#Central Nervous System (CNS) Depressants
Note
i was wondering if you could give some points and tips on writing about a character who is suffering from DRUG ABUSE
Writing A Drug Addict Character
Know Your Drugs
Was the drug invented? A scene using insulin set in 1820 is problematic since this treatment wasn’t discovered until the 1900s. Fentanyl shouldn’t be used in a 1930s scene since it wasn’t available for use until the 1960s—opium or morphine would be more accurate choices.
Was the method invented? Since insulin must be given as a shot, that scene is even less authentic as the hypodermic needle wasn’t invented until the mid-1800s. Older historical fiction could involve the use of poultices and mustard packs, while skin drug patches (transdermal patches) are only appropriate in more modern scenes.
The most common drugs abused by gangs are: Marijuana, Methamphetamine, Heroin, Cocaine
Or, it can be prescription drugs
Although many medications can be abused, the following three classes are most commonly abused:
Opioids—usually prescribed to treat pain;
Central nervous system (CNS) depressants—used to treat anxiety and sleep disorders; and
Stimulants—most often prescribed to treat attention deficit hyperactivity disorder (ADHD). (common example? caffeine)
Write In Stages
Stage 1: First Use
Some people use a substance for the first time out of curiosity, while others use substances due to peer pressure. People may also be prescribed medication, such as opioids, by their doctor. Individuals may view their first use as a one-time occurrence, but this opens the door for future use. Some people try a substance one time and never use it again.
You character will feel:
Angry and/or desperate
Miserable
Lonely
Trying to run away from a certain problem
Persuaded into doing drug
Guilty
Stage 2: Regular Use
If a person uses a substance and enjoys how it makes them feel or believes it will improve their life, they may start to use the substance regularly. They may use drugs or drink alcohol on the weekends while at parties or hanging out with friends. Occasional use may become a regular occurrence. It might become a part of a person’s routine.
Your character:
Will start getting in careless activities while doing drugs
Will probably be violent
Won’t think he has any issue whatsoever and shrug it off
Start associating themselves with harder drug users
Have a false sense of security that they’re able to quit whenever they want.
Stage 3: Risky Use
The next stage after regular use is risky use. A person will continue to use a substance despite the physical, mental, legal or social consequences. Their use likely started as a way to escape or have fun with peers but has now taken priority over other aspects of their life.
Your Character will feel:
uncomfortable around family members/friends who start to notice
Exhibit more reckless behavior
Driving under influence, stealing money to finance substance use, etc.
Underperforming at work or school
Experience tension in personal relationships
Stage 4: Dependence
The next stage is a physical, mental and emotional reliance on the substance. The individual is no longer using the substance for medical or recreational purposes. When a person doesn’t use the substance, their body will exhibit withdrawal symptoms, such as tremors, headaches, nausea, anxiety and muscle cramps.
Your Chracter Will:
Develop a sort of rountine/typical place where they abuse
Believe that the substance is essential for survival
Use substance even when it's unnecessary
Stage 5: Substance Use Disorder
While some people use dependency and substance use disorder interchangeably, they’re very different. Once a person develops a substance use disorder, substance misuse becomes a compulsion rather than a conscious choice. They’ll also experience severe physical and mental side effects, depending on the substance they’re using.
Your Character:
Has noe developed a chronic disease with the risk of relapse
Is now incapable of quitting on their own
Feel like life is impossible to deal with without the substance.
Lose their job, fail out of school, become isolated from friends and family or give up their passions or hobbies.
Research the Trends
Medical knowledge changes over time and with it the drugs prescribed. This then impacts the type of prescription drugs available on the streets.
late 1800s: chloral hydrate used for anxiety and insomnia > bromides > 1920s: barbiturates, barbital > benzodiazepines ("benzos") > early 2000s: opiod drugs > opiod drug bans led to growth of black markets: ilicit fentanyl > and so on...
Different countries/locations will have varying trends of drug abuse (depending on laws, availability, costs, etc.)
Research the Slag
look for "[drug name] trip report" on YouTube, etc. to get first-hand accounts of how drug addicts behave.
The main focus should always be to use the words your characters would use in ways that suit the world you have created.
The slang for certain drugs is a difficult vocabulary to maintain as it is ever-changing and varies based on country, region, town, even by streets. Some writers use what they know or have heard locally, others invent their own.
Resources
FDA (Food and Drug Administration) and DEA online databases and drug resources
Social networking groups focusing on related specialty writing topics, such as trauma or emergency medicine
Newspaper articles and medical journals are great places to find real cases.
The US national poison center
Helpful Vocab:
Addled - sense of confusion + complete lack of mental awareness
Crazed - emotional anguish experienced by the addict
Desperate
Despondent
Erratic
Fidgety
Hopeless
Impressionable
Struggling
#writing#writers and poets#creative writers#helping writers#creative writing#let's write#poets and writers#writers on tumblr#writeblr#resources for writers#writing inspiration#writing advice#writing prompt#writing tips#on writing#writer#writing community#writerscommunity#writer on tumblr#writer things#writer problems#writer community#writer stuff#writblr#writers of tumblr#writers community#writers block#writers life#writing questions#writing quotes
142 notes
·
View notes
Text
Delving Deeper into Neuron Anatomy and Brain Functionality (Part 2)
Welcome back, Tumblr enthusiasts! In Part 1, we took our first steps into the neuron and brain universe. Now, let's journey further into their astonishing anatomy and intricate physiology. 🌌💡
Now that we've dived even deeper into the neuron's inner workings and explored more brain regions, I hope you're as captivated as I am by the wonders of neuroscience. Continue to feed your curiosity and stay tuned for more brainy adventures! 🧠
Neuron Anatomy (Continued)
Myelin Sheath: Wrapped around many axons, this fatty insulating layer is like the neuron's protective armor. It speeds up the transmission of electrical signals by allowing them to "jump" from one gap in the myelin sheath, called the Nodes of Ranvier, to the next. Think of it as a high-speed neural highway.
Schwann Cells and Oligodendrocytes: These specialized cells produce the myelin sheath. In the peripheral nervous system (PNS), Schwann cells individually wrap around axons. In the central nervous system (CNS), oligodendrocytes extend processes to multiple axons, forming myelin sheaths around them.
Sensory and Motor Neurons: Neurons aren't one-size-fits-all; they come in different shapes and sizes. Sensory neurons (afferent) bring sensory information from your body and surroundings to your brain and spinal cord. Motor neurons (efferent) carry commands from the brain and spinal cord to muscles and glands, allowing you to move and react.
Neuron Physiology (Continued)
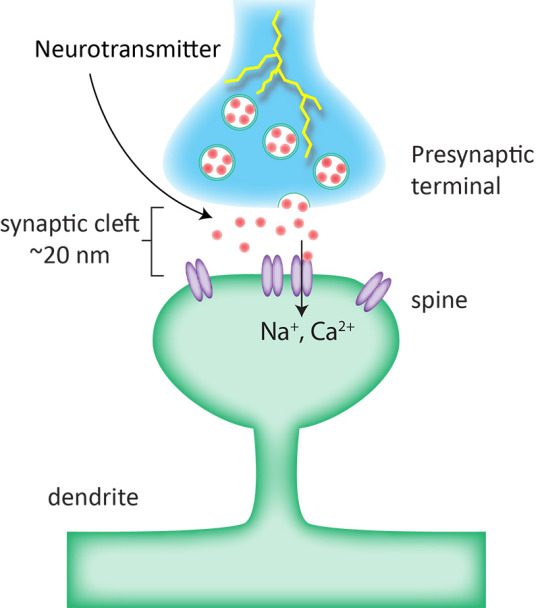
Neurotransmitters: These chemical messengers are the key to communication between neurons. When an action potential reaches the axon terminals, it triggers the release of neurotransmitters into the synapse. These molecules bind to receptors on the neighboring neuron, initiating or inhibiting a new electrical signal, depending on the neurotransmitter type.
Synaptic Plasticity: Neurons can change the strength of their connections through a phenomenon called synaptic plasticity. This allows us to adapt and learn. Two important types include long-term potentiation (LTP), which strengthens synapses, and long-term depression (LTD), which weakens them.
Brain Functionality (Continued)
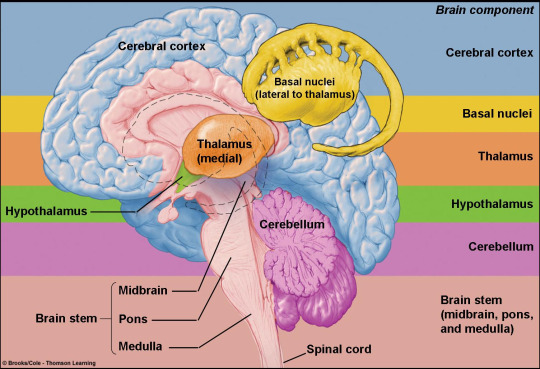
Thalamus: Often called the "relay station," the thalamus acts as a switchboard, directing sensory information (except for smell) to the appropriate regions of the cerebral cortex for further processing.
Hypothalamus: This small but mighty structure regulates many essential functions, including hunger, thirst, body temperature, and the body's internal clock (circadian rhythms).
Frontal Cortex: Located in the frontal lobes of the cerebral cortex, this region is responsible for higher cognitive functions like decision-making, planning, reasoning, and personality.
Temporal Lobes: These are crucial for auditory processing and memory. The hippocampus, nestled deep within the temporal lobes, is essential for forming new memories.
References
Purves, D., et al. (2017). "Neuroscience." Sinauer Associates, Inc.
Kandel, E. R., Schwartz, J. H., & Jessell, T. M. (2012). "Principles of Neural Science." McGraw-Hill Education.
#science#biology#college#education#school#student#medicine#doctors#health#healthcare#neuroscience#neurobiology#neurons#neurology#brains#nursing#higher education
77 notes
·
View notes
Text
Roofie
The colloquial name of the drug Rohypnol (flunitrazepam). It's a central nervous system depressant from the benzodiazepine family. Its medical uses are related to inducing sleep, combating anxiety and relaxing muscles. However, it is notorious for being used as a recreational drug due to also causing side effects of relaxation, disinhibition, increased sociability, euphoria and feelings of being high.
Its most infamous use, however, is its use as a date rape drug. In higher quantities it reduces reaction time, impairs physical and cognitive abilities, and can be known to induce amnesia.
It is colourless, scentless and odourless. It can be snorted, swallowed or dissolved. It typically comes in tablet form.
When cosumed with alcohol, other drugs or other CNS depressants, it can cause an increase of side-effects: more dinsinhibition, higher excitability and sociability... But it can also cause more dangerous side-effects such as slurred speech, loss of coordination, weakness, headache and respiratory depression.
In case of overdose, it can cause unconsciousness, coma, slowed cardiac rhythm and death. Overdose is more frequent and easy when consumed with alcohol, other drugs, or CNS depressants.
This prompt is related to any use of Rohypnol (or similar drugs like GHB) causing death. Used willingly or otherwise, recreationally, accidental consumption, overdose, impaired decision making leading to death, allergic reaction... As long as Rohypnol is involved, the prompt works.
#killacharacter#killacharacterbingo#writing challenge#bingo challenge#writing event#whump#writing bingo#whumpee#bingo card#whump prompt
11 notes
·
View notes
Note
dear dr. on mandated leave,
have you ever been in the room for an alcohol detox? is anaesthesia used to smooth out hardcore withdrawal symptoms, or just sedatives, or am i confusing which is which? basically, any thoughts alcohol use, alcohol withdrawal, AUD, & anaesthesia
hi! this will be a long one but thank you for the interesting question! i'm not an addiction specialist nor critical care specialist but this is what i know.
so, first of all, you are right in saying that sedatives are part of anaesthesia. there are several different types of anaesthesia that can be used combined or as individual treatments. in no particular order, there's general, local, regional, neuraxial, and sedation, each with different indications and goals.
AWS is part of critical care medicine (or intensive care) which is a sort of sub-specialty that requires prior training in anaesthesia, emergency, paediatrics or primary medicine, and there are further subcategories to critical care. some countries also have addiction specialists as a separate subcategory.
now, general anaesthesia (GA) masks the onset of AWS. approximately 1 in 5 patients in for surgery have an alcohol use disorder (AUD), for emergency surgery or aerodigestive oncology surgery this is about 50% if i'm remembering correctly. a side effect of general anaesthesia is emergence delirium (ED*), there are different forms of ED but a risk factor for ED is AUD. patients with AUD are also at higher risk of other surgical complications. this is just a bit of a side note.
AWS can range from mild to severe, sometimes it can be fatal. it is seen after a reduction in alcohol intake after a period of excessive use as chronic use of alcohol changes the brain chemistry, especially changes to the GABAergic system. the GABAergic system is the primary inhibitory neurotransmitter for the central nervous system (CNS); alcohol is a CNS depressant.
a short explanation of this is that episodic intoxication causes excessive production of GABA which has a sedative effect. chronic alcohol use changes the balance of the inhibitory signals and excitatory (glutamate) signals of the CNS, basically the body adjusts to the influx of GABA by over-producing glutamate. once a patient who chronically drinks alcohol stops or reduces the amount, the GABA signals are diminished and the excess glutamate causes AWS.
a lot of the drugs used in anaesthesia are GABA receptor agonists, the treatment of an overdose is a GABA receptor antagonist, which have a stimulant or convulsant effect. for example, propofol is a really common GABA receptor agonist in general anaesthesia.
so, you can imagine that in the acute phase of AWS, management of a patient's neurochemistry is crucial and this is managed with medication.
management of the signs and symptoms of AWS are generally:
a quiet room with minimal stimulation and low lighting.
fluid and electrolyte balance.
early sedation to manage acute symptoms and prevent injury.
nutrition management.
airway management in heavily sedated patients.
psychiatric treatment.
medication, especially benzodiazipines and anticonvulsants.
basically, a person experiencing AWS will likely be sedated early on and will require monitoring to prevent aspiration (entry of foreign materials into the airway and lungs). we have to be very careful what drugs we give and how much we give so that we don't mask the symptoms or over-sedate, propofol has been given in some cases but as mentioned above, GA masks the onset and patients have been observed coming out of GA with the same withdrawal symptoms they went under with.
there are different levels of sedation and as i don't manage this, i'm not too sure what level they would use as a standard but i would imagine that it would depend on the patient as i know some are deeply sedated.
typical monitoring devices** you will see under sedation:
3-lead ECG or 5-lead depending on cardiac history and concern. a 12-lead ECG is purely diagnostic so unless a cardiac event has taken place or is suspected to have taken place, it will not be used.
pulse oximetry.
IV access for fluid and electrolyte balance.
blood pressure, either non-invasively (cuff) or invasively (arterial line). typically it depends on the severity but generally we aim for non-invasive, cycling every 5 minutes if possible. an arterial line would more than likely not be used.
capnography which monitors the ETCO2 of a patient, this is end-tidal carbon dioxide so it's telling us how much is being exhaled. i could make a whole post on capnography alone, it's extremely valuable. capnography is measured with a gas analyser attached to the monitor and to the respiratory filter, it looks like a clear, thin tube.
my closing thoughts and footnotes are below the cut.
AUD and AWS need to be treated with compassion and sympathy as much as being treated medically. i have profound sympathy for people struggling with addiction, it's an incredibly difficult thing to manage alone and it is so important to be somebody that the patient can trust and find comfort in.
we see a lot of shame in people struggling with addiction and it is incredibly difficult to seek help, people are often deterred because they think their healthcare provider will judge them which, unfortunately in some cases, is true. i think a really important part of this branch of medicine is breaking the stigma that surrounds addiction.
i have had patients confide in me because i go out of my way to make sure they can feel comfortable talking to me, from there i ask if they would like me to put them in contact with support services. i offer to call a psychiatrist in, and i listen. i listen to them talk about the heavy stuff, i listen to them talk about the light stuff, i listen to everything.
as one of my old teachers said:
"listening is a valuable tool in medicine. let your patients talk to you, let them rant, let them cry, let them shed some of that burden. you might be the first person that's listened to them in a long time."
*this is why it is so important to be aware of what medical terminology we are using and who we are using it with. ED to me is emergence delirium but to most others it's probably erectile dysfunction. PND generally is post-natal depression, to me it is perioperative neurocognitive disorders.
**i tried to find some good pictures of anaesthetic monitors so that i could label the different values and waveforms but they all looked ugly or had watermarks and it would also make this page way too long.
2 notes
·
View notes
Text
I have been looking up fibromyalgia for over a year, since the first time I got diagnosed with it, and in all of my research I never saw it put so plainly: it is a disorder of the Central Nervous System. No FUCKING wonder anxiety features as such a symptom. My Actual Nervous System is constantly and far too easily overstimulated. I had no idea doctors had a coherent idea of what fibro is. NEITHER of my rheumatologists said shit about my nervous system, and I was led to believe that the CNS depressant they gave me was less "actual fibro treatment" and more "off-label shot in the dark, let us know if it works" (because it's a seizure medication and it IS off-label).
Goddamn. No fucking wonder. I literally have "physical anxiety at any given moment" disorder. I have been fighting doctors for years saying "yes I have anxiety but it is coming from inside the house and it has very specific triggers that again come from INSIDE THE BODY. Anxiety isn't making my body fall apart, my body is falling apart and causing anxiety. Stop treating it like it's general anxiety about the world and find out what inside of me is causing it physically."
I am still deeply skeptical of being given a diagnosis of exclusion with no tests to exclude anything, but now I feel like at least maybe they weren't entirely full of shit going off a list of diffuse symptoms.
#head in my hands what the fuck I had no idea it was actually understood on some level#I've heard about fibro my whole life as 'that disease enough women have that it's probably at least a little real'#not as an actual recognized thing with a mechanism by which to treat it#chronic-les
13 notes
·
View notes
Note
Howdy, do u have any information on types of drugs used by SRA and RA?
It would depend on the groups/individuals' access to the drug as well as their financial ability to pay for the drug.
Drugs can be categorised by the way they affect the body.
Depressants – slow down the function of the central nervous system
Hallucinogens – affect one's senses and changes the way they see, hear, taste, smell or feel things
Stimulants – speed up the function of the central nervous system.
The drug categories can be broken down further:
Stimulants
Inhalants
Depressants
Opioids
Steroids
Hallucinogens
Prescription drugs
Then the type of drug. For example some stimulants are;
Cocaine
Methamphetamines
Amphetamines
Ritalin
Cylert
Drugs from each of these categories can affect a person's central nervous system and impair a person's normal faculties.
(1) Central Nervous System (CNS) Depressants
CNS depressants slow down the operations of the brain and the body. Examples of CNS depressants include alcohol, barbiturates, anti-anxiety tranquillisers (e.g., Valium, Librium, Xanax, Prozac, and Thorazine), GHB (gamma hydroxybutyrate), Rohypnol, and many other antidepressants (e.g., Zoloft, Paxil).
(2) CNS Stimulants
CNS stimulants accelerate the heart rate and elevate the blood pressure and "speed-up," or over-stimulate, the body. Examples of CNS stimulants include cocaine, "crack" cocaine, amphetamines, and methamphetamine ("crank").
(3) Hallucinogens
Hallucinogens cause the user to perceive things differently than they actually are. Examples include LSD, peyote, psilocybin and MDMA (Ecstasy).
(4) Dissociative Anesthetics
Dissociative anaesthetics include drugs that inhibit pain by cutting off or dissociating the brain's perception of the pain. PCP, its analogs, and dextromethoraphan are examples of dissociative anesthetics.
(5) Narcotic Analgesics
Narcotic analgesics relieve pain, induce euphoria, and create mood changes in the user. Examples of narcotic analgesics include opium, codeine, heroin, demerol, darvon, morphine, methadone, Vicodin, and oxycontin.
(6) Inhalants
Inhalants include a wide variety of breathable substances that produce mind-altering results and effects. Examples of inhalants include Toluene, plastic cement, paint, gasoline, paint thinners, hair sprays, and various anaesthetic gases.
Oz
9 notes
·
View notes
Link
For decades, neurological, psychological, and cognitive alterations, as well as other glandular manifestations (EGM), have been described and are being considered to be part of Sjögren’s syndrome (SS). Dry eye and dry mouth are major findings in SS. The lacrimal glands (LG), ocular surface (OS), and salivary glands (SG) are linked to the central nervous system (CNS) at the brainstem and hippocampus. Once compromised, these CNS sites may be responsible for autonomic and functional disturbances that are related to major and EGM in SS. Recent studies have confirmed that the kynurenine metabolic pathway (KP) can be stimulated by interferon-γ (IFN-γ) and other cytokines, activating indoleamine 2,3-dioxygenase (IDO) in SS. This pathway interferes with serotonergic and glutamatergic neurotransmission, mostly in the hippocampus and other structures of the CNS. Therefore, it is plausible that KP induces neurological manifestations and contributes to the discrepancy between symptoms and signs, including manifestations of hyperalgesia and depression in SS patients with weaker signs of sicca, for example. Observations from clinical studies in acquired immune deficiency syndrome (AIDS), graft-versus-host disease, and lupus, as well as from experimental studies, support this hypothesis. However, the obtained results for SS are controversial, as discussed in this study. Therapeutic strategies have been reexamined and new options designed and tested to regulate the KP. In the future, the confirmation and application of this concept may help to elucidate the mosaic of SS manifestations.
2 notes
·
View notes
Note
Mold can have some pretty serious impacts. Such as:
"cognitive impairments, including memory, concentration, and attention span difficulties. Changes in behavior, such as increased irritability, mood swings, anxiety, depression, and difficulty sleeping"
"headaches and migraines"
"Disruption in Sleep-Wake Cycles"
"development or worsening of certain neurological disorders, such as multiple sclerosis (MS), Parkinson’s disease, and Alzheimer’s disease."
"potential to directly damage the central nervous system (CNS), leading to neuropathy (nerve damage), tremors, dizziness, coordination problems, and even seizures in severe cases."
"cause or worsen anxiety and depression"
Ohhh that's not good at all- that's really not good!
0 notes
Text
Is Red Ginseng Good For The Nervous System?

Red ginseng, a revered herb in traditional medicine, has been used for centuries for its myriad health benefits. Known scientifically as Panax ginseng, it undergoes a steaming and drying process that gives it its distinct red color and enhances its medicinal properties. Among its many potential benefits, red ginseng is often praised for its positive effects on the nervous system. This article explores the ways in which red ginseng can support nervous system health, backed by scientific evidence and practical insights.
Understanding the Nervous System
Structure and Function
The nervous system is a complex network that coordinates the body’s activities. It consists of two main parts: the central nervous system (CNS), which includes the brain and spinal cord, and the peripheral nervous system (PNS), which connects the CNS to the rest of the body. The nervous system is responsible for sensory input, information processing, and motor output, playing a crucial role in everything from reflexes to cognitive functions.
Common Nervous System Disorders
Several disorders can affect the nervous system, including:
Anxiety and Depression: Mental health conditions characterized by excessive worry, fear, sadness, and other emotional disturbances.
Neurodegenerative Diseases: Conditions like Alzheimer's and Parkinson's disease that involve the progressive degeneration of nerve cells.
Neuropathic Pain: Chronic pain resulting from nerve damage, often associated with conditions like diabetes or shingles.
Cognitive Decline: Age-related decline in cognitive functions such as memory, attention, and decision-making.
Red Ginseng’s Impact on the Nervous System
Cognitive Function and Memory
Red ginseng is known for its potential to enhance cognitive function and memory. This is largely attributed to its active compounds, ginsenosides, which have neuroprotective properties.
Scientific Evidence
A study published in the Journal of Ginseng Research demonstrated that red ginseng extract improved cognitive performance in healthy adults. Another study in Phytotherapy Research found that ginsenosides could enhance memory and learning by promoting the growth and differentiation of neural stem cells in the brain.
Stress and Anxiety Reduction
Red ginseng is classified as an adaptogen, meaning it helps the body resist stressors of all kinds, whether physical, chemical, or biological. It can modulate the stress response and reduce symptoms of anxiety.
Scientific Evidence
Research published in Biological & Pharmaceutical Bulletin indicated that red ginseng has anxiolytic effects, reducing anxiety in animal models. Another study in the Journal of Ethnopharmacology found that red ginseng reduced stress and improved mood in participants by regulating the hypothalamic-pituitary-adrenal (HPA) axis, which plays a key role in the stress response.
Neuroprotection and Anti-Inflammatory Effects
Inflammation and oxidative stress are significant contributors to neurodegenerative diseases and other nervous system disorders. Red ginseng’s anti-inflammatory and antioxidant properties can help protect the nervous system from these damaging processes.
Scientific Evidence
A study in Oxidative Medicine and Cellular Longevity highlighted that red ginseng reduced oxidative stress and inflammation in the brain, offering neuroprotection. Additionally, research in Neuropharmacology demonstrated that ginsenosides inhibited neuroinflammation, a critical factor in the progression of neurodegenerative diseases.
Energy and Mood Enhancement
Red ginseng is also known for its ability to enhance energy levels and improve mood, which can be particularly beneficial for individuals with nervous system disorders that cause fatigue and emotional disturbances.
Scientific Evidence
A study published in Current Clinical Pharmacology found that red ginseng improved mood and increased energy in individuals with chronic fatigue. Another study in the Journal of Alternative and Complementary Medicine reported that red ginseng supplementation led to significant improvements in mood and overall well-being.
Practical Considerations for Using Red Ginseng
Dosage and Forms
Red ginseng is available in various forms, including capsules, tablets, powders, and teas. The appropriate dosage can vary based on the specific product and individual health needs. It is generally recommended to start with a lower dose and gradually increase it while monitoring the body's response.
Combining with Other Supplements
For enhanced nervous system support, red ginseng can be combined with other supplements known for their neuroprotective and cognitive benefits, such as:
Ginkgo Biloba: Known for improving blood flow to the brain and enhancing cognitive function.
Omega-3 Fatty Acids: Essential fats that support brain health and reduce inflammation.
B Vitamins: Crucial for nerve function and energy metabolism.
Potential Side Effects and Interactions
While red ginseng is generally considered safe, it can cause side effects in some individuals, including headaches, digestive issues, and sleep disturbances. It may also interact with certain medications, such as blood thinners and diabetes medications. Consulting with a healthcare provider before starting red ginseng supplementation is essential, especially for those with underlying health conditions or those taking other medications.
Conclusion
Red ginseng offers a range of benefits for the nervous system, from enhancing cognitive function and memory to reducing stress and anxiety, providing neuroprotection, and boosting energy and mood. Scientific research supports many of these claims, highlighting the potential of red ginseng as a valuable supplement for nervous system health.
0 notes
Text
How Psychological Factors Impact Gut Function: Exploring the Mind-Gut Connection
The intricate relationship between the mind and the gut has fascinated researchers for decades. Increasingly, science is uncovering the profound ways in which our mental state can influence our digestive health. This complex interplay, often referred to as the "gut-brain axis," reveals that psychological factors such as stress, anxiety, and depression can significantly impact gut function. Let's delve into the fascinating connection between our mind and gut.
The Gut-Brain Axis: A Two-Way Street
The gut-brain axis refers to the bidirectional communication between the central nervous system (CNS) and the enteric nervous system (ENS), which governs the function of the gastrointestinal (GI) tract. This communication pathway includes neural, hormonal, and immunological signaling. It's through this axis that our mental state can influence gut function, and vice versa.
Stress and Gut Health
Stress is one of the most well-documented psychological factors affecting gut health. When we experience stress, the body releases hormones like cortisol, which can alter gut motility and increase inflammation. Chronic stress can exacerbate conditions such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD), leading to symptoms like abdominal pain, diarrhea, and constipation.
Anxiety and Digestive Disorders
Anxiety can also have a profound impact on the gut. The feeling of "butterflies" in the stomach during anxious moments is a testament to this connection. In more severe cases, anxiety can disrupt normal digestive processes, leading to symptoms such as nausea, bloating, and changes in bowel habits. Individuals with anxiety disorders are often more sensitive to sensations in the gut, which can amplify symptoms of digestive discomfort.
Depression and Gut Microbiota
Emerging research suggests that depression can alter the composition of gut microbiota—the diverse community of microorganisms living in our intestines. A healthy gut microbiome is crucial for proper digestion, nutrient absorption, and immune function. Depression-related changes in gut microbiota can lead to dysbiosis, a microbial imbalance that contributes to gastrointestinal issues and further affects mental health, creating a vicious cycle.

The Role of Gut Microbiota
The gut microbiota plays a pivotal role in the gut-brain axis. These microorganisms produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which influence mood and behavior. An imbalance in gut microbiota can affect the production of these neurotransmitters, linking gut health directly to psychological well-being. Probiotics and dietary changes that promote a healthy microbiome have shown promise in alleviating symptoms of both digestive and mental health disorders.
Mindful Eating and Digestive Health
Given the strong connection between psychological factors and gut function, adopting practices that promote mental well-being can improve digestive health. Mindful eating—paying full attention to the experience of eating and drinking—can reduce stress and enhance digestion. Techniques such as deep breathing, meditation, and regular physical activity can also support the gut-brain axis by reducing stress and promoting a balanced gut microbiome.
Seeking Professional Help
For individuals experiencing persistent gastrointestinal issues alongside psychological distress, seeking professional help is crucial. Gastroenterologists and mental health professionals can work together to address the multifaceted nature of these conditions. Treatments may include medications, dietary changes, cognitive-behavioral therapy (CBT), and other interventions aimed at improving both mental and digestive health.
Conclusion
The connection between psychological factors and gut function underscores the importance of a holistic approach to health. Understanding the gut-brain axis allows for more effective management of conditions that impact both the mind and the gut. By addressing mental health, we can foster better digestive health, and vice versa, paving the way for overall well-being.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference
Short Name: 14GHUCG2024
Dates: December 17-19, 2024
Venue: Dubai, UAE
Email: [email protected]
Visit: https://gastroenterology.universeconferences.com/
Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/
Register here: https://gastroenterology.universeconferences.com/registration/
Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/
Call Us: +1 (207) 707-7298
WhatsApp Us: +442033222718
0 notes
Text
Amphetamine Powder: Usage Guide and Side Effects

Introduction
Amphetamine powder is a potent central nervous system stimulant prescribed primarily for treating attention deficit hyperactivity disorder (ADHD) and narcolepsy. It is also known for its potential misuse due to its stimulating effects. Understanding its proper usage, potential benefits, and associated risks is crucial for safe and effective treatment.
Usage Guide
1. Medical Use
a. Dosage
ADHD:
Adults and children over 6 years: The typical starting dose is 5 mg once or twice daily, which can be increased by 5 mg at weekly intervals based on the patient's response. The usual effective dose ranges from 20 to 60 mg per day.
Narcolepsy:
Adults: The usual starting dose is 10 mg daily, divided into two to three doses. The dose can be increased by 10 mg at weekly intervals. The typical effective dose ranges from 20 to 60 mg per day.
b. Administration
Amphetamine powder prescribed for medical use is typically provided in pill or capsule form. If prescribed as a powder, it should be taken orally and can be mixed with water or another liquid.
c. Timing
It is usually taken in the morning to avoid insomnia. Some patients may need a second dose around noon or early afternoon.
d. Follow Doctor’s Instructions
Always follow the prescribing doctor's instructions precisely. Do not adjust the dose without consulting the doctor.
2. Recreational Use (Illicit and Unsafe)
a. Dosage
Illicit users often consume amphetamine powder in higher doses, significantly increasing the risk of side effects and dependence.
b. Administration Methods
Recreational use often involves snorting, swallowing, or dissolving the powder in water and injecting it. These methods are dangerous and can lead to serious health complications.
c. Risk of Overdose
Recreational use poses a high risk of overdose, which can be fatal.
Side Effects
1. Common Side Effects
Cardiovascular: Increased heart rate, elevated blood pressure, palpitations.
CNS: Insomnia, nervousness, restlessness, dizziness, headache.
Gastrointestinal: Dry mouth, loss of appetite, weight loss, stomach pain, nausea.
2. Serious Side Effects
Psychiatric: Severe anxiety, paranoia, hallucinations, aggression.
Cardiovascular: Heart attack, stroke, severe hypertension.
Dependence and Withdrawal: Risk of developing tolerance, dependence, and experiencing withdrawal symptoms such as fatigue, depression, and sleep disturbances upon cessation.
3. Long-term Effects
Mental Health: Long-term use can lead to severe mental health issues, including psychosis, depression, and anxiety disorders.
Physical Health: Chronic use can result in severe dental problems ("meth mouth"), skin sores, and significant weight loss.
Precautions and Contraindications
1. Medical History
Inform your doctor about any history of heart disease, mental health issues, or substance abuse.
2. Interactions
Amphetamines can interact with other medications, including antidepressants, antihypertensives, and medications for seizures. Always inform your doctor about all medications and supplements you are taking.
3. Pregnancy and Breastfeeding
Amphetamines should be avoided during pregnancy and breastfeeding due to potential harm to the fetus or infant.
Conclusion
While amphetamine powder can be beneficial for certain medical conditions when used as prescribed, it carries significant risks, particularly when used recreationally or inappropriately. Always follow medical advice strictly and be aware of the potential side effects and risks associated with its use. If you or someone you know is struggling with amphetamine misuse, seek professional help promptly.
For more information visit here:Evergreen Pharmacy Center
1 note
·
View note
Text
Is Ketamine an Opioid?

No, ketamine is not an opioid, despite frequent confusion due to their similar pain-relief functions. While both are potent analgesics, they differ in pharmacological mechanisms and chemical structures. Ketamine acts as an NMDA receptor antagonist, whereas opioids bind to opioid receptors. However, their shared usage in pain management and presence in medical and recreational settings contribute to ongoing confusion.
In terms of similarities, both ketamine and opioids provide pain relief through distinct pathways and can depress the central nervous system, leading to sedation and respiratory depression. However, differences between the two drugs are significant. Ketamine modulates glutamatergic transmission, while opioids bind to opioid receptors. Ketamine is less likely to cause respiratory depression and is not associated with constipation, tolerance, dependence, and addiction like opioids. Additionally, ketamine can induce hallucinations and perceptual distortions, unlike opioids. Opioids have a higher potential for abuse and addiction compared to ketamine, and they are mainly used for pain management, whereas ketamine is used for both pain relief and anesthesia.
Regarding ketamine overdose, it is possible, though rare when used therapeutically. Symptoms include confusion, hallucinations, respiratory depression, and loss of consciousness, with severe cases leading to respiratory depression or cardiovascular collapse. Overdose risk increases in recreational use, where doses and purity are unknown. It's essential to follow dosage guidelines and avoid mixing ketamine with other CNS depressants. In case of a suspected overdose, immediate medical attention is necessary.
Visit us here to learn more.
0 notes
Text
Comprehensive Overview of Aurobindo Pharma Ltd
Introduction to Aurobindo Pharma Ltd
Aurobindo Pharma Ltd is a leading global pharmaceutical company headquartered in Hyderabad, India. Established in 1986, the company has grown to become a significant player in the global market, offering a wide range of generic pharmaceuticals and active pharmaceutical ingredients (APIs). With a commitment to quality, innovation, and sustainability, Aurobindo Pharma has established a robust presence in over 150 countries.
Global Presence and Locations
Aurobindo Pharma's strategic locations worldwide play a crucial role in its global operations. The company operates through an extensive network of manufacturing facilities, research and development (R&D) centers, and distribution hubs. Below is a detailed breakdown of Aurobindo Pharma’s key locations.
Manufacturing Facilities
Aurobindo Pharma boasts state-of-the-art manufacturing facilities spread across various regions. These facilities are compliant with international regulatory standards, including the US FDA, UK MHRA, and WHO. The company’s manufacturing units are categorized into formulations, APIs, and specialty products.
India: Aurobindo has multiple manufacturing units across India, primarily in Hyderabad, Visakhapatnam, and Bengaluru. These facilities focus on producing a broad spectrum of pharmaceutical products, including oral, injectable, and topical formulations.
USA: Aurobindo Pharma USA operates several manufacturing and packaging facilities. These units support the company’s extensive portfolio of generic products in the US market.
Europe: The company’s European operations include manufacturing sites in countries like Italy and Portugal. These facilities specialize in high-quality generic drugs tailored for the European market.
Research and Development Centers
Innovation is at the heart of Aurobindo Pharma’s growth strategy. The company invests significantly in R&D to develop new and improved pharmaceutical products.
Hyderabad, India: The primary R&D hub is located in Hyderabad, equipped with cutting-edge technology and staffed by a team of highly skilled scientists and researchers.
New Jersey, USA: Aurobindo Pharma USA’s R&D center focuses on developing generic formulations and conducting clinical trials to ensure compliance with US regulatory standards.
Europe: Aurobindo’s R&D centers in Europe collaborate closely with local regulatory bodies to develop products that meet stringent European standards.
Distribution Hubs
Aurobindo Pharma’s global distribution network ensures the timely delivery of products to various markets. The company’s logistics infrastructure is designed to handle large volumes efficiently while maintaining the integrity and quality of the pharmaceuticals.
North America: Distribution centers in the USA and Canada serve as critical points for the North American market, ensuring rapid and efficient delivery of products.
Europe: Strategic distribution hubs across Europe facilitate seamless supply chain operations, enabling Aurobindo to meet the demands of the European market.
Asia-Pacific: The company’s distribution network in the Asia-Pacific region supports its growing market share in countries such as China, Japan, and Australia.
Product Portfolio
Aurobindo Pharma’s diverse product portfolio includes generic pharmaceuticals, APIs, and specialty products. The company’s commitment to affordability and quality has made it a trusted name in the healthcare industry.
Generic Pharmaceuticals
Aurobindo’s generic product line covers a wide range of therapeutic areas, including:
Cardiovascular: Medications for hypertension, heart failure, and other cardiovascular conditions.
Central Nervous System (CNS): Treatments for epilepsy, depression, and anxiety disorders.
Gastroenterology: Drugs for acid-related disorders, gastrointestinal infections, and liver diseases.
Anti-Retrovirals (ARVs): A comprehensive range of ARVs for the treatment of HIV/AIDS.
Active Pharmaceutical Ingredients (APIs)
Aurobindo Pharma is a major supplier of high-quality APIs used in the production of various pharmaceutical formulations. The company’s API portfolio includes:
Antibiotics: Broad-spectrum antibiotics for treating bacterial infections.
Anti-Diabetics: APIs for oral hypoglycemic agents.
Anti-Allergics: Ingredients used in the formulation of anti-allergic medications.
Specialty Products
Aurobindo’s specialty product range includes biosimilars and novel drug delivery systems. The company’s focus on niche segments has enabled it to cater to specific medical needs with innovative solutions.
Commitment to Quality and Compliance
Quality is a cornerstone of Aurobindo Pharma’s operations. The company adheres to stringent quality control measures and regulatory compliances across all its facilities.
Regulatory Approvals
Aurobindo Pharma’s products are approved by major regulatory bodies worldwide, including:
US Food and Drug Administration (FDA)
European Medicines Agency (EMA)
World Health Organization (WHO)
Therapeutic Goods Administration (TGA), Australia
Quality Control Systems
The company employs advanced quality control systems to ensure the highest standards of product safety and efficacy. Regular audits and inspections are conducted to maintain compliance with international standards.
Sustainability Initiatives
Aurobindo Pharma is committed to sustainable practices that minimize environmental impact. The company’s sustainability initiatives include:
Green Manufacturing: Adoption of eco-friendly manufacturing processes to reduce carbon footprint.
Waste Management: Efficient waste management systems to handle pharmaceutical waste responsibly.
Energy Conservation: Implementation of energy-saving measures and use of renewable energy sources.
Future Outlook and Strategic Goals
Aurobindo Pharma global presence further through strategic acquisitions, partnerships, and continuous innovation. The company’s future goals include expanding its product portfolio, entering new markets, and enhancing its R&D capabilities to address unmet medical needs.
0 notes
Text
Simple Daily Practices to Calm and Regulate Your Nervous System

In the hustle and bustle of modern life, it's easy to feel overwhelmed by stress and anxiety. From work deadlines to family obligations, the demands of daily living can take a toll on our nervous system, leaving us feeling frazzled and out of balance. However, by incorporating simple daily practices into our routine, we can calm and regulate our nervous system, promoting a greater sense of calm and well-being. In this blog post, we'll explore a variety of techniques and strategies that you can implement to support your nervous system and cultivate inner peace.
Understanding the Nervous System
Before we delve into specific practices, let's take a moment to understand the role of the nervous system in our overall health and well-being. The nervous system is a complex network of nerves and cells that transmit signals between different parts of the body, allowing us to respond to stimuli and regulate various bodily functions. It consists of two main components: the central nervous system (CNS), which includes the brain and spinal cord, and the peripheral nervous system (PNS), which connects the CNS to the rest of the body.
The Impact of Stress on the Nervous System
Stress is a natural response to perceived threats or challenges, triggering the body's "fight or flight" response and releasing hormones like cortisol and adrenaline. While this response is essential for survival in dangerous situations, chronic stress can have detrimental effects on the nervous system. Prolonged activation of the stress response can lead to increased inflammation, elevated blood pressure, and disruptions in hormone levels, contributing to a wide range of health problems, including anxiety, depression, and cardiovascular disease.
Daily Practices for Nervous System Regulation
Now that we understand the importance of regulating our nervous system, let's explore some simple daily practices that can help promote relaxation and calmness:
Mindful Breathing: Take a few moments each day to practice mindful breathing. Sit or lie down in a comfortable position, close your eyes, and focus on your breath as it enters and leaves your body. Notice the sensations of each inhale and exhale, allowing yourself to fully experience the present moment.
Progressive Muscle Relaxation: Progressive muscle relaxation is a technique that involves tensing and relaxing different muscle groups in the body. Start by tensing the muscles in your feet and slowly work your way up to your head, progressively releasing tension with each breath. This practice can help reduce physical tension and promote a sense of relaxation.
Nature Walks: Spending time in nature is a powerful way to calm the nervous system and reduce stress. Take a leisurely walk in the park or along a nature trail, allowing yourself to fully immerse in the sights, sounds, and smells of the natural world. Notice the beauty of your surroundings and let go of any worries or distractions.
Journaling: Journaling is a valuable tool for processing emotions and reducing mental clutter. Set aside time each day to write down your thoughts, feelings, and experiences in a journal. This practice can help you gain clarity, perspective, and insight into your inner world, leading to greater emotional balance and well-being.
Gratitude Practice: Cultivating an attitude of gratitude can have profound effects on the nervous system. Take a moment each day to reflect on the things you're grateful for, whether it's the support of loved ones, the beauty of nature, or the simple pleasures of everyday life. Expressing gratitude can shift your focus from negativity to positivity, promoting a sense of peace and contentment.
Conclusion
In conclusion, incorporating simple daily practices into your routine can help calm and regulate your nervous system, promoting greater resilience and well-being in the face of stress and uncertainty. Whether it's mindful breathing, progressive muscle relaxation, nature walks, journaling, or gratitude practice, find what works best for you and make it a priority in your daily life. By nurturing your nervous system with care and compassion, you can cultivate inner peace and thrive in all aspects of your life.
1 note
·
View note
Text
Understanding Neurology: Exploring the Complexities of the Brain and Nervous System
Neurology is the branch of medicine that focuses on the study and treatment of disorders of the nervous system. This intricate system comprises the brain, spinal cord, and peripheral nerves, controlling everything from basic motor functions to complex cognitive processes. Here are some key points to delve deeper into the realm of neurology:
Structure and Function of the Nervous System: The nervous system can be broadly divided into two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS consists of the brain and spinal cord, while the PNS includes all the nerves outside the CNS. Each component plays a crucial role in transmitting signals and coordinating bodily functions.
Neurons and Neurotransmitters: Neurons are the building blocks of the nervous system, responsible for transmitting electrical and chemical signals. Neurotransmitters are the chemical messengers that allow communication between neurons. Imbalances in neurotransmitter levels are often implicated in various neurological disorders, such as Parkinson's disease and depression.
Common Neurological Disorders: Neurology encompasses a wide range of disorders, including epilepsy, stroke, Alzheimer's disease, multiple sclerosis, and migraine. These conditions can arise from various causes, such as genetics, infections, trauma, or autoimmune responses, leading to diverse symptoms and complications.
Diagnostic Techniques: Neurologists utilize a variety of diagnostic tools to assess and diagnose neurological conditions. These may include neurological exams, imaging studies (such as MRI and CT scans), electroencephalography (EEG), nerve conduction studies, and lumbar puncture (spinal tap).
Treatment Modalities: Treatment approaches in neurology aim to manage symptoms, slow disease progression, and improve quality of life. Depending on the condition, treatment may involve medications, physical therapy, surgery, lifestyle modifications, or a combination of these interventions.
Advancements in Research: Ongoing research in neurology continues to deepen our understanding of the brain and nervous system, paving the way for innovative treatments and interventions. Areas of focus include neuroplasticity, neurogenetics, stem cell therapy, and the development of targeted therapies for neurological disorders.
Multidisciplinary Approach: Neurological care often requires collaboration among various healthcare professionals, including neurologists, neurosurgeons, neuropsychologists, physical therapists, occupational therapists, and speech-language pathologists. This multidisciplinary approach ensures comprehensive care tailored to each patient's needs.
Understanding neurology is crucial not only for healthcare professionals but also for individuals seeking to comprehend the complexities of the human brain and nervous system. By exploring these key points, we gain insight into the fascinating world of neurology and its profound impact on human health and well-being.
best neurologist in hyderabad
#best neurologist in hyderabad#top neurologist in hyderabad#neurologist#neurologist in hyderabad#neurologist in kukatpally
0 notes
Text
Xanthine Derivatives as Emerging Neuroprotective Agents
In recent years, xanthine derivatives have garnered significant interest in the field of neurology, primarily due to their potential as neuroprotective agents. Historically recognized for their role in respiratory conditions as bronchodilators, these compounds are now being explored for their capacity to guard against neurodegenerative diseases such as Parkinson’s, Alzheimer’s, and multiple sclerosis. This shift toward neurological applications highlights a promising area of pharmacological research, where the multifunctional nature of xanthine derivatives could offer new avenues for treatment strategies.
Understanding Xanthine Derivatives
Xanthine derivatives, which include well-known compounds such as caffeine, theobromine, and theophylline, are purine bases found naturally in plants and animals. They have various systemic effects, most notably as stimulants of the central nervous system (CNS). Their mechanisms of action typically involve phosphodiesterase inhibition, adenosine receptor antagonism, and modulation of intracellular calcium levels—all of which contribute to their psychoactive and physiological effects.
Mechanisms of Neuroprotection
The potential neuroprotective mechanisms of xanthine derivatives are multifaceted. One key aspect is their ability to modulate neurotransmitter systems, particularly adenosine receptors in the brain. Adenosine acts as a CNS depressant and plays a role in promoting sleep and suppressing arousal. By blocking adenosine receptors, xanthine derivatives can enhance neuronal firing and increase dopamine and glutamate release, which are crucial for cognitive function and overall brain health.
Moreover, xanthine derivatives have been shown to exhibit antioxidant properties. Neurodegenerative diseases often involve oxidative stress, where harmful free radicals cause cellular damage. Xanthines can mitigate this by neutralizing free radicals and reducing oxidative stress, thereby protecting neuronal integrity and function.
Research and Evidence
Extensive research has been conducted to evaluate the neuroprotective potential of these compounds. For instance, studies have suggested that caffeine, the most widely consumed xanthine, may reduce the risk of developing Parkinson’s disease. Research indicates that caffeine may help in maintaining dopamine levels in the brain, which are critically depleted in Parkinson’s patients. Similarly, epidemiological studies have found a correlation between caffeine consumption and a reduced risk of Alzheimer’s disease, hypothesizing that caffeine’s ability to inhibit amyloid-beta production—a key factor in Alzheimer’s pathology—may play a role.
In experimental models, theophylline has shown promise in reducing neuronal damage in models of ischemic stroke. By inhibiting phosphodiesterase, theophylline helps in elevating cyclic AMP levels, which can have protective effects against cell death in acute neurodegenerative conditions.
Clinical Implications and Future Directions
The translation of these findings into clinical practice could revolutionize the management of neurodegenerative disorders. Currently, most neuroprotective strategies focus on managing symptoms rather than halting disease progression. Xanthine derivatives could potentially fill this gap, offering not only symptomatic relief but also a means to protect against neuronal degradation over time.
However, more clinical trials are needed to substantiate these effects in human populations and to understand the optimal dosages and potential side effects. The challenge lies in balancing efficacy with safety, particularly because excessive consumption of xanthine derivatives can lead to side effects like insomnia, nervousness, and in some cases, cardiovascular issues.
Conclusion
As research progresses, xanthine derivatives continue to be a focal point of interest for their neuroprotective properties. Their widespread availability and relatively low cost also make them attractive candidates for large-scale use if their efficacy and safety are clinically confirmed. Moving forward, it will be crucial to conduct detailed studies to elucidate the mechanisms through which these agents exert their effects and to establish clinical guidelines for their use in neurology. Harnessing the power of xanthine derivatives could indeed pave the way for novel therapies in combating the complex challenge of neurodegenerative diseases, potentially improving quality of life for millions of affected individuals worldwide.
0 notes