#prepregnancy
Text
Which Nutrient Should be Taken in the Month Before Pregnancy?

Maintaining a healthy diet before pregnancy is necessary for the health of both the mother and the baby. In order to secure a hustle-free pregnancy, it is needed to include plenty of nutrient-rich foods in your regular diet. Some common nutrients for pregnant women include protein, iron, calcium, and folate.
Nutrition before Pregnancy
Diet and nutrition before pregnancy are extremely important for a women's health and the health of her future baby as well. Eating a balanced nutritional-based diet is best for getting the right amount of nutrients and important vitamins, and minerals.
Some nutrients are sometimes important for pre-pregnancy. Folic acid is one amazing nutrient, and it is consulted that all pregnant women take a prenatal vitamin that contains folic acid. Folic acid plays an important role to prevent certain birth defects of the baby's brain as well as the spine.
Another important nutrient before pregnancy is calcium. Calcium (1) is beneficial to build strong bones and teeth in the baby. Research said that before pregnancy, you should consume around 1000 mg of calcium per day. Good sources of calcium like dairy products, green vegetables which are leafy, and nuts too.
Read: What are the pros and cons of prenatal Vitamins
A woman who is looking for more options then, they should make sure they are getting enough balanced protein. For your future baby, protein is important for the fetus's growth and development. Pre-pregnancy, you should eat around 70 grams of protein per day. Good sources of protein you will get in meat, poultry, fish, eggs, dairy products, spinach, and legumes.
This is a true fact that a healthy diet is important for pregnant women, but at the same time for those who are trying to conceive. Women who are trying to conceive should be assured that they are in taking enough folic acid, calcium, and protein.
Supplements for Pregnancy Nutrition
There are many supplements available that are recommended by your nutritionist that can help you to meet your nutrient needs. Some of the best pregnancy supplements for women include,
Folic acid:
This helps to prevent birth defects in the brain and spine of the baby.
Iron:
Iron is as more as important for making red blood cells that carry oxygen to the baby. Most pregnant women should take an iron supplement.
Calcium:
Calcium is important for your future baby’s baby's teeth and bones. Pregnant women should try to consume 1200 mg of calcium per day.
Omega-3 fatty acids:
This nutrient is for the baby’s overall eye health and brain development. Before pregnancy or after pregnancy women may need supplements that contain omega-3 fatty acids. (2)
more ...
0 notes
Text
The joy of breastfeeding is that no matter how much I eat I'm somehow still RAVENOUS
#pregnancy was not like this for me#like at all#but now ive lost nearly 20 pounds from my prepregnancy weight after less than 2 months#like im fine. im not unhealthy#my body just hasnt reached it equilibrium yet#k gonna go eat a second lunch now and then feed baby again byeeeee
5 notes
·
View notes
Text

Throwback to prepregnancy
#hairy girl#hairy ginger#baby mama#pregnant girls#pregnant babe#pregnant teen#hairygirls#bikini barista#pregnancy sex#pregnancy progression
384 notes
·
View notes
Text
guy who gets pregnant with like A LOT of babies and it makes his dating profile pictures outdated so fucking quick. like he's two months along and he shows up to a date and the person is like Um because he looks like he could give birth any second but then he's like Oh yeah i just got pregnant like 7 weeks ago.
(but of course he never updates it so he ends up absolutely massive in the third trimester and showing up on dates barely able to fit through the door when his dates were expecting his tiny skinny ass prepregnancy body)
99 notes
·
View notes
Text

Both these guys gave birth last year and they think they can still fit into their prepregnancy pants. Dress like that they will probably both be pregnant again by the end of the day
36 notes
·
View notes
Text
Things I know
Prenatal care/high risk management can stay at my local hospital.
I will go back to the delivery hospital in 4-6 weeks to meet the whole team (cardiologist, cardiac surgery team, nicu staff, mfm doctor, etc)
Definitely delivering during week 38 unless I go into labor naturally but MFM very much wants induction so I don't have to drive 1.5 hours in labor.
Preference is v delivery (using the plumbing as it was intended which were the words from the mfm).
Social worker from delivery hospital will help with accommodations for me and little miss if her brother needs and extended nicu stay.
Surgery will definitely happen between 3-6 months.
Currently unclear if little man will need medicine or shunt placement immediately after birth but there is the possibility that if it is needed it could happen in the cath lab and not with surgery.
His surgery will be there but all treatment and check ups (except those directly related to surgery) will be with the ped cardiologist here.
Cardiologist thinks he'll probably need another surgery when he's around 10 but may not need anymore after that - it's just wait and see kind of thing.
Cardiologist said that Shaun White (who has the same heart defect as little man) is now the norm for kids with TOF and that's what our goal is basically - healthy but still monitored and aware.
Both babies are estimated at almost 2lbs - they gained a whole oz between Thursday at my growth scan and today!!
Both babies looked really good today. They were both kicking so much during the echo and the ultrasound.
I've gained 2lbs from prepregnancy weight (no one is concerned about that because obesity).
The prevalence of Jesus on the crucifix in every room was very disconcerting (Catholic hospital but was still not excepting that in every patient room, the waiting room, and the lobbies I was in).
I've now met my deductible and out of pocket max (they reset Sept 1).
Today was a long day but I feel like I have a somewhat better handle on things and a somewhat better idea of how I move forward. And more answers than before. It's terrifying to know what lies ahead, but the doctors are positive and the plan is more solid.
13 notes
·
View notes
Photo
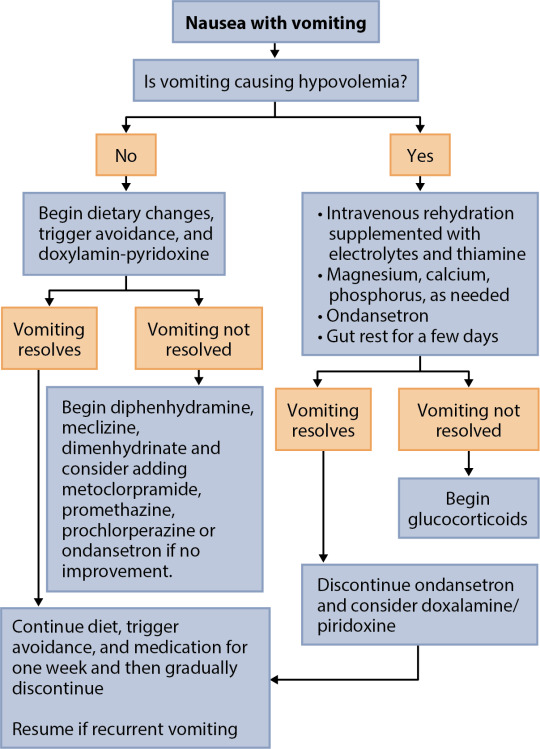
Hyperemesis gravidarum (HG) is a condition that causes frequent vomiting in pregnant women. It is similar to morning sickness, except the symptoms are much more severe. Diagnosis is based on symptoms of severe nausea and vomiting in conjunction with a loss of more than 5% of the patient's prepregnancy weight. It usually occurs in the first trimester, and symptoms usually resolve by mid-pregnancy regardless of severity and need for therapy.
Pregnant women with severe vomiting should present to the emergency room if they have symptoms of hypovolemia, which include decreased energy, postural dizziness, thirst, tachycardia, or decreased urine volume or frequency. These women should be treated with IV fluids. It is also important to replenish other vitamins and minerals such as thiamine, folic acid, magnesium, calcium, and phosphorus. Antiemetic medications may be used, but the risks of a small increase in congenital anomalies for patients under 10 weeks' gestation must be considered. The first line antiemetic medication in hospitalized patients with HG is ondansetron.
Once vomiting is controlled and the patient is sent home, there are a variety of options to manage nausea. These include ginger-containing foods, vitamin B6 (Pyridoxine), and the combination doxylamine-pyridoxine. Doxylamine is an antihistamine that is traditionally used as a sleep aid medication. Ginger has been found to decrease nausea, but it has not been found to reduce vomiting. Pyridoxine has also been found to significantly reduce nausea, but not vomiting. It is often used first line due to its efficacy and minimal side effects. The combination doxylamine-pyridoxine has been found to help with both nausea and vomiting. Other alternative treatments such as acupuncture and hypnosis have also been found to be helpful in some patients.
3 notes
·
View notes
Text
Establishing a relationship with a trusted gynecologist is essential for comprehensive and personalized care. A gynecologist can offer guidance on birth control options, prepregnancy and prenatal care, relief from menopause symptoms, mental health issues, and more. By building a rapport with a gynecologist, individuals can receive tailored advice, necessary screenings, vaccinations, and support for their specific health needs. Seek consultation with the best gynecologist in Lucknow Dr. S Sharma at Sanjivini Super Speciality Hospital Lucknow.
0 notes
Text
0 notes
Link
Check out this listing I just added to my Poshmark closet: TAYLOR from PEA IN A POD maternity dress.
0 notes
Text
Pre-Pregnancy Counseling: A Stepping Stone to Parenthood

Do you have a baby bump? Yes! Then, before you jump in the air with joy, you should take a look at pregnancy counseling, because expecting a baby requires a lot of acceptance and awareness, and that makes it a stepping stone to parenthood, a path of responsibility and mindfulness.
Pre-pregnancy counseling is a motto that pre-empts the certain risk factors pertaining a women’s, the fetus and neonatal health from entering an unfavorable phase. The one-to-one interaction with the professional can be a great aide in optimizing the health care of mother and child, which also extends to the family ties, as their care is invested from the first days.
Education about the pregnancy journey in pre-pregnancy course is open to all genders, sexualities and parents, as they offer a holistic approach to better parenting. Regardless of whether you are planning a pregnancy or using contraception, the pre-pregnancy counseling is applicable to both parties.

As the saying goes, health status can't be the same forever, over growing time potential risks can occur anytime. Thus, pre-pregnancy counseling does not last for a day, but it occurs several times for ensuring a healthy and happy baby journey!
Day in and out whenever an expectant mother gets counselled, fresh knowledge is added to her advantage for handling the situation. There is a certainty of several chronic conditions viz; diabetes, hypertension, thyroid and mental health require monitoring during pre-pregnancy for a desirable outcome.
In the pre-pregnancy counseling sessions, a crucial assessment for examining STDs is a must with a vivid screening for any probable genetic conditions that might pass down to the life growing inside.
The other important matter of concern here is to debrief on possible strong addictions namely, liquor, nicotine consumption, drugs or any other medicines taken for some underlining or nonmedical reasons.
There is also a significant survey conducted on partner violence during intimacy during prepregnancy counseling as it has entirely a direct impact on the mother and child both.

The expert guidance - Suggestions from the desk of the American College of Obstetrician and Gynecologists
The ACOG institute emphasizes the opportunity to stroke the iron hard and discuss overall wellness, and healthy habits as a routine irrespective of the patient for a successful outcome.
“Would you like to become pregnant next year?” Serves the purpose, of the right to speak out one's heart for suitable guidance without coyness.
The goal of prepregnancy counseling is to ensure a pregnancy that is away from the instructions and if any challenges occur one has the tact to handle it with expert guidance.
An annual influenza inoculation is mandatory for every patient unbiased as it is for additional benefit.
Prepregnancy is not limited to basic health checkups and discussions a patient's lifestyle and underlining conditions are crucial to tap on! If discovered to be a specific virus prone or any infection or allergies due to climate/ certain food types must be cautioned beforehand as travelling is a massive no.
Appropriate nourishment and vitamins are so significant for a healthy pregnancy tenure. Always fall back on your medical adviser for the proportion of food intake that suits your body the best during the prepregnancy period.
Read More: https://www.drshubhragoyal.com/welcome/blogs/pre-pregnancy-counseling:-a-stepping-stone-to-parenthood
#Pre-Pregnancy Counseling#pre pregnancy genetic counseling#Preconception Counseling#Family Planning Advice#Reproductive Health Consultation#Pre-Pregnancy Health Tips#Fertility Planning#Pre-Pregnancy Genetic Counseling#Genetic Screening before Pregnancy#Preconception Genetic Testing#Genetic Counseling Services#Prenatal Risk Assessment#Planning for Pregnancy#Healthy Pregnancy Preparation#Conception Readiness Guidance#Fertility Awareness Counseling#Pre-Pregnancy Wellness#Genetic Health Evaluation#Pregnancy Readiness Consultation#Hereditary Disease Counseling#Carrier Screening before Pregnancy#Counseling for Future Parents#Genetic Risk Assessment for Pregnancy#Family Health History Review#Reproductive Life Planning#Pre-Pregnancy Checkup
1 note
·
View note
Text
i’m not even sure if or when we want to be parents, but we’ve been talking about it. And yesterday, he said he was thinking about it.
It doesn’t stress me out anymore like it used to. I don’t have a strong urge of no anymore either.
But i do feel scared. Of things going wrong. Particularly because of my obesity, a BMI of 39.3!! I need to reduce weight from 113 kg to 83 kg before even we start to conceive.
So here i am researching stuff.
Offspring of overweight and obese women are at increased risk to be born large-for-gestational age and become overweight or obese as children or adults. Risk relates to maternal preconceptual weight, weight gain, and maternal glucose metabolism during pregnancy and breastfeeding.
After the pregnancy, mothers continue to influence their infants’ weight gain and weight status. Breastfeeding is one factor that promotes optimal weight gain in infants. Risk reduction is related to exclusivity and duration of breastfeeding. One postulated mechanism is the promotion of self-regulation of appetite in the infant. Another important factor is the timing of introduction of supplemental baby foods. Infants who receive first baby foods later in the first 6 months exhibit lower risk for obesity than those who receive baby foods early in that period. In addition, the family food and activity environment are important predictors of early weight gain.
For the newborn infant, the strongest predictor of later obesity is maternal preconceptual BMI. The mother’s preconceptual weight status is a marker of both environmental and genetic risk for the child. Genetic traits from the family can influence obesity risk.
Excess gestational weight gain is associated with risk for both the infant and the mother. In approximately two-thirds of U.S. pregnancies, weight gain exceeds Institute of Medicine guidelines.
Risks for Infant: Excess gestational weight gain is associated with fetal macrosomia and increased risk for developing childhood obesity. Macrosomic infants are at increased risk of obesity in childhood and adulthood compared to normal birthweight infants. Thus, more optimal gestational weight gain decreases risk for high birthweight.
It is well documented that many women increase caloric intake and decrease physical activity during pregnancy. Based on knowledge gained from nutrition and physical activity interventions promoting behavior change techniques, limiting excess caloric intake and increasing exercise during pregnancy may reduce gestational weight gain. Curbing excess gestational weight gain has been associated with lower risk of childhood overweight. This is true even when first and second trimester weight gain have exceeded the recommended guidelines.
Infants’ individual weight gain trajectories continue on a consistent path from prenatal into postnatal life. The effect of gestational weight gain on infant weight continues after birth, as fetal weight in the last trimester is associated with infant weight gain in the first months of life and subsequent risk for obesity.
Risks for mother: Excess gestational weight gain not only presents health risks for the mother during pregnancy, labor, and delivery, but also significant increased risk for postpartum weight retention. Furthermore, return to prepregnancy weight is important not only for the mother’s health, but also the health of her future infants.
<source>
0 notes
Text
Week 28
Still here, still miserable. I can eat and keep down 1-2 small meals a day (with Zofran and Pepcid), but for hours after eating I'm nauseous amd have heartburn. I haven't gotten back to my prepregnancy weight yet, even. Everything hurts. My back and legs and hips ache, and I have sharp pain in my left hip/glute (sciatica, probably!) which makes it really hard to do...anything. But I would take the muscle/skeletal pain over the nausea any day if I could choose. Having both simultaneously is a new level of cruel. I ate a small bowl of potato chips three hours ago and it's just sitting there, unmoving. If I don't eat dinner I get nauseous-hungry by bedtime, but if I do eat dinner I'm nauseous till bedtime anyway. Three more fucking months of this!!
1 note
·
View note
Photo

Ya girl decided to try on my pre pregnancy workout clothes😂 Swipe to see how it’s going😅 Full video of me trying on my pre pregnancy workout clothes at 8 months pregnant link in the bio!😅 let’s just say it was a MAJOR STRUGGLE!!! Also, I am uploading 2X a week up until Christmas!! Stay tuned for those videos!! #beunstoppable #pregnant #pregnancy #pregnantlife #pregnantathlete #fitpregnancy #fitpregnancyjourney #fitmom #crossfit #prepregnancy #crossfitathlete #fitnessjourney #fitgirl https://www.instagram.com/p/CXJD_SqO-0W/?utm_medium=tumblr
#beunstoppable#pregnant#pregnancy#pregnantlife#pregnantathlete#fitpregnancy#fitpregnancyjourney#fitmom#crossfit#prepregnancy#crossfitathlete#fitnessjourney#fitgirl
7 notes
·
View notes
Text
Tips for Healthy pre-pregnancy
Pre-conception nutrition is the most essential part of fitting own self up for pregnancy. Most Importantly upcoming mothers should concentrate more on weight such as your weight compared with your height and what food you are having for lunch or dinner will play a vital role in your health during this time and the health of your growing fetus.

Pre-pregnancy weight will straight away influence your baby's growth. If you'll do research you’ll find that underweight women are more likely to gives birth to small weight babies, even though they may gain the same amount in pregnancy as normal-weight women. Overweight women have increased risks for problems in pregnancy such as thyroid, diabetes or high blood pressure. So, there should be proper weight and as per that proper proportion of nutrients should be eaten to be healthy so that baby also is a healthy baby and mother will also be fit and healthy after pregnancy.
List of nutritious substance to maintain weight and growth
The following are some advice on how and what to eat to lead a healthy life during pregnancy. Making sure you’re having proper food and avoiding unhealthy nutrition, and also maintain a balanced lifestyle. By maintaining this you will give your body a particular shape to make, and then grow, a baby.
Leafy Green Veggies like spinach, kale, broccoli, etc. Which are rich in fiber, vitamin C, vitamin K, vitamin A, calcium, iron, folate and potassium. vitamin which helps a pre-pregnant woman to prevent neural tube defects, including spina bifida, during the earliest stages of fetal development. Don’t eat only salads every day have enough quantity of food affording to your need.
Coconut oil is very good if includes regularly in your pre-pregnancy diet. It can help settle your digestive system. A spoonful of this oil can help relieve pregnancy nausea as well as Hyperacidity. You can even add this oil heartburn soup Or bowl full of raw organic vegetable salad as breakfast. Coconut oil has powerful anti-viral and anti-fungal properties - Lauric acid and capric acid is present in coconut oil will be part of the adipose tissue for growing fetus and also it helps milk store of a lactating mother in the later stage. It will also boost up your immune system and thus, your growing baby will be free from fungal and inflected viruses as well.
Calcium is used to build a baby's bones and teeth. It’s very much essential to have calcium in your diet, if you do not consume enough calcium, the mineral will be drawn from the mother's stores in her bones and given to the baby to meet the ultimatum of pregnancy. Dairy products are also strengthened with vitamin D, this nutrient also plays a vital role with calcium in the progress of a baby's bones and teeth.
Enough Protein is needed for would-be mother, most women don't have problems getting enough protein-rich foods in their diets. Still, I will recommend that it’s better to consult your gynecologist for which kind of protein intake is suitable for you. Pregnant lady should include protein-rich foods such as meat, poultry, fish, dried beans and peas, eggs, nuts, tofu.
Eat fruits like raspberries, blueberries, and strawberries are very good and tasty as well. They're stocked with phytonutrients -- plant compounds that help fight disease. It contains lots of vitamin C, which is mandatory for proper collagen formation, it’s an opener to strengthening your membranes.low in vitamin C in your diet may increase the risk of premature delivery. In your breakfast, have a Plate full of berries and layer them with yogurt and high-fiber lentils.
Apart from taking healthy nutrients, pre-pregnant women should maintain a healthy lifestyle as well.
Stress can inflict havoc on your body by boosting diabetes levels also can affect I’m blood pressure which can suppress ovulation and decrease sperm count. Stress can stagnate energy and constrict blood flow. This stuff can help you manage your stress. Again I mention before doing all these do consult your physician positively.
Breathing exercises
Meditation
Hot oil massage on hair
Proper Sleep
Acupressure
Reading Journals
Listening light music,
Take a relaxing bath
What you shouldn’t intake during pregnancy or if you are planning for it.
Forgot intake of alcohol if you are planning to conceive, during pregnancy, and till breastfeeding. Drinking alcohol during pregnancy causes(FAS) fetal alcohol syndrome.
Stop consuming foods which lead to food poisoning or other disease caused by bacteria. These include everyone's choice like soft cheeses, paté, cold meats, pre-prepared salads, raw or smoky seafood, and raw eggs. Make sure that eggs, meat, and fish you eat are cooked properly and should be fresh not like buying from the market yesterday and cooking day after that.
Choose fresh fish. Some fish carry out more amount of mercury than others. Like if you want to eat Canned tuna which is very much affordable and also full of omega-3s. You can serve this 2 Or 3 in week. Here is some list of fish you can have while pregnant in your pre-pregnant period. Like- Shrimps, Salmon, Catfish, crab, etc.
Never ever skip breakfast rather you should have proper nutritional breakfast during this time.If you can cut off caffeine that’s well and good Or just keep your caffeine consumption to a maximum of 200 mg per day.Don’t forget caffeine is also in chocolate, tea, some soft and energy drinks too. Don’t take prot5 shake without prescribed by your physician.
Check it out and ping us for more such tips !!
Visit: www.drmanjunathivf.com
Call us: +91 73381 90382
1 note
·
View note
Text
There are 3 stages of labor. The first stage is divided into the latent and active phases.
The first stage occurs when labor begins and ends with complete dilation of the cervix. Broken down further, the latent phase of the first stage occurs first and is considered to have more gradual changes in the cervix and less regular contractions. Once the cervix reaches 6 cm, the latent phase of the first stage is complete. The active phase of the first stage is from 6 cm to 10 cm of cervical dilation. The time it takes for a woman to reach a certain point of cervical dilation will vary depending on multiple factors including number of previous births (parity).
The second stage of labor starts when the cervix is completely dilated at 10 cm and ends with delivery of the baby. The third and final stage of labor occurs between the time of delivery of the baby and delivery of the placenta.
In the primigravida, a lack of cervical change for more than 20 hours during the latent phase is considered failure to progress.
Contraindications to breastfeeding
Infants with Special Dietary Requirements
Galatosemia
Phenylketonuria (may be partially breastfed)
Maternal Infectious Disease
Cytomegalovirus – may or may not breastfeed, depending on individual circumstances
Herpes – if active on breast, may use other breast if not affected
HIV – may or may not breastfeed, depending on individual circumstances
Human T-lymphotropic virus type 1 or 2 infection – transmitted primarily through breastfeeding
Tuberculosis – if not contagious or may resume feeding after 2 weeks of treatment
Maternal Drugs
Chemotherapy agents – certain agents, discontinue breastfeeding for as long as they remain in the milk
Drugs of abuse – discontinue breastfeeding until drugs are out of maternal system
Primaquine and quinine – contraindicated if either infant or mother has G6PD
Metronidazole – discontinue breastfeeding until at least 12-24 hours after medication
Sulfa drugs – may be a problem in infants with jaundice or G6PD, stressed or premature
Radioactive isotope – discontinue breastfeeding for as long as the radioactivity is in the milk
Current guidelines for changes in weight during the course of pregnancy are based on prepregnancy body mass index (BMI). An increase of 100 to 300 kcal/d is recommended during the course of pregnancy, whereas an increase of 500 kcal/d is recommended during breastfeeding in the postpartum period. Excessive weight gain is greater than 1.5 kg per month, whereas inadequate weight gain is less than 1 kg per month.
Guidelines for weight gain according to BMI are divided into 4 categories: underweight (BMI less than 18.5), normal weight (BMI 18.5-24.9), overweight (BMI 25.0-29.9), and severely overweight (BMI ≥ 30.0). The recommended weight gain is 28 to 40 pounds for underweight patients, 25 to 35 pounds for patients in the normal weight category, 15 to 25 pounds for overweight patients, and 11 to 20 pounds for severely overweight patients.
To maintain a healthy pregnancy, women should consume on average about 340 kcal/day in the second trimester and 450 kcal per day in the third trimester. This averages out to 300 kcal/day throughout the course of the pregnancy.
Most pregnant women have a glucose screening test between 24 and 28 weeks of pregnancy. This is considered the second trimester.
Group B Streptococcus (GBS) is the leading cause of neonatal infection whose primary risk factors are maternal colonization of the genitourinary and gastrointestinal tracts. For this reason, GBS screening with a vaginal-rectal culture should be performed in all pregnant women between 36w0d and 37w6d gestation. All women with positive screening results should receive appropriate intrapartum prophylaxis, unless a prelabor cesarean section is performed with intact membranes. The gold standard for intrapartum GBS prophylaxis is IV penicillin G or IV ampicillin for at least 4 hours prior to delivery. If delivery occurs less than 4 hours following antibiotic therapy, a CBC and blood culture should be drawn and the child should be closely monitored for signs of sepsis. If a woman is allergic to penicillin and has a low risk for anaphylaxis, then a cephalosporin can be used such as cefazolin. Those with high risk or previous anaphylaxis can be treated with clindamycin (if susceptible) or vancomycin.
Two clinical syndromes of invasive GBS disease exist in newborns. The first is GBS early-onset disease (EOD), which presents in the first 7 days of life and occurs secondary to vertical transmissions. GBS EOD is most likely to be characterized by sepsis or pneumonia. Proper prophylaxis in labor is meant to prevent GBS EOD. The second syndrome is GBS late-onset disease, which presents between 7 days after birth and 2-3 months of age and is commonly presents as meningitis. Late-onset GBS is typically acquired via horizontal transmission and thus intrapartum GBS prophylaxis does not decrease its risk.
Protraction is defined as a slow rate of cervical change less than 1.2 cm/h for the nullipara and less than 1.5 cm/h for the multipara. Arrest disorders consist of complete cessation of progress. Arrest disorders include secondary arrest of dilation (no progress in cervical dilation in more than 2 hours), arrest of descent (fetal head does not descend for more than 1 hour in nullipara and more than 0.5 hours in multipara), and failure of descent (no descent). The most common cause of a protraction disorder is inadequate uterine activity. Although external tocodynamometry can only evaluate the time interval between contractions, a contraction interval of 4 to 7 minutes is likely not sufficient to cause cervical change. Internal tocodynamometry via an intrauterine pressure catheter (IUPC) allows the physician to evaluate contraction interval and strength of contractions. An IUPC is frequently used when inadequate uterine activity is suspected owing to a protraction or arrest disorder. Once inadequate uterine activity is diagnosed with an IUPC, oxytocin is usually administered.
Although the finding of glucosuria may be concerning in most patients, it is normal during pregnancy for a pregnant woman’s kidneys to have a decreased threshold for glucose. Thus, glucosuria is common during pregnancy and found in about 50% of patients.
1 note
·
View note