacia, Upssala, Sweeden), and 100U of MoMLV reverse transcriptase (BRL, Bethesda, MD). After incubation, cDNA solution was diluted 1:5 to 50 microL final volume. The cDNA integrity was assessed by amplifying a 296 bp fragment of the ABL1 gene. Samples positive for ABL1 were then investigated for the BCR/ABL1 rearrangement by qualitative PCR. Five microLs of cDNA were PCR-amplified using the following set of primers: EA500 5’ TGTGATTATAGCCTAAGACCCGGAG 3’, and R112 5’ TTGTCGTGTCCGAGGCCACC 3’. Thirty-five cycles of PCR were performed as follows: denaturation (30 sec at 96°C), annealing (30 sec at 60°C), and extension (30 sec at 72°C). Samples were tested twice, and both positive and negative controls were included in all experiments.
Amplified products were visualized on a 2% agarose gel stained with ethidium bromide (19).REF
Case report
In July 2020, a 40-years-old woman, presenting only with moderate fatigue, was diagnosed with pre-B ALL, L2 subtype. The peripheral blood count showed: Hb 9.3 g/dl; WBC 17x109/L; PLT 56x109/L. The bone marrow aspirate was hypocellular with 80% of lymphoid blasts. The karyotype was: 46,XX, del(6)(8q21q25), t(9;9)(p11;q22), t(14;18)(q32;q21)(10/20). The immuphenotype, assessed by flow cytometry, was: CD19+, CD22+, TdT+, CD20-, CD3-, CD10-.
The molecular analysis carried out by PCR confirmed a BCL2/IGH rearrangement (mcr breakpoint) but also unveiled a BCR/ABL1 (E1-A2 /p190) rearrangement. Thus, FISH analysis was also performed. The probe for BCR/ABL1 dual fusion gene gave two green signals and two red signals as expected from samples not carrying the ABL1 rearrangement. Molecular analysis was then repeated confirming the previous results. We administered a standard induction therapy (doxorubicine, vincristine, L-asparaginase, and prednisone plus imatinib), and an intensified consolidation therapy (idarubicine and high dose cytarabine) obtaining a molecular complete remission (CR). Particularly, neither BCL/IGH nor BCR/ABL1 rearrangements were detected. Other 2 consolidation courses were then administered (BFM-B regimen, including vincristine, ifosfamide, methothrexate, teniposide, high dose cytarabine, and dexamethasone; and BFM-A regimen, including vincristine, doxorubicine, cyclophosphamide, high dose methothrexate, and dexamethasone) associated with imatinib. Bone marrow harvest and autologous bone marrow transplantation were then performed, lacking a HLA-matched donor. Twelve months after the first documentation of CR, the patient relapsed. The bone marrow aspirate was hypercellular with 90% of leukemic cells. The karyotype was: 46 XX, t(1;5)(p32;q31), del(12)(p11;p13)(14/15); the molecular analysis conducted by PCR showed the BCL2/IGH rearrangement, whereas there was no evidence of the BCR/ABL1 fusion transcript. Salvage therapy with liposomal daunorubicin and intermediate dose cytarabine (23) was then administered, obtaining a second molecular CR (disappearance of BCL2/IGH). Two months later, a second relapse occurred. The karyotype was: 46 XX, t(1,5)(p32;q31), del(12)(p11;p13)(29/30). The molecular analysis showed again only the BCL2/IGH rearrangement, without evidence of the BCR/ABL1 fusion gene. Despite of neuro-meningeal prophylaxis, there was clinical evidence of CNS involvement. Compassionate treatment with campath-1H, 30 mg/dose, for 5 doses, was administered i. v., obtaining a peripheral blood blast clearance, but not a CR. The patients eventually died 17 months after diagnosis due to leukemic progression.
DISCUSSION
BCR/ABL1 and BCL2/IGH rearrangements are common molecular abnormalities in B-cell malignancies. In particular, the BCR/ABL1 rearrangement is the most frequent genetic aberration in adult B-ALL(20–22). On the other hand, t(14;18)(q32;q21) with BCL2/IGH rearrangement is the most common abnormality in tumors derived from peripheral B-lymphocytes, whereas it is absolutely rare in B-cell precursor malignancies (24). However, while the biological role of BCR/ABL1 in acute leukemia is at least partially well known(25), the significance of BCL2 in ALL is still largely indefinite. BCL2 overexpression, without BCL2/IGH rearrangement, is frequent in ALL, and does not seem to be associated with a poorer prognosis (26). On the contrary, t(14;18)(q32;q21) and BCL2/IGH rearrangement are a rarity in ALL, but are associated with very aggressive tumors. Morphologically, the described cases are often L3, according to their immunophenotype of mature B-ALL, with Burkitt-like features. Notably, in all cases, complex karyotypes were observed, with almost constant involvement of the 8q24 locus and MYC deregulation(5–13). Sequential emergence of molecular abnormalities has been proposed in these cases, with progression from indolent (BCL2/IGH positive) to aggressive (BCL2/IGH and MYC positive) B-cell tumors (5–13). Therefore, they most likely represented leukemic variants of high-grade B-cell lymphomas with “double hits”. On the clinical ground, most of the patients presented with rapidly worsening general condition, fever, fatigue, night sweat, and weight loss; massive bone marrow and blood involvement, nodal and extra-nodal infiltration were also present. Clinical course was aggressive, with a median overall survival usually below than 12 months(5–13).
To the best of our knowledge, the association between t(14;18)(q32;q21) and BCR/ABL1 rearrangement has not been previously described in ALL. Nevertheless, a case of co-existing
BCR/ABL1 and BCL2/IGH rearrangements was reported in a MDS case(27). Our patient presented with a pre-B ALL, L2 subtype, carrying the t(14;18)(q32;q21) and other additional chromosomal aberrations, such as del(6)(q21;q25) and t(9;9)(p11;p22) but lacking 8q24 involvement; the BCR/ABL1 rearrangement was documented only by molecular analysis. Clinical course was aggressive, with recurrent relapses, CNS involvement, and death within seventeen months. Interestingly, at relapse, the patient presented a different karyotype [t(1,5)(p32;q31), del(12)(p11;p13), quite common as secondary abnormalities], still showing the BCL2/IGH rearrangement. Furthermore, during the clinical history of the patient, other chromosomal aberrations appeared. The relationship between the molecular events, and even a possible sequential appearance cannot be established. No peculiar morphologic or immunophenotipic patterns can be identified, to be easily associated to either one translocation, and the bad prognosis could be conferred by both the main genetic alterations; however, a dominant role of BCL2/IGH should be hypothesized, since it was always present during all disease phases. In this regard, based on the lack of cytogenetic evidence of Philadelphia chromosome we cannot exclude that BCR/ABL1 rearrangement constituted a sub-clonal lesion, cleared out by the more specific targeted therapy (chemotherapy plus imatinib).
Certainly, the treatment of t(14;18)(q32;q21) positive ALL remains a major problem, as conventional therapy are scarcely effective. Probably, the highly proliferating phenotype is made highly insensitive to chemotherapy by the antiapoptotic effect of BCL2, as observed in high-grade B-cell lymphomas with double hits.
The present case, besides its unicity, also confirmed the importance of molecular testing after cytogenetic analysis in human leukemia. Future experiences and hopefully trials will be useful to improve the current treatment of t(14;18)(q32;q21) positive ALL by adopting more rationally targeted therapies such as BCL2 inhibitors (eg venetoclax), peroxisome proliferator-activated receptor-gamma ligands (28), or others.
For more information: https://jmedcasereportsimages.org/about-us/
For more submission : https://jmedcasereportsimages.org/
#B-acute lymphoid leukemia#BCR/ABL1#t(14;18)(q32#q21)#BCL2#Philadelphia chromosome#apoptosis#Imatinib#targeted therapy#Cytogenetic Nomenclature#Genikon#DNA#Pier Paolo Piccaluga#jcrmhs
0 notes