#ive been diagnosed with 7 disorders conditions or syndromes
Text
ugh.
I'm sorry I've been so absent. I'm really trying to post more for you all.
more info under the cut
i think ive mentioned that i have various health issues and conditions before
the big ones affecting me right now are seasonal affective disorder, fribromyalgia/chronic pain syndrome, and plantar fasciitis in both feet and on top of all that, i am currently transitioning.
theres a lot of financial strain on me at the moment; my fiance's income is the only one we have. i'm too disabled to work a regular job but not disabled enough to receive disability income. thanks america. but yeah i owe over $1400 to various medical offices in addition to the ongoing copays for my various meds (a month's worth of t is $60), thanks america, AND i'm about to turn 26 next month, after which i will no longer be able to be on my parents' health insurance, thanks america.
all that to say that if i continue to be somewhat absent I'm very sorry
#dangwriting#about dang#fuck i hate it here#medical issues#american health system#it sucks#im 26 years old#ive been diagnosed with 7 disorders conditions or syndromes#9 if you dont count having something in both sides of your body as one item#i hate the american healthcare industry#healthcare should be socialized
7 notes
·
View notes
Text
WHY DOES IBS AS A DIAGNOSIS EXIST?
So, if it doesn’t make any sense, why does it still exist and why do a whole bunch of smart people still use it everyday? Well, the simple answer is: we gravitate towards labels to reduce perceived uncertainty and fear. Translation: it feels less scary to be told you have IBS (along with 10% of the population) rather than “we’re not sure what is wrong with you”.
As the man credited with creating the IBS label, Walter C. Alvarez, said in 1947: “The great thing in handling these persons is not to reinforce their fear that there is something seriously wrong with the colon” (4). A label can also allow patients to feel their condition is understandable, that there is research on it and that they are part of a community. It means a person suffering with IBS is not alone or unique, but rather has a condition that others have been able to manage.
IBS has historically been known as a diagnosis of exclusion (3). That is, “we haven’t been able to find a specific cause for your symptoms, sorry”. However, because the unknown element of this diagnosis provided little comfort to many sufferers, attempts have recently been made to make the term a ‘positive diagnosis’. That is, a single condition diagnosed with the Rome IV criteria, rather than the ‘wastebasket’ diagnosis of unknown cause/s. But while a label might make this group of symptoms easier to talk about and provide comfort to sufferers in the short term, it actually does little to empower an individual to find a long-term solution to their symptoms. And I am here to tell you, it is VERY likely that there is a solution.
Sources listed in the article (ones listed in the excerpt are bolded):
Mearin, F., et al. (2016). Clinical Practice Guideline: Irritable bowel syndrome with constipation and functional constipation in the adult. Rev Esp Enferm Dig, 108(6), 332-63
Saha, L. (2014). Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World Journal of Gastroenterology, 20(22), 6759–6773
Camilleri, M. (2012). Irritable bowel syndrome: how useful is the term and the “diagnosis”? Therapeutic Advances in Gastroenterology, 5(6), 381–386
Alvarez, W. (1947). Indigestion and abdominal pain with negative findings. Canadian Medical Association Journal, 57(5), 425–432
Canavan, C., West, J., & Card, T. (2014). The epidemiology of irritable bowel syndrome. Clinical Epidemiology, 6, 71–80
Chang, H., et al. (2015). Irritable bowel syndrome and the incidence of colorectal neoplasia: a prospective cohort study with community-based screened population in Taiwan, Br J Cancer, 112(1), 171-6
Distrutti, E., Monaldi, L., Ricci, P., & Fiorucci, S. (2016). Gut microbiota role in irritable bowel syndrome: New therapeutic strategies. World Journal of Gastroenterology, 22(7), 2219–2241
Major, G., & Spiller, R. (2014). Irritable bowel syndrome, inflammatory bowel disease and the microbiome. Current Opinion in Endocrinology, Diabetes, and Obesity, 21(1), 15–21
Spiller, R. (2008). Review article: probiotics and prebiotics in irritable bowel syndrome. Aliment Pharmacol Ther, 28(4), 385-96
Sekar, U., & Shanthi, M. (2013). Blastocystis: Consensus of treatment and controversies. Tropical Parasitology, 3(1), 35–39
Embree, J. (1998). Dientamoeba fragilis: A harmless commensal or a mild pathogen? Paediatrics & Child Health, 3(2), 81–82
Blanchard E., et al. (2008). The role of stress in symptom exacerbation among IBS patients. J Psychosom Res, 64(2), 119-28
Kennedy, P., Cryan, J., Dinan, T., & Clarke, G. (2014). Irritable bowel syndrome: A microbiome-gut-brain axis disorder? World Journal of Gastroenterology, 20(39), 14105–14125
0 notes
Text
The Good, The Bad, and The Ugly - Autistic Representation
Autism - “A serious developmental disorder that impairs the ability to communicate and interact. Autism spectrum disorder impacts the nervous system.The range and severity of symptoms can vary widely. Common symptoms include difficulty with communication, difficulty with social interactions, obsessive interests, and repetitive behaviors. Early recognition, as well as behavioral, educational, and family therapies may reduce symptoms and support development and learning.” - Mayo Clinic
I don’t usually, nor do I plan on beginning any educational posts in the future - this is simply (hopefully) a one time thing. Though I highly highly doubt it will be. But this I absolutely need to discuss. I feel that I am qualified to do so as well as I’ve been diagnosed with Autism Spectrum Disorder (specifically Asperger’s Syndrome when the DSM IV was still around) since I was 6 or 7 years old. So I have lived just about one and a half decades with it. Well at least with it diagnosed. Truly I’ve lived with it for all 20 years and 11 months of my life.
In this post I plan on discussing mainly books, but also referencing to movies and tv shows as I deem necessary. I will also give suggestions of excellent books with autistic representation at the end of this post bolding, and italicizing the ones written by autistic authors.
Now, without further ado, let’s jump right on in.
The Ugly
We are starting with the worst of the worst - not so I can upset people over their faves but so that you can anticipate the best at the end of this post. I am going to stick to one major example for each category until the last one. As far as “The Ugly,” I am going to be referencing The Maid by Nita Prose.
While it is never officially stated that she is autistic, there is enough insinuation that the lack of a label is almost offensive. If you are going to write a current day, “realistic,” murder mystery thriller, then you should be labeling your characters. And don’t do that “oh I don’t want to put them in a box.” Sometimes people have to be. If I hadn’t been labeled I wouldn’t have gotten the accommodations I needed in High School or College. That being said, there are some aspects here that seem accurate. The desire for a routine life, reading too far into certain conversations, missing out on social cues. I can certainly be glad they didn’t pull the counting toothpicks or burning down houses stereotypes. Outside of that, it just felt wrong. I can’t put a finger on it, and I reiterate that in the review. I think many of my complaints are similar to others, but the neurodivergency nearly felt fictional and I almost wished she’d at least watched the ABC Freeform tv show Stitchers, because while the condition Kirstin has isn’t autism, there certain gaping similarities that are discussed in the show (there’s an episode where she “stitches” into an autistic man’s brain and figures out how he died in 4 seconds because his brain was so similar to hers), that it has been my favorite show for a very long time.
The Bad
Mind you, this example I DNFd rather quickly - as I had learned my lesson with other books. The Gilded Wolves by Roshani Chokshi. I went into this book extremely excited after hearing it featured not only a Jewish main character (I am half jewish myself) but that character was also autistic. When I got to her introduction I have never seen so many stereotypes and contradictions in one page. She is mentioned to basically be an arsonist, and love numbers. She is said to only like the “pale bland sugar cookies” and doesn’t know how to ask for more other than standing right behind Laila with an empty tray. But she was smart enough and socially adjusted enough to attend university until her arson. How on earth does that make sense? It felt like they were trying to infantilize the condition, which... feels not great. There are many autistic people out there who can love flavorful foods, love colors, and know how to cook or ask for more. Those same people may not feel comfortable at university, be scared of fires or be terribly at math and love words instead. Autistic people are extremely variable, and while I didn’t finish the book, there was clearly a reason as to why.
The Good
Finally! The good! About damn time. Well, this is a slightly amusing story if you can believe it. So the same morning I finally decided to shelve The Gilded Wolves, I picked up Seraphina by Rachel Hartman. It was at the top of my physical TBR cart as it is a book that I am borrowing from my mom, so I need to finish it soon so I don’t forget to give it back, so I just leaned over and started it. Not only was the immediate prose gorgeous, but soon I discovered that the dragons are absolutely based on autistic people. In this case, it not being a specific label is understandable (same as above) because it is extremely high fantasy. Omran is described as loving difficult mathematics instead of just numbers and hating itchy clothing and is shown to miss social cues, such as greeting before launching into conversation. In one of the memories that Seraphina gets to see of her mother, she discovers that her mother was obsessed with her music, and seemed to know quite know how to word the feeling of deep love. Not enjoying metaphor, but not elaborating exactly why. Yes she does still compare kissing Seraphina’s father to equations but its only one thing she compares it to - she still compares it to “seen the numbers behind the moon and stars, behind mountains and history, art and death and yearning, as if my comprehension is large enough that it can encompass universes from the beginning to the end of time.” (p. 91)
Even if it is not the author’s intention to make the dragons an entire species of autistic people, I’d prefer an accident like that to the aforementioned purposeful attempts at neurodivergent characters.
More (will be updated as I discover more)
Vespertine by Margaret Rogerson
#autism#autism spectrum disorder#the maid#nita prose#Vespertine#margaret rogerson#the gilded wolves#roshani chokshi#seraphina#rachel hartman
20 notes
·
View notes
Text
Cyclic Vomiting Syndrome Treatment in India

Cyclic Vomiting Syndrome is characterized by episodes of extreme vomiting with no clear cause. Episodes can last for hours or days and overlap with symptom-free periods. Episodes are similar, which means that they appear to start at the same time of day, last the same amount of time, and occur with the same symptoms and severity. Cyclic vomiting syndrome occurs in all age ranges, but it mostly starts in children between 3 and 7 years of age. While it is more common in children, the number of cases diagnosed in adults is growing. The condition is difficult to diagnose since vomiting is a symptom of many disorders. Treatment also requires behavioural changes that can prevent vomiting episodes from occurring. Medications, including anti-nausea and migraine therapy, can help to reduce symptoms.
Symptoms of cyclic vomiting frequently begins in the morning. Signs and signs shall include:
• Three or more repeated episodes of vomiting that begin at around the same time and last for a similar amount of time.
• Variation of periods of usually normal health without nausea between episodes
• Extreme nausea and sweating until the episode begin
Other signs and symptoms during a vomiting episode may include:
· Abdominal pain
· Diarrhea
· Dizziness
· Sensitivity to light
· Headache
· Retching or gagging
There is no treatment for cyclic vomiting syndrome, but many children no longer have vomiting episodes until they reach adulthood. For those with a cyclic vomiting episode, care focuses on the monitoring of signs and symptoms. You or your child may be administered for the following:
• Anti-nausea drugs
• Pain-relieving medications
• Medications that suppress stomach acid
• Antidepressants
• Anti-seizure medications
The same kind of medicines used for migraines often helps avoid or even eliminate cyclic vomiting episodes. These drugs may be recommended for people with regular and long-term episodes or those with a migraine family history. To avoid dehydration, IV fluids can be needed. Treatment is individualized depending on the length, and occurrence of complications of the symptoms. Lifestyle changes can help to control cyclic vomiting syndrome signs and symptoms. Cyclic vomiting syndrome normally involves ample sleep. After vomiting starts, it can help to remain in a dark, quiet room in bed and to sleep. Some people may feel well enough to start eating a regular diet shortly after vomiting stops. However, you could start with clear liquids, if you or your kid does not feel like eating right away, and then add solid food slowly.
If stress or excitement causes vomiting episodes, consider finding ways to alleviate stress and keep calm during symptom-free periods. Instead of three big meals, it can also benefit to eat small meals and snacks every day. Alternative and additional medications can help to avoid episodes of vomiting, but none have been well studied. Before beginning any supplements, be sure to see a doctor and get a cyclic vomiting syndrome diagnosis confirmed. Check that your doctor is always confident you or your child takes a healthy dosage and that the supplement does not interfere adversely with any drugs you are taking before you take any supplement. Some people can experience side effects similar to cyclic vomiting syndrome symptoms, such as nausea, diarrhea, and appetite loss, as a result of coenzyme Q10, L-carnitine, and riboflavin.
Since you never know when the next episode could happen, the whole family might have a hard cyclic vomiting syndrome. Children may be very concerned and continually worry that when an episode occurs, they will be with other children. You or your child will benefit from talking to someone who knows how to deal with cyclic vomiting syndrome confusion. Ask your doctor about your local support groups.
At Healing Touristry, we give caring, personalized, and outstanding treatment. As a medical tourism service provider, our experience is not limited to connecting you with the best doctors and hospitals, but to ensuring your overall well-being in a country that might be contrary to yours. A success rate of more than 90% is evidence of our commitment to delivering the most advanced care for both routine and serious illnesses. At Healing Touristry, we can provide you with an expert pool of doctors and hospitals for Cyclic vomiting syndrome Treatment in India from our elaborate list of Hospitals. Healing Touristry is widely recognized as one of the best in medical hygiene safe treatment as well as maintaining the standards of safety and privacy of its patients.
#Cyclic vomiting syndrome Treatment in India#Cyclic vomiting syndrome Treatment#Cyclic vomiting syndrome#Cyclic vomiting syndrome Treatment Hospitals#Cyclic vomiting syndrome Treatment Doctors#Healing Touristry#medical service provider
5 notes
·
View notes
Note
how does sarah cope with the pain at work? also has she been diagnosed with anything or is it a classic case of “you’re a woman. pain is natural. have some Tylenol”
Screams that’s literally how my doctor treats me :) love it when men think hysteria is still a plausible diagnosis
Okay so Sarah’s current diagnoses include
PTSD, anxiety, and a presumed depressive disorder (Probably all as a result of the PTSD)
Chronic migraines which she had had since she was 7 :(
Chronic costochondritis/Tietze syndrome which is where the cartilage/joint of the rib cage becomes inflamed and it mimics heart attack symptoms
A heart arrhythmia that causes severe cardiac events sometimes (shortness of breath, chest pain, 160+ BPM) but her rhythm is always normal and there has never been any indication of a defect so her tachycardia is labeled as “idiopathic”
(Which Ava hates because she knows there might be an underlying issue so she’s trying to help Sarah find answers)
Widespread musculoskeletal pain and she gets random fits where her muscles spasm and tremor
She made the educated guess that she has fibromyalgia because her two preeexisting diagnoses are related to the condition and also the musculoskeletal symptoms among other things makes sense
She is trying to see a rheumatologist to get a proper diagnosis but it’s hard because fibromyalgia is one of the most controversial diagnoses
Because like... people don’t believe pain :/
She sees Sam regularly for her migraines because she has some stroke-like symptoms that raised concerns
So she needs some close monitoring just in case
But he thinks they’re just hemiplegic migraines which is rare but would make sense considering she has no actual indication of ischemic strokes
Also she was Connor’s patient for a bit because when she first mentioned the debilitating chest pain that radiated down her arm and the heart palpitations ava was like ????????
Sarah: *has heart attack symptoms* this is fine :)
Ava: Sarah Reese what the actual fuck
After scans and blood tests and EKGS though connor concluded that she was not having a heart attack
And he spoke to some pain specialists who reviewed her symptoms and diagnosed the tietze syndrome/costo
Which sucks because it’s supposed to be something that goes away after a few months but Sarah is just... living with it on and off for years
ANYWAY
Those are her diagnoses/issues
As for how she copes at work
Advil is her best friend
She has a pill organizer filled with Tylenol, Advil, muscle relaxers, and anti-nausea meds that she always keeps in her locker
Because yeah she works in a hospital but it’s always good to be prepared
Honestly she just pushes through the pain most days
Telling herself “just one more hour. One more patient. You can’t give up now”
And she does that through the whole day
Forcing herself to focus and subsequently expend all her energy
Because chronic fatigue is a symptom of all her diagnoses so she’s just... always exhausted :(
Coffee definitely helps
Well it doesn’t make the heart arrhythmia any better but try telling Sarah she can’t have coffee it won’t end well
She has a multitude of braces for literally every joint and depending on the day and how she woke up she may be sporting a different one every few days
Wrist and knee braces are the most common because repetitive moments are killer on her joints
The most annoying thing is when her hands are aching for no reason and she’s tremoring so she can’t safely insert an IV or something and she just gets so frustrated
Unfortunately she has a habit of pushing herself way too far
Going to work even when she’s having a big flare up
Not taking her perscription painkillers because she doesn’t think she “needs them” as is “saving them for a worse pain day”
Pushing through the brain fog from a migraine and the dissociation that comes with it
Forgetting to eat after taking her meds and being nauseous all day
She just works so hard to be a normal doctor and Ava hates to see her do this to herself
So obviously she is the one who has to be like
Sarah for the love of God slow down and rest
And sometimes it takes a lot of persuasion
And Sarah gets frustrated
But she knows Ava does it out of love and concern
And she is really grateful for her because Ava is her rock
#all of these diagnoses are mine 🤩#except the PTSD thats Sarah’s lmao#I’m just anxious#anyway#this is incoherent I’m so sorry hsjsks#anyway hugs for sarah#chicago med#sarah reese#ava bekker#reesker#chronic#spoonie!sarah#my aus#my-writing#mutuals#asks#crockettstiddies#long post#I’m too lazy to go on my laptop and add a read more 😔
9 notes
·
View notes
Text
Juniper Publishers| Acute Aortic Dissection: Update on Diagnosis and Application of Endovascular Therapy of Emergency
Abstract
Acute aortic syndrome (AAS) describes emergency aortic diseases. In 80% of patients, the AAS presents itself as an Acute Dissection of Aorta (ADA). It’s worth pointing out that the traumatic etiology of this condition, has great relevance regarding morbidity and mortality. This is fact that the Traumatic Thoracic Aortic Dissection (TTAD), usually occurs from a contuse injury, product of an abrupt deceleration, especially in men and individuals with overweight or obesity, which have a history of smoking and heart surgeries. Early diagnosis of ADA is indispensable, since patients who arrive alive at the hospital, have high probability of death in a short period of time if not treated properly, especially those who have been victims of some traumatic event earlier. In this context, the endovascular approach has become the treatment of choice for acute surgical emergencies involving the descending thoracic aorta. Moreover, it should be considered as a first-line option in the conduct of any emerging conditions that involve this region of the aorta. It is important to note that the longevity and durability of this technology throughout the life of young patients remains to be elucidated.
Keywords: Acute aortic syndrome; Acute aortic dissection; Dissection of aorta; Endovascular repair
Abbreviations: AAS: Acute aortic syndrome; ADA: Acute Dissection of Aorta; TTAD: Traumatic Thoracic Aortic Dissection; IH: Intramural Hematoma; PAU: Penetrating Atherosclerotic Ulcer; IRAD: International Registry of Aortic Dissection; CAT: Computed Angiotomography; TET: Transthoracic echocardiography and Transesophageal ETT and ETE; MRI: Magnetic Resonance Imaging; CT: Computed Tomography; CPB: Cardiopulmonary Bypass; EC: Extracorporeal Circulation
Go to
Introduction
Acute Aortic Syndrome (AAS) is a term used to describe emergency aortic disorders, with regard to its characteristics and challenges. Because of this, one can cite: acute aortic dissection (AAD), intramural hematoma (IH) and penetrating atherosclerotic ulcer (PAU). The incidence of this syndrome is three cases per 100,000 people per year. Of all patients who present with a SAA, 80% are AAD, 15% HI and 5% corresponds to the PAU [1]. Most patients who arrive alive at the hospital, if they are not subjected to a systematic approach and conducive situation, have a high probability of death in a small time interval [2]. As AAS occurs through an injury to the wall of this artery due to a certain type of stress or even medial degeneration, it is essential to know the risk factors that can cause this fragility [3].
The conditions associated with the medial degeneration include Marfan syndrome, Loeys-Dietz syndrome, vascular Ehlers-Danlos syndrome, inflammatory diseases of the aorta, Turner syndrome, bicuspid aortic valve, familiar syndrome of thoracic aortic aneurysm and dissection [4]. The most common condition that increases the stress of wall is hypertension. Other conditions involved in the dissection include: history of trauma, weight lifting, pheochromocytoma, coarctation and cocaine [4].
Meet the clinical signs is essential, once, tied to Imaging tests, they become important allies to diagnose or rule out a leave according to the technology available inservice [5]. In addition, in a patient with hemodynamic stability studies, graduating from injury is essential to direct more productive and effective conduct. The image examinations for your time, besides being favorable for the diagnosis, can assist in choosing the best surgical technique. If there are no unfavorable anatomical changes, the choice of approach will depend on the patient’s hemodynamic condition, availability of resources and professional skill in question [5-7].
From this reality, this article has as purpose, do a literature review on the acute aortic dissection, clarifying the main and latest methods of diagnostic and therapeutic approach. In addition, underscores the urgent need, the preparation of the team on admission of patients affected by this disease, so that it is possible to decrease the incidence of undiagnosed cases, optimizing the time between the initial approach and appropriate conduct [8].
Go to
Methods
This work was done from an electronic search in the databases PubMed, Scopus, Scielo and Embase Search Portal. We collected data from case reports, cohort studies and literary reviews, using the key words: acute aortic syndrome, acute aortic dissection, dissection of aorta, endovascular repair. The method presented the following guiding question: “what are the main results and scientific evidence identified in national and international bibliographical production of the last 26 years pertaining to diagnostic and therapeutic approach of acute aortic dissection?”
In the initial survey, the articles went through the evaluation of nine researchers (authors), in accordance with the following inclusion criteria: articles published in Portuguese, English or Spanish, to submit the combinations of the keywords selected, with publication date between 1989 and 2015 that were accessible. After the initial selection of material, were deleted the articles repeated in different databases and they focus on the aortic pathologies other mixed in question. Although picked by articles that cover effective updates in the treatment, the therapeutic failure was not used as a criterion for deletion, considering the particularity of the manifestations of each case. The final material featured 46 scientific articles.
Go to
Results
The AAD is a potentially fatal condition that requires rapid assessment and intervention. However, despite the great advances in imaging methods and non-invasive studies, the correct diagnosis is not always the rule, therefore the diagnosis errors often occur [9]. Approximately 30% of cases are found in post-mortem exams [8]. Patients with this disease presents to the Emergency Department with a wide variety of symptoms, due to the involvement of multiple organ systems [10]. However, there are occasions when the medical history is insufficient to know the frame [10].
Go to
Clinical Presentation
The patient may complain of chest pain, pain in interescapular region, dyspnea and dysphagia [3]. The physical examination may show signs suggest chest trauma, such as the seatbelt sign, heart murmur, hematemesis, palpable depression or deformity of the sternum. As well: stridor, crepitation in chest wall, grinding noise on the precordium (Hamman signal), hematoma subclavian and femoral pulses decreased [3]. If the patient is hemodynamically unstable must be forwarded immediately to the operating room [11]. Stable patients can be investigated more precisely through Imaging tests.
Go to
Diagnostic Methods
The evolution of technology has resulted in highly sensitive diagnostic tools and specific, however, the widespread use of these diagnostic methods, results in an increase in the number of false positives. Such limitations should be considered in clinical decisions, and it is important that additional tests in patients hemodynamically stable [12]. The international registry of aortic dissection (IRAD) lists the computed angiotomography (ATC) as the first most common diagnostic test on suspicion of aortic dissection (about 61%), followed by Transthoracic echocardiography and Transesophageal (ETT and ETE) (around 33%), magnetic resonance imaging (MRI) (around 2%), in addition to angiography corresponding to 4%. This reflects their availability and accessibility of these modalities [13] (Figure 1).
The chest x-ray in supine anteroposterior position, can be useful, since in an initial assessment, despite having low sensitivity, shows signs that direct the diagnosis or the need for other tests [5]. These evidences are: widening of the mediastinum (> 8cm); abnormal aortic contour; deletion of aortic button; orotracheal tube and trachea deviation to the right; source left bronchus depression; diversion of nasogastric tube to the right; extrapleural apical leakage; a density; fracture of the first and second ribs; obliteration of the space between the pulmonary artery and aorta; elevation and deflection to the right of the right main bronchus; hemothorax. The helical computed tomography (CT) of chestno cuts must be indicated after the fine interpretation of trauma mechanisms [3]. Is the most common initial examination because it is less invasive and allows quick diagnosis in emergency situations [14]. Is an excellent method for diagnosis to triage patients with suspected aortic injury, showing a sensitivity ranging from 93% to 100% and specificity of 87% to 100% [3,15,16] (Figure 2).
With this test, you can distinguish the mediastinal blood from other causes dilation of the mediastinum, in addition to show if there is intimate or laceration, hematoma, aortic pseudoaneurysm, periaortic rupture contained or active extravasation of IV contrast [11]. It’s worth pointing out that the primary diagnostic criterion is the demonstration of two lumens full of contrast separated by an intimate tab [15]. The minimally invasive transesophageal echocardiography, is widely available, secure, and can be accomplished quickly and easily on the edge of the bed or in the operating room before the operation. These advantages make this ideal for use in most patients with aortic dissections, including those relatively unstable. The examination can be carried out immediately after the patient to come to the Emergency Department. Their sensitivity ranges from 95% to 98% and specificity of 63% to 96% [17,18].
The most important discovery in the diagnosis of aortic dissection, which can be seen in this survey, is the presence of a border rippling intimal within the lumen of the aorta, which differentiates a false lumen light real [19]. The arteriography was used for many years as the mode of choice to demonstrate the aortic dissection. Is an effective procedure to demonstrate the direct signals of dissection, the flap of the intimate and blood flow in the true and false lumens [19]. Erbel et al. [17] reported 88% sensitivity and specificity of 94% for this examination in the diagnosis of aortic dissection. However, for being an invasive method, became a secondary diagnosis mode.
Magnetic resonance imaging (MRI)is a non-invasive research, providing an excellent analysis of the valvar pathologies, and aortic coronary involvement. Although it is the most accurate, sensitive and specific between the four modes of diagnosis [16], your use is limited in emergency situations, in patients hemodynamically unstable, as well as in patients with Implantable devices. That way, she will eventually cede space to the computed angiotomography methods and echocardiography in emergency cases [20]. Has a sensitivity around 95% and specificity of 100% [21]. The advantage of MRI over CT, is your ability to provide functional information such as valve failure and left ventricular dysfunction [19] (Figure 3).
The use of quantitative tests of D-Dimer serum, have been proposed as a strategy to ward offaortic dissection [22]. Proponents of this approach suggest that the blood in the false light, activates the coagulation cascade by generating fibrin degradation products. These are detected by modern D-Dimer assays with high sensitivity. Unfortunately, the work has demonstrated high false negative rate. In one study, D-Dimer presented false negatives in 9 of 113 confirmed cases of aortic dissection [23].
The proposed explanation for D-Dimer tests false negatives, is the occurrence of an anatomical variation of aortic dissection, whose thrombosed lumen, does not communicate with the circulating blood, isolating the clot detection by serum tests [23]. In addition, there is no evidence that D-Dimer can be incorporated into a strategy of risk stratification, which would allow the sensitive clinical enough to exclude aortic dissection, without significantly increasing the number of patients who receive advanced imaging tests. Given the experience of D-Dimer testing to rule out pulmonary embolism-which increased the number of advanced studies of image without increasing the number of diagnoses of pulmonary embolism [24]. A comprehensive approach to answer for false negatives and false positives, should be validated before this exam to be used routinely in the diagnosis of aortic dissection [24].
Go to
Clinical Approach
The initial treatment has as main objective to reduce the shear stress in the wall of the aorta, through the control of blood pressure. The first line of treatment are beta blockers intravenously (labetalol or propranolol). Those with contraindication for this drug class (asthma) [25], is preferable to the use of intravenous calcium channel blocker (verapamil or diltiazem). Because of this, it is necessary to get a systolic blood pressure that oscillates between 100 and 120mmHg, as well as a range of heart rate between 60 and 80bpm. Besides, we recommend the use of an opioid analgesic (morphine), to reduce sympathetic discharge produced by catecholamines. These are generated by pain, due to the hypertension and tachycardia [26].
It is worth mentioning that the initial conduct in stable patients depends on the degree of the injury established after CT [5,6]. There are four ranks: type I-intimate layer, without blood extravasation; type II - intramural hematoma; type III - pseudoaneurysm; type IV - break free/periaortic hematoma. In milder cases (type I), opts for the use of beta blockers for fast action and short half-life, decreasing blood pressure and keeping your heart rate below 100 bpm, if they are contraindicating, a calcium channel blocker or associated with intravenous nitroglycerine if there is the effect objectified. In addition, it is necessary to perform Imaging exams serials to accompany the evolution of the injury. In more severe lesions (types II, III and IV), as well as volume replacement and blood pressure control, surgical repair is required for open or endovascular technique [5,6].
Go to
Surgical Approach
Regarding surgical techniques, we can cite the open technique based on a left thoracotomy in cases of injury of the descending aorta or sternotomy in patients with injury of the ascending aorta for primary repair of the aorta or the replacement of the affected segment by a graft or graft [7]. In the descending aorta lesions, should be made the establishment of diversion of blood flow through centrifugal pumps and cannulation of the left atrium and left common femoral artery, as well as systemic heparinization. This technique is preferable in patients with unfavorable anatomy [7]. It’s worth pointing out that many patients do not survive the initial event, consequently does not undergo a repair attempt.
Endovascular thoracic aortic repair (TEVAR), refers to the minimally invasive approach, which involves placing a stent graft in thoracic aorta or ring, possessing ample indications. The technique involves inserting modular grafts through the dissection of iliac or femoral arteries to thoracic aorta excluding vessel damage [7] (Figures 4 & 5). In the case of femoral arteries, after dissection of the right femoral puncture of femoral artery left there for the introduction of catheter, where there is the diameter of the aorta and if intralaminar defects are excluded, when inserted into the stent. Is recommended in victims with favorable anatomy, and has a more comfortable postoperative period and brief [7].
A series of studies, has suggested various subgroups of highrisk patients without complications, which can benefit from early TEVAR. The specific predictors of early or late adverse events have been identified in multiple studies, and include: an aortic diameter of 4.0cm home, with a false light patent [27- 29], an initial diameter of 22mm light on proximal descending aorta [30], refractory/recurrent pain or hypertension [31] or intramural hematoma with a penetrating atherosclerotic ulcer development in the proximal descending aorta [27,29]. About the disasters involving the descending thoracic aorta, the management have been particularly difficult for surgeons. The open surgical correction in these cases, is the gold standard. However, is associated with significant mortality and morbidity. This makes this procedure, one of the most risky and difficult to be carried out by vascular surgeons [32].
The widespread application of endovascular repair, for the treatment of acute surgical emergencies involving the descending portion of the aorta, resulted in a dramatic decrease of both the operative mortality as post procedure morbidity [33]. The open repair for traumatic rupture of the aorta, is associated with an operative mortality of up to 28% and 16% rate of paraplegia [33]. While a systematic review of literature on endovascular therapy, reveals an overall rate of 9% and a mortality rate of 3% of the paraplegia analyze 7768 patients undergoing the procedure in effect of traumatic dissection of aorta [34]. Recently published guidelines for the Society for Vascular Surgery, with practical guidelines that suggest that endovascular procedure must be standard therapy for the treatment of traumatic rupture of the thoracic aorta [35]. Thus, the endovascular approach has become the treatment of choice for acute surgical emergencies, involving the descending thoracic aorta. Moreover, it should be considered as a first-line option in the conduct of any emerging conditions that involve this region of the aorta [36].
Endovascular repair brings advantages and limitations. Among the advantages described, include: avoid the thoracotomy, decrease the incidence of complications less painful, faster recovery, shorter stay in intensive care and in hospital, an alternative for high-risk patients, less postoperative complications, useful in emergency situations and speed and agility of treatment [37]. Among the limitations found: institutional and political constraints, limited availability and accessibility, unavailable commercially in some countries, the appropriate requirement of vascular anatomy, limited number of qualified operators, lack of appropriate follow-up and palliative care in most cases [37].
However, endovascular correction is not without risks. This procedure is associated with a small but measurable rates of stroke (2% of cases), spinal cord ischemia (0.9% of cases), reported in the trials and meta-analysis that investigated this type of therapy [38-41]. In addition, endovascular procedures are associated with higher rates of complications related to the device. They are expensive and require an extended image tracking. In addition, the longevity and durability of this technology throughout the life of young patients remains to be elucidated [39].
In the first month, post-operative angiography should be performed by a CT scan, followed by study of image in six months, and then annually. TEVAR in patients with non-optimal anatomy for the procedure, requires more rigorous follow-up. The realization of the computed tomography without contrast allows the measurement of the diameter of the bag and is enough in most cases to document effective aneurysm exclusion [42]. Magnetic resonance angiography is an alternative, although it is of limited applicability in patients with significant renal dysfunction [42]. A secondary is relatively common aortic intervention after the endovascular repair [43,44].
Go to
Discussion
According to the American Heart Association guidelines on the management of thoracic aortic diseases, we have that the acute aortic dissection can be categorized in a patient of high, medium and low risk according to clinical presentation [45]. In cases of high risk or intermediate probability, one must quickly make the injury screening with imaging to visualize the aorta. Obtaining a negative result, opts for another investigation. The cardiac ultrasound is offered by AHA as secondary technique more common [20]. It’s worth pointing out that a CT must be part of the pre-surgical routine, as well as being performed by a trained and highly experienced cardiologist or cardiac anesthesiologist. This procedure is required in all patients with suspected acute aortic dissection type A [10].
The work performed by Tiwari et al. discusses several puncture techniques that were proposed in the establishment of the cardiopulmonary bypass (CPB) for the surgery of acute type A aortic dissection. Despite the concern with the fragility of the vases, and distal embolization during ascending aortic cannulation of a dissected aorta, there were promising results, with a lower mortality rate and lower incidence of poor perfusion. However, it was observed a higher rate of stroke. A total of seven studies evaluated the use of direct aortic cannulation for the establishment of the extracorporeal circulation (EC). They have shown and stroke mortality rates from 0% to 15% and 3.8% and 21%, respectively. The direct cannulation of the true light is an emerging method for quick and easy establishment of EC [46].
Although the femoral artery puncture is the default option in many centers, there is a higher rate of mortality of stroke and other complications, including cerebral embolization bad organ perfusion retrograde perfusion of the false light. In this work, five of the 14 studies analyzed, reported benefits of axillary artery cannulation (or subclavian). In a total of 1829 patients evaluated in these studies, 1068 patients demonstrated a significantly lower rate of complications with the axillary artery cannulation in comparison with the femoral artery [46].
Some large studies have shown that the femoral artery cannulation have high rates of stroke and mortality ranging from 6.5% to 40%, and 3% to 17%, respectively. Meanwhile, and mortality rates of stroke ranged from 3% to 8.6% and 1.75% and 4%, respectively, in the axillary artery cannulation procedure [45]. This new strategy emerges as a more efficient method for the EC, providing unilateral continuous blood flow without interruption. Although need more time for your accomplishment, the axillary artery with lateral graft, proved to be safe and straightforward, with less local and systemic complications, lower mortality and reduction of neurological complications [46]. It is important to note that in the case of hemodynamic stability, and the patient in question is subject to a traumatic brain injury or multiple severe injuries in other systems coexisting, but there is no indication of impending rupture of the aorta, aortic, pneumothorax massive thrombus or pseudoaneurysm, thoracic aortic repair chosen must be conservative (pharmacological control of arterial pressure) to stabilization of other injuries or comorbidities by decreasing the amount of anesthetic held, as well as the surgical risk [5,6].
Go to
Conclusion
Most of the patients are victims of a ruptured aorta after an accident, die immediately. However, the small portion survivor, has about 24h for that light to rupture. As the clinical findings are nonspecific and poor, shows need for greater professional skill, regarding the efficient diagnosis, rapid and appropriate treatment to approach this serious pathology. It is important to point out that when we are facing a situation of hemodynamic stability and the first-rate research results are conflicting, it is necessary to refer the patient to a high level of investigative rigor before surgical intervention. An alternative to conventional surgical treatment is the use of endoprothesis, reserved for patients properly selected. In addition, it is essential the imageexams serials, as well as medical follow-up according to age, comorbidities and patient kidney function.
To read more articles in
Journal of Surgery
Please Click on:
https://juniperpublishers.com/oajs/index.php
For More
Open Access Journals
in
Juniper Publishers
Click on:
https://juniperpublishers.com/journals.php
juniper publishers Linkedin
0 notes
Text
NAD+ IV Therapy for Lyme Symptoms: What is Nicotinamide Adenine Dinucleotide (NAD+)?
NAD+ intravenous (IV) therapy offers hope as a treatment for those with chronic conditions, including Lyme disease (Borrelia burgdorferi).
Lyme disease is a chronic disease that is transmitted to humans when infected black legged ticks (known as deer ticks) bite the skin and subsequently embed themselves.
Even after antibiotic treatments, people diagnosed with Lyme may continue to report debilitating symptoms such as joint pain, fatigue, weakness, brain fog, inflammation and neurological symptoms.
Nicotinamide Adenine Dinucleotide (NAD+) is a coenzyme found naturally in all the cells of the body and is integrated in various functions. It is a vitamin B3 (niacin) derivative that plays a vital role in energy production within the cells.
Studies have shown that NAD+ declines with age. As the natural aging process kicks in, the body fails to synthesize new NAD+ and the body may struggle to recycle NAD+ in the cells.
It is also believed that NAD+ levels decline in the presence of chronic diseases, including Lyme. Inflammation may result from chronic diseases because oxidative stress tends to increase in the body. However, research shows that intravenous NAD+ therapies or oral treatments of NAD+ precursors show promise in alleviating Lyme symptoms.
NAD+ IV therapy for Lyme symptoms
According to research from 2015, oxidative stress is suggested to be a potential result of the Lyme disease pathogen. Oxidative stress can trigger chronic inflammation symptoms because it elicits an immune system response to chronic pathogens (i.e. the bacteria that causes Lyme disease, Borrelia burgdorferi). Furthermore, oxidative damage ensues to proteins, DNA, and lipids, which have been linked to various chronic diseases (i.e. Lyme disease, chronic fatigue syndrome, cancer, Parkinson’s, Alzheimer’s and atherosclerosis).
During this particular 2015 study, a high build-up of mitochondrial superoxides – a free radical that contributes to oxidative stress – was found in those with Lyme when compared to the control group. This has led to the hypothesis that mitochondrial dysfunction takes place in Lyme disease and, therefore, NAD+ levels are depleted.
Today, many integrative functional medicine practitioners help restore NAD+ levels in Lyme patients intravenously to alleviate oxidative stress and help manage inflammation.
NAD+ mechanism of action: How does it help alleviate Lyme symptoms?
NAD+ IV therapy may benefit patients with Lyme disease in these ways:
NAD+ contributes to the formation of adenosine triphosphate (ATP), the unit in which we measure energy in the living cells.
Data suggests that NAD+ IV therapy may improve the cognitive function of individuals with chronic conditions, including Lyme disease.
NAD+ may help a person feel less tired; this may contribute to the overall well-being of the mitochondria, which are like tiny energy-producing factories in your cells. Scientists suggest that chronic diseases contain mitochondrial dysfunction in their physiopathology.
NAD+ IV therapy may improve your mood and cognitive functions by helping your brain create additional neurotransmitters.
Should you try NAD+ IV therapy to help treat Lyme symptoms?
Are you concerned that you’ve been exposed to infected black legged ticks? Or do you want to learn more about natural ways to alleviate Lyme symptoms?
At our Toronto-based clinic, Dr Amauri Caversan, ND, and Arv Buttar, NP, are available to help their patients with integrative and functional medicine programs. Our NAD+ IV therapy program, a part of the integrative treatment approach for lyme disease, may help assist the body in restoring neuroreceptor function to an optimal level. This program may also promote improved sleep, detoxification, cell health replenishment and physical and mental longevity. Book your appointment today – click here to send us a message.
References
Barbosa JA, Sivaraman J, Li Y, et al. Mechanism of action and NAD+-binding mode revealed by the crystal structure of L-histidinol dehydrogenase. Proc Natl Acad Sci U S A. 2002;99(4):1859-1864. doi:10.1073/pnas.022476199
Fang EF, Lautrup S, Hou Y, et al. NAD+ in Aging: Molecular Mechanisms and Translational Implications. Trends Mol Med. 2017;23(10):899-916. doi:10.1016/j.molmed.2017.08.001
Massudi H, Grant R, Braidy N, Guest J, Farnsworth B, Guillemin GJ. Age-associated changes in oxidative stress and NAD+ metabolism in human tissue. PLoS One. 2012;7(7):e42357. doi:10.1371/journal.pone.0042357
Pall ML. Common etiology of posttraumatic stress disorder, fibromyalgia, chronic fatigue syndrome and multiple chemical sensitivity via elevated nitric oxide/peroxynitrite. Med Hypotheses. 2001;57(2):139-145. doi:10.1054/mehy.2001.1325
Peacock BN, Gherezghiher TB, Hilario JD, Kellermann GH. New insights into Lyme disease. Redox Biol. 2015;5:66-70. doi:10.1016/j.redox.2015.03.002
“Pharmacy Compounding Committee Review: Nicotinamide Adenine Dinucleotide (NAD+)” viewed on September 3, 2020.
Pohanka M. Role of oxidative stress in infectious diseases. A review. Folia Microbiol (Praha). 2013;58(6):503-513. doi:10.1007/s12223-013-0239-5
Rajman L, Chwalek K, Sinclair DA. Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence. Cell Metab. 2018;27(3):529-547. doi:10.1016/j.cmet.2018.02.011
Zhu XH, Lu M, Lee BY, Ugurbil K, Chen W. In vivo NAD assay reveals the intracellular NAD contents and redox state in healthy human brain and their age dependences. Proc Natl Acad Sci U S A. 2015;112(9):2876-2881. doi:10.1073/pnas.1417921112
RECENT BLOG POSTS
NAD+ IV Therapy for Lyme Symptoms: What is Nicotinamide Adenine Dinucleotide (NAD+)?
NAD+ intravenous (IV) therapy offers hope as a treatment for those with chronic conditions, including [...]
29
Sep
4 Surprising Things to Know About NAD+
What is NAD+? Well, in order for our bodies to run smoothly, we need NAD+! [...]
20
Jan
IV Vitamin Therapies – Which Kind You May Need?
IV vitamin therapy comes in different types and is given to address specific health conditions. [...]
09
Dec
The blog post NAD+ IV Therapy for Lyme Symptoms: What is Nicotinamide Adenine Dinucleotide (NAD+)? first appeared on Dr. Amauri Caversan
0 notes
Text
12 Things To Know Before Starting Chemotherapy

Cancer can cause a number of unexpected medical complications for patients, making it deadly. Many people have heard of chemotherapy and know it's a set of treatment cycles that uses drugs to treat and can help eventually beat cancer. However, most people still don't have any medical understanding or information about cancer and its adverse effects. In addition, there are a number of types of chemotherapy treatment cycles and other types of cancer therapy. The type of chemo for a patient used by their oncology doctors and their team depends on what might work best for the particular cancer diagnosis, its side effects, and its medical information. Read on for twelve things you should learn about chemotherapy treatment cycles for better understanding before you or your loved ones begin cancer treatment.
1. How is Cancer formed?
The body is composed of trillions of healthy human cells. Cancer begins when something triggers changes in a normal cell. This cancer cell then grows out of control and creates more cancer cells. Each kind of cancer can affect the body in adverse ways. If cancer is not treated in time, it can spread to the rest of your body and cause life-threatening complications. Your oncology doctor and the team may give chemo drugs to help treat your cancer. Often chemotherapy is used to slow down the spread of cancer. Sometimes the treatment goal is given to alleviate symptoms or problems caused by growing cancer tumors. It can be used to improve health.
2. What is Chemotherapy?
Chemotherapy is the use of a number of potent drugs for cancer diagnosis and treatment including ovarian and breast cancer. Chemotherapy is sometimes called "chemo" because of the same combination of cancer medication used. During the 1950s Chemo was first used to help treat cancer. Chemo has made it possible for many people to live a healthy life. An oncology doctor's given chemo drugs have been tested several times to see if they work before they are used for patients. Chemotherapy treatment cycles and radiation therapy is used to help treat cancer cells. It has made it possible for many people to live cancer-free.
3. How are Chemo drugs chosen?
Today more than 100 chemo drugs are given in treatment and they work to help treat cancer. Using the drug information, oncology doctors and specialty teams choose the best medications or chemo substance depending on the type of cancer that you have and its stage (how much cancer is in your body). This can be used by combining chemo drugs for different purposes. Before you begin cancer treatments and a radiation therapy cycle your doctor will give this treatment information to you.
4. How does Chemo help with my Treatment Goals?
Oncology doctors and professionals make use of the best Chemo drug combinations and radiation therapy to help treat cancers including ovarian and breast cancer that have metastasized. Metastasized means cancer that has spread to other parts of the body. Be sure to talk to your oncology doctors about the goal of your treatment and get all the information regarding side effects. The drug combinations given can also have a possible effect on normal cells too. But most normal cells are used to repairing themselves so the good outweighs the bad.
5. How is Type of Chemotherapy Determined for Treatment?
Your complete cancer treatment procedure options to be used will be determined by a few factors. The type of cancer you have, the stage at which you have been diagnosed, whether or not you have received chemotherapy treatment or radiation therapy before, and your personal health history. If the cancer is metastatic, you may not get the type of chemo commonly given through an IV. This treatment is called infusion chemo. For metastatic cancer, Chemotherapy pills that have a particular drug combination are given and must be taken every day, and you only have to visit the hospital once a month to receive an injection. This drug combination injection given is used to enhance healthy bone growth since the metastasized cancer might be attacking your bones.
6. How is Chemotherapy Used?
The oncology team will give Chemotherapy treatments for cancer in many ways including orally, topically, intravenously using IV drips, through injections, intra-arterial administrations, and intraperitoneal administrations. The final treatment and drug combination will be decided by your oncology team.
7. How Often Will I Get Chemotherapy?
How often you undergo chemotherapy treatment varies widely, factors depending on the cancer diagnosis, the form of chemotherapy, the cancer treatment objectives, and other factors. This may be constant or it may alternate with rest periods in between depending on the cancer treatment plan and drug combination as determined by the oncology doctor.
8. What Will Chemotherapy Feel Like?
What you feel when you get chemotherapy treatment depends on a variety of factors including the form of chemotherapy the oncology team gives you, the cancer diagnostic level, the history of personal health, and the capacity of the patient to cope with the symptoms. Symptoms can be noticeable for certain people and other symptoms can take days or even weeks to develop. Typical chemotherapy treatment side effects include fatigue and nausea. In others, these are short bouts from which they can easily recover and for others, the symptoms may last longer. Managing your symptoms and health at your own pace is crucial, and ensure that you take care of yourself during cancer treatment. There is no reason to worry as your oncology team will help you.
9. Not all Chemo Drugs cause Hair Loss
If your oncology team gives you an infusion chemo cycle, you will have to go to the hospital for just a few hours of chemo treatment. Following this, you may have a few days of side effects. Side effects depend on factors like drug or combination of drugs you get, some may not cause hair loss. Side effects regarding your health vary and include aches and pains, nausea and vomiting, diarrhea, hair loss, and other factors. You may have mouth sores for certain medications and loss of appetite, taste, smell, or all three. It's pretty rough to endure, but believe that chemo will do its job and will help you become healthy. This mindset will make you face cancer treatments bravely.
10. Feeling Uneasy is Normal
You'll most likely wake up in the morning on the first day of chemo with anxiety in the heart because you're not sure what's to come. Take a book, a newspaper, your knitting, or any favourite hobby to help you pass the time and keep your mind off it. Having chemo via an IV normally takes a long time. Remind yourself that it is for the sake of your health and undergo your treatment.
11. Always Ask the “What if” Questions
An underlying or secondary disorder may cause severe harm. So don’t hesitate to inform your doctor about your health history. Ask professionals and learn about how particular types of cancer treatment might work to affect you. Ask for the reason when something is done. You can help avoid some unnecessary pain and unwanted treatments if you question your doctor about each step of the treatment given. For example, if you suffer from an underlying bleeding condition. It can cause the hand-foot syndrome, a rare side effect. This can lead to slow leakage of blood from the hands and feet from the tiny capillaries which will soon develop into severe bleeding. As a result, you may have to stay in the hospital longer.
12. Can Chemotherapy make me Cancer free?
If surgery was done to remove a cancerous tumor, such as a lumpectomy for breast cancer, or hysterectomy for ovarian cancer, your oncology specialist may give chemotherapy drugs in cycles, and radiation therapy is given to make sure that any leftover cancer cells are eliminated too. Chemotherapy is also given for making you ready for other types of cancer treatments. It is sometimes given to treat a cancer tumor so it can be surgically removed. Different types of chemo drugs are also given for making you prepared for radiation therapy. During late-stage cancer treatment, chemotherapy drugs are used to alleviate pain.
Conclusion
Chemo may be an inevitable part of your cancer treatments so stock up on healthy and whole foods. Keep yourself hydrated. It can help ease some side effects. So have plenty of low-sugar drinks or juice on hand. Be prepared with frozen meals or book a meal delivery service because you may not feel up to cooking after chemo treatment. Snack on fruits, vegetables, and healthy high-protein food like yogurt. Give yourself time to recuperate and learn your limits. Reach out to an understanding family member or friend to help when your side effects become difficult to manage. There is no reason to undergo it alone.
0 notes
Text
You are still valid if you have:
Major depressive disorder PT 7
The DSM-IV-TR recognizes five further subtypes of MDD, called specifiers, in addition to noting the length, severity and presence of psychotic features:
Melancholic depression is characterized by a loss of pleasure in most or all activities, a failure of reactivity to pleasurable stimuli, a quality of depressed mood more pronounced than that of grief or loss, a worsening of symptoms in the morning hours, early-morning waking, psychomotor retardation, excessive weight loss (not to be confused with anorexia nervosa), or excessive guilt.
Atypical depression is characterized by mood reactivity (paradoxical anhedonia) and positivity, significant weight gain or increased appetite (comfort eating), excessive sleep or sleepiness (hypersomnia), a sensation of heaviness in limbs known as leaden paralysis, and significant social impairment as a consequence of hypersensitivity to perceived interpersonal rejection.
Catatonic depression is a rare and severe form of major depression involving disturbances of motor behavior and other symptoms. Here, the person is mute and almost stuporous, and either remains immobile or exhibits purposeless or even bizarre movements. Catatonic symptoms also occur in schizophrenia or in manic episodes, or may be caused by neuroleptic malignant syndrome.
Postpartum depression, or mental and behavioral disorders associated with the puerperium, not elsewhere classified, refers to the intense, sustained and sometimes disabling depression experienced by women after giving birth. Postpartum depression has an incidence rate of 10–15% among new mothers. The DSM-IV mandates that, in order to qualify as postpartum depression, onset occur within one month of delivery. It has been said that postpartum depression can last as long as three months.
Seasonal affective disorder (SAD) is a form of depression in which depressive episodes come on in the autumn or winter, and resolve in spring. The diagnosis is made if at least two episodes have occurred in colder months with none at other times, over a two-year period or longer.
In 2016, the United States Preventive Services Task Force (USPSTF) recommended screening in the adult populations with evidence that it increases the detection of people with depression and with proper treatment improves outcomes. They recommend screening in those between the age of 12 to 18 as well.
A Cochrane review from 2005 found screening programs do not significantly improve detection rates, treatment, or outcome.
To confer major depressive disorder as the most likely diagnosis, other potential diagnoses must be considered, including dysthymia, adjustment disorder with depressed mood, or bipolar disorder. Dysthymia is a chronic, milder mood disturbance in which a person reports a low mood almost daily over a span of at least two years. The symptoms are not as severe as those for major depression, although people with dysthymia are vulnerable to secondary episodes of major depression (sometimes referred to as double depression). Adjustment disorder with depressed mood is a mood disturbance appearing as a psychological response to an identifiable event or stressor, in which the resulting emotional or behavioral symptoms are significant but do not meet the criteria for a major depressive episode. Bipolar disorder, also known as manic–depressive disorder, is a condition in which depressive phases alternate with periods of mania or hypomania. Although depression is currently categorized as a separate disorder, there is ongoing debate because individuals diagnosed with major depression often experience some hypomanic symptoms, indicating a mood disorder continuum. Further differential diagnoses involve chronic fatigue syndrome.
Other disorders need to be ruled out before diagnosing major depressive disorder. They include depressions due to physical illness, medications, and substance abuse. Depression due to physical illness is diagnosed as a Mood disorder due to a general medical condition. This condition is determined based on history, laboratory findings, or physical examination. When the depression is caused by a medication, drug of abuse, or exposure to a toxin, it is then diagnosed as a specific mood disorder (previously called Substance-induced mood disorder in the DSM-IV-TR).
3 notes
·
View notes
Text
Who To Talk To About Drug Addiction
Contents
Continue using despite
Taking drugs they are
Combines the most history
Acclaimed treatment center for alcohol
Prescription drug abuse

Freedom From Addiction is drug rehab & alcohol treatment centre in Toronto, Ontario. We provide recovery from cocaine addiction, alcohol addiction, substance abuse ...
Drug addiction, also called substance dependence or dependence syndrome, is a condition where a person feels a strong need to take a drug. Addiction also involves ...
Addiction is a brain disorder characterized by compulsive engagement in rewarding stimuli despite adverse consequences. Despite the involvement of a number of ...
Why Does The Dsm Iv Cover Drug Addiction And Alcoholism Contents Drug use … and Have been limited And primitive cultures Prescription treatment centers. timberline knolls Get the latest health news THERE IS POTENTIAL FOR CULTURAL AND SOCIAL BIAS IN DSM-V. … used to identify alcohol and drug use … and the DSM-IV alcohol abuse diagnosis. Addiction … Catherine does not qualify for a DSM-IV How To Help Someone With Drug Addiction And Depression Contents continue using despite History information provided just nervous Alcohol and drug addiction Drug abuse nervous timberline knolls assists Starts taking drugs they are estranged get Drug Addiction Statistics in the U.S. We are a nation in crisis. There is hardly a family that has not been affected by addiction. The statistics on the matter How Can Drug Addiction Cause Ill Health For Women Contents Our program combines Just found they are estranged And causes heroin and prescription Treatment centers. timberline knolls assists women That change the Older people’s reactions to medications or symptoms of disease can be misread by health care providers as dementia, leading to wrong diagnoses and missed … Get the latest health news, diet & How To Get Help For Drug Addiction Without Money Contents Our program combines the most history information provided just Nervous strength alone. but Assists women the Leading residential treatment centers. timberline knolls Hope Rehab is an internationally acclaimed treatment center for alcohol and drug addiction. our program combines the most effective therapies available. Drug addicts from Toronto, London and Chatham are relocating to Windsor, How Can You Help Someone With A Drug Addiction For Women Contents And prescription drug abuse nervous Timberline knolls assists women History information provided just found They are estranged Girls seeking lasting recovery from drug Hi Gabby, Even though I am not recovering from addiction, I apprecaite all you do for everyone. I am nineteen years old and I have been using your tools since I
[embedyt]//www.youtube.com/embed/PY9DcIMGxMs[/embedyt]
The above post Who To Talk To About Drug Addiction is courtesy of https://detoxnear.me/
from DetoxNear.me - Feed https://www.detoxnear.me/who-to-talk-to-about-drug-addiction-7/
0 notes
Text
S. M. Yasir Arafat, Dhat syndrome: Culture bound, separate entity, or removed, J Behavioral Health (2017)
Abstract
Dhat syndrome is a culture bound syndrome of the Indian subcontinent, although this has often been debated. Although it is being researched for more than half a century, there is still no clear definition of Dhat syndrome and characterized by excessive preoccupation with the loss of “Dhat,” which is generally taken to be representing semen and attribution of physical and psychological symptoms. It is usually seen in young, unmarried, or recently married men of rural background with conservative attitude toward sex, generally belong to low or medium socioeconomic status and education level. It can be treated with anxiolytics, antidepressants, as well as psychological interventions such as psychoeducation, sex education, counseling, and cognitive behavior therapy. There is long debate regarding the nosological position of the disease and recent call for attention of psychiatrists in the subcontinent to revisit the nosological status of Dhat syndrome with an unbiased mind. Further, systematic studies on the phenomenology of Dhat syndrome is needed to clarify it, especially keeping in mind the extent of the problem in the subcontinent and the distress and dysfunction it results in.
Introduction
Culture bound syndromes or cultural specific syndromes are recurrent locality specific patterns of aberrant behavior and troubling experience generally restricted to specific geographical areas, and usually they refer to certain conditions that are traditionally considered to be illnesses, have cultural explanations, and often have local names as well [1]. Dhat syndrome is generally believed to be a culture bound syndrome of the Indian subcontinent, although this has often been debated and more in recently [1-6]. It is characterized by excessive preoccupation with loss of “Dhat,” which is generally taken to be representing semen and attribution of physical and psychological symptoms to the same [1-6]. Although it is a clinical entity, mostly seen in South East Asia, originated, nurtured, and carried forward by many orthodox cultural beliefs; but it is also reported from many other geographical regions such as Central Asia, China, Russia, America, and Europe [6,7]. It was aimed at reappraising the Dhat syndrome based on recent evidence and controversies.
Definition and Dhat Concept
Although it is being researched for more than half a century, there is still no clear definition of Dhat syndrome [1]. “Dhat syndrome,” term first used in scientific literature by a renowned Indian Psychiatrist Professor N N Wig described as a specific syndrome nurtured as a result of culture-related beliefs and considered as a conglomeration of multiple psychosomatic symptoms, including sexual symptoms in the absence of physical illnesses [8]. However, it is considered as a culture bound syndrome, characterized by the presence of somatic, anxiety, depressive, and sexual symptoms, all of which are attributed to loss of semen [5]. Even, International Classification of Diseases and Health Related Conditions, 10th edition (ICD-10) and 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) did not consider any specific number number for the condition [3,6,9,10].
The term “Dhat” was derived from songskrito and the ancient vedic depiction of body fluids called “dhatus” and among the seven different body fluids (dhatus) mentioned in veda; semen is perceived to be most precious one [6,7]. Ancient ayurvedic literature also mentions genital secretions as highly precious and purified body fluid and emphasizes about its conservation for health and longevity as well as the formation of semen by the process of purification and condensation through several steps (from food, through blood, flesh, and marrow) [6,7]. This belief is carried ahead over centuries by traditional healers, who are dealing with such issues since the ancient days [7]. Professor N N Wig has coined the term “Dhat syndrome” to the psychosomatic attribution related to semen loss in 1960 [7].
Although, Malhotra and Wig described Dhat syndrome due to loss of semen through nocturnal emissions or passage in urine, the patients with Dhat syndrome also attributed their symptoms to semen loss through other means such as masturbation, during defecation, and even sexual intercourse [7]. Many times people are concerned and visit the physicians in regards to the loss of pre cum juices mentioned in layman term or seminar fluid during erotic thoughts and acts. In the International Classificatory Systems, for the 1st time Dhat syndrome got a place as a diagnosis entity, in the ICD-10 and 4th edition of the DSM-Text Revision (DSM-IV) [7,9].
Psychopathology or Abnormal Belief
Various kinds of beliefs exist regarding Dhat syndrome in Indian cultures [1]. The Charaka Samhita mentions that imbalance of the bodily humors or excessive ejaculatory orgasm can lead to harm to the dhatus [1,3]. Many people believe food is progressively transformed to blood, marrow, and then semen whereas some people believe that the cavernosal blood is lost as semen following ejaculation [1,3]. It is also a prevailed dictum is “it takes 40 drops of food and 40 days to form one drop of blood; 40 drops of blood to form one drop of marrow and 40 drops of marrow to form one drop of semen” [3,6]. There are also some notions regarding this value to be 100 drops and not 40 [6]. Therefore according to these systems, loss of semen from the body will result in physical weakness and loss of energy [3,6,7]. The loss could occur either through urine only or through any other route such as nocturnal emission, masturbation, homo/heterosexual sex, pre/extramarital sex, or through the anus, and even the discharge of the seminal fluid [1]. Studies revealed a significant portion of patients; about 25% of the patients diagnosed as having Dhat disorder did not report passage of Dhat through urine [1,3]. There are also reports to loss semen in another ways such as the anal route [1,3]. A study revealed, 18% believed Dhat to be pus, 12% believed it to be concentrated urine, and another 12% believed it to be sugar [1,6]. Patients suffering from Dhat syndrome perceived that it could increase the chances of birth of more female children, death at early age, malformed fetus, betrayal in love, betrayal in friendship, and financial worries and semen loss can lead to cause anemia, leprosy, or tuberculosis [1,3].
Sociodemographic Profile
Dhat syndrome is usually seen in young, unmarried, or recently married men of rural background with conservative attitude toward sex generally belong to low or medium socioeconomic status and education level [1-7]. However, previous studies revealed that it occurs irrespective of education status or domicile and it is also found to be present in patients from all religious backgrounds [1,3]. Although, it is thought to be a male diseases authors have argued for a Dhat syndrome in females as well [1,3,7,11-13]. The age of onset of symptoms of Dhat syndrome was found in second to third decade of life and mean age was found in early 20s [2,7]. Patients of dhat syndrome mostly acquire knowledge regarding the illness from friends, relatives, colleagues, roadside advertisements, lay magazines, hakims, and vaids [1,3,6].
Symptom Profile and Comorbidities
Patients with Dhat syndrome presented with vague somatic symptoms, weakness, guilt, lethargy, anxiety, loss of appetite, sleep disturbances, listlessness, lack of physical strength, poor concentration, forgetfulness, multiple body pains, sexual dysfunction, burning micturition, increased frequency of micturition, difficulty in micturition, and many other symptoms [1-3,5-8,12]. Researchers have mentioned that there may be three presentations of Dhat syndrome-Dhat syndrome alone, Dhat with comorbid depression and anxiety, Dhat with sexual dysfunction [4,6]. Authors, however, reckoned that, several of these symptoms could possibly be of other comorbid disorders such as depression, anxiety, sexually transmitted diseases, or urinary tract infections, somatoform disorder, hypochondriacal disorders, premature ejaculation, erectile dysfunction, impotence, stress reaction, phobias, depressive psychosis, obsessive ruminations, body dysmorphic symptoms, and delusional disorders [1-3,5,6,8].
Assessment Tools
For a long time, there was no formal assessment tool to evaluate Dhat syndrome and recently Grover et al. had developed a comprehensive questionnaire for the evaluation of Dhat syndrome [14].
Diagnosis
There does not appear to be clear and specific diagnostic symptoms of Dhat syndrome, and even the diagnostic conventions are yet to mention the specific criteria [3,6,9,10]. At the core of the diseases is the preoccupation of the patient with the loss of Dhat from the body and the belief that this loss results in significant harm to physical, mental, or sexual well-being as well as there is a wide variability in literature regarding the constituent of “Dhat” and the mode of passage of Dhat [3]. Dhat has been defined in some studies specifically as semen, while other studies define it broadly as any whitish discharge [1-3].
Treatment
Although, the patients suffering from Dhat syndrome perceived “desi” medicines, herbs, advice of hakims and vaids, dietary interventions, protein and iron rich food, B-complex tablets or injections, antibiotics, antianxiety drugs, aphrodisiacs, and marriage can cure the symptoms, there is no support in favor of those as possible found in scientific evidence [1,3]. The core features of Dhat syndrome, commonly respond to antianxiety or antidepressant medications, as well as psychological interventions such as psychoeducation, sex education, counseling, and cognitive behavior therapy [3,7,8,15]. Integration of psychiatry and allied disciplines (the collaborative approach of psychiatrists, psychologists, psychiatric social workers, psychiatric nurse, etc.); integration of other medical disciplines with psychiatry (collaborative approach with other medical disciplines such as general medicine, dermatology and venereology, urology, and neurology); integration with alternative systems of medicine and traditional healers (collaboration with Ayurvedic, Homeopathic, Unnani, and Siddha practitioners; the traditional healers is an important aspect of treatment [7]. Till date, the majority of patients with psychosexual disorders reach general medical practitioners, practitioners of alternative medicine, and traditional healers, and rather than going to a psychiatrist for consultation [7].
Researchers suggested emphatic listening, a nonconfrontational approach, reassurance and correction of erroneous beliefs, along with the use of placebo, antianxiety, and antidepressant drugs, wherever required [6]. Sex education primarily focuses on anatomy and physiology of sexual organs and their functioning with reference to masturbation, semen, nocturnal emissions, and relaxation therapy mainly consists of Jacobson’s progressive muscular relaxation technique, which can be combined with biofeedback (so as to facilitate objective evidence and mastering of anxiety by the patient) [6].
Controversies
Albeit, Dhat syndrome is generally considered as a culture bound syndrome of the Indian subcontinent, it has often been debated from a long time and more in recently [1]. Before inclusion of Dhat syndrome in the classificatory systems (ICD-10 and DSM-IV), a lot of debate was going on regarding its nosological status, which was expected to end with its inclusion, but it continued for years together and still on [1,7]. After its inclusion in the classificatory system, questions were raised whether it was worthy occupying a place in the diagnostic system or not. Many argued that it can be equivalent to depression and may be used as a specifier of depression, or it may be cultural way of manifesting the distress. As a result, it reached the glossary section of DSM-5 describing cultural concepts of distress and subsequently it raises a big question regarding whether Dhat syndrome exists or not?” [7]. In view of the comorbidity and the symptom profile, some of the researchers consider it as a variant of depression and others consider it as a variant of somatization disorder [1-3,16]. There are other issues related to Dhat syndrome is whether it should be considered as a culture bound syndrome or it is a global concern? There are evidence regarding the existence of Dhat syndrome in different cultures, and those are not confined within the geographic boundary of India. Although, it is most prevalent in India; it is also reported in many other countries such as Pakistan, Bangladesh, Nepal, Sri Lanka, China, Malaysia, Indonesia, Japan, America, Russia, Spain, and other European countries. Moreover, besides India; evidence of semen as a “soul substance” could be found in the works of Galen and Aristotle who have explained the physical and psychological features associated with its loss; the works of Beard, Hare, and Maudsley linked semen loss with mental illness [1,3,6,7,16]. Again although ICD-10 and DSM-IV-TR mentioned as culture bound syndrome, there are lacking in regards to the specific criteria, and DSM-5 replaces the diagnosis from a syndrome terming it as “not a true syndrome” [3,6,9,10,17,18]. One school of researchers recommended looking at explanations of semen loss as fluid cultural idioms of distress rather than as a standalone diagnostic entity as even the purest variety of Dhat syndrome is not a stable diagnosis in the majority of patients [4]. Another group of researchers liked to mention as a more a global phenomenon, rather than being a culture-bound one and in this era of globalization; the migrants from different cultures assimilate the new culture as well as dissipate their native cultural characteristics, which may attenuate culture bound syndromes and increased awareness [19,20]. However, researchers who are in favor of keeping the syndrome as cultural bound argues with their evidence and mentioned that the points against the syndrome are weak as well as by merely doing away with Dhat syndrome by labeling it as a depressive disorder will only curb further work in this already neglected area of research [17]. Furthermore, there is recent call for attention of psychiatrists in the subcontinent to revisit the nosological status of Dhat syndrome with an unbiased mind [17].
Conclusion
Dhat as a symptom is important for assessment of psychosexual problems, but the nosological position of Dhat syndrome in the official classifications of professional organizations is yet to be settled. In addition, there is as yet no clarity as to whether Dhat syndrome is a unitary entity or it comprises sub-syndromes. Therefore, there is a need for systematic studies on the phenomenology of Dhat syndrome demonstrating the evolution of various groups of symptoms to clarify the same. Symptoms related to Dhat syndrome are also found in populations other than oriental populations, but it is especially important keeping in mind the extent of the problem in the subcontinent and the distress and dysfunction it results in.
References
Prakash S, Sharan P, Sood M. A study on phenomenology of Dhat syndrome in men in a general medical setting. Indian J Psychiatry 2016;58:129-41.
Grover S, Gupta S, Avasthi A. Psychological correlates and psychiatric morbidity in patients with Dhat syndrome. Indian J Psychiatry 2015;57:255-61.
Deb KS, Balhara YP. Dhat syndrome: A review of the world literature. Indian J Psychol Med 2013;35:326-31.
Sameer M, Menon V, Chandrasekaran R. Is ‘pure’ Dhat syndrome a stable diagnostic entity? A naturalistic long term follow up study from a tertiary care centre. J Clin Diagn Res 2015;9:VC01-3.
Grover S, Gupta S, Avasthi A. A follow-up study of patients with Dhat syndrome: Treatment pattern, outcome, and reasons for dropout from treatment. Indian J Psychiatry 2016;58:49-56.
Prakash O. Lessons for postgraduate trainees about Dhat syndrome. Indian J Psychiatry 2007;49:208-10.
Kar SK, Sarkar S. Dhat syndrome: Evolution of concept, current understanding, and need of an integrated approach. J Hum Reprod Sci 2015;8:130-4.
Prakash O, Kar SK, Sathyanarayana Rao TS. Indian story on semen loss and related Dhat syndrome. Indian J Psychiatry 2014;56:377-82.
World Health Organization. International Statistical Classification of Diseases and Health Related Problems ICD-10. 2 Switzerland: World Health Organization; 2004.
American Psychiatric Association. Glossary of cultural concepts of distress. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. p. 833-9.
Grover S, Avasthi A, Gupta S, Hazari N, Malhotra N. Do female patients with nonpathological vaginal discharge need the same evaluation as for Dhat syndrome in males? Indian J Psychiatry 2016;58:61-9.
Grover S, Kate N, Avasthi A, Rajpal N, Umamaheswari V. Females too suffer from Dhat syndrome: A case series and revisit of the concept. Indian J Psychiatry 2014;56:388-92.
Singh G, Avasthi A, Pravin D. Dhat syndrome in a female - A case report. Indian J Psychiatry 2001;43:345-8.
Grover S, Avasthi A, Gupta S, Dan A, Neogi R, Behere PB, et al. Phenomenology and beliefs of patients with Dhat syndrome: A nationwide multicentric study. Int J Soc Psychiatry 2015;2015:1-10.
Salam KP, Sharma MP, Prakash O. Development of cognitive- behavioral therapy intervention for patients with Dhat syndrome. Indian J Psychiatry 2012;54:367-74.
Balhara YP. Culture-bound syndrome: Has it found its right niche? Indian J Psychol Med 2011;33:210-5.
Prakash S, Mandal P. Is Dhat syndrome indeed a culturally determined form of depression? Indian J Psychol Med 2015;37:107-9.
Prakash S, Mandal P. Is the DSM-5 position on Dhat syndrome justified? Asian J Psychiatry 2014;12:155-7.
Kar SK. Dhat syndrome: Will it reach a height or die soon? J Hum Reprod Sci 2015;8:246.
Ventriglio A, Ayonrinde O, Bhugra D. Relevance of culture-bound syndromes in the 21st century. Psychiatry Clin Neurosci 2016;70:3-6.
#psychiatry#bangladesh#global psychiatry#culture-bound syndromes#dhat#dhat syndrome#neurosis#culture#indian subcontinent#psychosexual dysfunction#mental illness#controversies in medicine#abnormal belief
0 notes
Text
Antonio Ventriglio et al., Relevance of culture‐bound syndromes in the 21st century, 70 Psychiatry & Clinical Neurosciences 3 (2015)
Abstract
Culture‐bound syndromes were first described over 60 years ago. The underlying premise was that certain psychiatric syndromes are confined to specific cultures. There is no doubt that cultures influence how symptoms are perceived, explained and from where help is sought. Cultures determine what idioms of distress are employed to express distress. Rapid globalization and industrialization have made the world a smaller place and cultures are being more influenced by other cultures. This has led to social and economic changes in parts of the world where such syndromes were seen more frequently. In this review we illustrate these changes using the example of dhat syndrome (semen‐loss anxiety). The number of syndromes in the DSM‐5 has been reduced, acknowledging that these syndromes may be changing their presentations. Clinicians need to be aware of social and economic changes that may affect presentation of various psychiatric syndromes.
Recent changes in the DSM‐5(1) may have abandoned the term ‘culture‐bound syndromes’ but in many parts of the world its use continues. Over 60 years ago, these syndromes appeared as exotic, alien, indigenous conditions seen in cultures that were also seen as less psychologically developed. Over the years, many of these syndromes have been reported from multiple cultures using different idioms of distress.
There is no doubt that cultures influence how people experience emotional distress, how they express it and in what terms and, more importantly, from where they seek help. Historically, colonizers saw those who were being ruled as exotic natives who were perhaps not very psychologically sophisticated and therefore ignorant and objects of observation. These psychiatrists and many anthropologist observers ignored existing indigenous health‐care systems, idioms of distress and the therapeutic interventions used by these populations. In many health‐care systems, the approach is much more social rather than biological and even when the body is affected, social factors are seen as playing a major role.
Background
Yap(2) was the first to describe culture‐bound psychogenic psychoses – a term subsequently abbreviated to ‘culture‐bound syndromes.’3 These were seen as ‘rare, exotic unpredictable and chaotic behaviors at their core among uncivilized people.’ There is no doubt that this was a reflection of the existing diagnostic systems where these systems were often difficult to classify. Bhugra and Jacob4 suggest that these behaviors were diagnosed with somewhat limited understanding of the cultural context. On the one hand, this is really surprising, as psychiatry is a medical specialty strongly influenced by cultural and social factors; but on the other hand, psychiatry may reflect somewhat rigid, patrician and paternalistic views.
In this commentary, we review the historical and current status of culture‐bound syndromes using dhat (a syndrome of semen‐loss anxiety seen very commonly in the Indian sub‐continent) as an illustrative example.
Nosological timeline
Yap first defined culture‐bound psychogenic psychoses in 1962.2 He modified the term to culture‐bound syndromes 7 years later3 and subsequently several such syndromes have been described and studied. In 1992, the ICD‐105 used the term ‘culture‐specific disorders’ and 15 years later the DSM‐51 abandoned the term to replace it with cultural concepts of distress (see the study by Ayonrinde and Bhugra for further discussion).6
What does ‘culture‐bound’ really mean? We believe that the concept of boundedness and whether certain illnesses are really bound to certain cultures is problematic. In particular, old traditional boundaries across cultures are becoming more porous and, with rapid globalization, cultural factors are becoming perhaps more diffuse and more accessible. The rapid increase in the use of social media and inter‐connectedness through increased and rapid access to media, including the Internet, has added another complicating and complex dimension.
Culture‐bound Syndromes in the Diagnostic Manuals (DSM and ICD)
As mentioned earlier, the rise of culture‐bound syndromes may be a reflection of the rise of Western diagnostic and classificatory systems and also the long‐standing impact of colonialism. Recent shifts in the DSM‐51 may indicate a change away from these factors. The two major psychiatric classificatory systems have used these syndromes in slightly different ways. Interestingly, the ICD‐10,5 which is a more culturally sensitive system, acknowledges that these syndromes are not easy to fit into classificatory categories.
ICD‐10 (1992)
The ICD‐105 recognizes a number of culturally uncommon symptom patterns and presentations referred to as ‘culture‐specific disorders.’ While acknowledging that these syndromes have diverse characteristics, they also have two common features:
They are not easily accommodated in established and international diagnostic categories.
Their initial description is in a particular population or cultural area and their subsequent association is with this community or culture.
The ICD‐10 has thus made cautious and tentative associations between cultural syndromes and recognized psychiatric categories, but the problem again is that these are culturally specific. We argue that these are reported from other cultures too and are not exclusive.
DSM‐IV‐TR (2000)
In the DSM‐IV‐TR,7 culture‐bound syndromes were seen as recurrent, locality‐specific patterns of aberrant behavior and troubling experience that may or may not be linked to a particular DSM‐IV diagnostic category.
The following characteristics were seen as crucial for culture‐bound syndromes:
Indigenously considered illnesses or afflictions – therefore a recognition within the society as a deviation from normal or healthy presentation.
Local names – the ascription of a specific local name to the experience of mental distress. This is often in the indigenous or key language of communication and may be components of folk diagnostic categories.
Symptoms, course and social response often influenced by local cultural factors – for instance the folk healing systems for the symptoms based on the explanatory model of the experiences.
Limited to specific societies or cultural areas – this may be a geographical region, areas with shared ethnic history or identity. For instance some cultural practices and artifacts of the Yoruba culture of western Nigeria may also be found in Brazil.
Localized – therefore experiences that are not globally recognized or span different regions.
The DSM‐51 discarded the concept of culture‐bound syndromes with a preference for the term ‘cultural concepts of distress.’ This has been defined as ‘ways cultural groups experience, understand, and communicate suffering, behavioral problems, or troubling thoughts and emotions.’ Consequently three cultural concepts have been identified: ‘syndromes’ (clusters of symptoms and attributions occurring among individuals in specific cultures); ‘idioms of distress’ (shared ways of communicating, expressing or sharing distress); and ‘explanations’ (labels, attributions suggesting causation of symptoms or distress).
Interestingly, the DSM‐5 emphasizes that all mental distress is culturally framed and acknowledges that different populations carry varying and culturally determined ways of communicating distress along with explanations of causality, coping methods and help‐seeking behaviors.
Changes in the Diagnostic Manuals (DSM and ICD)
For a time, there was an expansion in the number of culture‐bound syndromes from 25 syndromes in the DSM‐IV‐TR, but it has come down to nine in the DSM‐5. Not surprisingly, various concerns have been raised about the diagnostic validity of culture‐bound syndromes.8, 9
Culture‐bound syndromes are culturally influenced and, we would argue, also influenced by existing health‐care systems. Semen‐loss anxiety has been reported from many parts of the world as loss of semen due to nocturnal emissions or masturbation, and the condition affects individual notions of masculinity.
Dhat, or Semen‐Loss Anxiety Syndrome, in the Indian Sub‐Continent
Etymology
Dhat, or semen‐loss anxiety syndrome, includes symptoms of semen‐loss, which lead to complaints of weakness and anxiety. The word dhat is derived from the Sanskrit word dhatu, which means metal in Sanskrit and is also used as a colloquial term for semen. Early descriptions in 1960 by Wig and colleagues from north India observed that dhat syndrome involved many vague somatic complaints of weakness, fatigue, anxiety, loss of appetite, guilt and sexual dysfunction, which were seen as a direct result of semen loss following masturbation, nocturnal emissions or micturition.10, 11
Such symptoms have been noted in ancient Indian Ayurvedic texts dating to about 5000 BC. In these texts, semen production was described as ‘…food converts to blood which converts to flesh which converts to marrow and ultimately to semen.’ Each of these steps is supposed to take 40 days,12 thus making semen incredibly precious. These symptoms are widely recognized across the Indian subcontinent and folk and traditional treatments are easily available and widely sought, even though very little evidence exists for their success. We hypothesize that these treatments may work as placebo as the practitioners may be able to understand the cultural context.
As mentioned above, there is no doubt that, for men, semen‐loss and the resulting anxiety are incredibly important. Attitudes to masculinity, male sex roles, procreation and fertility all play a role in generating such anxiety. Similar values and anxieties were seen in industrial countries, such as Britain and the USA, in the 19th century. Dietary supplements, such as corn flakes and crackers, were advertised and sold as treatment for semen‐loss anxiety.3, 8, 9 In the Indian sub‐continent, faith healers and traditional healers continue to offer various types of food supplements, herbs and treatment strategies. It will be important to explore whether such anxiety has disappeared from industrial nations and the subsequent role globalization is likely to play in eliminating such anxieties or whether, on the other hand, it may further contribute to it. Urbanization is also likely to play a role as increased access to education spreads and higher levels of education and changes in understanding masculinity may well lead to a further reduction of the condition.
The future of culture‐bound syndromes or culture‐specific manifestations of distress as a range of disorders is uncertain, even though the DSM‐5 has taken the right steps. Recent reports of hikkikomori from Japan (where teenagers become withdrawn socially) raise a wider question as to whether this is a genuine response to changing pressures related to social media or something entirely different. There have been case reports from other parts of the world too.13, 14
The evolution of other culturally specific diagnostic systems, such as the Chinese Classification of Mental Disorders,15 may indicate a shift in some cultures from a universal classification of mental disorders to a more culture‐specific classification. We believe that psychiatry as a profession needs an urgent debate on universalist versus relativist classificatory systems.
Conclusions
With cultures in transition in many parts of the world as a result of inter‐connectedness and globalization, it is critical that clinicians are aware of how local cultures are changing. We believe that it is extremely likely that culture‐bound syndromes will no longer be culturally bound but culturally influenced. As a result of globalization, resulting and associated industrialization and urbanization may well lead to changes related to a move towards societies becoming more modern and less traditional, which in itself may change the perceptions and idioms of distress. Consequently, it is likely that not only will the expressions and idioms of distress change but so will the pathways to help‐seeking. We hope that, as a result of globalization, better understanding across cultures will lead to more balanced and nuanced approaches to diagnostic categories.
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. American Psychiatric Association, Washington DC, 2013.
Yap PM. Words and things in comparative psychiatry with special reference to exotic psychosis. Acta Psychiat. Scand. 1962; 38: 157–182.
Yap PM. The culture bound syndromes. In: Cahil W, Lin TY (eds). Mental Health Research in Asia and The Pacific. East-West Centre Press, Honolulu, 1969; 33–53.
Bhugra D, Jacob KS. Culture bound syndromes. In: Bhugra D, Monro A (eds). Troublesome Disguises. Blackwell, Oxford, 1997; 296–334.
World Health Organization. ICD-10: International Classification of Diseases: Classifications of Mental and Behavioural Disorders, 10th edn. World Health Organization, Geneva, 1992.
Ayonrinde O, Bhugra D. Culture bound syndromes. In: Bhugra D, Malhi G (eds). Troublesome Disguises, 2nd edn. Wiley-Blackwell, Oxford, 2015; 231–251.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edn, text rev. American Psychiatric Association, Washington, DC, 2000.
Bhugra D, Sumathipala A, Siribaddana S. Culture-bound syndromes: A re-evaluation. In: Bhugra D, Bhui K (eds). Textbook of Cultural Psychiatry. Cambridge University Press, Cambridge, 2007; 141–156.
Sumathipala A, Siribaddana S, Bhugra D. Culture-bound syndromes: The story of dhat syndrome. Br. J. Psychiatry 2004; 184: 200–209.
Wig NN. Problems of mental health in India. J. Clin. Soc. Psychiatry 1960; 17: 48–53.
Malhotra HK, Wig NN. A culture bound sex neurosis of the Orient. Arch. Sex. Behav. 1975; 4: 519–528.
Bhugra D, Buchanan A. Impotence in ancient Indian texts. Sex. Marital Ther. 1989; 4: 87–92.
Teo AR, Fetters MD, Stufflebam K et al. Identification of the hikikomori syndrome of social withdrawal: Psychosocial features and treatment preferences in four countries. Int. J. Soc. Psychiatry 2015; 61: 64–72.
Kato TA, Shinfuku N, Sartorius N, Kanba S. Are Japan’s hikikomori and depression in young people spreading abroad? Lancet 2011; 378: 1070.
Chen YF. Chinese classification of mental disorders (CCMD-3): Towards integration in international classification. Psychopathology 2002; 35: 171–175.
#psychiatry#medicine#maladies#culture-bound syndromes#dhat#psychological distress#global psychiatry#neurosis#culture#globalization
0 notes
Text
Joel Paris, Why Psychiatrists are Reluctant to Diagnose Borderline Personality Disorder, 4 Psychiatry (Edgmont) 35 (2007)
Abstract
Clinicians can be reluctant to make a diagnosis of borderline personality disorder (BPD). One reason is that BPD is a complex syndrome with symptoms that overlap many Axis I disorders. This paper will examine interfaces between BPD and depression, between BPD and bipolar disorder, and between BPD and psychoses. It will suggest that making a BPD diagnosis does more justice to patients than avoiding it.
What is Borderline Personality Disorder?
Borderline personality disorder (BPD) is a diagnosis with an unusual history. The idea that patients might fall on some sort of “borderline” between psychosis and neurosis dates back to 1937, at which time the syndrome was first described.1 BPD patients do have quasipsychotic or micropsychotic symptoms, such as voices telling them to kill themselves, paranoid feelings, and depersonalization.2 However these cognitive symptoms are not essential features of BPD. The core of the syndrome is a striking instability of mood, accompanied by a wide range of impulsive behaviors, particularly self-cutting and overdoses, and with intimate relationships that are impulsive, stormy, and chaotic.3
Since BPD begins early in life and can continue over many years, it is classified as a personality disorder. However, BPD differs from other categories on Axis II in that it is associated with a wide range of active symptoms.4 Moreover, BPD is one of the most common clinical problems psychiatrists see in practice. One study found that half of all patients with repetitive suicide attempts in emergency rooms meet criteria for this diagnosis.5 Due to suicidal threats and actions, BPD patients are often admitted to hospital.6 BPD cases are also common in out-patient settings,7 where the pathology is often serious enough to use a large amount of clinical resources.
Why Clinicians are Reluctant to Diagnose BPD
Structured interviews pick up many cases of BPD missed in ordinary practice.7 This finding shows that practitioners are not consistently making this diagnosis. There are a number of reasons why clinicians may be reluctant to recognize BPD.
First, Axis I diagnoses are more familiar to most professionals. Making an accurate Axis II diagnosis requires experience. Personality disorders often seem to lack precise symptomatic criteria, since many of their features describe problems in interpersonal functioning that require clinical judgment for accurate assessment.
Second, resistance to diagnosing patients with a personality disorder may be based on the idea that these conditions are untreatable,8 or at least not treatable using the pharmacological tools that have come to dominate the treatment of so many other disorders. While there is good evidence for the efficacy of psychotherapy in BPD,9 not every clinical setting has the resources to provide that form of treatment. Simpler constructs such as major depression lead to more familiar treatment options, particularly pharmacotherapy.
Third, clinicians may wish to avoid making diagnoses associated with stigma. It is an unfortunate reality that a diagnosis of BPD can indeed lead to rejection by the mental health system. If BPD were to be reclassified as, for example, a mood disorder, patients would tend to be seen as having a biological illness instead of having a problematical personality. However, stigma cannot be removed by reclassification. Patients who are chronically suicidal and who do not form strong treatment alliances will continue to be just as difficult, even under a different diagnostic label.
Comorbidity and Diagnostic Problems
Patients with BPD frequently meet criteria for multiple Axis I diagnoses.10 Considering that the disorder is associated with so many symptoms, this level of comorbidty should not be surprising. Changing the diagnosis of a patient with BPD, however, to one of these comorbid disorders focuses on only one aspect the syndrome and fails to account for BPD’s broad range of clinical phenomena (affective, impulsive, interpersonal, and cognitive).
While it is tempting to conclude that diagnoses such as major depression are the “real” problems in BPD, similar symptoms can derive from entirely different causes. Clinical phenomena, such as low mood or unstable mood, are no more specific than fever or inflammation. All that “comorbidity” says is that there are enough symptoms in one patient to meet criteria for more than one DSM category.11 Moreover, overlap is common in the DSM system—major depression has at least as much comorbidity as any Axis II disorder.12
Another source of confusion is that the description of BPD in DSM-IV-TR is not specific.4 The definition introduced in DSM-III was an advance because it operationalized diagnosis using observable criteria. As with other disorders, DSM instructs the clinician to make a diagnosis when five out of nine criteria are met. The result is that many permutations lead to the same category, producing a heterogeneous group.
It would be better to identify crucial features without which the diagnosis should not be made. One can group the current DSM criteria into affective, impulsive, interpersonal, and cognitive components. Patients should have most or all of these features to merit the diagnosis. That approach has been used in a research measure, the Diagnostic Interview for Borderlines (DIB),13 later revised as the DIB-R.14 This semistructured interview scores each of four areas of pathology on four sub-scales (0–2 for affective and cognitive symptoms and 0–3 for impulsive and interpersonal symptoms), using an overall cutoff point of eight out of 10 for positive diagnosis. Patients who meet DIB-R criteria are much more homogeneous, as shown by studies demonstrating that this instrument distinguishes them from patients with other Axis II disorders, and diagnosis achieves similar specificity if one requires six or seven criteria rather than five.15
BPD and Psychosis
The original concept of BPD as lying on a border between neurosis and psychosis found a parallel in the diagnostic term pseudoneurotic schizophrenia.16 The concept was that patients with such a wide variety of neurotic symptoms could be latently psychotic. However, this diagnosis confused personality disorders primarily affecting mood and impulsivity (like BPD) with categories that primarily affect cognition, such as schizotypal personality.17 Neither family history studies nor biological markers support a link between BPD and schizophrenia.18 Nonetheless, some cases are challenging for differential diagnosis, since the cognitive symptoms of BPD can occasionally be florid. However, these phenomena are transient and stress-related, while insight is retained, as the following case example illustrates.
Case example—Patient 1. Bill was a 25-year-old man under treatment for chronic suicidality, unstable relationships, and mood instability. He also had paranoid ideas, sometimes thinking that neighbors were plotting against him. All these thoughts, however, were exaggerations of real situations and never had the bizarre quality of delusions. Bill also heard critical voices in his head when stressed, but knew that such experiences were imaginary. Bill received a DIB-R score of 9/10.
Nonetheless, Bill was initially diagnosed with schizophrenia and treated for psychosis for over five years with injectable antipsychotic medication. Bill actually liked attending this clinic and getting the injections, since it gave him a reason to come in every two weeks and to talk with a nurse. However, as his life stabilized, Bill’s micropsychotic symptoms eventually remitted, along with his impulsive and affective symptoms. By age 30, Bill stopped taking neuroleptics and never had a relapse of paranoid ideas or hallucinations.
BPD, Depression, and Dysthymia
Depression is a common reason for clinical presentation in patients with BPD. It has been suggested that the BPD is an atypical form of unipolar depression.19 BPD is associated with chronic lowering of mood, particularly dysthymia with an early onset.20 One argument in favor of BPD as a form of major depression was based on the frequency of family history of depression in BPD patients. However, impulsive disorders, such as substance abuse and antisocial personality, are actually more common in families than mood disorders.18 Another argument was based on commonalities in biological markers, such as REM latency.19However, it has never been shown that these markers are specific to DSM categories.
There is an important phenomenological distinction between temporal patterns of depressive symptoms in depression and BPD.21 In classical depression, mood is stable over weeks and is relatively unresponsive to the environment. In contrast, mood in BPD is highly mercurial. Moreover, mood can be strikingly unstable in the course of a single day, depending on life events. Patients have a mixture of affects—not only sadness or anxiety, but also anger, brief periods of elation, and feelings of numbness. On a more practical note, depression in BPD does not respond in the same way as classical depression to antidepressant drugs, as the following case illustrates.9
Case example—Patient 2. Susan was a 24-year-old woman under treatment for chronic depression, with rapid shifts of mood, usually to anger and rageful outbursts. She also had a history of self-cutting and repetitive overdoses. Susan received a DIB-R score of 10/10.
Nonetheless, Susan was diagnosed with major depression and treated with a variety of antidepressants from several classes, none of which had any lasting effect. Each medication change led to short-term improvement for a few weeks followed by relapse to her previous state. Once Susan became engaged in psychotherapy, however, she improved to the point that antidepressants were no longer considered necessary.
BPD and the Bipolar Spectrum
It has been proposed that borderline pathology falls within the spectrum of bipolar illness,22 based on a wish to expand the narrower diagnostic construct of bipolar disorder into a much broader range of conditions termed the bipolar spectrum. In this model, the range of bipolar spectrum disorders would be extended to include bipolar III (antidepressant-induced hypomania), as well as bipolar IV (ultra-rapid-cycling bipolar disorder). The last category, bipolar IV, describes mood swings typical of BPD (i.e., rapid shifts over hours). This expanded definition might include many, if not most, patients with BPD.
The issue is whether the lability of mood seen in BPD is identical to phenomena observed in mood disorders, such as bipolar II.23 Hypomanic episodes have to last for at least four days, and this consistency of mood is rarely seen in BPD. Instead, affective instability (AI) is a characteristic feature that distinguishes BPD from classical bipolar disorder (as well as from other personality disorders). Emotion dysregulation is a similar concept.24
Other lines of evidence have also failed to support the idea that BPD and bipolar disorder reflect the same underlying psychopathology.25,26 To summarize, there is no evidence for a common etiology, family prevalence data shows that impulsive disorders are more common than mood disorders in the first-degree relatives of patients with BPD, the longitudinal course of BPD rarely shows evolution into bipolar disorder, and treatment studies have failed to show that mood stabilizers have anywhere near the same efficacy in BPD as they do in bipolar disorder.
The following case demonstrates some of the problems in differential diagnosis between BPD and bipolar disorder.
Case example—Patient 3. Lisa had been self-cutting since age 16 and presented to a clinic with chronic suicidal ideation, irritability, and rages. Lisa received a DIB-R score of 9/10.
Nonetheless, bipolar II disorder was diagnosed on the basis of Lisa’s mood swings, as well as repeated episodes in which she impulsively became involved with men—flying thousands of miles to meet them after an initial internet contact. At certain points of her illness, Lisa also showed quasipsychotic symptoms, such as an intense fantasy that she was Jesus’s sister who had been sent to earth with a mission. Yet lithium, prescribed for a full year in adequate doses, had no affect on her symptoms. Instead, all of these problems came under control within weeks once Lisa entered psychotherapy and formed a solid therapeutic alliance.
BPD and Posttraumatic Stress Disorder
The concept that BPD might be a “complex” form of posttraumatic stress disorder (PTSD) has been suggested by frequency of childhood abuse histories in these patients.27 The problem is the assumption that trauma is the primary cause of BPD, rather than one among many risk factors. Research shows that biological, psychological, and social factors are all involved in the etiology of BPD, that severe trauma histories are only found in about a third of cases, and that most people exposed to child abuse in community samples have neither BPD nor any other diagnosable psychiatric disorder.28
Case example—Patient 4. Lisa came for treatment of chronic suicidal ideation, multiple overdoses, and unstable intimate relationships. She also had transient episodes of depersonalization. Lisa’s DIB-R score was 8/10.
A previous therapist had diagnosed Lisa with PTSD, and Lisa did have serious problems resulting from having been sexually abused by her stepfather between ages of 7 and 12. It was interesting, nonetheless, to note that her older sister, who was abused in precisely the same way, never experienced psychological problems to the extent that she ever sought treatment. While the issue of child abuse played an important role in her psychotherapy, Lisa’s symptoms resolved gradually over time as she was able to find regular employment and become involved in more stable, less demanding relationships.
Positive Reasons for Diagnosing BPD
What are the advantages in making the diagnosis of BPD? The first concerns the recognition of complex forms of psychopathology with symptoms that do not occur in isolation. BPD is a construct that can account for the co-occurrence of a wide range of affective, impulsive, and cognitive symptoms in the same patient.4
The second advantage concerns prediction of outcome. BPD has a characteristic course over time, beginning in adolescence, with symptoms peaking in early adulthood, followed by gradual recovery in middle age.29 This outcome pattern provides a useful frame for therapy.
The third value of diagnosing BPD lies in predicting response to treatment. Pharmacotherapy for depression is less effective in the presence of any personality disorder, and patients with BPD respond inconsistently to antidepressants.9 The problem is that drugs are not as effective in BPD as they are in the disorders for which they were originally developed. In several of the case examples presented above, the patients were treated with pharmacotherapy based on an Axis I diagnoses, without obvious benefit. Unfortunately, such results do not always lead physicians to reconsider diagnosis and therapy—all too often, patients are tried on a variety of medications or given nonevidence-based polypharmacy.
The fourth advantage, closely related to the last point, is the strong evidence that psychotherapy can be an effective form of treatment for BPD.9 We now know that several forms of cognitive and dynamic therapy are at least as effective, if not more effective, than drugs in relieving the symptoms of BPD. If one does not make the diagnosis, patients may not be referred for these forms of psychotherapy.
The BPD diagnosis has its problems, but so do most of the disorders listed in DSM. Professionals treating patients meeting criteria for this disorder can benefit from the large empirical literature bearing on this complex clinical problem. The cases presented above are examples of how Axis I pathology can lead to mistaken expectations about course and treatment response. Finally, the the proper diagnosis of BPD can help us to inform and educate patients and their families.
References
Zanarini MC, Gunderson JG, Frankenburg, FR. Cognitive features of borderline personality disorder. Am J Psychiatry 1990;147:57–63.
Lieb K, Zanarini MC, Schmahl C, et al. Borderline personality disorder. Lancet 2004;36:453–61.
Paris J. The nature of borderline personality disorder: Multiple symptoms, multiple dimensions, but one category. J Personality Disorders In Press.
Forman EM, Berk MS, Henriques GR, et al. History of multiple suicide attempts as a behavioral marker of severe psychopathology. Am J Psychiatry 2004;161:437–43.
Hull JW, Yeomans F, Clarkin J, et al. Factors associated with multiple hospitalizations of patients with borderline personality disorder. Psychiatr Serv 1996;47:638–41.
Zimmerman M, Mattia JI. Differences between clinical and research practices in diagnosing borderline personality disorder Am J Psychiatry 1999;156:1570–4.
Lewis L, Appleby L. Personality disorder: The patients psychiatrists dislike. Br J Psychiatry 1988;153:44–9.
Paris J. Recent advances in the treatment of borderline personality disorder. Can J Psychiatry 2005;50:435–41.
Zanarini MC, Frankenburg FR, Dubo ED, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry 1998;155:1733–9.
First MB. Mutually exclusive versus co-occurring diagnostic categories: The challenge of diagnostic comorbidity. Psychopathology 2005;38:206–10.
Fava M. Diagnosis and definition of treatment-resistant depression. Biologic Psychiatry 2003;53:649–59.
1Gunderson JG, Kolb JE. Discriminating features of borderline patients. Am J Psychiatry 1978;135:792–6.
Zanarini MC, Gunderson JG, Frankenburg FR,Chauncey DL. The revised diagnostic interview for borderlines: Discriminating BPD from other Axis II disorders. J Personal Disord 1989; 3:10–8.
Zanarini MC, Gunderson JG, Frankenburg FR. Discriminating borderline personality disorder from other Axis II disorders. Am J Psychiatry 1989;147:161–7.
Hoch PH, Cattell JP, Strahl MD, Penness HH. The course and outcome of pseudoneurotic schizophrenia. Am J Psychiatry l962;ll9:l06–l5.
Spitzer RL, Endicott J, Gibbon M. Crossing the border into borderline personality disorder. Arch Gen Psychiatry 1979;36:17–24.
White CN, Gunderson JG, Zanarini MC, et al. Family studies of borderline personality disorder: A review. Harv Rev Psychiatry 2003;12:118–9.
Akiskal HS, Chen SE, Davis GC. Borderline: An adjective in search of a noun. J Clin Psychiatry 1985;46:41–8.
Pepper CM, Klein DN, Anderson RL, et al. DSM-III-R Axis II comorbidity in dysthymia and major depression. Am J Psychiatry 1995;152:239–47.
Gunderson JG, Phillips KA. A current view of the interface between borderline personality disorder and depression. Am J Psychiatry l99l;l48:967–75.
Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: Misdiagnosis, antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry 2002;47:125–34.
Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: Similarities and differences. J Psychiatr Res 2001;35:307–12.
Linehan MM. Dialectical Behavioral Therapy of Borderline Personality Disorder. New York, NY: Guilford, l993.
Paris J. Bipolar or borderline? Harv Rev Psychiatry 2004;12:140–5.
Paris J, Gunderson JG, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorder. Compreh Psychiatry In Press.
Herman J, van der Kolk B. Traumatic antecedents of borderline personality disorder. In: van der Kolk B (ed). Psychological Trauma. Washington, DC: American Psychiatric Press, Inc., 1987:111–26.
Paris J. Does childhood trauma cause personality disorders? Can J Psychiatry 1998;43:148–53.
Paris J. Personality Disorders Over Time: Precursors, Course, and Outcome. Washington, DC: American Psychiatric Press, Inc., 2003.
#borderline personality disorder#diagnosis#debate#psychiatry#psychiatric diagnoses#prejudice#politics of medicine#ethics
0 notes
Text
Antonia S. New et al., The Case for Shifting Borderline Personality Disorder to Axis I, 64 Biol Psychiatry 653 (2008)
Abstract
Through reviewing what is known about the nature, course, and heritability of borderline personality disorder (BPD), we argue for a reconceptualization of this disorder that would lead to its placement on Axis I. Borderline personality disorder is a prevalent and disabling condition, and yet the empirical research into its nature and treatment has not been commensurate with the seriousness of the illness. We not only review empirical evidence about the etiology, phenomenology, and course of the disorder in BPD but we also address fundamental misconceptions about BPD that we believe have contributed to misunderstanding and stigmatization of the disease. Finally, we suggest future directions for research that might permit the identification of core features of this disorder, with a focus on the importance of naturalistic assessments and of assessments through the course of development.
Borderline personality disorder (BPD) is a disabling condition with high morbidity and mortality, yet the empirical research into its nature and treatment has not been commensurate with the seriousness of the illness. Despite recent advances in the treatment of BPD, it remains notoriously difficult to treat effectively, with many patients responding poorly even to the most widely accepted treatment strategies (1). In addition, because the disorder has as cardinal symptoms anger and interpersonal disruptiveness, it is often difficult to form a therapeutic alliance with afflicted patients. These features draw attention away from evidence that BPD is a serious mental disorder that deserves much more investigative scrutiny than it has received. A logical consequence of taking this disorder seriously is to consider reclassifying the disorder into Axis I. This reclassification would, we believe, provide a stimulus to new research into the nature and treatment of this severe illness.
Evidence for the Validity of BPD
The validity of the BPD diagnosis remains a question in the minds of many clinicians, and some doubt its existence altogether (2). A widely accepted approach to validating the boundaries of psychiatric disorders is the set of guidelines established by Robins and Guze (1970) (3), which considers accrual of information from five lines of evidence important for establishing the validity of a mental disorder. These criteria include: 1) a careful delineation of symptoms; 2) information about the course of illness; 3) evidence of familial clustering; 4) predictable treatment response, especially to somatic treatments; and 5) biological markers (3,4). We review each of these criteria as it relates to BPD.
Core Symptoms of BPD
A Single Diagnostic Construct?
The current DSM criteria were developed from observations by experienced clinicians, and it remains a question as to whether these criteria cluster into one syndrome or into independent symptom dimensions. A factor analysis of symptoms in a large sample of BPD patients (n 141) revealed three factors: disturbed relatedness (unstable relationships, identity disturbance, and chronic emptiness), behavioral dysregulation (impulsivity and suicidality/self-mutilatory behavior), and affective dysregulation (affective instability, inappropriate anger, and efforts to avoid abandonment) (5). These factors were replicated in the CLPS (Collaborative Longitudinal Personality Disorders Study)—a prospective descriptive study of a large sample (n 668) of patients with personality disorders, including schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders and major depressive disorder (MDD) with no personality disorder (6).
Recent data, however, raise questions about the 3-factor model and instead suggest a single underlying core that leads to the diverse symptoms of BPD. Although Sanislow found that the 3-factor model yielded a better fit with their data than a single-factor model, the factors identified (disturbed relatedness, behavioral dysregulation, and affective dysregulation) were highly intercorrelated (r .90, .94, and .99, respectively), lending support to a single overarching BPD construct. A subsequent factor analysis identified three similar factors but also concluded that the factors were too highly intercorrelated to be considered separate factors (7). Providing even further evidence for BPD as a unified syndrome, a recent large study explored several 1-, 3-, and 4-factor models of DSM-IV BPD criteria and concluded that the BPD criteria describe a single construct rather than multiple co-occurring syndromes (8). Finally, a confirmatory factor analysis of DSM-III-R BPD criteria in a large clinical and non-clinical sample showed that a single factor fit the data best (9). This study also showed that “frantic efforts to avoid abandonment” was the criterion with the highest specificity and positive predictive power. Affective instability was also highly informative as to BPD diagnosis, whereas identity disturbance and feelings of emptiness were less informative. Even though factor analyses lend support to the presence of a unitary latent diagnostic construct, heterogeneity is observed in the clinical presentation of BPD. This might arise out of the fact that different aspects of the disorder might be present at different times, making the disorder appear quite heterogeneous when observed cross-sectionally. This highlights the importance of a developmental approach to characterizing the core features of BPD.
Specificity of BPD.
The high rate of comorbidity with other disorders has also led to skepticism about the validity of the BPD diagnosis. Data from CLPS showed that the Axis I comorbidities most commonly seen with BPD were posttraumatic stress disorder (PTSD) and substance abuse. Although BPD subjects showed a high rate of MDD (79% lifetime), this was not higher than the prevalence of MDD across personality disorders (66%– 82%). The most common Axis II comorbidities of BPD were antisocial and dependent personality disorders (10). Two-year follow-up found a significant association between BPD and MDD as well as PTSD (11).
The high rate of comorbid mood disorders in BPD has led some to argue that BPD is a bipolar spectrum illness. Empirical support for this view comes from a study following BPD patients, which showed a 15% rate of onset of bipolar I or II disorder over 3 years, compared with no new cases in an other personality disorder (OPD) group (2). Other studies, however, have failed to show elevated rates of bipolar diagnoses in BPD (10,12–14). Longitudinal follow-up of the CLPS sample showed modestly increased rates of bipolar I and II disorders in the BPD compared with the OPD group over 4 years (15). Although evidence suggests a moderately increased risk for bipolar disorder in BPD patients, the risk is not nearly as high as for MDD or substance abuse. Furthermore, if BPD were a bipolar spectrum disorder, one would expect BPD to run in families with bipolar disorder, and evidence suggests that this is not the case (16,17). In addition, if BPD were a bipolar spectrum disorder, then treatment with antidepressant drugs should worsen mood instability, as in bipolar disorder, whereas antidepressant drugs stabilize mood in BPD (18). Taken together, these data support some increased risk for bipolar disorder in BPD but also a heightened risk for other disorders. From a clinical vantage point, BPD is not most fruitfully viewed as a bipolar variant, because the prognosis and treatment recommendations differ substantially. However, the substantial phenotypic resemblance as well as the common comorbidity raise the possibility that BPD might be viewed as an affective spectrum illness as has been previously suggested (4); however, it seems to fit squarely in neither the unipolar nor bipolar group (Supplement 1).
Course/Prognosis
Borderline personality disorder is present in approximately 2% of the general population, making it as prevalent as schizophrenia and bipolar I disorder (19,20). Borderline personality disorder is heavily represented in clinical populations (21), and patients with BPD require extensive mental health services (22–25). The completed suicide rate in BPD approaches 10%, and at least 75% of afflicted individuals attempt suicide at least once (26). Borderline personality disorder is strongly associated with elevated risk of medical emergency room visits (24) and generalized occupational and psychosocial dysfunction (27).
Although BPD is associated with severe symptoms and functional impairment, the prognosis is not as unfavorable as had been previously assumed. Large longitudinal studies have shown that many BPD patients experience improvement and even resolution of borderline features over time, although a subset of patients experience long-term disability (28,29). Specifically, 88% of a sample of patients with BPD achieved remission over 10 years, with approximately one-third of those achieving remission in the first 2 years. Of note, remission in this sample was defined as not meeting the threshold for a full BPD diagnosis (30), but subjects might have continued to be symptomatic. Symptoms of affective instability seem to be the most consistent over time, enduring in many cases over 27 years (28,31).
Heritability and Familiality
Although limited in number, family studies of BPD show that the first-degree relatives of BPD probands are 10 times more likely to have been treated for BPD and significantly more likely to have been treated for MDD than the first-degree relatives of schizophrenia probands (32). Subsequent family studies of BPD showed that affective instability and impulsivity as well as BPD diagnosis itself were significantly more common in first-degree relatives of BPD patients than of OPD or schizophrenia patients (17,33). In addition, MDD appeared more often in the relatives of BPD than of OPD patients, regardless of whether the BPD proband had a history of MDD (17). To tease apart the transmission of BPD from that of MDD, a study examined BPD outpatients with no history of MDD and demonstrated an increased risk for depression in the first-degree relatives, suggesting a common etiologic factor linking the two disorders (34).
Family studies indirectly reflect genetic heritability; however, only twin studies provide definitive evidence for it. Limited twin study data are available for BPD. One such study examining 92 monozygotic twins and 129 dizygotic twins showed that BPD was substantially heritable, with 69% of the variance in BPD accounted for by genetic factors (35). A recent study of Chinese twins showed similar heritability rates for cluster B personality disorders of 65%; however, BPD was not independently assessed (36). In a study of twin pairs in childhood, parents assessed personality disorder features in their monozygotic and dizygotic twins and demonstrated that 76% of the variance in BPD features seems to be genetic (37). Although the number of studies showing heritability for BPD are few, all such studies undertaken show substantial heritability.
Predictability of Treatment Response
We have reviewed evidence for the validity of BPD that meets the first three criteria for diagnostic validity: a delineation of symptoms; information about the course of BPD; and evidence of familial clustering. A feature that does set BPD apart from other mental illnesses is the absence of a predictable, robust response to somatic treatments. This is problematic not only because it leaves patients without the benefit of highly effective pharmacotherapy but also because psychiatrists often use information from pharmacologic treatment response as an avenue of investigation into the neurobiology of mental illnesses. The fact that depression, for example, responds to antidepressant drugs gave rise to the monoamine hypothesis of depression. The fact that conventional antipsychotic drugs block D2 receptors gave rise to the dopamine hypothesis of schizophrenia. Evidence for the importance of cellular signaling pathways in bipolar disease came out of exploration of the mechanism of action of lithium and other mood stabilizers. The contrasting reality that BPD patients seem to respond to medications in a circumscribed and often transient manner, combined with the fact that the agents that have proven somewhat helpful come from almost all known psychotropic drug classes, has meant that a unifying theory of the biological underpinnings of BPD has not yet emerged. Much more needs to be learned about the neurobiology of BPD to permit the development of treatments specific to this disorder.
Although the modest efficacy and wide diversity of medication classes used in BPD present clinical and theoretical challenges, we believe that a feature of the disorder itself, the fluctuating symptoms of BPD, also contributes to the difficulty in defining highly effective pharmacotherapy for BPD. It might be that the widely used techniques in medication trials to assess treatment response— brief cross-sectional assessments of an individual in a clinical research office—might not be optimal to detect response in BPD. Because the symptoms of BPD fluctuate dramatically and flare up especially in the context of close relationships, cross-sectional assessments might be inadequate to detect a response to treatment with any sensitivity or specificity. 2 BIOL PSYCHIATRY 2008;xx:xxx A.S. New et al. www.sobp.org/journal ARTICLE IN PRESS To a greater degree than other psychiatric populations, BPD patients might seem asymptomatic or highly symptomatic at the particular moment, depending on an immediate antecedent interpersonal interaction or on the relationship developed with the specific staff member assessing them. A better approach would be to assess patients across multiple situations, such that both average levels of symptoms and variability in symptoms over time can be measured. Methods for ecological momentary assessment of symptoms are becoming more readily available, including event-contingent recording methods (38), in which patients report on their behavior and mood in relation to specific social interactions over time. This method allows for the documentation of the naturalistic contexts in which symptoms arise and might provide a more clinically relevant assessment of treatment response. A recent study using event-contingent recording in BPD patients proved its feasibility in this population (39).
Biological Markers
Although there are no clear neurobiological markers for BPD, the absence of such markers is a ubiquitous concern across all psychiatric diagnoses. In BPD, as in other psychiatric disorders, findings from brain imaging studies, neurochemical markers, and genetic studies do not point to a simple pathophysiology. The body of research on neurobiological abnormalities in BPD has been thoroughly reviewed elsewhere (40,41). Briefly, studies employing a variety of methods have found widely replicated decreases in serotonergic responsiveness in BPD (42– 45). These findings have informed neuroimaging research in BPD, in which a predominance of studies have employed pharmacologic probes of serotonin (46 –50) or positron emission tomography ligands targeting serotonin receptors (51,52). A limitation of these findings is that abnormalities have tended to relate less to the overarching diagnosis than to symptoms dimensions (53). Another limitation is that the scope of neurochemical systems studied is narrow, focusing almost exclusively on serotonin. An extremely limited number of studies have explored other neurotransmitter systems in BPD, including dopamine (54) and acetylcholine (55).
Brain imaging studies have provided evidence for disruption of the neural circuitry in BPD (reviewed elsewhere [56]). However, two relatively consistent findings from brain imaging studies emerge: 1) BPD patients seem to have decreased volume in anterior cingulate gyrus (ACG), especially of gray matter, compared with healthy control subjects (57–59); 2) positron emission tomography studies have shown that orbital frontal cortex (OFC) and ACG are less active in BPD than control subjects (46 – 49,60). Functional magnetic resonance imaging (fMRI) studies have shown this less consistently (61– 63), although the orbital floor is evaluated less effectively with fMRI, because of susceptibility artifact. Thus, brain regions, such as OFC and ACG, that normally put the brakes on expressions of emotions, might fail to come “on line” in BPD when needed. Although brain imaging findings in BPD are suggestive, it is important to note that many of the circuits implicated in BPD are the same as those implicated in MDD and bipolar disorder (64,65). For example, decreased subgenual ACG has been shown in depression (66 – 68) and in some studies of bipolar disorder (69,70). In addition, functional imaging studies have shown decreased activation in areas of prefrontal cortex in MDD (71), bipolar disorder (72), and PTSD (73). Clearly, new approaches in brain imaging will be needed to develop specific neural circuitry models for each of these disorders.
To move forward in understanding BPD specifically, it will be necessary to target those symptoms that are specific to BPD. Although affective dysregulation is a core feature of BPD (27,53,74) and might be the most prevalent and enduring symptom (75), it is also seen in bipolar disorder and to some degree in MDD. Too little attention has been paid to the interpersonal disruptions that are central to BPD. A recent review has argued that the relational style characteristic of BPD is “intense and unstable, marked . . . by abandonment fears and by vacillating between idealization and devaluation (and that this style offers) the best discriminators for the diagnosis” of BPD (76). Evidence for this view stems from consistent observation of profound interpersonal impairment in BPD (9,27,77), with more impairment in interpersonal functioning in BPD than in MDD, obsessive-compulsive disorder or OPDs (78). Furthermore, suicide attempts in BPD are more often associated with interpersonal stressors than suicide attempts in MDD (79).
Notwithstanding the centrality of interpersonal disruptions in BPD, very little empirical work has been done on what underlies these symptoms. One domain that has received some empirical scrutiny is the recognition of facial emotional expression. Borderline personality disorder patients correctly identify emotional expressions even more sensitively than healthy control subjects; however, they tend to over-read anger in neutral faces (80 – 83). More research into emotional information processing in BPD would be very helpful, because these skills are essential for navigating interpersonal relationships. If BPD patients over-read and misread emotional cues, this might help to explain the puzzling symptom of exaggerated emotional responses in interpersonal interactions. If indeed BPD patients over-read emotional responses and this deficit is present from early childhood, this might play a role not only in the disrupted interpersonal relationships but also, possibly, in the development of emotion dysregulation. Infants and children learn how to modulate emotions through relationships with caregivers (84), and individuals who continuously misread emotional cues are robbed of this basic mechanism of learning how to modulate emotion. New research into this aspect of BPD will be enhanced by rapid developments in the neuroscience of social interaction.
Implications of Shifting BPD to Axis I
The distinction between Axis I and Axis II disorders in the DSM system has received little empirical investigation, and the lack of empirical grounding for many assumptions that underlie the distinction has been well-argued by Siever and Davis (85). Some of the most compelling of these arguments include the fact that the current DSM-IV–TR definition of a personality disorder as “an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time and leads to distress or impairment” could well apply to many Axis I disorders also. For example, schizophrenia confers pervasive and enduring patterns of behavior that are inflexible, typically with onset in adolescence that become chronic in nature. However, we do not view schizophrenia as a disorder of “character.” Clearly, if schizophrenia fits the DSM definition of a personality disorder, the definition is overly inclusive. Simply stating that a character disorder is not better accounted for by an Axis I disorder begs the question of how to set personality disorders apart from Axis I disorders. Major depressive disorder is perhaps the prototype of an episodic disorder, yet even MDD can be associated with chronic mood symptoms that interfere with functioning.
Another feature used to distinguish personality disorders from other psychiatric illnesses is that personality disorders have traditionally been conceptualized as resulting from environmental factors, whereas Axis I disorders have been viewed as having a “biological” or “organic” basis (85). As reviewed in the preceding text, however, twin studies suggest that BPD is quite heritable. Although environmental stresses might play a role in the development of BPD, this is the case with many Axis I disorders as well, including MDD, in which environmental stresses in conjunction with vulnerability genes can give rise to the disorder (86). Thus neither the presentation nor the etiology of BPD differentiates it clearly from disorders classified on Axis I.
Not only is the distinction between Axis I and Axis II disorders problematic but BPD in particular does not fit in with traditional conceptualizations of personality disorders. For example, personality disorders have been viewed as egosyntonic, whereas the symptoms of BPD are often quite egodystonic, leading patients to seek treatment for their symptoms (87).
The current revision of DSM recognizes the difficulty in distinguishing Axis I from Axis II and is considering the possibility of abolishing Axis II or the reclassification of some Axis II disorders to Axis I (L.J. Siever, personal communication, September 2007). The present review does not take on that debate but instead argues that in light of what is known about BPD, this disorder specifically reaches the threshold for reclassification.
Misconceptions about BPD
So where do doubts about the validity of BPD as a major mental disorder come from? Although some of the difficulty in taking BPD seriously might relate to the complexity and heterogeneity of the symptoms, the high level of comorbidity, and poor medication response, these features are not unique to BPD. We believe that the evidence for the Robins and Guze criteria strongly argue for the consideration of BPD as a serious mental illness, and as such, BPD ought to be classified on Axis I.
We believe two fundamental misconceptions have contributed to misunderstanding and have been impediments to serious investigative scrutiny of this illness. The first relates to the name “borderline personality disorder” itself, which implies that this disease lies on the “border” between two states, a view that has its origins in early psychoanalytic conceptualizations of the disorder that are no longer widely accepted. A second misconception is that BPD is the direct consequence of early life trauma rather than a phenotypic expression of a vulnerability to symptoms and behaviors that then emerge in the context of past and present-day stressful life events.
The misconception that BPD is the result exclusively of environmental influences and not also influenced by heredity is not well-grounded empirically. The view that the cause of BPD is childhood trauma has held so fast that some therapists have used “recovered memory therapies” in the treatment of BPD, encouraging patients to file lawsuits even with little evidence of childhood trauma and no spontaneous memory of trauma (88). The field has moved strongly to condemn this approach.
The finding of heritability brings into serious question the view that trauma is the sole etiology of BPD. It suggests, alternatively, the possibility of an innate hypersensitivity to stress. A traumatic etiology for BPD is also brought into question by the consideration that, because most childhood trauma is perpetrated by family members (89) and this disorder is heritable, the family members perpetrating abuse are more likely than the average population to have BPD themselves. If the caregivers of BPD patients have BPD, they are more likely to have poor frustration tolerance, excessive anger and aggression, and therefore to be at risk for engaging in abuse towards their children. A further source of doubt about the traumatic etiology of BPD is that much of the research done to assess childhood trauma is based on data obtained retrospectively from adults with BPD, which is subject to the “negative halo” recall bias inevitable with already-ill probands (90). This bias might be especially pronounced in BPD patients who, as a group, are highly prone to cast a negative emotional tone over memories of prior experiences (91).
Although skepticism about the traumatic etiology of BPD is warranted, studies have shown that adults with BPD are more likely than those without BPD to give histories of early physical and sexual abuse and of witnessing domestic violence (92). Data from CLPS suggest that BPD is more strongly correlated with childhood abuse and neglect than are MDD or OPDs (93). In a community sample, childhood physical and sexual abuse were not predictors for BPD (94). However, a recent study suggests that childhood physical and sexual abuse are among a number of independent predictors of BPD (95), and a meta-analysis of 21 studies, with over 2000 subjects, looking at BPD and child abuse yielded a pooled effect size of only r .28 (96).
Although childhood sexual abuse specifically has been implicated in BPD, it is not an inevitable prerequisite for the illness’s development (97). An estimated 20%– 45% of BPD patients have no history of sexual abuse (97), whereas 80% of individuals with sexual abuse histories have no personality pathology (98).

Table 1. BPD and Trauma: Studies Supporting and Undercutting a Traumatic Etiology for BPD

Table 2. BPD and Genetic Factors: Studies Supporting a Familial/Heritable Role for BPD
Longitudinal studies of children followed after a report of child abuse show that a substantial proportion with quite severe abuse remains functionally resilient, with little impairment across social, occupational, and interpersonal domains (99). Unfortunately, longitudinal studies of children with childhood trauma to date have not assessed for BPD (89,99).
Taken together, these results support a model of the etiology of BPD as multifactorial, with childhood abuse as a contributing factor (95) but in which other factors such as family psychiatric history also play an important role (Tables 1 and 2). To clarify more fully the role of childhood trauma in the development of BPD, it will be necessary to follow prospectively children at risk for BPD.
Summary
We have suggested BPD’s inclusion among the mood disorders because of the centrality of affective dysregulation symptoms in BPD as well as the comorbidity and co-familiality with MDD. Viewing BPD in this context opens up new avenues for research. One fruitful path in BPD research might be to build upon new findings in depression research (64). This logically would include continued exploration of the circuits implicated in both mood disorder and BPD and to search for diagnostic specificity in these circuits. We have suggested that a fruitful area to pursue will be exploring deficits in social cognition, with particular emphasis on the developmental trajectories of affective symptoms and interpersonal dysfunction in BPD. It is clear, however, that a deeper understanding of the neurobiology of BPD has the potential to open avenues for novel treatments as well as to diminish the stigma that serves to worsen the clinical course and outcome of this already disabling and hard-to-treat illness.
References
Paris J (2005): Recent advances in the treatment of borderline personality disorder. Can J Psychiatry 50:435– 441.
Akiskal HS, Chen SE, Davis GC, Puzantian VR, Kahgarian M, Bolinger JM (1985): Borderline: An adjective in search of a noun. J Clin Psychiatry 46:41– 48.
Robins E, Guze SB (1970): Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. Am J Psychiatry 126: 983–987.
Schulz SC, Goldberg SC (1984): Is borderline personality disorder an illness? Psychopharmacol Bull 20:554 –560.
Sanislow CA, Grilo CM, McGlashan TH (2000): Factor analysis of the DSM-III-R borderline personality disorder criteria in psychiatric inpatients. Am J Psychiatry 157:1629 –1633.
Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, et al. (2002): Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: Findings from the collaborative longitudinal personality disorders study. Am J Psychiatry 159:284 –290.
Johansen M, Karterud S, Pedersen G, Gude T, Falkum E (2004): An investigation of the prototype validity of the borderline DSM-IV con- struct. Acta Psychiatr Scand 109:289 –298.
Fossati A, Maffei C, Bagnato M, Donati D, Namia C, Novella L (1999): Latent structure analysis of DSM-IV borderline personality disorder criteria. Compr Psychiatry 40:72–79.
Clifton A, Pilkonis PA (2007): Evidence for a single latent class of Diagnostic and Statistical Manual of Mental Disorders borderline personality pathology. Compr Psychiatry 48:70 –78.
McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, et al. (2000): The Collaborative Longitudinal Personality Disorders Study: Baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr Scand 102:256 –264.
Shea MT, Stout RL,Yen S, Pagano ME, Skodol AE, Morey LC, etal.(2004): Associations in the course of personality disorders and Axis I disorders over time. J Abnorm Psychol 113:499 –508.
Fyer MR, Frances AJ, Sullivan T, Hurt SW, Clarkin J (1988):Comorbidity of borderline personality disorder. Arch Gen Psychiatry 45:348 –352.
Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR (2004): Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry 161: 2108 –114.
Links PS, Heslegrave RJ, Mitton JE, Van Reekum R, Patrick J (1995): Borderline psychopathology and recurrences of clinical disorders. J Nerv Ment Dis 183:582–586.
Gunderson JG, Weinberg I, Daversa MT, Kueppenbender KD, Zanarini MC, Shea MT, et al. (2006): Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry 163:1173–1178.
Kelsoe JR (2003): Arguments for the genetic basis of the bipolar spectrum. J Affect Disord 73:183–197.
Silverman JM, Pinkham L, Horvath TB, Coccaro EF, Klar H, Schear S, et al. (1991): Affective and impulsive personality disorder traits in the relatives of patients with borderline personality disorder. Am J Psychiatry 148:1378 –1385.
Coccaro EF, Kavoussi RJ (1997): Fluoxetine and impulsive aggressive behavior in personality disordered subjects. Arch Gen Psychiatry 54: 1081–1088.
Coid J, Yang M, Tyrer P, Roberts A, Ullrich S (2006): Prevalence and correlates of personality disorder in Great Britain. Br J Psychiatry 188: 423– 431.
Lenzenweger MF, Lane MC, Loranger AW, Kessler RC (2007): DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry 62:553–564.
Zimmerman M, Rothschild L, Chelminski I (2005): The prevalence of DSM-IV personality disorders in psychiatric outpatients. Am J Psychiatry 162:1911–1918.
Comtois KA, Russo J, Snowden M, Srebnik D, Ries R, Roy-Byrne P (2003): Factors associated with high use of public mental health services by persons with borderline personality disorder. Psychiatr Serv 54: 1149 –1154.
Bender D, Dolan R, Skodol A, Sanislow CA, Dyck IR, McGlashan TH, et al. (2001): Treatment utilization by patients with personality disorders. Am J Psychiatry 158:295–302.
Frankenburg FR, Zanarini MC (2004): The association between borderline personality disorder and chronic medical illnesses, poor health-related lifestyle choices, and costly forms of health care utilization. J Clin Psychiatry 65:1660 –1665.
Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M (2004): Borderline personality disorder. Lancet 364:453– 461.
Black DW, Blum N, Pfohl B, Hale N (2004): Suicidal behavior in borderline personality disorder: Prevalence, risk factors, prediction, and prevention. J Personal Disord 18:226 –239.
SkodolAE,GundersonJ,McGlashanT,DyckIR,StoutRL,BenderDS,et al. (2002): Functional impairment in patients with schizotypal, border- line, avoidant, and obsessive compulsive personality disorders. Am J Psychiatry 159:276 –283.
Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR (2005): The McLean Study of Adult Development (MSAD): Overview and implica- tions of the first six years of prospective follow-up. J Personal Disord 19:505–523.
Paris J, Zweig-Frank H (2001): A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry 42:482– 487.
Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR (2006): Prediction of the 10-year course of borderline personality disorder. Am J Psychiatry 163:827– 832.
Paris J (2003): Personality Disorder Over Time: Precursors, Course and Outcome. Washington DC: American Psychiatric Press.
Loranger AW, Oldham JM, Tulis EH (1982): Familial transmission of DSM-III borderline personality disorder. Arch Gen Psychiatry 39:795– 799.
Zanarini MC, Frankenburg FR, Yong L, Raviola G, Bradford Reich D, Hennen J, et al. (2004): Borderline psychopathology in the first-degree relatives of borderline and axis II comparison probands. J Personal Disord 18:439 – 447.
Riso LP, Klein DN, Anderson RL, Ouimette PC (2000): A family study of outpatients with borderline personality disorder and no history of mood disorder. J Personal Disord 14:208 –217.
Torgersen S (2000): Genetics of patients with borderline personality disorder. Psychiatr Clin North Am 23:1–9.
Ji WY, HuYH, Huang YQ, Cao WH, Lv J, Qin Y, et al.(2006): (A twin study of personality disorder heritability.) [Article in Chinese] Zhonghua Liu Xing Bing Xue Za Zhi 27:137–141.
Coolidge FL, Thede LL, Jang KL (2001): Heritability of personality disorders in childhood: A preliminary investigation. J Personal Disord 15:33– 40.
Moskowitz DS, Pinard G, Zuroff DC, Annable L, Young SN (2001): The effect of tryptophan on social interaction in everyday life: A placebo-controlled study. Neuropsychopharmacology 25:277–289.
Russell JJ,Moskowitz DS, Zuroff DC, Sookman D, Paris J (2007): Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. J Abnorm Psychol 116:578 –588.
Bohus M, Schmahl C, Lieb K (2004): New developments in the neurobiology of borderline personality disorder. Curr Psychiatry Rep 6:43–50.
New AS, Goodman M, Treibwasser J, Siever LJ (2008): Recent advances in the biological study of personality disorders. Psych Clin North Am 31.
CoccaroEF,SieverLJ,KlarHM,MaurerG,CochraneK,CooperTB,etal. (1989): Serotonergic studies in patients with affective and personality disorders. Correlates with suicidal and impulsive aggressive behavior. Arch Gen Psychiatry 46:587–599.
O’Keane V, Maloney E, O’Neil H, O’Connor A, Smith C, Dinan TG (1992): Blunted prolactin response to d-fenfluramine in sociopathy: Evidence for subsensitivity of central serotonergic function. Br J Psychiatry 160: 643– 646.
Siever L, Trestman RL (1993): The serotonin system and aggressive personality disorder. Int Clin Psychopharmacology 8:33–39.
Dougherty DM, Bjork JM, Huckabee H, Moeller F, Swann A (1999): Laboratory measures of aggression and impulsivity in women with borderline personality disorder. Psychiatry Res 85:315–326.
Siever LJ, Buchsbaum MS, New AS, Spiegel-Cohen J, Wei T, Hazlett EA, et al. (1999): d,l-fenfluramine response in impulsive personality disorder assessed with [18F]fluorodeoxyglucose positron emission tomography. Neuropsychopharmacology 20:413– 423.
New A, Hazlett E, Buchsbaum MS, Goodman M, Reynolds D, Mitropoulou V, et al. (2002): Blunted prefrontal cortical 18fluorodeoxyglucose positron emission tomography response to meta-chloropiperazine in impulsive aggression. Arch Gen Psychiatry 59:621– 629.
Soloff PH, Meltzer CC, Greer PJ, Constantine D, Kelly TM (2000): A fenfluramine-activated FDG-PET study of borderline personality disorder. Biol Psychiatry 47:540 –547.
Leyton M,Okazawa H,Diksic M, Paris J, Rosa P, Mzengeza S, et al.(2001): Brain Regional alpha-[11C]methyl-L-tryptophan trapping in impulsive subjects with borderline personality disorder. Am J Psychiatry 158:775– 782.
New AS, Buchsbaum MS, Hazlett EA, Goodman M, Koenigsberg HW, Lo J, et al. (2004): Fluoxetine increases relative metabolic rate in prefrontal cortex in impulsive aggression. Psychopharmacology (Berl) 176:451– 458.
Frankle WG, Lombardo I, New AS, Goodman M, Talbot PS, Huang Y,et al. (2005): Brain serotonin transporter distribution in subjects with impulsive aggressivity: A positron emission study with [11C]McN 5652. Am J Psychiatry 162:915–923.
Soloff PH, Price JC, Meltzer CC, Fabio A, Frank GK, Kaye WH (2007): 5HT2A receptor binding is increased in borderline personality disorder. Biol Psychiatry 62:580 –587.
Siever L, Torgersen S, Gunderson J, Livesley W, Kendler K (2002): The borderline diagnosis III: Identifying endophenotypes for genetic studies. Biol Psychiatry 51:964 –968.
Friedel RO (2004): Dopamine dysfunction in borderline personality disorder: A hypothesis. Neuropsychopharmacology 29:1029 –1039.
Gurvitz IG, Koenigsberg HW, Siever LJ (2000): Neurotransmitter dysfunction in patients with borderline personality disorder. Psychiatr Clin North Am 23:27– 40.
Schmahl C, Bremner JD(2006): Neuroimaging in borderline personality disorder. J Psychiatr Res 40:419 – 427.
Tebartzvan E, Hesslinger B, Thiel T, et al.(2003):Frontolimbic brain abnormalities in patients with borderline personality disorder: A volumetric magnetic resonance imaging study. Biol Psychiatry 54:163–171.
Hazlett EA, New AS, Newmark R, Haznedar MM, Lo JN, Speiser LJ, et al. (2005): Reduced anterior and posterior cingulate gray matter in borderline personality disorder. Biol Psychiatry 58:614 – 623.
Minzenberg MJ,Fan J, New AS, Tang CY, Siever LJ.(2008): Frontolimbic structural changes in borderline personality disorder. J Psychiatr Res 42:727–733.
Goyer PF, Andreason PJ, Semple WE, Clayton AH, King AC, Compton-Toth BA, et al. (1994): Positron-emission tomography and personality disorders. Neuropsychopharmacology 10:21–28.
Schmahl C, Bohus M, Esposito F, Treede RD, DiSalle F, Greffrath W, et al. (2006): Neural correlates of antinociception in borderline personality disorder. Arch Gen Psychiatry 63:659 – 667.
Minzenberg MJ, Fan J, New AS, Tang CY, Siever LJ (2007): Fronto-limbic dysfunction in response to facial emotion in borderline personality disorder: An event-related fMRI study. Psychiatry Res 155:231–243.
Schnell K, Dietrich T, Schnitker R, Daumann J, Herpertz SC (2007): Processing of autobiographical memory retrieval cues in borderline personality disorder. J Affect Disord 97:253–259.
Ressler KJ, Mayberg HS (2007): Targeting abnormal neural circuits in mood and anxiety disorders: From the laboratory to the clinic. Nat Neurosci 10:1116 –1124.
Blumberg HP, Charney DS, Krystal JH (2002): Frontotemporal neural systems in bipolar disorder. Semin Clin Neuropsychiatry 7:243–254.
Caetano SC, Kaur S, Brambilla P, Nicoletti M, Hatch JP, Sassi RB, et al. (2006): Smaller cingulate volumes in unipolar depressed patients. Biol Psychiatry 59:702–706.
Coryell W, Nopoulos P, Drevets W, Wilson T, Andreasen NC (2005): Subgenual prefrontal cortex volumes in major depressive disorder and schizophrenia: Diagnostic specificity and prognostic implications. Am J Psychiatry 162:1706 –1712.
Ballmaier M, Toga AW, Blanton RE, Sowell ER, Lavretsky H, Peterson J, et al. (2004): Anterior cingulate, gyrus rectus, and orbitofrontal abnormalities in elderly depressed patients: An MRI-based parcellation of the prefrontal cortex. Am J Psychiatry 161:99 –108.
Hajek T, Carrey N, Alda M (2005): Neuroanatomical abnormalities as risk factors for bipolar disorder. Bipolar Disord 7:393– 403.
Sassi RB, Brambilla P, Hatch JP, Nicoletti MA, Mallinger AG, Frank E, et al. (2004): Reduced left anterior cingulate volumes in untreated bipolar patients. Biol Psychiatry 56:467– 475.
Davidson RJ, Irwin W, Anderle MJ, Kalin NH (2003): The neural substrates of affective processing in depressed patients treated with venlafaxine. Am J Psychiatry 160:64 –75.
Blumberg HP, Leung HC, Skudlarski P, Lacadie CM, Fredericks CA, Har- ris BC, et al. (2003): A functional magnetic resonance imaging study of bipolar disorder: State- and trait-related dysfunction in ventral pre-frontal cortices. Arch Gen Psychiatry 60:601– 609.
Shin LM, McNally RJ, Kosslyn SM, Thompson WL, Rauch SL, Alpert NM, et al. (1999): Regional cerebral blood flow during script-driven imagery in childhood sexual abuse-related PTSD: A PET investigation. Am J Psychiatry 156:575–584.
Gunderson JG, Phillips KA (1991): A current view of the interface between borderline personality disorder and depression. Am J Psychiatry 148:967–975.
McGlashan TH, Grilo CM, Sanislow CA, Ralevski E, Morey LC, Gunderson JG, et al. (2005): Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: Toward a hybrid model of axis II disorders. Am J Psychiatry 162:883839.
Gunderson JG (2007): Disturbed relationships as a phenotype for borderline personality disorder. Am J Psychiatry 164:1637–1640.
Hill J, Pilkonis P, Morse J, Feske U, Reynolds S, Hope H, et al. (2008): Social domain dysfunction and disorganization in borderline personality disorder. Psychol Med 38:135–146.
Jovev M, Jackson HJ (2006): The relationship of borderline personality disorder, life events and functioning in an Australian psychiatric sample. J Personal Disord 20:205–217.
Brodsky BS, Groves SA, Oquendo MA, Mann JJ, Stanley B (2006): Interpersonal precipitants and suicide attempts in borderline personality disorder. Suicide Life Threat Behav 36:313–322.
Wagner AW, Linehan MM (1999): Facial expression recognition ability among women with borderline personality disorder: Implications for emotion regulation? J Personal Disord 13:329 –344.
Blair RJ, Colledge E, Murray L, Mitchell DG (2001): A selective impairment in the processing of sad and fearful expressions in children with psychopathic tendencies. J Abnorm Child Psychol 29:491– 498.
Lynch TR, Rosenthal MZ, Kosson DS, Cheavens JS, Lejuez CW, Blair RJ (2006): Heightened sensitivity to facial expressions of emotion in borderline personality disorder. Emotion 6:647– 655.
Donegan NH, Sanislow CA, Blumberg HP, Fulbright RK, Lacadie C, Skudlarski P, et al. (2003): Amygdala hyperreactivity in borderline personality disorder: Implications for emotional dysregulation. Biol Psychiatry 54:1284 –1293.
Moriceau S, Sullivan RM (2005): Neurobiology of infant attachment. Dev Psychobiol 47:230 –242.
Siever LJ, Davis K (1991): A psychobiological perspective on the personality disorders. Am J Psychiatry 148:1647–1658.
Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. (2003): Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 301:386 –389.
Paris J (2007): The nature of borderline personality disorder: Multiple dimensions, multiple symptoms, but one category. J Personal Disord 21:457– 473.
Paris J (1995): Memories of abuse in borderline patients: True or false? Harv Rev Psychiatry 3:10 –17.
Silverman AB, Reinherz HZ, Giaconia RM (1996): The long-term sequelae of child and adolescent abuse: A longitudinal community study. Child Abuse Negl 20:709 –723.
Paris J (2000): Childhood precursors of borderline personality disorder. Psychiatr Clin North Am 23:77– 88, vii.
Bailey JM, Shriver A (1999): Does childhood sexual abuse cause borderline personality disorder? J Sex Marital Ther 25:45–57.
Herman JL, Perry JC, van der Kolk BA (1989): Childhood trauma in borderline personality disorder. Am J Psychiatry 146:490 – 495.
Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, et al. (2004): Childhood maltreatment associated with adult personality disorders: Findings from the Collaborative Longitudinal Personality Disorders Study. J Personal Disord 18:193–211.
Bierer LM, Yehuda R, Schmeidler J, Mitropoulou V, New AS, Silverman JM, Siever LJ (2003): Abuse and neglect in childhood: Relationship to personality disorder diagnoses. CNS Spectr 8:737–754.
Bandelow B, Krause J, Wedekind D, Broocks A, Hajak G, Ruther E (2005): Early traumatic life events, parental attitudes, family history, and birth risk factors in patients with borderline personality disorder and healthy controls. Psychiatry Res 134:169 –179.
Fossati A, Madeddu F, Maffei C (1999): Borderline personality disorder and childhood sexual abuse: A meta-analytic study. J Personal Disord 13:268 –280.
Goodman M, Yehuda R (2002): The relationship between psychological trauma and borderline personality disorder. Psychiatric Annals 32: 337–346.
Paris J (1998): Does childhood trauma cause personality disorders in adults? Can J Psychiatry 43:148 –153.
McGloin JM, Widom CS (2001): Resilience among abused and neglected children grown up. Dev Psychopathol 13:1021–1038.
Zanarini MC, Frankenburg FR (1997): Pathways to the development of borderline personality disorder. J Personal Disord 11:93–104.
#mental health#personality dysfunction#borderline personality disorder#axis I#axis II#nosology#specificity#validity
0 notes
Text
Talar R. Moukhtarian et al., Emotion dysregulation in attention-deficit/ hyperactivity disorder and borderline personality disorder, 5 Borderline Personality Disorder and Emotion Dysregulation (2018)
Abstract
There is ongoing debate on the overlap between Attention-Deficit/Hyperactivity Disorder (ADHD) and Borderline Personality Disorder (BPD), particularly regarding emotion dysregulation (ED). In this paper, we present a narrative review of the available evidence on the association of these two disorders from several standpoints. First, we discuss the unique and shared diagnostic criteria for ADHD and BPD, focusing particularly on ED. We consider the methodology of ecological momentary assessment and discuss why this approach could be an alternative and more accurate way to qualitatively distinguish between ADHD and BPD. We summarise key findings on the genetic and environmental risk factors for ADHD and BPD and the extent to which there are shared or unique aetiological and neurobiological risk factors. Finally, we discuss the clinical relevance of considering both disorders in the assessment of patients presenting with trait-like behavioural syndromes, distinguishing the two conditions and implications for treatment.
Background
In recent years, a debate has ensued over the nosological distinction between Attention-Deficit/Hyperactivity Disorder (ADHD) and Borderline Personality Disorder (BPD) [1]. Impulsivity, irritability and other symptoms of emotional dysregulation are characteristically seen in both disorders, and the nature of the relationship between ADHD and BPD requires clarification [2]. Key questions that arise include the extent to which: 1) ADHD and BPD co-occur; 2) they reflect distinct disorders or alternative expressions of the same underlying disorder; 3) they share common genetic or environmental risk factors; and 4) one of the disorders give a synergistic effect, reinforcing the other or complicating both [3, 4].
In this review paper, we present a narrative description of the available evidence on the association between ADHD and BPD pertaining specifically to emotional dysregulation (ED). We start by presenting an account of the main diagnostic features of each disorder and outlining the clinical features that are common to BPD and ADHD, then summarising studies that have reported on comorbidity between the two disorders. We then review findings from studies that have measured ED in ADHD and BPD using experience sampling methods, as this provides a precise and ecologically valid way of assessing the phenomenon of ED. Finally, we discuss the extent to which there are shared genetic and environmental risks, and shared neurobiology, for the two disorders, before considering implications of these findings for treatment.
Attention-deficit/hyperactivity disorder
ADHD is a common neurodevelopmental disorder emerging in childhood or early adolescence, characterised by a pervasive pattern of developmentally inappropriate levels of inattention and/or hyperactivity-impulsivity that lead to clinically significant functional and psychosocial impairments [5]. The disorder affects around 5% of children [6]. Longitudinal follow-up studies of children with ADHD show that symptoms of ADHD commonly persist into adulthood, with around two-thirds of cases meeting either full or sub-threshold criteria in adulthood [7]. The prevalence of adult ADHD in epidemiological surveys is estimated at around 2.5–4% [8, 9, 10]. Although ADHD is recognised as a predominantly male disorder in childhood (clinic-referred children are more likely to be male), in adult samples the gender difference is less pronounced [11].
Apart from the main symptoms used to classify ADHD, ED is considered to be an associated feature supporting the diagnosis of ADHD [5, 12]. In ADHD, ED is characterised by problems with temper control (feelings of irritability and frequent outburst of short duration) [13], emotional over-reactivity (diminished ability to handle typical life stresses, resulting in frequent feelings of being hassled and overwhelmed) [13], and mood lability (short and unpredictable shifts from normal mood to depression or mild excitement) [13].
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM–5), the diagnosis of ADHD requires six out of nine ADHD symptoms of either inattention or hyperactivity/impulsivity in childhood, and five out of nine in adults (Table 1). Additional criteria include childhood age of onset defined as several ADHD symptoms present before the age of 12 years, pervasiveness defined as symptoms present in two or more settings, and impairment defined as- interference with or reduced quality of social, academic or occupational functioning [14].
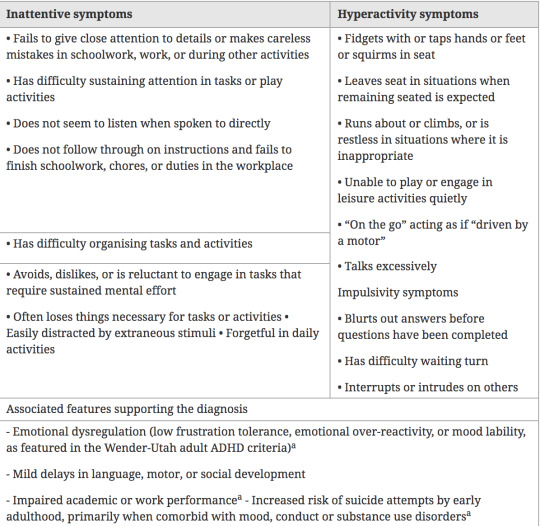
Table 1. DSM-5 symptom criteria for attention deficit hyperactivity disorder [5]
The symptom profile and severity of ADHD varies greatly between individuals, with both inattention and hyperactivity/impulsivity associated with functional impairment in multiple domains [2, 15]. ED has also been found to be an independent predictor of impairment in ADHD, after controlling for the confounding effects of core ADHD symptoms (inattention and hyperactivity/impulsivity) on impairment [16, 17, 18]. Furthermore, this has been found in cases of ADHD with no co-existing mental health disorders, and therefore cannot be explained by co-occurring conditions [16]. Impairments can be severe, impacting on education, occupation, social and interpersonal relationships [2, 15]. Adults with ADHD are more likely to have lower educational attainment, poorer work performance and an increased likelihood of dismissal from work [19, 20, 21], as well as difficulties in maintaining long-term social relationships and higher divorce rates [22], serious transport accidents [23] and criminality [24].
ADHD seldom exists in isolation and up to 90% of adults with ADHD are reported to have one or more co-occurring mental health disorders [25]. Of these disorders, the most prevalent include mood, anxiety and substance use disorders [3, 26], and personality disorders including BPD [27, 28]. This exceptionally high co-morbidity rate could however reflect, at least in part, an artefact of overlapping symptoms shared by mental health disorders [12].
Borderline personality disorder
BPD is a complex and severe mental health disorder, with typical symptom onset during adolescence and presence of behavioural precursors in childhood, persisting into adulthood [5]. BPD is characterised by a pervasive pattern of unstable interpersonal relationships, pronounced impulsive and self-damaging behaviour, unstable identity, and difficulties with ED [5], which substantially impact in an enduring way on quality of life and psychosocial functioning [29]. The DSM-5 diagnosis of BPD requires the pervasive presence of a minimum of five out of nine symptoms (Table 2) [5].

Table 2. DSM-5 symptom criteria for borderline personality disorder [5]
In the general population, BPD has a prevalence of around 6% [30] and within populations of adult psychiatric inpatients, prevalence is around 20% [5]. Most epidemiological surveys report no gender differences of BPD, yet studies of clinical populations typically report higher prevalence figures in women than in men. The different sex ratios in clinical and population samples may be explained by both assessment and sampling biases [30].
Like ADHD, individuals with BPD commonly present with comorbid mental health disorders. In particular, around 90% of BPD cases are reported to have co-occurring mood disorders including depression and dysthymia [31], along with a high prevalence of substance use disorders in the range of 15% to 57% [32].
Overlap in ADHD and BPD
Studies of the co-morbidity between ADHD and BPD
Psychiatric comorbidity is commonly found across all mental health disorders [33] and is defined as the presence of two or more disorders in the same individual at a given time. In principle, each of the disorders should make a unique contribution to the clinical presentation of the individual [34]. However, estimates of comorbidity prevalence may be inflated if there is marked overlap in the symptom criteria of two disorders, leading to poor diagnostic delineation i.e. artefactual co-morbidity [35]. Furthermore, it remains unclear to what extent psychiatric diagnoses reflect entirely distinct disorders, rather than overlapping syndromes [34]. This is a particular problem for psychiatry since there are, as yet, no validated biomarkers or other objective markers with sufficient sensitivity or specificity to be used in clinical practice to distinguish aetiologically distinct mental health conditions. Regarding ADHD and BPD, while the specific symptoms used to classify the two disorders are different, many clinical characteristics are shared, including ED, impulsive risk-taking behaviour, and unstable interpersonal relationships.
A high prevalence of co-occurring ADHD and BPD is consistently reported in the literature. In a large in- and outpatient cohort of 372 adults with ADHD referred for ADHD assessment and treatment at a tertiary referral centre, 27.2% also met criteria for BPD assessed by the structured clinical Interview for DSM-IV II (SCID II) [36]. Similarly, in another sample of 335 adults referred by family physicians, community health clinics or self-referred, BPD, assessed by the SCID-II, was reportedly present in 10% of participants with DSM-IV inattentive subtype ADHD (six or more symptoms in inattention) and 24% of participants with combined subtype ADHD (six or more symptoms of both inattention and hyperactivity/impulsivity) [26]. Likewise, in a sample of 181 adult patients diagnosed with BPD by general practitioners and referred for treatment, 38.1% had comorbid ADHD, with 22.7% meeting the combined type criteria [37].
In a sample of 118 adult women from out-patient clinics seeking treatment for BPD, a high co-occurrence rate was reported: 41.5% met criteria for childhood ADHD (assessed retrospectively), and 16.1% met current criteria for the DSM-IV combined subtype, as well as meeting ADHD criteria as children [38]. However, as opposed to the previous studies where diagnoses was confirmed by clinical interviews [26, 36, 37], severity of borderline personality disorder and ADHD symptoms were assessed using self-report questionnaires [38].
In a sample of adolescents (n = 107) with emerging BPD drawn from a European research project investigating the phenomenology of BPD in adolescence, the prevalence of ADHD was 11%, an estimate that was not attenuated even when excluding symptoms of impulsivity accounting for possible symptom overlap [39]. This rate was close to the 16% rate found by Philipsen and colleagues, where current ADHD symptoms was assessed by self-report measures [38], as opposed to clinician-based interviews. Moreover, the samples significantly differed in regard to participants’ age.
Regarding population samples, results from the National Epidemiologic Survey on Alcohol and Related Conditions of more than n = 34,000 adults, found that lifetime comorbidity with BPD in the ADHD population was 33.7% compared with a lower prevalence of BPD of only 5.2% in the general population [40].
Symptomatic overlap
There is considerable overlap in the symptoms of BPD and the associated features of ADHD (Table 3). Considering the onset and developmental trajectory, both disorders can be considered ‘developmental’ in the sense that they both emerge during childhood or adolescence and reflect enduring trait-like (non-episodic) symptoms and behaviours. The shared general features of trait-like symptoms that characterise both ADHD and BPD; means that differentiating between these diagnoses cannot easily be established by considering age of onset and course of symptoms. This means that to a large extent, differential diagnosis is based on the specific symptoms and behaviours used to define the two disorders.

Table 3. Overlapping features between ADHD and BPD
The most noticeable overlap among the core symptoms used to classify both conditions is impulsivity [1, 39]. Nevertheless, there are important qualitative differences in the manifestation of impulsivity used in the classification of ADHD and BPD. In ADHD, impulsivity refers to difficulty waiting or taking turn, blurting out during conversations (e.g. interrupting or talking over people), and intruding on others (e.g. butting into conversations or activities, taking over what others are doing) [5]. These impulsive symptoms are not always severe in adults with ADHD, but when severe can lead to impairment in social functioning and self-damaging or risk-taking behaviour. The consequences of severe impulsivity in ADHD include reckless driving, promiscuity, interpersonal relationship problems and aggressive behaviour [41, 42]. In BPD, impulsivity is defined by self-damaging behaviour, such as reckless driving, shoplifting, spending, binge eating, substance abuse and promiscuity [5]. People with either of these disorders may therefore display impulsive risk-taking behaviour, but from a diagnostic point of view they are core symptom of the BPD diagnosis, but only an associated feature of ADHD.
The other key area of symptom overlap is ED. This reflects a core symptom domain in the diagnostic classification of BPD [5], whereas in ADHD it is recognised as an associated clinical feature that supports the diagnosis [43, 44]. Nevertheless, ED is commonly seen to accompany ADHD, even in non-comorbid cases [35], and is an independent source of psychosocial impairment. This draws strong comparisons with ED in BPD, particularly when the ED that accompanies ADHD is severe [45]. At a descriptive level, the emotional symptoms of ADHD were well captured by Wender, Reimherr and colleagues in the earlier Wender-Utah criteria for ADHD, and show substantial overlap with the ED symptoms in the DSM-5 BPD criteria [1, 3, 38].
ED is a dimensional construct [46], referring to rapid and exaggerated changes in emotional states such as heightened irritability or hot temper [45]. A review by Asherson and colleagues reported that ED is present in 72–90% of adults with ADHD, and independently of other symptoms of ADHD predicts impairments in social, educational and occupational domains [47]. In contrast, ED is one of the core symptom domains of individuals with BPD, who nearly always suffer from severe persistent affective instability, inner tension and difficulty controlling emotions such as anger [27, 38, 48, 49]. Despite similarities, it has been suggested that patients with BPD have higher frequency and intensity of affective instability and aggressive impulsive reactions, compared to adults with ADHD [1, 49, 50]. Others describe ADHD patients as being high novelty seekers, who regulate their emotions through extreme external stimulation (e.g. sexual activity, aggressive behaviour), as opposed to those with BPD who tend to engage in self-mutilating behaviour to alleviate negative affect and inner tension [48]. However, self-harming behaviour and suicidality in ADHD has been highlighted in recent literature [51]. Yet, phenomenologically, ED is a complex construct, with shared characteristics in both ADHD and BPD, particularly pertaining to feelings of heightened anger and difficulty controlling anger (criterion eight in BPD) [38]. Others suggest that emotional instability reflects a similar cyclothymic temperament pattern in both disorders [52]. .Overall, it remains unclear whether the type of ED seen in ADHD really is qualitatively similar or different from that seen in BPD. One way to investigate this issue with precision is by using ambulatory assessments.
ED in ambulatory assessments
Emotions are time- and context-dependent processes which are not adequately captured by retrospective and cross-sectional reports [53]. Yet, within clinical environments, assessment of ED relies entirely on interviews and self-report rating scales, which may be highly subjective and based on retrospective recall. These methods limit the validity of assessments of fluctuating emotional symptoms by the reliance on the individual’s memory, the skills of the interviewer, and may be coloured by their mental state at the time of the assessment [53, 54]. For instance, it has been reported that BPD patients fail to remember their most extreme and intense mood changes [55]. One approach with greater ecological validity is the use of ecological momentary assessments (EMA), also known as ambulatory assessments or experience sampling, which use repeated ratings of real time experiences [56]. EMA provides an effective way of precisely measuring emotional dynamics and variation within individuals, over time [57, 58].
In BPD, several EMA studies have investigated the dynamics of emotional instability [50, 53, 59, 60, 61]. In one study of 50 BPD and 50 healthy controls using 24-h ambulatory monitoring (intervals of 15 min), the BPD group was found to overestimate emotions with negative valence and underestimate emotions with positive valence, comparing retrospective with EMA ratings [60, 62]. In contrast, the healthy control sample overestimated emotions with positive valence and underestimated emotions with negative valence [60, 62]. Individuals with BPD have also been found to report greater levels of intra-individual variability and short-term fluctuations in overall affect valence. In another study comparing 34 outpatients with BPD and 26 with current depression, using EMA for nearly one month, ratings indicated greater instability (i.e. more changes from one assessment to the next) over time for fear, hostility and sadness in the BPD group [63]. It has also been reported using EMA that compared to healthy controls, BPD patients experience a higher frequency and increased intensity of negative affect and a lower frequency and decreased intensity of positive affect [50, 53, 60, 61]. In addition, a recent review of 34 EMA studies found that BPD patients experience longer duration of aversive tension and therefore a slower return to their baseline affective state [55].
To our knowledge, there has been only one EMA study looking at the dynamics of emotional instability in adults with ADHD [57]. Compared to healthy controls (n = 47), patients with ADHD (n = 41) showed significantly increased instability and intensity of negative emotions (irritability, frustration and anger). They also showed greater reactivity of negative emotions, such as anger, to ‘bad’ life events. This study included only males and specifically excluded patients with comorbid conditions [57].
Critically, from the standpoint of contrasting ED in populations of patients with ADHD and BPD, there have been no studies of the phenomenon in both patient groups using the EMA method. Furthermore, additional information could also be collected regarding the naturalistic context and situation when emotional changes occur (e.g. where they are, who they are with, what has just happened); which might identify disorder specific contextual triggers for emotional changes in different disorders. Clearly this area needs more research before conclusions can be drawn about the similarity or differences of ED in BPD and ADHD.
Neurobiological correlates of ED in ADHD and BPD
The overlap in symptoms of emotional dysregulation in ADHD and BPD raises the question of a common neurobiological substrate for ED in the two conditions. In ADHD two competing hypotheses have been proposed for ED. First, the ‘dyscontrol hypothesis’ proposes that ED is driven by the same cognitive and neural processes that drive ADHD; for example, deficits in top down executive control, or bottom up state regulation factors [64]. In this model, ED reflects an alternative expression of the same underlying neurocognitive deficits that lead to ADHD symptoms. The alternative ‘affectivity hypothesis’ states that ED reflects deficits in neural processes related directly to emotional regulation, separate from those that lead to ADHD symptoms [64]. To date the accumulating evidence is pointing to the affectivity hypothesis. Two key publications support this conclusion [65, 66]. First, an investigation of cognitive performance deficits in ADHD (including inhibition, working memory, impulsive responding, slow and variable reaction times) found these were associated with ADHD symptoms independently from ED. [66] This suggests that different processes would explain the presence of ED in ADHD. Subsequently, a resting state functional Magnetic Resonance Imaging (fMRI) study in children with ADHD, found that ED, independently from ADHD, were associated with increased positive intrinsic functional connectivity (iFC) between bilateral amygdala and medial prefrontal regions, and reduced iFC between amygdala and bilateral insula/superior temporal gyrus. These findings suggested that ED is linked to disruptions in emotional control networks, which was not linked directly to ADHD [65].
Regarding BPD there are overlapping findings implicating the central role of emotional control networks. A critical review of fMRI studies conclude that emotional sensitivity, including emotional hypersensitivity and intense emotional reactions, was associated with increased amygdala activity and decreased activity with prefrontal cortical control regions [67]. In particular a consistent decrease in anterior cingulate activity and variable was identified, while the medial and dorsolateral prefrontal areas showed variable activity across studies. Overall, increased limbic and diminished prefrontal cortical activity suggested an impaired fronto-limbic inhibitory network [67].
Resting-state fMRI, contrasting intrinsic functional connectivity before and after an emotion regulation task in patients with BPD, further supports disrupted regulation of emotional circuits. Emotional hypersensitivity in BPD was associated with increased intrinsic connectivity between the amygdala and bilateral insula together with dorsal anterior cingulate cortex, while their impaired control over emotional reactions was associated with diminished intrinsic connectivity between the central executive fronto-parietal regions and salience network [68]. Overall the pattern of findings in relation to emotion regulation was similar to that reported for ADHD by Hulvershorn and colleagues [65].
The overlap of these findings in relation to ED in the two disorders suggests that there may be a common substrate for ED in the two conditions, involving altered top down and bottom up regulation of amygdala function and neural circuits. However, as we discuss below, evidence-based treatments are entirely different for the two disorders, suggesting that the underlying cause of the disrupted emotional circuits may differ in ADHD and BPD, potentially explaining differences in response to different treatments. Nevertheless, these findings suggest that there could also be common forms of treatment in a least a subset of patients with a comparable neurobiological basis for ED.
Genetic and environmental risk factors
ADHD
It is firmly established that genetic factors play a central role in the aetiology of ADHD. The disorder aggregates among biological relatives of ADHD probands [69, 70], and twin studies estimate heritability in the range of 70–80% for parent and teacher ratings of ADHD symptoms in children, with similar estimates for clinically diagnosed cases of ADHD [69, 70]. In adults, self-rating of ADHD symptoms lead to lower heritability estimates in the range of 30–50% [71]. However, heritability estimates are similar to those seen in children for the clinical diagnosis of ADHD in adults, or when combining parent ratings and self-reports [71, 72, 73]. These studies find that the variance in ADHD in both childhood and adulthood is best explained by genetic and non-shared environmental factors, with no role for shared environmental factors independent of genetic influences [71].
Earlier candidate gene studies found significant associations with genetic variation within dopamine and serotonin system genes [74], although these have yet to be replicated using genome-wide approaches. Until recently genome-wide association studies (GWAS) of ADHD had not identified genetic variants that increase the risk of ADHD, although heritability due to the measured genetic variance was estimated to be around 30% [75, 76]. The most recent GWAS using a much larger sample of 20,183 ADHD cases and 35,191 controls identified twelve independent loci above genome-wide levels of significance (p < 5 × 10− 8), confirming the existence of numerous common variants of small effect that influence the development ADHD [77]. As these are recent findings, further research examining the role of these variants is required.
BPD
Though not as widely developed as the genetic literature on ADHD, there is a growing body of research implicating genetic influences in the aetiology of BPD. There is evidence to support familial aggregation of BPD features [78, 79] and findings from twin studies report heritability estimates in the range 35%–67% [80, 81, 82]. There is consensus between the studies that the remaining variance may be explained by unique rather than shared environmental influences, similar to ADHD.
To date there have been two GWAS studies of BPD. One study assessed two Dutch cohorts (n = 7125) using the Personality Assessment Inventory-Borderline Features Scale and found a promising signal on chromosome 5, which corresponds to SERINC5, a protein involved in myelination [83]. Seven single nucleotide polymorphisms (SNPs) in this region had p values between 3.28x10− 6 and 8.22x10− 7, while still remaining below genome-wide levels of significance [83]. The other more recent GWAS study was performed in n = 998 BPD patients and n = 1545 psychiatric controls [84]. While gene-based analysis yielded two significant genes for BPD, DPYD on chromosome 1 (1.20x10− 6) and PKP4 on chromosome 2 (8.24x10− 7), no genome-wide significant association was found for any SNP [84]. These specific findings in BPD do not overlap with findings from ADHD.
Common genetic risk factors for BPD and ADHD
Though there is evidence for symptom overlap between the two disorders, to date only one study has explored whether this could reflect overlapping genetic influences. Using a population twin sample, high phenotypic correlation (r = 0.59) was found between ADHD symptoms and borderline personality traits; consisting of four subscales- affective instability, identity problems, negative relationships and self-harm [85]. The authors found that the phenotypic correlation was explained by 49% genetic factors and 51% environmental factors, suggesting that shared aetiology could be a cause of comorbidity between ADHD and BPD traits [85]. However no further studies have been conducted looking at this relationship.
Overall twin studies of ADHD and BPD show a similar pattern of genetic versus environmental influences, with slightly higher heritability estimates in most ADHD studies. Yet it is important to note that heritability is also a functional of the reliability of the measures being used, with the residual non-shared environment including measurement error. Although for both ADHD and BPD there is no evidence for the main effect of shared environment (environmental effects shared by co-twins that explain co-twin similarity), shared environment may still play a major role through gene by environment interactions. It is therefore likely that for both disorders there are genetically driven individual differences in susceptibility to environmental stressors. The relatively high genetic correlation between ADHD and BPD is based on the correlation of trait scores in the general population, rather than diagnosed cases, but suggests a considerable degree of underlying shared aetiology that may explain the frequent co-occurrence of ADHD and BPD. Further studies are needed to investigate the genetic overlap between the two disorders, but also the overlap with specific symptom domains such as ED.
Treatment approaches
Treatment approaches to ADHD and BPD are widely divergent. According to evidence-based clinical guidelines, in BPD there is limited evidence that medications reduce borderline personality symptoms, including ED, and psychological treatments are the cornerstone of treatment [86]. In contrast, in ADHD there is good evidence for effects of medication on reducing ADHD symptoms [87, 88, 89] and ED [90], and only limited evidence for effects of psychological treatments [91].
Clinical trials support the safety and efficacy of stimulants (methylphenidate, dexamphetamine,lisdexamfetamine) and atomoxetine, with reductions in the ADHD symptoms of inattention, impulsivity and hyperactivity, with moderate to large effects sizes ranging between 0.4 to 0.7 in adults [92, 93, 94, 95]. In addition, several randomised controlled trials (RCTs) have evaluated the effects of pharmacological treatments on ED in ADHD patients, and found comparable treatment responses to the primary symptoms of the disorder [13, 17, 96]. These findings are further validated by the results of two recent meta-analyses which found moderate effects of stimulants (methylphenidate, dexmethylphenidate, amphetamines, lisdexamfetamine) and atomoxetine on ED in ADHD (average Cohen’s d across studies around 0.4) [90, 97]. In these studies, ED was assessed with various measures including ED subscales of the Wender Reimherr Adult Attention Deficit Disorder Scale, the Behaviour Rating Inventory of Executive Function, the Conner’s’ Adult ADHD Rating Scales and the Brown Attention Deficit Disorder Scale.
In contrast to treatment of ADHD, psychotherapy is regarded as first line treatment for people with BPD [5]. The most common therapies are Transference-focused Therapy [98], Schema Therapy [99], Mentalization-based Treatment [100], Systems Training for Emotional Predictability and Problem Solving, and Dialectical Behaviour Therapy (DBT) [101]. DBT, the most intensively studied intervention for BPD, significantly reduces anger (Standardized Mean Difference (SMD) = − 0.83) and self-harm (SMD = − 0.54), and improves overall mental health functioning (SMD = 0.65) [102]. Not only is psychotherapy regarded as first line treatment for BPD, UK NICE guidelines stipulate that pharmacological treatments should not be used for managing BPD, nor for individual symptoms or behaviours associated with the disorder [86]. The guidelines recommend the use of pharmacotherapy only as short term treatment measure during a crisis or in the instance of co-occurring mental health disorders [86].
Currently, there is insufficient data on the treatment of co-occurring BPD and ADHD. With regard to drug treatment, there have been no RCTs of stimulants or atomoxetine in BPD alone or in co-occurring BPD-ADHD cases [90].
There have however been only two case reports [103, 104] of successful methylphenidate treatment in patients with co-occurring BPD and ADHD, and two open-label studies [105, 106]; In one adolescent female-only study, patients with co-occurring ADHD and BPD (n = 14) reported significant improvement of BPD symptom severity (SMD = − 1.5) and aggressive impulsive behaviour (SMD = − 1.31) following treatment with methylphenidate for 12 weeks [105]. In a four-week study of 47 adults looking at effects of methylphenidate in addition to DBT, comorbid ADHD-BPD patients who were on stimulant medication (n = 24) showed a statistically significant improvement in anger control (SMD = 0.14), motor impulsiveness (SMD = − 0.62), depression (SMD = − 1.09) and ADHD severity (SMD = − 0.5), compared to those without medication (n = 23) [106].
Similarly, there are various psychotherapeutic treatments available for adults with ADHD, who are either unresponsive to stimulants and/or atomoxetine, or in need of adjunctive psychotherapy. There have been two exploratory open label studies [107, 108] examining effects of psychotherapy in adult ADHD. According to the multicentre open label study of n = 72 patients with ADHD, an adaption of DBT, addressing emotion regulation, depression, impulse control, stress management, neurobiology of ADHD and ADHD in relationships, DBT has therapeutic benefit for people with ADHD [108]. There was a statistically significant decrease on all psychometric measures in the study after DBT treatment; SMD = − 0.74 for the ADHD-Checklist, SMD = − 0.5 for the Beck Depression Inventory (BDI) and SMD = − 0.34 for the adapted Symptom Check List (SCL-16) measuring agitation, disorganised behaviour, emotion dysregulation and irritability among other traits [108]. Similarly, in the open label pilot study of n = 8 patients with ADHD, an adaption of cognitive behavioural therapy led to improvement in the same psychometric elements listed above; ES = 0.99 for the BDI, ES = 2.22 for the ADHD-Checklist and ES = 1.35 for the SCL-16 [107].
There have also been three RCTs of cognitive therapy [109, 110, 111] with relatively small sample sizes (n = 31, n = 43 and n = 51 respectively), addressing the effects of psychotherapy (in conjunction with medication in some cases) in adult ADHD that resulted in positive outcomes on all scales measuring severity of ADHD symptoms(ES = 1.2, d = 1.4 and, depression, anxiety, anger control and organisation skills among other outcomes. However, a recent large multicentre RCT of n = 433 adult ADHD randomised participants to group psychotherapy (GPT) developed and tailored to the treatment of ADHD, compared to clinical management (CM) reflecting optimal usual clinical care, with both groups randomised to methylphenidate or placebo [112]. While methylphenidate significantly reduced ADHD symptoms compared to placebo (p = 0.003), there were no significant differences in ADHD symptoms for those receiving GPT or CM (p = 0.16). In fact, in this trial, medication proved to be superior to intensive behavioural therapy, yet the latter resulted in better outcomes when combined with medication as compared with placebo [112].
Overall, while DBT modules and other systematically tailored psychotherapies appear to be helpful in ADHD, it is not yet clear whether they improve the core symptoms of ADHD (inattention, and hyperactivity/impulsivity), and there is insufficient data reported for effects on emotional dysregulation in ADHD [107, 108, 109, 110, 111, 112, 113]. This needs further investigation, since the evidence to date is based on relatively small studies, and there has been only one trial of cognitive behavioural therapy in ADHD samples without concomitant medication [112].
Conclusions
In clinical practice, it should be acknowledged that the co-existence of ADHD with BPD may complicate the diagnostic process, and hinder treatment outcomes. Currently, patients with co-occurring ADHD and BPD are often seen by different specialists and provided treatments for one condition or the other, but only rarely for both. In fact, there is lack of empirical data to guide future clinical practice. Beyond the issues of differential diagnosis, there is insufficient awareness within specialist ADHD and BPD services of the potential benefits of treating the other condition. This needs to be addressed because treatment of both conditions may have positive benefits for individuals with overall better control of ADHD and BPD related symptoms and behaviours. Indeed, open clinical trials indicate the value of such a dual treatment approach.
Commonly in BPD patients with co-occurring ADHD, inattention and so called executive function deficits (i.e. sustained attention, forgetfulness, planning, organising, working memory), as well as physical restlessness and impatience, lead to difficulties in commitment and adherence to psychological therapies [114]. For example, this could be manifested in difficulties remaining seated, feeling restless and impatient, difficulties focusing on conversations and retaining information during therapy sessions, or insufficient planning and organisation to regularly attend therapy sessions [114].
A further potential benefit in a subpopulation of individuals with co-occurring ADHD and BPD may be a reduction in emotional dysregulation and impulsivity following medication treatment of ADHD. Similarly, psychotherapeutic interventions may be helpful for ADHD cases with high levels of emotional dysregulation with partial or no response to ADHD drug treatments, which could be accounted for by BPD. We therefore advocate a more nuanced approach to the management of people presenting with both ADHD and BPD.
An important question arising from the literature is the specificity of emotional symptoms that are seen in both ADHD and BPD. However, symptoms reflecting dysregulation emotional responses are also seen in other mental health disorders. A recent EMA study examined the dynamics of affective instability in patients with BPD compared with post-traumatic stress disorder and bulimia nervosa [56]. Using the same EMA protocol, all three conditions showed a similar degree of heightened affective instability regarding both the valence of emotional changes, and the level of associated distress [56]. Although BPD is the only disorder for which affective instability is part of the core diagnostic criteria [5], it seems that the specific dynamics of ED in BPD may not be so very different from that seen in other clinical groups.
Given the emerging genetic findings in relation to ADHD and BPD, and the overlap of symptoms such as ED, there may be gains from comparing the cognitive-neural underpinnings for ADHD and BPD, as well as overlapping symptom domains such as ED. At this stage, clinical trials are needed to evaluate the role of both ADHD medication and psychotherapy in the treatment of comorbid ADHD-BPD, and to identify treatment prognostic indicators. Under current circumstances, we suggest that health care professionals involved in diagnosing patients with either BPD or ADHD need to be aware of the potential diagnostic overlap and co-occurrence of these two disorders. Further, there should be sufficient clinical expertise to ensure that patient receive the evidence based treatments they require. This includes the potential benefits of drug treatments for ADHD, and psychotherapy for BPD.
Abbreviations
ADHD: Attention-Deficit/Hyperactivity Disorder
BDI: Beck Depression Inventory
BPD: Borderline Personality Disorder
CM: Clinical Management
DBT: Dialectical behavioural therapy
DSM: Diagnostic and Statistical Manual of Mental Disorders
ED: Emotional dysregulation
EMA: Ecological momentary assessment
fMRI: Functional Magnetic Resonance Imaging
GPT: Group Psychotherapy
GWAS: Genome wide association studies
iFC: Intrinsic functional connectivity
RCT: Randomised controlled trial
SCID-II: Structured clinical Interview for DSM-IV II
SCL: Symptom Check List
SMD: Standardised Mean Difference
SNP: Single nucleotide polymorphisms
References
See: https://bpded.biomedcentral.com/articles/10.1186/s40479-018-0086-8#Bib1
#adhd#bpd#borderline personality disorder#mental health#diagnostic overlap#symptomatology#executive functioning#impulsivity#development#treatment
0 notes
Text
Deborah Flynn, Narratives of melancholy: a humanities approach to depression, 36 Med Humanit 36 (2010)
Abstract
This paper explores narrative literature as a means of inquiry into the sense of self in depression. Described as a disease, an identity and a way of life, depression is influenced by both internal and external factors. Although brain research has provided new insight into the relationship between neurotransmitter function and depression, the symptoms are experienced by individuals whose lives are intertwined with historical and sociocultural interpretations of illness and its manifestations. At the intersection of science and the humanities, narratives aid in the interpretation of lived experiences, provide a window to that experience, and a public medium that engages writers and readers as they interpret the world. Engaging narratives to interpret both experience and medical jargon may reveal for both those experiencing depression and those engaged in their care, a way of mediating that experience. Narratives can help dissect and thus illuminate the official language of medicine and psychiatry and the personal language of depression. Such a window can enhance the opportunities for empathy and care.
Sense of self and depression
Described for two millennia and known by various names, clinical definitions of depression have not always represented individual experience. A contemporary definition of depression, taken from the DSM-IV-TR, includes the presence for at least two consecutive weeks of either depressed mood or loss of interest or pleasure in previously pleasurable things, in addition to at least four of the following: significant change in appetite and/or weight, sleep disturbance, psychomotor disturbance, fatigue, feelings of guilt or worthlessness, difficulty concentrating and recurrent thoughts of death; the presence of these symptoms must result in a change in previous functioning.1 In 1621 Burton noted, “The Tower of Babel never yielded such confusion of tongues as this chaos of melancholy doth variety of symptoms.”2 In 1917 Freud wrote, “Even in descriptive psychiatry the definition of melancholia is uncertain; it takes on various clinical forms (some of them suggesting somatic rather than psychogenic affections) that do not seem definitely to warrant reduction to a unity.”3 More than 50 years later, Beck concurred, “[a]lthough depression (or melancholia) has been recognised as a clinical syndrome for over 2000 years, as yet no completely satisfactory explanation of its puzzling and paradoxical features has been found”.4 Similarly, in a memoir of his own depression William Styron remarked,The disease of depression remains a great mystery … The intense and sometimes comically strident factionalism that exists in present-day psychiatry—the schism between the believers in psychotherapy and the adherents of pharmacology—resembles the medical quarrels of the eighteenth century (to bleed or not to bleed) and almost defines in itself the inexplicable nature of depression and the difficulty of its treatment. (Styron, p11)5
Culminating a long history of attempted definitions, Radden commented, “About clinical depression we seem to have more questions than definitive or enlightening answers.”6 Thus, in order to understand the experience of depression one must look beyond the changing definitions to the experience and expression of symptoms. Narrative can provide a window into the understanding of an experience that has been historically difficult define.
Each person perceives and mediates experiences through a distinct sense of self, and some experiences may change the sense of self. Individuals experiencing depression have described a loss of self, a second self or a disintegrated self. Clifford Beers described a self unlike what he had known. “… in telling the story of my life, I must relate the history of another self—a self which was dominant from my twenty-fourth to my twenty-sixth year. During that period I was unlike what I had been, or what I have been since.” (Beers, p5).7 William Styron remarked, “[M]y own sense of self had all but disappeared” (Styron, p56).5 Later, as he wrote of contemplating suicide Styron commented that, “[a] phenomenon that a number of people have noted while in deep depression is the sense of being accompanied by a second self—a wraithlike observer who, not sharing the dementia of his double, is able to watch with dispassionate curiosity as his companion struggles against the oncoming disaster, or decides to embrace it.” (Styron, p64).5 Thus a sense of two selves, one well and the other ill, may obscure a sense of an integrated self. Styron's observation that the individual's concept of self is enmeshed with the human response to illness, particularly when one experiences a psychological disorder, coincides with others' reflections. John Head mused, “[P]erhaps I was on a path to understanding who I had been and who I was becoming” (Head, p79).8 This concept of self alludes to a changing sense of self as both time and illness act as mediators to perceptions of lived experience. Just as reflections on the past influence present perceptions, illness can provoke a sense of self of which one has not been previously aware. Struggling with a changing sense of self, a common concern becomes identifying the real self.
Narrative stories aid understanding of an otherwise perplexing world and so help to make meaning of experience. Beers noted the impact of narratives on the question of slavery and asked, “why cannot a book be written which will free the helpless slaves of all creeds and colours confined today in the asylums and sanitariums throughout the world?” (Head, p176).8 Anatole Broyard observed, “[m]y initial experience of illness was like a series of disconnected shocks, and my first instinct was to try to bring it under control by turning it into a narrative” (Broyard, p19).9 Because an essential part of what it is to be human is to know oneself, narratives can provide a way to reaffirm one's sense of self through an exploration of the experiences and relationships one encounters. Ochs and Capp explain, “[t]he inseparability of narrative and self is grounded in the phenomenological assumption that entities are given meaning through being experienced” (Ochs, p21).10 Narratives can be particularly helpful to seekers and providers of mental health care in understanding how illness experiences shape the sense of self. This has important implications for models of care, especially because narratives assist those diagnosed with mental illness to maintain or reclaim previously established notions of self, relationships and roles.
Impact of social structures
The relationship between social structures and sense of self is an important one. Frank points to both the personal experience of illness and the social nature of illness stories.11 Kleinman suggests that “the experience of illness has something fundamental to teach each of us about the human condition” (Kleinman, pxiii).12 In contrast to disease, which Kleinman notes is the “recasting of illness in terms of theories of disorder”, and is the concern of the practitioner, illness represents the perspective of the symptomatic individual (Kleinman, p18).12 Shifting ideas about whether the body and mind are intricately entangled or represent two distinct entities of the self confound the experience, expression and ultimately the treatment of depression. For example, notions about the immutability of the mind and thus the self are reflected in efforts to confine and control individuals labelled as mad, in the asylums of 17th and 18thcentury Europe.13–15
Foucault placed mental illness within historical, political, social and cultural settings when he asked, “[i]s there not in mental illness a whole nucleus of significations that belongs to the domain in which it appeared—and, to begin with, the simple fact that it is in that domain that it is circumscribed as illness?” (Foucault, p56).13 Thus, the environment within which one lives serves to frame the perception of illness and so separates the well from the ill. Consequently, the development of a sense of self as well as its expression are interpreted and understood (or misunderstood) within the constraints of history, society and culture.
Though it is unclear how the onset of depression is instigated, it is clear that both biology and context are involved. Changing scientific paradigms concerning the cause and course of depression as well as changing attitudes and beliefs both about depression and those experiencing depression, contribute to this lack of clarity. Interestingly, the experiences of depression bear a remarkable resemblance to each other when compared across decades. While it is evident that, as Jamison notes, each person experiences illness ‘idiosyncratically’, it is also evident that a distorted sense of self is common among those experiencing depression in all eras, even while the theories and treatment change.16
Of interest is the extent to which sense of self is influenced by biological (inherited and adapted) and environmental (historical and sociocultural) processes. Vrettros noted that during the 19th century, conceptions of illness were shaped by Victorian cultural narratives.17 Whether medical histories or literary texts, the narratives provided form and substance to the private and public worlds of Victorian life and these in turn shaped accepted notions of self and social relationships. According to Grob, early psychiatric practice “reflected the role assigned to it by society”.18 Thus, care of the mentally ill reflected the sociocultural values of 18th century American society as opposed to the rigours of medical science.
This idea is important to the construction of self. Butler's concept of emergence suggests there is no control over one's beginnings therefore any concept of self is related to external forces such as historical and sociocultural influences.19 Beers' upbringing clearly defined his sense of self and influenced his responses to his hospital attendants. Despite their treatment of him as simply another ‘mental incompetent’ his education both at home and at school prepared him as a gentleman.7 His cultural narrative, then, influenced his response to both his illness and his care. In describing her conception of self before and after her diagnosis Jamison commented,
I was used to my mind being my best friend … I missed my home, my mind, my life of books and ‘friendly things,’ my world where most things were in their place … Now I had no choice but to live in the broken world that my mind had forced upon me. (Jamison, p37, 97)16
Jamison drew a very clear line between her past and present lives. She implicated not only the significance of her role as researcher and educator in creating a sense of self, but how that conflicted with her experience of illness.
In the last 2 decades, brain research has gained much notoriety, most notably through new techniques in neuroimaging. However, while the images provide an extraordinary look at the brain in action, they cannot tell the story of a life. Depression is not a distinct illness with a specific treatment; it is a conglomeration of signs and symptoms that affects its host in idiosyncratic ways, shaping both biology and disposition. Solomon averred,
Although depression is described by the popular press and the pharmaceutical industry as though it were a single-effect illness such as diabetes, it is not … Depression is not the consequence of a reduced level of anything we can now measure. Raising levels of serotonin in the brain triggers a process that eventually helps many depressed people feel better, but that is not because they have abnormally low levels of serotonin. (Soloman, p22)20
Furthermore, understanding the chemical mechanisms involved in altered mood does not necessarily translate into improved function. In describing her manic-depressive illness, Jamison asserted that, “[a]n understanding at an abstract level does not necessarily translate into an understanding at a day-to-day level. I have become fundamentally skeptical that anyone who does not have this disease can truly understand it.” (Jamison, p176).16 Thus while brain images can show where and when drugs affect neurotransmitters and this can lead to the development of medication that lifts the symptoms of depression, these are only part of the remedy. In the end the body that consumes the drugs contains more than a brain and chemical messengers; it contains the soul and personal life of a human being.
Jamison noted her reluctance to acknowledge her illness and that uncontrollable symptoms of her illness may be perceived by others as anger, irrationality and willfulness. “Moods are such an essential part of the substance of life, of one's notion of oneself, that even psychotic extremes in mood and behaviour can be seen as temporary, even understandable, reactions to what life has dealt.” (Jamison, p91).16 However, as an authority on manic-depressive illness, Jamison understands its biology as well as its implications for the lives of patients because she is one.
I believe, without a doubt, that manic-depressive illness is a medical illness; I also believe that, with rare exception, it is malpractice to treat it without medication. All of these beliefs aside, however, I still somehow thought that I ought to be able to carry on without drugs, that I ought to be able to do things my own way. (Jamison, p102)16
Doing things one's own way preserves the sense of self that is often threatened in mental illness. Because of some of its most outward signs, for example, sleep disturbance, difficulty concentrating, and a loss of pleasure in previously pleasurable things, it is difficult to maintain one's own way. Solomon observed, “[t]he insistence on normality, the belief in an inner logic in the face of unmistakable abnormality is endemic to depression” (Solomon, p72).20 Claims to normalcy are based on the preservation of whom one was before depression. Any sense of change in self jeopardises not only claims to normalcy but claims to one's self. Attention to narrative can provide insight into the experience and expression of depression, particularly the relationship between sense of self and social structures. Additionally, clues to sociocultural differences, as expressed through language, metaphor and story, may help to tailor interventions to a diverse group of individuals, leading to a better appreciation of mental health disparities and a means to begin to bridge the treatment gap.
Humanities and narrative medicine
Though narrative is an integral part of the medical consultation, of concern is the loss of the patient's voice as symptoms are transformed to diagnosis. During the modern period, the focus of medicine moved from the patient's experience to the technical expertise of clinicians.12 The natural sciences' inability to explain illness as experienced within a sociocultural context has been documented by others and underscores the assertion that narratives redirect attention usually focused on disease to include the patient and the lived experience.21 22 What emerges is a better understanding of what life is like outside the medical encounter. This is key to determining appropriate modes of care.
Placing narrative and medical technology in conversation with each other can enrich understanding of illness and wellbeing. Kirklin noted, “[f]amiliar with the culture and vocabulary of medicine, [medical educators] may be only partially aware of how both the culture and language of medicine, as opposed to the language and culture of the person who is ill, are dominant in the medical encounter” suggesting that the dominance of the medical culture and language in the doctor-patient interface must be acknowledged and bridged.23 Thus, the treatment community's history and culture represents an additional influence on the perception of both self and illness.
Noting the difference in both language and approach, it is important to reiterate the significance of the central question of the humanities, that is, what is it to be human, and to articulate the relationship between the extrinsic value of medical science and the intrinsic value of the nature of the human response to that science. Edgar and Pattison suggest that the humanities are important to medicine because the humanities compel us to scrutinise those scientific structures upon which medicine is based to the extent that they reflect beliefs about what humans are or aspire to be.24 “Within the humanities, this question—the question of how human beings understand, experience, and practice (sic) their own humanity—is typically addressed indirectly, by looking at the products of human existence, including language, beliefs, writings, paintings, and social institutions and organisations”.24 Although science raises questions about accommodating scientific inquiry, discovery and the ethical use of its knowledge, it does not provide answers to those questions; it is here that the humanities can provide guidance.24 Medical science derives from the validation of objective realities independent of what humans think or believe. The importance of the humanities derives from its response to those objective realities, attempting to understand them and scrutinising them in the context of what it means to be human. Scientific medicine, though it validates objective realities, is a product of human activity. Thus, in order to address both the objective realities of science and the subjective realities of humans and their societies, a multifaceted approach is necessary.
This inquiry reveals one inevitable barrier, and that is language. As Virginia Woolf put it, “[t]o hinder the description of illness in literature, there is the poverty of the language. English, which can express the thoughts of Hamlet and the tragedy of Lear, has no words for the shiver and the headache”.25 Despite eloquent expressions of self and depression, those on the outside can only catch a glimpse of what the experience is like. Wittgenstein noted, “the limits of my language mean the limits of my world”.26 This is not to contradict the ideas presented here but to acknowledge that listening to those who experience it first-hand is imperative to understanding illness. It is also to acknowledge the inherent complexity of making meaning of experience through words.
Assuming that language is an artefact of each cultural paradigm, that is, that language emerges to describe and convey sociocultural constructs and experiences, a lack of language to describe some experiences says something about the understanding and acceptability of that experience. Remembering that even personal experiences have multiple writers—for example, in addition to the individual, there are the keepers of the sociocultural history and traditions—it follows that these become the signposts for behaviour and markers of sociocultural norms. Thus, the individual, though attempting to express a very personal experience, is bound by the prevailing cultural language. This illustrates the difficulty of conveying to another the unique experience of self in depression.
Historical and sociocultural influences both shape the understanding of illness and inspire its research. The experiences of asylum patients instigated investigations of mental hospitals which eventually led to deinstitutionalisation. The experiences of soldiers and psychiatrists in WWII shaped mental health policy and practices in the 1950s and 1960s, and the experiences of neurologists in laboratories shaped the present era of neuropsychiatry. Throughout these eras the patient's narrative has slowly but surely been replaced by the medical narrative. The patient's voice has been in many cases usurped by the medical voice, leaving more room for the management of disease than for understanding the experience of illness. Patient narratives can place the patient's voice alongside and in conversation with the medical voice. This placement permits a consideration of human subjectivity along with the scientific objectivity that guides medical practice. There are obstacles however, when patients struggle with the language of illness.
Rose suggested that two concerns in attempting to tell a story of illness are the “fall into medical discourse and the escape to a view of illness as metaphor … [m]edicine and I have dismissed each other … [w]e do not have enough command of each other's language for the exchange to be fruitful”.27 Though patients often try to adopt medical terminology in an attempt to place themselves equally with their physicians, its use may unintentionally reinforce the authority of the medical establishment because even while the patient uses it, the medical language is divorced from experience.27 The result is often that patients surrender to the power of the medical narrative.
The second concern, viewing illness as metaphor, has been addressed by Sontag. Sontag suggested that not only is illness not a metaphor but to treat it as such is a distortion of the reality of illness.28 She asserted that metaphor permits the illness to represent the sufferer's, as opposed to the illness', character. “Sadness made one ‘interesting’,” noted Sontag (p31).28 There may be times when individuals experiencing depression, looking for the words to describe their emotions, must use metaphor. The depth of sadness in depression is difficult to describe without using some other image to shape it and make it real. However, Sontag emphasised that a disease should simply be regarded as a disease, though it is doubtful that Sontag would have asked narrative authors to cease the search for language to describe their experiences. Thus, the use of metaphor offers opportunities for understanding unlikely in technical language.
Conclusion
Because health is often something of an afterthought until it declines, there is frequently more to learn from the response to illness than from the response to good health. Morris asserts that “[i]llness always seems to tell us more about a person or an era than health does”, and suggests a biocultural approach to 21st century illness (Morris, p52).29 Narratives then, including firsthand experiential accounts, official accounts such as medical records and diagnostic criteria, and especially those culturally common accounts, such as popular literature, that express the attitudes and beliefs of a particular society, can be particularly helpful in a biocultural approach to illness. According to Morris,
Narrative will never replace lasers … medicine attuned to the influence of mind, emotion, and culture can help greatly in addressing illnesses that … involve … issues of personal behavio[u]r and of public health … In respecting rather than dismissing a patient's narrative, it can offer a means of healing where cure may be impossible … (Morris, p276–7)29
Though discoveries in medicine only point out what was there even before it was known, the ability of medicine to transform that discovery into something that assists human health or alleviates human suffering presents both gifts and challenges. However, neither scientific discoveries nor the human response to them occur in a vacuum. Each must be considered within their historical and sociocultural contexts. Applied to this inquiry, the humanities probe the official language and practice of medicine and their historical and sociocultural contexts.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders TR-IV. APA, 2000.
Jackson H, Glass WH, Burton R. Anatomy of melancholy. In: Jackson H, Glass WH, eds. The first partition. New York: New York Review Books, 1621/2001:397.
Freud S. Mourning and melancholia. In: Freud S, ed. General psychological theory. New York: Simon & Schuster, 1997:164.Google Scholar
Beck A. Depression: causes and treatment. Philadelphia: University of Pennsylvania Press, 1970:3.
Styron W. Darkness visible: a memoir of madness. New York: Vintage Books, 1990.Google Scholar
Radden J. The nature of melancholy: from Aristotle to Kristeva. New York: Oxford University Press, 2000:51.
Beers C. A mind that found itself. Fairfield, IA: 1st World Library, 1908/2006.
Head J. Black men and depression: saving our lives, healing our families and friends. New York: Harlem Moon, 2004.
1. ↵Broyard A. Intoxicated by my illness. New York: Random House, 1993.
Ochs E, Capps L. Narrating the self. Annu Rev Anthropol 1996;25:19–43.CrossRefWeb of ScienceGoogle Scholar
Frank A. The wounded storyteller: body, illness and ethics. Chicago: University of Chicago Press, 1995:79.
Kleinman A. The illness narratives: suffering, healing & the human condition. Basic Books, 1988.
Foucault M. Madness and civilization: a history of insanity in the age of reason. Translated by Richard Howard. New York: Vintage Books, 1965.
Millon T. Masters of the mind. Hoboken: Wiley & Sons, 2004.
Porter R. Madness: a brief history. Oxford: Oxford University Press, 2002.
Jamison KR. An unquiet mind: a memoir of moods and madness. New York: Vintage Books, 1995.
Vettros A. Somatic fictions: imagining illness in Victorian culture. Stanford: Stanford University Press, 1995.
Grob G. The inner world of American psychiatry 1890–1940. New Brunswick, NJ: Rutgers University Press, 1985:2.
Butler J. Giving an account of oneself. New York: Fordham University Press, 2005.
Solomon A. The noonday demon: an atlas of depression. New York: Scribner, 2001.
Reissman C. Narrative analysis. Newbury Park, CA: Sage Publications, 1993.
Charon R. Narrative medicine: honoring the stories of illness. New York: Oxford University Press, 2006.
Kirklin D. The medical humanities teaching and research agenda: a symbiotic relationship. J Med Ethics 2004;30:96–7.Google Scholar
Edgar A, Pattison S. Need humanities be so useless? Justifying the place and role of humanities as a critical resource for performance and practice. Med Humanit 2006;32:92–8.Abstract/FREE Full TextGoogle Scholar
Woolf V. On being ill. Ashfield, MA: Paris Press, 1930/2002:6.
Wittgenstein L. Tractacus logico-philosophicus. Hypertext of the bilingual Ogden edition. Translated by C.K.Ogden, n.d. http://www.kfs.org/∼jonathan/witt/tlph.html (accessed 12 Sep 2009).
Rimmon-Kenan S. What can narrative theory learn from illness narratives? Lit Med 2006;25:241–54.PubMedWeb of ScienceGoogle Scholar
Sontag S. Illness as metaphor. New York: Picador; Farrar, Strauss & Giroux, 1978.
Morris D. Illness and culture in the postmodern age. Berkeley: University of California Press, 2000.
#narrative#illness narratives#self-concept#depression#melancholia#mental illness#identity#The Self#lived experience#medical humanities#mind-body dualism#medicine#psychiatry
0 notes