#Gallbladder Function Tests
Explore tagged Tumblr posts
Text
#Gallbladder Function#Gallstones#Cholecystectomy#Bile Production#Bile Storage#Liver and Gallbladder#Gallbladder Disease#Cholecystitis#Gallbladder Pain#Fatty Liver#Gallbladder Removal#Ultrasound Gallbladder#Digestive Health#Biliary System#Cholelithiasis#Gallbladder Infection#Post-surgery Gallbladder Care#Gallbladder Polyps#Jaundice and Gallbladder#Gallbladder Function Tests#health & fitness
1 note
·
View note
Text
How are Gallstones Diagnosed?
Gallstones are diagnosed through various methods, including medical history assessment, physical examination, and diagnostic tests. A healthcare professional may inquire about symptoms, risk factors, and family history to evaluate the possibility of gallstones. Physical examination techniques, such as abdominal palpation, can help identify signs of tenderness or enlargement of the gallbladder. Diagnostic tests commonly used for gallstone diagnosis include ultrasound imaging, which provides a visual image of the gallbladder and any present stones, and blood tests to assess liver function and detect any associated complications. These diagnostic measures aid in accurately diagnosing gallstones and determining the appropriate course of treatment.
#Gallstones diagnosis#Gallbladder health#Gallstone symptoms#Medical history assessment#Physical examination#Diagnostic tests for gallstones#Ultrasound imaging#Liver function tests#Abdominal tenderness#Gallstone complications
0 notes
Text


**Health update**
So I never wanted to make another post like this but here I am.. I was hoping to just get better and never bring it up again.
To get those of you up to speed. I was diagnosed with CKD back in late 2021. I’ve been battling that for a while now. I’m actually doing really well in that regard. During a routine MRI in Nov 2023 for my kidneys we found what looked to be a hepatic steatosis and splenomegaly. It was later determined and I was diagnosed with hepatic tumors and splenomegaly. I also had a fairly large gallstone and what appeared to be a tumor/cyst on my gallbladder. We decided it was just better to remove my GB and the tumors all at the same time. So in January of this year I had laparoscopic cholecystectomy/tumor removal. That’s what the scars on my stomach are from. The tumors were tested and were benign. That was a huge relief. But it left my liver fairly damaged. I wasn’t to concerned about because your liver can and will heal itself. I recovered well and felt great.
Fast forward 9 months. I wasn’t feeling very well. So I made an appointment with my PCP and she wanted me to do a bloodwork panel. This is normal. We actually do blood once a month but really only check kidneys, thyroid, and hormones. So I did the panel and when the test results came in my Dr called me immediately. She ordered another AST/hepatic function panel for my liver, kidneys and pancreas.
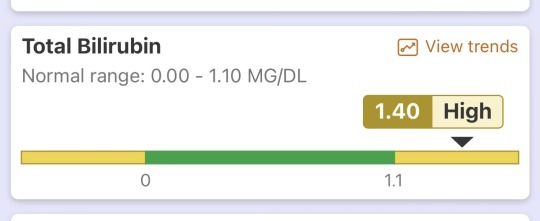
After those test results came in she had me come to her office. I was met with her and a Hepatologist. They broke the news to me that unfortunately my liver not doing well according to the bloodwork. My pancreas/kidneys are actually pretty ok rn which is cool. But my total bilirubin is 1.4 mg/dl. At 1.5 mg/dl total bilirubin is where we really start looking at the possibility of Cirrhosis. If you don’t know what that is. Google it. Now I’m not saying I have this rn but it seems to be looking that way 🫤
They were telling me they could see my bilirubin trending up over the course of the past few months of bloodwork. Also previously being diagnosed with Splenomegaly which is a tell tale sign of Cirrhosis apparently. They’re pretty sure I have it or will have it. They want to run more tests and see how bad or good it is and we’ll go from there. It seems like they have a pretty good plan. Also for those of you that are going to say get a second opinion.. I got a second and a third. They said the same thing go figure..
So again I find myself going in and out of the hospital again. I don’t wish this life upon anyone. It’s not fun. Being chronically/terminally ill is no fucking joke. If it’s not one thing it’s another. It’s tiring and I’m soo tired. Honestly I can’t wait until it’s all over.. forever.
Anyway I figured I’d give you a bit of an update on my health and such. A lot of you ask in my DMs. It’s hard to answer everyone so a post like this gets it out there. But yea if you made it this far thank you and I love you 🫶🏻
#im sick#still sick#always will be sick#if it’s not one thing it’s another#health#chronic illness#terminally ill#please dont feel sorry for me#I don’t want that#trans#transgender#trans pride#transisbeautiful#mtf#transgirl#girlslikeus#mtf hrt#maletofemale#transformation#trans woman#trans women#trans women are beautiful#transexual#actually trans#this is what trans looks like#trans people#trans positivity#mtf positivity#actually mtf#mtf pride
169 notes
·
View notes
Text
shoutout to the ER for performing a CT scan, saying that my non existent gallbladder is present and functioning on the results, ordering a nuclear medicine test for its functionality only for me to get here, tell them i have no gallbladder and the technicians are on my behalf pissed the fuck off at the emergency department for somehow missing that an entire organ of mine is missing. they double checked the CT scan results and confirmed that it very much did not show up on the scan at all.
great fucking job. no it's not like i want these medical tests to give me answers so i can find a way to lessen my suffering. it's not like I'm tired of being in pain. fucking thanks. i think your doctor needs to go back to fucking medical school if he can't fucking tell if an entire organ is present or not.
#i understand the gallbladder is small. i know. i don't need to be told this. that shouldn't impact any of this.#updates
109 notes
·
View notes
Text
Quick Health Update
The Ao3 curse has finally found me, folks.
I spent all night in the emergency room with severe upper right chest burning/pain that had been ongoing for over eight days (but had come and gone since January). My attending physician believed it was my gallbladder and I spent all night undergoing different tests to verify if I needed emergency surgery.
I didn’t need surgery (and it’s not my gallbladder).
That being said, I am incredibly tired, have many additional doctor appointments this week, and I have a funeral to go to this weekend.
Y’all will likely not see anything from me until next week. I need some rest and my brain can’t function enough to put the words in my head to the page.
I appreciate your patience and understanding during this time.
With love,
~ Poppy
47 notes
·
View notes
Text
some bad from today: my gallbladder looks fine in both structure and function, so nothing will be done about my last three months of food issues! hooray!
some good: the tests i've had done to tell me NOTHING weren't as expensive as i thought and i set up a payment plan earlier for them (bundled together bc they're from they same hospital)
10 notes
·
View notes
Text
thank you so much everyone who helped me i'm so grateful. this whole week after my diagnosis has felt so hopeless and scary but i'm so humbled by all the support that has come my way. i am trying my hardest to get healthy again because i don't want to die the way my mom did.
under the cut i am gonna put more about what i have been going through with my type 2 diabetes and fatty liver disease. i am going to be talking about food and eating patterns and somewhat disordered eating so tw for that in case you are curious.
i hope this can help some people though.
i have been very scared since my doctor told me i have fatty liver because i watched my mom die from cirrhosis of the liver - which is a real possibility for me now if i don't make changes.
i saw how awful the progression of that disease is.
when my mom was diagnosed she was already jaundiced and had full blown cirrhosis, which i did not understand at the time meant that it was irreversible and that she was absolutely going to die unless she recieved a live transplant. cirrhosis occurs when your liver has received so much damage that it has become scar tissue and cannot function any longer. your liver is an organ you cannot live without. if it is caught very early you have the option of a transplant, but since her disease had progressed so far her heart was not functioning properly and she had a 75% chance of dying on the operating table.
simple fatty liver usually does not cause symptoms and if it does, as with me, they are mild and can be ignored. this is why usually people do not know until it's too late and larger symptoms such as jaundice (yellow skin and eyes), red palms, swelling in the legs and stomach, confusion and hallucinations are present.
this has all scared me so much because i have ptsd from her illness and death, not only did i see all this happen to my mother very quickly- she was diagnosed in 2008 and died in 2010- but now i see it very differently. i understand now that she did not take her diabetes seriously enough, and taking her off the pedestal i have put her on has been hard. i remember how unhealthy she ate while diabetic, i remember how high her blood sugar was. i remember hiding bread and oreos from her. and now i understand that she must have had fatty liver and not known it, and because she already had hepatitis in the past AND was on a medication for depression known as cymbalta, her disease skyrocketed. she was not dieting, she was not exercising and she died without understanding how she got there so fast because non alcoholic fatty liver is SILENT until it's too late and it's not something doctors generally look for.
i do not blame my mother. she had a lot of mental and physical issues that i do not, and everyday i am so grateful that she raised me. but i now know that if they had tested her liver enzymes in say, 2005 or 2006, and told her what i know now, she may still be alive if she had changed her way of living. and that is hard.
when i was laying down for the gallbladder ultrasound there was something telling me it was my liver, and i imagined how scared she must have been in that situation but having no way to get better the way i still do. my mother loved me more than anything, and knowing she was going to die and leave me (her words) was something i know she felt guilty about until the final weeks of her life. i fully believe if she knew what i know, she would have changed.
i am not jaundice, i do not have serious symptoms except occasional discomfort in my abdomen. the craziest part is that this all happened on the anniversary of my mother's death, june 24th.
if she is still somewhere in existance, maybe she was warning me to change before it was too late.
the truth is until now i did not understand the connection between what you eat and your liver, especially if you are diabetic or prediabetic. i am trying really hard not to blame myself, but the truth is my diet for the last few years have been absolutely atrocious. i would wake up and have a sugary iced coffee and a chocolate croissant every day. for lunch i would have pizza or something fast and easy like that and when i got home i would have pasta almost every day. then i would have snacks like chocolate covered pretzels or a pint of ice cream like it was nothing.
if i had been more careful, maybe i wouldn't be where i am now. but the past is the past and truth be told i have an addiction to sugar. the first two weeks after my diabetes diagnosis i felt insane. i cried in the grocery store because i wanted to get candy and soda so bad. it was physically painful not to. but... now a month later those cravings are gone. i do not even WANT a ben & jerrys - as if something in my body switched. and that step was hard, but it has been worth it.
the hardest part has been finding food in the us that is actually healthy and not MARKETED to be healthy. these are different things and i learned that recently too.
i want to make it clear that i am not shaming how anyone eats. i am not trying to lose weight because i don't like looking fat. i actually realized i am going to miss my fat body as i start to slim down. but i have to do this to live- this is not the case for everyone but it is for me.
now, if you made it this far i want to tell you some warning signs that i was seriously ill that i ignored for months.
1. i noticed random parts of the skin my body getting darker, specifically beneath and between my breasts and behind my neck. this is a sign of diabetes. i also noticed my skin would tear very easily, specifically my hands.
2. i had to pee all the time. like. literally every 15-20 minutes. at one point i was getting up to pee about 7 times a night. and when i did it smelled like liquid cane sugar. this was my first "oh shit" moment.
3. this is taboo to talk about but i suspected i was diabetic when i suddenly got a really severe yeast infection.
4. my skin was breaking out like it never had. i also had light colored stools.
5. oddly dizzy and feeling weird. down the list bc everyone knows this one.
6. lastly. pain in my upper right stomach, under the ribs. if you feel pain here and are either diabetic or prediabetic, ask your doctor to check your liver enzymes and if you cannot see a doctor consider making changes to your life style within your personal capacity.
anyway, thank you for helping me and if you read this thank youuu for that as well and i hope it's somewhat helpful to someone out there 🫶🏻
51 notes
·
View notes
Text
PATIENT MEDICAL RECORD SURGICAL REPORT #957
Patient Name: Misha Lupical Age: 14 Sex: Male Date of Surgery: ██ ██ ███ Surgeons: Doctor Paene Lupical, Petya Yordanovich (cardiologist) Anasthesiologist: Malcolm Grey Procedure: Organ Transplantation and Cardiovascular Augmentation
PRE-OP NOTES
Diagnosis: Multiple organ failure (lungs, gallbladder, liver, kidneys, spleen) due to malignancy and systemic toxicity; cardiovascular inefficiency requiring augmentation
Planned Procedure:
Organ Transplants: - Gallbladder, lungs, liver, kidneys, spleen excision and synthetic organ implantation - Major arterial and venous reinforcement with synthetic materials - Connection of transplanted organs to neurological implant
Cardiovascular Augmentation: - Secondary four-chamber heart implantation (continuous steady-state circulation with pre-coded heart rates for rest and different exertion modes)
Structural EnhancementsL - Endoskeletal reinforcement with flexible carbon-fiber mesh (beneath ribs)
Anesthesia plan: - General anesthesia with neuromuscular blockade - Continuous hemodynamic and neurological monitoring - Peripheral nerve stimulation for post-op functional assessment INTRA-OP NOTES:
Anesthesia Induction: - Patient intubated and placed under general anesthesia by anesthesiologist Malcolm Grey - Central venous access obtained (catheter inserted in subclavian vein) - Cardiopulmonary monitoring initiated
Intra-operation Actions: - Diseased lungs, liver, spleen, gallbladder, and kidneys removed - Synthetic organ replacements positioned and vascular connections established by Doctor Petya Yordanovich - Major arterial and venous structures reinforced with synthetic conduits - Endoskeletal mesh placed beneath ribcage; no interference with respiratory motion detected
Complications: - Initial rejection response to liver implant triggered hypercytokinemia, requiring instant immunosuppressive therapy - Temporary hypotension following spleen replacement; stabilized with IV fluids - Unexpected clot formation near secondary heart implantation site, requiring immediate removal and anticoagulant administration - Delayed vascular integration of synthetic kidneys, leading to brief renal hypoperfusion; resolved with perfusion adjustment
Closure & Recovery: - Hemostasis confirmed across all surgical sites - Incisions closed with bio-compatible sutures and synthetic dermal grafts - Patient transferred to ICU for post-op observation POST-OP NOTES:
Immediate Post-Op Status: - Patient successfully extubated, spontaneous respiration intact - Secondary heart maintaining consistent circulation with expected oxygen levels (confirmed by Dr. Petya Yordanovich) - Moderate pain and discomfort noted, managed with analgesics
Complications: - Acute hypertension episodes likely cause by vascular reinforcement adaptation; managed with a vasodilator medication - Persistent metabolic imbalance due to synthetic liver requiring enzyme therapy for stabilization - Mild pulmonary edema in left synthetic lung, resolving with respiratory support Ongoing Monitoring & Adjustments: - Secondary heart function optimization for long-term stability - Periodic enzyme regulation assessment for synthetic liver - Renal output monitoring for continued integration - Regular pulmonary function tests for synthetic lung efficiency
Discharge Plan: - Estimated hospital stay - 12-16 days - Physical rehabilitation for systemic adaptation (done by Doctor Lea Anderson and physical therapist John O'Nella) - Regular biomonitoring for cardiovascular and organ function stability - Regular neural implant monitoring to check for the integration of transplanted organs and their proper function
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
tags: @tobeyinabox
2 notes
·
View notes
Text
It's been a long rough week with a senior cat who won't eat, getting hospitalized, and has culminated in her having surgery for a feeding tube insertion. Her scans came back tumor free, though her liver enzymes look awful, and her gallbladder tests are a little wonky.
Amazingly for a 14 year old cat, her kidney function is fantastic, and all the rest of her blood work looks great. The vets all love and adore her and think she's perfect.
Hopefully she'll start eating soon, but for now, on the exciting adventure of tube feeding a cat.
Cat tax:

3 notes
·
View notes
Text
Like I planned on my costume months ago but it feels weirdly apt after all the tests and procedures and surgeries I’ve gotten this year, it feels like I haven’t been in control of my own body. They tell me what I should eat and when I should eat and they stick things into me and take things out and it’s…a lot.
But I DO feel so much better with my treacherous, barely functioning gallbladder out, so hopefully once I stop with this plague I caught at the festival I’ll feel even better.
#last year wasn’t so bad#like I had a cavity filled I think??#and I had two endoscopies#but mostly it was normal#not like 2022 where I got all these surgeries and tests and procedures done#knock on wood we fixed everything or found says to manage it#and now I can just maintain this
2 notes
·
View notes
Text
*Health complaining ahead*
I'm the heaviest I've ever been and my health is fucked. I feel gross so I eat like shit, so I feel gross.. and what sucks is the things my body defines as Shit are not historically the things my brain would call Shit. Like just a sandwich or noodles make my whole system lose its mind.
I've been nauseous after meals on and off for over a month. My esophagus feels raw from acid. My stomach hurts, like not just a tummy ache but actual pain.
They didn't find anything on the ultrasound except the hiatal hernia we already knew about. And they're still telling me that's not the problem.
They put me on Voquezna which I loved, until it turned my pee brown. I think for that 10 days my GI system was healing, but it would have destroyed my kidneys to stay on it. They put me back on pantoprazole, aka the thing that wasn't working.
They ordered a gallbladder test for hopefully next week but if that's the issue I'm prob looking at surgery.
Last year the told me I had SIBO, gave me a round of Xifaxan and didn't bother with a follow up. They also told me I have a wheat allergy, but they couldn't confirm Celiac or EOE on the EGD. Just the hernia which again, apparently, is not the problem.
I didn't make any diet changes but now I think I need to. There's a box of gluten free spaghetti lurking in our cupboard.
I guess the reason I'm scared, the reason I haven't tried diet changes, is because right now I'm eating for comfort. I'm eating whatever I think won't come back up. I'm gaining weight even though I'm on this horrible starve-scarf rollercoaster.
And I'm scared that if I don't like the food I have to eat, that I just won't eat. Which thanks to genetic hypoglycemia, is basically a choice to stop functioning. Signing up to be incapable. Taking my brain out of my head and walking away.
So idk. I'm a hair frustrated. My mom joked that I need a team like Dr House to do a differential on me, but that's either out of my price range or not a thing that exists.
2 notes
·
View notes
Text
Choosing the Right Gastrointestinal Tract Drug – Factors to Consider
The gastrointestinal (GI) tract is a complex system responsible for digestion and absorption of nutrients. Given its critical function, disorders affecting the GI tract can significantly impact overall health and quality of life. Selecting the right medication to treat these conditions is essential for effective management and recovery. Centurion HealthCare, a leading gastrointestinal tract drugs supplier in India, offers a range of high-quality medications designed to address various GI disorders. In this article, we will explore the factors to consider when choosing the right gastrointestinal tract drug, and why Centurion HealthCare stands out in the best pharmaceutical industry in India.

Understanding Gastrointestinal Tract Disorders
GI tract disorders encompass a wide range of conditions affecting different parts of the digestive system, including the esophagus, stomach, intestines, liver, pancreas, and gallbladder. Common GI disorders include:
Gastroesophageal Reflux Disease (GERD)
Peptic Ulcer Disease
Irritable Bowel Syndrome (IBS)
Inflammatory Bowel Disease (IBD)
Hepatitis
Pancreatitis
Each condition requires specific treatment strategies and medications to manage symptoms, promote healing, and prevent complications.
Factors to Consider When Choosing a Gastrointestinal Tract Drug
Choosing the right drug for treating GI disorders involves multiple factors, including the specific condition, the patient’s medical history, and potential side effects. Here are key considerations:
1. Accurate Diagnosis
An accurate diagnosis is the first step in selecting the appropriate medication. Physicians use various diagnostic tools such as endoscopy, colonoscopy, imaging studies, and laboratory tests to identify the specific GI disorder. Understanding the underlying cause and severity of the condition is crucial for effective treatment.
2. Mechanism of Action
Different gastrointestinal tract drugs work through various mechanisms to achieve therapeutic effects. Understanding how a drug works helps in selecting the most suitable option. Common mechanisms include:
Antacids: Neutralize stomach acid, providing quick relief from heartburn and indigestion.
Proton Pump Inhibitors (PPIs): Reduce the production of stomach acid, effective in treating GERD and peptic ulcers.
H2 Receptor Antagonists: Decrease acid production by blocking histamine receptors in the stomach lining.
Prokinetics: Enhance gut motility, useful in conditions like gastroparesis.
Antispasmodics: Relieve intestinal cramps and spasms, often used in IBS treatment.
Anti-inflammatory Drugs: Reduce inflammation in the GI tract, essential for managing IBD.
3. Efficacy and Safety
The efficacy and safety profile of a drug are critical factors in the decision-making process. Clinical trials and real-world studies provide valuable information on a drug’s effectiveness and potential side effects. Physicians must weigh the benefits against the risks to ensure the chosen medication offers the best possible outcome for the patient.
4. Patient-Specific Factors
Each patient is unique, and various individual factors can influence drug selection. These include:
Age: Certain drugs may be more suitable for children, adults, or the elderly.
Medical History: Pre-existing conditions, such as kidney or liver disease, can affect drug metabolism and tolerance.
Allergies: Patients with known drug allergies must avoid medications that could trigger adverse reactions.
Concurrent Medications: Drug interactions can impact efficacy and safety, requiring careful consideration of all medications the patient is currently taking.
5. Route of Administration
The route of administration can affect the drug’s efficacy and patient compliance. Common routes for GI drugs include:
Oral: Tablets, capsules, and liquids are convenient for most patients.
Intravenous: Used in severe cases or when oral administration is not feasible.
Topical: Suppositories and enemas are used for localized treatment in the lower GI tract.
6. Cost and Availability
Cost can be a significant factor, especially for long-term treatments. Generic versions of drugs often offer the same efficacy as brand-name medications at a lower cost. Availability of the drug in the local market is also crucial to ensure uninterrupted treatment.
Centurion HealthCare: Leading the Way in GI Tract Drug Supply
Centurion HealthCare has established itself as a premier gastrointestinal tract drugs supplier in India, renowned for its commitment to quality, innovation, and patient care. Here’s why Centurion HealthCare is a trusted name in the best pharmaceutical industry in India:
1. Comprehensive Product Range
Centurion HealthCare offers a wide range of gastrointestinal tract drugs, catering to various GI disorders. Their product portfolio includes antacids, PPIs, H2 receptor antagonists, prokinetics, antispasmodics, and anti-inflammatory medications, ensuring comprehensive treatment options for healthcare providers.
2. Quality Assurance
Quality is at the heart of Centurion HealthCare’s operations. The company adheres to stringent quality control measures, from raw material sourcing to final product testing, ensuring that every medication meets international standards for safety and efficacy.
3. Research and Development
Centurion HealthCare invests heavily in research and development to stay at the forefront of pharmaceutical innovation. Their R&D team continuously works on developing new formulations and improving existing products to address emerging healthcare needs.
4. Patient-Centric Approach
Understanding that each patient is unique, Centurion HealthCare adopts a patient-centric approach in drug development and supply. Their medications are designed to provide maximum therapeutic benefit with minimal side effects, enhancing patient outcomes and quality of life.
5. Global Reach
As a leading gastrointestinal tract drugs supplier, Centurion HealthCare has a robust distribution network that ensures their products are available not only across India but also in international markets. Their commitment to excellence has earned them a reputation as a reliable partner for healthcare providers worldwide.
6. Affordability
Centurion HealthCare is dedicated to making high-quality medications accessible to all. Their cost-effective solutions, including generic versions of popular GI drugs, help reduce the financial burden on patients while maintaining high standards of care.
Conclusion
Choosing the right gastrointestinal tract drug involves careful consideration of various factors, including accurate diagnosis, mechanism of action, efficacy, safety, patient-specific factors, route of administration, and cost. Centurion HealthCare, as a leading gastrointestinal tract drugs supplier in India, excels in providing high-quality, effective medications that cater to the diverse needs of patients with GI disorders.
With a commitment to quality, innovation, and patient-centric care, Centurion HealthCare stands out in the best pharmaceutical industry in India. Their comprehensive product range, stringent quality assurance, advanced R&D, global reach, and affordability make them a trusted partner for healthcare providers seeking reliable solutions for GI tract disorders.
By choosing Centurion HealthCare, you can be confident in the quality and efficacy of the medications you are prescribing or consuming, ensuring the best possible outcomes for gastrointestinal health.
#Best Indian pharma industry 2024#Best pharmaceutical industry in India#Gastrointestinal tract drugs supplier#Gastrointestinal tract drugs supplier in India
3 notes
·
View notes
Text
So, I hadn't realized this, but it looks like I haven't really said much about my progressive illness, ME/CFS, on tumblr post-2017. And I imagine that as I post here more again, I'll encounter people who are unfamiliar with me, so I'll try to give a synopsis:
I started having increasingly frequent headaches and then constant burning in my eyes in high school, which we might have payed more attention to if, in my senior year, we hadn't discovered a congenital malformation in my brain that would end up either killing me or permanently damaging my brain if not removed. Before going off to college, I had a craniotomy (surgical procedure where they cut open your skull; I have a big scar under my hair) to remove it that went well.
In college the headaches became one singular headache that just didn't ever end, and the pain started expanding down my body. We started paying attention at this point, but were still kind of distracted as my anxiety and depressive disorders were discovered and diagnosed and I started treatment for them that went well.
I took a medical leave of absence as the headache grew worse, I struggled in school for a mystery reason that I now know was ADHD, and I developed gallstones (I ended up having my gallbladder removed). Over the next couple years, the headache increased to a migraine with the extra symptoms migraines involve and the pain expanded to encompass my entire body. In 2016, I then started experiencing Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, which I was lucky enough to be diagnosed with 6 months into my fatigue symptoms. As my fatigue increased, my cognitive function was impaired and it became increasingly rare that I was able to think clearly enough to draw, hence why I posted very little art for a few years.
If you've kept up on the Long Covid epidemic, you've probably heard about ME/CFS, and so you may already know that ME/CFS has no existing treatment or cure. All you can do is desperately try to treat your symptoms, struggling through the barrier of doctors completely unfamiliar with the illness, who are also often unwilling to educate themselves and persistent that you must actually have something they're already familiar with instead.
I've had very little success treating the pain despite trying everything the various neurologists I've seen over the years have thought to try. (if it's something with real medical evidence behind it, I can guarantee I've tried it and I've also been tested for like...every immune disorder.) I currently get 9 take-as-needed doses of a medication that lasts about 2 hours and ever so slightly decreases my pain most of the time (sometimes it doesn't work at all). And that's all I have to go on for 25 days. Again, my pain is unending. I never don't have a migraine. I'm just using my migraine meds to take the edge off when it gets particularly bad. I do have meds I take for symptoms like nausea and digestive issues that don't get rid of them, but do lessen them.
But the biggest thing was I started Low Dose Abilify for the cognitive fatigue in 2021. It actually worked and helped a little bit with physical fatigue as well. The difference was quickly outwardly apparent even at a very low dosage, not to mention inwardly apparent to myself. I've slowly titrated up, in between trying other medications for my symptoms, over the past couple years, and in January 2023 realized that my cognitive function had improved enough that I could regularly draw again and physically could sit up long enough to do so, even though I'm still forced to do so from my bed, which is why I now draw on an ipad. As far as I can tell, this is due to the combination of Abilify and the iron infusions I now get. I'm currently navigating what I am now capable of, and that means experimenting with making art regularly again. -Teaset
13 notes
·
View notes
Text
So what do I do when the only med that’s actually gotten rid of my pain is an opioid. Ibuprofen doesn’t work. Otc pain meds do not work. I take the “limit” a day. I try not to do it all in one sitting. Migraines, back pain, joint pain, pain from a gallbladder they refuse to take out because I don’t have visible stones (literally told, “well it’s probably just not working right” and getting no help). My shoulders hurt. My neck hurts. My muscles ache. I stretch and try and work through it. Resting doesn’t help. Too long in bed makes me hurt, and that’s if I can sleep.
There’s not a natural option I’ve found. 1. I’m allergic or at least extremely sensitive to weed, not to mention it’s illegal in my state and I have a job that drug tests. 2. wtf natural thing even works. I haven’t found shit.
They won’t prescribe me stronger pain meds. I can still go to work, still function, so “obviously” I’m not in that much pain right? Just take ibuprofen. Get some rest. Exercise (even tho that also causes even more excruciating pain and then add even more exhaustion).
So wtf do I do?
#mushroomwillow rambles#chronic pain#chronic pain solutions#chronic pain is a bitch#medication alternatives#chrinic illness#chronic fatigue
5 notes
·
View notes
Text
the beginning of the end.
I’ve always found comfort in writing. There’s something therapeutic about it. Being able to put your thoughts down on paper, releasing all that’s scrambling around in your head - it’s nice. It also helps to organize my thoughts and to process them too. So, that’s what I’m going to do - put my journalism degree to use (finally!!!) and write. There’s been a lot going on in my life lately and I need to get it all out of my head somehow. So here we are - a new blog. I don’t think I’ve had a blog since I was in middle school or something. Remember LiveJournal? Is that still a thing?
Anyways, If you’re uncomfortable with the female anatomy and its functions then please move on, this story or this blog isn’t for you.
But, I’m finally at the beginning of the end. The end of monthly pain that I’ve suffered from since I was about 13 years old. The end of torturous periods. The end of sleepless nights doubled over willing and praying that the cramps would stop. The end of sitting at my desk during work, sweating my ass off because my body is in so much pain and it’s taking all that it can out of me. The end of wondering if I can make it through a social event without feeling like I want to die. Hoping and praying that I’m doing enough on the outside to mask the pain - making sure that everyone else around me has no idea that I’m hurting because I don’t want to be a burden or ruin anyone’s plans, moods, etc. The end of spending money on feminine products, spending money on heating pads, remedies, medications - all of which never really solved anything.
How did we get here? How did I get to the beginning of the end? Well, about a year ago I started experiencing some strange pains in my stomach. Pain that kept me up at night. There was nothing that made it better, but nothing that made it worse either. Just a constant pain lingering on the lower right side of my abdomen. I thought it could have been appendicitis. Or, perhaps it’s just some gas? Or - maybe something is up with my gallbladder. Maybe my IUD was out of place. But no, none of that. Nothing ever showed up on X-rays, tests, ultrasounds, or blood work to indicate an issue.
So, I carried on.
Until about a month ago.
One morning in October, I woke up with the worst cramps I’ve ever had in my life. We’re talking 15/10 on a scale of 10. The pain had me pretty messed up. I know I logged into my computer to work that day - but I also remember only laying down on my beanbag chair in my office and squeezing a pillow so tightly, hoping the pain would go away. After laying with a heating pad and loading up on a large amount of ibuprofen, I was finally able to call my OBGYN’s office. All I wanted at that point was to talk to a nurse, to have it documented that I was in a lot of pain and to make sure it was on my record so that my gynecologist and I could talk about it during my annual wellness exam, that was only a few weeks away. The nurse couldn’t have been any more sympathetic to what I was going through. She could tell in my voice that I was uncomfortable. She took down my information, wrote down all that I was dealing with, and then spoke to my doctor. My doctor recommended an ultrasound - mostly to check and make sure that my IUD was in its right spot, but to also see if something else might be causing my discomfort.
So, a week later, I had my ultrasound appointment.
Now, this isn’t any normal ultrasound. This was a transvaginal ultrasound. Doesn’t sound fun, does it?
It’s not.
Let me break it down for you. It’s a stranger, with a wand, probing around your private parts for a good 45 minutes and taking pictures of your insides. She’s not really explaining what she’s looking at, but instead trying to have a discussion about what halloween costume she’s going to wear that weekend. It quite frankly was the worst 45 minutes of my life. I hated every moment of it. While the tech was trying to make it as easy and comfortable as possible for me - it wasn’t. It was painful. All I could do was stare at the ceiling and try my hardest not to react to any movements by her or cry.
Once it was over, the waiting game began.
I had an appointment scheduled with my gynecologist a week and a half after that ultrasound took place. It was a long 10 days. But that appointment literally changed EVERYTHING.
My doctor and a surgeon reviewed my ultrasound. They were able to determine a few things. First,I had 2 different diseases that I was diagnosed with - endometriosis and adenomyosis. Second, I likely would never be able to have children. Third, what I thought was ‘normal’ (aka the horrible cramps and all the other exponentially worse experiences of being a woman on a monthly basis) - was and is not normal at all. But, with all that bad news, I FINALLY had answers on why I have been suffering most of my life.
For those of you who don’t know, endometriosis is a disease where the lining/tissue of your uterus grows outside of your uterus. The tissue can be found in the fallopian tubes, on the ovaries, on many different parts of your body. Every month, when that tissue sheds from the uterus (your period), the tissue everywhere else in the body has nowhere to go to escape, causing pain. The hormones released by your ovaries triggers the endometriosis, causing pain. Adenomyosis takes it a step further - that same tissue - (again, which should ONLY be in your uterus) actually grows within the muscles and walls of the uterus. So every time hormones are released, or your uterus contracts (cramps) - it squeezes that tissue in the muscles making the pain 1000000000x worse than ‘normal’ period cramps. (or so I’m told. I can’t tell you what a normal period cramp feels like.)
So great. I finally have a diagnosis. It actually gave me some relief. I suddenly have an explanation for what I’ve been going through. I no longer feel crazy for complaining about how bad my cramps are. I no longer have to gaslight myself (I’m really good at this) into thinking that it’s all in my head, that it’s not ‘that’ bad, etc. I actually have a medical diagnosis to explain all that’s happening. I have tons of research to do! I can learn how to live with this and have a normal life! Right?
Well… sort of.
You see, while medications can help with endometriosis and you can even have a surgery to have it scraped away from your body and get some relief - the relief may not be permanent. The only way for it to totally go away is naturally, through menopause. Which in reality could be 10, 15, 20, maybe even 30 years away. But, there is no medicine to help fix adenomyosis. Again, I could wait for menopause for the adenomyosis to go away too.
But, the only way to fix adenomyosis is through surgery.
By removing my uterus.
A hysterectomy.
Hysterectomy. That’s a pretty big word. That’s a pretty big deal. There’s a lot of finality with a hysterectomy. No more periods - which in turn means no more pain. It also means never being able to have children. That’s okay too - I never had a desire to have children, and thankfully neither does my husband. But in a weird way, it also feels like a bit of an identity crisis. Like a loss of a part of my femininity. And that’s been a bit of a struggle. And I think I’ll eventually talk about these things in other posts in the future.
But I was faced with this decision - do I medicate the endometriosis and deal with the adenomyosis until menopause, or do I get the hysterectomy and live my life free from monthly pain?
For me, it was a simple choice. I chose hysterectomy.
My hysterectomy will be scheduled soon. I met with my surgeon a couple of weeks ago.. He’s really great. I feel comfortable with him and I feel comfortable with my decision. This decision will ultimately improve my quality of life. It will make my life a hell of a lot easier and will allow me to enjoy life to the fullest.
I never would have imagined going through this surgery, especially at 35 years old. There have been many times when I’ve had cramps where I’ve thought “can’t I just get rid of it all?!” And now, finally, I can.
You might be wondering why I am sharing this. Well, to be completely honest, I hope that I will be able to help others who are going through the same thing or, receive this diagnosis. Especially younger women. I hope that I can help them stand up and advocate for themselves and their health. I’ve been dealt a bad hand when it comes to doctors as of late and if I didn’t advocate for myself and also take the time to research doctors to make sure I have nothing but the best from here on out - who knows where I would be. I also hope that this will help me to connect to other women who may have already gone through all of this. To find others who UNDERSTAND. It can feel very isolating when you’re sick or have a sickness and no one really understands. I also hope it will help me process all of this. This is a major surgery. I’m having multiple ORGANS removed from my body. That’s crazy. That’s something that I’m still having a hard time wrapping my head around.
So, I hope being able to write about this, the process, my feelings, my recovery - will just help to make it that much easier for me. I have a lot on my mind surrounding this procedure and a lot that I want to discuss.. There’s a lot of what ifs and there are a lot of fears. But there’s also hope. So while this is the beginning of the end of my relationship with my uterus, it will also bring a new beginning to my life.
Excited to start the countdown til I can say, “See you later, ovulater!”
6 notes
·
View notes
Text
When I was 19 I experienced biliary dyskinesia. I collapsed on the bathroom floor from severe abdominal pain and fought the urge to call an ambulance because of the cost and called my ex-mother in law instead. She thought I was being dramatic but took me to a walk in clinic and they said nothing was wrong. I threw up excessively; 1 sip of water thrown up in 30 seconds and every 20 minutes from nothing at all. A couple of days in I went to the ER and was told “well you’re 19 and 135lbs, it couldn’t possibly be your gallbladder” and wouldn’t test it. They sent me home with a hefty dose of painkiller and I thought I was better for the next 24 hours, then straight back into horrendous pain.
For 2 1/2 weeks there were constant ER and clinic visits. I couldn’t eat or drink anything and lost a significant amount of weight, I took baths 5+ times a day to soothe the pain and ate Tylenol like it was candy and was lucky if I could keep it down. I started throwing up coffee grounds that they said wasn’t blood. I couldn’t sleep either, waking up multiple times to throw up and cry, but all the doctors kept saying over and over was “we don’t know what’s wrong” and “it could be stress” or “let’s run some tests to see if it’s ulcers” but refused to check for my gallbladder.
Finally, after they were annoyed with me showing up complaining, they said “let’s run a HIDA scan” and, lo and behold, my gallbladder was only functioning at 11%. Shocker!!! Who could have known??!!
[I think I should mention that after the removal surgery they woke me up and immediately made me get dressed and leave within 30 minutes. I was barely conscious.] [also the surgeon looked at me curled up and crying on his examination table the day before surgery and told me I didn’t have to have it removed if I didn’t want to and it would pass on its own]
Anyway, TL;DR I went through the worst pain of my life and thought I was dying and the doctors didn’t care.
Doctors should snark at each other more, be a bit mean. Not for no reason, mind you. But if five doctors blow me off about symptoms and doctor number six FINALLY runs actual tests and gets a diagnosis, I think it should be Doctor Six's right to call up the other five and tell them they're lazy pieces of shit. That should be socially encouraged. Those first five doctors clearly can't listen to patients, but maybe another doctor might finally get to them.
#my ex husband told me after everything that he thought I was faking it so I wouldn’t have to work#there’s a reason we’re divorced and that’s just 1 out of 1000
78K notes
·
View notes