#cholesterol and triglycerides
Explore tagged Tumblr posts
Text
#cholesterol levels#ldl cholesterol#ldl cholesterol levels#bad cholesterol#foods high in saturated#reduce cholesterol#cholesterol naturally#lowering cholesterol#hdl cholesterol#foods that lower cholesterol#foods high in saturated fat#reduce their cholesterol#reduce their cholesterol levels#total cholesterol#cholesterol lowering#cholesterol diet#cholesterol and triglycerides#cholesterol with diet#levels of ldl cholesterol#levels of ldl cholesterol and triglycerides#improve your cholesterol#cholesterol#healthy#heart#fats#eat#eating#exercise#fiber#vegetables
0 notes
Text

foods for a healthy heart ❤️ lower blood pressure, cholesterol, triglycerides
#health#wellness#health and wellness#food#healthy food#heart health#heart#triglycerides#blood pressure#cholesterol#vegan#plant based#vegetarian#plantbased
23 notes
·
View notes
Text
What’s Inside a Lipid Droplet? Beyond Just Fat
Following my exploration of adipose hypertrophy and mitosis and building on my broader journey to understand weight loss and metabolism, I’m now delving into the inner workings of fat cells. This post, part of my series on Dan Snell’s blog, focuses on the composition of lipid droplets within adipocytes—the storage units of fat in our bodies. While we often think of fat as just stored energy,…
#Adipocytes#Cellular health#Cholesterol esters#Energy release#Fat Storage#Fat-soluble toxins#Fat-soluble vitamins#Lipid droplet#Metabolism#Triglycerides
0 notes
Video
youtube
ČAJ OD LIŠĆA ZELENIH ORAHA ZA PROČIŠĆAVANJE KRVI
#youtube#triglycerides#cholesterol#holesterol#čišćenje krvi#zeleni orasi#arterije#krvni sudovi#arteroskleroza#žutica#hemoroidi#bubrežna oboljenja#kožne bolesti#kalcifikacija
0 notes
Text
#LDL Cholesterol (Low-Density Lipoprotein)#HDL Cholesterol (High-Density Lipoprotein)#Total Cholesterol#Triglycerides#Cholesterol Levels#Hyperlipidemia#Heart Disease Risk#Diet and Cholesterol#Statins#Lifestyle Changes#Blood Test for Cholesterol#Cholesterol Management#Family History of High Cholesterol#Symptoms of High Cholesterol#Cholesterol Guidelines#health & fitness#health and wellness
0 notes
Text
Chế độ ăn giảm nồng độ cholesterol và triglyceride
Cholesterol và triglyceride là hai loại chất béo quan trọng trong máu. Trong khi cơ thể cần cholesterol để xây dựng tế bào khỏe mạnh, thì nồng độ cholesterol cao lại là tác nhân chính dẫn đến bệnh tim mạch. Triglyceride, mặt khác, cung cấp năng lượng cho cơ thể nhưng nếu ở mức cao cũng gây ra nhiều nguy cơ cho sức khỏe.
Tin vui là bạn hoàn toàn có thể kiểm soát nồng độ cholesterol và triglyceride thông qua chế độ ăn uống khoa học, hợp lý. Bài viết này sẽ cung cấp cho bạn kiến thức đầy đủ và chi tiết về chế độ ăn giảm cholesterol và triglyceride hiệu quả, giúp bạn bảo vệ sức khỏe trái tim lâu dài.
1. Hiểu Rõ Kẻ Thù Của Trái Tim: Cholesterol và Triglyceride
1.1. Cholesterol:
Có hai loại cholesterol chính:
Cholesterol LDL (xấu): Gây tích tụ mảng bám trong động mạch, làm tắc nghẽn dòng máu, tăng nguy cơ đau tim và đột quỵ.
Cholesterol HDL (tốt): Giúp vận chuyển cholesterol LDL khỏi động mạch về gan để xử lý, bảo vệ tim mạch.
1.2. Triglyceride:
Là một dạng chất béo khác trong máu. Nồng độ triglyceride cao làm tăng nguy cơ xơ vữa động mạch, đặc biệt khi kết hợp với cholesterol LDL cao hoặc cholesterol HDL thấp.
2. Nguyên Nhân Gây Tăng Cholesterol và Triglyceride
Chế độ ăn uống không lành mạnh: Tiêu thụ nhiều chất béo bão hòa, chất béo chuyển hóa, cholesterol và đường.
Lối sống ít vận động: Ít vận động, lười tập thể dục.
Béo phì: Thừa cân, béo phì làm tăng nguy cơ rối loạn lipid máu.
Yếu tố di truyền: Tiền sử gia đình có người mắc bệnh tim mạch, rối loạn lipid máu.
Tuổi tác và giới tính: Nguy cơ mắc bệnh tim mạch tăng theo tuổi tác, đặc biệt là phụ nữ sau mãn kinh.
Một số bệnh lý: Bệnh tiểu đường, suy giáp, bệnh gan, bệnh thận...
Sử dụng một số loại thuốc: Thuốc tránh thai, thuốc corticoid...
3. Chế Độ Ăn Giảm Cholesterol và Triglyceride: Nên Và Không Nên
3.1. Những Thực Phẩm Nên Hạn Chế:
Chất béo bão hòa: Tìm thấy nhiều trong thịt mỡ, da gia cầm, mỡ động vật, bơ, phô mai, đồ chiên rán... Hãy chọn thịt nạc, bỏ da gia cầm, hạn chế đồ ăn nhanh và chế biến sẵn.
Chất béo chuyển hóa: Thường ẩn mình trong các loại thực phẩm chế biến sẵn, bánh kẹo, margarine... Hãy đọc kỹ nhãn mác sản phẩm và tránh xa những sản phẩm có chứa "trans fat" hoặc "partially hydrogenated oil".
Cholesterol trong thực phẩm: Lòng đỏ trứng, nội tạng động vật, hải sản có vỏ cứng... Hạn chế tiêu thụ những thực phẩm này.
Đường bổ sung: Nước ngọt, bánh kẹo, nước tăng lực, siro... Giảm thiểu tối đa lượng đường bổ sung trong chế độ ăn.
Rượu bia: Uống nhiều rượu bia làm tăng triglyceride và huyết áp, không tốt cho sức khỏe tim mạch.
3.2. Thực Phẩm Nên Tăng Cường:
Chất béo không bão hòa đơn: Dầu ô liu, dầu hạt cải, quả bơ, các loại hạt (hạnh nhân, óc chó, hạt điều...).
Chất béo không bão hòa đa: Dầu đậu nành, dầu ngô, các loại cá béo (cá hồi, cá thu, cá trích...).
Axit béo Omega-3: Cá béo, hạt chia, hạt lanh, quả óc chó... Omega-3 có tác dụng giảm triglyceride, tăng cholesterol HDL và cải thiện sức khỏe tim mạch.
Chất xơ hòa tan: Yến mạch, các loại đậu, táo, lê, cam, bưởi... Chất xơ hòa tan giúp giảm hấp thu cholesterol vào máu.
Thực phẩm giàu sterol và stanol thực vật: Ngũ cốc bổ sung, sữa chua, margarine... Sterol và stanol thực vật có tác dụng ngăn chặn hấp thu cholesterol trong ruột.
Trái cây và rau củ: Cung cấp vitamin, khoáng chất, chất chống oxy hóa và chất xơ, giúp kiểm soát cholesterol và triglyceride.
3.3. Mẹo Xây Dựng Thực Đơn Giảm Cholesterol và Triglyceride:
Ăn đa dạng thực phẩm: Đảm bảo cung cấp đầy đủ dưỡng chất cho cơ thể.
Chọn ngũ cốc nguyên hạt: Gạo lứt, bánh mì nguyên cám, mì ống nguyên cám...
Nấu ăn lành mạnh: Hấp, luộc, nướng thay vì chiên rán.
Kiểm soát khẩu phần ăn: Không ăn quá no, chia nhỏ bữa ăn.
Uống đủ nước: Khoảng 2 lít nước mỗi ngày.
Thay đổi lối sống: Tập thể dục đều đặn, duy trì cân nặng hợp lý, bỏ thuốc lá.
4. Lời Khuyên Từ Chuyên Gia
Tham khảo ý kiến bác sĩ hoặc chuyên gia dinh dưỡng để được tư vấn chế độ ăn phù hợp với tình trạng sức khỏe của bạn.
Kiểm tra nồng độ cholesterol và triglyceride định kỳ để theo dõi hiệu quả của chế độ ăn uống và điều chỉnh cho phù hợp.
Chế độ ăn uống đóng vai trò vô cùng quan trọng trong việc kiểm soát cholesterol và triglyceride, từ đó giảm thiểu nguy cơ mắc bệnh tim mạch. Hãy thay đổi chế độ ăn ngay hôm nay để bảo vệ trái tim khỏe mạnh và tận hưởng cuộc sống viên mãn!
👉 Cùng tìm hiểu ngay: https://www.acare.abbott.vn/giam-mo-mau-bang-che-do-an/

0 notes
Text
Lipid Profile Test: Understanding Cardiovascular Health
Learn about lipid profile blood test, its significance, results interpretation & managing cholesterol levels. Ensure heart health with lipid profile test.
#lipid profile test#lipid profile blood test#cardiovascular health#cholesterol test#lipid panel#cholesterol levels#triglycerides#heart disease#HDL cholesterol#LDL cholesterol.
0 notes
Text
Lipid Profile Test: Understanding Cardiovascular Health.
Learn about lipid profile blood test, its significance, results interpretation & managing cholesterol levels. Ensure heart health with lipid profile test.
#lipid profile test#lipid profile blood test#cardiovascular health#cholesterol test#lipid panel#cholesterol levels#triglycerides#heart disease#HDL cholesterol#LDL cholesterol.
0 notes
Text
Monitor Your Heart Health with a Comprehensive Lipid Profile Test by RML Pathology

Stay on top of your cardiovascular health with RML Pathology’s comprehensive Lipid Profile Test. Our state-of-the-art diagnostic services measure crucial cholesterol levels, including HDL, LDL, and triglycerides, to give you a complete picture of your heart health. With accurate results, expert analysis, and convenient home sample collection, RML Pathology ensures you receive the best care possible. Book your Lipid Profile Test today and take a proactive step towards a healthier heart!
#Lipid Profile Test#RML Pathology#heart health#cholesterol levels#HDL#LDL#triglycerides#cardiovascular health#diagnostic services#accurate results#expert analysis#home sample collection#book Lipid Profile Test#healthier heart#proactive health.
1 note
·
View note
Video
youtube
איך להוריד כולסטרול, איך מעלים כולסטרול טוב, איך להוריד כולסטרול ללא תרופות #כולסטרול #טריגליצרידים #שומניםבדם #cholesterol #triglycerides
#youtube#איך להוריד כולסטרול איך מעלים כולסטרול טוב איך להוריד כולסטרול ללא תרופות כולסטרול טריגליצרידים שומניםבדם cholesterol triglycerides
1 note
·
View note
Text
Lipid Profile Blood Test: Get the best Analysis at Qris Health, Delhi
Get a comprehensive lipid profile blood test in Delhi at Qris Health Lab. Our advanced diagnostics provide detailed insights into your cholesterol levels, triglycerides, and overall heart health. Swift results and expert analysis ensure timely interventions. Trust Qris Health Lab for accurate assessments and proactive management of your lipid profile. Schedule your test today. Book now (9289589692) for a Lipid Profile Blood Test in Delhi.
#QrisHealth#LipidProfile#BloodTest#HealthCheckup#Delhi#Cholesterol#Triglycerides#HeartHealth#DiagnosticTesting
0 notes
Text

Long duration and worsening #MetabolicSyndrome (cluster of risk factors specific for #cardiovasculardisease including #obesity, #hypertension, #diabetes, high #triglyceride levels, and low #HDL #cholesterol levels) is associated with increased risk of various #cancers especially breast, endometrial, kidney, colorectal, and liver cancers.
https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.35235
#metabolic syndrome#cardiovascular disease#obesity#hypertension#diabetes#high triglycerides#HDL cholesterol#cancers
0 notes
Video
youtube
Očistite i podmladite svoje tijelo: Efikasan recept za smanjenje masnoće...
0 notes
Text

All About Cholesterol! The Latest Science on How Blood Levels of HDL, LDL and More Relate to Cardiovascular Health
— By Amber Dance | February 14, 2024
When C. Michael Gibson of Boston saw his doctor in the spring of 2023, the blood test results were confusing. His cholesterol levels were decent — he was already taking statins to keep the “bad” cholesterol low — but the arteries delivering blood to his heart were nonetheless crammed with dangerous plaque. “It didn’t make sense,” says Gibson, himself a cardiologist at Beth Israel Deaconess Medical Center.
So Gibson asked his physician to check his blood for a specific kind of cholesterol called lipoprotein(a). And there was the explanation: He had more than double the normal amount of that cholesterol. Gibson turned out to be one of the unlucky people who has inherited a predisposition toward high lipoprotein(a) levels; he suspects that his grandfather, who died of a heart attack at age 45, had it too.
About one in five people have this unfortunate heritage, and there’s nothing they can do to combat it — but soon that might change. Scientists are researching medications that can lower lipoprotein(a), as well as other approaches that could slash the risk of cardiovascular disease more than drugs like statins can.
Statins, approved in the late 1980s to lower levels of low-density lipoprotein (LDL) cholesterol, have been a lifesaving tool: They cut risk of heart attack and stroke by up to 50 percent for the more than 200 million people globally who take the medications. Yet even statin takers still get heart disease, and some still die. Cardiovascular disease remains the leading cause of death in the United States and across the world. Clearly, something’s been missing from the cholesterol picture.
The picture coming into focus today incorporates not just bad, LDL cholesterol and good, high-density lipoprotein (HDL) cholesterol, but also lipoprotein(a) and a poorly understood substance called “remnant cholesterol.” Medical researchers aim to minimize all of these except HDL. And HDL cholesterol itself, though it’s still understood to be beneficial, has turned out to be more complex than anticipated. Various attempts to raise HDL levels haven’t improved people’s health beyond what statins already achieve.
Yet despite this and other disappointments in which medicines haven’t panned out as expected, many researchers feel optimistic about treatments currently in clinical trials. “It’s really an exciting time,” says Stephen Nicholls, a cardiologist at Monash Health in Melbourne, Australia.
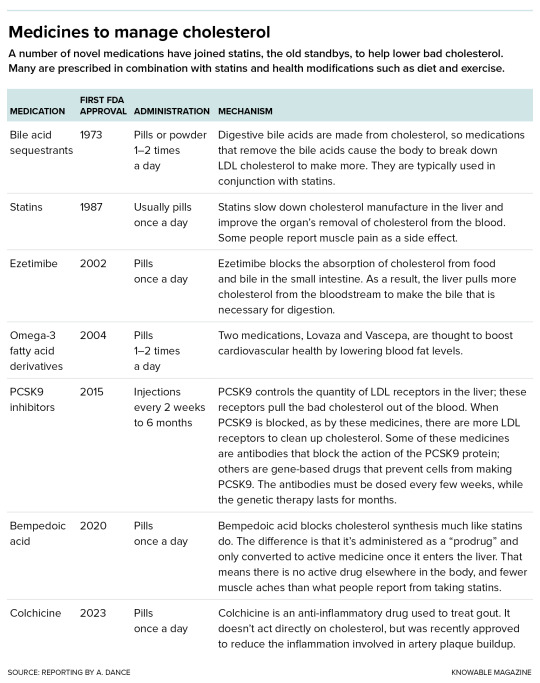
The list of drugs used to address high LDL cholesterol is growing.
LDL Cholesterol
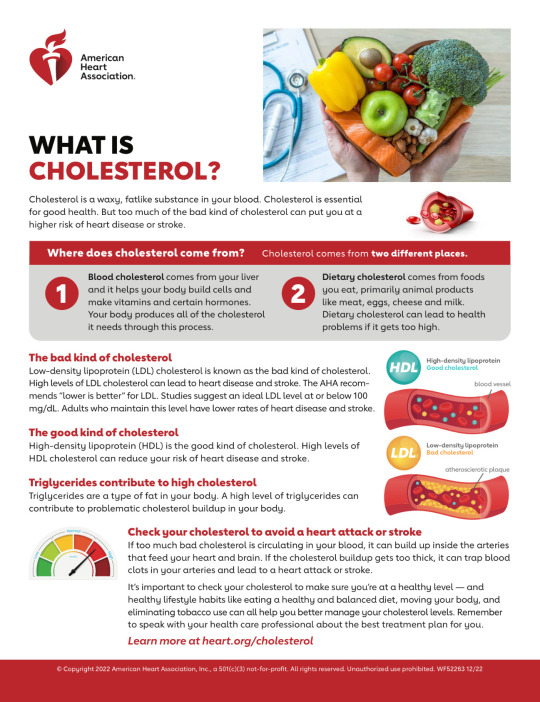
Though it gets a bad rap among the health-conscious, cholesterol plays important roles in our body: It helps to control the stability and fluidity of cell membranes and is an important starting ingredient for making hormones such as testosterone and estrogen. What matters for our health is the company that the cholesterol molecule keeps when it travels.
Its waxy nature means it can’t mix well with water, so it can’t pass through the bloodstream on its own: Lone cholesterol molecules would separate out, like oil does in water. Cholesterol’s solution is to join up with complexes of proteins and fats, called lipoproteins, that carry it around. These lipoprotein carriers include LDL, HDL and other types. Cholesterol, in addition to being cargo, is a structural part of these carriers, too.
Lipoproteins are made in the gut and liver, and they deliver cholesterol and fat to body tissues. Fat goes to muscles, to be used for energy, or to fat tissue for storage. Cholesterol is dropped off in tissues to be incorporated into cell membranes or made into hormones. Cholesterol can also be returned to the liver where it can be stored, incorporated into new lipoproteins, turned into bile acids used by the digestive system to break down fats, or sent to be excreted.
When the delivery particles from the liver have dropped off most of their fats, they become LDL particles, which are still jam-packed with cholesterol. The problem happens when these LDL particles, instead of returning to the liver to be recycled, squeeze into blood vessel walls and get chemically modified. There, they incite or exacerbate an immune reaction called inflammation. In response, immune cells come in to eat LDL particles — but if they eat too much, they can get stuck in the blood vessel wall. This forms the beginnings of an atherosclerotic plaque.
Over time, that plaque accumulates more cholesterol, more fat and more immune cells, reducing the space through which blood can flow and deliver oxygen to tissues. If a plaque limits blood supply to the heart, it might cause chest pain called angina. A plaque might also lead to formation of a blood clot, which may break off and clog vessels elsewhere. The clot might cause a stroke in the brain, for example, or a heart attack.
Today, it’s clear that the less LDL cholesterol in the bloodstream, the better. Statins are good at achieving this, cutting LDL cholesterol levels by up to about half. And for those who need a bigger effect, or who can’t tolerate statins (muscle pain or weakness is an occasional side effect), there are newer medicines. “We now have the ability to get almost anyone’s LDL cholesterol down into the range that we would consider appropriate,” says Steven Nissen, a cardiologist at the Cleveland Clinic in Ohio.
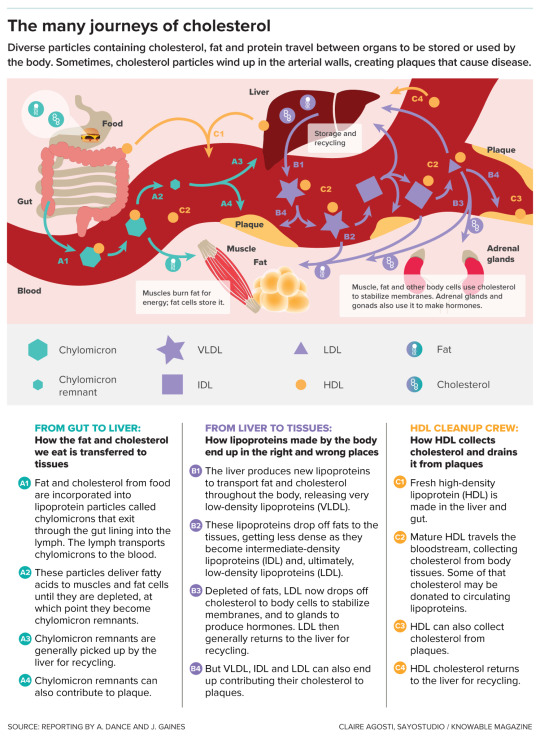
As cholesterol moves around the body within various protein- and fat-containing particles, it aids in important functions but also has the potential to create health risks.
Lipoprotein(a)
But these LDL-cholesterol treatments generally don’t do much against levels of lipoprotein(a), pronounced “lipoprotein-little-a.” This substance, composed of LDL cholesterol particles plus an extra protein, apolipoprotein(a), is mysterious: Scientists don’t know what its natural job is, though since apolipoprotein(a) has some similarity to a protein involved in blood clotting, it might have a role in wound healing. But it can’t be all that important to animal survival: Weirdly, the gene that carries instructions for making apolipoprotein(a) is found only in certain primates. (A similar gene evolved in hedgehogs.)
It’s also unclear why lipoprotein(a) is such a bad version of cholesterol, but it’s clearly up to no good much of the time. It delivers cholesterol to the blood vessel walls like LDL does, promotes blood clotting that blocks arteries and can cause inflammation and increase the risk of clots. And if your lipoprotein(a) is high — too bad. “Statins won’t get it down,” laments Gibson. “Exercise doesn’t get it down. Diet doesn’t get it down.”
Some of the newer LDL cholesterol-lowering drugs can reduce lipoprotein(a) cholesterol a bit, but probably not enough to significantly reduce cardiovascular risk, says Anand Rohatgi, a cardiologist at the University of Texas Southwestern Medical Center in Dallas. The only thing physicians can do, in extreme cases, is to regularly administer a blood-cleaning procedure called apheresis to remove lipoprotein(a).
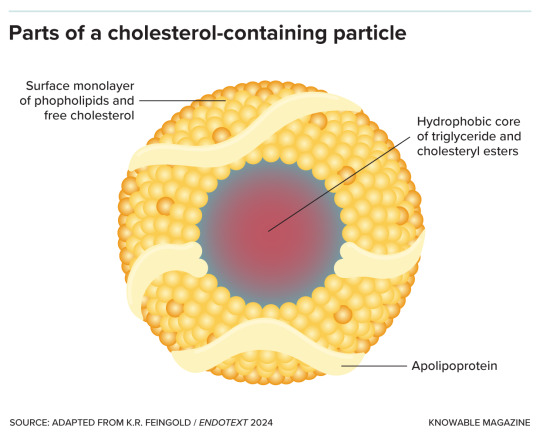
Lipoprotein particles are made up of a core containing fat in the form of triglycerides and cholesterol in the form of cholesteryl esters, surrounded by phospholipids, free cholesterol molecules and apolipoprotein.
For a long time, doctors ignored lipoprotein(a). “Nobody measured it, because you could not do anything about it,” says Prakriti Gaba, a cardiologist at Brigham and Women’s Hospital in Boston. That may be about to change now that several groups are testing medicines that target the substance. (Gaba got her own levels checked at a cardiology conference, where booths offering free tests have sprung up recently.)
Many of these experimental medications use genetic technology to silence the apolipoprotein(a) gene. In a handful of small studies, involving dozens to a few hundred subjects each, different apolipoprotein(a)-silencing therapies cut lipoprotein(a) levels by varying levels, from no change up to 92 percent. But it isn’t yet known whether cutting lipoprotein(a) will actually reduce cardiovascular problems. “We won’t know for a while,” says Leslie Cho, a cardiologist at the Cleveland Clinic who’s coleading one of the trials.
Cho’s HORIZON study, the farthest along, is testing a lipoprotein(a)-gene-silencing treatment compared to a placebo in more than 8,300 people with high lipoprotein(a) and a history of heart problems such as heart attack or stroke. The hope is that reducing lipoprotein(a) will decrease the rate of heart attacks, strokes, need for a medical procedure to improve blood flow, and death, but HORIZON isn’t expected to have results until 2025. Another trial that Gaba is involved in, called OCEAN(a)-Outcomes, is testing a similar approach in about 6,000 people, but is not expected to be completed until the end of 2026.
HDL Cholesterol
Just as lipoprotein(a) and LDL cholesterol are known as the baddies, HDL cholesterol has long been considered a good guy. HDL particles are thought to help by sucking cholesterol out of plaques. The HDL then takes this cholesterol to the liver for recycling or disposal. It’s the cardiovascular system’s cholesterol “garbage truck,” says Bob Eckel, a retired cardiometabolic physician and professor emeritus at the University of Colorado Anschutz Medical Campus.
If high levels of HDL cholesterol are good, scientists reasoned, then more of this cleanup crew should be even better. Exercising and weight loss can both raise HDL cholesterol. Scientists have tried to do the same with medications — but with disappointing results. The drugs did raise HDL cholesterol levels, yes, but they didn’t save lives in people already on statins, and they were weaker than statins at stopping heart attacks and strokes. “To sum it up very simplistically, approaches to raise HDL failed. Nothing really worked,” says Anatol Kontush, a lipid biochemist at the Sorbonne University in Paris.
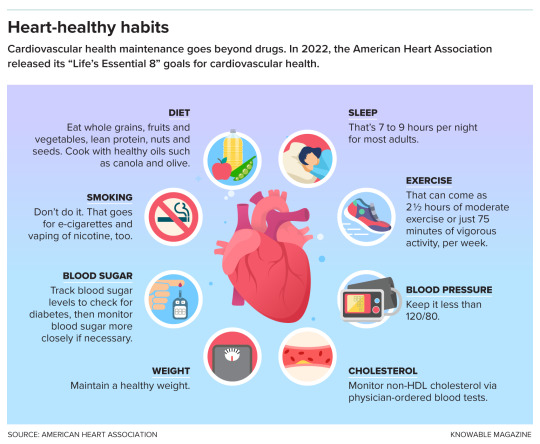
Lifestyle changes can help to reduce the risk of heart disease.
It’s not entirely clear why raising HDL cholesterol in statin-takers bombed. It might be that the idea of boosting HDL cholesterol was simply wrong. High HDL cholesterol might be a marker for good cardiovascular health, rather than a direct cause of it, says Rohatgi. If so, artificially amplifying its levels wouldn’t help.
But the problem also might have been an overly simplistic understanding of HDL cholesterol. Scientists now know that HDL comes in many types and can do many jobs. In addition to hoovering up cholesterol from plaques, it can fight inflammation — that’s good. But sometimes, HDL can turn bad and promote inflammation instead, Cho says, though it’s not clear how. And, she adds, people who are genetically wired to make too much HDL cholesterol can have an enhanced risk for heart disease.
The problem, then, may be that various drugs meant to amplify HDL cholesterol focused on quantity over quality, and increased the wrong kind of HDL. For example, one promising category of drugs raised HDL levels by inhibiting an enzyme that transfers cholesterol away from HDL particles, giving it to LDL particles. Several studies found these inhibitors failed to improve heart health. It might be that stopping the transfer of cholesterol away from HDL particles means the particles had less capacity to pick up new cholesterol from plaques, leaving the cholesterol to languish there. In other words, these garbage trucks were already full.
So the new plan, a last-ditch effort to save lives with HDL, is to help HDL do its cholesterol-removal job better, rather than to just make more of it. Gibson, for example, is chairing a clinical trial of a medicine called CSL112. It’s made of the key protein component of HDL particles — that is, it’s the starting material for HDL particles but still empty of cholesterol. These CSL112 molecules seem to work by creating new HDL molecules primed to pack in as much cholesterol as they can possibly hold. In a preliminary study of more than 1,200 people, two-thirds of whom received CSL112 infusions, the treatment was safe. And when the scientists took blood samples for lab tests, they found that the higher the dose of CSL112 participants received, the more their blood was able to suck up cholesterol.

Depending on their composition, lipoprotein particles can be of different sizes and densities, from small and dense like HDL to large and less dense like chylomicrons and VLDL.
In another study called AEGIS-II, the researchers tested CSL112 infusions in a larger group of people who had just suffered a heart attack and could be most likely to benefit from treatment. Following 18,200 people for a year, it asked whether CSL112 prevents second heart attacks, strokes and death in this population. “That’s a really big, definitive study, and if that doesn’t work, then I suspect the field will completely abandon HDL,” said Nicholls some months back.
In mid-February, CSL of King of Prussia, Pennsylvania — CSL112’s makers — announced that the study did not achieve its main goal of reducing major cardiac events such as stroke, heart attack or death. The researchers are still analyzing the data and will present results in more depth at the American College of Cardiology conference in April.
Triglycerides
If the HDL waters seem murky, the situation with triglycerides, the fatty component of blood that’s carried around in lipoprotein particles, is muddier still. The amount a person has depends on lifestyle: diet, exercise and so on. High triglycerides are linked to a greater risk for cardiovascular disease, and very high levels can lead to inflammation of the pancreas, known as pancreatitis. Thus, it made sense to posit that getting rid of triglycerides would be a healthy thing to do, and many studies have attempted just that — with boggling results.
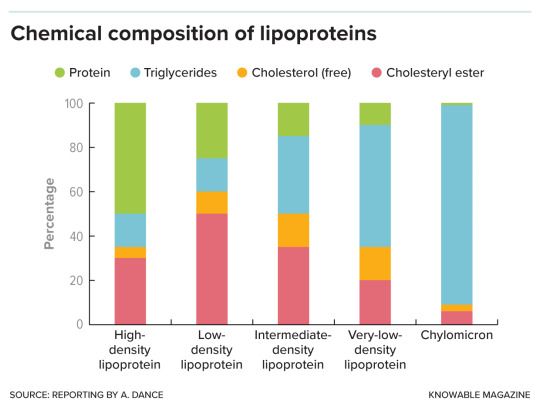
Lipoproteins are made up of protein, fat in the form of triglycerides, and cholesterol — both free cholesterol and a chemically modified, cholesteryl ester, form. The proportion of each varies with lipoprotein type.
One top candidate to reduce triglycerides is based on fish oil, which is high in the omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Diets rich in fatty fish or omega-3s have long been linked to lower rates of cardiovascular problems. The fish or fish oil supplements are thought to work by cutting down on fat production by the liver.
So, in a study called REDUCE-IT, researchers tested a highly purified derivative of EPA in more than 4,000 people with cardiovascular disease or diabetes. They compared these patients to a similar number of people who received inert mineral oil as a placebo.
At first glance, the results reported in 2019 looked “really spectacular,” says Nicholls, who wasn’t involved in the trial. In the group that had taken the EPA for about five years, risk of major cardiovascular problems or death dropped by 25 percent or more compared to those getting a placebo. But oddly, this benefit came without a big reduction in the triglycerides themselves.
In other words, “if EPA is working, it’s doing something other than lowering triglycerides,” says Kenneth Feingold, an endocrinologist and emeritus professor of medicine at the University of California, San Francisco. EPA might counter inflammation, for example, or stabilize the membranes of heart cells.
Based on the REDUCE-IT results, the US Food and Drug Administration approved the purified EPA derivative in 2019 as a medicine for people with high triglycerides and other cardiovascular risk factors. But things got more confusing in 2020, when Nicholls, Nissen and colleagues published another trial, called STRENGTH. This study also aimed to lower triglycerides in high-risk patients, about 6,500 of them, using EPA plus DHA. The researchers compared these patients to people who received a corn oil placebo. But the team halted their study early because, although triglyceride levels did fall, EPA plus DHA didn’t seem to have any beneficial effect on the rate of heart attack, stroke, hospitalization for heart problems, or death.
Researchers are still debating why REDUCE-IT hit paydirt but STRENGTH faltered. Looking back at REDUCE-IT, some experts see a problem with the mineral oil placebo that was used. LDL cholesterol levels and signs of inflammation went up in that group — and if the control participants were worse off than if they’d received nothing at all, then their data would make the experimental treatment look better than it really is.
But Gibson, who was part of the REDUCE-IT team, argues for a different explanation: that pure EPA is better than the EPA/DHA combo. And supporting REDUCE-IT’s conclusions, he points to an older, 1990s study that compared people taking EPA plus statins with people taking statins alone and also found fewer major coronary events in the EPA group.
Then, in 2022, came the latest blow to the once-promising idea of lowering triglycerides: the PROMINENT trial, in which Eckel and colleagues tested a drug called pemafibrate that reduces blood triglycerides. The 10,000-plus study participants had type 2 diabetes, high triglycerides and low HDL, and were at risk for cardiovascular events. But even though triglyceride levels fell by about 26 percent, on average, in the group receiving the drug, this made no difference to the rate of cardiovascular events.
Taken together, the results suggest that triglycerides indicate poor cardiovascular health without being the reason behind the problem. “Triglycerides were just innocent bystanders,” concludes Eckel. The exception, he adds, might be people with very high triglycerides who are at risk of pancreatitis and might still benefit from triglyceride-lowering treatment.
Remnant Cholesterol
This is a loosely used term, with science still to be settled. In the doctor’s office, physicians assume that any cholesterol that isn’t HDL or LDL is a leftover or “remnant” fraction. From a molecular point of view, remnant cholesterol is a fat-delivering lipoprotein in an intermediate state: It left the liver, loaded with fat and cholesterol, and has dropped off some of its triglycerides in the body’s tissues, but not so much of its cargo that it’s become an LDL lipoprotein. Chylomicrons from the gut, once depleted of fats, also become remnant particles.
In people with healthy metabolisms, the body quickly disposes of remnant particles. But if a person has a problem such as diabetes or obesity, these fatty remnants might stick around. Remnant cholesterol may accumulate in atherosclerotic plaques, potentially making it as dangerous as the classic bad LDL cholesterol. Indeed, high levels of remnant cholesterol have been linked to cardiovascular disease in some studies, quite independently of patients’ LDL cholesterol measurements. That suggests that getting rid of those remnants could be beneficial.
The substances remain a bit of a black box, though. “We still don’t know precisely how to define them, we don’t know precisely how to measure them, so it’s kind of difficult to be precise about remnants,” says Feingold. Nonetheless, some researchers are interested in treatments that might target remnants in addition to, or instead of, triglycerides. For example, Nicholas Marston, a cardiologist at Brigham and Women’s, and colleagues are testing a medication called olezarsen that, he says, appears to promote clearance of the cholesterol-carrying particles. But it will take more study to learn if that translates into fewer cardiovascular problems.
Remnant cholesterol is “probably important,” says Nissen — so even though the science is still nascent, he says he feels hopeful about the potential of treatments targeting it.
In sum, the emerging picture is one in which certain forms of HDL cholesterol are good and all the other lipoproteins are bad. The best approach, experts suggest, may be to reduce all the non-HDL cholesterol — whether by diet and exercise or some of these new medicines, should they prove effective.
“If it’s not HDL, we should minimize it,” says Feingold. “The lower, the better.”
— Editor’s Note: This article was amended February 15, 2024, to add the preliminary results of the AEGIS-II trial aimed at raising levels of HDL and to remove a speculative quote about the ramifications of a positive result from the trial.
#Source: KnowledgeMagazine.Org#Cholesterol#Latest Science#Blood Levels of HDL | LDL#Cardiovascular 🫀 Health#Medicines to Manage#Lipoprotein#Triglycerides#Remnant Cholesterol
0 notes
Text
What Does A Lipid Panel Test If The Lipid Profile Is High?
The lipid panel tests for the number of triglycerides, cholesterol, and HDLC in your bloodstream. Triglycerides are a form of fat produced by the liver during digestion. Cholesterol is a type of fat produced by each cell's mitochondria as part of metabolism and it can be found in your blood vessels too. High-density lipoprotein (HDL) removes fats from the walls of arteries and carries them to the liver where they become low-density lipoprotein (LDL). LDLs carry cholesterol that cannot be used to make cells or hormones back into body cells to be recycled back into appropriate tissues such as skin or muscle.
0 notes