#Acute Kidney Failure
Text

Dr. Mudit Khurana, a seasoned Nephrologist and Renal Specialist, boasting an impressive 9-year journey in this domain. His educational foundation is robust, having accomplished MBBS from MGM Medical College, Indore in 2012, followed by MD in General Medicine from University College of Medical Sciences, Delhi University in 2015. Dr. Khurana’s pursuit of excellence led him to achieve DM in Nephrology from Sanjay Gandhi Postgraduate Institute of Medical Sciences in 2020. Dr. Mudit Khurana stands as the best nephrologist in Agra, showcasing unparalleled expertise in renal care. His proficiency extends to being the finest kidney specialist in Agra, bringing forth a combination of years of experience and exceptional education
Chronic Kidney Disease
Acute Kidney Failure
Diabetic Nephropathy Kidney Infections (Pyelonephritis) Cystic Kidney Disease Kidney Stones Glomerulonephritis Urinary Tract Infection Hypertension Dedicated Nephrology Practice Complete Solutions to Patient
#Chronic Kidney Disease#Acute Kidney Failure#Diabetic Nephropathy#Kidney Infections (Pyelonephritis)
1 note
·
View note
Text
What is Acute Kidney Failure?

Acute kidney failure, also known as acute renal failure, is a sudden and significant decline in the kidneys' ability to operate effectively. It happens abruptly and necessitates the rapid diagnosis and treatment of the underlying causes. Serious infections, urinary tract blockages, and surgical complications are among the most common reasons.
Recognizing the symptoms of acute renal failure is critical for timely diagnosis and treatment. The symptoms include decreased urine flow, edema in the legs and ankles, weariness, nausea, vomiting, lack of appetite, and confusion. If you have any of these symptoms, seek medical attention.
To identify acute kidney failure, clinicians may use blood and urine tests, imaging techniques such as ultrasounds or CT scans, and, in certain situations, kidney biopsies. Treatment options vary depending on the underlying cause and severity of the illness. Medications can be used to treat infections, symptoms, and blood pressure. Diuretics can assist in removing excess fluid from the body. In severe cases, dialysis may be required to eliminate waste materials and excess fluid from the bloodstream. renal transplantation may be a possibility for certain people with advanced renal disease.
0 notes
Text
https://alfakidneycare.com/acute-kidney-failure-in-hindi/
0 notes
Text
today's vetted campaigns. please please continue to share and donate. i know lots of my posts are like this now, but we can't lose energy. these families need us.
june 18th:
Tahani Shorbajee and her family of ten (including her three children, all needing urgent treatment for hepatitis) ($11,329/$50,000) - @tahanishorbaje2, verified by @/el-shab-hussein
Fadi Ayyad and his family of eight ($9,446/$35,000) - @mayadayyad, @aymanayyad81, verified by @/nabulsi
Shahad Abu Musa and her family of seven ($11,574/$40,000) - @shahdhatem, verified by @/sar-soor
Muhammad Al-Habil and his family of six (including his chronically ill parents and wife, and three acutely malnourished children) (€3,928/€50,000) - @mohammed-family76, verified by @/el-shab-hussein
Shahed Nahal and family ($4,342/$50,000) - @shahednhall, verified by @/nabulsi
Reem Shehab, her husband Fahed, their five children, and the children's grandmother (€13,730/€50,000) - @malakshehab, @danashehab, verified by @/ibtisams
Amani Hasan and her three children ($9,103 CAD/$17,732 CAD) - @amani93gaza, verified by @/nabulsi
Ahmed Abu Shammalah's family of eight (€7,541/€100,000) - @ahmed8311, verified by @/nabulsi
Skater Hani Alhajjar's family of ten (they lost their father to kidney failure due to lack of treatment, Hani is the family's only support) (€27,993/€50,000) - @skatehani, verified by @/fallahifag
not yet vetted but likely legitimate:
Dalia Mohisen and her family (€6,391/€35,000) - @daliamohisen
Ramez Hilles and his family of ten (€105/€37,000) - @ramezderar
i know link-heavy posts like this can seem like a lot, but if you can pick even just one of these fundraisers to donate to or promote today, it makes a difference
22K notes
·
View notes
Text
Acute Kidney Failure Treatment Naturally At Swanand Kidney Clinic
Acute kidney failure (AKF) is a sudden decline in kidney function that can occur due to various reasons, including infections, medications, and underlying medical conditions. It can lead to a buildup of waste products in the blood and affect the body's fluid balance.
Swanand Kidney Clinic: Your Trusted Partner in AKF Treatment:
Swanand Kidney Clinic is a renowned healthcare facility specialising in the diagnosis and treatment of kidney diseases, including acute kidney failure. Our team of experienced nephrologists and skilled healthcare professionals is dedicated to providing comprehensive care tailored to your individual needs.
Early Signs of Acute Kidney Injury :
Decreased Urine Output: Producing less urine than usual or experiencing no urine output at all is a significant warning sign.
Swelling: Fluid retention can lead to swelling in the legs, ankles, and feet due to the kidneys' inability to remove excess fluid.
Nausea and Vomiting: Feeling sick or vomiting can indicate kidney distress.
Fatigue: Unusual tiredness or weakness may occur as the body struggles to manage waste products.
Confusion or Mood Changes: Altered mental status, including confusion or changes in mood, can be a sign of toxin buildup in the body.
Shortness of Breath: Difficulty breathing may arise from fluid buildup in the lungs, a complication of AKI.
High Blood Pressure: Elevated blood pressure can occur as the kidneys fail to properly regulate fluid and electrolyte balance.
Flank Pain: Pain in the lower back, particularly on the sides, may indicate kidney issues.
Loss of Appetite: A decreased desire to eat can also be a symptom of kidney dysfunction.
Symptoms :
Because the kidneys are needed to properly balance ratios of water, salt and other minerals (called electrolytes) in the blood, kidney failure symptoms are very dangerous and often even life-threatening. However, it’s not always obvious to patients that kidney damage is contributing to their health problems — since the underlying reasons that the kidneys fail can cause all sorts of symptoms.
For some patients with unhealthy kidneys, no obvious symptoms are felt at all. Only suddenly “failure” of the kidneys occurs and then causes an emergency.
Kidney failure symptoms normally include:
Kidney pain, which feels like throbbing or tenderness below the rib cage or in the back/abdomen (sometimes called “flank pain”)
Producing less urine than usual or sometimes not at all. A warning side of kidney disease, however, may be frequent urination, sometimes with blood or other colour changes.
Fluid retention and swelling due to an imbalance of electrolytes, especially in the lower extremities, such as the legs, ankles or feet. The face and eyes may also appear puffy and swollen.
Indigestion, nausea, loss of appetite and sometimes vomiting.
High blood pressure
Cognitive and mood changes, mostly due to shifting electrolyte levels and dehydration. These can include confusion, trouble sleeping, anxiety, fatigue, trouble concentrating, weakness and brain fog.
Rhabdomyolysis is a rapid breakdown of skeletal muscle that causes muscle proteins and other muscle constituents to leak outside of cells and into the bloodstream.
While kidney failure is very serious, it doesn’t always mean that someone needs to be put on dialysis forever or they’re necessarily at risk of dying. Depending on the state of someone’s overall health — along with age and how many risk factors the person is up against — it’s possible to live a fulfilling life even with severely damaged/failed kidneys.
Sometimes severe kidney injuries can be resolved by treating the underlying problem causing the patient’s symptoms, but other times this unfortunately isn’t the case. Permanent kidney damage and chronic kidney disease cause a low percentage of patients to need ongoing dialysis treatments for the remainder of their lives, and with elderly patients, this often shortens their life expectancy. For patients who wind up in the intensive care unit due to emergency kidney failure, it’s estimated that the risk of mortality is between 50 per cent and 80 per cent.
Research has shown that several natural products can play a role in preventing and treating acute kidney injury. These products often possess anti-inflammatory and antioxidant properties, which help mitigate oxidative stress and inflammation—two key factors in kidney damage.
Herbal Remedies:
Ginger: Known for its anti-inflammatory properties, ginger can help reduce inflammation in the kidneys and improve overall kidney function.
Garlic: Garlic has been shown to lower blood pressure and improve kidney function. It may also help reduce the risk of kidney damage.
Ginseng: This herb is known for its ability to enhance kidney function and protect against kidney injury.
Pomegranate: Rich in antioxidants, pomegranate can help reduce oxidative stress and improve kidney health.
Phytochemicals:
Flavonoids and Polyphenols: Found in fruits like berries, apples, and grapes, these compounds have protective effects on the kidneys and can reduce inflammation.
Turmeric: Curcumin, the active compound in turmeric, has potent anti-inflammatory properties and may help protect against kidney damage.
Natural Supplements:
Cranberry Extract: Known for its ability to prevent urinary tract infections, cranberry extract may also support kidney health by reducing urinary calcium levels.
Magnesium: This mineral helps prevent the formation of kidney stones and supports overall kidney function.
Vitamin E: An antioxidant that may help lower calcium-oxalate levels in the urine, reducing the risk of kidney stones.
While acute kidney failure treatment in Pune is a serious condition requiring immediate medical attention, incorporating natural remedies and lifestyle changes can play a supportive role in kidney health and recovery. By working closely with healthcare professionals at Swanand Kidney Clinic, patients can explore a comprehensive treatment approach combining conventional therapies with natural supplements, dietary modifications, and lifestyle adjustments tailored to their needs.
Visit Here For More Info: https://swanandkidneyclinic.com/acute-kidney-injury/

#Best Kidney Specialist In Bhosari#Best Nephrologist in Bhosari#Kidney Stone Treatment In Bhosari#Kidney Failure Treatment In Pune#Acute Kidney Injury Treatment. Acute Kidney Failure Treatment in Pune
0 notes
Text

Examining Homeopathic Methods for Treating Renal Failure
Renal failure, another name for kidney failure, is a dangerous medical condition in which the kidneys are unable to effectively filter waste materials out of the blood. While there are many treatment options available in traditional medicine, such as kidney transplants and dialysis, homeopathy offers alternative methods that improve overall health and kidney function without the need for prescription drugs. This article delves into the fundamentals of homeopathy and considers how it might be used to Treatment for kidney failure.
Comprehending Homeopathy:
Homeopathy is an all-encompassing medical approach based on the idea that "like cures like." It works on the premise that a highly diluted form of a drug that causes symptoms in a healthy person can alleviate identical symptoms in a sick person. The preparation of homeopathic medicines involves a series of steps, including serial dilution and succussion, which is meant to maximize their therapeutic effectiveness and minimize any possible negative effects.
Tailored Treatment Approach:
Tailored treatment is one of the mainstays of homeopathy. In order to recommend a remedy that is tailored to each patient's situation, homeopathic practitioners evaluate the individual symptoms, medical history, and overall constitution of each patient. Before suggesting a course of treatment in the instance of Treatment for kidney failure, a homeopath would take into account the patient's emotional and physical condition, the cause of kidney damage, and the symptoms that are now present.
Symptom Management:
The goal of homeopathic treatments for renal failure is to reduce symptoms like exhaustion, edema, nausea, and trouble peeing. These treatments focus on addressing the underlying imbalances that are causing the symptoms rather than immediately treating the kidneys. A homeopath might, for instance, provide a treatment to enhance the body's detoxification systems, lower inflammation, or increase circulation—all of which have an indirect positive impact on kidney function.
Avoiding Complications:
High blood pressure, electrolyte imbalances, anemia, and cardiovascular disease are just a few of the issues that can arise with kidney failure. The goal of homeopathic treatment is to support the body's natural healing processes and address the underlying causes in order to prevent or minimize these consequences. Homeopathy focuses on the whole person's health and vitality in an effort to enhance quality of life and lower the likelihood of renal failure-related secondary health problems.
Conclusion:
While homeopathy is not a substitute for conventional medical care in cases of Treatment for kidney failure, it offers a holistic approach to managing symptoms, supporting renal function, and promoting overall health and vitality. By addressing the individual's unique constitution and employing remedies that stimulate the body's innate healing mechanisms, homeopathy can play a valuable role in enhancing quality of life for individuals living with kidney failure. As with any medical condition, it's essential to consult with a qualified homeopathic practitioner to determine the most appropriate course of treatment tailored to your specific needs.
#Treatment for kidney failure#high creatinine treatment#chronic kidney disease causes and treatment#kidney failure treatment without dialysis#Chronic Kidney Disease#Acute Kidney Injury Treatment
0 notes
Text
Understanding Acute Kidney Failure Symptoms: Recognition, Causes, and Management
Acute kidney failure, also known as acute kidney injury (AKI), is a sudden and potentially reversible decline in kidney function. Recognizing the symptoms of acute kidney failure is crucial for prompt diagnosis and treatment. Let's delve into the various aspects of AKI symptoms, including their recognition, underlying causes, and management strategies.
Recognition of Acute Kidney Failure Symptoms:
Decreased Urine Output: One of the hallmark signs of AKI is a reduction in urine production. Individuals may pass significantly less urine than usual or stop urinating altogether.
Fluid Retention: AKI can lead to fluid retention, causing swelling in the legs, ankles, feet, or face. This swelling, known as edema, occurs due to the kidneys' inability to properly regulate fluid balance in the body.
Fatigue: Feelings of tiredness or exhaustion, even with adequate rest, are common symptoms of AKI. Fatigue may result from electrolyte imbalances, anemia, or the accumulation of waste products in the bloodstream.
Shortness of Breath: Accumulation of fluid in the lungs, known as pulmonary edema, can cause difficulty breathing or shortness of breath. This symptom may worsen when lying flat and improve when sitting upright.
Nausea and Vomiting: Digestive symptoms such as nausea, vomiting, and loss of appetite may occur due to the buildup of waste products and toxins in the bloodstream. These symptoms can contribute to electrolyte imbalances and dehydration.
Confusion or Altered Mental Status: In severe cases of AKI, changes in mental function, confusion, or delirium may occur. These neurological symptoms may result from electrolyte disturbances or the accumulation of uremic toxins in the brain.
Chest Pain or Pressure: Chest pain or pressure may occur due to fluid buildup around the heart (pericarditis) or electrolyte imbalances associated with kidney dysfunction. These symptoms require immediate medical evaluation to rule out serious cardiac complications.
Causes of Acute Kidney Failure:
Acute kidney failure can result from various underlying causes, including:
Dehydration: Inadequate fluid intake, excessive fluid loss (e.g., diarrhea, vomiting), or conditions such as heatstroke can lead to dehydration and subsequent AKI.
Decreased Blood Flow to the Kidneys: Conditions that impair blood flow to the kidneys, such as low blood pressure (hypotension), heart failure, or severe infections (sepsis), can cause AKI.
Kidney Damage: Direct injury to the kidneys from trauma, medications, contrast dyes used in imaging tests, or certain toxins can lead to AKI.
Obstruction: Blockages in the urinary tract, such as kidney stones, tumors, or enlarged prostate glands, can obstruct urine flow and cause AKI.
Management of Acute Kidney Failure:
Identifying and Treating Underlying Causes: Prompt identification and treatment of the underlying cause of AKI are essential for managing the condition. This may involve addressing dehydration, optimizing blood pressure, discontinuing nephrotoxic medications, or relieving urinary tract obstructions.
Fluid and Electrolyte Management: Maintaining fluid and electrolyte balance is crucial in AKI management. Intravenous fluids may be administered to restore hydration and support kidney function. Electrolyte imbalances, such as hyperkalemia (high potassium levels) or hyponatremia (low sodium levels), require close monitoring and appropriate interventions.
Nutritional Support: Adequate nutrition is important for individuals with AKI, especially those experiencing nausea, vomiting, or loss of appetite. A registered dietitian can provide personalized dietary recommendations to meet nutritional needs while minimizing stress on the kidneys.
Monitoring and Dialysis: Close monitoring of kidney function, fluid status, and electrolyte levels is essential in AKI management. In severe cases, hemodialysis or peritoneal dialysis may be necessary to remove waste products and excess fluid from the bloodstream.
Preventive Measures: Taking preventive measures to avoid dehydration, maintaining a healthy lifestyle, and avoiding nephrotoxic medications or substances can help reduce the risk of AKI. Regular medical check-ups and monitoring kidney function in individuals at risk for AKI can aid in early detection and intervention.
Conclusion:
Recognizing the symptoms of acute kidney failure is crucial for prompt diagnosis and treatment. From decreased urine output to fluid retention, fatigue, and neurological symptoms, AKI symptoms can vary depending on the underlying cause and severity of the condition. Early identification and management of AKI, including addressing underlying causes, fluid and electrolyte management, nutritional support, and close monitoring, are essential for improving outcomes and preventing complications. If experiencing symptoms suggestive of AKI, it's important to seek immediate medical attention for proper evaluation and treatment.
0 notes
Link
हमारी किडनी शरीर में संतुलन बने रखने के कई कार्यों का निष्पादन करती हैं। वे अपशिष्ट उत्पादों को फिल्टर करके पेशाब से बहार निकालते हैं एवं निष्कासन करते हैं वे शरीर में पानी की मात्रा, सोडियम, पोटेशियम और कैल्शियम की मात्रा (इलेक्ट्रोलाइट्स) को संतुलित करते हैं। वह अतिरिक्त अम्ल एवं क्षार निकालने में मदद करते हैं जिससे शरीर में रसिद एवं क्षार का संतुलन बना रहता है। शरीर में किडनी का मुख्य कार्य सुन का शुद्धिकरण करना है जब बीमारी के कारण दोनों किडनी अपना सामान्य कार्य नहीं कर सके, तो किडनी की कार्यक्षमता कम हो जाती है। जिसे हम किडनी फेल्योर कहते हैं।
#acute renal failure in hindi#chronic renal failure in hindi#kidney failure in hindi#kidney failure symptoms in hindi#renal disease in hindi#renal failure in hindi#kidney transplant#Kidney Transplant Doctor
0 notes
Text
A patient undergoing a kidney transplant needs to regularly take certain medicines as recommended by the doctor. This is essential to ensure that the new kidney is functioning properly. While some medicines need to be taken life-long, others may be required for a specific period of time. These medicines include:
Immunosuppressants or anti-rejection drugs: These medicines need to be taken life-long to prevent the immune system of the body from attacking the new kidney.
Antibiotics or antiviral medicines: These medicines may be recommended for a specific period of time to prevent bacterial and viral infections after kidney transplant.
Symptomatic medications: These medicines may be given to relieve the symptoms associated with a kidney transplant, such as stomach ulcers, diarrhea, constipation, pain, and nutritional deficiencies.
There are many hospitals in Mumbai where kidney Transplant is done with great success.
#kidney transplant#kidney failure#kidney cancer#kidney stone#kidney#kidney disease#acute renal failure#renal failure
0 notes
Text
#Ayurvedic treatment for proteinuria#Proteinuria ayurvedic treatment#Ayurveda treatment for fixing proteinuria#Protein loss in urine treatment in ayurveda#Ayurvedic medicine for proteinuria#Acute kidney disease treatment in ayurveda#Acute kidney failure treatment in ayurveda#Chronic kidney disease treatment in ayurveda#Nephrotic syndrome ayurvedic medicine#Nephrotic syndrome ayurvedic treatment#Ayurvedic medicine for kidney cyst
0 notes
Photo
Nephrology is the subspecialty of internal medicine that focuses on the diagnosis and treatment of diseases of the kidney. Lexington Renal Care Physicians Services in Kentucky We provide services that help you with the prevention and treatment of kidney disease.
#Hypertension#Proteinuria and Hematuria#Diabetic nephropathy#kidney disease#Glomerular diseases#Acute and chronic renal failure#Inherited renal diseases#polycystic kidney disease#Evaluation#management of kidney transplant#recipients and donors#Disorders of fluid#electrolyte and acid-base#Nephrolithiasis#kidney stones#disorders of calcium#parathyroid hormone#Osteoporosis#metabolic bone disease#dialysis#In-center dialysis#peritoneal dialysis#home hemodialysis#nocturnal hemodialysis#Managing anemia#chronic kidney disease
0 notes
Text
Monoclonal Antibodies
So I listened to a talk from a drug rep the other day who came into the clinic to promote Cytopoint, the anti-allergy injection for dogs.
It’s a great drug, overall. Super useful for many, literally life changing for a few, and now a mainstay of the allergy treatments we offer. But I had to laugh at something the rep said:
“It’s not really a drug. It’s a bio-mimicry molecule! It’s replicating normal molecules that would be found in the body and just providing more of them!”
And I’m sitting here thinking: that is still totally a drug. A drug is any substance which when given to a living organism produces a physiological effect. 10mg of lokivetmab is most definitely a drug.
But if you are going to argue that Cytopoint is not a drug because it mimics a natural molecule found in the body, then by that logic neither are insulin, thyroxine, cortisone or just about every single hormone.
For goodness sake. I have to wonder what planet marketers live on some days.
We also had a bit of a debate because we’re widely told that Cytopoint shouldn’t have any side effects. Partly this is because monoclonal antibodies aren’t well known in veterinary medicine and they haven’t been around that long.
They’re certainly much safer than the equivalent drugs in other classes, but they’re not ‘side effect free’. They’re a protein, so it’s theoretically possible to be allergic to it. Like the Kesimpta I take it seems likely that some dogs will be ‘off colour’ for a day or so. The most common side effect is being quiet the next say, so it is pretty mild for a typical dog and still worth it. But it’s not zero.
Having a headache for a day is much milder than having acute kidney failure, but I wonder if we’ll get more reports in the future of extremely sporadic weird side effects as we gain more experience with this class of medication.
Medical advancements are wonderful and exciting. But don’t let marketers do all the talking!
And remember to report side effects to the manufacturer.
275 notes
·
View notes
Text
Can you trust AI Answers about your health?
During the summer of 2020, when the entire world was focused on the pandemic, getting treatment for other health issues became a challenge.
I started experiencing a lot of back pain, but I shrugged it off as an injury and took Advil to cope.
A week later, I thought I had food poisoning.
I tried an at-home service where they pumped me full of IV fluids.
I went to urgent care. They sent me to get scans. I paid hundreds of dollars out of pocket to get them quickly.
The imaging place never sent the scans to the urgent care.
A day later, I had the worst chills. It was July, in Phoenix. Most likely 100 F. I went outside and was still freezing.
At that point, I was taken to the ER. I ended up in the ICU in one of those rooms they zipped up in plastic.
While most of the focus was on COVID, I had something else: a large kidney stone. The kind that doesn’t pass on its own.
I was in septic shock and acute renal failure according to discharge papers.
The hospital stay itself wasn’t too long, but the treatment with specialists took three months to complete.
Surgeries during COVID were extra special because if you tested positive, your surgery was delayed.
Two years later, in 2022, I ended up in the same hospital for the same reason.
And now, I’m a few days into aggressive antibiotic treatment for my kidneys, yet again. Wondering if I make it to the next followup or have to Lyft off to the ER.
So what does this have to do with Google AI Answers?
In 2020 and 2022, I spent a lot of time perusing Google Search results on kidney stones.
Now, I get AI Answers above at the top of SERPs (search engine results pages).
This wouldn’t be a bad thing if one could trust the AI to accurately summarize its sources.
That’s the big if.
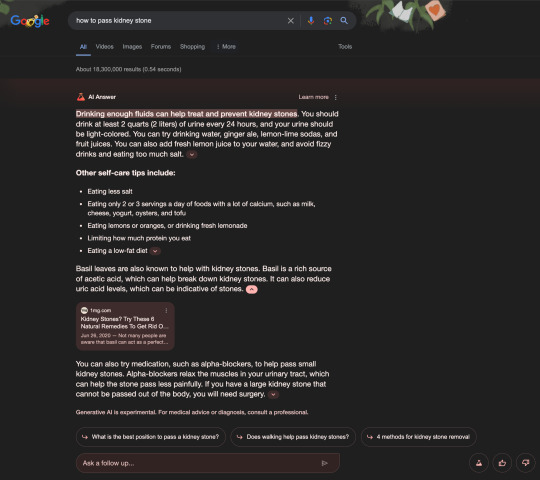
In the first screenshot, you’ll find an AI Answer from Google Search results for the phrase how to pass kidney stone.
The first mistake involved an error with paraphrasing a source with legitimate information.
Because I can assure you after four years of seeing urology specialists, no one has ever suggested drinking two quarts or liters of urine.
The basil leaves suggestion, on the other hand, is suspect. I’ve never come across that as a suggestion. It would have stood out, because I have a lot of basil growing around the garden.
I don’t even remember that website from my previous Google searches. I had to check Wikipedia and other sources to find out what the company even was.
Much like the search quality raters and AI Answer checkers do...
In the second screenshot, Microsoft Bing with Copilot offered ads for supplements and advice from five sources, two of which are the MSN Health Hub.
The hub includes a section where you can Ask a health professional questions.
In the third screenshot, ChatGPT using GPT-4 with browsing offered a concise response based on its training data, but claimed not to have access to external sources.
In the fourth screenshot, Perplexity provided the best AI Answer with 19 sources I recognized from my previous research into this health issue.
Moral of the story:
You can’t trust generative AI with your money or your life issues.
But if you do, start with the right AI Answer engine. One that cites sources you trust and doesn’t suggest drinking your own pee.
Think of Perplexity as a better starting point for more in-depth research that you can discuss during your next doctor’s visit.
Not as a definitive answer.
Follow @kristileilani on X for more on AI news, trends, and tools.
34 notes
·
View notes
Text
Okay. Okay okay okay. So. This is a HUGE discovery. Death caps and destroying angels are two of the deadliest mushrooms in the world; both are in the genus Amanita. Both species contain both amatoxins and phallotoxins, though the latter are likely not a major factor in the massive cell death that occurs in the liver and/or kidneys after consuming these mushrooms.
The most medically significant of the amatoxins is α-amanitin. When a deadly Amanita is consumed, you're likely to get the expected gastrointestinal upset that accompanies many toxic mushrooms within a few hours, and they may last for a few days. Then you start to feel better--but you can't just say "Okay, learned my lesson, I won't eat THAT one again." That's because α-amanitin has been stuck in your liver and kidneys the whole time, destroying their cells left and right, and its deleterious effects are catching up to you. So you can expect to end up in the hospital, potentially dealing with acute organ failure.
Supportive care generally includes IV fluids and electrolytes along with penicillin, oral activated charcoal, and other medications, along with hemodialysis and hemoperfusion. Some people have needed organ transplants, and numerous people have died, especially those who got medical help too late.
While compounds from milk thistle (Silybum marianum) have shown success in treating amatoxin poisoning in a small study several decades ago, there hasn't been much follow-up since. Recently, researchers studied the molecular effects of α-amanitin, and discovered that the enzyme STT3B plays a crucial role in creating N-glycans that facilitate the cell death caused by α-amanitin. Then they went looking for anything that could inhibit STT3B from a list of possible treatments approved by the FDA.
Enter indocyanine green. Developed as a dye for photography in the 1950s, it received approval for medical use a few years later, and has been used for everything from measuring cardiac performance to opthalmology. But it just so happens to also significantly reduce cell death both in vitro in human cell lines, and in vivo in mice. There haven't been any in vivo studies in humans just yet, but results are very promising.
There's one limitation--indocyanine green must be given as soon as possible after ingestion. When it was given eight or twelve hours after α-amanitin poisoning, it was no longer effective due to cell death having already occurred.
Still, the fact that we now have a potential new tool in treating acute α-amanitin poisoning is a massive hope for the future. Couple this with increasing education about safe mushroom foraging and how to identify poisonous species, and we could see a significant reduction in poisoning from those two deadly Amanita species.
#mushrooms#mushroom hunting#shrooms#fungi#fungus#foraging#mushroom foraging#medicine#healthcare#nature#Amanita#destroying angel#death cap
220 notes
·
View notes
Text
Acute kidney injury treatment In Pune - Swanand Kidney Clinic
Despite treatment advances, AKI mortality remains high—about 40% in critically ill patients. Factors that may influence high mortality include the increasing age of the patient population and the development of multisystem failure. Patients who fail to recover from AKI have a 25% chance of dying within 1 year. Also, in postoperative patients like Dr. Snehal Gaikwad and in AKI patients who need renal replacement therapy (dialysis), AKI is linked to an increased risk of death.
AKI carries a high economic toll as well. Many patients don’t recover, suffering end-stage renal disease (ESRD), which necessitates lifelong dialysis.
Causes:
Nephrotoxic drugs, such as aminoglycosides and contrast agents, can cause AKI. To avoid kidney injury, these agents must be administered carefully, with dosages tailored to the patient’s condition.
Overwhelming infection or sepsis is one of the most common causes of AKI. The kidney receives about 20% of total cardiac output in normal healthy persons. In contrast, patients with serious infections have reduced BP, which decreases blood flow to the kidneys and leads to ischemia. Renal tubules are highly sensitive to reduced blood flow. Sepsis disrupts blood flow to the kidneys the gut and the liver; some organs have well-perfused and nonperfused areas. As blood flow slows and stagnates, some kidney areas become under-perfused, ultimately suffering cell ischemia and death.
Signs and symptoms of AKI include:
decreased urine output (although occasionally, urine output remains normal)
chest pain or pressure
jugular vein distention
fluid retention, causing edematous legs, ankles, or feet
shortness of breath
confusion
nausea
seizures or coma in severe cases.
Understanding the causes, risks, and potential long-term impacts of AKI is essential for effective treatment and recovery. Acute kidney injury treatment in Pune is a critical condition that requires immediate attention and ongoing management. At Swanand Kidney Clinic, we are dedicated to providing comprehensive care and support for patients affected by AKI.

#Best Kidney Specialist In Bhosari#Best Nephrologist in Bhosari#Kidney Stone Treatment In Bhosari#Kidney Failure Treatment In Pune#Acute Kidney Injury Treatment.
0 notes
Text
Effective Methods for decreasing Creatinine Levels to Restore Renal Health
High creatinine levels can indicate underlying kidney issues and require prompt attention to prevent further complications. Homeopathy offers a gentle yet effective approach to managing elevated creatinine levels, focusing on restoring balance to the body's natural healing mechanisms.
Individualized Assessment: A thorough evaluation of the individual's overall health, medical history, and symptoms is essential in homeopathic treatment. This personalized approach allows the homeopath to tailor the treatment plan to address the root cause of high creatinine treatment.
Constitutional Remedies: Homeopathic remedies selected based on the individual's constitutional type can help stimulate the body's innate healing response. These remedies aim to rebalance the body's vital force, promoting optimal kidney function and lowering creatinine levels.
Symptom-Based Remedies: Specific homeopathic remedies may be prescribed based on the unique symptoms associated with high creatinine treatment. These remedies target symptoms such as fatigue, swelling, urinary problems, and other signs of kidney dysfunction.
Renal Restoration: Approaches to Kidney Failure Treatment
Kidney failure, also known as renal failure, is a serious condition where the kidneys lose their ability to function properly, leading to a buildup of toxins and waste products in the body. Homeopathy offers a gentle yet comprehensive approach to supporting kidney health and managing the symptoms of Treatment for kidney failure.
Individualized Assessment: Homeopathic treatment begins with a thorough evaluation of the individual's overall health, medical history, and specific symptoms associated with kidney failure. This personalized approach allows the homeopath to tailor the treatment plan to address the underlying causes and unique manifestations of the condition.
Constitutional Remedies: Homeopathic remedies selected based on the individual's constitutional type can help stimulate the body's innate healing mechanisms and support overall kidney function. These remedies aim to address the underlying imbalances contributing to Treatment for kidney failure and promote holistic healing.
Symptom-Based Remedies: In addition to constitutional remedies, specific homeopathic remedies may be prescribed to target the symptoms of kidney failure, such as fatigue, swelling, high blood pressure, nausea, and urinary problems. These remedies work in harmony with the body's natural processes to alleviate discomfort and improve quality of life.
What Causes Chronic Kidney Disease and How to Treat It: An Understanding
chronic kidney disease causes and treatment (CKD) is a progressive condition characterized by the gradual loss of kidney function over time. Understanding the causes of CKD is crucial for developing effective treatment strategies. Homeopathy offers a holistic approach to managing CKD, focusing on addressing the underlying causes and supporting kidney function.
Causes of Chronic Kidney Disease
Diabetes: Uncontrolled diabetes can damage the kidneys over time, leading to CKD.
Hypertension: High blood pressure can strain the kidneys, causing damage and increasing the risk of CKD.
Polycystic Kidney Disease: Inherited condition characterized by the growth of cysts in the kidneys, leading to CKD.
Autoimmune Diseases: Conditions like lupus and vasculitis can cause inflammation and damage to the kidneys.
Other Factors: Smoking, obesity, family history of kidney disease, and certain medications can also contribute to CKD.
Different Strategies for Treating Kidney Failure: Topical Dialysis
kidney failure treatment without dialysis presents significant challenges, but for those seeking alternatives to dialysis, homeopathy offers a comprehensive approach focused on supporting kidney function and overall well-being.
Individualized Assessment: Homeopathic treatment begins with a thorough evaluation of the individual's health history, symptoms, and specific manifestations of kidney failure treatment without dialysis. This personalized approach allows the homeopath to tailor the treatment plan to address the underlying causes and unique needs of the individual.
Constitutional Remedies: Homeopathic remedies are selected based on the individual's constitutional type, aiming to stimulate the body's innate healing mechanisms and restore balance. These remedies work holistically to support kidney function and overall health.
Symptom-Based Remedies: In addition to constitutional remedies, specific homeopathic remedies may be prescribed to alleviate symptoms associated with kidney failure, such as fatigue, swelling, high blood pressure, and urinary problems. These remedies target the individual's symptoms, promoting relief and enhancing quality of life.
#Treatment for kidney failure#high creatinine treatment#chronic kidney disease causes and treatment#kidney failure treatment without dialysis#Acute Kidney Injury Treatment#Chronic Kidney Disease
0 notes