#Electrophysiology Studies
Text
Role of Electrophysiology Studies and Radiofrequency Ablation in Managing Arrhythmias
Discover the pivotal role of Electrophysiology Studies & Radiofrequency Ablation in effectively managing arrhythmias at Mukat Hospital. Learn about cutting-edge techniques & specialized care for a healthier heart.

Read more: https://www.mukathospital.com/electrophysiology-study-radiofrequency-ablation/
1 note
·
View note
Text



2024-02-02
New semester new me — not really though, despite my highest hopes. It’s only the end of the first week and I’ve already got work piling up. Absolutely wild.
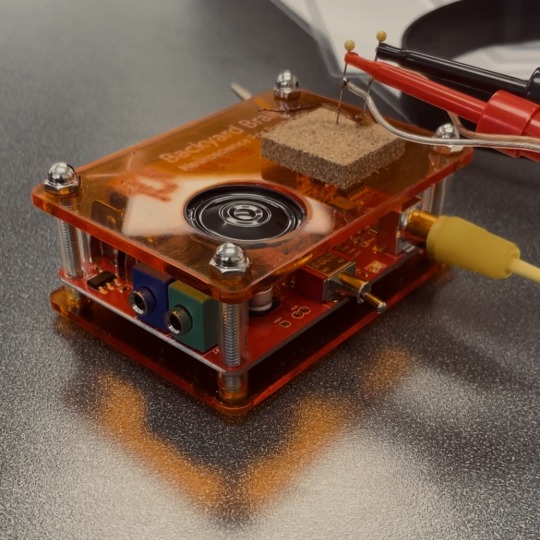
#bottom left is an electrophysiology workshop I went to#we made a cockroach leg dance to cotton eye joe#disclaimer: no cockroaches were harmed during this experiment#they were anethetized and legs grow back in 3 months#studyblr#studyspo#study aesthetic#aesthetic#student#my posts#study#chaotic academia#stem academia
19 notes
·
View notes
Text
In the short movie represented, taken from the university archive, you can look at a curious experiment that took place in the firs years of the '900, when physiologist were working on the relationship between electricity and the human body. A brief report accompanies the movie.
Colette De La Beatrix was the countess of a small town called "Holy Lady in the Countryside", she was married to a professor of that time. Unfortunately at the age of 32 she suffered a terrible accident while riding her horse. She was embossed down from the saddle and the horse stomped her right in the center of her chest, destroying the frontal part of her rib cage. She was saved miraculously by the university's surgeon that had to remove her sternum leaving her most vital organ covered only by a thin layer of skin. Usually she wore an iron plate to cover and protect her exposed heart. Her husband convinced her to take advantage of the events and participate in his studies about electrophysiology. She happily took part to them and once results were gathered they decided to show them to the other professors and film the experiment.
The movie starts with the countess sitting on a woodden bench. her entire chest is exposed and the shape of her beating heart is clearly visible. A rudimental microphone, linked to a gramophone, is held by a belt on the center of her chest and picks up her heartbeat. Two electrodes are attached on the oppiside sides of her heart linking the organ with what was probably a battery.
The report is divided into different parts:
Initial- Countess initial heart rate: 85 bpm
Showing the audience her condition and her synus rhythm at rest.
Single electrical pulses are charged on her heart to demonstrate electricity can start artificial systoles. Audience is encouraged to feel the countess' carotid pulse to further proove the experiment effectiveness.
This part ends with a note hand-written.
"remember to tell the audience to never directly touch her heart to avoid dangerous ahrrythmias".
Part 2- Artificial pacing at 120bpm
The machine delivers a series of consecutive impulses to create an artificial rhythm. The countess's heart reacts to each pulse correctly contracting in a new manually-induced pace. Audience is encouraged to feel the countess' carotid pulse under the influence of the continuous pulses.
NOTE: After the pulses are interrupted the countess' heart recovers its initial pace immediately.
Part 3- Reaching physiological limit, 187bpm
To demonstrate total control on the countess' heart rhythm the heart is artificially paced at her maximum heart rate (220 - her age 32). electrical pacing can realize the same results as a strenuous physical effort. The battery completely bypassed her local pacemaker. Audience is encouraged to feel the countess' carotid pulse and look at her beating heart.
NOTE: Frank and Starling were right, the artificial rhythm seems hard to sustain for her system. The fast her heart gets the less efective its beating becomes.
NOTE2: Her heart takes some long pauses in order to recover.
Part 4- Beyond physiological limits 240bpm
The domain over her natural pacemaker is so absolute that its natural limit can be higly bypassed. The heart is paced at an innatural rhythm. Audience is encouraged to feel the countess' carotid pulse and look at her beating heart.
NOTE: Audience report that just a very tiny wave of blood can be felt at her neck after each heart contraction.
NOTE2: The countess's heart seems unable to follow each electrical pulse as some dyastoles seem abolished in a tetanus like manner.
NOTE3: The procedure is interrupted as the countess lost consciousness for a brief period of time.
NOTE4: Once the machine is turned off a long period of asystole is seen with subsequent ahrrythmias after the spontaneous pulsation restarted. Heart exhaustion?
another hand-written part:
"I should have never tried this on my wife"
What the report doesn't says is that countess Colette De La Beatrix died of sudden cardiac arrest few days late.
251 notes
·
View notes
Text
Alzheimer's-like brain changes found in long COVID patients - Published Sept 2, 2024
New research from the University of Kentucky's Sanders-Brown Center on Aging shows compelling evidence that the cognitive impairments observed in long COVID patients share striking similarities with those seen in Alzheimer's disease and related dementias.
The study, published in Alzheimer's & Dementia, highlights a potential commonality in brain disorders across these conditions that could pave the way for new avenues in research and treatment.
The study was a global effort, and brought together experts from various fields of neuroscience. Researchers at the UK College of Medicine led the study, including Yang Jiang, Ph.D., professor in the Department of Behavioral Science; Chris Norris, Ph.D., professor in the Department of Pharmacology and Nutritional Sciences; and Bob Sompol, Ph.D., assistant professor in the Department of Pharmacology and Nutritional Sciences. Their work focuses on electrophysiology, neuroinflammation, astrocytes and synaptic functions.
"This project benefited greatly from interdisciplinary collaboration," Jiang said. "We had input from experts, associated with the Alzheimer's Association International Society to Advance Alzheimer's Research and Treatment (ISTAART), across six countries, including the U.S., Turkey, Ireland, Italy, Argentina and Chile."
Jiang and the collaborative team focused their work on understanding the "brain fog" that many COVID-19 survivors experience, even months after recovering from the virus. This fog includes memory problems, confusion and difficulty concentrating. According to Jiang, "The slowing and abnormality of intrinsic brain activity in COVID-19 patients resemble those seen in Alzheimer's and related dementias."
This research sheds light on the connection between the two conditions, suggesting that they may share underlying biological mechanisms. Both long COVID and Alzheimer's disease involve neuroinflammation, the activation of brain support cells known as astrocytes and abnormal brain activity. These factors can lead to significant cognitive impairments, making it difficult for patients to think clearly or remember information.
The idea that COVID-19 could lead to Alzheimer's-like brain changes is a significant development.
"People don't usually connect COVID-19 with Alzheimer's disease," Jiang said. "But our review of emerging evidence suggests otherwise."
The research reveals that the cognitive issues caused by COVID-19 reflect similar underlying brain changes as those in dementia. The study's insights emphasize the importance of regular brain function check-ups for these populations, particularly through the use of affordable and accessible tools like electroencephalography (EEG).
The study not only highlights the shared traits between long COVID and Alzheimer's, but also points to the importance of further research.
"The new insight opens avenues for future research and clinical practice, particularly in studying brain oscillations related to neural biomarkers of mild cognitive impairment in people with long COVID," said Jiang.
One of the key findings is the role of astrocytes—support cells in the brain that have not been as thoroughly studied as neurons. The research suggests that damage or activation of these cells by COVID-19 can cause synaptic dysfunctions, leading to the abnormal brain activity observed in both conditions. This discovery is significant because it may help explain why EEG patterns in COVID-19 patients resemble those seen in the early stages of neurodegenerative diseases like Alzheimer's.
Researchers believe this work could have a direct impact on patient care. They are advocating for routine EEG exams to detect early brain changes in both COVID-19 survivors and those at risk for cognitive decline.
"EEG patterns in COVID-19 patients resemble those seen in early neurodegenerative diseases," said Norris.
"These similarities may be due to shared issues such as brain inflammation, astrocyte activity, low oxygen levels and blood vessel damage," said Sompol.
By detecting these changes early, health care providers could potentially identify at-risk individuals sooner and implement interventions to prevent or slow the progression of cognitive decline.
As research continues, the team is particularly interested in how EEG monitoring can predict long-term outcomes in COVID-19 patients and assess the effectiveness of treatments aimed at preventing cognitive decline.
More information: Yang Jiang et al, Parallel electrophysiological abnormalities due to COVID‐19 infection and to Alzheimer's disease and related dementia, Alzheimer's & Dementia (2024). DOI: 10.1002/alz.14089
alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.14089
#covid#mask up#pandemic#covid 19#wear a mask#sars cov 2#coronavirus#public health#still coviding#wear a respirator#long covid
54 notes
·
View notes
Text

the adventure of tb and gb writing a 2763 page essay about the benefits of in vivo and in vitro electrophysiological study towards the understanding of neural connections dictating basic motor control and like, astrophysics or something idk
#NEEEEEEEERD#not like that topic hasnt already been covered. but whatever#bfdi#tpot#tennis ball#golf ball
75 notes
·
View notes
Text
sorry to come back to this but this truly fascinates and concerns me for so many reasons
obligatory "Ah sweet. Man-made horrors beyond my comprehension." comment
so first of all: brain organoids. which are grown from human stem cells into just little brains with underdeveloped eyes, they have a lifespan of about 100 days because they are an organ without a system.
these brain organoids are something that have a lot of potential when it comes to studying any number of things. just off the top of my head i would think- the process of human development, disease studies, healing tissue development, foetal and premature development of consciousness, ect ect ect i'm not informed on this type of research so i will freely admit idk.
and they are using 16 at a time as processors with computer chips. okay sure, scifi aside, the structure of an organ being used for it's complexity compared to the limitations of material and efficiency in current technology makes sense. if it helps imagine if a branch or a kidney were hooked up to a computer chip and we found out that it worked as good or better than mechanical processors for a fraction of the energy use. i am also not informed on how most technology works, please keep in mind, but i am also not opposed to the idea of combining these types of technologies in theory. and the biggest downfall currently is short shelf-life of the organoids required.
but the thing is, i think, that this is specifically an early development of a brain, at what point is consciousness defined? there is no sensory system beyond the basic light perception of the eyes and the input to the brain but at what point is the responses automatic and at what point is it complex enough to be aware in some abstract way. this question is one that can be applied to any form of animal of course.... but i think also that it is strange that these organoids are being specifically developed from human stem cells and not any number of other animal as a brain is a brain and at the small scale they are growing these organoids most of the speculative benefits of human logic are irrelevant- they are operating at pre mature infant levels which could just as easily be achieved by any number of apes cells surely?
is there going to be a developmental cut off for these organoids? at what point of biological development is the ethical ick factor for consciousness? because of how stem cells are able to be harvested in a non destructive fashion things like lab grown meat make sense to me- those are consumed but can also offset the requirements for the meat industry- and if these organoids are also grown from stem cells that's great but at what point is making that many to be burnt through as processors a wasteful use when there are other possible avenues of study? the wide commercial release of such experimental tech seems a little risky considering how quickly new technologies are exploited- just look at bitcoin farms and ai scraping- for the sake of profit with no care for ethical implementation or construction or impact.
this is a weird post from me but sorry i just have some questions i want you the person reading this to think about with me, seperate to any deep reading of the science because i wanna focus on the personal reaction to the concepts, (feel free to read the science tho i encourage it) just something to chew on i'm not expecting any philosophically concrete answers:
would you use the brain organoid processor tech if you had the chance?
why?
Why is it important that these have to be grown from human stem cells
where is the line between organ and being/consciousness
let's contend: there is the world (physical) and there is the senses (contact with the physical) and there is the experience (interpretation)
is it the senses or the experience that makes a creature conscious? how complex do the senses need to be before the experience is positive or negative?
where is that experiencial definition? is it as simple as feels good feels bad?
is it the tendency to circulate repeatedly on the same neural pathway? how are those neurological reactions controlled? are they controlled?
how do you feel about scientific testing on humans?
how do you feel about scientific testing on animals?
how do you feel about scientific testing on plants?
how do you feel about scientific testing on fungi?
how do you feel about scientific testing on single celled organisms?
how do you feel about scientific testing on organs?
how do you feel about scientific testing on technology?
what do you consider the line to be for ethical research? is it funding? is it theory versus practice? is it use of information? is it method of data collection? is it intent? is it implementation? is it within a limitation of precedent? is it within a limitation of subject? are there areas you think should be left alone on principle? why?
what level of complexity is required for the question of consent of participant?
where should limitations be imposed on use? why would limitations be necessary? who has the right to information? who has the right to profit?
Who is profiting from these studies? where will this technology be used? who is competing with this technology? what other technologies might this impact? will other technologies using the same concept adhere to the same limitations/ethics?
do you think everyone using the brain organoid based processors for $500pcm are thinking about these questions? should they have to?
disclaimer: i am uneducated and uninformed in the fields of science and technology so this is one hundo percent a personal response to information i have very little context for. But i also think it's important to think actively about technology and avoid complacency about the way it impacts our lives so doing little thought exercises in response to articles like this is, I think, a good thing.
43 notes
·
View notes
Text
Following a heart attack during Memorial Day weekend (the weekend before last), my dad had a quadruple bypass on Tuesday. On Thursday my dad's heart stopped. He was fully conscious when it happened, and in fact only lost consciousness when his ICU nurse gave him drugs to knock him out and hopefully prevent him from remembering anything that was happening. He is hooked up to a respirator, so there was no oxygen lost to his brain during any of this. After 15 min. his heartbeat was stabilized and they took him to be examined, as the original thought was it could have been caused by either the cow valves or his new arteries not taking properly. A bad stitch was also proposed to us as a possible cause. None of those things were found, the surgery itself was a success.
Last night at 2:00 am my dad's heart stopped again. This time it took 12 minutes for him to be stabilized. Like the first time, he had come out of the sedation just the day before. He was fully conscious again as it happened, so the nurse gave him drugs to knock him out, and wow but I am hoping he really won't remember either of these incidents. I can not tell you how grateful I am that the state my parents live in has legistlation on the books mandating that ICU nurses never have more than two cases at a time.
Based on the second incident they are now saying it was probably down to an electrical misfire in his heart, and the EP (electrophysiologic) Cardiology team will be seeing him tomorrow to both figure out the exact cause and determine best next steps. As of now the options on the table as I understand them are further studies and/or numbing a faulty nerve and/or putting in a pacemaker and/or putting in an AICD device (implanted defibrillator).
My mother and I are currently trying to stay hopeful that the EP will be able to figure out what is going wrong with my dad's electrical impulses and fix whatever it is. All of that said, it is really hard to see him in the ICU day after day, especially since with the exception of Wednesday and late in the day yesterday he has been sedated and unconscious since the surgery. The toll this recovery is taking on my mother and I emotionally is far larger then I had expected it to before his surgery.
We are currently camped out in a hotel room near the hospital (Who opens a theme B&B across the street from a regional feeder hospital? You have a captive audience already, who don't want themeing at the expense of functionality. Based on conversations during breakfast EVERYONE is there because a smaller hospital sent a loved one to the place across the street when they determined the case was outside their capabilities) and talk of little else together. Spending every single day with her (during Pride! This is my Pride month!) freaking out about my dad's condition has been A LOT. A very banal example of what happens when you spend multiple days with your mother like this: yesterday she complained that I snore, and then followed that up by (in the literal exact tone she cooed at me as a baby) telling me that it is a "very cute" snore. This was even less amusing to me because my mother snores and her snore is just awful. This is of course to say nothing of us setting each other off when we are upset because we are on top of each other all day every day.
24 notes
·
View notes
Text
molecular bionics engineering
👩🏼🔬🧠🧬📚🔬🦾🧮



• a complex engineering course, which combines biological and chemical studies with electronical and programming courses. it’s not a typical engineering degree, you can specialize in a several scientific masters degrees, and companies will race for your knowledge!
• first two semesters are about the basic engineering classes: discrete mathematics, calculus, physics for engineers, electronics, programming, also we have classes from biology and chemistry blocks, as well, like: basic chem (with laboratory), basic bio, cell biology, organic chemistry (with laboratory).
• our university has mandatory, also a lots of elective classes for neuroscience, which is truly the most interesting thing for me! we will study some audiology based courses in our 3rd academic year when we study more about coclear implants and its programming/building schedule. furthermore, we can add a lot of different elective classes from the 4 big blocks: biology, chemistry, physics or informatics, so it’s so diferse how you can “specialize” in this bachelor’s degree.
• the best part of this course is the worst one, too: you choose your own interests and classes, this degree covers literally everything in between STEM! some of my classmates says it’s the negative of our major, but in my opinion that’s the beauty of this! personally, everything in neuroscience amazes me now and i can’t literally choose one specialty (recently i’m so interested in molecular neuroscience and neurophysiology, but electrophysiology overall or specifically neuroplasticism has a spot in my heart, too), and yes, i’m in my first year at uni but i’m so excited for future researches and publications, i wanna work at a laboratory asap and start my life as a real STEM girlie:D
#saját#studyblr#lizystudying#myown#lizysinpain#studying#study#study vibes#bionics#engineer#engineering#engineer student#lizysbionics#university vibes#uni student
49 notes
·
View notes
Note
For the Past Life Durgetash asks: 5 & 6!
Ask meme here! Thank you lovely!
5. Their favourite 'strictly business associates' bonding activity on a Saturday night? Please don't leave out any of the bloody gory details.
Oh I can go two ways with this. Domestic and unhinged. A domestic night for them usually came later on in the piece, in the last few years before Orin absconded with her, and they were both working frantically to make sure their plans came to pass. They'd usually both be on opposite ends of one of the couches, legs entwined while they both poured over their respective books and notebooks - Enver reading Gondian treatises on the volatility of black powder and any necromantic essays on neurology and electrophysiology he could get his hands on, Kass reading absolutely everything and anything under the sun in her voracious thirst for knowledge. Druidic alchemical guides, dry political theses on various class movements, insanely complex discussions on spelljammer technology. She doesn't get the peace to study or read quietly at home, so they sometimes fell asleep like that.
Unhinged, they played incredibly deranged sexual games with a lot of their prey, especially when they were younger. There was at least one occasion when Gortash invited several rival leaders of various smuggling and merc groups to dinner, only for them all to be paralysed by a poison in the food, at which point Kass trotted out dressed in a terribly slutty french maid outfit pretending to serve drinks, while she actually slit all of their throats one by one while Gortash pretended to berate her for being clumsy in front of his guests. They all had to sit there paralysed and waiting for their turn to die while she teetered around the table in stiletto heels pretending she was trying to clean up the blood with napkins. And then Kass and Enver fucked on the table while the last one sat frozen and forced to watch
6. Describe their dynamic in one sentence. Without using toxic.
I'm going to love you on purpose.
It's a challenge. It's a taunt. It's a mocking reminder that they can't control one another no matter how hard they both try to twist each other. It's a desperate life buoy for a little boy sold into demonic slavery and for a little girl who was dumped on top of a pedestal and told she was untouchable. It's a moment of defiance. It's a love confession whispered late at night. It's the one thing that finally broke both of them.
8 notes
·
View notes
Text
Ultimately, these relationships threaten the sustainability of healthcare and expose patients to unnecessary risk or harm, according to Alice Fabbri, Ph.D., and Quinn Grundy, Ph.D., authors of an edit
Etienne de la Boetie2
Sep 17, 2024
by Suzanne Burdick, Ph.D.
Makers of drug and medical devices target doctors early in their careers, through payments, free meals and sponsored education, to “cultivate long term, reciprocal relationships,” according to the authors of an editorial published Monday in The BMJ.
“Ultimately, these relationships threaten the sustainability of healthcare and expose patients to unnecessary risk or harm,” wrote Alice Fabbri, Ph.D., and Quinn Grundy, Ph.D.
Fabbri is a health department lecturer at the University of Bath in England. Grundy is an assistant professor of nursing at the University of Toronto in Canada. In their Sept. 9 editorial, they cited studies documenting levels of Big Pharma industry payments made to early-career physicians.
For instance, a study published Sept. 1 in JAMA Internal Medicine showed that among 5,533 U.S. cardiology fellows, 73% received “industry marketing payments” in the year before graduating and 88% received payments in the first few years after they graduated.
“For fellows in specialties that use a lot of technology (referred to as ‘procedural intensive’),” Fabbri and Grundy noted, “the proportion was even higher: 80% received payments before graduating, and 96% afterwards.”
More industry payments are given to cardiologists than to any other type of specialist, they said. “In one study, just 11 of 195 directors of cardiac catheterisation and electrophysiology laboratories received no industry payments in a single calendar year.”
5 notes
·
View notes
Text
@lieahsblog Has been screaming into the void and sharing regular updates on this particular campaign to help boost it for Razan, her mother Ghada and their family.
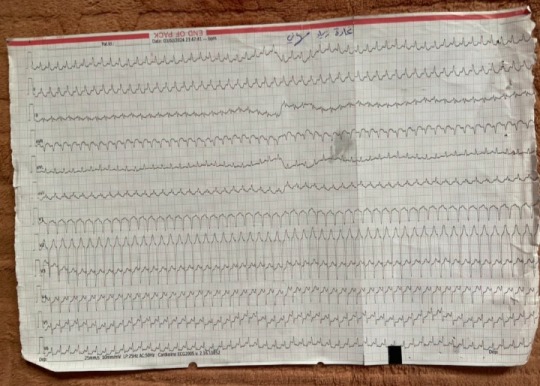
Ghada has a heart condition and needs medical intervention that she can't get in Gaza. Razan shared her mother's ECG:
And the details of her mother's report:
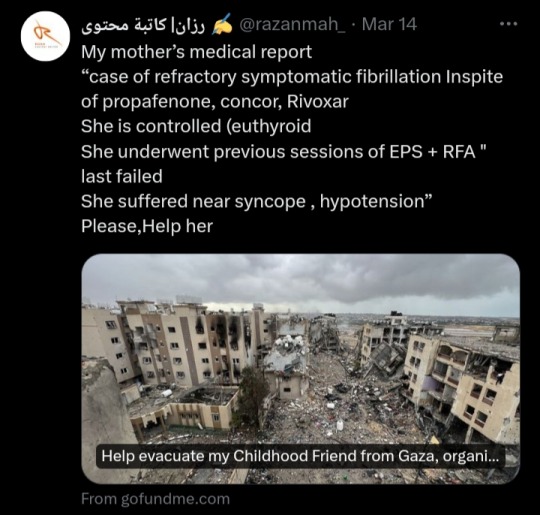
All to help us understand the URGENCY
Basically, Ghada has an abnormal heartbeat (arrhythmia) despite her medications. She did Electrophysiology Studies (EPS) to identify the cause and a Radiofrequency Ablation (RFA) to try to remove the problem area from the heart once it was found but the procedure failed and Ghada had a drop in blood pressure and near loss of consciousness.
This isn't something Razan should have had to do at all, sharing private medical details with the world, it should be enough that they genuinely need help. Hell, her family and other families in Gaza shouldn't have to be pleading for donations to be able to leave their own home and live either.
We can get shows that have been off air for years trending. We can create viral posts on the most random topics. I know there a lot of families that need help and maybe that's tiring to keep seeing for some but that's the reality. Gaza is suffering a horrific genocide and forced famine and a complete breakdown of their healthcare. They need help and a simple reblog can help them. If you really can't donate at least share but if you can spare anything at all please do it!
#gaza#go fund me#donations#urgent appeal#urgent medical care needed#donate if you can#mutual aid#go fund them#boost#signal boost#boost the signal#please help#please share#save palestinians#current events#free gaza#palestine#free palestine#reblog#genocide in gaza#heart condition#cardiac arrhythmia#gofundme#urgent#help needed#gaza fundraiser#medical aid for palestinians#even a small donation can go a long way#donation for gaza#evacuation
11 notes
·
View notes
Text
Understanding Dysautonomia: A Comprehensive Overview
Dysautonomia refers to a group of disorders characterized by abnormalities in the autonomic nervous system (ANS), which regulates involuntary bodily functions such as heart rate, blood pressure, digestion, and temperature regulation. This condition can lead to a range of symptoms and significantly impact a person's quality of life. This article explores what dysautonomia is, its types, symptoms, causes, diagnosis, and management.
What is Dysautonomia?
The autonomic nervous system is responsible for controlling the automatic functions of the body that we don’t consciously regulate. Dysautonomia occurs when this system malfunctions, leading to symptoms that affect various physiological processes. The term "dysautonomia" encompasses several different disorders that affect the ANS, each with its own specific manifestations and underlying causes.
Types of Dysautonomia
Dysautonomia can manifest in several forms, including:
Postural Orthostatic Tachycardia Syndrome (POTS): A condition where an abnormal increase in heart rate occurs when transitioning from lying down to standing up, often accompanied by dizziness, palpitations, and fatigue.
Neurocardiogenic Syncope (NCS): Characterized by fainting or near-fainting episodes due to a sudden drop in heart rate and blood pressure, often triggered by standing for long periods or emotional stress.
Multiple System Atrophy (MSA): A rare, progressive neurodegenerative disorder that affects the autonomic functions along with motor control, leading to symptoms like balance problems, difficulty walking, and urinary dysfunction.
Pure Autonomic Failure (PAF): A condition marked by a gradual decline in autonomic function, leading to symptoms such as low blood pressure, fainting, and difficulty regulating body temperature.
Autoimmune Autonomic Ganglionopathy (AAG): An autoimmune disorder where the body's immune system attacks the autonomic ganglia (clusters of nerve cells), impairing the communication between the nervous system and various organs.
Symptoms of Dysautonomia
The symptoms of dysautonomia can vary widely depending on the specific type of disorder and the individual affected. Common symptoms include:
Orthostatic Intolerance: Dizziness, lightheadedness, or fainting upon standing up.
Tachycardia: Abnormally rapid heart rate, especially when transitioning to an upright position.
Blood Pressure Abnormalities: Sudden drops or increases in blood pressure, leading to symptoms like fainting or headaches.
Digestive Issues: Nausea, bloating, or difficulty swallowing.
Temperature Regulation Problems: Sensitivity to heat or cold, excessive sweating, or feeling unusually hot or cold.
Fatigue and Weakness: Persistent tiredness and a general sense of weakness.
Causes of Dysautonomia
The causes of dysautonomia can be diverse and may include:
Genetic Factors: Some forms of dysautonomia, like familial dysautonomia, have a genetic basis.
Autoimmune Conditions: Disorders like autoimmune autonomic ganglionopathy involve the immune system attacking autonomic nerves.
Neurological Conditions: Neurodegenerative diseases such as multiple system atrophy can affect the autonomic nervous system.
Infections or Injuries: Certain infections or traumatic injuries can impact autonomic function.
Idiopathic: In some cases, the cause of dysautonomia is unknown.
Diagnosis
Diagnosing dysautonomia typically involves a thorough evaluation by a healthcare provider, which may include:
Medical History and Symptom Assessment: Detailed discussion of symptoms and medical history.
Physical Examination: Assessment of blood pressure, heart rate, and other vital signs in different positions.
Autonomic Function Tests: Specialized tests, such as tilt table testing or active stand tests, to evaluate how the autonomic nervous system responds to changes in posture.
Laboratory Tests: To rule out other conditions and identify potential underlying causes.
Imaging and Electrophysiological Studies: In some cases, imaging or nerve conduction studies may be used to assess the extent of autonomic dysfunction.
Management and Treatment
Management of dysautonomia focuses on alleviating symptoms and improving quality of life. Treatment strategies may include:
Medications: Drugs to regulate blood pressure, heart rate, and other symptoms. Examples include beta-blockers, fludrocortisone, and midodrine.
Lifestyle Modifications: Recommendations for diet, fluid intake, and physical activity to manage symptoms and improve overall health.
Physical Therapy: Exercises and strategies to improve physical conditioning and enhance tolerance to upright positions.
Cognitive Behavioral Therapy (CBT): To help manage symptoms related to stress and anxiety.
Supportive Measures: Measures such as compression garments or elevating the head of the bed to manage blood pressure and orthostatic intolerance.
Research and Future Directions
Ongoing research aims to better understand dysautonomia and develop more effective treatments. Key areas of focus include:
Understanding Pathophysiology: Investigating the underlying mechanisms of dysautonomia to develop targeted therapies.
New Therapeutic Approaches: Exploring novel medications and interventions to improve symptom management.
Patient Education and Support: Enhancing resources and support networks for individuals affected by dysautonomia.
Conclusion
Dysautonomia represents a complex and often challenging group of disorders affecting the autonomic nervous system. While there is no one-size-fits-all treatment, advancements in research and a comprehensive approach to management can help improve the lives of those affected. Early diagnosis and personalized care are essential for managing symptoms and enhancing quality of life for individuals with dysautonomia.
2 notes
·
View notes
Text
Professor Emeritus Peter Schiller, a pioneer researcher of the visual system, dies at 92
New Post has been published on https://thedigitalinsider.com/professor-emeritus-peter-schiller-a-pioneer-researcher-of-the-visual-system-dies-at-92/
Professor Emeritus Peter Schiller, a pioneer researcher of the visual system, dies at 92


Peter Schiller, professor emeritus in the Department of Brain and Cognitive Sciences and a member of the MIT faculty since 1964, died on Dec. 23, 2023. He was 92.
Born in Berlin to Hungarian parents in 1931, Schiller and his family returned to Budapest in 1934, where they endured World War II; in 1947 he moved to the United States with his father and stepmother. Schiller attended college at Duke University, where he was on the soccer and tennis teams and received his bachelor’s degree in 1955. He then went on to earn his PhD with Morton Weiner at Clark University, where he studied cortical involvement in visual masking. In 1962, he came to what was then the Department of Psychology at MIT for postdoctoral research. Schiller was appointed an assistant professor in 1964 and full professor in 1971. He was appointed to the Dorothy Poitras Chair for Medical Physiology in 1986 and retired in 2013.
“Peter Schiller was a towering figure in the field of visual neurophysiology,” says Mriganka Sur, the Newton Professor of Neuroscience. “He was one of the pioneers of experimental studies in nonhuman primates, and his laboratory, together with those of Emilio Bizzi and Ann Graybiel, established MIT as a leading center of research in brain mechanisms of visual and motor function.”
Recalls John Maunsell, the Albert D. Lasker Distinguished Service Professor of Neurobiology at the University of Chicago, who did postdoctoral research with Schiller, “Peter was the boldest experimentalist I’ve ever known. Once he engaged with a question, he was unintimidated by how exacting, intricate, or extensive the required experiments might be. Over the years he produced an impressive range of results that others viewed as beyond reach.”
Schiller’s former PhD student Michael Stryker, the W.F. Ganong Professor of Physiology at the University of California at San Francisco, writes, “Schiller was merciless in his criticism of weakly supported conclusions, whether by students or by major figures in the field. He demanded good data, real measurements, no matter how hard they were to make.”
Schiller’s research spanned multiple areas. As a graduate student, he designed an apparatus, the five-field tachitoscope, that rigorously controlled the timing and sequence of images shown to each eye in order to study visual masking and the generation of optical illusions. With it, Schiller demonstrated that several well-known optical illusions are generated in the cortex of the brain rather than by processes in the peripheral visual system.
Seeking postdoctoral research, he turned to his father’s friend, Hans-Lukas Teuber, who had just accepted an offer to be founding head of the Department of Psychology at MIT. Schiller learned how to make single-unit electrophysiological recordings from the brains of awake animals, which added a new dimension to his studies of the circuitry and mechanisms of cortical processing in the visual system. Among other findings, he saw that brightness masking in the visual system was caused by interactions among retinal neurons, in contrast to the cortical mechanism of illusions.
In 1964, Schiller was appointed assistant professor. Soon after, he embarked on productive collaborations with Emilio Bizzi, who had just arrived in the Department of Psychology. Schiller and Bizzi, who is now an Institute Professor Emeritus, shared an interest in the neural control of movement; they set to work on the oculomotor system and how it guides saccades, the rapid eye movements that center objects of interest in the visual field. They quantified the firing patterns of motor neurons that generate saccadic eye movements; paired with studies of the superior colliculus, the brain center that guides saccades in primates, and the frontal eye fields of the cortex, they outlined a fundamental scheme for the control of saccades, in which one system identifies targets in the visual scene and another generates eye movements to direct the gaze toward the target.
Continuing his dissection of visual circuitry, Schiller and his colleagues traced the connections that two different types of retinal cells, known as parasol cells and midget cells, send from the retina to the lateral geniculate nucleus of the thalamus. They discovered that each cell type connects to a different area, and that this physical segregation reflects a functional difference: Midget cells process color and fine texture while parasol cells carry motion and depth information. He then turned to the ON and OFF channels of the visual system — channels originating in different types of retinal neurons: some which respond to the onset of light, others that respond to the offset of light, and others that respond to both on and off. Building on earlier work by others, and inspired by recent discoveries of ways to pharmacologically isolate ON and OFF systems, Schiller and several of his students extended the previous studies to primates and developed an explanation for the evolutionary benefit of what seems at first like a paradoxical system: that the ON/OFF system allows animals to perceive both increments and decrements in contrast and brightness more rapidly, a beneficial attribute if those shifts, for instance, represent the approach of a predator.
At the same time, the Schiller lab delved further into the role of various parts of the cortex in visual processing, especially the areas known as V4 and MT, later steps in visual processing pathways. Through single-neuron recordings and by making lesions in specific areas of the brain in the animals they studied, they revealed that area V4 has a major role in the selection of visual targets that are smaller or have lower contrast compared to other stimuli in a scene, an ability that, for example, helps an animal unmask a camouflaged predator or prey. Strikingly, he showed that many variations in images that are important for perception have a delayed influence on the responses of neurons in the primary visual cortex, indicating that they are produced by feedback from higher stages of visual processing.
Schiller’s many significant contributions to vision science were recognized with his election to the National Academy of Sciences and the American Academy of Arts and Sciences in 2007, and, in his home country, he was made an honorary member of the Magyar Tudományos Akadémia, the Hungarian Academy of Sciences, in 2008.
Schiller’s legacy is also evident in his students and trainees. Schiller counted more than 50 students and postdocs who passed through his lab in its 50 years. Four of his trainees have since been elected to the National Academy of Sciences: graduate students Larry Squire and Stryker, and postdocs Maunsell and Nikos Logothetis.
His mentorship also extended to faculty colleagues, recalls Picower professor of neuroscience Earl Miller: “He generously took me under his wing when I began at MIT, offering invaluable advice that steered me in the right direction. I will forever be grateful to him. His mentorship style was not coddling. It was direct and frank, just like Peter always was. I remember early in my nascent career when I was rattled by finding myself in a scientific disagreement with a senior investigator. Peter calmed me down, in his way. He said, ‘Don’t worry, controversy is great for a career.’ But he quickly added, ‘As long as you are right; otherwise, well …’
Schiller’s creative streak did not just influence his scientific thinking; he was an accomplished guitar and piano player, and he loved building complex and abstract sculptures, many of them constructed from angular pieces of colored glass. He is survived by his three children, David, Kyle, and Sarah, and five grandchildren. His wife, Ann Howell, died in 1999.
#2023#Advice#Angular#Animals#approach#Arts#berlin#Born#Brain#Brain and cognitive sciences#brains#Building#career#cell#Cells#Children#college#Color#data#direction#Discoveries#election#experimental#explanation#eye#eye movements#Faculty#Full#Fundamental#how
2 notes
·
View notes
Text
UK researchers find Alzheimer’s-like brain changes in long COVID patients - Published Aug 30, 2024
LEXINGTON, Ky (Aug. 30, 2024) — New research from the University of Kentucky’s Sanders-Brown Center on Aging shows compelling evidence that the cognitive impairments observed in long COVID patients share striking similarities with those seen in Alzheimer’s disease and related dementias.
The study, published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, highlights a potential commonality in brain disorders across these conditions that could pave the way for new avenues in research and treatment.
The study was a global effort, funded by a multitude of grants from the U.S. National Institutes of Health, the Alzheimer’s Association and international organizations. The project also brought together experts from various fields of neuroscience.
Researchers at the UK College of Medicine led the study, including Yang Jiang, Ph.D., professor in the Department of Behavioral Science; Chris Norris, Ph.D., professor in the Department of Pharmacology and Nutritional Sciences; and Bob Sompol, Ph.D., assistant professor in the Department of Pharmacology and Nutritional Sciences. Their work focuses on electrophysiology, neuroinflammation, astrocytes and synaptic functions.
“This project benefited greatly from interdisciplinary collaboration,” Jiang said. “We had input from experts, associated with the Alzheimer’s Association International Society to Advance Alzheimer's Research and Treatment (ISTAART), across six countries, including the U.S., Turkey, Ireland, Italy, Argentina and Chile.”
Jiang and the collaborative team focused their work on understanding the “brain fog” that many COVID-19 survivors experience, even months after recovering from the virus. This fog includes memory problems, confusion and difficulty concentrating. According to Jiang, “the slowing and abnormality of intrinsic brain activity in COVID-19 patients resemble those seen in Alzheimer’s and related dementias.”
This research sheds light on the connection between the two conditions, suggesting that they may share underlying biological mechanisms. Both long COVID and Alzheimer’s disease involve neuroinflammation, the activation of brain support cells known as astrocytes and abnormal brain activity. These factors can lead to significant cognitive impairments, making it difficult for patients to think clearly or remember information.
The idea that COVID-19 could lead to Alzheimer’s-like brain changes is a significant development.
“People don’t usually connect COVID-19 with Alzheimer’s disease,” Jiang said, “but our review of emerging evidence suggests otherwise.”
The publication in Alzheimer’s & Dementia reveals that the cognitive issues caused by COVID-19 reflect similar underlying brain changes as those in dementia.
The study’s insights emphasize the importance of regular brain function check-ups for these populations, particularly through the use of affordable and accessible tools like electroencephalography (EEG).
The study not only highlights the shared traits between long COVID and Alzheimer’s, but also points to the importance of further research.
“The new insight opens avenues for future research and clinical practice, particularly in studying brain oscillations related to neural biomarkers of mild cognitive impairment in people with long COVID,” said Jiang.
One of the key findings is the role of astrocytes — support cells in the brain that have not been as thoroughly studied as neurons. The research suggests that damage or activation of these cells by COVID-19 can cause synaptic dysfunctions, leading to the abnormal brain activity observed in both conditions. This discovery is significant because it may help explain why EEG patterns in COVID-19 patients resemble those seen in the early stages of neurodegenerative diseases like Alzheimer’s.
Researchers believe this work could have a direct impact on patient care. They are advocating for routine EEG exams to detect early brain changes in both COVID-19 survivors and those at risk for cognitive decline.
“EEG patterns in COVID-19 patients resemble those seen in early neurodegenerative diseases,” said Norris.
“These similarities may be due to shared issues such as brain inflammation, astrocyte activity, low oxygen levels and blood vessel damage,” said Sompol.
By detecting these changes early, health care providers could potentially identify at-risk individuals sooner and implement interventions to prevent or slow the progression of cognitive decline.
As research continues, the team is particularly interested in how EEG monitoring can predict long-term outcomes in COVID-19 patients and assess the effectiveness of treatments aimed at preventing cognitive decline.
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers P30AG072946, P01AG078116 and R56AG060608. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Link to study: alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.14089
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator#covid news#long covid
26 notes
·
View notes
Text

Mapping human brain function is a longstanding goal of neuroscience that promises to inform the development of new treatments for brain disorders. Early maps of human brain function were based on locations of brain damage or brain stimulation that caused a change in function. Over time, this approach was largely replaced by technologies such as functional neuroimaging, which identify brain regions correlated with behaviors or symptoms. Despite their advantages, these technologies reveal correlation, not causation. This creates challenges for interpreting the data generated from these tools and using them to develop treatments for brain disorders. A return to causal mapping of human brain function based on brain lesions and brain stimulation is underway. New approaches can combine these causal sources of information with modern neuroimaging and electrophysiology techniques to gain new insights into the functions of specific brain areas. In this Review, we provide a definition of causality for translational research, propose a continuum along which to assess the relative strength of causal information from human brain mapping studies, and discuss recent advances in causal brain mapping and their relevance for developing treatments.
6 notes
·
View notes
Text
Finally got back to the heart doctor today. I had someone to advocate for me in the doctor's office and brief notes to talk about with the cardiologist, only to find out that I needed less bravery than I thought.
The nurse on the phone didn't give me the whole story.
Yes, I have a first degree heart block that's pretty much constant, but what she didn't tell me is that I also have an occasional 2nd degree type 1 heart block, an inappropriate sinus rhythm.
And even though it's only type 1, since I'm symptomatic--noticable skipped beats, dizziness and pre-syncope, fatigue, shortness of breath--they are sending me an electrophysiologist to figure out exactly where and why the arrhythmia is originating from, and to figure out if--and this is the kicker to my 23 year old self--my heart issues would be fixed if I had a pacemaker.
A pacemaker was brought up for me. At 23. Wow.
the electrophysiology study scares me a lot, it seems really involved and I'll still be partially awake for it, but hopefully it won't be that bad.
4 notes
·
View notes