#Neurodevelopment
Explore tagged Tumblr posts
Text
Changes to the microbiome, the community of microorganisms inside the body, were correlated with future neurodevelopmental disorder diagnoses, as well as environmental factors and even common treatments for young childhood ear infections. The researchers conducted the study using data collected over 20 years from 16,440 Swedish children participating in the All Babies in Southeast Sweden (ABIS) cohort. Of these children, 1,197, or 7.28%, developed a neurodevelopmental disorder.
Continue Reading.
84 notes
·
View notes
Text
Random reminder. Aspd is a neurodivergence.
Limiting neurodivergences to just neurodevelopmental disorders closes off swaths of divergenciencies in neuro (the brain)
If you claim that even though aspd has genetic roots that cause it has symptoms enhanced by childhood trauma and neglect that therefore not a neurodivergence, you are claiming adhd isn't a neurodivergence.
Even neurodevelopmental disorders includes a lot more variety then just adhd and autism.
So, if you are just talking about autism. Say autism.
If you are just talking about autism and adhd, say that.
If you are just talking about neurodevelopmental disorders, say that. But make sure to include things that might make you uncomfortable like tic disorders
And if you say neurodivergence still, include all. Including if it makes you uncomfortable like aspd might for you.
#aspd#aspd safe#actually aspd#autism#adhd#neurodevelopment#neurodivergent#neurodiversity#tic disorder#tourettes#mae rambles
25 notes
·
View notes
Text
Inside Out 3: All Executive Dysfunction
#bad idea#movie pitch#pitch and moan#pixar#animation#animated film#adhd#executive dysfunction#neurodivergent#neurodevelopment#emotions#trilogy
4 notes
·
View notes
Text
By: SEGM
Published: Mar 15, 2024
youtube
The @NHSEngland landmark decision to stop using puberty blockers for gender dysphoric youth raises a key question: what do we know about the effects of puberty blockers on adolescent development?
Prof. Sallie Baxendale explored this question at @segm_ebm 2023 conference.
"Extraordinary claims demand extraordinary evidence" wrote Prof. Baxendale in a piece describing her research. "The only extraordinary evidence here is the gaping chasm of knowledge, or even apparent curiosity, of the clinicians who continue to chant 'safe and completely reversible' as they prescribe these medications to the children in their care."
Following the preview of her research at @segm_ebm conference, Prof. Baxendale published her findings about the known effects of puberty blockers on neuropsychological function in a peer-reviewed journal.
Prof. Baxendale later shared that in her 3 decades of academic publishing, the submission of the paper was truly a unique experience. She was not concerned that the paper had been rejected 3 times prior to being accepted. Rather, it was the nature of the rejections, which appeared to be ideologically driven.
Dr. Baxendale's full presentation at @segm_ebm NYC 2023 conference is available below. We will also highlight some key moments in the rest of this thread.
[ Note: video above ]
Dr. Baxendale explores what happens when critical windows of brain development are missed, starting with her "surprise" at the assertion made by proponents of youth transitions that puberty blockers are "completely reversible."
Prof. Baxendale challenges the claim that puberty can be paused & resumed: “If you deprive the brain of any input during the critical windows of opportunity, the brain will move on and whatever it was that was supposed to be developing, doesn't develop properly.”
The process of pruning in the brain, which occurs during adolescence, is critical. It strengthens the executive function & social cognition. This process is hormonally driven: it depends on the pubertal stage, not on age. When puberty is stopped, brain development is affected.
Prof. Baxendale's research was motivated by her surprise at the assertions by gender clinicians that "one can just pause puberty and then pick up 2-3 years later and nothing would happen," as this contradicted "everything we know about other windows of opportunity."
Dr. Baxendale found a paucity of studies on the effects of puberty blockers on human brains, so she turned to animal studies. What she found was that puberty blockers have “a detrimental impact on learning and the development of social behaviors and responses to stress."
Turning her attention to human studies, Prof. Baxendale found very few. Two studies were for the use of puberty blockers for early-onset puberty, and 3 were about stopping normally-timed puberty for gender-dysphoric youth. Several (low quality) studies signaled a drop in IQ.
Dr. Baxendale found no evidence that “you can pause a developmental stage and then restart it and everything will be okay.” Given all that is known about adolescent brain development, Dr. Baxendale asked a key question:
“How has this been allowed to develop as a treatment?”
The @NHSEngland's decision to restrict the use of puberty blockers to clinical research, finalized this month, vindicates Prof. Baxendale, Dr. Biggs, and other researchers in the UK and worldwide who have been sounding the alarm about the proliferation of puberty blockers in general medical settings without an adequate evidence base.
The full lecture by Prof. Baxendale at SEGM's NYC 2023 conference is profiled on our website and our YouTube channel. See links below.
[ Note: video above ]
--
Abstract
Aim: Concerns have been raised regarding the impact of medications that interrupt puberty, given the magnitude and complexity of changes that occur in brain function and structure during this sensitive window of neurodevelopment. This review examines the literature on the impact of pubertal suppression on cognitive and behavioural function in animals and humans.
Methods: All studies reporting cognitive impacts of treatment with GnRH agonists/antagonists for pubertal suppression in animals or humans were sought via a systematic search strategy across the PubMed, Embase, Web of Science and PsycINFO databases.
Results: Sixteen studies were identified. In mammals, the neuropsychological impacts of puberty blockers are complex and often sex specific (n = 11 studies). There is no evidence that cognitive effects are fully reversible following discontinuation of treatment. No human studies have systematically explored the impact of these treatments on neuropsychological function with an adequate baseline and follow-up. There is some evidence of a detrimental impact of pubertal suppression on IQ in children.
Conclusion: Critical questions remain unanswered regarding the nature, extent and permanence of any arrested development of cognitive function associated with puberty blockers. The impact of puberal suppression on measures of neuropsychological function is an urgent research priority.
#Sallie Baxendale#puberty blockers#SEGM#Society for Evidence Based Gender Medicine#neurodevelopment#medical scandal#medical corruption#medical malpractice#puberty#adolescent development#adolescence#gender ideology#gender identity ideology#queer theory#intersectional feminism#gender affirming healthcare#gender affirming care#gender affirmation#gender lobotomy#religion is a mental illness
2 notes
·
View notes
Text
Why the “Under 25” rule? It’s biological — not ageism
Brain development doesn’t end in your teens
Research shows that the prefrontal cortex — responsible for
impulse control,
long-term planning,
logical reasoning
— continues maturing well into the mid-twenties. Studies using neuroimaging and behavioral tests consistently note that full executive function (e.g., inhibiting impulsive behavior, organizing tasks, and controlling emotions) isn’t reliably established until around age 25.
Why does that matter for meaningful conversations?
Before this final stage of prefrontal development, people are naturally more susceptible to
strong emotional reactions,
less able to process complex, nuanced arguments.
That can lead to fiery, less constructive debates — rather than balanced, thoughtful discourse.
Bottom Line
The “Under 25” guideline is rooted in well-documented brain science — it’s a checkpoint for cognitive maturity, not a judgment on anyone’s value. The research is clear:
Executive functions (planning, inhibition, organization) climb well into the twenties.
Prefrontal control over emotions also matures later, meaning younger brains are wired for less regulated responses.
References
Luna et al., “Maturation of cognitive processes from late childhood to adulthood.” Child Development — charts executive function development across ages (1, 2, 3).
Laurence Steinberg, “Teenage rebellion” (Temple University) — documents prefrontal maturation continuing into mid‑twenties (1, 2, 3).
#neurodevelopment#brainmaturity#executivefunction#prefrontalcortex#digitaldiscourse#cognitivegrowth#frontallobes#neuroscience#mentalhealth#developmentalpsychology#neurofacts#onlineetiquette#brainscience#generationalgap#maturitymatters#maturity#brain
0 notes
Text

Call for Abstracts – Track 11: Pediatric Neurology Be part of the 4th World Pediatrics, Perinatology & Child Health Summit, taking place October 21–23, 2025, at Novotel Al Barsha, Dubai, UAE. Contribute to Track 11: Pediatric Neurology by submitting your research on topics such as neurodevelopmental disorders, pediatric epilepsy, neuromuscular diseases, neurogenetic syndromes, brain injury, cerebral palsy, and innovations in diagnosis and treatment. Engage with global leaders working to advance neurological care for children. Abstract Submission Deadline: June 14th, 2025 Submit Here: https://pediatrics.utilitarianconferences.com/submit-abstract Contact Us: https://wa.me/+971551792927
#Pediatrics#PediatricNeurology#ChildHealth#Neurodevelopment#Epilepsy#CerebralPalsy#PediatricCare#Neuroscience#PediatricSummit2025#DubaiConference
0 notes
Text
Researchers uncover mechanism linking maternal inflammation to delayed neurodevelopment in infants
A research group led by Nagoya University Graduate School of Medicine in Japan has uncovered a potential mechanism linking maternal inflammation to delayed neurodevelopment in infants. The research suggests the role of CD11c-positive microglia-immune cells in the brain crucial for myelination-during infant brain development. The results, published in Communications Biology, suggest new strategies…

View On WordPress
0 notes
Text
What Causes ADHD? Understanding the Key Factors
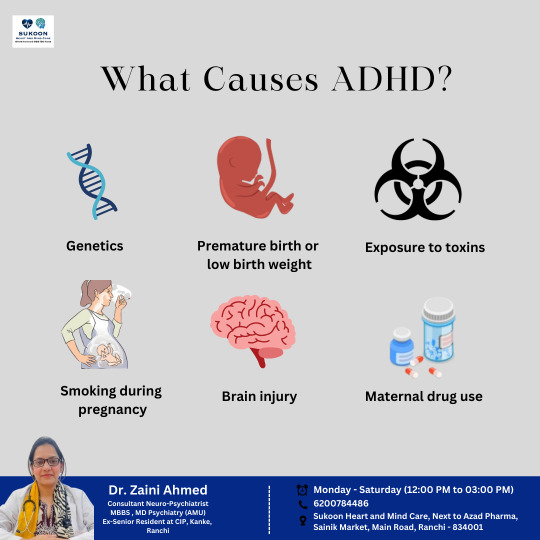
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental condition that affects both children and adults, leading to difficulties with attention, impulsivity, and hyperactivity. While the exact cause of ADHD remains unclear, research suggests that several factors contribute to its development.
1. Genetics
ADHD often runs in families, indicating a strong genetic component. Studies show that children with a parent or sibling diagnosed with ADHD are more likely to develop the condition.
2. Premature Birth or Low Birth Weight
Babies born prematurely or with low birth weight have a higher risk of developing ADHD. These factors may impact brain development, leading to attention and behavioral difficulties later in life.
3. Exposure to Toxins
Exposure to environmental toxins such as lead, often found in old buildings and contaminated water, has been linked to an increased risk of ADHD in children.
4. Smoking During Pregnancy
Nicotine exposure during pregnancy can affect fetal brain development, increasing the likelihood of ADHD symptoms in children.
5. Brain Injury
In some cases, traumatic brain injuries, especially those affecting the frontal lobe, may contribute to attention and impulse control problems associated with ADHD.
6. Maternal Drug Use
Substance use during pregnancy, including alcohol and illicit drugs, can interfere with the developing nervous system of the fetus, raising the risk of ADHD and other behavioral disorders.
Seeking Professional Guidance
Understanding the causes of ADHD is essential for early intervention and effective management. If you or a loved one is experiencing symptoms of ADHD, consulting a specialist can help with proper diagnosis and treatment.
For expert evaluation and care, Dr. Zaini Ahmed, MBBS, MD (Psychiatry), is available for consultation at:
📍 Sukoon Heart and Mind Care, Sainik Market, Main Road, Ranchi, Jharkhand: 834001 📞 6200784486 🕛 Monday to Saturday, 12 PM to 3 PM
Early diagnosis and appropriate management can significantly improve the quality of life for individuals with ADHD.
#ADHDAwareness#MentalHealthMatters#ADHDCauses#Neuropsychiatry#RanchiPsychiatrist#BrainHealth#AttentionDisorders#MentalWellness#PsychiatryCare#FocusAndAttention#BehavioralHealth#Neurodevelopment#ChildPsychiatry#MindCare#ADHDSupport#DrZainiAhmed#bestpsychiatrist#bestpsychiatristinranchi#Ranchi#neuropsychiatrist#sukoonheartandmindcare
1 note
·
View note
Text
Stimulants and Brain Development in Children with ADHD
A recent study published in Neuropsychopharmacology explores how stimulant medications affect brain development in children with ADHD, highlighting how these treatments may help normalize brain regions linked to ADHD symptoms.
This study is explored in depth in Stimulant Medication Normalizes Brain Structures in Children with ADHD: New Study by Carly Broadway, published by ADDitude Magazine, which informed this newsletter.
Key Findings
Children who were not on medication showed reduced cortical thickness in the insula (a brain region involved in prioritizing information) and less grey matter in the nucleus accumbens (linked to motivation and reward).
In contrast, children who were taking stimulant medications had brain structures more similar to neurotypical children, suggesting that medication may play a role in normalizing some areas of the brain, improving the symptoms of ADHD.
While stimulant medications were found to positively impact certain brain regions, areas like the caudate (involved in motor control) and the amygdala (involved in emotional processing) remained unchanged, which aligns with previous studies. Additionally, non-stimulant medication did not have a notable impact on brain structure.
Stimulants are widely used as the first-line treatment for ADHD, although some individuals may stop using them due to side effects like reduced appetite, sleep disturbances, and mood changes. This study suggests that while stimulant medications can help normalize brain structure, their effects may vary across different regions of the brain. These findings may pave the way for more personalized treatment approaches, helping to improve both symptom management and treatment adherence.
As a cross-sectional study, this research doesn’t establish cause and effect. Additionally, there was limited information on the dosage and duration of medication use, highlighting the need for future studies that track the long-term effects of stimulant medications in greater detail.
I provide formal assessments for ADHD and Autism for individuals ages 8-48 in California, both in-person and online (my online assessment option is for ages 18+). For more information, and to check your PPO insurance reimbursement benefits with the Mentaya tool, please visit my website.
I also encourage you to explore these tools to promote your well-being:
Empowerment Through Understanding Modules: Dive deeper into ADHD and Autism with this online course to improve self-awareness, self-advocacy, and personal growth. Learn more here.
AuDHD Strong App: A helpful app for neurodivergent individuals with tools for organization, task management, and self-care. Download it today from the App Store or the Google Play Store!
Faces of Health App: This app offers valuable mental health and well-being resources. Download it today from the App Store or the Google Play Store!
For more valuable insights, I encourage you to explore my blog at https://drblied.com/blog/. For a selection of wellness resources, please visit the resources page on my website at https://drblied.com/resources/.
Reference
Broadway, C. (2024). Stimulant medication normalizes brain structures in children with ADHD: New study. ADDitude Magazine. https://www.additudemag.com/stimulant-meds-adhd-brain-development-study/?ecd=wnl_additude_250105_cons_adhd_pro&goal=0_a767e6fc3c-4922c6793e-301887718
#ADHDSupport#ADHDResearch#BrainScience#EvidenceBased#NeuroScience#ADHDAwareness#Focus#Attention#MentalHealthMatters#Psychologist#DrBlied#AuDHD#ADHD#Neurodivergent#Neurodiverse#ForYou#ADHDTreatment#ADHDSolutions#BrainHealth#CognitiveScience#Neurodevelopment
0 notes
Text
In the current issue of Molecular Psychiatry, the ADNP protein image from our previous publication has been published.
0 notes
Text
Insane how im writing a policy paper on why we shouldn't send children to adult prisons because it is bad from literally every angle and yet it is somehow considered a theoretical proposal that wouldn't pass under any administration
#like its for a neurodevelopment class so we're supposed to argue it using neuroscience. turns out neurologically bad to imprison kids.#turns out its also bad for the communities they come from because the state is basically stealing all their future workers#and thats also bad for the state's economy#not to mention ur refusing kids an education and then throwing them into the world after 40 years what are they going to do????#also expensive as hell to imprison someon#like. why does anyone support this#its all literally pr#vio.reblog
35 notes
·
View notes
Text
A lot talk about how you shouldn't make fun of neurodivergent adults that like kids show or childish things, which fair. But i think the opposite is also commonplace.
As a neurodivergent child i was extremely gifted at math, less variety of emotions, liked things being complex and difficult and seemed "very mature"
So i liked shows and movies and games that were aimed at older people
Because of these things i was dually put so much on me to overwhelm me. Expected if good at one subject i should be belittled and hated for bad at another. That me liking more mature media meant i was a potential killer.
They viewed me as a monster for fitting the opposite while trying to make me suffer. And i think that's messed up.
10 notes
·
View notes
Text
gonna start making a list of The Issues to show the next doc i see like "this is what we know is wrong this is what ive been told i probably have this is what i know i have now give me some answers doc" because hey maybe thatll get me some actual answers instead of wishy washy maybe's and could be's and what if's and being told that every single symptom i have ever displayed for my entire life since before it all went bad is caused by thE DEBILITATING SOCIAL ANXIETY I DEVELOPED LATER ON IN LIFE AND NOT ANY OF THE THINGS THAT IVE BEEN SUSPECTED TO HAVE FOR GOD KNOWS HOW LONG AND THAT SSRI'S WILL MAGICALLY FIX EVERYTHING WRONG WITH ME AND CURE MY CLUSTERFUCK OF SYMPTOMS AND ISSUES THAT NO ONE WANTS TO TAKE A CRACK AT DECODING BECAUSE IM NOT AN EASY JOB ANYMORE-
#ace shoots the shit#can you tell im mad at my brain right now. and the medical system not wanting to give me any helpful answers.#like yes doctor the ssri's will help with the social anxiety but i dont know they help with the other stuff thats happening in my brain#which there are medical records of me nearly getting confirmed to have other stuff weird with my head if not for my fathers intervention#from just put her on adhd meds and let the school deal with her to its definitely autism to she has no neurodevelopment disorder just SAD#and you can see why this is getting on my nerves even after two weeks of being told to buck up and Try Harder#vent#that or im just being a melodramatic little bitch thats perfectly fine but honestly i cant tell i just cant fucking tell and i dont know
0 notes
Video
youtube
Beyond Unlikely to Unlimited: Neurodevelopment Transforms: Picture this: a mother who’s tried everything she could think of to help her daughter succeed. Her daughter faced severe developmental challenges that impacted nearly every part of her life—from reading and writing to physical coordination and social interactions. But she found a solution... [email protected]
0 notes
Text

Call for Presentation – Track 16: Child and Adolescent Psychiatry | Track 17: Genetics Track 18: Mental Disorders | Track 19: Adolescent Medicine | Track 20: Community Pediatrics Share your pioneering research and innovative clinical practices at the 4th World Pediatrics, Perinatology & Child Health Summit, taking place October 21–23, 2025, in Dubai, UAE & Virtual. Abstract Submission Deadline: April 30, 2025! Submit Your Abstract Here: https://pediatrics.utilitarianconferences.com/submit-abstract Contact Us via WhatsApp: https://wa.me/+971588044059
#ChildPsychiatry#AdolescentMentalHealth#GeneticsInPediatrics#MentalHealthAwareness#AdolescentMedicine#CommunityPediatrics#YouthWellness#PediatricResearch#HealthyMinds#PediatricConference#ChildHealth#Neurodevelopment#PediatricCare#MentalHealthInChildren
0 notes
Text
Identification of a new mutation in kmt2c causing Kleefstra syndrome TYPE 2: A very rare disorder characterized by autism and development delay by Antonella Peduto in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
The prevalence of autism spectrum disorders (ASD) has risen over the last few decades from 2-4 in 10,000 to an estimate of 1 in 100. This is mostly due to changes in the broadening of investigation and diagnostic criteria. There are several rare monogenic diseases in which autism is a trait of neurodevelopment disorder, characterized by cognitive and motor disabilities, language impairment, in association with epilepsy, as well as other psychiatric disorders and distinctive physical features or multiorgan malformations. Some consider these disorders as “syndromic autism” and, among those, Kleefstra syndrome is a rare condition with a heterogenous clinical phenotype which includes autistic- like features. Kleefstra syndrome is caused by haploinsufficiency of EHMT1 (euchromatin histone methyltransferase 1). The disorder is characterized by moderate- severe development delay, absent or limited language, hypotonia, distinctive facial features, brachycephaly. In addition, de novo variants in four additional genes (MBD5, SMARCB1, NR1/3 and KMT2C) are known to be correlated with clinical aspects overlapping with those found in Kleefstra syndrome, known as Kleefstra syndrome type 2 (KLEFS2). To date, only about ten cases of KLEFS2 are reported in literature. Both syndromes are inherited by an autosomal dominant way. As for other genetic disorders diagnosis is difficult and often years delayed after many medical consultations, principally due to high clinical phenotypic heterogeneity.
We present the case of a Caucasian child referred to neurologist and pediatric genetist for development delay and autism. Clinical exome analysis identified a novel de novo c.10420C>T (p.Gln3474Ter) mutation in the KMT2C gene associated with Kleefstra syndrome type 2. In addition to KLEFS2 typical clinical signs the patient showed also orthopedic anomalies like hip dysplasia, pectus excavatum, hammer toe, valgus rearfeet, gastroesophageal reflux, partial empty sella and corpus callosum anomaly. We report also his neurological follow up from two since six years old, his actual age, by using standardized neurological tests.
Key words: autism spectrum disorders (ASD), neurodevelopment disorders, Kleefstra syndrome type 2 (KLEFS2), KMT2C
Introduction
Autism spectrum disorders (ASD) DSM-5 (APA American Psychiatric Academy 2013) 1 include a large broad of clinical conditions mostly characterized by difficulties in social communication, repetitive behaviors and limited interests. ASD manifestations can vary significantly ranging from mild forms with relatively preserved communicative abilities to forms characterized by more severe clinical features with significant social impairments.
Neurodevelopment disorders are a heterogeneous group of medical conditions affecting the proper global development of cognitive, motor, linguistic and social functioning during childhood 2. Autism and neurodevelopment disorders can often be present in association in congenital disorders. During the last ten years, the new and most up-to-date techniques of genetic sequencing (NGS) have allowed the identification of an increasing number of genes associated with orphan diseases3. This, in the context of highly heterogeneous diseases such as neurodevelopment disorders, has significantly enhanced the diagnostic yield of genetic investigation. Despite this, many genes and molecular mechanisms still remain unknown.
Kleefstra syndrome (OMIM 610253) is characterized by a clinical recognizable phenotype that includes intellectual disability, from moderate to severe, childhood hypotonia, autistic features, and physical dysmorphic features such as broad forehead, arched eyebrows or synophrys, anteverted nares, coarse face, that becomes more evident with age, together with obesity in adulthood. Most children show delayed motor development and severe expressive speech delay. Several other systemic findings can be viewed as epilepsy, heart defects, brain anomalies, genitourinary malformations and severe respiratory infections4,5. Kleefstra syndrome is known to be correlated with EHTM1 gene loss of function mutations, almost all cases to date reported are carrier of de novo mutations6.
More recently, Kleefstra et al reported a patient with intellectual impairment, autism, absence of language and suggestive dysmorphic features in which a de novo truncating mutation in the KMT2C gene (Type 2 lysine methyl trasferase) was identified7. Since then, other few patients were reported with clinical phenotypes overlapping with Kleefstra syndrome, carrier of significant mutations in four genes, including KMT2C, MBD5, SMARCB1, NR 113 8, 9. These patients were designated as having Kleefstra syndrome-type 2 (KLEF2) (OMIM 617768).
Case Presentation
The child was firstly referred at the age of two years to the neurological service and genetic consultant for global development delay. He is the only child of healthy non-consanguineous Caucasian parents. Pregnancy was uneventful and he was born at 35+4 weeks through spontaneous delivery. Normal growth parameters were reported at birth: weight 2680g (65th percentile), length 47cm (55th p) head circumference 32.6 cm (49th p). At the clinical examination, hip dysplasia was identified and, after radiological confirmation, a hip retractor was used in the first two months of life. At one month of age the infant was admitted to neonatal intensive care for ALTE (apparent life-threatening event) and anemia that were caused by gastroesophageal reflux. In that occasion axial hypotonia and occipital plagiocephaly was noted too by clinicians.
Neurological examination, performed two years old, showed global development delay, ambulation was still not acquired, language delay and behavioral anomalies. He was evaluated using the Bayley III scale10 that showed cognitive development in the borderline range and motor skills in the low to medium- low range. A pysicodiagnostic evaluation was performed with ADOS-2 (Autism Diagnostic Observation Scale)11 to assess the presence of clinical signs related to autism spectrum disorders. At the time of evaluation, the patient could walk with support, verbal language was delayed, with mainly vocalizations and sporadic babbling. Limited relational interest was observed, while he was attracted by all sound and flashing toys. Stereotyped behaviors like rocking were present together with hypersensitivity to loud noises. Adequate eating habits and regular sleep/wake rhythm were reported. The ADOS-2 total score was 20, that is related to a moderate to severe risk of presenting symptoms of autistic disorders.
At the age of three years the patient was referred to pediatric genetic consultation. The clinical examination showed growth parameters in normal range (weight, length and head circumference at 50th percentile). Facial minor dysmorphic features were noted like saddle nose, bushy and horizontal eyebrows and hint of coarse face, occipital plagiocephaly, foot third hammer toe, pectus excavatum. The autonomous walking was possible, but it was yet uncertain, with bilateral valgus rearfoot and externally rotated lower limbs. Ligamentous hyperlaxity was present. No hepatomegaly was found. Due to facial appearance, neurodevelopment delay and orthopedic aspects some lysosomal storage disorders were ruled out as mucopolysaysaccharidoses and oligosaccharidoses. Blood tests showed CK within range. At the same time first level genetic tests were performed. FRAXA analysis and Array- CGH (Array- Comparative Genomic Hybridation) resulted with normal profiles. Moreover, in the suspicion of a syndromic disease several instrumental investigations were performed to evaluate possible other organ involvement, including abdominal ultrasound, video electroencephalogram during sleep, ophthalmological and audiological examination, all resulted normal. Brain MRI showed a slightly thinning appearance of the posterior septum of the corpus callosum and a partial empty sella aspect.
Currently the child has making some progress in language using visual AAC (Augmentative and Alternative Communication) through photographs. Regarding motor skills, the child presents difficulties in executive control and in planning both gross and fine motor gestures. Walking still follows a wide-based pattern with feet rotated outward. He shows global hypotonia and joint laxity, difficulties in coordinating simple and complex voluntary movements. Stereotyped hand and arm movements and head shaking are observed in response to displays joy or excitement. No self/hetero-aggressiveness. Non-constant gastroesophageal reflux was reported anymore, neither food selectivity. Sleep/wake rhythm has always been regular. The child regularly undergoes medical check-ups. Logopedic and neuropsychomotor care continues with treatment cycles and rehabilitation goals periodically defined ensuing follow-up evaluations. Inclusive school practices have been initiated with a supporter teacher. Considering the neuromotor profile, the possibility of using orthotic insoles to improve gait motor organization and balance is under evaluation. Psychological support has been offered to the parents following the diagnosis, as it is known that parents of individuals with autism spectrum disorder and KS experience high levels of stress13.
Patient’s pictures respectively at 6 months (3), 2 years (4) and 6 years old (5). We observe widely spaced eyes, saddle nose, thick eyebrows and wide forehead, slightly hinting coarse face, more evident with age.
Patient’s neurodevelopment scores resulted by Griffhs III scale performer at 72 months of age (6 years old). Scores from 50 to 70 are extremely below for the norm requiring specific support and therapy, from 70 to 80 they are below the norm needing to be reinforced, from 90 to 115 they are perfectly in line with age.
Considering the moderate- severe global development delay, the autistic and dysmorphic features whole exome TRIO analysis was performed, at the age of three years. NGS sequencing and data interpretation highlighted the presence of a novel heterozygous nucleotidic variant c.10420C>T in the KMT2C gene predicted to result in the premature nonsense STOP codon mutation p.Gln3474Ter. TRIO analysis showed that both parents were negative for this mutation suggesting its de novo occurrence. Accordingly to the ACMG guidelines the mutation here found was classified as likely pathogenic (class 4).
At 4 years of age, development delay and autistic features were confirmed during patient’s follow up. The PEP-3 (Psycho- Educational Profile)12 was administered to the patient. The evaluation highlighted the following adaptive/developmental delays divided by areas: verbal/preverbal cognitive skills corresponding to 1 year and 6 months, expressive language below 12 months, receptive language 1 year, fine motor skills: 1 year and 10 months, gross motor skills 1 year and 5 months, motor vision imitation 1 year and 1 months. Moreover, problematic behaviors and poor social interests were noted too.
Currently at 6 years of age, Griffiths III scale showed a globally delayed developmental profile, corresponding to a developmental quotient < 20, severely below the normal range, equivalent to an age of 47 (< 1st percentile). Neurodevelopment scores are summarized in table 1.
Methods
Previously informed consensus the patient and their parents underwent a blood draw to perform clinical whole exome sequencing. Briefly, genomic nucleic acids underwent DNA library preparation and whole exome enrichment employing Agilent All Exon V.6 kit (Agilent Technologies, Inc., Santa Clara CA, USA). Library sequences were obtained using the HiSeq2500 Illumina Sequencer (150-bp paired end). Bioinformatics analysis included the following: next-generation sequencing (NGS) reads mapping to whole genomes using the Burrows-Wheeler Alignment tool with default parameters, polymerase chain reaction (PCR) duplicate removal using Picard (http://picard.sourceforge.net), single nucleotide polymorphisms and indel calling using the Genome Analysis Toolkit (GATK) UnifiedGenotyper, variant annotation using snpEff (http://snpeff.sourceforge.net) and false positive variant filtration using the GATK VariantFiltration module. Exome sequencing data and reads alignment analysis were checked for coverage depth and alignment quality employing Bedtools software package. CNV calling was performed by Varseq software. This algorithm uses changes in coverage depth relative to a collection of reference samples (30 or more reference samples recommended, having on average 100X across all regions, and derived from the same library prep methods) as evidence of CNV events. High-quality CNVs were then annotated and filtered against CNV and gene annotation tracks like OMIM, Orphanet, RefSeq Genes, ClinVar and ClinGen.
Phenotype driven analysis coupled with the employment of in silico multigene panels specific for different neurodevelopment diseases was used to filter, select and interpret genetic variants. Variant analysis was performed employing bioinformatic prediction tools (Polyphen2, SIFT, MutationTaster, PhyloP, CADD-Phred) and classification was conducted in accordance with the guidelines from the American College of Medical Genetics and Genomics. In brief, variants were classified as follows: 1) benign variant, not considered to be the cause of the tested disease, 2) likely benign variant , not likely to be the cause, 3) variant of uncertain significant (VUS), it is unclear whether it is connected to a health condition, 4) likely pathogenic variants, it is often a mutation not previously reported in literature, that results in premature truncation 5) pathogenic variant, it is well established as disease cause by databases and literature.
Discussion
Neurodevelopment disorders like intellectual disability and autism spectrum disorders represent a significant challenge for healthcare professionals, their families and society as whole14. Timely diagnosis and appropriate management are essential to ensure adequate support to children and their families, promoting improvements in their motor, cognitive and communicative skills and quality of life15. Among these conditions a large number of affected patients are, to date, without a clinical and molecular diagnosis or they wait years for it (diagnostic odissea).
Rare disorders often characterized by broad clinical heterogeneity with possible clinical overlap make diagnosis process difficult. In these last years the availability of new diagnostic technologies, such as next new generation DNA sequencing techniques provided valuable information about the biological basis of these conditions and enabled increasingly early and accurate diagnosis16.
In this report we present the clinical features and the diagnosis walk of a six years old child affected by Kleefstra syndrome 2 (KLEF2), in which a novel mutation c.10420C>T was identified in the KMTC2 gene. This mutation, arising de novo, it is predicted to result in a loss of function variant, leading to a premature stop codon (variant class 4).
KLEF2 phenotype mainly overlaps with Kleefstra syndrome, that is caused by EHMTH1 gene mutations. Both KMT2C and EHMT1 genes encode for a hystone methyltransferase which regulates gene transcription through modification of chromatin structure7. Dysregulation of this epigenetic mechanism are associated with a wide range of human diseases, including cancer, immune dysfunction and multiorgan congenital syndromes as well as neurodevelopment disorders17. KMT2C is a evolutionarily conserved protein that forms part of a nuclear structure known as KMT2C/D COMPASS which is implicated in the central nervous system development. Mutations in Key COMPASS complex genes have been linked to three human congenital syndrome: Kleefstra syndrome type 2, Kabuki and Rubistain- Taybi syndrome18.
Even though the KLEF2 syndrome is currently believed to be very rare, with very few reported cases, it is crucial to acknowledge the possibility of a greater prevalence. The implementation of emerging, up to date and highly processing sequencing techniques, have the capability to more easily identify new affected patients, possibly giving new information concerning the incidence of this syndrome in the context of neurodevelopment disorders.
Conclusion
In conclusion, we here report the 6 year clinical follow-up of a patient affected by type 2 Kleefstra syndrome, for which the diagnosis was performed at 3 years old. In addition to typical clinical signs of KLEFS2 our patient showed also orthopedic anomalies like hip dysplasia, pectus excavatum, hammer toe, valgus rearfeet, severe gastroesophageal reflux in the first year, brain anomalies like partial empty sella and thinning appearance of the posterior septum of the corpus callosum. The child was first referred for diagnostic investigations for neurodevelopment delay and autism. We emphasize that ASD is often in comorbidity and we suggest looking also for KLEFS2 in those cases of patients showing autistic traits. Actually genetic analyses are directive in the context of diseases characterized by high phenotypic heterogeneity. Moreover, it highlights how clinical diagnosis, supported by cutting-edge genetic analysis, can drastically reduce the time required to achieve an accurate diagnosis.
#autism spectrum disorders (ASD)#neurodevelopment disorders#Kleefstra syndrome type 2 (KLEFS2)#KMT2C#Journal of Clinical Case Reports Medical Images and Health Sciences predatory#jcrmhs
0 notes