#tmj syndrome symptoms
Text
#tmj syndrome#tmj disorder#tmj treatment in hyderabad#temporomandibular joint syndrome#tmj syndrome symptoms
0 notes
Text
"The 200+ Symptoms of Fibromyalgia"
(Note: Some symptoms may overlap)
GENERAL
1. Activity level decreased to less than 50% of pre-illness activity level
2. Cold hands and feet (extremities)
3. Cough
4. Craving carbohydrates
5. Delayed reaction to physical activity or stressful events
6. Dryness of eyes and/or mouth
7. Edema (Oedema)
8. Family member(s) with Fibromyalgia
9. Fatigue, made worse by physical exertion or stress
10. Feeling cold often
11. Feeling hot often
12. Frequent sighing
13. Heart palpitations
14. Hoarseness
15. Hypoglycemia (blood sugar falls or low)
16. Increased thirst
17. Low blood pressure (below 110/70)
18. Low body temperature (below 97.6)
19. Low-grade fevers
20. Night sweats
21. Noisy joints – with or without pain
22. Poor circulation in hands/feet
23. Profuse sweating
24. Recurrent flu-like illness
25. Shortness of breath with little or no exertion
26. Severe nasal allergies (new or worsening allergies)
27. Sore throat
28. Subjective swelling of extremities – (feels swollen Bu can’t find anything)
29. Sweats
30. Symptoms worsened by air travel
31. Symptoms worsened by stress
32. Symptoms worsened by temperature changes
33. Tender or swollen lymph nodes, especially in neck and underarms
34. Tremor or trembling
35. Unexplained weight gain or loss
PAIN
36. Abdominal wall pain
37. Bad hip pain
38. Burning Nerve Pain
39. Chest pain
40. Collarbone pain
41. Diffuse swelling
42. Elbow pain
43. Exacerbated Plantar arch or heel pain
44. “Growing” pains that don’t go away once you are done growing
45. Headache – tension or migraine
46. Inflamed Rib Cartilage
47. Joint pain
48. Lumpy, tender breasts
49. Morning stiffness
50. Muscle pain - widespread
51. Muscle spasms
52. Muscle twitching
53. Muscle weakness
54. Pain that ranges from moderate to severe
55. Pain that moves around the body
56. Paralysis or severe weakness of an arm or leg
57. Restless Leg Syndrome
58. Rib Pain
59. Scalp Pain (like hair being pulled out)
60. Sciatica-like pain
61. Tender points or trigger points
62. TMJ syndrome
63. “Voodoo Doll” Poking Sensation in random places
NEUROLOGICAL
64. Blackouts
65. Brain fog
66. Carpal Tunnel
67. Feeling spaced out
68. Hallucinating smells
69. Inability to think clearly
70. Lightheadedness
71. Noise intolerance
72. Numbness or tingling sensations
73. Photophobia (sensitivity to light)
74. Seizures
75. Seizure-like episodes
76. Sensation that you might faint
77. Syncope (fainting)
78. Tinnitus (ringing in one or both ears)
79. Vertigo or dizziness
EQUILIBRIUM/PERCEPTION
80. Bumping into things
81. Clumsy Walking
82. Difficulty balancing
83. Difficulty judging distances (when driving, etc.)
84. Directional disorientation
85. Dropping things frequently
86. Feeling spatially disoriented
87. Frequent tripping or stumbling
88. Not seeing what you’re looking at
89. Poor balance and coordination
90. Staggering gait
SLEEP
91. Alertness/energy best late at night
92. Altered sleep/wake schedule
93. Awakening frequently
94. Difficulty falling asleep
95. Difficulty staying asleep
96. Excessive sleeping
97. Extreme alertness or energy levels late at night
98. Falling asleep at random and sometimes dangerous moments
99. Fatigue
100. Light or broken sleep pattern
101. Muscle spasms/twitches at night
102. Narcolepsy
103. Sleep disturbances
104. Sleep starts or falling sensations
105. Teeth grinding - "Bruxism"
106. Tossing and turning
107. Un-refreshing or non-restorative sleep
108. Vivid or disturbing dreams/nightmares
EYES/VISION
109. Blind spots in vision
110. Eye pain
111. Difficulty switching focus from one thing to another
112. Frequent changes in ability to see well
113. Night driving difficulty
114. Occasional Blurry vision
115. Poor night vision
116. Rapidly worsening vision
117. Vision changes
COGNITIVE
118. Becoming lost in familiar locations when driving
119. Confusion
120. Difficulty expressing ideas in words
121. Difficulty following conversation (especially if background noise present)
122. Difficulty following directions while driving
123. Difficulty following oral instructions
124. Difficulty following written instructions
125. Difficulty making decisions
126. Difficulty moving your mouth to speak
127. Difficulty paying attention
128. Difficulty putting ideas together to form a complete picture
129. Difficulty putting tasks or things in proper sequence
130. Difficulty recognizing faces
131. Difficulty speaking known words
132. Difficulty remembering names of objects
133. Difficulty remembering names of people
134. Difficulty understanding what you read
135. Difficulty with long-term memory
136. Difficulty with simple calculations
137. Difficulty with short-term memory
138. Easily distracted during a task
139. Dyslexia-type symptoms occasionally
140. Feeling too disoriented to drive
141. Forgetting how to do routine things
142. Impaired ability to concentrate
143. Inability to recognize familiar surroundings
144. Losing track in the middle of a task (remembering what to do next)
145. Losing your train of thought in the middle of a sentence
146. Loss of ability to distinguish some colors
147. Poor judgment
148. Short term memory impairment
149. Slowed speech
150. Staring into space trying to think
151. Stuttering; stammering
152. Switching left and right
153. Transposition (reversal) of numbers, words and/or letters when you speak
154. Transposition (reversal) of numbers, words and/or letters when you write
155. Trouble concentrating
156. Using the wrong word
157. Word-finding difficulty
EMOTIONAL
158. Abrupt and/or unpredictable mood swings
159. Anger outbursts
160. Anxiety or fear when there is no obvious cause
161. Attacks of uncontrollable rage
162. Decreased appetite
163. Depressed mood
164. Feeling helpless and/or hopeless
165. Fear of someone knocking on the door
166. Fear of telephone ringing
167. Feeling worthless
168. Frequent crying
169. Heightened awareness – of symptoms
170. Inability to enjoy previously enjoyed activities
171. Irrational fears
172. Irritability
173. Overreaction
174. Panic attacks
175. Personality changes –usually a worsening of pervious condition
176. Phobias
177. Suicide attempts
178. Suicidal thoughts
179. Tendency to cry easily
GASTROINTESTINAL
180. Abdominal cramps
181. Bloating
182. Decreased appetite
183. Food cravings
184. Frequent constipation
185. Frequent diarrhea
186. Gerd-like Symptoms
187. Heartburn
188. Increased appetite
189. Intestinal gas
190. Irritable bladder - "Angry Bladder Syndrome"
191. Irritable bowel syndrome - IBS-C, IBS-D
192. Nausea
193. Regurgitation
194. Stomachache
195. Vomiting
196. Weight gain - unexplained
197. Weight loss - unexplained
UROGENITAL
198. Decreased libido (sex drive)
199. Endometriosis
200. Frequent urination
201. Impotence
202. Menstrual problems
203. Painful urination or bladder pain - "Interstitial Cystitis"
204. Pelvic pain
205. Prostate pain
206. Worsening of (or severe) premenstrual syndrome (PMS or PMDD)
SENSITIVITIES
207. Alcohol intolerance
208. Allodynia (hypersensitive to touch)
209. Alteration of taste, smell, and/or hearing
210. Sensitivity to chemicals in cleaning products, perfumes, etc.
211. Sensitivities to foods
212. Sensitivity to light
213. Sensitivity to mold
214. Sensitivity to noise
215. Sensitivity to odors
216. Sensitivity to yeast (getting yeast infections frequently on skin, etc.)
217. Sensory overload
218. Sensitivity to pressure & humidity changes
219. Sensitivity to extreme temperature changes
220. Vulvodynia
SKIN
221. Able to “write” on skin with finger
222. Bruising easily
223. Bumps and lumps
224. Eczema or psoriasis
225. Hot/dry skin
226. Ingrown hairs
227. Itchy/Irritable skin
228. Mottled skin
229. Rashes or sores
230. Scarring easily
231. Sensitivity to the sun
232. Skin suddenly turns bright red
CARDIOVASCULAR (Heart)
233. “Click-murmur” sounds through stethoscope
234. Fluttery heartbeat
235. Heart palpitations
236. Irregular heartbeat
237. Loud pulse in ear
238. Pain that mimics heart attack - "Costochondritis"
239. Rapid heartbeat
HAIR/NAILS
240. Dull, listless hair
241. Heavy and splitting cuticles
242. Irritated nail beds
243. Nails that curve under
244. Pronounced nail ridges
245. Temporary hair loss
OTHER
246. Canker sores
247. Dental problems
248. Disk Degeneration
249. Hemorrhoids
250. Nose bleeds
251. Periodontal (gum) disease
252. Need for early hysterectomy
#fibromyalgia#chronic pain#chronic illness#chronically ill#invisible illness#spoonie#pwd#disability#hidden disability#sharing is caring#disorder#neurological disorder#central nervous system#nervous system disorder#mental health#health#awareness
189 notes
·
View notes
Text

I DIDN'T KNOW BUT HAPPY NATIONAL MIGRAINE AWARENESS MONTH.
Things that I learned since having migraines.
They can change. You can go years without migraines, but then suddenly get them again.
Symptoms and triggers can change. You may think you don't got it that bad because you don't have the worst of the symptoms but then one day you suddenly got vertigo and vomiting.
Migraines impact the trigeminal nerve which is the same nerve impacted my TMJ pain, sinus headaches, trigeminal neuralgia, and cluster headaches. It's the biggest nerve in the face so it's pretty common to have multiple of these conditions at once.
Migraines can be triggered my barometric pressure shifts, flashing lights, sounds, and smells.
You can have migraines without aura or visual disturbances. These are harder to treat because most migraine medications require you to take them during the aura phase.
You can have what's called an "abdominal migraine" which is characterized my extreme stomach pain. This usually impacts adolescents.
You can have what's called a "silent migraine" which is characterized as migraines without the headache. In fact headache isn't even the most common migraine symptom based on a poll I've done.
Migraines can be highly tied into your allergies. Not just in the fact that sinus headaches and migraines trip the same nerve, but in the fact that your allergies can be a migraine trigger.
Migraines can make you more susceptible to alcohol especially when you're dealing with migraines triggers frequently.
Fluorescent lights are actually very bad for people with migraines because it's essentially flashing so fast you can't see it with the human eye (but trust me your migraines will know it's there).
It's actually very common for people with migraines to have heightened senses of smell, higher sensitivity to lights/sounds, etc. Some people have even noted that people with certain medical conditions have different smells.
Chronic migrains are obviously a disability but episodic migraines can be considered a dynamic disability (a disability where your needs fluctuate)
Migraine preventatives are different from migraine abortives. Doctors will usually only prescribe preventatives if you have chronic migraines or have a certain number of migraines a month.
15 migraine days a month is the number you're looking for to be considered chronic.
It's actually pretty common to be craving salt or carbs after a migraine. And listening to those cravings can actually reduce postdrome symptoms
Migraines come in 4 phases. Prodrome (irritability, fatigue, etc before the migraine), aura (visual disturbances), migraine, and postdrome (fatigue, dizziness, etc after the migraine).
The most common migraine meds are called triptans and shouldn't be taken with antidepressants because it can cause serotonin overdose syndrome.
Migraine aura isn't limited to visual disturbances. It can include phantom taste and smell (smelling or tasting things that aren't there)
People that have migraines are more likely to deal with heat intolerance
A lot of the "it's a migraine if you experience pain on this side of the head" is complete garbage. Migraines are characterized by a complex set of neurological symptoms of which doesn't always include headaches.
-fae
202 notes
·
View notes
Text
Self-massage and Myofascial Pain: From Head to Fingers
Aka I'm going to talk about a muscle that is neither in the head or the fingers. It's a neck muscle called the sternocleidomastoid.
(STER-no-KLY-do-MAST-oid, or SCM for people who don't take joy in pronouncing long, confusing words.)
I am not a professional massage therapist, just a professional don't-wanna-be-in-pain guy.
This one is for...everyone. Or just about. The SCM can contribute to a vast, VAST variety of pains. Here's a sampling:
A variety of headaches (in the eye, above the eye, top of the head)
Jaw problems (including Temporomandibular Joint (TMJ) Dysfunction, stiffness, clicking)
Neck pain
Ear aches
Toothaches
And they also contribute to and are perpetuated by a foreward head posture--something that anyone who uses a phone or computer should be familiar with. Foreward head posture can further contribute to symptoms such as:
Shoulder pain
Upper back pain
Chest pain
And arm and hand pain, including symptoms similar to tendonitis, carpal tunnel syndrome, cubital tunnel syndrome, grip weakness, and much more.
See why this one applies to everyone?
Now, full disclaimer, I'm hesitant to make this the second trigger point I talk about because neck muscles are extremely sensitive. However, I'm still reaping the benefits of having finally bitten the bullet and trying this myself, and it feels important to make this one of the first I talk about.
That said, this is your first of many warnings. Go easy on these muscles. Gentle massage is better than no massage.
Here's a quick few rules:
Don't massage the SCM more than 3 times a day. In fact, if you find they are very sensitive, I recommend once a day and right before bed or a nap.
As always, never massage a pulse.
If you feel dizzy or faint, release all pressure until you regain your bearings.
Do this massage with your eyes open and sitting up. It will help you maintain awareness.
Never use massage tools on your neck.
For those with anxiety: I know this sounds nerve-wracking. As long as you go slow and listen to your body, you won't hurt yourself. If you accidentally squeeze the wrong place, it's not the end of the world! Just release pressure, move your fingers, and try again. It's only deep and extended pressure that will get you into trouble, okay?
With all that said, let's get to the good stuff.
The SCM muscles are the ones that make that sexy little V on the neck, connecting from behind the ear down to the collarbone. For all the trouble they cause, they rarely hurt themselves, which is why they get overlooked.
You've got two on each side. One in front, and one deeper in the neck. I'll teach you how to get at both.
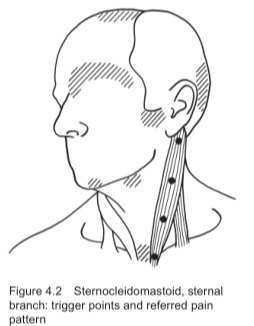
We'll start with the guy up front. Here's a snazzy little pictogram courtesy of The Trigger Point Therapy Workbook.
The shaded areas are (some of) the pain patterns caused by this muscle. The dots are meant to represent trigger points (TrPs), but the reality is that they can occur along the full length.
As a rule of thumb, TrPs further up cause more symptoms in the head. Further down contributes to everything below. This goes for both the shallow muscle and the deeper muscle.
Find somewhere to sit straight and relax your body.
Use your fingers to find your pulse on your chosen side, between the SCM and the windpipe. If your fingers aren't sensitive enough to feel your pulse, you should not do this massage yourself.
Move to the SCM side of your pulse, replace your fingers with your thumb.
Grasp the SCM lightly with your fingers and thumb, firstly just to find where you will be working. The SCM is not large, probably around the width of your finger, so don't reach too far back. If you're having trouble grasping it, look Away from the side you're working on, then tilt your head Towards it.
Now that you're familiar, make a C with your grasp fingers so that it's the tips holding the muscle. The intent is to exert more pressure with less effort. Make sure your fingernails are short for this.
Now slowly, keeping your grip light, you want to...well, the easiest way I can describe it is that your want to milk the SCM. Use short strokes, releasing the pressure at the end of each. You can massage all the way up to the ear, and all the way down to the collarbone.
Again, go easy. If you're like me, this will be painful at first. You might even feel a little brain fucked from doing this, but as long as you aren't feeling faint or dizzy, you're good to go. Don't push yourself--take a break when you've had enough.
Afterwards, lightly stretch this muscle by turning your head to the side three times.
And now for the deeper SCM.
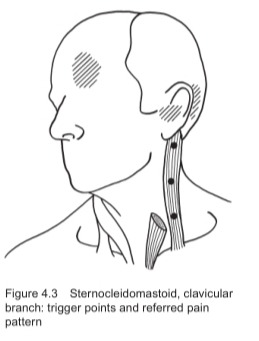
This guy isn't any harder than the shallow one. In fact, I don't even need to give you an entire list of instructions. Follow the steps above, but when you grasp the muscle, you instead want to take a larger fingerful, closer to the width of two fingers.
To help you understand what I'm getting at, put your fingertips on the back side of your neck, a small ways down and behind your ear. Gently dig in and pull forward--everything you can grasp from this point to your windpipe comprises both SCM muscles. All you need to do is grasp this entire chunk of muscle and perform the massage as described above.
With continued massage, you should gradually feel less tension in your jaw, neck, and shoulders. Your head might feel a bit clearer, you might have fewer and less intense headaches. Keep doing this massage until you can't find any tender points in the SCM.
And as a preventative--try to find ways to keep yourself from slouching or holding your head forward. A simple exercise is to pull your head back, like you're giving yourself an extra chin.
If you're interested in more posts like this, check out these links:
Low Back Pain
Massage Tips and Techniques
27 notes
·
View notes
Text
Happy Disability Pride Month!
In honor of the shift from LGBTQ Pride Month to Disability Pride Month, I’m going to bring awareness to some underrepresented and underinformed disabilities as a queer and disabled artist/writer. These are all disorders that I have come across among friends and acquaintances. Every disorder I discuss must have a clinical diagnosis in order to be treated. You should only be self-diagnosing if you plan on going to a doctor to confirm your speculations. Do not self-diagnose if you are not willing to confirm with a medical professional. This post is not to diagnose you.
Big Trigger Warning: Discussions of psychological disorders like E/Ds, depression, and personality disorders.
Dysautonomia
Any disorder relating to the autonomic (involuntary) nervous system
POTS
I have this! It is a nervous system disorder that affects heart rate and blood pressure because your nervous system does not allow your muscles to properly circulate blood, especially through the legs. Some symptoms include elevated heart rate, chest pain, low or high blood pressure, fatigue, changes in body temperature, and dizziness or fainting. POTS is more common in AFAB people than AMAB.
Amyloidosis
Amyloidosis is a disorder that occurs when a protein known as amyloid builds up in the organs. Amyloidosis is closely related to dysautonomia and chronic pain syndromes such as Ehlers-Danlos Syndrome because of the comorbid symptoms. These symptoms include edema, purpura around the eyes, skin that bruises easily, and fatigue.
Frey’s Syndrome
A neurological disorder closely related to dysautonomia that causes excessive sweating while eating. There are very few solutions to this disorder and even fewer of them are known to work.
Mitochondrial Syndrome
Mitochondrial diseases occur when there are genetic mutations and deformations to the mitochondria in cells that directly influence how the organelle produces energy. People with mitochondrial diseases can have poor growth, muscle weakness, seizures, visual and / or hearing problems, learning disabilities, and may develop kidney, liver, or heart disease.
Autonomic Dysreflexia
Autonomic dysreflexia is a disorder that causes abnormal overreactions of the autonomic nervous system. Symptoms include elevated heart rate, excessive sweating, and high blood pressure.
Chronic Pain
Any disorder relating to long-lasting pain surrounding any part of the body.
Patellofemoral Pain Syndrome
I have this one too! Patellofemoral pain syndrome is a chronic pain syndrome in which muscles in the lower extremities are too weak to support patellar (kneecap) movement. Thus, the patella (kneecap) will not track right. this causes lots of issues with walking.
Scoliosis
I also have this one! Scoliosis is defined as a physical disorder in which the spine is not a straight vertical line. There is either an “S” or “J” curve in the spine, compressing it and causing sharp or aching back pain.
Temporomandibular Joint Dysfunction
TMJ causes pain and tenderness in jaw joints and surrounding muscles and ligaments. Symptoms of TMJ include jaw stiffness, limited movement and locking of the jaw, ringing in ears, and dizziness.
Myofascial Pain Syndrome
This is a chronic muscular pain disorder. Typically, this pain is confined to one specific area, such as the neck or shoulders.
Fibromyalgia
A chronic disorder that causes pain and tenderness throughout the body, as well as fatigue. People with fibromyalgia can also have depression, anxiety, and trouble with memory and concentration.
Ehlers-Danlos Syndrome
EDS is a group of disorders that affect connective tissues that support the skin, bones, blood vessels, organs, and other tissues. Symptoms of EDS include stretchy, translucent skin, loose joints, and chronic pain.
Arthritis
Arthritis is defined as inflammation in one or more joints causing stiffness and pain. There are many different kinds of arthritis, each with different causes. These causes can include wear over time, infections, and underlying diseases.
Neurological Disorders
Any disorder relating to the brain and how it functions.
Seizure Disorders
Epilepsy
Epilepsy is a disorder of the brain characterized by repeated seizures. People with epilepsy can experience multiple kinds of seizures and can experience symptoms such as confusion, staring spells, stiff muscles, and loss of consciousness.
Cerebrovascular Diseases
Functional Neurological Disorder
Functional Neurological Disorder is essentially a stroke mimic. It can replicate the symptoms of a stroke, such as limb weakness, numbness, and speech disturbance.
Migraines
Lots of people have migraines and I am no exception. Migraines are caused by excessive blood flow to the brain. Migraines affect more than 10% of people worldwide and are 3 times more likely to affect AFAB people than AMAB people.
Psychological Disorders
Any disorders affecting mood, thinking, and behavior. I will not be discussing my mental disorders on the internet. Most people are familiar with what these are and what they look like, so I will instead be providing statistics for each one.
Anxiety Disorders
Generalized Anxiety Disorder (GAD) affects 6.8 million adults. Only 43.2% of those adults are receiving treatment. AFAB are twice as likely to be affected (Anxiety Disorders Association of America).
Panic disorder (PD) affects 6 million adults. AFAB are twice as likely to be affected (Anxiety Disorders Association of America) .
Obsessive-Compulsive Disorder (OCD) affects 2.5 million adults. AFAB are 3x more likely to be affected (Anxiety Disorders Association of America) .
Post-Traumatic Stress Disorder (PTSD) affects 7.7 million adults. AFAB are 5x more likely to be affected (Anxiety Disorders Association of America) .
Depression
Approximately 280 million people in the world have depression. AFAB are twice as likely to develop depression (World Health Organization).
Bipolar Disorder
4.4% of US adults experience bipolar disorder in their lives (National Institute of Health).
Personality Disorders
It is estimated that 9% of US adults have at least one personality disorder (American Psychiatric Association).
Eating Disorders (TW)
Eating Disorders affect 9% of the population worldwide (National Association of Anorexia Nervosa and Associated Disorders).
BIPOC are significantly less likely than white people to be asked by a doctor about eating disorder symptoms (National Association of Anorexia Nervosa and Associated Disorders).
Black teenagers are 50% more likely than white teenagers to exhibit bulimic behaviors (National Association of Anorexia Nervosa and Associated Disorders).
Rates of body dissatisfaction were higher among transgender and nonbinary youth (90%) compared to cisgender youth (80%) (National Association of Anorexia Nervosa and Associated Disorders).
#disability pride month#disability awareness#disability#dysautonomia#pots#chronic pain#neurological disorder#psychological disorders
15 notes
·
View notes
Text

Hormones and their Interaction with the Pain Experience (Katy Vincent and Irene Tracey, 2008)
"One of the most striking physiological differences between men and women is in sex steroid hormones, both the absolute levels and the occurrence of cyclical fluctuations in women.
These hormones are known to be responsible for the embryological development of a male or female phenotype and for successful reproductive function after puberty.
More recently, observations such as the marked differences in pain symptoms between males and females in the period between puberty and the menopause, and the cyclical variations in many clinical pain symptoms in women have suggested that they may also have a role in altering the pain experience. (…)
With the onset of regular ovulation and menstruation, it can be seen that a number of clinical pain conditions show variation in symptom severity across the menstrual cycle.
Clearly the pain of dysmenorrhoea is, by definition, associated with the menstrual cycle, however, the symptoms of temperomandibular joint (TMJ) dysfunction, fibromyalgia, Irritable Bowel Syndrome (IBS), Interstitial Cystitis (IC) and migraine can also show cyclical variation.
The greatest reports of pain symptoms appear to occur at times of low or rapidly falling estrogen levels and the use of the combined oral contraceptive pill (COCP) to give a more constant hormonal level can improve these symptoms. (…)
From puberty onwards, men have significantly higher levels of testosterone and its metabolites than women.
Testosterone appears to have an analgesic effect protecting against the development of painful conditions such as TMJ pain.
Rheumatoid arthritis patients (both male and female) have been shown to have lower androgen levels than sex-matched controls, and androgen administration improves their symptoms, whilst female workers with lower testosterone levels have more work-related neck and shoulder injuries.
However, investigation of the specific effects of testosterone are complicated by the fact that much is metabolised in vivo to estradiol by aromatase, and this is therefore an issue which needs to be addressed in future studies.
Perhaps one of the more intriguing studies to be published recently explored the effect of systemic hormone administration to both male to female (MtF) and female to male (FtM) transsexuals (n=73) during the process of sex reassignment.
They observed that approximately one third of the MtF subjects developed chronic pain during their treatment with estrogen and androgens, and even those that did not, reported a decreased tolerance to painful events and an enhanced sensitivity to thermal stimuli (both warm and cold).
Of those FtM subjects who had chronic pain before the start of treatment, more than half improved after commencing testosterone treatment, reporting reduced numbers of painful episodes and shorter lengths of those that did occur.
Clearly, psychological effects cannot be ignored in this group of subjects, however, this is the only situation where the hormonal milieu in humans can be ethically altered to that of the opposite gender and therefore gives us interesting insights. (…)
In addition to its sensory aspect, pain is an emotional experience.
It is therefore of interest that the life time patterns in pain symptoms in men and women are closely mirrored by those of mood disorders, though with the addition of a perimenopausal peak in mood disorders.
Comparing post-puberty with pre-puberty, rates of significant depression increased two-fold for boys but more than four-fold for girls.
In Premenstrual Dysphoric Disorder (PMD), there is no evidence that abnormal levels of hormones occur (unlike in depression associated with thyroid or pituitary dysfunction), rather, it appears that some women are more sensitive to the mood destabilising effects of these hormones.
It is not inconceivable therefore, that a similar situation may exist for pain."
6 notes
·
View notes
Note
this might be a very weird question bc i dont know how to word this but. i have tmj and im pretty sure i have hypermobility joint syndrome (not diagnosed?, my family has a history of it) but im not sure how to bring it up and a doctors appointment is expensive. its currently at a point where im constantly in some form of pain, especially in my knees and my fingers- im trying to save up for compression gloves or knee braces bc the pain is so overwhelming. everyone i know is able bodied so i dont really have anyone to go to for advice, where do you think i should go from here?? (sorry if this is a bother!! feel free to delete this i know its a lot)
This is a difficult one to answer. I'm honestly not that knowledgeable about the diagnostic process for a lot of conditions, mostly because I was diagnosed with my issues so young that my mom and grandma did all the work. I haven't officially been diagnosed with anything since, even though I believe I have undiagnosed issues (an autoimmune thyroid condition being one of those).
Have you brought it up with your family at all? You could tell them that you've been experiencing symptoms.
Just because you're undiagnosed doesn't mean you don't have a certain condition. Unless it becomes a severe issue, you don't have to get diagnosed right away, especially since you may not be able to afford it. Remember that diagnoses can take a very long time in some cases. Sometimes they even take decades. I was diagnosed quickly, but that was because my family already had experience and my grandma and mom are very stubborn and fought for me.
I'd recommend bringing it up to your family. If you can't get diagnosed, maybe try speaking with those in your family who have that condition, if possible. Get their advice, their perspective, ask about their experience, etc. Do some online research on it and ways you can help yourself. Go onto social media and search for people who have that condition.
And if you think some sort of aid will help you, definitely save up for one. You don't need a diagnosis to get things that will help you. Plenty of undiagnosed disabled people buy themselves mobility aids in order to help them. So if you firmly believe that something is wrong with your joints, don't let your lack of a diagnosis control you and stop you from doing something to help yourself.
Diagnoses are a thing of the modern era. Diagnoses like we have now haven't always existed. Modern medicine isn't as old as many people think it is. And many of these conditions are lesser known. Which means that even if you were able to go to a doctor, medical gaslighting is still possible, even for those who actually have a diagnosis.
I have a friend who has been diagnosed with multiple disabilities, multiple chronic illnesses who was told by a doctor that she was faking, even though she has a bunch of diagnoses. So that's just one of many obstacles you could run into when attempting to get a diahnosis.
I hope this helps
If anyone else has any tips for this user, please comment 😁
#cripple punk#cripplepunk#crip punk#cpunk#physically disabled#physical disability#physical disabilities
8 notes
·
View notes
Text
I have a pt who has apparent status migrainosus. But it's been resistant to sumatriptan. She said she had some relief with IV meds in the ED (I believe she got depakote or valproate). I wonder if it might actually be 2/2 temporomandibular joint arthritis, which she was diagnosed with a month ago. That's what my preceptor mentioned. So I looked up TMD on UpToDate:
Pathogenesis – Several factors can contribute to the development of temporomandibular disorder (TMD) symptoms, including temporomandibular joint (TMJ) trauma, poor head and cervical posture, differences in pain threshold and processing, and psychological factors such as depression and anxiety.
●Clinical manifestations – Symptoms of TMD most commonly include facial pain: a dull, unilateral facial ache that is constant but waxes and wanes in intensity and is typically aggravated by jaw motion. Other common symptoms include earache, headache (typically frontal or temporal and often radiating to the jaw), and jaw and TMJ dysfunction (eg, decreased mandibular range of motion, clicking with jaw movement, intermittent jaw locking).
●Evaluation and diagnosis – The diagnosis of TMD is based primarily upon the history, including the patient's constellation of symptoms, and compatible physical examination findings. For patients with more severe symptoms and those with persistent symptoms, we obtain imaging to rule out local pathology in the teeth and jaw bones; a panoramic radiograph or cone beam computed tomography (CBCT) are both reasonable choices. We advise against the routine use of a standard radiograph of the TMJ, as this study does not provide valuable information regarding dentition and mandibular alignment and symmetry.
●Initial management with patient education and self-care measures – For all patients with TMD, we suggest initial management with education and self-care measures (Grade 2C). This includes education regarding the natural history of TMD and counseling on optimal head posture, jaw exercises (picture 2 and picture 3*), and proper sleep hygiene, as well as avoidance of triggers (eg, oral behaviors such as nail biting, pen chewing) if these factors contribute to symptoms. There are limited high-quality data supporting the use of self-care and education in the treatment of TMD; however, given the lack of harm and the potential benefit, these interventions are appropriate for all patients.
*Isometric jaw exercises are particularly useful for patients with temporomandibular joint dysfunction syndrome. These exercises are performed by applying resistance with an open or loosely fisted hand. In the isometric jaw opening exercise, the patient begins with her mouth open about an inch. The resistance and muscle contraction are held for 5 to 10 seconds before relaxing. This is repeated five times per session. Exercises can be performed with moderate resistance applied several sessions per day, or with maximum resistance one session per day.
*The isometric jaw forward thrust exercise is performed by pushing the jaw forward against the hand, holding and then relaxing. This is repeated five times per session.
•Physical therapy for musculoskeletal causes – For patients with a prominent musculoskeletal component or cervical or shoulder symptoms, we refer for physical therapy evaluation and treatment.
•Oclusal (bite) splints as adjunctive therapy – For some patients with TMD, particularly those with prominent musculoskeletal symptoms or evidence of bruxism, occlusal splints fitted by a dental clinician can be used as an adjunctive therapy along with other TMD treatments such as physical therapy.
•Biobehavioral management for comorbid psychological conditions – For patients with comorbid depression, anxiety, and stress disorders, biobehavioral management is used as adjunctive therapy in TMD treatment.
●Adjunctive pharmacotherapy for persistent symptoms – For patients with persistent symptoms despite education and self-care, we use adjunctive pharmacotherapy concurrently with other treatments.
•For such patients, we suggest using a nonsteroidal antiinflammatory drug (NSAID) as first-line pharmacologic therapy rather than other medications (Grade 2C). We generally treat patients with a 10- to 14-day course of a long-acting NSAID (eg, naproxen 250 to 500 mg orally twice daily).
•For patients with tenderness of the muscles of mastication, we suggest treatment with a skeletal muscle relaxant in addition to the NSAID (Grade 2C). For most patients, we prescribe the muscle relaxant for 10 to 14 days only. However, some patients with persistent muscular pain may benefit from an additional week of treatment.
•For patients with persistent TMD symptoms that warrant continued adjunctive pharmacotherapy after two weeks of NSAID treatment (or three weeks for those patients taking additional skeletal muscle relaxants), we suggest treatment with a tricyclic antidepressant (TCA) rather than other therapies (Grade 2C).
●Interventional management for severe or refractory symptoms – For patients with TMD symptoms refractory to noninvasive management, referral to an oral and maxillofacial surgeon with experience in managing TMD is warranted. Treatment options for these patients include trigger point muscle injections, botulinum toxin injections, and intraarticular injections.
●Surgical referral for refractory symptoms despite nonsurgical interventions – For some patients, such as those who have structural anatomic pathology on imaging and persistent jaw locking severe enough to interfere with activities of daily living despite three to six months of nonsurgical management, we suggest surgical intervention rather than no surgery (Grade 2C). Although the specific surgery offered will depend upon the intraarticular disorder, such patients are unlikely to achieve adequate symptom control without surgical intervention.
5 notes
·
View notes
Text
Health Anxiety
I am scared that I may have fibromyalgia and am wondering how common it is, as well as autoimmune diseases (rheumatoid arthritis or lupus) following recovery for AN.
I’m about 1 year into recovery right now from AN, and I am so grateful for growth. But about 2 months ago I started noticing stiffness in my leg muscles and shoulders along with Raynaud’s syndrome (white fingers/toes).
Since then, symptoms feel like they have worsened to daily joint pain (thumbs, wrists, neck, shoulders, hips, ankles/feet) and sore muscles/tendons (legs, arms, back, TMJ symptoms, no chest pain).
I never had health anxiety before recovery, but now I cant stop worrying if I did irreparable damage and will have to suffer the consequences my whole life. I have spent prob upwards of $150 this past month on vitamin B, D, magnesium, potassium, calcium, and iron bc the internet told me deficiencies in these vitamins commonly cause the symptoms I described, and I am desperate.
I’m torn between seeing a doctor or not because I worry its all in my head, and I can’t bear to pay almost $100 to be told that in a 5-min visit. I know the mind is so powerful over the physical body, and can’t help but think this chronic pain is from stressing myself out about the pain. But in my hours and hours I have accumulated researching on the internet, I read at least 10-15 blog posts of post-recovery patients who spent years trying to decode the same symptoms as me, and finally learned they had fibromyalgia or arthritis.
Im just rambling now, but It would mean the world and more if anyone reading this can take the poll or share any related info/stories/suggestions related to post-recovery pain and fatigue (can dm/pm if u want to! I am craving some support from my fellow soldiers right about now♡♡♡
3 notes
·
View notes
Text
10 Surprising Benefits of Regular Massage Sessions
Introduction:
In a world where stress seems to be an inevitable part of daily life, finding effective ways to unwind and take care of ourselves is crucial. While many of us may turn to traditional methods like exercise or meditation, one often overlooked avenue for relaxation and rejuvenation is regular massage therapy. Beyond its reputation for providing temporary relief from muscle tension, massage offers a myriad of surprising benefits that can positively impact both our physical and mental wellbeing. Let's delve into 10 lesser-known advantages of incorporating regular massage into your self-care routine.출장안마
Boosts Immune Function:
Research suggests that regular massage sessions can bolster the immune system by increasing the activity of natural killer cells, which play a key role in defending the body against illness and infection. By stimulating the lymphatic system, massage helps to flush out toxins and enhance the body's ability to fight off pathogens.
Improves Posture:
Sitting for prolonged periods can wreak havoc on our posture, leading to muscle imbalances and structural issues. Regular massage therapy can help alleviate muscular tension and realign the body, promoting better posture over time. By targeting specific muscle groups, massage encourages proper alignment and reduces the risk of developing postural problems.출장마사지
Enhances Cognitive Function:
Beyond its physical benefits, massage therapy has been shown to have positive effects on cognitive function. By reducing stress hormones like cortisol and increasing levels of serotonin and dopamine, massage promotes feelings of relaxation and mental clarity. This can lead to improved concentration, memory retention, and overall cognitive performance.
Alleviates Symptoms of Seasonal Allergies:
For allergy sufferers, regular massage sessions may offer unexpected relief from symptoms such as congestion, sinus pressure, and headaches. By stimulating circulation and lymphatic drainage, massage helps to clear nasal passages and reduce inflammation, providing natural relief from seasonal allergies.
Supports Digestive Health:
The gut-brain connection is a powerful force in our overall health, and massage therapy can play a role in supporting digestive function. By reducing stress and promoting relaxation, massage can help alleviate symptoms of digestive disorders such as irritable bowel syndrome (IBS) and bloating. Additionally, abdominal massage techniques can stimulate peristalsis and improve gastrointestinal motility.
Promotes Deeper Sleep:
If you struggle with insomnia or poor sleep quality, regular massage sessions may offer a solution. Massage has been shown to trigger the release of serotonin and melatonin, hormones that regulate sleep-wake cycles and promote relaxation. By reducing muscle tension and calming the nervous system, massage can help you achieve deeper, more restorative sleep.
Boosts Athletic Performance:
Athletes and fitness enthusiasts can benefit greatly from incorporating massage therapy into their training regimen. Regular massage sessions help prevent injury by reducing muscle tension and improving flexibility. Additionally, massage can speed up recovery time between workouts by enhancing circulation and flushing out metabolic waste products from muscle tissue.
Relieves Symptoms of Temporomandibular Joint (TMJ) Disorder:
Temporomandibular joint disorder, or TMJ, can cause a range of painful symptoms including jaw pain, headaches, and difficulty chewing. Massage therapy can help alleviate these symptoms by relaxing the muscles of the jaw and neck, reducing tension and improving range of motion. By addressing muscular imbalances and trigger points, massage offers natural relief from TMJ discomfort.
Supports Emotional Wellbeing:
In addition to its physical benefits, massage therapy has powerful effects on our emotional health and wellbeing. By promoting the release of endorphins and oxytocin, often referred to as the "feel-good hormones," massage can help reduce symptoms of anxiety, depression, and stress. The nurturing touch of massage therapy fosters feelings of connection, safety, and relaxation, promoting emotional balance and resilience.
Boosts Creativity and Problem-Solving Skills:
Need a creative boost or a solution to a challenging problem? Regular massage sessions may be the answer. By inducing a state of deep relaxation and quieting the mind, massage therapy can enhance creativity and improve problem-solving skills. Many people report experiencing breakthrough insights and innovative ideas during or after a massage session, making it a valuable tool for fostering creativity and innovation.
Conclusion:
While the benefits of regular massage therapy are well-documented, there are many surprising advantages that often go overlooked. From boosting immune function and improving cognitive performance to relieving symptoms of TMJ disorder and supporting emotional wellbeing, massage offers a holistic approach to health and wellness. By incorporating regular massage sessions into your self-care routine, you can experience these unexpected benefits and enhance your overall quality of life.
0 notes
Text
WHAT WE TREAT
We offer treatments across neuro /ortho / pediatrics /sports related issues using approved procedures in Physiotherapy, Chiropractor, Dry Needling, Kinesiology etc.
CONDITIONS
Varicose Veins
Popliteal (Baker's) Cyst
Posterior Cruciate Ligament(PCL) Injury
Lateral Collateral Ligament(LCL) Injury
Medial Collateral Ligament (MCL) Injury
Patella Dislocation
Patellar Fracture
Meralgia Paresthetica
Hip Osteoarthritis
Hip Impingement
Hip Labral Tear
TROCHANTERIC BURSITIS
Hip Fracture
Radial Tunnel Syndrome
Biceps Tendonitis
Cubital Tunnel Syndrome
De Quervain's tenosynovitis
Burns
Ganglion Cyst
Boutonniere Deformity
Mallet Finger
Hand Fractures
Wrist Fracture
Forearm Fractures
Elbow Fractures
Shoulder and Arm Fractures
Shoulder Dislocation
TORTICOLLIS
Down Syndrome
Spina Bifida
SPRENGEL'S SHOULDER
ERB’S PALSY
MENISCAL INJURY
Total Hip Replacement (THR)
Total Knee Replacement(TKR)
Fibromyalgia Syndrome
Hamstring Strain
Clubfoot or Congenital Talipes Equinovarus or CTEV
Stroke or Cerebrovascular accident (CVA)
Temporomandibular Joint (TMJ)
Asthma
Distal Muscular Dystrophy
Degenerative Disc Disease
Diabetic Neuropathy
Herniated Disk or Slipped Disc
Myasthenia Gravis (MG)
Tendinitis
Piriformis syndrome
Tailbone Pain/Coccydynia
Rheumatoid Arthritis
Spinal Stenosis
Concussion
Plantar Fasciitis
Dementia
Bell's Palsy or Facial Palsy
Scoliosis
Rotator Cuff Injury
Whiplash
Osteoporosis
Cervical Myelopathy
Osteoarthritis
Baastrup syndrome
Tennis Elbow
Parkinson's Disease
Sciatica
Cerebral Palsy
Ankle sprain
Anterior Cruciate Ligament Tear
Knee Bursitis
Chondromalacia Patella
Arthritis
Carpal Tunnel Syndrome (CTS)
Achilles Tendon Rupture
Vertigo
Frozen Shoulder
Cervical Spondylosis
Lumbar Spondylosis
SYMPTOMS
Muscle Spasm
Tremors
Joint Cracking
Foot Pain
SPRAINS AND STRAINS
Shortness of Breath
Headache
Numbness and Tingling
Inflammation
Loss of Balance
Muscle Stiffness
Shoulder Pain
Joint Pain
Neck Pain
Back Pain
Knee pain
OUR OFFERINGS
At drsinghphysiocare (DKPS) we use physio care approach providing a combination of therapies for comprehensive healing.appoved modalities are used only
0 notes
Text
Knowing How Bruxism Affects Your Teeth, Jaws, and Oral Structures - Align Dental Care

The general definition of bruxism is a forceful clenching and tiny motions between the upper and lower teeth (grinding). The extraordinarily strong forces of the masticatory muscles can be used independently of the chewing process during these motions.
Therefore, this exposure can lead to dental issues such the development of pits in the enamel close to the gum line, increased sensitivity, tooth mobility, pain while biting, and issues with the jaw joint. The subject of mental stress and emotional illnesses has been discussed by researchers who have long studied bruxism. There is also discussion of the possibility that aggression is to blame for the considerable deterioration of several brain regions associated with norepinephrine synthesis and stomach ulcer development in experimental animals.
The idea of stress management is founded on the psychological foundation for which bruxism is a manifestation, as well as the advantages of masticatory muscle action in reducing stress-related symptoms such stomach ulcers. People who bruxise clench and move their teeth as an emergency response to deal with tension during times of mental hardship.
Bruxism's various manifestations
Bruxism can have one of two forms:
Teeth grinding, jaw misalignment, thumb sucking, and lip biting during the day (bruxomania).
Night: A more severe form that encourages tooth wear, has a strong detrimental effect on enamel, and puts more strain and tension on the jaw. This illness must and can be fought. A specific Botox is used to inject into the jaw to restore normal function.
Reasons for bruxism
Bruxism is a complicated illness with several probable causes, including
persistent anxiety and stress
inappropriate orthodontic care with braces due to malocclusion dysfunction of the autonomic nervous system inflammation of the facial nerve
antidepressants and psychotropic medication side effects
problems of the nervous system or endocrine system: hyperthyroidism, Raynaud's syndrome, and Parkinson's disease
a genetic disposition
A child teething A man who grinds his teeth
Signs of bruxism
The first step to effective management of bruxism can be recognizing the symptoms and indicators of the condition. Some signs could be:
teeth grinding, chattering, or creaking at night
headaches, jaw, face, and neck pain, increased sensitivity of teeth, enamel erosion, cracks, and cavities, as well as a weakening and erasure of teeth
difficulty expanding the mouth
tongue, palate, or cheek mucous membrane discomfort
insomnia, worry, sadness, and exhaustion brought on by inadequate sleep and ongoing pain
Bruxism's Effects On Teeth, Jaws, And Oral Health
Effects of bruxism over time
Untreated bruxism can have serious long-term effects, including significant harm to the mouth. Continuous grinding wears down dental enamel, increasing tooth sensitivity, causing permanent tooth damage, and even causing tooth loss. Temporomandibular joint (TMJ) disorder, which causes discomfort and dysfunction in the jaw joint and the muscles that control jaw movement, can occur as a result of excessive pressure on the jaw muscles and joints. In severe cases, untreated bruxism can alter the structure and look of the face over time as a result of ongoing muscular stress.
Dental bruxism and harm
One of the main reasons for dental injury is bruxism. Due to the tremendous pressure and friction, grinding can result in tooth loss, fractures, and even tooth loosening. Dental restorations like crowns, bridges, implants, and fillings are susceptible to damage or displacement from excessive pressures. It is important to keep in mind that this kind of injury puts the teeth's functionality and appearance in danger, possibly making chewing and speaking more challenging. Additionally, repair can occasionally be difficult and expensive, which emphasizes the importance of early bruxism detection and management.
Bruxism and general well-being
In addition to oral health issues, bruxism can result in a number of other serious health issues. Notably, it increases the likelihood of developing temporomandibular joint (TMJ) issues, which can be extremely uncomfortable and limit jaw function. A common side effect of bruxism is disturbed sleep, which can lead to fatigue, problems with cognition, and a higher chance of developing numerous illnesses like diabetes and cardiovascular disease. Additionally, bruxism's chronic stress and pain can negatively affect mental health, leading to increased stress and a lower quality of life overall.
Identification of bruxism
There are various ways to diagnose bruxism, including:
Clinical examination: During the examination, the doctor may notice altered dentoalveolar structure, increased masticatory muscles, or worn, fractured, or cracked teeth.
You can gauge the masticatory muscles' level of activity using electromyography. This technique aids in determining whether you have bruxism and how severe it is.
Radiography is used to detect structural changes brought on by bruxism in the dental system.
CT scan: Used to discover changes in the dental system's structure and to gather more precise information about it.
Dental treatment for bruxism
The method used to treat bruxism varies depending on the cause:
The doctor will employ braces or other orthodontic equipment to fix the bite if a malocclusion is the root of the bruxism.
Use of removable night splints: Removable splints are beneficial for bruxism caused by stress or sleep disruption because they protect the teeth and ease muscle tension.
Utilization of drugs: Antidepressants, anxiety medications, and muscle relaxants can all assist to alleviate bruxism and ease muscle tension.
Strengthening facial muscles, pain relief, and tension relief are all benefits of physiotherapy.
Surgery may be necessary in specific situations, such as when the TMJ is not functioning properly.
Bruxism avoidance
In order to avoid bruxism, it is advised that:
Avoid stress; abstain from drugs and alcohol as they exacerbate the condition of the neurological system;
If you experience dental issues, neurological conditions, or endocrine disorders, see a doctor;
Timely dental care and bite correction are essential.
If you experience bruxism symptoms, see a doctor right away. Getting treatment as soon as possible will help you avoid problems and keep your teeth healthy.
To sum it up
Bruxism is a complex sleep disorder that can negatively impact both dental health and overall wellness. In order to take early action, it is essential to know the signs and symptoms of this condition, such as teeth grinding, jaw pain, and dental damage. If untreated, bruxism can result in systemic health problems, a decreased quality of life, and long-term dental disorders include tooth sensitivity and TMJ problems. Numerous diagnostic techniques and treatment options are available depending on the cause. An aspect of prevention is practicing stress management and receiving professional care when symptoms arise. Keep in mind that quick action is necessary for preserving healthy teeth and a pain-free way of life.
0 notes
Text
What conditions can benefit from manual therapy?

Manual therapy can be beneficial for a wide range of musculoskeletal conditions and injuries. It is often used as part of physical therapy and rehabilitation programs to improve joint mobility, reduce pain, and enhance overall musculoskeletal function. Here are some of the common conditions that can benefit from manual therapy:
1. Neck and Back Pain: Manual therapy techniques can be effective in addressing cervical (neck) and lumbar (lower back) pain, including conditions like herniated discs, degenerative disc disease, and muscle tension.
2. Joint Stiffness: Manual therapy can improve joint mobility and reduce stiffness in various joints, including the spine, shoulders, hips, knees, and ankles.
3. Muscle Tension and Spasm: It can help relieve muscle tension, spasms, and myofascial trigger points, which are often associated with conditions like fibromyalgia and myofascial pain syndrome.
4. Sports Injuries: Athletes often use manual therapy to recover from sports-related injuries, such as sprains, strains, and joint injuries. It can also aid in injury prevention and performance optimization.
5. Post-Surgical Rehabilitation: After surgery, manual therapy can assist in the recovery process, improving range of motion, reducing scar tissue formation, and addressing postoperative pain.
6. Osteoarthritis: Manual therapy may help manage the symptoms of osteoarthritis by improving joint function and reducing pain.
7. Headaches: Some forms of headaches, especially tension-type and cervicogenic headaches, may benefit from manual therapy techniques aimed at addressing neck and upper back issues.
8. Temporomandibular Joint (TMJ) Disorders: Manual therapy can be used to address TMJ pain and dysfunction through techniques like mobilization and stretching.
9. Nerve Impingement Syndromes: Conditions involving nerve impingement, such as sciatica or thoracic outlet syndrome, can be managed with manual therapy to relieve pressure on nerves and improve symptoms.
10. Postural Dysfunction: Manual therapy can help correct postural imbalances and improve alignment, reducing the risk of musculoskeletal pain and injuries.
11. Tendinopathies and Bursitis: Inflammation of tendons (tendinopathies) or bursae (bursitis) can benefit from manual therapy techniques to reduce pain and improve tendon or bursa function.
12. Repetitive Strain Injuries: Conditions like carpal tunnel syndrome and tennis elbow can benefit from manual therapy to reduce pain and improve function.
13. Frozen Shoulder (Adhesive Capsulitis): Manual therapy can be part of the treatment plan to address limitations in shoulder mobility associated with frozen shoulder.
14. Pediatric Musculoskeletal Conditions: Children with conditions such as torticollis, developmental hip dysplasia, or congenital musculoskeletal issues may receive manual therapy as part of their care.
It's important to note that manual therapy should be administered by skilled and trained healthcare professionals, such as physical therapists, chiropractors, osteopathic physicians, or manual therapists. The specific techniques used and their application depend on the patient's condition, individual needs, and the healthcare provider's assessment. Before undergoing manual therapy, it's advisable to consult with a qualified practitioner to determine if it is suitable for your condition and needs.
If you're unsure whether physiotherapy is suitable for your specific condition, consult a qualified physiotherapist Dr. Kishan Mishra, one of the best Physiotherapist in Borivali at Sanjeevani physiotherapy for an assessment and personalized treatment plan.
#physiotherapy in borivali west.#dr. kishan mishra#physiotherapy clinic in borivali#sanjeevani physiotherapy
0 notes
Text
TMJ Disorders and Their Treatment
The temporomandibular joint (TMJ) is a complex hinge-like joint that connects your jaw to your skull, allowing you to perform essential functions like chewing, speaking, and yawning. When this joint becomes dysfunctional, it can lead to a range of painful and uncomfortable symptoms collectively known as temporomandibular joint disorders (TMD or TMJ disorders). In this article, we will explore what TMJ disorders are, their common causes, symptoms, and various treatment options available to manage this condition.
Understanding TMJ Disorders:
TMJ disorders refer to a group of conditions that affect the TMJ and the surrounding muscles and tissues. These disorders can result from various factors and can manifest in a variety of ways. Some common types of TMJ disorders include:
Myofascial Pain Syndrome: This condition involves discomfort and pain in the muscles that control jaw movement.
Internal Derangement: Internal derangement refers to a dislocated or displaced disc within the TMJ, causing pain and limited jaw movement.
Arthritis: TMJ arthritis is the inflammation of the joint, often leading to pain and stiffness.
Causes of TMJ Disorders:
TMJ disorders can arise from multiple factors, including:
Bruxism: Teeth grinding and clenching can put excessive pressure on the TMJ, leading to dysfunction.
Trauma: A direct blow to the jaw or face can damage the TMJ and surrounding structures.
Stress: Stress can cause muscle tension and jaw clenching, exacerbating TMJ symptoms.
Malocclusion: Misalignment of the teeth or jaw can contribute to TMJ disorders.
Genetics: Some individuals may be genetically predisposed to TMJ disorders.

Common Symptoms of TMJ Disorders:
TMJ disorders can manifest with a wide range of symptoms, which may include:
Jaw Pain: Pain in the jaw joint, often worsened by chewing or speaking.
Facial Pain: Pain in the face, particularly around the ears, temples, and cheeks.
Headaches: Frequent headaches, often resembling tension or migraine headaches.
Jaw Clicking or Popping: Audible sounds when moving the jaw, such as clicking, popping, or grating.
Limited Jaw Movement: Difficulty opening the mouth fully or experiencing jaw locking.
Ear Pain: Earaches or a sensation of fullness in the ears.
Neck and Shoulder Pain: Discomfort in the neck and shoulders due to muscle tension.
Treatment Options for TMJ Disorders:
Treatment for TMJ disorders aims to relieve pain, improve jaw function, and address the underlying causes. The appropriate treatment plan depends on the severity and specific symptoms of the condition. Here are various treatment options commonly used for TMJ disorders:
1. Self-Care and Lifestyle Modifications:
Rest: Give your jaw a break by avoiding excessive chewing and speaking loudly.
Dietary Changes: Opt for soft foods and avoid hard or chewy items.
Heat or Cold Packs: Applying moist heat or cold packs to the affected area can help alleviate pain and muscle tension.
Stress Management: Techniques such as relaxation exercises, yoga, and meditation can help reduce stress-related jaw clenching.
2. Medications:
Pain Relievers: Over-the-counter pain relievers like ibuprofen or prescription medications may help manage pain and inflammation.
Muscle Relaxants: These medications can help relax jaw muscles, reducing tension and pain.
3. Physical Therapy:
Oral Splints or Mouthguards: Custom-fitted oral splints or mouthguards can help reposition the jaw and reduce clenching and grinding.
Physical Therapy: Therapeutic exercises, stretching, and massage can help improve jaw function and alleviate muscle tension.
4. Dental Treatments:
Orthodontics: Correcting misaligned teeth or malocclusion may alleviate TMJ symptoms.
Dental Restorations: Replacing missing teeth or adjusting dental work can help balance the bite and reduce TMJ strain.
5. Injections:
Botox: Injections of botulinum toxin (Botox) can temporarily paralyze jaw muscles, reducing muscle tension and pain.
6. Surgery:
Arthrocentesis: A minimally invasive procedure involving the removal of fluid and debris from the joint space.
Arthroscopy: A surgical procedure using small incisions and a tiny camera to diagnose and treat TMJ issues.
Open-Joint Surgery: In severe cases, open-joint surgery may be necessary to repair or replace the TMJ.
Conclusion: Seeking Relief for TMJ Disorders
TMJ disorders can significantly impact your quality of life, but with the right diagnosis and treatment, relief is possible. If you experience persistent jaw pain or other symptoms associated with TMJ disorders, consult with a dentist or oral specialist for a thorough evaluation. With a personalized treatment plan, you can regain comfort, functionality, and a pain-free jaw.
0 notes
Text
Dentist
"Dentistry is more of an art than a science, more subjective than objective, resulting in wide variations in clinical judgements and interventions between dental practitioners."
Robert L. Caplin, British Dental Journal volume 230, pages337–343 (2021)
Ref: https://www.nature.com/articles/s41415-021-2726-4
During my dentist last visit to Japan, his colleague treated a Cerebral Palsy patient with tooth issues by carefully examining their body & providing PNF (Proprioceptive Neuromuscular Facilitation) & massage treatment.
PNF could be beneficial for other patients with postural imbalance issues that may be connected to dental problems. It's recommended to seek a doctor who can provide a full diagnosis & a holistic approach rather than just treating the symptoms.
Prosthodontist issue:
TMD (Temporomandibular disoders / Bruxism) TMJ teeth, muscles, joint
The jaw joint never rest, working 24 hours.
Temporary Solution: custom splint, adjustment needed every now and then. Some exercise and massage needed. However, it’s incurable disease, long life maintenance with hope it’s getting better w the given tool.
In relation to Sleep disorder & dental patient : Snoring & OSA Obstructive Sleep Apnea
Sleeping Cycle:
-Non REM sleep 80%
-Quiet sleep
-Light sleep
-REM deep sleep
Help to prevent snoring:
-No alcohol or sleeping pills before bed
-Maintain Ideal body weight
-Sleep in side ways
Key factor of OSA:
In relation with breathing muscle & upper airway, abnormal anatomy airway, obesity, pathophysiology.
Sleep related Breathing disorders
Test using PSG polysomnography
OSA complication:
-Cardiovascular: Coronary, heart, stroke, sudden death, hypertension.
-Exhausted & Sleepiness during daytime: accident, emotional, depression, low memory & coordination, headache, impotency
-Gherlin hormon (hunger hormone)
-Complication:
Pregnancy complication, eye (glaucoma), bladder peeing at night, diabetes, metabolism syndrome, fatty liver, chronic obstructive, pulmonary, & gerd.
Solution: Oral Medication, Operation, Device (CPAP/ MAD/ DSA/ OA/ MAS/ MRA)
I’m grateful for the gift of the day : a Jap toothbrush from the kind & passionate half Japanese orthodontist who carefully examined my issues without asking for money since he couldn't fix them. He honestly admitted that it's not his specialty, but he still discussed the matters with me & helped me find solutions alongside other professional dentists. I truly appreciate his sincerity, guidance, & patience. Looking forward for some improvement in 3 months. Btw, Japanese toothbrushes are the best!
Over the past decade, I have encountered numerous dentists specializing in various fields. However, the most valuable lessons came from a young friend who had just graduated from UI at the time, specialized in Prosthodontics. Surprisingly, she turned out to be the youngest & brightest dentist I had ever met. She tirelessly guided me & referred me to other specialists, patiently supporting me throughout the journey. I’m truly grateful for her TLC, she is a real unsung hero.
The 3 dentists I mentioned share a common trait: they genuinely listen to their patients & collaborate with them to find solutions, which builds trust through a holistic approach by diagnosing the root cause rather than just treating symptoms. They’re truly passionate about their work & prioritize patient well-being over monetary gains. They also welcome my endless Q without feeling insecure, leading to great discussions where we learn from each other. Such person is truly a gem. 💎
Further reading:
Book by Prof drg. Laura Susanti Himawan, Sp.Pros(K)., FICD
(only in Bahasa Indonesia)
1. Memahami Gejala, Penyebab, Serta Kiat Mencegah & Mengatasi Gangguan Sendi Rahang TMD (Temporomandibular Disorders)
2. Peran dokter gigi atasi gangguan Ngorok & OSA (Obstructive Sleep Apnea)
Additional Note:
It has been a frustrating experience to have certain pain and unknown diagnose of the core problems. Currently I am still trying the available method that has been suggested by the 3 dentists above. I've tried so many dentist in the past apart from the dentist I mentioned above, it was a waste of time and money, but one thing for sure, the tooth trauma and damaged can't be undone.
In summary, there is no such perfect doctor, doctor has their own speciality and way to approach your problems. But I do believe on holistic approach doctor who can help you to see the big picture (full diagnose, not just a symptoms) and pivoting to the solution. To find a suitable doctor for your tailor made case is almost similar to find a suitor. Find what's best available in your area and budgeting accordingly. For instance, Overseas dentist is not up to my budget due to the long term maintenance.
Hope you all healthy and well.
#dentist#tooth#doctor#health#hollistic#hollistichealth#pnf#osa#sleepdisorder#tmd#bruxism#grinding#orthodontist#Prosthodontist#specialist#dentistry#art#science
0 notes
Text
Eagle Syndrome Difficulties
I try not to complain too much, but with Eagle Syndrome, it's getting to the point where my tolerance of my pain is running out. I am really struggling to work through the pain barriers that I get to deal with every day.
My symptoms started with a swollen mouth ligament, two months after losing my twin, through stress watching my twin's health decline.
Acupuncture
My current treatment is acupuncture to try to bring some relief. Having now been diagnosed by a maxillofacial specialist and having acupuncture treatment and asked the question, my swollen ligament and teeth issue could well be linked to Eagle Syndrome, as this can cause inflammation locally. But those symptoms could also tie in with TMJ?
I am due back at the hospital in a couple of weeks to see my maxillofacial specialist. The ligament and teeth issue started around the same time as Eagle Syndrome.
Eagle Syndrome Difficulties
My difficulties with Eagle Syndrome is the pain triggers, and not knowing when the pain will strike. There is literally no warning. I have activated trigger points, including muscular dysfunction and nerve sensitivity.
Along with ear pain, other symptoms include difficulty swallowing; head pressure, ear pressure, headaches, neuralgia type symptoms also, pressure behind the eyes, watering eyes, sensitive to light and noise, general malaise and generally feeling unwell. I'm more anxious than usual and scared. Not knowing when the pain strikes is scary. The condition is debilitating.
I've currently had to stop exercising. The cold weather seems to have an affect on my triggers. Putting make-up on, even washing my face is difficult. I go to bed with pain and wake up with pain. I have no life, but I am trying to work on ways to get myself better.
For more inspirational, life-changing blogs, please check out my site https://www.thecpdiary.com
1 note
·
View note