Text

i've been having some trouble falling asleep lately
#art#i'll be yapping in the tags#its not that im depressed or anything. it is the opposite actually#ive been using this medicine for quite some time. and it made all my negative emotions disappear#“oh wow huh but isnt it great you don't feel bad anymore”. this is the same thing my psychiatrist told me when we were discussing this topic#in hindsight it was kinda silly of her to say. i can't believe i pay a ridiculous amount of money per session just to hear shit like that#but she's cute and im a pathetic homosexual who'll seethe at the sight of other specialists like a beaten dog so I will let it slide i guess#we see each other twice a year anyway and all i need from her is the prescription for happy pills. anyway the happypillen#i would fight god if it means i can use stertraline for the rest of my life. thanks to it i can and i do live#but I don't really feel like myself anymore. do you get what i mean#the things that have been giving me anxiety attacks or flashbacks not so long ago? i feel almost nothing about it at this momet#it still haunts me to this day but the intensity of my feelings and emotions does not reach even 1/5 of what it was before#i do not want to disclose more specific topics so i will use a simple example. i used to be afraid of dogs#the fear was so severe that the mere sight of the tiniest little barfing creature was enough for me to freeze#now i can pass one without any problem. the fear i feel today is nothing more than a shadow of bygone times (something i do out of habit)#but i guess this example is not objective enough since my close irl friend has a dog that i became fond of#im still pretty sure this dog of her is capable of biting my ass off if necessary but im not afraid of it#because fear is not an option in this brain of mine at this moment#i don't feel any anxiety sadness or anger anymore. even if something close to it begins to rise in me it shuns down within a few minutes#i can't even cry. i am craving emotions that i was so eagerly trying to dispose of back then#i feel the most mentally stable I have ever been and at the same time i feel pretty much dead.#perhaps i just got used to the fact that sorrow accompanied me for a very long time and i should learn to live without it#perhaps sorrow is just as important as happiness and its absence is a mere side effect of the happy pills#and i have to put up with it in order to have a functional brain#perhaps we people are never happy with what we have in our hands. also i hate drawing#one's can tell since the picture i attached is raw as fuck#but even despite my praised mental stability if i were to stay alone with it even for a minute longer i would go insane#next time i will draw something lighter and cuter. like my favorite kpop boy or fortnite. maybe in the next century#thanks for coming to my tedtalk. bye#i made a typo in the word “sertraline” but im too lazy to fix it i would fight god for you but i will not do this im sorry zoloft
3 notes
·
View notes
Note
I have GAD, clinical depression, and panic disorder. Im also pregnant and my psychiatrist has been telling me since before I was pregnant that he will not let me take Zoloft past 20 weeks “it’s too dangerous for the fetus” well im at 19 weeks, just lowered the dosage for the first time and had my first panic disorder episode in years. My OBGYN has told me she’s completely fine with me taking Zoloft the whole pregnancy and the “fears” this guy has been yelling about are rare and that my health actually needs to come before the fetus’s since my health literally directly affects the fetus. So I put my fucking foot down today and sent him a message not asking, but telling him I will not be stopping Zoloft. I may have to quickly get a new psychiatrist if he decides his campaign against psych medications (which…is a major part of his job but ok) is more important than my mental and yes PHYSICAL well-being (brain fog, eye strain, fatigue and headache today made me unable to do any of my work for my job or even basic functions to care for myself like bathing or brushing my teeth) is less important than the fetus which would not grow at all without me, but I’ve just had enough. It’s going to be a bitch and a half to find a new psychiatrist and start all over again with someone but I can’t take him anymore. I’m in the U.S. btw. I just can’t stand people who stigmatize and demonize mental and emotional illness as somehow optional for treatment because of “ooo scary drugs are bad” mentality even when they WORK IN PSYCHIATRY AND HAVE ACCESS TO THE ACTUAL, PRESENT DAY DATA SHOWING HOW MEDICATIONS WORK. It should be the person’s choice what their treatment is and how they pursue it, medication or not. My womb doesn’t make me a second class citizen either and I’m so tired of that mentality as well. Sorry I just really needed to rant and felt like you’d understand where I was coming from on this. Ugh. Anyway, I am wishing you all the best in your recovery from your recent traumas and continued contentment, peace, and happiness!
I fully support you. In the end it should be up to you whether to go off a medication, pregnant or not. He can make suggestions and have his opinions, but you should have the final say. And if he's not letting you decide, you're in your full right to go see someone else. Especially if there's not even medical consensus that the med might actually harm the fetus.
14 notes
·
View notes
Text
ok i got to a point where i finally felt normal enough again after going cold turkey off wellbutrin+zoloft (lol please don’t do this btw) and a few weeks ago i started taking ashwagandha and extra strength magnesium gelcaps in the mornings again and i do feel different. more alert less foggy less obsessive. more motivation to do other things. i still think i need more iron and b6/12. thankfully tension tamer tea has some of the latter and i can get actual pills for all of them at the store. very important to take care of asap since i just know i won’t be comfortable cooking in our new living situation/we won’t have our own fridge space. once i get those levels back up umm i’m hoping i’ll be able to have enough energy to move around/stand up without being lightheaded and the variety of types of jobs im comfortable applying for will open up considerably. i really really want to try the ketamine clinic but i think that’s just going to have to wait until we’re in our own place again and we have more expendable cash. and who knows maybe i’ll magically feel better and i won’t need to spend all that money begging my brain to love me despite the physical circumstances
16 notes
·
View notes
Text
I'm on OB rotation again. I asked the attending what are things the PCP should know about prenatal and postpartum pts. Stuff we discussed:
SSRIs can be continued during pregnancy. I often see patients on Zoloft during pregnancy if they need an antidepressant. In fact, I just started a prenatal patient on Zoloft the other day in clinic. It is safe to continue SSRIs during pregnancy because you should treat the patient's depression. Babies can come out sort of jittery because of the SSRI, but that goes away.
Postpartum patients will have bleeding somewhat similar to a menstrual period right after giving birth. It starts to decrease and becomes like a brownish color and can last up to 6 weeks postpartum. Any bleeding beyond that point is abnormal.
There is some evidence that if you have estrogen-containing birth control, it can decrease milk supply. Actually, I had a patient in clinic recently who was seen by an attending and he started her on a progesterone only birth control so that it would not affect her milk supply. Estrogen decreases the patient's milk supply, so patients who plan to breast-feed should not be started on estrogen-containing birth control. Right after giving birth, your body has increased amounts of estrogen, so you would not start estrogen containing birth control until at least 6 weeks postpartum anyway. Increasing estrogen immediately postpartum increases risk of blood clots. For patients who plan to breastfeed and want to be on an oral contraceptive, use progesterone only oral contraceptives until she stops breastfeeding.
If the mother is breastfeeding at least every 4 hours, then this can be used for contraception. It's about 80% effective. Once baby starts sleeping through the night or once baby starts feeding more than every 4 hours, this method won't work! If you go more than 4 hours without breastfeeding, breastfeeding will not protect you from pregnancy! You can also ovulate before your menstrual period returns, so you can't say you can't get pregnant because your period has not returned yet!
I asked the attending I worked with today about how she goes about prescribing birth control. She said she will usually start with Sprintec. It's usually covered by insurance and if it's not covered, it's pretty affordable. She also said Junel is pretty well tolerated. Certain progestins in certain brands of birth control may work better for certain things like acne control, but she didn't have as much knowledge on that. I'll ask another attending again about that. I usually start people on Sprintec as well.
PCP should know that alkaline phosphatase is high in pregnant patients. It comes from the placenta. So don't be freaked out by that.
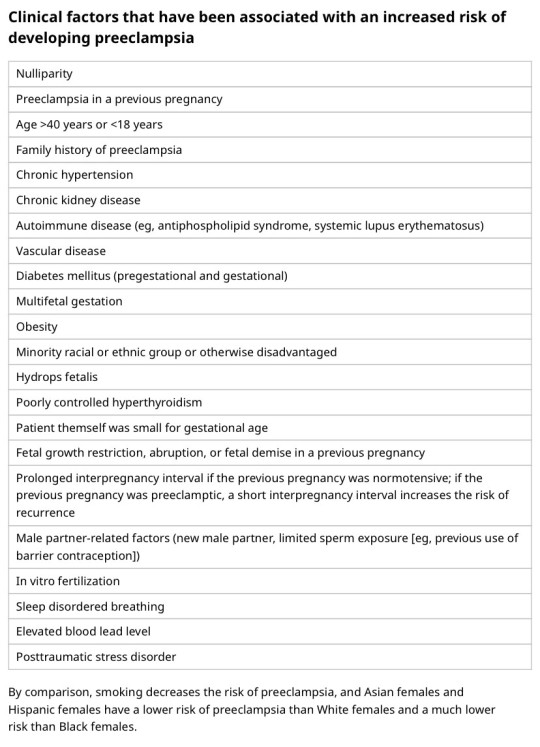
You should know HTN in pregnancy and preeclampsia workup. High BP is 140/90. Severely high BP is 160/110. Swelling occurs in many pregnant pts, but that should also alert you to start preeclampsia workup.
[Preeclampsia w/u from UpToDate:
Diagnostic evaluation
•Laboratory – Patients with suspected preeclampsia should have a complete blood count with platelets, creatinine level, liver chemistries, and determination of urinary protein excretion.
•Fetal status – Fetal status is assessed concurrently or postdiagnosis, depending on the degree of concern during maternal evaluation. At a minimum, a nonstress test or biophysical profile is performed if appropriate for gestational age. Ultrasound is used to evaluate amniotic fluid volume and estimate fetal weight, given the increased risk for oligohydramnios and growth restriction.
•Consultation with the neurology service is generally indicated in patients with neurologic deficits/abnormal neurologic examination, which may include ocular symptoms or a severe persistent headache that does not respond to initial routine management of preeclampsia.]
An important thing to review is physiology of pregnancy. Blood volume increases during pregnancy, so there are lots of new RBCs and that will throw off a HgbA1c reading, therefore HgbA1c is not measured during pregnancy and will not be accurate! My attending today told me there was a midwife who offered pts either HgbA1c or oral glucose tolerance tests to screen for gestational DM. The HgbA1c is not accurate in pregnancy, so this should not be done. That would be bad to miss a diagnosis of gestational diabetes. You have to wait until 3 months postpartum to measure HgbA1c to get an accurate reading. Had a pt who did not have a PCP prior to getting pregnant, was on insulin during the pregnancy, and after giving birth, still needs to establish with PCP for diabetes f/u. After you give birth, you insulin needs drastically change, so you don't need as much as you did when you were pregnant. So I stopped her insulin and advised that she f/u with her new PCP for diabetes care.
I still need to review fetal heart tracings. The attending today said the first thing to look at is the baseline (the baseline HR should be about 160 beats/min), then the variability, then look for accelerations and decelerations. If more than 32 weeks GA, accelerations are 15 beats/min above the baseline lasting at least 15 seconds. Early decelerations are representative of compression of the fetal head, which is normal during labor as baby moves down the pelvis/birth canal. Variable decelerations look sharper like a "V" and can represent compression of the umbilical cord. Late decelerations represent placental insufficiency.
ACOG has very helpful practice bulletins.
I can't take screen shots on my work laptop, so I'm just going to summarize gestational HTN w/u from UpToDate:
Gestational HTN: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions 4 hours apart after 20 weeks of gestation in a previously normotensive individual
And:
No proteinuria
No signs/symptoms of preeclampsia-related end-organ dysfunction (eg, thrombocytopenia, renal insufficiency, elevated liver transaminases, pulmonary edema, cerebral or visual symptoms)
Preeclampsia: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions at least 4 hours apart after 20 weeks of gestation in a previously normotensive individual. Patients with systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg should have blood pressure confirmed within a short interval (minutes) to facilitate timely administration of antihypertensive therapy.
And:
Proteinuria (≥300 mg per 24-hour urine collection [or this amount extrapolated from a timed collection], or protein:creatinine ratio ≥0.3, or urine dipstick reading ≥2+ [if other quantitative methods are not available]).
In a patient with new-onset hypertension without proteinuria, the diagnosis of preeclampsia can still be made if any features of severe disease are present.
Preeclampsia with severe features: In a patient with preeclampsia, presence of any of the following findings are features of severe disease:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg on 2 occasions at least 4 hours apart (unless antihypertensive therapy is initiated before this time)
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
Progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL [97 micromol/L] or doubling of the serum creatinine concentration in the absence of other renal disease)
Pulmonary edema
Persistent cerebral or visual disturbances
Eclampsia: A generalized seizure in a pt with preeclampsia that cannot be attributed to other causes.
HELLP syndrome: hemolysis, elevated liver enzymes, low platelets. Hypertension may be present (HELLP in such cases is often considered a variant of preeclampsia).
Chronic (pre-existing) hypertension: hypertension diagnosed or present before pregnancy or on at least 2 occasions before 20 weeks of gestation. Hypertension that is first diagnosed during pregnancy and persists for at least 12 weeks postpartum is also consider chronic hypertension.
Blood pressure criteria during pregnancy are:
Systolic ≥140 mmHg and/or diastolic ≥90 mmHg
Prepregnancy and 12 weeks postpartum blood pressure criteria are:
Stage 1 – Systolic 130 to 139 mmHg or diastolic 80 to 89 mmHg
Stage 2 – Systolic ≥140 mmHg or diastolic ≥90 mmHg
Chronic HTN with superimposed preeclampsia*:
Any of these findings in a patient with chronic hypertension:
A sudden increase in blood pressure that was previously well-controlled or an escalation of antihypertensive therapy to control blood pressure
New onset of proteinuria or a sudden increase in proteinuria in a patient with known proteinuria before or early in pregnancy
Significant new end-organ dysfunction consistent with preeclampsia after 20 weeks of gestation or postpartum
*Precise diagnosis is often challenging. High clinical suspicion is warranted given the increase in maternal and fetal-neonatal risks associated with superimposed preeclampsia.
Chronic hypertension with superimposed preeclampsia with severe features:
Any of these findings in a patient with chronic hypertension and superimposed preeclampsia:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg despite escalation of antihypertensive therapy
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
New-onset or worsening renal insufficiency
Pulmonary edema
Persistent cerebral or visual disturbances
A reduction in blood pressure early in pregnancy is a normal physiologic occurrence. For this reason, women with chronic hypertension may be normotensive at their first few prenatal visits. Later in pregnancy, when their blood pressure returns to its prepregnancy baseline, they may appear to be developing preeclampsia or gestational hypertension if there are no documented prepregnancy blood pressure measurements.
BP: blood pressure.
* Blood pressure should be elevated on at least two occasions at least four hours apart. However, if systolic pressure is ≥160 mmHg or diastolic pressure is ≥110 mmHg, confirmation after a short interval, even within a few minutes, is acceptable to facilitate timely initiation of antihypertensive therapy.
¶ The onset of preeclampsia and gestational hypertension is almost always after 20 weeks of gestation. Preeclampsia before 20 weeks of gestation may be associated with a complete or partial molar pregnancy or fetal hydrops. Postpartum preeclampsia usually presents within two days of delivery. The term "delayed postpartum preeclampsia" is used for signs and symptoms of the disease leading to readmission more than two days but less than six weeks after delivery.
Δ Significant proteinuria is defined as ≥0.3 g in a 24-hour urine specimen or protein/creatinine ratio ≥0.3 (mg/mg) (34 mg/mmol) in a random urine specimen or dipstick ≥1+ if a quantitative measurement is unavailable.
◊ Almost all women with the new onset of hypertension and proteinuria at this gestational age or postpartum have preeclampsia, but a rare patient may have occult renal disease exacerbated by the physiologic changes of pregnancy. An active urine sediment (red and white cells and/or cellular casts) is consistent with a proliferative glomerular disorder but not a feature of preeclampsia. Women with chronic hypertension who had proteinuria prior to or in early pregnancy may develop superimposed preeclampsia. This can be difficult to diagnose definitively, but should be suspected when blood pressure increases significantly (especially acutely) in the last half of pregnancy/postpartum or signs/symptoms associated with the severe end of the disease spectrum develop.
§ Photopsia (flashes of light), scotomata (dark areas or gaps in the visual field), blurred vision, or temporary blindness (rare); severe headache (ie, incapacitating, "the worst headache I've ever had") or headache that persists and progresses despite analgesic therapy; altered mental status. Seizure occurrence upgrades the diagnosis to eclampsia.¥ The differential diagnosis of preeclampsia with severe features includes but is not limited to:
Antiphospholipid syndrome
Acute fatty liver of pregnancy
Thrombotic thrombocytopenic purpura (TTP)
Hemolytic uremic syndrome (HUS)
The laboratory findings in these disorders overlap with those in preeclampsia with severe features. (Refer to table in the UpToDate topic on the clinical manifestations and diagnosis of preeclampsia.) The prepregnancy history, magnitude and spectrum of laboratory abnormalities, and additional presence of signs and symptoms not typically associated with preeclampsia help in making the correct diagnosis, which is not always possible during pregnancy.
In addition, a variety of medical disorders may be associated with hypertension and one or more of the signs and symptoms that occur in women with preeclampsia with severe features. These patients can usually be distinguished from patients with preeclampsia by taking a detailed history, performing a thorough physical examination, and obtaining relevant laboratory studies.‡ In contrast to preeclampsia, gestational hypertension is not associated with end-organ involvement, so neither proteinuria nor the symptoms or laboratory findings of preeclampsia are present.
#OB#OBGYN#birth control#gestational HTN#preeclampsia#eclampsia#breastfeeding#gestational diabetes#fetal heart tracing#FHT
2 notes
·
View notes
Text
hello moots i have a question because i am Fucking Stupid. my friend is writing a fantasy novel and having a panic attack because they chose to work on an important piece of world building when they have been out of zoloft for a couple days because of insurance things. so we're having fun.
i am also, as i said, fucking stupid. if said friend needed advice on incorporating other cultures/religions/mythologies into a fantasy world, and wanted to speak to someone about those cultures, how would they find them? this is a stupid question, because i don't seek out other humans if i can help it but i should know this and i fuckin don't. stupid.
and this is less of a "hey do you, my follower, fall into blank category? are you an expert on blank mythology?" and more of, "do you have advice for how to go about finding/hiring someone who would actually be able to help?" like, is there a good subreddit or a tag on tumblr or like anything i can give them to help them organize their thoughts and questions when they don't have the brain space to do so at the moment?
3 notes
·
View notes
Text
Jennifer Hallner, 27 (USA 1997)
In 1997, Jennifer Marie Hallner was killed by a legal abortion in Maryland. The abortion facility responsible for her death was Potomac Family Planning.
She was 6 weeks pregnant and underwent a D&C abortion at the hands of Earl McLeod. It’s important to note that she was perfectly healthy and had no pre-existing medical problems. She should be alive today.
Jennifer was put in the recovery section at 10:10 A.M. with an abnormally high heart rate. She was put on an oxygen mask, but all of the monitors were disconnected from her. 10 minutes later, an employee only identified as Nurse W realized Jennifer was unresponsive.
W’s response was questionable at best. First she told someone to get Jennifer a Zoloft. Zoloft is an antidepressant, which would do absolutely nothing to help revive Jennifer. As the assistant left, W changed the request to Zofran. (It’s possible that she got the two medications mixed up.) However, Zofran is an antiemetic and Jennifer was not showing any signs of vomiting. It’s unclear what this was supposed to do, if anything.
W left an unconscious Jennifer and went into the operating room herself. She asked Dr. K (the anesthesiologist) for Zofran. K did not evaluate Jennifer’s condition but handed over the Zofran anyway. At about 10:25, Nurse W administered Zofran to Jennifer’s IV. Not surprisingly, it did nothing to revive her.
W returned to the procedure room and asked K for Romazicon, a drug used to reverse the effects of drugs used for anesthesia. K again provided the drug to W without examining Jennifer at all.
An employee identified as Nurse H went to check Jennifer’s blood pressure and realized Jennifer’s pupils were fixed and dilated and she had no pulse. H went to get K, who finally examined Jennifer. By this time Jennifer’s blood pressure dropped to an alarming 60/40 and she was still completely unresponsive.
The incompetence continued. The staff who attempted CPR used the pediatric-size bag valve mask on hand, which was the only one on the crash cart. (The fact that an abortion facility had only pediatric emergency equipment on hand raises some disturbing questions about how young their clients tended to be.) McLeod didn’t call 911 until 10:42 and failed to use monitoring equipment. Paramedics arrived to find Jennifer in cardiac arrest. The anesthesiologist could not tell them anything about the patient’s heart electrical activity, which he should have been noting on an EKG. The medics noted the use of a pediatric bag-valve mask (which was not giving Jennifer enough oxygen), and the fact that nobody had put a breathing tube into the patient to make sure that air was being pumped into her lungs and not her stomach.
The medics immediately placed the necessary monitors on Jennifer and used equipment that was actually capable of helping her. Paramedics got Jennifer to Shady Grove Adventist Hospital at 11:09 a.m. The ER doctor noticed that her pupils were fixed and dilated. After aggressive resuscitative efforts by ER staff, Jennifer’s heart was restored to a stable rhythm, and she was admitted to the Intensive Care Unit. But despite their best efforts, she died at 4:15 a.m. on December 21.
The appalled paramedics reported McLeod to the medical board, which faulted him with failure to provide adequate and readily-available post-operative monitoring equipment, and failure to provide adequate emergency supplies. The board also required him to get his staff properly certified in CPR.
An interesting note: The medical board indicates that McLeod told them that when he first opened his abortion facility, he contacted the state asking for guidelines for a freestanding abortion facility. He said he was told that there were none.
McLeod also ran the Hillcrest abortion facility in Harrisburg, Pennsylvania, where Kelly Morse was killed in 1996. She was also not adequately resuscitated. Kelly’s husband filed suit, saying, “No respiration rate was recorded, no pulse was checked and no blood pressure was measured. No EKG was applied. No cardiac monitoring was conducted. No pulse oximeter was applied. No intubation or emergency tracheotomy was performed.” Apparently McLeod didn’t learn from Kelly’s death the lessons that would have saved Jennifer’s life.
(Maryland State Board of Physician Quality Assurance Case Number 98-0472)
(Documentation of Kelly’s suspension)
(Petition by Jennifer’s family)
lawsuit by Jennifer’s family
#death from legal abortion#tw abortion#pro life#tw ab*rtion#tw murder#abortion debate#abortion is not healthcare#abortion#pro choice#unsafe yet legal
11 notes
·
View notes
Text
Mental health/medication talk:
I just got done telling my doctor how much Zoloft has helped me in comparison to Wellbutrin and he did an actual happy dance in his seat. This 50/60’s year old man did a happy dance like a toddler getting ice cream.
And it has. In terms of my ptsd, that’s not an overnight fix obviously. But it has helped tremendously with being in situations regarding being in vehicles and on public transportation.
I’m not saying ya girl is gonna start driving any time soon. But it’s nice getting into a car and not feeling a sense of dread every time.
Yes, it’s kind of stumped my writing a bit. But honestly, there’s more important shit to deal with in terms of dealing with my mental health and a new job and living my life and dealing with grief and loss and it’s…a lot going on. So to be able to sit here and feel content and not stressed even about writing?
Feels good man. Feels fucking amazing.
8 notes
·
View notes
Note
hiii i know this was a bit further back when you asked but i just wanted to pass you on some advice while i still remember to lol. don't be scared to try adhd meds! they're one of the most well researched medications out there, don't do what i did and hold them off as a last resort. i can only DO fitness, get better sleep etc because i'm on the meds and therefore can actually function with day to day tasks better lol. try and get ritalin IR (instant release) they're 10mg (you can even split it and just try 5mg if you're advised to first) and it only last four hours then it goes out of your system so there's no need to worry. i'm not american and a lot of the weirder adhd meds they have aren't allowed in my country but ritalin is very trustworthy and pretty much internationally available, haven't met anyone with adhd who's had a bad time from it, so it's definitely a good place to start. i'm also on sertraline (zoloft in america, considered one of the safest antidepressant/anti anxiety med) for my anxiety and there's a lot of research to support that they actually improve off of each other and are more effective!
also r/adhdwomen is a great community i recommend it to everyone even if they're not a woman tbh. i don't really go to r/adhd there's too many negative vibes
the how to adhd youtube channel is also good
and if you take away anything from all this please please read any of the distraction series of books by hallowell and ratey personally they are my most trusted source (you don't have to read in order the newer the book the better the research) worldwide the system is failing so many through lack of resources and sheer ignorance so how you survive is by educating yourself and being a part of the community
thank you so much this is so informative i rly appreciate it!!!
i've been watching all of how to adhd's videos she's rly good! lots of important information!
my psych in college recommended zoloft to me but i was a little scared so i was on wellbutrin and lexapro instead which he said was lighter?
i'll check out the other resources thank u!!
7 notes
·
View notes
Text
An important thing I want to say to trans women and transfems (and other women too, in fact)
Excessive sweating and body odor can sometimes be seen as unfeminine. Don't believe that lie. EVERYONE sweats and experiences BO, sometimes quite a lot, regardless of sex or gender; it's completely normal and natural, especially if you're taking a medication like sertraline (Zoloft) that makes you more prone to overheating. You probably knew all that though, so here's what I actually want to say:
If you are or were using a deodorant marketed towards men, and it's working for you, then there's nothing wrong with continuing to use it. There's also nothing wrong with switching over. Trust me, as an AFAB person who spent most of her life using deodorants marketed towards women, I used to have sweat literally dripping down my sides even when all I was doing was calmly sitting in a chair. The antiperspirant qualities in something like Old Spice tend to be much stronger, and personally I use the lavender Gentleman's Blend stuff so that I don't smell like my dad.
Ultimately, use whatever makes you feel the most comfortable in your own skin. Just be aware that a lot of corporations are stupid lol
#I'm really sorry if this comes off as out of touch or anything like that#I just don't want you to be as sweaty and miserable as I was#trans#transgender#transfem#transfemme#mtf#nb#nonbinary#genderqueer
5 notes
·
View notes
Text
Top 5 Medications for Depression
What are the best medications for depression? Find out here!
Depression affects millions of people in the United States every year. It can cause feelings of sadness, hopelessness, anxiety, and even thoughts of suicide. While there are many different types of treatments available, medication remains an important part of treatment.
Citalopram
Celexa is one of the most commonly prescribed antidepressants in the U.S. It works by increasing levels of serotonin in the brain. Serotonin is a neurotransmitter that helps regulate mood and behavior.
Escitalopram
Lexapro is an antidepressant medication that has been approved by the FDA since 2002. It is used to treat major depressive disorder, panic disorder, social anxiety disorder, obsessive compulsive disorder, postpartum depression, premenstrual dysphoric disorder, and generalized anxiety disorder.
Prozac
Prozac is one of the most commonly prescribed antidepressants in the world. It was first introduced as a treatment for depression in 1987. It works by increasing levels of serotonin in the brain. Serotonin is a neurotransmitter that helps regulate mood and behavior.
Fluvoxamine
Fluvoxamine (Luvaxa) is an antidepressant medication used to treat major depressive disorder (MDD). It belongs to a class of drugs called selective serotonin reuptake inhibitors (SSRIs), which work by blocking the reabsorption of serotonin back into the presynaptic neuron. This allows more serotonin to remain available at the synapse, where it binds with postsynaptic receptors and triggers a response.
Zoloft
Zoloft is like Celexa on steroids. Zoloft is actually my favorite depression medication. It not only balances the chemicals in your brain to make you feel better but it also gives you energy. The impact of the Zoloft in the brain also gives you a real sense of well being. Zoloft also treats panic disorder as well as depression. I have both conditions and Zoloft works for both.
#mental illness#bipolor#mental disorder#mental health#mental problems#mental wellbeing#mentalheathawareness#mentally exhausted
5 notes
·
View notes
Text
so i went down to 75mg of zoloft on thursday night. i had tension headaches friday-sunday, but i get those anyway so it's very hard to tell if that was due to the dose decrease or due to other factors (resuming desk work, resuming shoulder pt). as of yesterday i'm not having headaches, and i'm not feeling any other withdrawal symptoms.
generally i don't feel much different except that i may feel a bit more emotional? not in a mood swing way, just that my emotions feel slightly heightened? again, hard to tell what's changing vs what i'm just paying a lot of attention to.
i have not had any increase in obsessive thoughts, which is my main concern. it's important to note, though, that when i first started zoloft i was put on 50mg, and at that point i reached a massive reduction in obsessive thoughts. the only reason i went up to 100mg is because my new psych at the time told me that 50mg couldn't actually have any impact. going from 50 to 100 didn't seem to change much for me with the thoughts (though i am trying to remember events from 2011, so who knows)
it's been very difficult to find experiences from other people about getting off medications that aren't from people who have had extremely bad experiences with medications and with the medical system. this is why i'm posting about this- just for variety. generally speaking, my medication has helped me so, so much, and i'm tinkering now just because i want to know how much work the medication is doing versus me having developed skills and mechanisms for handling my anxiety and ocd.
0 notes
Note
Hi Love, I hope you're doing alright. I saw both of your posts about not doing well and getting medicine for your panic disorder.
And I wanna say. I'm so proud of you for taking that step. The first step of getting a doctor and getting the meds is always the hardest.
I do have a few tips, although I don't have a panic disorder. I have severe depression, anxiety and adhd.
(Down below is quite a bit of info. Perhaps even scary/nervewracking. And I'm not trying to scare you so I'm so sorry if I do. I just want you to know some things that I didn't personally know when I first started taking meds)
I want to note though. Keep your head up. Don't stop trying. The first medicine doesn't always work for everyone. The whole process is trial and error to find the one that works for you. So if it doesn't help, don't feel too bad yeah?
I know that for me, it took 5 different types before getting to Zoloft which works for me. And I'm currently on my 4th attempt to find one for my Adhd.
I read in your thing of if get weightloss from meds. I'm sure your doctor mentioned it but I want to mention it. If you're someone whose weight fluctuates and you find your self lose or gain 10 pounds. It's not bad. But keep an eye on it, make sure it's not a constant and only a sudden one and done.
For me. Zoloft made me gain 15 pounds. And after trying so many times to get a med to work. I honestly don't care. I'd rather be mentally okay. Ofc it's different for everyone but just know it's normal.
Something my doctor never mentioned, was be absolutely careful when it comes to missing your meds. Some meds it's totally okay to just drop it. But others like Zoloft and high dosages, If you cold turkey it, it can Hurt a lot.
If you get any symptoms of feeling sick within first two days of taking a new med. Stop. Idc what a doctor says "you'll get used to it" or "it's a gradual thing" absolutely not. The pain and suffering of getting sick from a medicine is not worth it. I tried powering through once before and I severely regret it.
There's good doctors and bad doctors. Good who actually do the research on meds and bad who go based off of old informational packets.
Idk about most meds. But if a doc says "this used to be used for this. But it's not anymore cause it doesn't work" DONT. if you get prescribed it. Research it before taking one.
I got prescribed blood pressure meds that my doctor said "isn't used to treat that anymore" and said it will help me sleep. I probably almost died cause I already have low blood pressure and got given meds to lower blood pressure.
That's all I can remember at the moment. But If you have any questions, you're more than welcome to come to my DMs.
I really hope you have a safe experience and find something that helps you. We all care for you and wish you the best.
Hello my sweet kind anon🤍 Whoever you are, this means lot to me, you coming into my askbox to encourage me. You're sweetheart🤍🤍
No worrries, you didn't scare me at all !! I am thankful for these tips!!
Yes, you're totally right!! I know, mental health is more important than number of your weight and I need to learn that. If I will be heavier but happier, I won't care too!!
Oh my, I didn't know that!!! That it isn't good to feel sick when taking meds! My doctor didn't tell me about it😶 Thank you so much for telling me, oh my god!! I just need to talk about my doctor about it! And I need to change my meds probably too! 🤔
Oh my god, I am sorry for you that you almost died!!! That's horrible but it's doctor's fault!! How could this happen??!! This stuff shouldn't NEVER happen. Some doctors really should think before saying!!!
But you know what, I am happy for you that you found meds - Zoloft and that it helped you!!
i just had phone call with my doctor, i am gonna take other meds!!
Thank you so much sweet nonnie, you're an angel!! And I am here for you too, if you needed me, anytime. I'll try to help you. I love you so much!
And you're damn strong!! Know that
We all can do that!!!!
1 note
·
View note
Text
Gary Null’s Newsletter Issue 062
In this week’s Gary Null’s Newsletter:
The Cult of Modern Psychiatry
Gary Null's Show Notes
Recipe for Spaghetti and Shiitake Saffron Tomato Sauce
The Cult of Modern Psychiatry
By Gary Null, PhD and Richard Gale
Recently New York Times reporter Matt Richtel published an article entitled “This Teen Was Prescribed 10 Psychiatric Drugs: She’s Not Alone.” The article begins as an honest indictment of psychiatry’s rising irresponsible practice of over prescribing multiple powerful drugs for teens struggling with anxiety, depression and other behavioral disorders. Richtel states the problem clearly. “Many psychiatric drugs commonly prescribed to adolescents are not approved for people under 18. And they are being prescribed in combinations that have not been studied for safety or for their long-term impact on the developing brain.” The practice of prescribing multiple psychiatric drugs, known as polypharmacy, to any given patient has “gone mainstream.” Many of these drugs, such as the entire class of selective serotonin reuptake inhibitors, or SSRIs, carry black box warnings. Because psychiatry has never proven itself as an exact science, physicians frequently experiment by switching drugs, prescribing drugs for conditions they were not licensed for, and combining drugs into highly toxic cocktails. The Times article documents several cases where young adults were taking 9 and 10 drugs simply for a diagnosis of anxiety and depression. In practice, psychiatry is largely based on guesswork rather than empirical evidence.
Admirably, Richtel’s article identifies a crucial problem in modern psychiatric practice for treating common mental disorders. However it suffers from the sin of omission. It fails to specifically identify the nature of the teen’s suffering from polypharmacy practice. Nor does Richtel mention that these drugs commonly cause the very mental illnesses they are prescribed to relieve. He also fails to mention that the entire Chemical Imbalance Theory upon which psychiatric medication for depression is based remains unproven. As we will explore in detail, the theory may be completely erroneous as a fundamental tenet for treating such disorders with drugs.
Richtel’s omissions are no surprise. The New York Times and the National Institute of Mental Health that the newspaper writes on behalf of has lost all credibility for promoting blatant psychiatric quackery. Having been one of the nation’s loudest media cheerleaders for US military interventions in the Middle East, when did the Times ever take responsibility for accurately reporting on the high rates of suicide among military personnel due to the overprescribing of psychiatric medications? It is now well established that SSRIs contribute to suicidal and homicidal ideation. This was the reason for the CDC slapping a black box warning on SSRIs. By omitting the most important facts regarding the failures of SSRIs and other psychopharmaceutical drugs, the mainstream media and the entire psychiatric establishment has been manufacturing madness for decades. So where has the Times and the mainstream media been for the past fifty years when reporting the actual cause of anxiety and depression, and offering legitimate criticisms for prescribing SSRIs and other medications.
In 1986, the pharmaceutical company Eli Lilly released its antidepressant drug Prozac, the world’s first SSRI. Prozac has been called a wonder drug. Since its approval over fifteen other SSRIs, including Paxil, Zoloft, Luvox, and Celexa are now commonly prescribed for depression, obsessive compulsive disorder, anxiety and post traumatic stress. The popularity of SSRIs has skyrocketed. Today, one in every six Americans, approximately 77 million Americans, is taking psychiatric medication, and a quarter of these are long term users. Forty-five million and 31 million for depression and anxiety respectively. This ratio jumps to an incredible 21% among women between the ages of 45 and 64. During the first couple months of the Covid-19 pandemic prescriptions for depression, anxiety and insomnia increased by 21 percent. Worldwide, mental illness is now the leading cause of disability among children. Since 2015, antidepressant use among children between 5-12 has grown 41 percent, the majority being boys.
Active members and veterans of the US military have become especially dependent on psychiatric medications. Seventeen percent of active duty service members are currently taking antidepressants, sedatives, and other psychiatric drugs, which is 7 percent higher than the wider US population. In 2020 the Department of Veterans Affairs reported that it needed to spend $682 million more in 2021 to deal with the epidemic of mental health disorders within the military. Fifty three million dollars was necessary for suicide protection alone, which now averages 20 suicides per day. A decade ago, the Pentagon spent $280 million on psychiatric drugs.
Along with the rise in antidepressant use, there has been a surge in the creation of many new clinical diagnoses for mental disorders. What would have been considered just a few years ago to be rebellious behavior among teenagers is now termed Oppositional Defiant disorder; what was once looked upon as a child not wanting to do math homework is now classified as Mathematics Disorder. The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) includes normal behaviors that have been pathologized as mental disorders. These include Binge Eating Disorder, Caffeine Withdrawal, Hoarding Disorder and Social Communication Withdrawal. As the psychiatric establishment increasingly asserts its importance by pathologizing normal human behaviors, tens of millions of Americans are popping pills in an attempt to find mental wellbeing. All the while, Big Pharma is making a killing; antidepressant drug salesalone are predicted to top $22 billion by 2027 and global sales for all psychiatric drugs are anticipated to reach $41 billion by 2025.
Considering how widely SSRIs are prescribed, you would be forgiven for thinking that this class of drugs is highly safe and effective. In point of fact, these drugs come with a host of devastating and sometimes deadly health implications. Examining the state of the medical industrial complex deeper still makes one thing abundantly clear: Psychiatry is NOT a science but a massively destructive unscientific experiment fueled by a medical industrial complex that values profits over human life and wellbeing.
Let's break it down:
FACT: Psychiatric Drugs are Dangerous
Volumes of solid scientific evidence demonstrate that SSRIs carry serious and sometimes deadly side effects. These adverse effects include akathisia (a condition in which a person feels compelled to move about), permanent neurological damage, bone fracture, birth defects, sexual dysfunction, suicide (especially in children and teenagers) and acts of violence.[1-5] Shockingly, evidence indicates that SSRI use in patients can, in fact, exacerbate and lengthen bouts of depression and significantly promote relapse.[6]
Most alarming has been the relationship between suicides and psychiatric drug use. The year 2021 saw suicide among military personnel reach an all time high. Since 911, the number of active duty and veteran suicides is over four times greater than actual combat causalities. In other words, more active-duty American soldiers are ending their own lives than are dying in battle. Could it be that the rising rates of suicide among members of the US military are being fueled by SSRIs and other psychiatric medications? A body of research suggests that the answer is yes.
A meta-analysis appearing in the British Medical Journal, which pooled data from more than 700 studies and 87,650 patients, found that that there exists an "association between the use of SSRIs and increased risk of fatal and non-fatal suicide attempts" The researchers stated in their conclusion that methodological limitations may have caused them to actually underestimate the real risk of suicide.[7]
In 2004, the FDA required SSRI manufactures to place a black box label on SSRI drugs stating suicide as a lethal side effect. How many more deaths have to occur before the FDA bans these dangerous medications altogether?
FACT: Psychiatric Drugs are NOT Effective
Back in 1967, a British psychiatrist proposed the Chemical Imbalance Theory, which established a template for future research to search for mental disorders in chemical imbalances that may be observed in the brain. It is also the underlying basis for the belief that the neurotransmitter serotonin is responsible for what has become the Serotonin Theory of Depression. However, a large state of the art “umbrella review evaluation” conducted by a consortium of eight universities investigated the relationship between serotonin and depression and found that there is no convincing evidence to make this claim. Furthermore, many studies show that SSRIs are generally no more effective than a placebo (sugar pill) for treating depression. The authors of one meta-analysis examining the effectiveness of using SSRIs in patients with depression remarked that:
"These findings suggest that, compared with placebo, the new-generation antidepressants do not produce clinically significant improvements in depression in patients who initially have moderate or even very severe depression, but show significant effects only in the most severely depressed patients"[8]
Upon closer investigation, it's little wonder that these drugs aren't efficacious. Psychiatric authorities still contend that mental illness has its roots in "chemical imbalances" in the brain that may be mediated through pharmaceuticals. The only problem is that there is no compelling evidence to confirm this hypothesis. To the contrary, there is increasing evidence to debunk the chemical imbalance theory altogether. Furthermore, studies prove that SSRIs can adversely interfere and disturb normal brain function; SSRIs ultimately reduce the brain's ability to respond to serotonin.[9] This is a possible reason that many individuals on SSRIs are more likely to suffer from depression for longer periods of time, and relapse more frequently.
FACT: Psychiatric Diagnoses Have No Basis in Science
The American Psychiatric Association's Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is the definitive guide for psychiatric diagnoses. Of the nearly 300 mental disorders outlined in the DSM-5, the criteria for determining mental illness are based solely on subjectively measured and described behaviors. There are no blood tests, no brain scans or urine samples- not one biological marker to validate the existence of these so-called conditions.
The flawed nature of conventional mental health diagnoses has been pointed out for years. In a 2010 opinion piece for the Los Angeles Times, Allen Frances, chairman of the taskforce that created the DSM-4, commented on the absurdity of the ever-expanding pool of mental disorders stating the following:
“The first draft of the next edition of the DSM, posted for comment with much fanfare last month, is filled with suggestions that would multiply our mistakes and extend the reach of psychiatry dramatically deeper into the ever-shrinking domain of the normal. This wholesale medical imperialization of normality could potentially create tens of millions of innocent bystanders who would be mislabeled as having a mental disorder. The pharmaceutical industry would have a field day -- despite the lack of solid evidence of any effective treatments for these newly proposed diagnoses.”
Even more damning was a deathbed confession in 2009 by the eminent child psychiatrist, Dr. Leon Eisenberg. In his final interview, Eisenberg reportedly revealed that "ADHD is a prime example of a fictitious disease." The bombshell came at the end of Eisenberg's long career developing foundational theories in modern psychiatry that led to the creation of ADHD and other mental disorders.
Given the lack of scientific rigor with which the APA concocts new disorders, it shouldn't come as a surprise that the DMS-5 even outlines "internet gaming disorder" as a brain abnormality that warrants further study. The bottom line is that psychiatry's DSM handbook has as much credibility as a comic book.
FACT: The Psychiatric Establishment is Bought and Paid for by Big Pharma
Like the other branches of the medical-industrial complex, psychiatry is infested with conflicts of interest. One of the most outspoken critics of the pharmaceutical industry's extensive influence over modern medicine is Dr. Marcia Angell, the former editor-in-chief of the New England Journal of Medicine who is currently on the faculty at Harvard University’s School of Public Health.
In her New York Book Review article, Dr. Angell recounts the systemic corruption that has plagued the field of psychiatry:
“As psychiatry became a drug-intensive specialty, the pharmaceutical industry was quick to see the advantages of forming an alliance with the psychiatric profession. Drug companies began to lavish attention and largesse on psychiatrists, both individually and collectively, directly and indirectly. They showered gifts and free samples on practicing psychiatrists, hired them as consultants and speakers, bought them meals, helped pay for them to attend conferences, and supplied them with "educational" materials. When Minnesota and Vermont implemented "sunshine laws" that require drug companies to report all payments to doctors, psychiatrists were found to receive more money than physicians in any other specialty. The pharmaceutical industry also subsidizes meetings of the APA and other psychiatric conferences. About a fifth of APA funding now comes from drug companies.”
Dr. Angell goes on to describe how pharmaceutical companies manipulate study results to maximize profit streams from their drugs:
“...drug companies make very sure that their positive studies are published in medical journals and doctors know about them, while the negative ones often languish unseen within the FDA, which regards them as proprietary and therefore confidential. This practice greatly biases the medical literature, medical education, and treatment decisions.”
Upon further investigation not only are unfavorable clinical trial results concealed while positive results are highlighted and publicized, but the pharmaceutical industry has been embroiled in scandals involving fabricated study results. In one case, Dr. Scott S Reuben, a Massachusetts anesthesiologist and researcher, allegedly faked data for 21 studies on major medications. Several of the drugs reviewed in Reuben's studies, including Wyeth's antidepressant, Effexor FX, were presented in a favorable light without any supporting clinical evidence.
In our opinion, professional dishonesty is rampant in modernpsychiary. In 2013 The Economist published an article entitled "Unreliable Research: Trouble at the Lab." The paper covered the work of Dr. Daniele Fanelli at the University of Edinburgh, who studied the flaws of scientific research conducted at academic institutions. Dr. Fanelli stated that fraud is likely second to incompetence in generating erroneous results -- although determining the difference is difficult. Dr Fanelli evaluated 21 separate surveys by academics (mostly in the biomedical sciences but also in civil engineering, chemistry and economics) carried out across a 21 year period (1987 to 2008). Only 2% of respondents admitted falsifying or fabricating data, but 28% of respondents claimed to know of colleagues who engaged in questionable research practices.
Collusion and deception have become hallmarks of the medical establishment. Here are some examples of psychiatry's corruption by the pharmaceutical cartel.
Psychologist Lisa Cosgrove and her colleagues examined the conflicts of interest among the panel members tasked with updating the DSM-5 handbook. Her study noted that "69% of the DSM-5 task force members report having ties to the pharmaceutical industry. This represents a relative increase of 21% over the proportion of DSM-IV task force members with such ties (57% of DSM-IV task force members had ties)."[10]
Cosgrove points out that panel members are eligible to help edit the DSM as long as they are not paid more than $10,000 from drug companies per year (through consultancies and other jobs). In addition, members are permitted to own up to $50,000 in stock holdings in pharmaceutical firms and still serve in their position.
Moreover, the American Psychiatric Association meets in secret to develop the DSM. All of the task force members are required to sign non-disclosure agreements. This practice has been assailed by many, even former DSM chairman Robert Spitzer, who stated in an interview that "When I first heard about this agreement, I just went bonkers...transparency is necessary if the document is to have credibility."[11]
Groups such as the National Alliance on Mental Illness (NAMI) and the Anxiety and Depression Association of America (ADAA), which were allegedly founded to advocate on behalf of people with mental disorders, have been challenged for operating as front groups created to push the pharmaceutical industry’s profit-driven agenda.
In the 1970s and 1980s, leaders at the National Institute of Mental Health played a key role in helping found these professional organizations, such as NAMI, in order to enable drug companies to effectively lobby lawmakers in Washington and state capitols to fund more psychiatric research. These organizations have enjoyed a steady stream of generous financial support from drug makers for decades.
Psychiatrist Dr. Peter Breggin has alleged that NAMI is the “astroturf lobbying organization… for the psychopharmaceutical complex.” The organization controls 70 percent of the mainstream media’s messaging about mental health and psychological disorders. Its corporate sponsors are a Who’s Who of the nation’s largest firms in the drug and chemical industries, Wall Street banks, the most influential Silicon Valley companies and the major media networks. It dominates social media, with over 160 million impressions, to advance psychiatry’s drug-based model for dealing with mental illness. In a single year NAMI spent $3.5 million to grab state organizations to advocate on its behalf through its many hundreds of local chapters in every US state. And in 2021, NAMI’s annual report called for $2.1 billion of additional funding to advance its influence over state psychiatric organizations and the media. It is currently in a collaboration with Google to embark on an initiative that would flag internet searchers for psychological related disorders, such as anxiety, depression, obsessive compulsion, etc, thereby incorporating a vehicle for the psychiatric and drug industry to identify and reach out to internet users who may suffer from these mental afflictions. Very likely, this initiative will generate algorithms for pharmaceutical ads targeting the specific searches people make.
Given the overwhelming evidence implicating modern psychiatry as a sick and twisted farce designed to profit from human suffering, how could it be that this issue doesn't receive any substantive media coverage? Why hasn't this been exposed by The New York Times, CNN and MSNBC, or 60 Minutes? Could it be the hundreds of millions of dollars in advertising that the corporate media receives from Big Pharma each year? Perhaps this could lead to self-censorship.
The Dangers of SSRIs
We need to take a deeper look at the dangers associated with SSRIs. The most controversial issue surrounding the use of SSRIs--a possible connection to suicidal and homicidal thoughts and behavior in some users--made news in mid-2003 when the Food and Drug Administration recommended that Paxil not be used to treat depressed children and adolescents because regulators were reviewing reports from clinical trials of an increased risk of suicidal thinking and suicide attempts in young users.[12]
Although the Prozac era has ended for Eli Lilly, the availability of less costly generics means that fluoxetine may be more affordable for tens of millions of uninsured people. In addition to gaining approval for Prozac for indications besides depression (obsessive-compulsive disorder, bulimia nervosa, and panic disorder), Eli Lilly now markets two Prozac-related products that have their own patents: Sarafem is the version of Prozac approved for the treatment of premenstrual dysphoric disorder (PMDD).[13] It was the first prescription drug in the US with this indication. The second drug is Prozac Weekly, intended for the longer-term treatment of depression when symptoms have stabilized.[14]
IQVia (formerly IMS Health) has observed a trend toward "lifestyle indications" for antidepressants.[15] In addition to major depression and OCD, both Paxil and Zoloft are indicated for panic disorder, posttraumatic stress disorder, and social anxiety disorder. Zoloft also is approved for premenstrual dysphoric disorder, while Paxil is approved for generalized anxiety disorder. [16-17] Doctors, for their part, prescribe SSRIs for a wide range of conditions, such as headaches, substance abuse, eating disorders, back pain, impulsivity, upset stomach, irritability, hair pulling, nail biting, premature ejaculation, sexual addictions, and attention deficit disorder.[18]
One growing market for SSRIs and other psychiatric medications is young children and adolescents. This is despite some studies showing that antidepressants are no more effective than placebos in these patients.[19-22] Another study in the Journal of the American Medical Association found that psychotropic medications prescribed to preschoolers has rapidly increased.[23] An analysis of prescription claims among young Medicaid patients in North Carolina found that the use of Ritalin-type stimulants and Prozac-type antidepressants among children rose dramatically and that more were taking both drugs at once. Current figures record that 1 in 5 children have a mental health problem: 43 percent increase in ADHD, 37% rise in teen depression, and 200 percent increase in suicides among adolescents between 10-14 years of age. For 2020, the IQVia patient tracker database records over 6.1 million persons between 0-17 years of age on some type of psychiatric medication. Breaking down this statistic, 2.1 million are antidepressants, 3.1 million are taking anti-ADHD drugs such as Adderall, and another 1.2 million are on anti-anxiety drugs. Writing about the increase in psychiatric drugs prescribed for younger people, Jerry Rushton, MD, MPH, commented, "... the consistent increase in SSRI use and in dual prescriptions is especially surprising. We need further information about whether this is due to new unrecognized mental disorders, substitution for other therapies, or overprescription."
Serotonin and side effects
Prozac relieves depression by affecting the level of serotonin, a neurotransmitter that connects receptor sites and fires nerve cells. Joseph Glenmullen, MD, a clinical instructor in psychiatry at Harvard Medical School, explains in his book Prozac Backlash that the drug inhibits the reuptake of serotonin--a process in which a cell that releases this chemical messenger reabsorbs any unused portion of it. By blocking the reuptake of this neurotransmitter, Prozac boosts the level of serotonin and prolongs the serotonin signals in the brain.[24]
Dr. Glenmullen points out, however, that neurotransmitters like serotonin, adrenaline, and dopamine are connected by complex circuitry and function interdependently.
Changes in one neurotransmitter can set off changes in another. Thus, the idea that Prozac-type drugs work "selectively" on serotonin is an illusion. When the level of serotonin is artificially increased, the primary reaction in the brain is a drop in dopamine--a powerful secondary effect that was not understood when the new class of serotonin
boosters was introduced. The severe effects of the SSRIs are thought to be caused by the connections between the serotonin and dopamine systems. "Drugs producing a dopamine drop are well known to cause the dangerous side effects that are now appearing with Prozac and the other drugs in its class," Dr. Glenmullen writes. His term for these compensatory reactions in the brain is "Prozac backlash."[25]
Dr. Peter Breggin has also reported in Talking Back to Prozac: What Doctors Aren't Telling You About Today's Most Controversial Drug, that Prozac acts as a stimulant to the nervous system.[26] Therefore, it can produce side effects that mimic those of amphetamines and are exaggerations of the desired effects of Prozac in relieving depression.
According to Dr. Breggin, the FDA psychiatrist who wrote the agency's safety review of Prozac, the drug's effects--including nausea, insomnia, and nervousness--resemble the profile of a stimulant drug rather than a sedative. He notes that nearly all of the Prozac side effects listed in the Physician's Desk Reference "fit into the stimulant profile." Among others, these stimulant symptoms include headaches, nervousness, insomnia, anxiety, agitation, tremors, weight loss, nausea, diarrhea, mouth dryness, anorexia, and excessive sweating. He adds in The Antidepressant Fact Book that all of the SSRIs can cause insomnia, anxiety, agitation, and nervousness. These same effects and others are caused by the classic stimulants--methylphenidate, amphetamine, methamphetamine, Ecstasy, and cocaine. [27]
A drug that acts as a stimulant can also overstimulate the body systems. In Talking Back to Prozac, Dr. Breggin offers the example of a person who takes Prozac to relieve depression (the beneficial effect) and suffers from agitation and insomnia (the negative effects). These adverse reactions "are inherent in the stimulant effect that produces feelings of energy and well-being," he writes. "In this sense, the difference between 'therapeutic effects' and 'toxic effects' are merely steps along a continuum from mild to extreme toxicity."[28]
Between 2004 and 2019, the FDA’s Adverse Events Reporting System or FAERS reported over 7.3 million adverse events for 30 different antidepressants on the market. Across the board, SSRIs were the most responsible; however, one reason may be that SSRIs are more prescribed. It is not unusual for serious adverse effects to surface after a drug hits the market. Only then is a major new warning added to the label or the drug be withdrawn. The FDA informs doctors, but not the public that the approval of a drug does not mean it is safe.
In 2004, the FDA was compelled to issue a black box warning on virtually all antidepressant drugs. Four years later the FDA instituted a black box warning for all second generation antipsychotics due to rising deaths among elderly patients. It is not uncommon for drugs to eventually undergo greater scrutiny after they have been on the market for longer periods of time and drug injuries and deaths increase. It is estimated that there is a 20% chance that problems will arise with any given drug after its approval. One group of researchers stated, "The safety of new agents cannot be known with certainty until a drug has been on the market for many years." Now that pharmaceutical companies have easier access to fast track new drugs off the production line through the FDA’s regulatory review process, there has been a noticeable increase in black box warning for new drugs.
Dr. Glenmullen says that popular psychiatric drugs follow a "10-20-30 year pattern" in revealing their dangerous effects and falling into disfavor: About 10 years after their debut, the earliest signs of problems appear. At 20 years, there is enough data for the problems to be undeniable and a significant number of physicians to voice their concerns. At 20 years (or more), professional organizations and regulators actively work to stop overprescribing of the drug. At this point, drugs have become passé and lose their patent protection, and the manufacturers move on to more profitable drugs "that can be promoted as 'safer' because their hazards are not yet known." [29]
Comparisons of efficacy
SSRIs have no more specific effect on depression than do other antidepressants, including the tricycles and monoamine-oxidase inhibitors (MAOIs), according to Charles Medawar. As he explains in The Antidepressant Web, patients generally respond to antidepressants in about 60% to 70% of cases, while the typical response to placebo is 30% to 35%. Therefore, the popularity of SSRIs is due to the fact that most experts believe they are safer or otherwise more acceptable than the alternatives. And, in fact, promotional messages for SSRIs state three advantages: the drugs produce fewer unwanted side effects, are more acceptable to more patients, and are safer when overdosed.[30]
Despite the safety-related claims made in the medical literature, "the evidence overall does not suggest that SSRIs show any great and decisive safety advantage over alternatives in day to day use," says Medawar. Consider the results of trials comparing SSRI efficacy and safety with that of other antidepressants: "Two independent meta-analyses, each starting with a careful search of the literature to identify all properly controlled trials, have reached broadly similar conclusions--the SSRIs do have the edge on alternatives, but not by much."[31] One analysis of 62 trials found a 49% dropout rate for SSRIs versus a 54% rate for tricyclic antidepressants. A second analysis of 63 trials (16 comparing an SSRI with a nontricyclic) found that 3% fewer people stopped taking an SSRI because of the side effects. [32]
Other reviews also have found that the newer antidepressants are no more or less effective in treating depression than older-generation drugs. In a government study conducted by Dr. Cynthia Mulrow and colleagues, the researchers analyzed more than 300 randomized controlled trials and concluded there were no significant differences in efficacy between newer and older agents or in overall discontinuation rates.[33-34] Fewer people taking SSRIs stopped treatment due to adverse effects than those taking first-generation tricyclics (the rate difference was 4%). More than 80 studies found that newer antidepressants were more effective than placebo in treating major depression in adults. The response rate was 50% for the drugs, versus 32% for a placebo.
A more disturbing conclusion was reached by Dr. Irving Kirsch and colleagues who analyzed data sent to the FDA for approval of the six most commonly prescribed antidepressants over the course of a dozen years (Prozac, Paxil, Zoloft, Effexor, Serzone, and Celexa). Their analysis found that the response to placebo was almost as great as the response to the antidepressants. The mean difference on the Hamilton Rating Scale for Depression was two points, according to a report in Psychiatric Times. The difference was statistically, but not clinically, significant. The article states, "More than half of the clinical trials sponsored by the pharmaceutical companies failed to find significant drug/placebo difference, and there were no advantages to higher doses of antidepressants." The authors add, "The small difference between antidepressant and placebo has been referred to as a 'dirty little secret' by clinical trial researchers ..."[35]
Several recent studies have reported similar results, finding that an SSRI did not differ significantly from placebo in the treatment of depression.[36]
Footnotes:
[1] Koliscak, Lindsey P., and Eugene H. Makela. "Selective serotonin reuptake inhibitor-induced akathisia." Journal of the American Pharmacists Association 49.2 (2009): e28-e38. Print.
[2] Wu, Q., A. F. Bencaz, J. G. Hentz, and M. D. Crowell. "Selective serotonin reuptake inhibitor treatment and risk of fractures: a meta-analysis of cohort and case–control studies." Osteoporosis International 23.1 (2012): 365-375. Print.
[3] Bahrick, Audrey (2008). "Persistence of Sexual Dysfunction Side Effects after Discontinuation of Antidepressant Medications: Emerging Evidence". The Open Psychology Journal 1: 42–50. Retrieved 30 January 2014.
[4] Olfson M, Marcus SC, Shaffer D (August 2006). "Antidepressant drug therapy and suicide in severely depressed children and adults: A case-control study". Archives of General Psychiatry 63 (8): 865–72.
[5] Henry, Chantal, and Jacques Demotes-Mainard. "SSRIs, Suicide and Violent Behavior: Is there a Need for a Better Definition of the Depressive State?." Current Drug Safety 1.1 (2006): 59-62. pubmed.gov. Web. 18 Mar. 2014.
[6] van Weel-Baumgarten, EM, et al. "Treatment of depression related to recurrence: 10-year follow-up in general practice." Journal of Clinical of Pharmacy and Therapeutics 25.1 (2005): 61-6. pubmed.gov. Web. 24 Mar. 2014.
[7] Fergusson , Dean, et al.. "Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials." British Medical Journal 330 (2005): n. pag. BMJ.com. Web. 17 Mar. 2014.
[8] Kirsch, Irving, Brett J. Deacon, Tania B. Huedo-Medina, Alan Scoboria, Thomas J. Moore, and Blair T. Johnson. "Initial Severity And Antidepressant Benefits: A Meta-Analysis Of Data Submitted To The Food And Drug Administration." PLoS Medicine 5.2 (2008): e45. plosmedicine.org. Web. 18 Mar. 2014.
[9] Andrews, Paul W, et al.. "Blue again: perturbational effects of antidepressants suggest monoaminergic homeostasis in major depression ." Fronteirs in Psychology July (2011): n. pag. journal.frontiersin.org. Web. 17 Mar. 2014.
[10] Cosgrove, Lisa, and Sheldon Krimsky. "A Comparison of DSM-IV and DSM-5 Panel Members' Financial Associations with Industry: A Pernicious Problem Persists." PLoS Medicine 9.3 (2012): e1001190. plosmedicine.org. Web. 18 Mar. 2014.
[11] Carey, Benedict. "Psychiatry's Struggle to Revise The Book of Human Troubles." The New York Times. The New York Times, 17 Dec. 2008. Web. 27 Mar. 2014.
[12] U.S. Food and Drug Administration. FDA talk paper: FDA statement regarding the anti-depressant Paxil for pediatric population. June 19, 2003.
[13] U.S. Food and Drug Administration (FDA). New treatment approved for severe premenstrual symptoms. FDA Consumer magazine, Sep-Oct. 2000.
[14] U.S. Food and Drug Administration (FDA). Weekly Prozac dosage: treatment alternative for depression. FDA Consumer magazine, May-June 2001.
[15] IMS Health. Lifestyle indications for antidepressants. April 4, 2000. From www.ims-global.com/insight/news_story/news_story_000404b.htm.
[16] GlaxoSmithKline. Prescribing information for Paxil (paroxetine hydrochloride) Tablets and Oral Suspension. August 2003. From www.us.gsk.com/products/assets/us_paxil.pdf.
[17] Pfizer Inc. Prescribing information for Zoloft (sertraline hydrochloride) Tablets and Oral Concentrate. Revised September 2003. From www.pfizer.com/download/uspi_zoloft.pdf.
[18] Glenmullen, Joseph, M.D. Prozac backlash: overcoming the dangers of Prozac, Zoloft, Paxil, and other antidepressants with safe, effective alternatives. Touchstone, Simon & Schuster, New York, 2000, p. 14.
[19] Leonard M. Children are the hot new market for antidepressants. But is this how to make them feel better? Boston Sunday Globe, May 25, 1997, D1, D5 (cited in Glenmullen).
[20] Strauch B. Use of antidepression medicine for young patients has soared. New York Times, August 10, 1997, 1 (cited in Glenmullen).
[21] Martin A, Leslie D. Trends in psychotropic medication costs for children and adolescents, 1997-2000. Arch Pediatr Adolesc Med 2003 Oct; 157(10):997-1004.
[22] Fisher RL and Fisher S. Antidepressants for children. Is scientific support necessary? J Nerv Ment Dis 1996; 184:99-102 (cited in Glenmullen).
[23] Pellegrino D. Commentary: Clinical judgement, scientific data, and ethics: antidepressant therapy in adolescents and children. J Nerv Ment Dis 1996; 184:106-8 (cited in Glenmullen).
[24] Glenmullen, op. cit., p. 17.
[25] Ibid, pp. 17-20.
[26] Breggin, P.R., and Breggin, G.R. Talking back to Prozac: What doctors aren't telling you about today's most controversial drug. St. Martin's Press, New York, 1994, p. 121.
[27] Breggin, P.R. The antidepressant fact book. Perseus Publishing, Cambridge, MA, 2001, p. 46.
[28] Breggin and Breggin, 1994, p. 105.
[29] Glenmullen, op. cit., pp. 12-13.
[30] Medawar C. The antidepressant web--marketing depression and making medicines work. International Journal of Risk & Safety in Medicine 1997;10(2):75-126. Posted online at a Web site operated by Social Audit Ltd., the publishing arm of Public Interest Research Centre Ltd.: Last updated August 8, 2003.
[31] Anderson IM, Tomenson BM. Treatment discontinuation with selective serotonin reuptake inhibitors compared with tricyclic antidepressants: a meta-analysis. Brit Med J 1995 June 3; 310:1433-8 (cited in Medawar).
[32] Song F, Freemantle N, Sheldon TA, et al. Selective serotonin reuptake inhibitors: meta-analysis of efficacy and acceptability. Brit Med J 1993; 306:683-7 (cited in Medawar).
[33] Mulrow CD, Williams JW Jr, Trivedi M, Chiquette E, Aguilar C, et al. Treatment of depression--newer pharmacotherapies. Psychopharmacol Bull 1998; 34(4):409-795.
[34] Geddes JR, Freemantle N, Mason J, Eccles MP, Boynton J. SSRIs versus other antidepressants for depressive disorder. Cochrane Database Syst Rev 2000; (2):CD001851.
[35] Hollon SD, DeRubeis RJ, Shelton RC, Weiss B. The emperor's new drugs: effect size and moderate effects. Prevention & Treatment, 5 Artical 28, 2002 (cited in Kirsch and Antonuccio).
[36] Hypericum Depression Trial Study Group. Effect of Hypericum perforatum (St John's wort) in major depressive disorder: a randomized controlled trial. JAMA 2002 Apr 10; 287(14):1807-14.
Gary Null’s Show Notes
Survey: 9 in 10 adults have tried losing weight in past 5 years — but 44% gained more than 20 pounds
Nutrisystem, February 24, 2023
No, you’re not crazy and you’re not alone – losing weight continues to be a struggle for many Americans. A poll of 2,000 Americans who have tried to lose weight at any point in their life finds that 95 percent have tried to lose weight within the last five years. However, 44 percent have struggled so much over the past half decade, that they’ve ended up gaining 21 pounds or more.
For the year ahead, 62 percent say they are planning to lose an average of 22 pounds to reach their goals in 2023. Over half (58%), however, recognize their weight loss goal is ambitious. Although 72 percent say losing weight this year is a major priority for them, nearly as many (71%) believe there are a lot of challenges making it difficult for them to lose weight.
Commissioned by Nutrisystem, the study reveals the biggest challenges people face while trying to lose weight, including maintaining willpower (28%), lack of motivation (27%), eating healthy foods (27%), and overcoming hunger (27%). Other major challenges people face include the pure difficulty of losing weight (26%), the expense associated with weight loss (25%), and even finding time to work out (25%).
Many place the blame on distractions in their lives — like health issues (25%), money problems (23%), and social media (19%). Even where people work impacts their eating habits. Out of the 27 percent surveyed who say they work in a hybrid environment (half work-from-home, half in an office or on-location), 69 percent eat more frequently at home than they would at their workplace.
The study also reveals that 73 percent of Americans think losing weight is “great at first,” but then it slows down and plateaus. Similarly, 72 percent claim it “feels like forever” before they see any weight loss results. Even then, the average person can only tell they’ve lost weight after dropping 20 pounds.
The reasons why people choose to lose weight are typically personal. Many want to improve their appearance (43%), feel more confident in themselves (39%), and to address major health concerns (39%). When it comes to discussing their weight loss journey, 44 percent tend to keep the goal to themselves, while 40 percent don’t mind sharing their journey with others.
Fruits, vegetables, 'farm-to-fork continuum' vital to cancer prevention
Penn State University, February 19, 2023
After decades of research aimed at improving the yield, appearance and safety of fruits, vegetables and grains, it's time to focus science on the health benefits those foods can provide, according to a cancer researcher in Penn State's College of Agricultural Sciences.
But concentrating on the foods' potential alone won't adequately assess their cancer-fighting properties, noted Jairam Vanamala, associate professor of food science. Instead, he contends that researchers must consider the effect of how foods are harvested, handled, stored and prepared to aid the development of new and science-based strategies for cancer prevention.
The influence of that "farm-to-fork continuum" on the bioactive compounds in fruits, vegetables and grains is critical and has largely gone unstudied, he believes.
Vanamala pointed out that new cancer cases are expected to surge 57 percent worldwide in the next two decades. With most cancers containing numerous genetic alterations and the dysregulation of multiple critical cellular-signaling pathways, he doesn't expect a "silver bullet" treatment effective against most cancers to emerge.
"Instead, research should shift toward developing prevention strategies for cancer. Accumulating evidence suggests that a diet high in plant-based foods is preventive of a variety of chronic diseases, including cancer," he said. "A plethora of bioactive compounds—such as polyphenols, glucosinolates and carotenoids in fruits, vegetables, grains and legumes—are shown to suppress a variety of biological capabilities required for tumor growth."
"Many practices in the farm-to-fork continuum, including preharvest methods, postharvest storage and processing, and consumer practices, affect a food's bioactive compound content, composition and chemopreventive bioactivity," Vanamala explained. "Food system practices may be adjusted to improve the bioactive compound profile, elevating the cancer-fighting properties of fruits, vegetables and other food products."
For example, Vanamala said, recent studies reported that two types of bioactive compounds—polyphenols and isothiocyanates—possess cancer preventive/protective activity. "These two compounds are present in many whole foods, such as grapes, broccoli and others. However, no studies have been conducted on using farm-to-fork-function continuum on whole foods anti-cancer activity even though pre- and postharvest practices were shown to alter the content and composition of bioactive compounds."
Ramping up the amount of bioactive, cancer-fighting compounds in foods via the farm-to-fork continuum is especially critical because the number of servings of fruits increased by only 0.3 and vegetables by only 0.8 per capita during the last 30 years. Given the ineffectiveness of public healthcampaigns to increase fruit and vegetable consumption, Vanamala said, selection of cultivars with greater bioactive compound content may be a more effective means of improving the overall health of the population.
But consumer selection has the greatest impact on overall dietary intake of bioactive compounds. Though crop biodiversity has decreased, consumers still have the ability to choose foods with more bioactive compounds in many situations.
"Choosing red onions, purple-fleshed potatoes, or even blue corn chips instead of their respective white alternatives could lead to increased bioactive compound intakes," Vanamala said.
"By selecting a wide variety of whole foods—consuming a rainbow of foods—consumers can maximize the health benefits gained from fruit and vegetable bioactive compounds."
Exercise more effective than medicines to manage mental health, says study
University of South Australia, February 24, 2023
University of South Australia researchers are calling for exercise to be a mainstay approach for managing depression as a new study shows that physical activity is 1.5 times more effective than counseling or the leading medications.
Published in the British Journal of Sports Medicine, the review is the most comprehensive to date, encompassing 97 reviews, 1,039 trials and 128,119 participants. It shows that physical activity is extremely beneficial for improving symptoms of depression, anxiety, and distress.
Specifically, the review showed that exercisevinterventions that were 12 weeks or shorter were most effective at reducing mental health symptoms, highlighting the speed at which physical activity can make a change.
Lead researcher, Dr. Ben Singh, says physical activity must be prioritized to better manage the growing cases of mental health conditions.
"Physical activity is known to help improve mental health. Yet despite the evidence, it has not been widely adopted as a first-choice treatment," Dr. Singh says. "Our review shows that physical activity interventions can significantly reduce symptoms of depression and anxiety in all clinical populations, with some groups showing even greater signs of improvement.
"Higher intensity exercise had greater improvements for depression and anxiety, while longer durations had smaller effects when compared to short and mid-duration bursts.
"We also found that all types of physical activity and exercise were beneficial, including aerobic exercise such as walking, resistance training, Pilates, and yoga.
"Importantly, the research shows that it doesn't take much for exercise to make a positive change to your mental health."
Senior researcher, UniSA's Prof Carol Maher, says the study is the first to evaluate the effects of all types of physical activity on depression, anxiety, and psychological distress in all adult populations.
Recipe for Spaghetti and Shiitake Saffron Tomato Sauce
Share
About Gary Null
An internationally renowned expert in the field of health and nutrition, Gary Null, Ph.D is the author of over 70 best-selling books on healthy living and the director of over 100 critically acclaimed full-feature documentary films on natural health, self-empowerment and the environment. He is the host of ‘The Progressive Commentary Hour” and “The Gary Null Show”, the country’s longest running nationally syndicated health radio talk show which can be heard daily on here on the Progressive Radio Network.
Throughout his career, Gary Null has made hundreds of radio and television broadcasts throughout the country as an environmentalist, consumer advocate, investigative reporter and nutrition educator. More than 28 different Gary Null television specials have appeared on PBS stations throughout the nation, inspiring and motivating millions of viewers. He originated and completed more than one hundred major investigations on health issues resulting in the use of material by 20/20 and 60 Minutes. Dr. Null started this network to provide his followers with a media outlet for health and advocacy. For more of Dr. Null’s Work visit the Gary Null’s Work Section or Blog.GaryNull.com In addition to the Progressive Radio Network, Dr. Null has a full line of all-natural home and healthcare products that can be purchased at his Online Store.
As a paying subscriber you receive a 20% discount on Gary's vitamins and other products. Make your selection at Gary's Vitamin Closet: https://www.garysvitamincloset.com and call 646-926-5430 and tell the operator you are a subscriber.
Find articles, videos, back radio broadcasts, books, and more at GaryNull.com.
https://garynull.com
Hear Gary's radio show weekdays at noon Eastern Time on PRN.live
Disclaimer
While we have thoroughly researched the information we provide, and indicate its sources, information in this Gary Null Newsletter, and all Gary Null Newsletters, is for educational and informational purposes only, and is not intended to diagnose, treat, cure or prevent any disease or other condition. Consult your medical professional before choosing any treatment or course of action. Gary Null Newsletters are not liable for risks or issues associated with using or acting upon the information it provides.
Let us know what you would like to see in Gary's newsletter. Email us at [email protected]
If you are not subscribed, go to: https://garynull.substack.com to subscribe.
0 notes
Text

#it’s actually zoloft but that’s not important#meme#bts meme#bts proof#proof#bts yet to come#yet to come#yet to come (the most beautiful moment)#bts yet to come (the most beautiful moment)#i did a mock faint and hit my head on the back of the couch#i can’t really breathe rn but this is more unprintable#impirtant#whatever#jungkook#taehyung#v#jimin#jin#hobi#yoongi#joon#namjoon#rm#jhope#suga#bts funny#funny
2 notes
·
View notes
Note
I hope your brain is nicer to you until you get your meds!
THANK YOU!! Rn it just feels like I’m severely jetlagged and transcending this mortal plane but it should get better on Tuesday and be SUPER better within a month or so

#the Zoloft is supposed to help me make decisions and actually focus on more important tasks instead of hyperfixating#little scared about it because I’ve been hyperfixating as a self-comfort from my current stressors
5 notes
·
View notes
Text
The pharmacy still doesn’t have my antidepressants, so I’ve just been nauseas and achey lately. I’ve never had meds that took anywhere near this long to get refilled. I’m now getting a bit worried that by the time they arrive, I’ll have to readjust to actually having them in my body. How stupid would it be to just not take them anymore, even if the refills arrived? Probably pretty stupid. Blegh
Also, I beat Prey the other night and now I’ve got the big “now what?”
#this isn’t important#dang Prey was so good#i honestly havent sat down and actually finished a game in years so i’m pretty psyched on myself#feel a bit let down bc i wanted to see the end so bad that i basically did a speed run at the end to finish as fast as possible#i was so OP by the end i could just run through everything and nothing scared me#gonna do new game+ once i’ve played some other stuff for awhile#anyway... oh yeah im out of brain meds#it’s... whatever#i feel sick and out of it and i’ve just been eating junk and sleeping bc of it#i guess maybe that’s what i get for not taking a more name brand antidepressant#they always seem to be out#sorry i’m not cool enough for zoloft!#oh well#you can ignore this#text
2 notes
·
View notes