#Help Prevent Autoimmune Disease
Text
"The Biden administration on Thursday [August 15, 2024] released prices for the first 10 prescription drugs that were subject to landmark negotiations between drugmakers and Medicare, a milestone in a controversial process that aims to make costly medications more affordable for older Americans.
The government estimates that the new negotiated prices for the medications will lead to around $6 billion in net savings for the Medicare program in 2026 alone when they officially go into effect, or 22% net savings overall. That is based on the estimated savings the prices would have produced if they were in effect in 2023, senior administration officials told reporters Wednesday.
The Biden administration also expects the new prices to save Medicare enrollees $1.5 billion in out-of-pocket costs in 2026 alone.
“For so many people, being able to afford these drugs will mean the difference between debilitating illness and living full lives,” Chiquita Brooks-LaSure, administrator for the Centers for Medicare & Medicaid Services, told reporters. “These negotiated prices. They’re not just about costs. They are about helping to make sure that your father, your grandfather or you can live longer, healthier.”
It comes one day before the second anniversary of President Joe Biden’s signature Inflation Reduction Act, which gave Medicare the power to directly hash out drug prices with manufacturers for the first time in the federal program’s nearly 60-year history.
Here are the negotiated prices for a 30-day supply of the 10 drugs, along with their list prices based on 2023 prescription fills, according to a Biden administration fact sheet Thursday.
What Medicare and beneficiaries pay for a drug is often much less than the list price, which is what a wholesaler, distributor or other direct purchaser paid a manufacturer for a medication before any discounts...

The administration unveiled the first set of medications selected for the price talks in August 2023, kicking off a nearly yearlong negotiation period that ended at the beginning of the month.
The final prices give drugmakers, which fiercely oppose the policy, a glimpse of how much revenue they could expect to lose over the next few years. It also sets a precedent for the additional rounds of Medicare drug price negotiations, which will kick off in 2025 and beyond.
First 10 drugs subject to Medicare price negotiations
Eliquis, made by Bristol Myers Squibb, is used to prevent blood clotting to reduce the risk of stroke.
Jardiance, made by Boehringer Ingelheim and Eli Lilly, is used to lower blood sugar for people with Type 2 diabetes.
Xarelto, made by Johnson & Johnson, is used to prevent blood clotting, to reduce the risk of stroke.
Januvia, made by Merck, is used to lower blood sugar for people with Type 2 diabetes.
Farxiga, made by AstraZeneca, is used to treat Type 2 diabetes, heart failure and chronic kidney disease.
Entresto, made by Novartis, is used to treat certain types of heart failure.
Enbrel, made by Amgen, is used to treat autoimmune diseases such as rheumatoid arthritis.
Imbruvica, made by AbbVie and J&J, is used to treat different types of blood cancers.
Stelara, made by Janssen, is used to treat autoimmune diseases such as Crohn’s disease.
Fiasp and NovoLog, insulins made by Novo Nordisk.
In a statement Thursday, Biden called the new negotiated prices a “historic milestone” made possible because of the Inflation Reduction Act. He specifically touted Vice President Kamala Harris’ tiebreaking vote for the law in the Senate in 2022.
Harris, the Democratic presidential nominee, said in a statement that she was proud to cast that deciding vote, adding there is more work to be done to lower health-care costs for Americans.
“Today’s announcement will be lifechanging for so many of our loved ones across the nation, and we are not stopping here,” Harris said in a statement Thursday, noting that additional prescription drugs will be selected for future rounds of negotiations."
-via CNBC, August 15, 2024
#public health#healthcare#united states#us politics#biden#harris#kamala harris#medicare#medicaid#healthcare accessibility#prescription drugs#big pharma#insulin#good news#hope
3K notes
·
View notes
Text
Apropos of absolutely nothing at all, oral and throat cancers from HPV don’t only occur in guys; anyone who engages in oral sex should be on the lookout for them! Symptoms include sudden loss of taste, swelling, numbness, a persistent sore throat, and pain. HPV can also cause cancers of the phallus, vulva, and anus. Because it’s a viral related cancer it can be especially dangerous for those with immune conditions, including HIV or some autoimmune diseases treated with immunosuppressants.
However the HPV vaccine is effective at preventing all of these cancers. In countries with high uptake many forms of cervical cancers have vanished among young people. The vaccine is most effective for younger children between 10-13 so if you have kids, siblings, nieces or nephews, push for them to get it! It’s also now recommended for adults up to middle aged. Even if you’ve already contracted one HPV strain, the vaccine may still be helpful. Although there’s increasing evidence of efficacy at just one dose, it’s most effective if you get all three in the series so don’t wait.
And if you’re eligible for Pap smears, get them. They might not be comfortable but they are one of the most effective medical tests invented in the twentieth century.
100 notes
·
View notes
Text
Islanders living with Type 1 diabetes are eligible to receive help with the cost of insulin pumps and related supplies beginning Sept. 1.
The PEI Insulin Pump Program provides financial assistance to medically eligible residents, according to a news release from the province. The program was previously open to those up to age 25, however the province has now removed that age limit.
[...]
The province says there are approximately 1,100 people on Prince Edward Island who are living with Type 1 diabetes, which is an autoimmune disease that prevents the pancreas from producing insulin.
Continue Reading
Tagging: @newsfromstolenland
#diabetes#type 1 diabetes#insulin#healthcare#prince edward island#cdnpoli#canadian politics#canadian news#canada
59 notes
·
View notes
Text
An estimated 2.8 million people worldwide have multiple sclerosis (MS). This autoimmune condition is the result of the immune system damaging parts of the nerves in the brain and spinal cord, which can lead to problems with movement, vision, balance and sensation.
While many MS symptoms can be managed, there's currently no way to cure or prevent the condition. This is due to the complex immune response that leads to this disease.
But a blood test recently developed by me and my colleagues has allowed us to estimate the strength of the immune response in people with MS.
This finding may not only bring us one step closer to understanding the causes of MS, but to developing better treatments for the condition.
Continue Reading.
99 notes
·
View notes
Note
I saw your post and I'm so sorry. Elimination diets suck.
Can I ask how/where you buy the French flour?? 👀👀👀 as an autoimmune disease haver myself, this could be incredibly helpful for me. Thank you and good luck on your GF month 💛
I was gonna try through here this time. I’ve gotten a different brand through Amazon and really liked it but would like to avoid going through Amazon.
Only issue is they talk about needing to fridge the bag to prevent flour moths so I guess I need to look into that… didn’t have that problem with the other import I used.
29 notes
·
View notes
Text
Look, I understand the people who are giving examples for women getting abortions such as the fetus will die after birth or they cannot financially support a child. I completely agree that it’s important to come up with these examples because the other side doesn’t seem to understand that.
But here, the one place on the internet that I am able to say this, I don’t give a flying fuck if a women is having unprotected sex with every person on the block. I don’t care if people think they are “using abortion as birth control.” I don’t fucking care.
If a pregnant individual doesn’t want a baby for any fucking reason, they deserve to have an abortion. Full stop.
I know I’m what the other side is telling everyone that all pro-choicers are and I don’t fucking care. Are there options to help prevent pregnancy? Absolutely. I got an IUD for this exact reason. Should a person go out of their way to have unprotected sex knowing they have an abortion as a backup? No, of course not. But none of these things is a reason anyone should be forced to endure a pregnancy they don’t want or can’t physically, mentally, or financially handle.
I desperately want kids one day. I’m engaged to the love of my life and I have wanted children with him since we first started dating. But if I had gotten pregnant while in college? Abortion. If I had OR WILL get pregnant during a time where my debilitating autoimmune disease was/is so bad I couldn’t function? Abortion. If my IUD fails at a time where I can’t support a child? Abortion.
Everyone with a goddamn uterus should have the ability to decide if they want to carry a pregnancy or not. It disgusts me that in 2024, this is an issue once again.
I’m planning on attending medical school at some point in the next few years and I absolutely plan on advocating for abortion rights, regardless of my chosen specialty. And I know there are methods of activism I can do know. But I feel so completely powerless and it breaks my heart.
64 notes
·
View notes
Text
Long COVID: Lasting effects of COVID-19 - Mayo Clinic - Published Aug 25, 2024
After any coronavirus disease 2019 (COVID-19) illness, no matter how serious, some people report that symptoms stay for months. This lingering illness has often been called long COVID or post-COVID-19 syndrome. You might hear it called long-haul COVID or post-acute sequelae of SARS-CoV-2 (PASC).
There is no universal definition of long COVID right now.
In the U.S., some experts have defined long COVID as a long-lasting, called chronic, condition triggered by the virus that causes COVID-19. (1p31) The medical term for this is an infection-associated chronic condition.
As researchers learn more about long COVID, this definition may change.
What are the most common symptoms of long COVID?
In research studies, more than 200 symptoms have been linked to long COVID. Symptoms may stay the same over time, get worse, or go away and come back.
Common symptoms of long COVID include:
Extreme tiredness, especially after activity.
Problems with memory, often called brain fog.
A feeling of being lightheaded or dizzy.
Problems with taste or smell.
Other symptoms of long COVID include:
Sleep problems.
Shortness of breath.
Cough.
Headache.
Fast or irregular heartbeat.
Digestion problems, such as loose stools, constipation or bloating.
Some people with long COVID may have other illnesses. Diseases caused or made worse by long COVID include migraine, lung disease, autoimmune disease and chronic kidney disease.
Diseases that people may be diagnosed with due to long COVID include:
Heart disease.
Mood disorders.
Anxiety.
Stroke or blood clots.
Postural orthostatic tachycardia syndrome, also called POTS.
Myalgic encephalomyelitis-chronic fatigue syndrome, also called ME-CFS.
Mast cell activation syndrome.
Fibromyalgia.
Diabetes.
Hyperlipidemia.
People can get long COVID symptoms after catching the COVID-19 virus even if they never had COVID-19 symptoms. Also, long COVID symptoms can show up weeks or months after a person seems to have recovered.
And while the COVID-19 virus spreads from person to person, long COVID is not contagious and doesn't spread between people.
Why does COVID-19 cause ongoing health problems?
Current research has found that long COVID is a chronic condition triggered by the virus that causes COVID-19. The medical term for this is an infection-associated chronic condition.
Researchers don't know exactly how COVID-19 causes long-term illness, but they have some ideas. Theories include:
The virus that causes COVID-19 upsets immune system communication. This could lead immune cells to mistake the body's own cells as a threat and react to them, called an autoimmune reaction.
Having COVID-19 awakens viruses that haven't been cleared out of the body.
The coronavirus infection upsets the gut's ecosystem.
The virus may be able to survive in the gut and spread from there.
The virus affects the cells that line blood vessels.
The virus damages communication in the brain stem or a nerve that controls automatic functions in the body, called the vagus nerve.
Because the virus that causes COVID-19 continues to change, researchers can't say how many people have been affected by long COVID. Some researchers have estimated that 10% to 35% of people who have had COVID-19 went on to have long COVID.
What are the risk factors for long COVID?
Risk factors for long COVID are just starting to be known. In general, most research finds that long COVID is diagnosed more often in females of any age than in males. The long COVID risk also may be higher for people who have cardiovascular disease before getting sick.
Some research also shows that getting a COVID-19 vaccine may help prevent long COVID.
Many other factors may raise or lower your risk of long COVID, but research is still ongoing.
What should I do if I have long COVID symptoms?
See a healthcare professional if you have long COVID symptoms. Part of long COVID's definition is symptoms that last for three months.
But at this time, no test can say whether you have long COVID. Since you may not have symptoms if you have an infection with the COVID-19 virus, you may not know you had it. Some people have mild symptoms and don't take a COVID-19 test. Others may have had COVID-19 before testing was common.
Long COVID symptoms may come and go or be constant. They also can start any time after you had COVID-19. But symptoms still need to be documented for at least three months in order for a health care professional to diagnose long COVID.
Healthcare professionals may treat your symptoms or conditions before a long COVID-19 diagnosis. And they may work to rule out other conditions over the time you start having symptoms.
Your healthcare team might do lab tests, such as a complete blood count or liver function test. You might have other tests or procedures, such as chest X-rays, based on your symptoms.
The information you give and any test results can help your healthcare professional come up with a treatment plan.
Care for long COVID
It can be hard to get care for long COVID. Treatment may be delayed while you work with healthcare professionals. And people with long COVID may have their health problems dismissed by others, including healthcare professionals, family members or employers.
For people with cultural or language barriers, getting a long COVID diagnosis can be even harder. Pulling together information about symptoms and timing can be a challenge too. This is especially true when medical history is fragmented or when someone is managing symptoms related to memory or that affect the thought process.
Underdiagnosis may be more common among people who have less access to healthcare or who have limited financial resources.
If you're having long COVID symptoms, talk with your healthcare professional. It can help to have your medical records available before the appointment if you are starting to get care at a new medical office.
To prepare for your appointment, write down:
When your symptoms started and if they come and go.
What makes your symptoms worse.
How your symptoms affect your activities.
Questions you have about your illness.
List medicines and anything else you take, including nutrition supplements and pain medicine that you can get without a prescription. Some people find it helpful to bring a trusted person to the appointment to take notes.
Keep visit summaries and your notes in one place. That can help you track what actions you need to take or what you've already tried to treat your symptoms.
Also, you might find it helpful to connect with others in a support group and share resources.
How long can long COVID last?
The conditions linked as part of long COVID may get better over months or may last for years.
What treatment is available for long COVID?
Healthcare professionals treat long COVID based on the symptoms. For tiredness, your healthcare professional may suggest that you be active only as long as your symptoms stay stable. If you start to feel worse, rest and don't push through your tiredness.
For symptoms of pain, breathlessness or brain fog, work with your healthcare professional to find a treatment plan that works for you. That may include medicine you can get without a prescription for pain, prescription medicine, supplements and referrals to other healthcare team members.
For loss of taste or smell, a process to retrain the nerves involved in those processes may help some people. The process is called olfactory training. For people with POTS or a fast heartbeat, the healthcare professional may suggest prescription medicine as well as a plan to stay hydrated.
Treatment for other long COVID symptoms may be available so contact your healthcare professional for options.
Next steps for Long COVID
Long COVID makes life more difficult for many people. To provide better options for care, research is going on to better understand this illness. In the meantime, adults or children with long COVID may be able to get support for daily activities affected by the illness.
#long covid#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator
10 notes
·
View notes
Text
Why does Quinlan Vos wear hand wraps?
It's never explained why Quinlan wraps his hands in Disney or Legends Canon, so I am going to speculate wildly!



It's not a cultural thing; all of the Kiffu Guardians we see wear gloves and Tinte Vos is shown barehanded.
It's not to control his psychometry, since his fingers aren't covered and psychometry doesn't appear to require skin contact - his Dark Disciple character model is wearing gloves as part of his bounty hunter disguise, and he uses his psychometry multiple times throughout the book. Also, Vildar Mac is wearing gloves when he uses psychometry in the High Republic comics.
So what could be the reason? There's a few options I can think of:
Wrist support. People who participate in combat sports such as boxing will wrap their hands to stabilize their wrists by immobilizing the bones and ligaments there. This helps prevent sprains, fractures, and other injuries. Boxing wraps also help distribute the force of a punch more evenly across the hand and wrist and help prevent hyperflexion and overextension.
Compression for neuropathy. Specifically, I would guess, for small fiber peripheral neuropathy, which causes pain in the hands and feet. Compression can help alleviate this pain.


(Left is a boxing wrap, right is an elastic wrist brace.)
I personally feel the first option is more likely, where he wraps his wrists and keeps going up his forearms for the aesthetic™️. He just strikes me as person who is ready to get in a fistfight at any moment.
However, the second option lends itself to some interesting possibilities! Small fiber peripheral neuropathy can have many causes, including diabetes, thyroid disease, autoimmune disorders like Ehlers-Danlos, and certain medications.
20 notes
·
View notes
Text
alright i can breathe on my own again so back into this thought. here's a few ways all the elements work in healing in my brain*
Quintessence healing does a lot with the electrical impulses of the body; most of their work is possible due to their unique abilities to alleviate pain: neurological pains, including migraines. bone setting. internal, external, and extensive injury. sleep, dream, and memory. autoimmune disease. surgery. seizure disorders. acute pain. dentistry. general medical practice
Water healing is the most versatile, as the majority of organic material is driven by water: dermatology. uncontrolled/high fever. hyperthermia. burns. blood and blood pressure. sinuses. cartilage and collagen disorders. fainting disorders. chronic pain. vision disorders. scarring/scar healing/prevention
Fire healing deals a lot with pressure and relaxation: wound cautery. viral and bacterial illness (will start a fever or keep one in check - out of control fevers visit water). hypothermia. heat therapy: massage, hot baths, etc. physical therapy. arthritic/joint disorders, chronic pain
Air healing focuses mostly on areas of the body where oxygen or air pockets are at play: lung and breathing disorders. sinuses. learning, speech and communication, hearing. muscle pains. anxiety. fatigue and chronic fatigue
Earth healing works in grounding, and is also very diverse: mental health. psychiatrics and emotions. reproductive health. labor and delivery. balance and some fainting disorders. occupational therapy. creation of pharmacy products: tinctures, salves, ointments, orals, drops, etc.; creation of splints, casts, and assistive devices
Multi ghouls are cool in that, if they feel the call towards healing, they can lean on any element and pick up skills quickly and easily, depending on their unique makeup. Most assist in general practice medicine, but often blend powers from other elements together to create unique solutions for their patients
*please note no one ever needs be 'fixed,' and having any type of disorder or disability does not make anyone less, especially in the eyes of the abbey. the ghouls of the infirmary seek to help improve quality of life by easing symptoms for those that request it. there is nothing but love and respect for all residents and visitors of the infirmary 🤍
#i have so much i can say about this#please ask any questions you have i will talk about this forever#as i tell my patients we might not be able to heal the problem but we can make it more bearable 🤍#medical ghouls#nameless ghouls#the band ghost#ghoul headcanons#ghoul hcs
26 notes
·
View notes
Text
Around 40 000 years ago, Homo Sapiens came to Europe and genocided Homo Neanderthalensis (Adams event?). Thus, all modern humans in Europe and Northern Africa have a bit of Neanderthals DNA.
Logically, the Neanderthals DNA should have disappeared completely in modern humans by now... but it didn't. Why? Most likely because of adaptive introgression: process by which adaptation occurs via genetic variants that were introgressed into the recipient population from the donor population (introgression - incorporation of DNA from one species to the gene pool of another). Sapiens really needed some Neanderthals genes for protection from European infections.
The problem, however, is that Neanderthals genes protect us from infections in a short run. In a long run, our Sapiens bodies start to consider Neanderthals DNI as the alien DNI, causing rejection, which leads to different autoimmune disorders and sometimes even cancer. The bloodline curse we have to bear is paying for sinners of our ancestors...
In particular, biologists and archaeologists established a connection between Neanderthals DNI and kidney membranous neuropathy: the more you have Neanderthals genes, the higher the chance to develop such unpleasant disorder. COVID-19 severity is also dependent on the Neanderthal genome.
Neanderthals had lived in quite cold places in those times, and thus, they had to eat more meat. "Alas, though fat is easier to digest, it’s scarce in cold conditions, as prey animals themselves burn up their fat stores and grow lean. So Neanderthals must have eaten a great deal of protein, which is tough to metabolize and puts heavy demands on the liver and kidneys to remove toxic byproducts. In fact, we humans have a “protein ceiling” of between 35 and 50 percent of our diet; eating too much more can be dangerous. Ben-Dor thinks that Neanderthals’ bodies found a way to utilize more protein, developing enlarged livers and kidneys, and chests and pelvises that widened over the millennia to accommodate these beefed-up organs. To cope with the fat famine, Neanderthals probably also specialized in hunting gigantic animals like mammoths, which retain fat longer in poor conditions and require greater strength but less energy and speed to kill."
Since Neanderthals had such large kidneys, they needed a greater scale of kidney cleansing. And that's why they ate a lot of cranberries and lingonberries: even nowadays, cranberries extract is sold in pharmacies to people with kidney problems.
Cranberries properties: rich in antioxidant compounds, prevention of urinary tract infections, support anti-aging, skin health, heart health, reduce the risk of stomach ulcers, antibacterial properties, protect against certain cancers, support eye health and vision, promote a healthy immune system, etc.
Lingonberries are especially high in the antioxidant "anthocyanins," which is known to prevent oxidation of blood cholesterol and aid in keeping blood vessels healthy. Researchers believe these potent antioxidants may be able to help reduce the risk of heart disease and even some cancers.
Thus, people with kidney memranous neuropathy or with high risk of its development, people with severe post-COVID complications, people with high levels of Neanderthals DNI should come to Lithuania! :D We have a lot of cranberries and lingonberries sold not in pharmacies at wild prices but in average grocery stores! :D
#history#biology#medicine#archaeology#covid 19#post covid#membranous neuropathy#kidney disease#neanderthals#genetics#Lithuania#health#healthy food
8 notes
·
View notes
Text
The Physiology Of The Liver
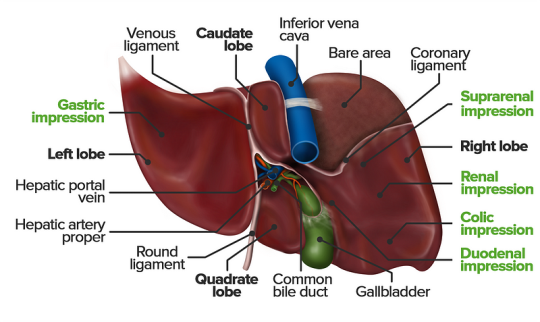
The liver is a vital organ responsible for numerous functions including metabolism, immunity, digestion, detoxification, and vitamin storage. It weighs around 2% of an adult’s body weight and is unique due to its dual blood supply from the portal vein (75%) and the hepatic artery (25%).
Cellular Structure
The liver’s functional unit is the lobule, which is hexagonal in shape. Each corner of the hexagon has a portal triad consisting of the portal vein, hepatic artery, and bile duct. The lobule is composed mainly of hepatocytes, which have distinct apical and basolateral membranes. Hepatocytes are categorized into three zones based on their function and blood supply:
Zone I (periportal region): Closest to the blood supply, involved in oxidative metabolism (e.g., gluconeogenesis, bile formation).
Zone II (pericentral region): Sits between Zones I and III.
Zone III: Farthest from the blood supply, primarily involved in detoxification and biotransformation.
Blood and bile flow in opposite directions within the liver. The space of Disse, between the hepatocytes and the sinusoidal lumen, contains Kupffer cells (macrophages) and Ito cells (fat-storing stellate cells).
Development
The liver develops from endodermal cells of the foregut as the hepatic diverticulum around the fourth week of embryonic development. It undergoes complex differentiation influenced by various pathways (e.g., Wnt/β-catenin, FGF). By the sixth week, the liver participates in hematopoiesis, and hepatocytes begin bile production by the 12th week.
Organ Systems and Functions
The liver interacts with multiple body systems:
Digestive and Metabolic Roles: Aids in digestion, stores fat-soluble vitamins, and handles cholesterol.
Hematological Functions: Produces clotting factors and proteins.
Detoxification: Metabolizes drugs and other xenobiotics through phase I (oxidation, reduction, hydrolysis) and phase II (conjugation) reactions.
Bilirubin Metabolism: Converts heme to unconjugated bilirubin, then conjugates it for excretion.
Hormonal and Protein Synthesis: Involved in thyroid hormone activation and synthesis of nearly all plasma proteins.
Related Testing
Liver function tests (LFTs), including ALT, AST, bilirubin, alkaline phosphatase, and gamma-glutamyl transpeptidase (GGT), help assess liver health. Imaging techniques like ultrasound, CT, and MRI are also employed to identify liver abnormalities.
Pathophysiology
Cirrhosis results from chronic liver injury (e.g., due to alcoholism, hepatitis B and C), leading to fibrosis and necrosis. It causes symptoms like portal hypertension, coagulopathy, and jaundice. Hepatitis viruses (A, B, C, D, E), autoimmune diseases (e.g., primary biliary cholangitis), and metabolic conditions (e.g., non-alcoholic fatty liver disease) also contribute to liver pathology.
Clinical Significance
Understanding liver physiology helps manage conditions like viral hepatitis, alcoholic liver disease, benign liver lesions, and liver cancers. Early detection through appropriate testing and management strategies is essential for preventing end-stage liver disease and improving patient outcomes
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at [email protected] and let us support you on your academic journey. We wish you success and professional excellence.
#medical students#healthcare#nursing school#nursing student#medicine#medical help#academic assignments#university student#medical university#university life#university#studying#study motivation#study blog#studyblr community#study inspiration#studyspo#studyblr#student#study aesthetic#medical student#aesthetic#medical school#case study
2 notes
·
View notes
Text
👁️ Unexpected Reasons for Eye Irritation: What You Need to Know👁️
Remember when I shared earlier this week about my recent eye issues? It got me thinking about the symbolic meaning behind our physical discomforts.

While we often attribute redness, irritation, and watering eyes to common causes like allergies or tiredness, there are several lesser-known factors that could be behind your eye discomfort. Here are some to consider, along with my symbolic interpretations for each.
1. Digital Eye Strain: Excessive screen time can lead to digital eye strain, causing symptoms like redness, dryness, and irritation. Consider taking breaks and using blue light-blocking glasses for relief. If you’re experiencing Digital Eye Strain, this may indicate the overwhelming demands of modern life and the need to find balance in digital consumption to avoid feeling drained and fatigued.
2. Meibomian Gland Dysfunction (MGD): Dysfunction of the glands in your eyelids can cause evaporative dry eye, leading to red, irritated eyes, especially in the mornings or after long periods of screen use. Symbolizes the importance of addressing underlying issues that may be obstructing our ability to see clearly and approach situations with clarity.
3. Blepharitis: Inflammation of the eyelids can result in red, swollen eyelids, itching, and irritation. Good lid hygiene and warm compresses can help manage symptoms.
4. Environmental Sensitivities: Smoke, air pollution, or strong odors can irritate your eyes, causing discomfort and watering. Symbolizes the impact of external influences on our perception and well-being, urging us to create environments that support our growth and comfort.
5. Dry Eye Syndrome: Low humidity, wind, air conditioning, and certain medications can contribute to dry eyes, leading to redness and irritation.Symbolizes the need for emotional nourishment and hydration in our lives, reminding us to seek fulfillment and connection to prevent feeling dried out and depleted.
6. Systemic Conditions: Autoimmune diseases, thyroid disorders, and hormonal changes can affect tear production and eye health, leading to dryness and irritation.Symbolizes the interconnectedness of our physical and emotional health, highlighting the importance of holistic well-being in maintaining clarity of vision and purpose.
7. Medications: Some medications can cause dry eyes as a side effect, so be mindful of any changes in your eye health when starting new medications. Symbolizes the potential side effects of relying solely on external solutions to our problems, encouraging us to seek natural remedies and lifestyle changes where possible.
8. Cosmetic Products: Certain makeup and skincare products may contain allergens or irritants that can cause redness, itching, and watering in sensitive individuals.
Hope this helps someone going through a similar issue!! Remember to stay informed, and take care of those precious peepers!
#blue eyed girl#eye health#healthy living#health#healthcare#healthylifestyle#medicine#public health#wellness#health and wellness#health & fitness#health care#immune system#mental health#energy#symbolism#symbols
3 notes
·
View notes
Text
I feel so, so defeated. My partner is on vacation, so I've been alone for about a week now. Work has really been a series of annoying problems for the past couple weeks — and I've had to involve my supervisor, which I have rarely had to do at all this year. Nothing I could have prevented, but I just really wish it wasn't this week that my name keeps popping up in her email due to problems, because we're about to get our placement assignments for next year, and I will honestly be really devastated if I get moved to a new site at work.
So I worked all through the weekend to try and get through some of the mess. Then I had a 3 hour dentist appointment on Monday. The only things I've been looking forward to have been going to my choir, should have been tonight, getting a haircut, which was scheduled for tomorrow, the weekend, which is supposed to be properly warm, and my partner coming home, on Monday.
But no. I just got my first ever positive covid test (from that wretched dentist appointment, perhaps...). I'm extremely grateful not to infect my partner, because she had a terrible time with covid... and I'm glad not to need to quarantine in a 1-bedroom apartment. But I feel so tired and I really wish someone else could clean the cat litter tonight. And make dinner. And do the laundry. And I feel so, so, miserable thinking about not seeing her for even longer than I thought. With shaggy overgrown hair. And if my autoimmune disease flares up (which the specialist I see told me it likely would with covid, or any cold/flu) perhaps some pain, too.
Work isn't even in a state where I can take a sick day right now... So I'm just going to work for free, but from home for once, for my last two remaining sick days. Then take a weekend that should have been fun and warm outside with a fresh haircut, awaiting my partner's return, and spend it completely indoors. Then, come Monday, not see my partner when she gets home, and decide whether I'd like to take an unpaid sick day and keep falling further behind, or risk infecting everyone at work.
Bleh. I probably should take some time for some gratitudes... like I have two legs that work for the most part, I have good doctor if I do have a flare up who will help me, summer is coming, my cat is really good, I have a whole house to quarantine in, I've had three offers already from friends/family to drop stuff off if I need it, I will see my partner again pretty soon, I will be fine, this will all pass...
...but man, this stinks!
#personal#and I feel so obnoxious for complaining#because my life is pretty good#and there's a lot going on in the world right now#but I just feel really sad#four years later... it finally happened
5 notes
·
View notes
Text
Understanding Different Types of Diabetes and Their Impact on the Body

Diabetes is a chronic condition that affects millions of people worldwide. It disrupts the body's ability to regulate blood sugar (glucose) levels, leading to serious health complications if not managed properly. There are several types of diabetes, each with unique characteristics and impacts on the body. This article will explore the different types of diabetes, how they affect the body, and the tests provided by RML Pathology to diagnose and manage this condition.
1. Type 1 Diabetes
Description:
Type 1 diabetes is an autoimmune disease where the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This results in little to no insulin production, which is essential for regulating blood sugar levels.
Impact on the Body:
Requires lifelong insulin therapy.
Increases the risk of complications such as diabetic ketoacidosis (DKA), a potentially life-threatening condition.
Long-term complications include cardiovascular disease, kidney damage (nephropathy), nerve damage (neuropathy), and vision problems (retinopathy).
Can cause frequent urination, excessive thirst, extreme hunger, weight loss, fatigue, and irritability.
2. Type 2 Diabetes
Description:
Type 2 diabetes is the most common form of diabetes. It occurs when the body becomes resistant to insulin or when the pancreas does not produce enough insulin. Lifestyle factors such as obesity, poor diet, and lack of exercise significantly contribute to its development.
Impact on the Body:
Often managed with lifestyle changes, oral medications, and sometimes insulin.
Can lead to complications like heart disease, stroke, kidney disease, eye problems, and nerve damage.
Symptoms include increased thirst, frequent urination, increased hunger, fatigue, blurred vision, slow-healing sores, and frequent infections.
3. Gestational Diabetes
Description:
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased needs. It usually resolves after childbirth but increases the risk of developing type 2 diabetes later in life.
Impact on the Body:
Can cause high blood pressure during pregnancy (preeclampsia).
Increases the risk of having a large baby, leading to complications during delivery.
May result in low blood sugar levels in the newborn and a higher risk of obesity and type 2 diabetes in the child later in life.
4. Prediabetes
Description:
Prediabetes is a condition where blood sugar levels are higher than normal but not high enough to be classified as type 2 diabetes. It is a critical stage for intervention to prevent the progression to type 2 diabetes.
Impact on the Body:
Often reversible with lifestyle changes such as diet and exercise.
Increases the risk of developing type 2 diabetes, heart disease, and stroke.
Symptoms are often absent or mild, making regular screening important.
Tests Provided by RML Pathology
RML Pathology offers a comprehensive range of tests to diagnose and manage diabetes effectively. These include:
Fasting Blood Glucose Test:
Measures blood sugar levels after fasting for at least 8 hours.
Helps diagnose diabetes and prediabetes.
HbA1c Test:
Provides an average blood sugar level over the past 2-3 months.
Used to diagnose diabetes and monitor long-term glucose control.
Oral Glucose Tolerance Test (OGTT):
Measures the body's response to a glucose solution.
Commonly used to diagnose gestational diabetes.
Random Blood Sugar Test:
Measures blood sugar levels at any time of the day.
Useful for diagnosing diabetes when symptoms are present.
Gestational Diabetes Test:
Specifically designed for pregnant women to detect gestational diabetes.
Conclusion
Understanding the different types of diabetes and their impact on the body is crucial for effective management and prevention. Regular testing and early detection play a vital role in managing diabetes and preventing complications. RML Pathology provides a wide range of diagnostic tests to help you monitor and manage your diabetes effectively. If you have any symptoms or risk factors for diabetes, consider visiting RML Pathology for a comprehensive evaluation.
Contact RML Pathology Today:
📞 7991602001, 7991602002 📞 0522-4034100 🌐 www.rmlpathology.com
Experience the best in diagnostics with RML Pathology – where your health is our priority.
#diabetes#type 1 diabetes#type 2 diabetes#gestational diabetes#prediabetes#diabetes management#blood sugar#glucose levels#RML Pathology#diabetes tests#HbA1c#fasting blood glucose#oral glucose tolerance test#random blood sugar test#health#healthcare#diabetes diagnosis
2 notes
·
View notes
Text
Tara Ghormley has always been an overachiever. She finished at the top of her class in high school, graduated summa cum laude from college and earned top honors in veterinary school. She went on to complete a rigorous training program and build a successful career as a veterinary internal medicine specialist. But in March 2020 she got infected with the SARS-CoV-2 virus—just the 24th case in the small, coastal central California town she lived in at the time, near the site of an early outbreak in the COVID pandemic. “I could have done without being first at this,” she says.
Almost three years after apparently clearing the virus from her body, Ghormley is still suffering. She gets exhausted quickly, her heartbeat suddenly races, and she goes through periods where she can't concentrate or think clearly. Ghormley and her husband, who have relocated to a Los Angeles suburb, once spent their free time visiting their “happiest place on Earth”—Disneyland—but her health prevented that for more than a year. She still spends most of her days off resting in the dark or going to her many doctors' appointments. Her early infection and ongoing symptoms make her one of the first people in the country with “long COVID,” a condition where symptoms persist for at least three months after the infection and can last for years. The syndrome is known by medical professionals as postacute sequelae of COVID-19, or PASC.
People with long COVID have symptoms such as pain, extreme fatigue and “brain fog,” or difficulty concentrating or remembering things. As of February 2022, the syndrome was estimated to affect about 16 million adults in the U.S. and had forced between two million and four million Americans out of the workforce, many of whom have yet to return. Long COVID often arises in otherwise healthy young people, and it can follow even a mild initial infection. The risk appears at least slightly higher in people who were hospitalized for COVID and in older adults (who end up in the hospital more often). Women and those at socioeconomic disadvantage also face higher risk, as do people who smoke, are obese, or have any of an array of health conditions, particularly autoimmune disease. Vaccination appears to reduce the danger but does not entirely prevent long COVID.
The most common, persistent and disabling symptoms of long COVID are neurological. Some are easily recognized as brain- or nerve-related: many people experience cognitive dysfunction in the form of difficulty with memory, attention, sleep and mood. Others may seem rooted more in the body than the brain, such as pain and postexertional malaise (PEM), a kind of “energy crash” that people experience after even mild exercise. But those, too, result from nerve dysfunction, often in the autonomic nervous system, which directs our bodies to breathe and digest food and generally runs our organs on autopilot. This so-called dysautonomia can lead to dizziness, a racing heart, high or low blood pressure, and gut disturbances, sometimes leaving people unable to work or even function independently.
25 notes
·
View notes
Text
Causes and risk factors in Chronic pancreatitis
Title: Understanding the Causes and Risk Factors of Chronic Pancreatitis
Chronic pancreatitis is a debilitating condition characterized by inflammation and irreversible damage to the pancreas. While the exact cause of chronic pancreatitis can vary from person to person, several factors contribute to its development. By understanding these causes and risk factors, individuals can take proactive steps to minimize their risk and manage the condition effectively.
1. Alcohol Consumption:
Chronic alcohol abuse is one of the leading causes of chronic pancreatitis. Excessive alcohol consumption over a prolonged period can damage pancreatic cells, leading to inflammation and scarring. It's essential to moderate alcohol intake and seek help if struggling with alcohol dependence.
2. Genetics:
Genetic factors play a significant role in predisposing individuals to chronic pancreatitis. Certain genetic mutations, such as mutations in the PRSS1, SPINK1, and CFTR genes, can increase the risk of developing the condition. Family history of pancreatitis or other pancreatic disorders also elevates the risk.
3. Smoking:
Smoking is a well-established risk factor for chronic pancreatitis. The harmful chemicals in tobacco smoke can damage the pancreas and impair its function over time. Quitting smoking is crucial for reducing the risk of developing chronic pancreatitis and improving overall health.
4. Gallstones:
Gallstones, which are hardened deposits in the gallbladder, can obstruct the pancreatic duct and lead to inflammation of the pancreas. This condition, known as biliary pancreatitis, can progress to chronic pancreatitis if left untreated. Managing gallstones promptly through medication or surgical removal can help prevent complications.
5. Autoimmune Diseases:
Autoimmune conditions such as autoimmune pancreatitis (AIP) can cause chronic inflammation of the pancreas. In AIP, the body's immune system mistakenly attacks the pancreatic tissue, triggering inflammation and scarring. Proper diagnosis and treatment are essential for managing autoimmune-related pancreatitis effectively.
6. Hereditary Factors:
In some cases, chronic pancreatitis can be inherited as a familial disorder. Individuals with a family history of the condition are at an increased risk of developing it themselves. Genetic counseling and screening may be recommended for those with a family history of chronic pancreatitis.
7. Hypertriglyceridemia:
Elevated levels of triglycerides in the blood, a condition known as hypertriglyceridemia, can contribute to the development of chronic pancreatitis. High triglyceride levels can lead to pancreatic inflammation and damage. Managing triglyceride levels through diet, exercise, and medication can help reduce the risk.
8. Other Risk Factors:
Obesity, certain medications, such as corticosteroids and diuretics, and certain medical conditions, such as cystic fibrosis and hypercalcemia, can also increase the risk of chronic pancreatitis. Identifying and addressing these risk factors early on is crucial for prevention and management.
Conclusion:
Chronic pancreatitis is a complex condition with multiple contributing factors. By understanding the causes and risk factors associated with the disease, individuals can make informed lifestyle choices and seek appropriate medical care to reduce their risk and manage the condition effectively. It's essential to adopt a holistic approach to health, including maintaining a healthy weight, avoiding excessive alcohol consumption, quitting smoking, and addressing underlying medical conditions, to promote pancreatic health and overall well-being.
#chronic illness#chronic pancreatitis#health#causes and riskfactors#blog posting#health blog#pain management#prevention strategies
2 notes
·
View notes