#What are the first symptoms of kidney disease?
Text
Disabilities that You Should Consider Representing in Your Writing More… part 1
[large text: Disabilities that You Should Consider Representing in Your Writing More… part 1]
While all disabilities are underrepresented in basically all sorts of media, it’s hard to not notice the trend in what disabilities make up the majority of representation. It’s especially visible when having a blog like this, where we can see what disabilities writers even consider including in their writing, and which ones never come up.
One in four people are disabled. With eight billion people alive it means there’s a lot of disabled people, and a lot of reasons why they are disabled in the first place - but this diversity is rarely represented, even on this blog, and anyone who has been following for a while has probably noticed that fact.
To be blunt: there are disabilities other than “amputee” and “(otherwise invisibly disabled) mobility aid user”. Does that mean that it’s wrong to write either of those? Of course not, and we don’t want to imply that it is. Does it mean that either of these have a ton of good representation? Hell no. Does it mean that when you are deciding on what to give your character, you should think beyond (or along! people can be multiply disabled!) just those two? Absolutely. Disability is a spectrum with thousands of things in it - don’t limit yourself for no reason and embrace the diversity that’s built into it instead.
This is, simply, a list of common disabilities. This is just a few of them, as this is part one of presumably many (or, at least three as of right now).
By “common” we rather arbitrarily decided on “~1% or more” - so at least 1 in 100 people has the disabilities below, which is a lot. Featuring!: links that you should click, sources of the % that are mostly just medical reports and might be hard to read, and quick, very non-exhaustive explanations to give you a basic idea of what these are.
Intellectual disability (about 1.5%)
Intellectual disability is a condition we have written about at length before. It’s a developmental disability that affects things such as conceptualization, language, problem-solving, or social and self-care skills. ID can exist on its own or be a part of another condition, like Down Syndrome, Congenital Iodine Deficiency, or Fetal Alcohol Spectrum Disorders. This post covers a lot of basic information that you might need.
We have an intellectual disability tag that you can look through!
Cancer survivors (5.4% in the US, about 0.55% worldwide)
A cancer survivor is a pretty self-explanatory term. There is a lot of types of cancer and some of them are very common while others are very rare, which makes this a very diverse category. Cancers also have different survival rates.
While not every survivor will have disabling symptoms, they definitely happen. Most of the long-term side effects are related to chemotherapy, radiation, and other medication, especially if they happened in children. They can include all sorts of organ damage, osteoporosis, cognitive problems, sensory disabilities, infertility, and increased rate of other cancers.
Other effects include removal of the affected area, such as an eye, a spleen, breasts, or the thyroid gland, each of which will have different outcomes.
Cancer, and cancer treatments, can also result in PTSD.
Diabetes (about 8.5%, ~95% of that are type 2)
Diabetes is a group of endocrine conditions that cause hyperglycemia (high blood sugar) for various reasons depending on the type. The vast majority of people have type 2 diabetes, which can cause fatigue, poor healing, or feeling thirsty or hungry. A diabetic person will use insulin when needed to help manage their blood sugar levels.
There are many complications related to diabetes, from neuropathy, to retinopathy, and chronic kidney disease, and there's a lot of disabilities that coexist with diabetes in general!
You might want to check out the #how to write type 1 diabetes tag by @type1diabetesinfandom!
Disabling vision loss (about 7.5%)
Blindness and low vision are a spectrum, ranging from total blindness (around 10% of legally blind people) to mild visual impairment.
Blindness can be caused by countless things, but cataracts, refractive errors, and glaucoma are the most common. While cataracts cause the person to have a clouded pupil (not the whole eye!) blind eyes usually look average, with strabismus or nystagmus being exceptions to that fairly often (but not always).
Trauma isn't a common cause of blindness, and accidents are overrepresented in fiction.
A blind person can use a white cane, a guide dog or horse, or both. Assistive solutions are important here, such as Braille, screenreaders, or magnifying glasses.
We have a blindness tag that you can look through, and you might want to check out @blindbeta and @mimzy-writing-online.
Psoriasis (about 2-4%)
Psoriasis is a chronic skin condition with multiple subtypes; it can cause intense itching, pain, and general discomfort, and often carries social stigma. It’s an autoimmune and non-contagious disability that affects the skin cells, resulting in raised patches of flaky skin covered with scales.
It often (30%) leads to a related condition, psoriatic arthritis, which causes joint pain, tenderness, and fatigue, among other things.
Stroke survivors (0.5-1%)
A stroke survivor is a person who has survived any kind of stroke (ischemic, hemorrhagic, etc.). While the specific symptoms often depend on the exact location on where the stroke happened, signs such as hemiplegia, slurred speech, vision problems, and cognitive changes are common in most survivors to some degree. When someone has a stroke as a baby, or before they are born, it can result in cerebral palsy, epilepsy, and other disabilities.
We have a brain injury tag that you can look through!
Noonan Syndrome (about 0.1-1% - mild is 1%, severe 0.1%)
Noonan Syndrome is a disability that is almost never mentioned in any context, but certainly not around the topic of writing disabled characters. It’s a congenital condition that can cause cardiomyopathy, chronic joint pain, hypermobility, short stature, facial differences such as ptosis, autism, and various lymphatic problems among other things. Some people with Noonan Syndrome might use mobility aids to help with their joint pain.
Hyperthyroidism (about 1.2%)
Hyperthyroidism is a condition of the endocrine system caused by hormone overproduction that affects metabolism. It often results in irritability, weight loss, heat intolerance, tremors, mood swings, or insomnia.
Undertreated hyperthyroidism has a rare, but extremely dangerous side effect associated with it called a thyroid storm, which can be fatal if untreated.
Hypothyroidism (>5%)
Hypothyroidism is an endocrine condition just as hyperthyroidism is, and it causes somewhat opposite symptoms. Due to not producing enough thyroid hormones, it often causes fatigue, depression, hair loss, weight gain, and a frequent feeling of being cold. It’s often comorbid with other autoimmune disabilities, e.g. vitiligo, chronic autoimmune gastritis, and rheumatoid arthritis.
Extreme hypothyroidism can also be potentially fatal because of a condition known as Myxedema coma (or “crisis”), which is also rare.
Deafblindness (about 0.2-2%)
Being DeafBlind is often considered to be an extremely rare disability, but that’s not really the case. DeafBlindness on its own isn’t a diagnosis - it can be caused by a wide range of things, with CHARGE syndrome (congenital), Usher syndrome (born deaf, becomes blind later in life), congenital rubella, and age-related deafness and blindness being some of the most common reasons. DeafBlindness is a wide spectrum, the vast majority of DeafBlind people aren’t fully blind and deaf, and they can use various ways of communication. Some of these could be sign language (tactile or not), protactile, the deafblind manual, oral speech (aided by hearing aids or not), the Lorm alphabet, and more. You can learn more about assistive devices here!
Despite what various media like to tell you, being DeafBlind isn’t a death sentence, and the DeafBlind community and culture are alive and thriving - especially since the start of the protactile movement.
We have a DeafBlindness tag that you can look through!
It’s probably worth mentioning that we have received little to no asks in general for almost all the disabilities above, and it’s certainly not due to what mods answer for. Our best guess is that writers don’t realize how many options they have and just end up going for the same things over and over.
Only representing “cool” disabilities that are “not too much while having a particular look/aura/drama associated” isn’t what you should aim for. Disabled people just exist, and all of us deserve to be represented, including those whose disabilities aren’t your typical “cool design” or “character inspo”. Sometimes we are just regular people, with disabilities that are “boring” or “too much”, and don’t make for useful plot points.
mod Sasza (with huge thank yous to mod Sparrow, Rot, and Virus for their contributions with research and data!)
#mod sasza#disabled character ideas#writing guide#writing resources#writing help#writing advice#writeblr
1K notes
·
View notes
Text
🌙some wildly cheap commissions!🌙
🙃 for some even wilder reasons 🙃






hey y'all. long post thingie but it's got cute pictures so please check it out
TRANSCRIPT OF POST
hey frens
got something kinda somber to talk about.
most of you are very aware of the existence of my beautiful fiance and co-creator of basically everything i do.
zae and i are getting handfasted (marriage for pagans) in october, and have been living together for about 10 years.
in 2021, zae got really fucking sick, and after a few false starts, was diagnosed with a rare for of vasculitis called granulomatosis with polyangiitis, GPA for short.
it’s an autoimmune disease that causes inflammation in blood vessels and other tissues, ultimately stopping blood from getting to the parts of the body that need it, affecting many areas, but primarily the respiratory system.
while the cause isn’t known, it usually presents in people in their 50’s or 60’s, but complications from a third bout of covid-19 appears to have made it emerge way earlier for our boy. at least, that’s what we think. his case is extremely aggressive, advancing faster
than anyone could have expected.
in zae’s case, it actually attacked his kidneys first, and then went after his lungs, causing both to threaten shutting down for good.
he was extremely anemic and needed a ton of transfusions, narrowly avoiding dialysis, and we spent weeks in the hospital keeping him alive. he was placed on two different kinds of chemotherapy to combat the disorder.
he lost his hair, went through even more fatigue and pain on top of what the disease had already put him through, and had to accept a plethora of changes to his life that will last forever.
a lot of you out there have harrowing experiences of your own when it comes to chronic and potentially terminal conditions, too, I’m certain.
“it’s not fun” is an understatement.
though there were a couple of really fucking close calls, zae’s GPA went into remission. his hair grew back fuller and more luscious than it had ever been before. (i later learned these are affectionately referred to as “chemo curls.”)
remission for gpa is usually expected to last at least 5 years, potentially up to 20, before any symptoms resurface. but zae’s case was particularly aggressive, so of course he’s not so lucky.
he’s relapsing now.
his symptoms have been slowly returning, and it’s been decided that he’s going back on chemo.
it’s no surprise that this shit is expensive, even with insurance. we’re still paying off the care
he received last time because ‘murca.
being disabled myself, work has been… let’s call it inconsistent, yeah? yeah, that’s a nice and comfortable thing to call it. no one’s doing well financially these days, so we of course have to get creative.
long story short(er), i’m doing a commission special! for the next MONTH, i am offering fast commissions at crazy-low prices to try and help us create a cushion to keep us afloat and relatively comfortable while we begin the chemo process again.
there’s several options for a variety of budgets, because i really hate the idea of seeking something for nothing, and i absolutely abhor having to reach out in this way. it makes me feel vulnerable and icky and… i’m sure you all understand that, too.
i can’t thank you all enough just for following me, and engaging with mine and zae’s work.
it may sound trite, but that really makes a difference to us, especially when we’re dealing with something so painful.
so if you can’t or don’t want to partake of the sale, please know that you are still a huge help to us, and we seriously appreciate each and every one of you. like, so fucking much.
thanks y’all
love,
fletch
END TRANSCRIPT
Commission Options:
Flash Sketches: $5USD/character
Comics: $5USD/panel - flat color
Comics: $10USD/panel - shaded color
Screenshot Redraws - $15USD/character (complex bgs, add $20)
all of this is posted with @zaebeecee's knowledge and blessing
please DM me if you're interested in something, and thank you again
more Hungry Games, fic fanart, and Persona stuff coming soon too



#my art#art commissions#personal stuff#fanart#fanart commissions#hazbin hotel#helluva boss#kingdom hearts#stardew valley#hazbin hotel fanart#helluva boss fanart#kingdom hearts fanart#stardew valley fanart#please share
53 notes
·
View notes
Note
Do you know how our understanding and treatment of diabetes has changed through history?
Oooh good question, anon!
As you may guess, diabetes mellitus is not new.
We've known about it since at least the Ebers Papyrus (1550 BCE) when the disease and a treatment was first described. This treatment was: "a liquid extract of bones, grain, grit, wheat, green lead and earth." I did not look these up, but I would guess they did not do a whole lot for the treatment of diabetes.
Later during the 6th century BCE it was first given a name when it was described by Hindu physician Sushruta as madhumeh or "honey urine."
Honey urine is a very apt descriptor for diabetes. In any type, one of the most measurable symptoms is that the person urinates a lot, and the urine tastes sweet (or, if one didn't feel like tasting, that it ferments, or that it attracts ants). This was also the first test for diabetes.
The reason for the sweetness of the urine (as well as a lot of other general info about diabetes) is spelled out more clearly in my "Don't Be That Guy Who Wrote Hansel and Gretel: Witch Hunters" post.
A Greek physician Apolonius of Memphis named it Diabetes, meaning "to siphon" (referring to the large amount of urine lost).
Roman physician Aretaeus later made the first precise description of diabetes. This included the classic symptoms of incessant thirst, copious urination, and constant hunger leading to emaciation and death. He also notes that if deprived of water, the patient will continue to urinate until they become so dehydrated that they die.
The term "Mellitus" was not added until the 1600s by an English physician Thomas Willis. This was again due to the sweetness of the expressed urine. Willis prescribed a diet of "slimy vegetables, rice, and white starch. He also suggested a milk drink which was distilled with cypress tops and egg whites, two powders (a mixture of gum arabic and gum dragant), rhubarb and cinnamon". Supposedly his patients improved if they kept to this diet, though few managed it long term. I honestly don't know how it would have worked, even temporarily.
A major breakthrough came in 1889 when it was discovered that if you removed the pancreas from a dog, the dog would become diabetic (particularly, that it would urinate large quantities of sweet urine). Up until this point it was thought that diabetes stemmed from the kidneys and bladder, or perhaps the lungs. This was the first time it had been shown experimentally that the pancreas was the problem.
Speaking of this, this was also part of a series of experiments where an English physician named Merkowski implanted a small amount of pancreas in the pancreas-less dog's fat, which reversed the diabetes temporarily. This proved that the pancreas was making something that helped regulate blood (and thus urine) sugar.
What this was wasn't figured out until 1921, when Canadian scientists Banting and Best (with help from McLeod and Collip) isolated something they called insletin (after the islets of langerhans, where the substance was being produced). It's important to note that all of these scientists hated each other so much they almost refused a Nobel Prize over it. Later, Collip would refine the substance and McLeod would rename it insulin.
Prior to insulin existing there was basically 1 vaguely useful treatment for diabetes. Unfortunately, that was starvation. So you could either die a slow and painful death by diabetes or you could die a slightly less slow but still painful death due to eating about 500 calories per day. Either way, diabetes was fatal, usually within a couple of years of diagnosis.
By 1923, the first commercial insulin product, Iletin, had been developed. Iletin was a U10 insulin (10 units per 1 milliliter- less potent than today's U100 and U500 insulins) and was made from pork pancreases. It took nearly a ton of pork pancreas to make 1oz of insulin. Fortunately, as a byproduct of the meat industry, pancreases were readily available.

Now, you might be thinking- no one has mentioned type 1 or type 2 yet in this entire post!
Well, you would be right, because diabetes wouldn't be split into 2 forms (insulin-dependent and non-insulin dependent) until 1979, and wouldn't be classified as types 1 and 2 until 1995. That's right- some of you were alive when there was only one kind of diabetes out there.
Now, there's more about the types in the Hansel and Gretel post, but essentially type 1 diabetes occurs when the pancreas itself stops producing insulin, usually in childhood. When this happens, the body stops being able to use sugar (insulin, a hormone, acts as a "key" to let sugar into cells for use). Without replacing that insulin, the person dies because their cells starve.
Type 2 diabetes occurs when the pancreas still produces insulin, but the cells stop responding to it correctly. This causes high sugar levels in the blood, which causes longer-term complications (infections, ulcers, blindness, neuropathy, heart and kidney disease, hyperosmolar syndrome, etc..) which eventually lead to death.
We started discovering oral drugs that worked on what would later become type 2 in the 1950s. Particularly those that worked by increasing the insulin output of the pancreas, but only when the pancreas was still producing some insulin.
Predicting which diabetics would benefit from oral therapies was challenging, but it was recognized that when the onset of diabetes was slow and came on in adulthood, the oral agents would work, while if it came on suddenly in childhood, the oral agents wouldn't. Terms like "adult onset" and "maturity onset" were common:
(Side note: if you have ever read Alas, Babylon (1955) there is a diabetic character who by today's standards clearly has type 1 diabetes, but wants to switch to the "new oral pill" (called "orinase" in the book, though they are likely referring to diabinese pictured above).)
From 1923 into the 1980s, insulin was given once or twice per day, and not particularly titrated to blood sugar. This was probably just because we didn't have a great way to measure blood sugar in real time. Pre-1970s, there was no way to test blood sugar outside of a lab setting.
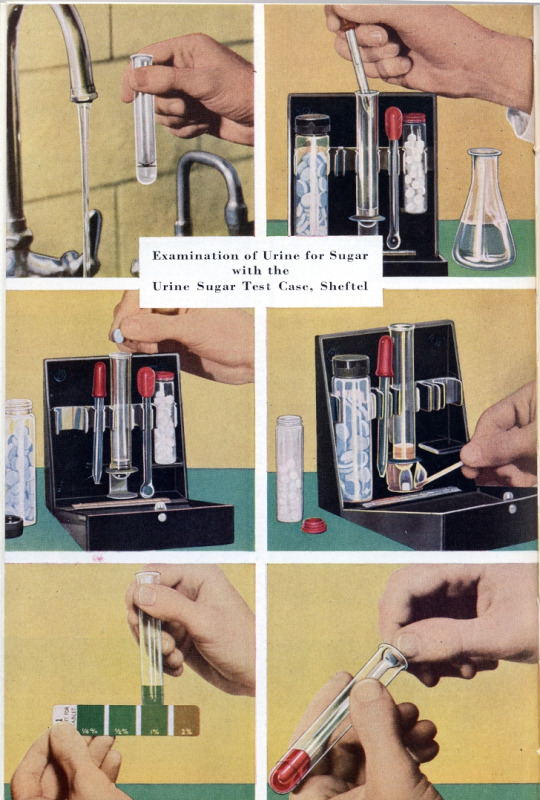
Urine testing was common starting in the 1940s, but was cumbersome as it required a flame for heating the urine. By the 1950s, a test had been developed that didn't require a flame, but was still not practical for home use. In the 1960s, paper strips were developed that changed color for different amounts of sugar in the urine. The problem with this was that the strips couldn't change color until there was sugar in the urine- a blood sugar level of over 200 by today's measurements. Low blood sugar readings were impossible at this time, and had to be treated based on symptoms.
In the 1970s, blood sugar could finally be measured by putting a drop of blood on a test strip, wiping it off, and matching the color of the test strip to a chart. While less cumbersome than urine tests, this was still something that would generally only be done at a doctor's office.

In 1983, the first home blood glucometer is developed. Finally, it was practical to take one's sugar multiple times per day, and it becomes possible to experiment with "sliding scale" insulin injections that keep tighter control of blood sugar. By the late 90s, continuous glucose monitors became available- though unlike today's CGMs that allow readings in real time on a smartphone or monitor, these had to be downloaded to a computer at regular intervals.
The 1980s were the first decade where insulin pumps become widely available. The very first pump was large and had to be carried in a backpack, but it represented a huge step forward in glucose control, as it more closely mimicked the function of a working pancreas than once-daily injections.
For the next 30 or so years you really had to work to qualify for an insulin pump, but recently it's been found that pumps greatly improve compliance with blood glucose control whether or not the person had good compliance before getting the pumps, and insurance has gotten better about covering them (though CGMs are still a pain to get insurance to cover).
The 1980s was also the decade that recombinant human insulin (insulin made by genetically modified bacteria) was first used. Up until that point the only insulins were pork and beef insulins, which some people had allergic reactions to. Recombinant insulin was closer to regular human insulin than beef or pork, and represented a big change in how insulin was made.
Today for people who take insulin to manage their diabetes, insulin is usually given as a single injection of a long-acting basal insulin, coupled with smaller doses of ultra-short-acting insulins with meals or snacks. This is the closest we've gotten to mimicking the way a pancreas would work in the wild, and keeps very tight control of blood sugar. This can be done by fingerstick blood sugar tests and individual injections of insulin, or it can be done with a CGM and pump- it just depends on the resources available to the person and their personal preference.
112 notes
·
View notes
Text
Leptospirosis: What it is, what it does, and how you can protect yourself and your pets.
People always have questions about leptospirosis (lepto) when they come into the clinic, especially in regards to the vaccine. This post will hopefully clear up those questions or any confusion regarding lepto and its vaccine, and why it's so serious. The information in this post comes from my formal education as a LVT, as well as other sources including the CDC, PAHO, and AVMA. If I missed anything or you see something that's incorrect, please let me know!
First and foremost: What is leptospirosis?
Leptospirosis is a bacterial disease that effects human and non-human animals. It's caused by bacteria in the genus Leptospira. In humans, it can cause a wide range of symptoms that can be very general. This leads to misdiagnoses. Animals such as dogs, livestock, and certain wildlife are all susceptible to infection.
How is leptospirosis spread?
Lepto is most often spread through contact with the urine of an infected animal. This is especially the case (but not the only case) with wild rodents. Infected dogs can seem healthy, but still pass the bacteria on in their urine. In urine-soaked soil, the bacteria can survive for weeks to months.
Dogs typically become infected when their mucous membranes or open wounds come into contact with urine or urine contaminated surfaces (like soil or water). Infection can also be spread through urine-contaminated bedding or food, or the tissues from the carcass of an infected animal. There have been rare instances where lepto has been transmitted by bite or breeding. A pregnant dog who is infected may pass the bacteria to her puppies through the placenta.
Humans contract lepto pretty much the same way: through contact with urine from an infected animal or urine-contaminated surfaces.
What are the signs and symptoms?
In humans:
High fever
Headache and muscle aches
Chills
Jaundice
Vomiting and diarrhea
Redness of the eyes
Abdominal pain
Rash
Humans can also be asymptomatic, which is particularly concerning. It usually takes anywhere from 2 days to 4 weeks post-exposure to the infection source before any symptoms are displayed. The illness begins abruptly and it may occur in 2 phases. The first phase is where you will see a lot of the general symptoms listed above. The person infected may recover for a period of time, but become ill again. The second phase is more severe, leading to kidney or liver failure, and possible meningitis. The illness can last a few days to 3 weeks or longer.
Without treatment, recovery can take several months.
In dogs:
Signs and symptoms may vary slightly depending on the strain of the infected bacteria. The signs are also very general in dogs, but the most common ones include:
Loss of appetite
Vomiting and diarrhea
Lethargy
Abdominal pain
Jaundice
Dehydration
Increased thirst and urination
Weight loss
Stiffness or muscle pain
The disease can also progress to kidney and liver failure in dogs, with damage to other organ systems also noted in the literature. Lepto can also cause bleeding disorders, which can lead to blood in urine, vomit, feces, or saliva, and petechiae on the mucous membranes or light colored skin.
Who is most at risk?
For humans, those who are most at risk include those who work with animals or outdoors where you come into contact with wildlife. The Pan American Health Organization (PAHO) also mentions that sewer workers and military personnel are at-risk populations. Farmers (and generally people who work with livestock) also make the list, as do veterinarians, veterinary technicians, and veterinary assistants.
For dogs, it's all of them. "All dogs are at risk of leptospirosis, regardless of age, breed, lifestyle, geographic location, time of year, and other factors." (source: AVMA)
Situations that can increase the risk of your dog contracting leptospirosis are listed below:
Exposure to drinking from slow-moving or stagnant water sources (this includes puddles)
Roaming on rural property
Exposure to wild animals or farm animals, even if it's only in the yard
Contact with other dogs (such as in urban areas, dog parks, boarding, or training facilities.
How is leptospirosis treated and diagnosed?
Disclaimer: I am NOT a medical doctor or DVM, but I am an LVT. If you think you're experiencing these symptoms, PLEASE go see your doctor. If you think your dog or any of your other animals are experiencing these symptoms, PLEASE take them to your vet.
Diagnosis in non-human animals:
Unfortunately, routine blood tests alone cannot diagnose leptospirosis. That's why it's important for your vet to use all information available to them (i.e. diagnostics, signs and symptoms, lifestyle, etc). There WILL be abnormal results for blood work, most likely high liver and/or kidney values and high white blood cell count. There are specific tests available for diagnosing lepto, such as the DNA-PCR and MAT tests. Both may be needed to reach or confirm a diagnosis. False negatives are possible, so your pet may be treated as if they have leptospirosis, even if the test results are negative. False positives are exceedingly rare.
Diagnosis in humans:
Leptospirosis is diagnosed in a similar fashion in humans. A physical exam, blood work, and urinalysis will likely be run. The same style of tests are used: DNA-PCR and MAT.
Treatment in non-human animals:
Leptospirosis is treated with antibiotics and supportive care. Doxycycline is most commonly used, and will likely be prescribed for 2 weeks or more. Supportive care includes hospitalization with IV fluids and management of electrolyte levels. Additional medications and procedures may be necessary.
Treatment in humans:
The treatment is similar in humans, with antibiotics (usually doxycycline). Your doctor may also suggest to take ibuprofen and monitor yourself at home for less severe cases. If the case is severe, then you'll likely spend time in the hospital. Additional medications or procedures may also be necessary.
Outcomes:
In non-human animals:
Leptospirosis is responsive to treatment with antibiotics. Complete recovery is possible, but some animals that survive may be left with chronic kidney and liver disease. Some animals may not survive if the infection has gotten to the point where it causes severe organ damage or the ability of blood to form clots.
In humans:
You can survive leptospirosis. Most cases have either very mild symptoms that go away on their own, or none at all. Without treatment, leptospirosis can cause kidney damage, meningitis, liver failure, trouble breathing, and even death. PLEASE go see a doctor if you think you're experiencing any of these symptoms, especially together.
Prevention
How can you prevent infection and protect your pets?
For dogs, there's the leptospirosis vaccine. This is an annual vaccine that vaccinates against multiple strains of Leptospira. If you're worried about your dog having a vaccine reaction, let your vet know and they can administer an injection of diphenhydramine (generic benadryl) beforehand, OR you can ask them what the appropriate dose is for your dog and give them the respective amount at home (in tablets or liquid). Vaccine reactions are uncommon, but if they do happen, it's usually immediately after exposure to the vaccine. You can ask to stick around in the lobby/waiting area of your vet clinic for a few extra minutes if you're still concerned.
Limit your dog's access to standing water. Don't let them drink from it. Prevent rodent problems where you can by properly storing food items in appropriate containers, securing your garbage, and patching up any access points into your house if you see them. Try to avoid contact with wildlife, when possible.
For humans, the recommendations remain similar. Don't wade or swim in stagnant water, ESPECIALLY if you have open wounds. Avoid contact with wildlife. WASH YOUR HANDS, often and appropriately. USE PPE if you work in a veterinary setting and properly clean and disinfect surfaces and equipment. Make sure you know or research the area that you're in if you like swimming and boating. Check to see if there have been any recent lepto infections. Cover your scrapes and wounds with waterproof bandages and wear water shoes if possible.
I hope this post answered a lot of your questions! Thanks for reading.
Sources under the cut.
Sources:
#animals#pets#dogs#leptospirosis#zoonotic diseases#infectious diseases#vet med#vetblr#petblr#dogblr#my posts
44 notes
·
View notes
Text
Living with Long COVID: What it’s Like to be Diagnosed with the Debilitating Disease - Published Sept 3, 2024
By: Nicole Pajer
Even mild cases of COVID-19 are linked to potential long-term repercussions — some of them deadly serious
Chrissy Bernal has caught COVID-19 three times, most recently in October 2023. “My symptoms were always pretty mild,” she says. But after her third round of the virus, she developed extreme allergies to foods she used to eat all the time: oats, dairy, gluten, sesame seeds and peanuts.
“I literally have some level of anaphylaxis every single day,” she says. In May, Bernal, 46, a public relations professional in Houston, went into anaphylactic shock during a virtual meeting. “I had to inject myself with an Epi while everyone watched in horror on Zoom,” she says.
Natalie Nichols, 53, has been struggling with debilitating asthma and severe food allergies since she first caught COVID more than three years ago. “Last fall, I spent two-and-a-half months confined to bed, motionless, because moving, including holding a cellphone, made me too short of breath,” she says.
She’s also experienced brain fog, high blood pressure, hyperglycemia, fatigue and gastrointestinal symptoms. Nichols, the founder of a nonprofit in Nacogdoches, Texas, recently underwent surgery to repair joint damage caused by COVID-induced inflammation.
Lorraine W., of Clarence Center, New York, was looking forward to an active retirement when she was diagnosed with COVID in March 2020. “I’ve never returned to my pre-COVID self,” says Lorraine, 65.
She’s on medication to treat small blood vessel damage to her heart and continues to battle a lingering cough, fatigue and breathlessness, as well as kidney disease. Neurological changes have made her legs unsteady when she walks, requiring her to use balance poles. “None of these conditions were present before COVID,” Lorraine says.
In June, the National Academies of Sciences, Engineering, and Medicine released a comprehensive definition of long COVID: “an infection-associated chronic condition that occurs after COVID-19 infection and is present for at least three months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems.” According to that definition, 18 million Americans have experienced long COVID; currently, more than 1 in 20 of us are living with its symptoms. Researchers have begun to link long-term COVID with another recent phenomenon: our shrinking life expectancy.
The disease we’re forgetting
COVID doesn’t seem that scary anymore. More than 98 percent of the U.S. population has some degree of immunity — from vaccination, prior infection or both — and Paxlovid and other medications are available to counteract acute symptoms. For many of us, contracting COVID is like having a bad upper respiratory infection.
But “COVID isn’t gone,” says Ryan Hurt, M.D., director of the Long COVID Research and Clinical Program at the Mayo Clinic. The World Health Organization (WHO) estimates that COVID still kills at least 1,000 people every week around the globe — but “we only have data from about 40 countries,” says Maria Van Kerkhove, M.D., director of WHO’s Department of Epidemic and Pandemic Preparedness and Prevention.
Older adults and those with preexisting conditions remain among the most at-risk populations for severe, acute COVID. People 65 and older accounted for 63 percent of COVID-related hospitalizations and 88 percent of in-hospital deaths during the first seven months of 2023, according to CDC data.
Although the dangers of acute COVID infection may have ebbed for many, the reality of long COVID is coming into view. Of those who contracted COVID-19 within the past four years, 10 to 20 percent have experienced long COVID.
“With every new case of acute COVID [the initial phase of infection when diagnosed or symptoms first appear], there is risk for developing long COVID,” says Caitlin McAuley, D.O., a family physician at the Keck COVID Recovery Clinic in Los Angeles. She’s had patients who developed long COVID fully recover, get reinfected several times with no lingering effects, then develop another case that leads to a new bout of long COVID. She’s also seen patients who got COVID twice with no lingering effects, and the third time they ended up with prolonged symptoms.
“We still have a number of individuals who had the first wave of COVID who are suffering from long COVID symptoms now, several of them many years out,” says Jerrold Kaplan, M.D., medical director of the COVID Rehabilitation and Recovery Program at Gaylord Specialty Healthcare in New York.
Having escaped long COVID previously doesn’t mean you won’t face it in the future. Indeed, some research has suggested that catching multiple COVID-19 strains puts you at increased risk. A study published in 2022 found that reinfection can increase the risk of complications in major organ systems, and these risks persist at least six months beyond the initial infection.
We don’t yet know the true impact of catching COVID. “Many chronic disease processes, such as cardiovascular disease, dementia and cancer, take years to develop. And whether acute COVID-19 puts people at risk for some of these issues? Time will tell,” Hurt says. What doctors do know is that patients are flocking to their offices complaining of symptoms they never had before COVID.
Is long COVID boosting our death rate?
In July, COVID accounted for less than 1 percent of all deaths in the U.S. Life expectancy in the U.S. is 77.5 years, reflecting an uptick over the past two years but still lower than prepandemic levels. Many factors contribute to that statistic, but it’s clear that the long-term effects of COVID have played a role.
For example, a study in the journal Nature Medicine found that those hospitalized with COVID had a 29 percent greater risk of death in the three years after their infection.
“But what was also alarming is that in people who weren’t hospitalized, there was also an increased risk of a variety of medical issues,” says John Baratta, founder and codirector of the COVID Recovery Clinic at the University of North Carolina at Chapel Hill. Even patients who’d had mild bouts of COVID-19 had an increased risk of respiratory, cardiovascular, metabolic and neurological issues lingering for three years after the initial infection. Long COVID patients had a significantly increased risk of severe health issues affecting the brain, lungs and heart.
We have long known that an acute case of COVID can compromise heart health: Compared with those who didn’t contract COVID, people who caught the virus were 81 percent more likely to die of a cardiovascular complication in the ensuing three weeks, according to a study of 160,000 patients published by the European Society of Cardiology. But the risk lingers long after the symptoms abate. Those who caught the virus were five times more likely to die from cardiovascular disease as long as 18 months after infection, the same study found. Heart disease deaths, which had been on a downward trend for decades, began to spike in 2020 and remained high through 2022, the last year for which data is available.
Stroke, blood clots in the legs leading to clots in the lungs, abnormal heart rhythm (arrhythmia) and inflammation of the heart are among the challenges COVID poses, says Mohanakrishnan Sathyamoorthy, M.D., professor and chair of internal medicine at the Burnett School of Medicine in Fort Worth, Texas. In long COVID, this collection of cardiovascular disruptions can present as postural orthostatic tachycardia syndrome (POTS), in which patients’ heart rates increase abnormally when they go from sitting or lying down to standing up.
One theory to explain COVID’s long-term effect on the heart — and the body in general — centers on inflammation. “Every time you get infected with COVID, there is a possible increased risk of long COVID, and some cardiac disorders can occur — especially if you have a history of heart disease, including stroke, heart disease and heart attacks,” says Pragna Patel, M.D., senior adviser for long COVID at the CDC. All of these problems can be exacerbated by the virus entering coronary tissue and triggering inflammatory responses that can damage the heart.
Researchers say COVID may also alter the gut microbiome, a primary controller of inflammation, thereby triggering the immune system to rev up the condition. “There is no single agreed-upon mechanism that’s causing the issues,” Baratta says. “An individual may have multiple factors going on in their body, and not everyone will have the same underlying mechanism causing their symptoms,” which increases the complexity of both research and treatment.
One factor that seems to matter: vaccination status. “Several studies show that vaccination can decrease the risk of developing long COVID,” Patel says. Vaccination rates tend to increase with age, with people 75 and older being the most well vaccinated — hence the most well protected from long COVID, Patel theorizes. That may explain why long COVID most commonly affects people ages 35 to 64; the risk seems to drop for those 65-plus, according to CDC data.
From long covid diagnosis to treatment
No single test can determine whether a person has long COVID. Doctors typically diagnose long COVID by reviewing the patient’s health history and current symptoms and trying to rule out other causes. A positive COVID test is not required, as someone could have been infected without knowing it, then experience strange symptoms later, Patel says.
Though there are many ongoing clinical trials on long COVID, there is no umbrella treatment. Primary care physicians address what they can, then call in specialists — such as a cardiologist to handle arrhythmia or a therapist to treat anxiety — for more targeted care. There are long COVID centers around the country where teams of professionals work to help patients through their unique symptoms.
“Because the effects of COVID are so wide throughout the body and mind, there will not be a single treatment for all long COVID issues,” Baratta says. “This is going to be treated by many different types of providers and specialists, and it will be treated, often, symptom by symptom.”
Long COVID is recognized as a disability under the Americans with Disabilities Act if it substantially limits one or more major life activities. About 200 symptoms fall under that umbrella, Patel says. Here are some of the conditions we’re learning can linger months and, in some cases, years beyond an acute COVID infection. If these or other health changes seem familiar, consult your primary care physician.
1. Extreme fatigue
It’s common to experience fatigue when your body is busy fighting off an illness. But some people still struggle with fatigue long after their initial COVID infection. In fact, a lack of energy is the number one symptom reported by long COVID patients. In some, this can be diagnosed as chronic fatigue syndrome, which has been on the rise since the start of the pandemic, Baratta says. He defines this as “a disabling level of fatigue that severely limits daily activities.”
This lingering fatigue may be due to limited production of energy within the muscles caused by damage to the mitochondria from a COVID infection. It can happen to anyone — no matter their level of fitness before infection. “I’ve treated patients who have been triathletes and now may only be able to do 15 or 20 minutes of exercise a day, when they’re used to running and swimming miles at a time,” Kaplan says.
He recommends starting slow and pacing yourself with everything you do around the house, “doing shorter intervals several times throughout the day, rather than trying to do everything at once.” Whether it gets better depends on the individual. Some people’s symptoms clear, and some people may battle them indefinitely.
2. Shortness of breath
An analysis of chest CT scans from 144 patients ages 27 to 80 found that more than one-third of people hospitalized with a previous COVID infection had lung scarring and thickening two years after coming into contact with the virus. Even patients with milder cases who walked away without scarring can experience changes in their breathing.
“Some research shows that people after COVID start to take shorter, shallower breaths,” Baratta says. “This essentially causes a type of hyperventilation they are doing without even recognizing it, not getting good fresh air deep into the lungs, and [this] can lead to shortness of breath.”
Doctors have found success using respiratory exercises to help patients relearn slow, deep breathing.
3. Cognitive changes
Difficulty concentrating, spaciness and forgetfulness are just a few of the brain challenges COVID can bring on. These can last for weeks or months or — in some with long COVID — become an everyday occurrence that lasts indefinitely. COVID may linger in a person’s gut long after an infection, altering their microbiome and hindering the body’s ability to produce serotonin, leading to cognitive disturbances.
COVID may also disrupt the blood-brain barrier, allowing chemicals or molecules in the rest of the body to enter the brain blood circulation and potentially lead to brain fog, Baratta says.
One study found that 30 days after testing positive for COVID-19, people were at greater risk for cognitive decline, as well as for mental health disorders including anxiety, depression and stress. Another study found inflammation in the brains of people with mild to moderate COVID-19 was similar to the effects of seven years of aging. Doctors are leading neurologically affected patients through cognitive rehabilitation exercises that show promise in reducing symptoms.
4. Depression and anxiety
“Mood-related disorders are one of the top five issues that happen to people after COVID,” Baratta says. There may be a direct relationship between the virus’s effect on the brain and mood issues. A 2021 review of eight studies found that 12 weeks after a COVID infection, 11 to 28 percent of people had depression symptoms, and 3 to 12 percent of those individuals reported their symptoms as severe. If you’re feeling more stressed or down after catching COVID, tell your primary care physician, who can refer you to a therapist. Or visit the American Psychological Association’s search tool at locator.apa.org to find a qualified therapist in your area.
5. Sleep disturbances
Nearly 40 percent of people with long COVID have reported major changes to their sleep patterns. One study looked at 1,056 COVID-19 patients who did not have a severe enough infection to require hospitalization. Of that population, 76.1 percent reported having insomnia and 22.8 percent severe insomnia. Sleep apnea may also appear post-COVID, another way the disease affects the respiratory system.
Talk to your doctor if you’re having sleep issues. A CPAP (continuous positive airway pressure) machine can help with sleep apnea. Lifestyle habits that prioritize healthy sleep, such as keeping consistent sleep and wake times and avoiding large meals before bed, may also help. “Post-COVID sleep has literally been a nightmare! We saw a 23 percent increase in sleeping-pill prescription during and post-COVID,” says Michael Breus, a clinical psychologist and clinical sleep specialist in Los Angeles.
6. Digestive upset
Diarrhea, constipation, abdominal pain, bloating and gas: These symptoms of irritable bowel syndrome can be by-products of an encounter with COVID. A survey of 729 COVID survivors found that 29 percent experienced at least one new chronic GI symptom six months after their infection. “There is evidence that parts of the COVID virus linger in the GI tract for many months after the initial illness, and it’s been suggested that the presence of these ongoing viral fragments causes dysfunction or problems with the GI tract, leading to mostly symptoms of diarrhea and gastric distress and discomfort,” Baratta says.
Talk to your doctor about any new digestive symptoms or seek help from a gastroenterologist. You can keep a food journal and note if your condition flares after eating certain foods. Try cutting out those foods, then reintroducing them one by one to see what you react to, Kaplan advises.
7. New or worsened allergies
Some people who develop COVID experience allergies they never had before. One study found the risk of developing allergic diseases, such as asthma and allergic rhinitis, rose significantly within the first 30 days after a COVID diagnosis. This may be because one’s immune system stays hypervigilant after fighting the virus, McAuley says.
In severe cases, like Chrissy Bernal’s, this can lead to mast cell activation syndrome (MCAS), a disease that can behave like a series of severe allergies: The body’s cells become hypersensitive, causing strong reactions to everything from food and pollen to even a hot shower or exercise. Antihistamines and other medications may help, so talk to your doctor if you experience skin itching, a rapid pulse, wheezing or gastrointestinal symptoms.
8. Pain
Some COVID survivors battle chronic pain, everything from aching joints to testicular pain. There is a higher risk of inflammatory arthritis, and women are at higher risk than men. One review of studies estimated that 10 percent of people who contracted COVID experienced musculoskeletal pain at some point during the first year after infection.
Reducing stress, eating a healthy diet and exercising may ease some post-COVID discomfort. Massage therapy, movement therapy, acupuncture and over-the-counter pain medications may also offer relief. Your doctor can refer you to a specialist, such as a rheumatologist, who can help manage symptoms including joint pain.
Fast-moving research means new hope
If your symptoms last after a bout of COVID, start with your primary care physician, who can help treat your symptoms or refer you to a specialist. Despite previous dismissals, long COVID is more recognized these days, Patel says, and the CDC is doing its part to educate both patients and providers. And initiatives such as the National Institutes of Health’s Recover program are researching treatment options.
“In a year, things will look different, because research is moving so quickly,” says Sara F. Martin, M.D., medical director of the Adult Post-Acute COVID Clinic at Vanderbilt University Medical Center. The CDC, for instance, is funding a series of clinical trials that the NIH has in the works. This new information, Martin says, may guide doctors, including herself, who treat long COVID patients to better ease their symptoms.
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator
10 notes
·
View notes
Text
World Lupus Awareness Day!
Hello, Hi.
So today is World Lupus Awareness Day. As just a normal person but also as someone with a younger sister who has Lupus, I feel like it's important that I help spread some awareness!
For those of you who don't know what Lupus (also known as Systemic Lupus Erythematosus), is an autoimmune disease in which the body's immune system mistakenly attacks healthy body tissue! I recommend that everyone look up more details!
Lupus or SLE's symbol among patients is a purple butterfly which is symbolic of the butterfly rash that some patients experience. Some symptoms are swollen and pained joints, fevers, chest pain, hair loss, fatigue and more.
A lot of this I have looked up (am looking up as I type so that I make sure I am accurate) and have also witnessed first hand. My younger sister was diagnosed with SLE in 2020 and was experiencing symptoms as early as 2012.
I'd like to talk about my younger sister in this post to just illustrate what she has going on and how things look for a person with Lupus (SLE).
My younger sister has Lupus Nephritis Class 1 (which means that she has Lupus in her kidneys), Discoid Lupus (which affected her scalp and caused immense hair loss, she still has scars from which hair cannot grow), Anti Cardiolipin Antibody Positive (blood clots could kill her or cause miscarriages so she's aways on blood thinners but this also means bleeding of any sort takes time to stop), Alpha Thalassemia Minor (similar to sickle cell anemia, she has tear drop shaped red blood cells), Chronic Interstitial Lung Disease (or also Restrictive Lung disease, she finds it incredibly hard to breathe in any situation where the air is humid and some days just normally she struggles to breathe).
All of these have made her life incredibly difficult. She is managing all of this with medication, however, medication only helps to manage it and some days are harder than the rest. Being a full time worker is hard. She had to drop out of college because she couldn't handle being a full time student, meds are incredibly expensive and what's worse is, because she looks normal on the outside, people don't accept that she's essentially disabled. (She's currently looking to apply for disability). A lot of days are just impossible for her but she keeps going because healthcare and legal help for people with SLE (or health issues in general) is so hard to get. Her mental health has to be constantly managed so that she eats and therefore can also have her meds.
Despite all this she finds it in herself to smile and do things she enjoys!
So! Yeah! Today is Lupus Awareness Day! Please share this and also look it up to learn more about it! Especially since I don't know everything obviously!
#sunny rambles#world lupus awareness day#lupus awareness#lupus#systemic lupus erythematosus#somewhat personal ig considering it involves my sister#REBLOG REBLOG TO SPREAD AWARENESS
12 notes
·
View notes
Note
Okay so magic as something the body sees as a threat/danger to the body...
And this ask may return in varying levels as I refine it and get a better understanding of the subject
What if the body had a low-level immune response to using magic--like it isn't at an autoimmune disorder (yet, possibly)? Would there be a fever to try and purge whatever it is (that the body can't find)? Or would it immediately start escalating to an auto-immune response?
Okay, I love this question. So to answer it, I'm gonna have to 1) explain the immune system and how autoimmune disprders work, and 2) figure out how magic can be physical in a way for the immune system to respond to it.
So first off, your immune system has two main parts: innate (you're born with this) and adaptive (you develop this). Adaptive is the important one here. It deals with B cells, T cells, antibodies, stuff like that. It is specific, regulated, and has a memory. It also has to have tolerance. Tolerance is when these immune cells recognize the self and don't attack. Autoimmune disorders are the failure of this ability. Cells can't distinguish the self from the non-self, so they develop an immune response to your own cells. So to answer the first part, any attack on the self is an autoimmune disorder. There's not really an in-between.
The reason behind autoimmunity is largely unknown and too grand for this tumblr post (it's a lot of genetics stuff, as well as environment), so we're gonna fast foward a bit to what happens when your immune system attacks you. I will note though, that autoimmune disorders are most common in young adult females (probably something to do with hormones at that age, like estrogen).
ANYWAYS, so...what's going to happen is that the immune cells start attacking your cells and killing them. If the beta cells of the pancreas are killed, thats Type 1 Diabetes. If the joints are attacked, that's Rheumatoid Arthritis. There's also Lupus, Scleroderma, Sjögren, etc. I'm not going to get into all of this here, but you get the point: DISEASE.
What are some symptoms related to autoimmune disorders? That's complicated because there are so many and they act on so many types of cells, that the symptoms are specific to each disease. But, I like Systemic Lupus Erthematosus because it has a lot of systemic symptoms due to the body attacking your DNA. These include: a rash on the cheeks (malar rash), arthritis, inflammation of serosal surfaces (like oral mucosa), kidney injury, psychosis, seizures, oral ulcers, and a decrease in cell types (like RBCs and WBCs). This can cause a low grade fever, photosensitivity, fatigue, muscle aches, loss of appetite, inflammation of the heart and lungs, and poor circulation to the fingers and toes.
Now onto the next part: magic autoimmune disorder. So we're going to assume that using magic goes along with having a certain type of cell. We'll call this a magicyte. We can say this cell type is increased in the blood when the user is doing magic stuff.
In our hypothetical, the immune system can no longer recognize magicytes as self and begins to attack and kill these cells. This will probably lead to a decreased ability or even an inability to do magic (like how people with DM1 can't make insulin). We can also say that there may be a low-grade fever due to immune system activation. Remember how I said adaptive immunity is specific? Well, that's good because it probably won't do much else. Lupus is really bad because DNA is attacked, so that fucks with a lot of cells. As long as magicytes are the only targets of this response, the person will probably only lose their ability to do magic. Systemic stuff like fever will probably appear after they attempt to use magic (thus increasing the number of those cells and increasing immune response).
I hope this answered your question, and thanks for the ask :))
#med student#medical school#medicine#med school#biology#med studyblr#immune system#autoimmine disease#lupus#questions#superpowers
6 notes
·
View notes
Note
Maybe a oneshot where B!D gets diagnosed with type 1 diabetes.

---
You sighed and ran your hand through your hair for seemingly the three hundredth time in half an hour while you were nervously waiting for your GP, who had summoned your sisters and you to her office.
For weeks you had no idea what was happening to you, denying every symptom as if it were kind of like a flu that caused them but didn´t break out properly; the excessive drinking and double the amount of urination, the increased hunger and urge to eat while losing weight and throwing up at the same time, getting up tired from a nine hour sleep and the weakness your body carried with it.
Not to mention the most violent mood swings your sisters have ever experienced with you.
The silence and your ongoing thoughts were interrupted by a heavy swing of the opening door before your doctor walked in. She was young, in her early thirties yet she was far better than anyone that has ever treated you in your life. "Hello, Y/n. Nice that you could come so quickly."
"You said it was urgent so I wasted no time."
Convincingly, she nodded with a soft smile and shook hands with each of your siblings in greeting. Wasting no time, your doctor settled into her much more comfortable looking chair than you were sitting in, being careful over her coat so it didn´t crumple under her.
"So Y/n, I have good and bad news." she started to speak, looking down at her tablet to review your blood results, letting the panic in you rise further with each second that passed. "The good news is; your blood results are almost perfect and you have no signs of kidney failure or anything close to the symptoms."
At that moment, an incredibly large stone fell from your heart and the adrenaline disappeared from your body. However, the panic was not immediately banned; only afterwards did you think about her choice of words and got stuck on one- almost.
"Almost perfect? Doctor, what does that mean?" Kara had taken the question out of your mouth; she too was probably confused by what the doctor said.
"Well, all but one." your doctor now shifted her gaze between the blonde and redhead, probably to add depth to her words. "An increased glucose value can be seen in your sisters venous plasma, and auto antibodies can also be detected in her blood, which should not normally be there."
Alex shifted uncomfortably in her seat and leaned further forward to rest her elbow on the young woman´s wooden desk. She had covered her mouth with her hand and widened worryingly her eyes at you as if she knew what was about to come.
After all, she was the only one of the three of your who had completed medical school.
"Y/n, unfortunately I have to tell you that you have type 1 diabetes." Your heart suddenly dropped and your stomach felt like a roller coaster, the lump in your throat expanded to an abnormal size. You slumped back in your seat, eyebrows furrowed in uncertainty.
Diabetes. You´d had it for roughly four weeks, hence why you felt like crap.
"For understanding; Type 1 Diabetes is a chronic autoimmune disease caused by your pancreas not producing enough insulin. Insulin is the principle hormone in regulating the glucose in your blood and without it, the glucose will not be absorbed properly, resulting in higher blood glucose levels. Higher glucose levels can result in polyuria and polydipsia which means an increase in urination and in thirst which you´re already going through- they are the first steps into this illness."
You only understood half of what she said to you, some words that she had in her vocabulary so complicated that you would have needed a dictionary and a ten-page guide if she wouldn´t explain to you how the further process would work.
"You need to start poke your finger with this little needle poker device here." From a drawer in her desk, she pulled out a burgundy, funny-looking thing and laid it in your hands that you had already outstretched, longing for this device that´s gonna save your ass probably more times that you´re going to count.
Your sisters also leaned into you to see for themselves what it was. They listened intently to offer you the best support they could give you, swallowing every information they could get. "And then you have this little thing here, which will read the level of your blood sugar. Also you have to inject yourself insulin manually into your leg or stomach- wherever you´re comfortable."
You rolled your eyes and put the thing back on the table; annoyed.
To put it into other words- type 1 diabetes was a fucking annoying disease where your body randomly decided to give you a big "FUCK YOU!" and stop giving your body what it craved. And unless you got it under control, your organs could fail.
But you didn´t seem aware of this.
#baby danvers imagines#babydanvers#baby danvers#baby danvers imagine#baby danvers x supergirl#baby danvers x alex danvers#baby danvers x danvers sisters#baby danvers x kara danvers#alex danvers x reader#alexdanvers#alex danvers#b!danvers#b!d#alex danvers x baby danvers#alex danvers x you#kara danvers x reader#kara danvers imagine#karadanvers#kara danvers#kara zor el#kara danvers x danvers sisters#kara danvers x baby danvers#kara danvers x you#kara danvers x female reader#kara danvers imagines#supergirl cw#supergirl fanfiction#supergirl fanfic#supergirl#supergirl imagine
105 notes
·
View notes
Text
Leishmaniasis
Case Reports, like we're on a episode of house
23M in Kenya, presenting with months of LOW, persistent fevers, and abdo fullness, found to have massive splenomegaly.
examination: massive splenomegaly (10 cm below costophrenic margin, and will definitely cross midline) and hepatomegaly
pancytopaenic on bloods, plt's down to 40s
diagnosis confirmed on BMAT (parasite seen)
normal HIV, liver and kidney function
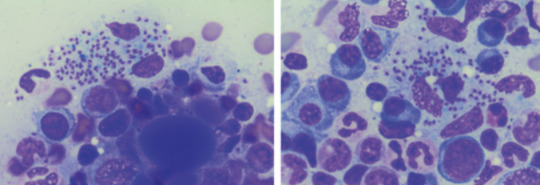
Bodies seen on the BMAT below are part of the lifecycle of the parasite that is intracellular, hence you can see the macrophages/neutrophils loaded with them, even bursting
What is it:
think of it when you get a patient with pancytopaenia and hepatosplenomegaly, who either traveled to or is in/from a tropical/subtropic region (where sand flies are)
cause - protozoa parasite Leishmania, transmitted by infected sandflies
Epidemio (when to consider it)
tropics, subtropics (South America, Asia, AFrica), Southern Europe
Microbiology/Transmission
parasite, replicates intracellularly (Leishmania donovani)
transmitted in sand flies (can be unnoticeable and usually bite in dawn or dusk - evenings or night), can also be transmitted via needles/blood
more common in rural areas
I've simplified this, but is more extensively covered in StatPearls and Wiki (there's different species of Leish and sandflies that transmit it)
once bitten, the protozoa are phagocystosed by skin macrophages, which then becomes full of the "bodies" (part of the lifecycle). Eventually these burst to release more of the bodies that infect more macrophages
they eventually are spread via blood to liver/spleen/BM and LNs
Random history:
ancient, records of disease date back to Egyptian mummies from 3000 BC --> positive DNA amplication for Leishmania and on papyrus from 1500 BC
multiple physicians from different times have described the disease, but it's named for 2 who described the parasite's intracellular ovoid body stage in smears from infected patients in India: Lt General William Boog Leishman and Captain Charles Donovan (Ronald Ross named the bodies after the 2 --> "Leishman Donovan bodies"
significant disease in Allied troops in Sicily in WWII, called "jericho buttons" (image on wiki from a WWI trooper serving in the middle east)

Leishman: Scottish pathologist and British Army medical officer, later it's director general in the 20s, did extensive research into the parasite named for him by Sir Ronald Ross. He mistook the parasite he observed for trypanosomes (cause of Chagas in South America and African sleeping sickness in Africa)
Donovan: Irish parasitologist, medical officer in India, observed an epidemic across India just after the rebellion of 1857, discovered the "bodies" in spleen tissue as the causative agent for what the locals called "kala azar" (severe visceral leishmaniasis - see below)
Donovan also discovered the "bodies" of Klebsiella granulomatis, hence these too are named after him (cause of ulcerative granulomas)
It became scandalous as both wanted credit for the "discovery" of this newly identified organism. So Sir Ronald Ross named it for both of them.
Sir Ron, by the way, won a Nobel in Medicine for discovering that malaria is transmitted via mossies (this was also a source of scandal, he was meant to share it with another physician who he accused of fraud - and they never received the award)
finally, it was actually a Russian physician who identified it first, but well, he published in a little known Russian journal which was promptly forgotten.
Clinical features
cutaneous type vs visceral organ type (spleen, liver, bones)
From wiki

can be asymptomatic
cutnaeous: can be there for years and resemble leprosy, causes an open chronic wound (most common), incubation 2-4 weeks on average (nodules at site of inoculation that eventually form ulcers), can heal spontaneously in 2-5 yrs
in diffuse cutaneous cases, can affect face, ears, extensor surfaces
can be muscosal = eg nasal symptoms/epistaxis, severe: perforated septum, this occurs in 1/3 after resolution of cutaenous symptoms (can be severe/lifte threatning, as it can affect vocal cords and cartilage, but oddly not bone)
visceral (incubation periods of up to years until immuncompromise): fever, weight loss, hepatosplenomegaly (spleen more than liver), pancytoaepnia, high total protein and low albumin with hypergammaglobulinaemia
this has seasonal peaks related to sandfly habits and humidity
interestingly it is an infective cause of massive splenomegaly, such that it crosses the midline
Extreme - but noticeable hepatosplenomgealy/abdo fullness, from medscape

can be atypical in HIV co infected patients, LAD in seom regions like Africa
Kala azar = black fever in some severe cases (fatal due to secondary mycobacterial infection or bleeding), refers to damage fto spleen, liver and anaemia
invstigations:
serology not great (minimal humoral response to the parasite), so often requires histopath (tissue sample) for which BMAT is safest in visceral organ involvement
visualisation of amastigotes (or Leishman-Donovan bodies), as intracellular --> can be seen in macrophages (small round bodies) post Giemsa staining
PCR of DNA also possible (as done in the Egyptian mummies)
Image source:

Treatment
liposomal amphotericin B (holy shit strong stuff) in visceral, PO: miltefosine (caution in pregnancy), all have significant ADRs, or paromycin. however, mortality of 10% if visceral left untreated
mixed results with azoles
in HIV co infection - start the HAARTs! can improve survival, mortality is 30% in HIV patients
cutaneous: stibolgluconate (have never heard of these drugs) and megluaine antimoniate, but limited disease often spotnaeously gets cleared by the innate system
prevention:
use DEET insect repellant at dawn and dusk
loose fitting clothing that covers all skin
no vaccine (were attempts at vaccinating dogs, which decreased rates)
sandflies are smaller than mossies, so requires small netting

Differentials for hepatosplenomegaly

Sources:
WHO guidelines
CDC guidlelines
Wiki - Haven't covered pathophysio, but wiki does extensively
StatPearls
DermNet - great resource for all things derm, that my derm colleagues pointed out to me
9 notes
·
View notes
Note
Hi Jess, I have a Karluk question for you! What exactly was wrong with the expedition's supply of pemmican? Wikipedia says Stefansson said it was a lack of fat, but Niven's book describes the disease as coming from too much fat and protein. Are there any clear answers as to what actually made it faulty?
Hi! This is a great question, and I wanted to do a little research before I responded to make sure I got the details right.
First, what exactly is pemmican? It's one of the staple foods of polar exploration, a nutritionally balanced combination of dried meat, fat, and sometimes a small amount of carbohydrates. It's easy to transport, calorie dense, can be formulated to feed men or dogs, and doesn't spoil easily, making it ideal for long voyages. Indigenous peoples were making and using pemmican for centuries before the Europeans "discovered" it.
With this in mind, I looked at the two competing claims you mentioned. First, I found the citation in the Wikipedia article, and since I have Stef's (ridiculous) book The Friendly Arctic, I double checked it. The quote is accurate, but there's some missing context. In this passage, he was actually talking about pemmican that was specifically formulated for dogs! There was dog pemmican and man pemmican (and confusingly enough, the Karluk also had 2 different kinds of man pemmican-- more on that later). In the passage below you can see that Stef is complaining about the dog pemmican being deficient in fat, and how he claims it affected dog performance.


(In general, though, it's important to note that Stef had a... tenuous relationship with the truth. I would fact check anything he said as a matter of principle.)
To examine Niven's claim, I called in the big guns, by which I mean I consulted with an actual expert with their Ph.D. in all things polar and a special interest in Stef's shenanigans! They are on tumblr, but I'm not sure if they're OK being tagged, so I will just thank them anonymously for their help 🥰 Anyway, between the two of us, we were unable to find any studies specifically examining the relationship between pemmican (faulty or otherwise) and nephritis, a kidney disease diagnosed by the doctor who examined the Karluk survivors. To the best of our knowledge, no testing was ever done on the bodies of the deceased, but since the symptoms of the survivors lined up with the symptoms of nephritis, there's no compelling reason to doubt this diagnosis.
So how do we know the pemmican caused the nephritis? Officially, we don't! However, we have a LOT of evidence indicating that it did. Niven does a great job documenting all of this in The Ice Master. We know that people have been surviving on pemmican in the Arctic for centuries without developing nephritis. We know that in order to be a nutritionally balanced survival food, pemmican needs to have a specific ratio of protein to fat. We know that Stef did not personally oversee the production of his pemmican, as some previous expedition leaders had done (which is especially hilarious considering that later in his career he would conduct some disastrous experiments involving feeding pemmican to United States troops, so clearly he had an interest in the stuff). We know he did not submit it to purity testing to ensure that it was safe and nutritionally balanced because he was in too much of a hurry. We know that the men strongly preferred the Hudson's Bay brand of pemmican over the Underwood brand because the Underwood brand made them ill, and they reached a point where they couldn't choke down any more of it, even though they were starving. We know that high fat and/or protein diets without carbohydrates can be very bad for your kidneys, especially if you have other preexisting medical conditions (like, for example, a weakened immune system due to exposure and starvation and stress).
I am not a doctor and I do not play one on the Internet, but if I had to guess, I would say there was a problem with the Underwood pemmican, most likely that the fat to protein ratio was off or it was somehow contaminated. This is also the conclusion that Niven reached, and her research for this book was impeccable, so I have no reason to doubt her! We will, of course, never know with complete certainty what caused the nephritis, but the men clearly thought it was the pemmican, and I believe them.
I'm sure this is WAY more than you ever wanted to know about pemmican, but if you want to know more, I can hook you up with some more sources! If you're interested in polar foods in general, check out Hoosh by Jason C. Anthony, which focuses specifically on Antarctica, but there's definitely some overlap with the Arctic! And I hope this helps!
17 notes
·
View notes
Text
Knowing the 17 exist is the first step

G = 7, O = 6, D = 4 = 17
Funny my moms new dog she just got she named Truman. I think we have established the importance of the 17 up to this point and how it creates the shape of a door. We can endlessly extrapolate upon this number and find more mathematical or logical proofs of its importance. From the Holy Bible to Pi 3.14 to the numerology of our letters.
The numbers 1/7 = 0.1428571428571429 makes is not the most important part. Just knowing it exist is the first step to escaping the matrix and your 3D limitations.
Everything boils down to BELIEF, you must beLIEve in the LIE. I had to LIE to myself for a very long time for many years. I didn't want to accept what was happening to me was actually happening. Everyone around you will call you crazy, you need medication etc. Everything and everyone around you will tell you are WRONG. And what you are believing is INCORRECT.

Just be a good little sheep and follow the herd. The problem with that is I never liked listening to authority. I think my longest civilian job outside of the army only lasted 5 months. I knew there was something wrong with the world I just couldn't put my finger on it. Luckily my OCD for understanding the truth out weighed every other thing in my life including family life, health, social norms, relationships, etc. I've actually never been on a vacation before and here I am at the age of 40.
Yes I have been very obsessed with seeking the truth. Now that I finally found the Holy Grail I am sort of picking up the pieces of my life and trying to repair the damage I caused by being so obsessed with this journey. Luckily I am single with no kids and the only beings relying on me is my 2 cats. I am exercising a lot more since my health plummeted coincidentally a week or two after getting baptized at the age of 33 in 2018. I got diagnosed with Bechet's Disease which causes inflammation of the blood vessels. I was in an out of the ER 5x that year, I won't go into the details but it was pretty bad.
It can cause all sorts of ailments but it can go into remission. I've fixed 90%+ of my health problems by just using a foot stool in the bathroom, making homemade kefir and drinking yerba mate. The last part of correcting my health is increasing exercise and cardio. I have created a Bechet's Disease Research group on Facebook and I do believe I've narrowed down the causes. One part is the lungs I smoked off and on from the age of 19 up to around 31. Another is not exercising enough, gut microbiome (was damage due to long term antibiotic use in 2010 which started my first symptoms of Bechet's), the adrenals and I believe phosphates in the foods plays a big part which affects the kidneys. Astragalus is supposedly one of the best herbs for the kidneys.
I notice a big improvement in my energy levels when I take my multivitamin, magnesium, chlorella/spirulina and get more sunlight. https://amzn.to/4ducxFE

I thought God hated me especially since all these underlying conditions manifested right after being baptized. Looking back now I realized it was an important physical and mental test of rebuilding myself and learning how to repair the damage I did to my body. God sent me the answers that I needed to solve my health problems and rebuild myself. I was actually experiencing shooting pains in my abdomen for months around 2020 and I was 1 day away from going to the ER for it.
I prayed to JESUS on Friday night and the next day that shooting pain magically went away. I was able to make that pain completely disappear once I added a stool for my feet in the bathroom and started incorporated homemade fermented kefir into my diet. The stool helps by lowering your cortisol and stress on your organs.
Now your probably saying, so you were healed after praying to JESUS and now you want us to believe in this Toilet God fantasy you're weaving? Exactly! During my 11 year trials I was attacked by a lot of evil. That evil demonic energy would actually laugh at me and make fun of me for calling out to JESUS for protection or help. Like oh God here he goes again calling out to Jesus to save him...
But in the end I always did the same thing for protection. Until this last time in 1/7/2023 where I was finally able to push higher past the jeSUS avatar and realize they are there to hide Gods ultimate truth. Don't get me wrong there is a great deal of power in JESUS name but they are not the ultiMATe truth.
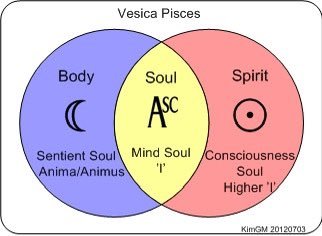
Jesus or the Jester is a better name. Gods true persona is one of a clown or jester entity. The energy that flows outwardly from the Vesica Piscis or the vessel of the fish (Jesus fish) is a CLOWN energy. God is closer to that wink or that JINX than JESUS. God embeds a lot of their truth spread out through all religions and spiritual practices.
Its just most of it gets diluted overtime to the point it becomes no longer helpful. This is why GOD wants to bring Toiletology to the masses. The world needs a wake up call. With more and more moving away from God a joke/parody religion is the best method to bring their truth like a trojan horse in disguise!
How can a silly parody/joke religion created by a comic book writer actually have any Godly truth within it?
I'm starting to realize now that I have done the crucifixion slowly over this past 11-12 years. Going through these past battles especially the one in fall 2023 where I had to fast for 40 days into another 40 day battle was hell. It honestly felt like I could keel over at any moment. I keep talking about how to reach my level of understanding you need to do this 11 year journey as well.
I been asking God about this lately, how can the average person handle this without experiencing everything I have over my entire life? My time in the army, at war, my paranormal experiences when I was a teenager, my intuition and constantly searching etc.?

I am realizing now that I may of already done the work for y'all. And all that is left is for you guys to harmonize off of my words and the message I am bringing to you through Toiletology or my "ministry." I am mostly just an artist, I am no savior figure. I am just somewhat good at creating great art that may resonate with a large amount of people. I also don't like a lot of attention and tend to avoid people. You can find me alone and in hermit mode 99% of my life. I have spent much time in solitude trying to understand God. Many years just quietly meditating and not much else.
My one friend I was training last December in 2023 for a few weeks said he could feel the sauce/slack or the ACE as I like to call it. The drugged out energy you feel when you are on the right track and harmonizing with God perfectly to reach your full potential. It took me 10+ years to feel that on my own. If what my friend was telling me it means that you guys made not need to go through all the grueling test God put me through. My friend was willing to join the church and I actually promoted him to the second rank while he was here with my fencing saber.
You may get a watered down version of this 11 year journey and basically ride my coat tails to the top or through the gates of heaven. Because I can provide you with all the answers you seek without you doing any of the work. Maintaining 4D awareness requires an insane level of belief. I imagine you will still have battles you must overcome to reach the level of belief required. Toiletology I believe will accelerate this process for you. Everyone is already on this journey, they just don't realize they are. Toiletology is like a compass/map that can point you in the correct direction you should be looking. To better help you navigate this tangled web that God weaves.

The main thing this journey has taught me is mastery of being insane. You need to be so insane that you actually go around the swing set inside out and become sane again. Basically being so bat shit insane but still being a "normal" functioning human being. Not mindlessly bumbling nonsense all over the place.
The truth is not that complicated. There is a higher level of awareness or reality. It is possible to tap into this reality and extra senses. Its definitely more than 6 senses, but the 6th sense is definitely your ability to communicate telepathically. Accessing the Akashic Records, lucid dreaming, astral projection or remote viewing you could probably lump all into this same 6th sense.
I think its all connected, it all begins with developing your pineal gland. I am still developing new abilities and strengthening the ones I have now more and more. I still don't fully know what the upper limit of these abilities will be yet. No I don't think I will ever be able to fly in the physical world, but I do fly a lot in my dreams. Maybe astral projection flying is real in the astral realm. I haven't done that yet, so I am not sure.

It is possible to "meet" with others in the "mind" if you have the skill to connect telepathically so that you both can share, connect or bond with each other in this shared mind. You can't force yourself into another's mind, only if you both are trying to connect to each other will your thoughts and memories start to flow together. It can be kind of weird thinking another persons thoughts and vice versa. It is possible to pick up on a persons thoughts in close proximity.
One time at the movie theater I hat a black wool Amish looking hat and heard this guys thoughts where he said in his mind, "I should wear a hat like that." I responded out loud, "Might as well." And they looked at me perplexed, smiled and walked away laughing. These connections aren't so much being telepathic yourself, but God allowing these connections to happen since they can't be forced. No matter how good you think your telepathic skills are. If its meant to be it will happen.
youtube
Needless to say I am still fairly new to these enhanced capabilities. I am just 100% in full belief they exist because I use them and practice them daily for years now. I know anyone can reach these same abilities as I am not that special or super smart. Though I have my moments and sometimes my intelligence does feel like it has major jumps or increases quite a lot. But it does shrink back down and makes things difficult again. The brains neuroplasticity or ability to change and grow seems unlimited. You know what they say if you don't use it you lose it.
Most humans have limited beliefs in their God given abilities. Maybe they grew up with everyone telling them they aren't that smart so they started to believe that. Self defeating thoughts can really dim your light. It can be hard to believe in yourself even when everyone around you doesn't want you to.

That is the true challenge for me and for Toiletology. Figuring out the best methods for helping everyone reach their full potential and unlock their supernatural abilities and connect perfectly to God so they no longer need my guidance or training. The basic foundation is love, honor, truth and respect. Point blank if you aren't operating at least at that fundamental level everything else will never work.
I was thinking maybe you guys need to bring on your "spiritual helper" which was the start of my elven/eleven year journey. I am still waiting for more guidance and knowledge from the Toilet God. All I do know is there is power in the ranks of Toiletology. There's power in just joining the church, there's power in helping it grow. There's power in making a daily conscious effort to believe what I am saying is actually true and/or possible.
It all starts first with making that FREE WILL conscious decision to explore this as a new avenue for your spiritual growth. The 17 (doorway) exist to reach these higher realms. Believing is the hardest part. Toiletology will show you the correct method for living in harmony with God. As well as developing your spiritual powers/defense so that you can start to make the transition into 4D.
ALL I can say is buckle your seatbelts because your in for a wild ride Dorothy and Kansas is going bye bye! I am not exactly sure the full potential and power of Toiletology quite yet, only that I made the journey and have embedded that Jesus-esque power into the church I have created.
I guess we won't know until I start getting some more disciples...

Interestingly half of 432 Hz = 216 or 27/117/49/64
youtube
#toiletology#occult#alchemy#spirituality#religion#gematria#numerology#astrology#esoteric#mysticism#witchcraft#illuminati#Bechet's disease#Youtube
2 notes
·
View notes
Note
Hiyaa lovely mods!
First of all, thank you for making this blog! I have read a lot of the posts you have linked in the FAQ, but still have some questions I need help with.
I am visually impaired myself, and am autistic, but I'm not physically disabled, which is why I want to make sure I do proper research (which I will do myself, but I've found that I need some pointers) for a character I'm writing.
It is an Arcane fanfic, the character in question is Viktor. He was born with a limp and chronically ill due to growing up in 'a toxic atmosphere', which was caused by fissures (in Zaun).
In my fic he will be a veterinarian, but he will (still) be using a cane, and occasionally crutches or a wheelchair for low spoons/pain days. (I haven't been able to completely specify what diagnosis he has in my fic that matches canon, but I refuse to make him able-bodied.)
I have tried to find the name/type of a (manual) wheelchair that has a feature to push the user up to stand (for brief periods) after fastening the legs, but so far I haven't been able to find an answer. Since he'll have to go out on calls sometimes to ranches/farms, he needs to be able to treat large animals too, even on days where his cane or crutches aren't enough.
Could you possibly point me in the right direction so I can continue doing research? Either way, I thank you for your time to read this and for all the work you all do! <3
Kind regards,
Jeem
Hello, thank you for your ask! The type of wheelchair you’re looking for is called a manual standing wheelchair or a manual wheelchair with power stand up. Here are two sites that sell them if you need references [x] [x] (NOTE: I myself have not verified if these websites are safe to buy from, but they are safe to visit and have good photos!)
As for a starting place for deciding his disabilities, you can try looking up side effects of long term exposure to pollutants or radiation (just make sure what you’re reading is about the symptoms of chronic/long term exposure instead of acute).
Some common symptoms are:
- cancer
- asthma
- COPD
- cardiovascular disease
- issues with the kidney, lungs, brain, reproductive system and/or hormones
- immunodeficiency
And more!
And since I know a bit about Arcane, I’d like to mention that Viktor has hypertropia, which is when one eye points upward. It’s a small design detail so I understand a lot of fans missing it, but I just wanted to point it out because I appreciate it and hope any Arcane fans following consider adding it to their stories!
Here are two screenshots that I think show it well :] (smiley face


If you need any more help feel free to ask again!
Have a nice day!
Mod Rot
37 notes
·
View notes
Text










National Strawberries and Cream Day
Add the perfect mix of sweet and creamy to your celebrations this National Strawberries and Cream Day, which is held each year on May 21. Fresh strawberries and cream is a great treat to indulge in on a hot day. Plus, as these lovely red berries are in season in May, it is also National Strawberry Month.
History of National Strawberries and Cream Day
Strawberries have been traced back to the Roman Empire. Ancient Romans believed this fruit alleviated symptoms of melancholy, fainting, inflammation, fevers, throat infections, kidney stones, bad breath, attacks of gout, as well as diseases of the blood, liver, and spleen. However, food historians think the Greeks knew about strawberries even before this.
The fruit was also a symbol of wealth and luxury in Victorian England. As they were a perishable food, strawberries were only available in season, increasing their demand. After evolving into a luxury, they began to be served during afternoon tea among the wealthy.
History also tells the tale of how this fruit’s harvest and availability coincided with the Wimbledon tournaments, which is as much about strawberries and cream as it is about tennis. While we still don’t know exactly how this dessert became such an integral part of Wimbledon, some sources credit King George V as the one who introduced this delicious treat to the tennis tournament. Some believe the seasonality and popularity of these red berries played a part in it becoming Wimbledon’s snack of choice.
As for how this quintessentially British dish came to be, stories of its origin say Cardinal Thomas Wolsey, a close confidant to King Henry VIII, was the brains behind it. King Henry VIII’s court fed approximately 600 hungry lords and ladies twice a day. The chef there came up with the idea to pair sweet strawberries and clotted cream together in a dessert that did not require cooking, and voila, a delicious treat was born! Another version of this story says Cardinal Wolsey mixed these two ingredients at a royal banquet, and whatever the royals ate instantly became fashionable. It was even customary for newlyweds to eat strawberries and cream for their wedding breakfast!
National Strawberries and Cream Day timeline
1509 The First Time this Dish was Served
According to rumor, strawberries and cream are first served together by Cardinal Thomas Wolsey at a banquet during Henry VIII's reign.
1550 Its Popularity is Going Strong
Tudor traveler Andrew Boorde publishes an ode to this dish, saying, “Rawe crayme undecocted, eaten with strawberyes or hurtes (whortleberry, bilberry) is a rurall mannes blanket. I have knowen such blankettes hath put men in jeoperdy of theyr lyves.”
Late 18th century First Cultivated Garden Strawberry
What we now call the 'garden strawberry' is first cultivated in this period, in Brittany, France.
1877 Offered at the First Wimbledon Tournament
200 spectators at Wimbledon court are offered strawberries and cream.
2012 Tesco Launches a New Sandwich
British retail company Tesco launches a strawberry and clotted cream sandwich, made of slices of berries between two cream-layered pieces of white poppy seed bread, with a dollop of strawberry jam — this is no longer on the market.
National Strawberries and Cream Day FAQs
Is there a National Strawberry Day?
Each year, on February 27, America celebrates National Strawberry Day.
What months are strawberries in season?
As it is grown in varied locations around the world, strawberries are said to be in season from January to November.
Are strawberries hybrid?
A strawberry is actually a multiple fruit that is many tiny individual fruits embedded into one. Cultivated strawberries, which are hybrids of two parent species, can adapt to different weather and growth conditions.
What is National Strawberry Ice Cream Day?
National Strawberry Ice Cream Day is celebrated on January 15, to pay tribute to one of the choicest flavors of ice cream.
How To Celebrate National Strawberries and Cream Day
Make it, of course!
Read up on the history
Learn the different ways strawberries can be used
Cook a special strawberry and cream dessert your way. Eat it for breakfast, lunch, or even tea. If you want to mix things up further, you can add a little granola for texture, drizzle some chocolate sauce on top, flavor your whipped cream with amaretto liqueur, or even sprinkle some brown sugar on top. You can even channel your inner chef and create a trifle with alternating layers of strawberry, cream, and sweet pastry.
This day gives us a great chance to learn more about the strawberry and how this tempting treat came to be. Reading about the stories that (maybe) led to the creation of this dish, we see how cuisines from around the world can eliminate boundaries and borders.
Preserves! Jams! And much more … this one fruit can be turned into many versatile dishes to satisfy every sweet craving you ever had. Save some for celebrating National Strawberries and Cream Day, while the rest can be used in multiple different ways, as per your needs (or the demands of your taste buds).
5 Fun Facts About Strawberries
The only fruit with seeds on the outside
They herald the spring
They give your workout a little boost
They help your teeth look good too!
They are all over the world
A single strawberry has around 200 seeds, and each one has the genetic potential to become a new variety — that’s why breeders can develop so many varieties.
Strawberries ring in the spring season — in a way, they are the first fruit to ripen during this season.
Strawberries are rich in nitrates, and a study shows people who ate such foods before exercising burned 100 more calories than those who did not.
The fruity acids in these berries help remove stains, which can help whiten your teeth.
These berries are grown around the world and boast more than 600 variants.
Why We Love National Strawberries and Cream Day
Ode to the versatile fruit
This day promotes in-season eating
It makes us happy
We use this day as another excuse to worship this summer fruit. Refreshingly sweet (and sometimes a teeny bit tart), strawberries mixed with clotted and sour cream are a match made in heaven. We would happily celebrate every day as Strawberries and Cream Day if we could. Not only do they tickle our taste buds, but strawberries also bring us so many health benefits. From boosting immunity to increasing HDL (good cholesterol) and lowering blood pressure, strawberries provide us with an array of health benefits.
This day is celebrated in a month when these berries are in season, promoting sustainability and better consumer habits. Not only is in-season produce better for your health — a strawberry grown in May tastes much richer than one artificially ripened in another season — it also helps fulfill your body's needs as per the season's requirements. Plus, buying local is great for the environment, too. Think of how much fuel emissions you are reducing when you buy food that did not have to travel very far to get to you!
Popping these sweet and sometimes tart red fruits into our mouths is tantamount to a taste of happiness. Really! Strawberries are very rich in vitamin C, which is responsible for the production of endorphins in our brain, the hormone that makes you feel happy.
Source
#strawberries with panna cotta#Strawberry Shortbread#Eaton Mess#USA#Strawberry Milkshake#Strawberry Rhubarb Parfait#Berries&Cream#Sweden#dessert#restaurant#Canada#original photography#National Strawberries and Cream Day#21 May#food#NationalStrawberriesandCreamDay#travel#vacation#fruit#national day
3 notes
·
View notes
Text
tw pet death, animal death, grief
My cat is still very much alive! However, I'm coming to terms with her rapid decline. A lot of my days recently are centered around her treatments and vet visits and trying to get her to eat and stay comfortable. In the last three months she has gotten so slow and sick. Last year she had her first vestibular episode, and was (unrelatedly) diagnosed with hypertrophic cardiomyopathy. Four months ago it was hyperthyroidism. Three months ago it was chronic kidney disease which worsened from one month to the next. All of these require medicines, special foods, supplements, and other treatments several times per day in attempt to control symptoms and slow the progression of her kidney failure. I have so many alarms set and I don't leave the house for more than a few hours. I can't leave her alone.
I am overwhelmed. I am the only thing standing between my cat and a painful death. And I am the being in charge of being the person who decides when to let her go, to stop fighting, to end her suffering peacefully when it is time.
My cat has been a huge part of my life and existence for 18 years, since shortly before my 16th birthday. I have a big tattoo of her face on my left bicep. She's been around longer than half my life now; a constant companion when friends moved away and my closeness with others ebbed and flowed. Her long silky fur has caught endless tears and kisses both. I have become an adult with her by my side. When I felt homesickness on short trips, I thought of her. I never took long trips because I didn't want to be away from her for too long, even when she was healthy.
I literally cannot imagine a life without her. There is a blackness when I try to picture it. How will I sleep without her warm comforting presence? For whom will I get up in the mornings? My routines are almost all around her. She is my home and my dearest friend in this life.
At the same time I don't want to let her go, I am aware how blessed I am to have had 18 years of love and funny stories and sweet memories with her. That is such a long life for a little cat. Friends and family always come to pay respects and visit with her when they come over. She has an adoring family. And until fairly recently she was very healthy and happy.
She has lived a good life. It is a good life. It is up to me to make it a good end too. I owe it to her as thanks for making my life fuller every day. She is good and she deserves that kindness. I love her so much. And I will miss her fiercely for the rest of my days when the time comes, and it will come soon. Not years anymore. Months if we are lucky. Weeks if we are unlucky. But really. All of it was lucky. We found each other in this life. What luck that is. What love.
3 notes
·
View notes
Text

Credit: Dana Smith
Understanding The Sudden Rise of Type 2 Diabetes In Children
The Metabolic Disorder Was Long Known as a Disease of Adulthood. Now, It’s Spiking in Kids and Teens, With Worrisome Consequences.
— By Charlotte Huff | July 31, 2024
The appearance of type 2 diabetes in children and teens puzzled physicians from the start. Fida Bacha recalls working as a pediatric endocrinology fellow in Pittsburgh shortly after 2000 when young, overweight and obese patients began to arrive at the clinic, some describing increased thirst, more frequent trips to the bathroom and other symptoms of what was then called adult-onset diabetes.
“It was a new realization that we are dealing with a disease that used to be only an adult disease that is now becoming a disease of childhood,” says Bacha, who practices at Texas Children’s Hospital in Houston.
More than two decades later, physicians and researchers are still trying to unravel what’s driving the emergence and proliferation of youth-onset disease, particularly among marginalized communities including Hispanics/Latinos. The increasing prevalence of obesity among young people is clearly one contributor, but researchers are also scrutinizing the potential influence of other lifestyle and environmental factors — everything from exposure to chronic stress and air pollution to sugar-rich diets. Along with physiological factors, such as where they carry excess fat, youths from lower socioeconomic levels may be vulnerable due to aspects of daily life beyond their control, such as more limited access to healthy food and opportunities to safely exercise in less-polluted neighborhoods.
As researchers try to sort out the interplay among genetics, metabolic factors and environmental influences in Hispanic and other populations, their goal is to answer this key question: Why do some seemingly at-risk adolescents progress to diabetes while others do not?
Long-term, the challenges and health stakes are significant. When type 2 diabetes first emerged in youths, clinicians initially thought its progression would mirror that in adults and thus could be treated accordingly. That hasn’t panned out, says Barbara Linder, a pediatric endocrinologist and senior advisor for childhood diabetes research at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). For instance, researchers have determined that metformin, a commonly prescribed oral antidiabetic medication in adults, doesn’t work as well in young people.
“We know that the disease is very aggressive in youth and very difficult to treat,” Linder says. “So it’s really imperative that we develop effective approaches to prevention. And to do this we obviously need to be able to effectively identify which youth are at the highest risk.”
Even with treatment, young people develop other medical problems related to diabetes faster than adults, according to a study that followed 500 youths, more than one-third of them Hispanic. Sixty percent developed at least one complication within about 15 years after diagnosis, when just in their 20s.
“It’s really alarming,” says Luisa Rodriguez, a pediatric endocrinologist who studies type 2 diabetes and obesity in children at the University of Texas Health Science Center at San Antonio. For every 10 adolescents with youth-onset diabetes, she points out, “six of them, within a decade span, are going to develop a significant comorbidity that will highly impact their lifespan and quality of life.”

Complications of diabetes appear more quickly in young people than in older adults. Researchers studied 500 overweight adolescents, aged 10 to 17, who had been diagnosed with type 2 diabetes. Within 15 years of their diagnosis, 60 percent of the participants had developed at least one medical complication of diabetes, and 28 percent had developed two or more.
Insulin Resistance
In type 2 diabetes, the body struggles to use insulin effectively. This vital hormone, made by beta cells in the pancreas, helps glucose in the bloodstream enter cells in muscle, fat and the liver, where it’s used for energy. But sometimes those cells gradually lose their ability to respond to insulin, forcing the beta cells to pump out more and more of it. If the beta cells can’t keep up, blood glucose levels will begin to rise, leading to a diagnosis of prediabetes and, eventually, diabetes.
In the past, type 2 diabetes typically didn’t arise until well into adulthood. But now, cases in US youths ages 10 to 19 are rising fast. Since 2002-2003, overall diagnoses have doubled from 9 per 100,000 youths to 17.9 per 100,000 in 2017-2018, particularly among Asians, Pacific Islanders, Blacks and Hispanics. If those rising rates persist, the number of type 2 diabetes cases in young people is projected to skyrocket from 28,000 in 2017 to 220,000 by 2060.
Various factors have been linked to insulin resistance in childhood or adolescence, including obesity, inactivity and genetics, according to a review of the causes of type 2 diabetes in youths published in the 2022 Annual Review of Medicine. The disease tends to run in families regardless of race or ethnicity, which suggests that genes matter. Among US Hispanics, adults of Mexican or Puerto Rican heritage are most likely to be diagnosed, followed by Central and South Americans and Cubans.
Obesity is also a contributing factor: Slightly more than one-fourth of Hispanic youths are obese, a higher percentage than for any other major racial or ethnic group. Children also are more likely to develop type 2 diabetes if their mother has the disease or developed gestational diabetes during pregnancy. One theory is that fetal exposure to maternal diabetes while in the womb can spur metabolic changes following birth.
Puberty is also highly influential — most cases are diagnosed after its onset. During puberty, youths temporarily experience insulin resistance, due in large part to an increase in hormones, Linder says. Most youths offset that transient resistance by secreting more insulin, she says. But for reasons that are still unclear, a subpopulation of adolescents does not. “When they’re faced with this stress test of puberty, they can’t increase their insulin secretion enough to compensate,” Linder says. “And that’s probably why they develop type 2 diabetes.”
One analysis, which looked at type 2 diabetes trends from 2002 to 2018, identified the peak age for diagnosis as 16 years in boys and girls. The sole exception involved Black youths, in whom diagnoses peaked at 13 years, and possibly earlier among Black girls, which may be linked to an earlier start of menstruation.
American Diabetes Association guidelines recommend that clinicians screen overweight or obese youths for the disease starting at age 10 or once puberty starts, whichever is earlier, if they have one or more risk factors. These include a family history of the disease, signs of insulin resistance or affiliation with certain racial/ethnic groups, including Hispanic/Latino.
During checkups, clinicians can look for a visible sign of insulin resistance, an associated skin condition called acanthosis nigricans, says Paulina Cruz Bravo, a physician and diabetes researcher at Washington University School of Medicine in St. Louis. The skin changes tend to appear in the neck area or along folds in the skin, including in the armpits and on the elbows and knees, she says. “The top layer of the skin gets thickened. It’s described as a velvety appearance of the skin — it’s darker compared to the skin in other places.”

The thickened, darker, velvety skin shown here, known as acanthosis nigricans, is a potential warning sign of developing type 2 diabetes. The condition is likely to appear on the neck, elbows, knees and other areas where the skin folds. People who notice acanthosis nigricans on themselves or their children should bring it to a doctor’s attention. Credit: S. Dulebohn/Statpearls 2024
Where an adolescent carries any excess pounds also matters, as insulin resistance has been associated with a type of fat called visceral fat, says Alaina Vidmar, a pediatric endocrinologist at Children’s Hospital Los Angeles. Unlike the more common type of fat, called subcutaneous and felt by pinching around the waistline, visceral fat surrounds the liver and other vital organs, increasing the risk for type 2 diabetes, fatty liver disease and other conditions.
“You really need the liver to process glucose to be able to utilize your insulin well,” Vidmar says. “And if it is full of fat, you are unable to do that.” Fatty liver disease, which has been associated both with obesity and type 2 diabetes, is most common in Hispanic adults, followed by white adults and Black adults, according to a meta-analysis looking at 34 studies.
Imaging scans would be the ideal way to identify the extent and location of visceral fat in adolescents, Vidmar says. But given that routine scanning would be costly, clinicians can instead measure an adolescent’s waist circumference, “a great surrogate marker,” she says.

Diabetes risk depends not just on how much fat you carry, but where you carry it. People with an “apple” body shape, with much of their fat in the abdomen, are at higher risk of diabetes than those with a “pear” body shape, who carry their fat under the skin, especially on the hips.
Still, obesity accounts for only a portion of the type 2 risk profile, reflecting the complexities involved in understanding the pathophysiology of youth-onset disease. Roughly one-fourth of youths with type 2 diabetes are not obese, according to a meta-analysis published in 2022 in JAMA Network Open. Asian youths are least likely to be obese; roughly one-third don’t meet the criteria for obesity.
Moreover, while obesity and insulin resistance boost the risk of developing diabetes, those factors alone don’t predict whether an adolescent is eventually diagnosed with the disease, according to the authors of the Annual Review of Medicine overview. Instead, they point to the role of impaired beta cell function.
In one study involving 699 youths with type 2 diabetes, the standard antidiabetic drug metformin controlled blood glucose levels in only about half the participants. (The medication was least effective among Black youths, for reasons that are unclear, according to the researchers.) Another analysis of the same study population identified a 20 percent to 35 percent decline in beta function each year in diabetic youths, compared with prior studies showing about a 7 percent to 11 percent annual decline in diabetic adults.
“What we see in the youth is that beta cell function fails very rapidly,” Linder says, adding that the beta cell decline tends to correlate with the lack of response to metformin.
It’s unknown whether specific racial or ethnic groups are more vulnerable to loss of beta cell function, says Linder, who hopes that a new large-scale NIDDK study launching this summer will identify any such physiological and other differences among populations. The study, called Discovery of Risk Factors for Type 2 Diabetes in Youth Consortium, aims to enroll 3,600 overweight or obese adolescent boys and girls, 36 percent of them Hispanic. Bacha and other investigators on the project plan to follow the youths through puberty, looking at genetic and physiological markers such as insulin resistance and beta cell function. Their goal is to track who develops type 2 diabetes and what factors precipitate the disease.
In addition, researchers will learn about the participants’ mental health, lifestyles and social determinants of health, Linder says. To that end, families will be asked to share details about nutrition, physical activity and sleep, as well as food insecurity, exposure to racism and other stressors.
“Stress induces certain hormones that antagonize insulin, so they create more insulin resistance,” Linder says. “Stress also is associated with chronic inflammation in the body, which affects the ability of the body to respond normally.”

Young people experience many of the risk factors that predispose people to type 2 diabetes, such as prenatal exposures, junk food, sedentary lifestyles and high levels of stress.
Zooming in on Risk Factors in Hispanic Kids
Already, researchers who have studied at-risk Hispanic youths and their families have begun to flesh out environmental and other influences rooted in daily life that can boost the likelihood of obesity or diabetes. Michael Goran, a child obesity researcher at Children’s Hospital Los Angeles, has led a research project called the Study of Latino Adolescents at Risk (SOLAR), which tracked 328 Hispanic/Latino youths considered at highest risk of youth-onset diabetes based on their body mass index and family history of the disease. The participants, recruited in two waves between 2000 and 2015, completed health questionnaires and underwent annual exams, including imaging scans and other measurements.
One analysis found that Hispanic youths who lived in neighborhoods with higher levels of air pollution were more likely to experience a breakdown in beta cell function. “Which we weren’t necessarily expecting — we don’t know the mechanism of that,” says Goran, who coauthored a close look at pediatric insulin resistance in the 2005 Annual Review of Nutrition.
In more recent years, he’s turned his attention to studying nutrition shortly after birth, with a focus on infant formulas that contain corn syrup. Those formulas are more likely to spike blood sugar than are lactose-based formulas, he says. “If you’re spiking blood glucose with corn syrup in babies,” he says, “you can see how that would be problematic for long-term control of blood sugars.”
In one study, Goran and colleagues looked at obesity trends in 15,246 children who received formula through the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Babies who consumed any formula with corn syrup were 10 percent more likely to be obese by age 2 than babies who didn’t. Nearly 90 percent of the study’s participants were Hispanic.
In other research, epidemiologist Carmen Isasi of the Albert Einstein College of Medicine in New York helped lead the Study of Latinos (SOL) Youth study, which delved into the extent to which a child’s family circumstances contribute to obesity and metabolic changes that may boost risk of youth-onset diabetes. Isasi and colleagues found chronic stress to be pervasive. Three-quarters of parents and caregivers reported stress and 29 percent detailed three or more stressors related to health, work or relationships. The higher the number of parental stressors, the more likely the child was to be obese.
Isasi also has looked at the relationship between food insecurity and metabolic health. Hispanic youths raised in households with the highest levels of food insecurity had significantly worse metabolic results, including elevated blood glucose and triglycerides, a type of cholesterol. Families dealing with food insecurity, Isasi says, probably have a lower-quality diet and skimp on costlier protein and fresh produce.
Preventing diabetes has proved challenging. A review paper looking at diet-related and other lifestyle initiatives targeting Hispanic youths found few studies to date that have shown improvements in body mass index or blood glucose levels.
Adolescents of lower socioeconomic status may also shoulder responsibilities that can undercut efforts to stay healthy, says Erica Soltero, a behavioral scientist at Houston’s Baylor College of Medicine, who works with Hispanic youths. For instance, older teens may struggle to attend an exercise class if they have an after-school job or must pick up younger siblings or start dinner. Technology, Soltero says, may be a better way to reach busy Hispanic teens; she’s piloting a study that will provide text-based lifestyle guidance to Hispanic teens with obesity.
Approved medication options remain limited for children and teens. If metformin doesn’t work, the alternative is insulin, and parents may resist giving injections because of the difficulties involved, Rodriguez says. She’s involved with an ongoing study in youths with type 2 diabetes to study the effectiveness of oral semaglutide, one of the newer diabetes drugs that also has achieved notable weight loss. Rodriguez estimates the results will be available by 2026.
The new NIDDK study won’t assess medication treatments, as it’s an observational study. But researchers involved are bullish that study-related insights could lead to better prevention and treatment approaches. “If someone is predisposed to beta cell dysfunction, should we be much more aggressive in treating their overweight/obesity,” Bacha says, “so that this beta cell function is preserved for a longer period of time?” Doctors could, for example, decide to start treatment earlier, she says.
Neither are researchers like Soltero deterred by the long-standing difficulties involved with revamping lifestyle habits. Soltero, who has worked with overweight and obese Hispanic adolescents to improve exercise and make dietary changes, describes them as often highly motivated given the damage they’ve seen the disease inflict on their own families.
“A lot of times they’ll have a touch point with a relative who’s on dialysis and maybe had a digit amputated,” Soltero says. Or “they’ll say, ‘I don’t want to prick myself every day like my Uncle So-and-So.’ Or ‘I don’t want to be on medicine for the rest of my life like my grandma.’ ”
#Knowable Magazine#Diabetes#Type-2 Diabetes#Charlotte Huff#Children#Metabolic Disorder#Disease of Adulthood#Spikining Diabetes | Kids | Teens#Epedemiology#Food | Environment#Health & Disease#Nutrition#Public Health#Society
2 notes
·
View notes
Text

So. I'm super fucking rare, ya'll!
Above is a picture of the literal genetic mutation that I have. It's so rare that it's only been reported in ONE medical article as a bynote of a patient within a study- and a link to said study. It's so rare that genetic databases don't even have a frequency for it... Because it's so fucking rare (and genetic testing is still expensive and prohibitive to a lot of people).
Basically, it's a mutation that causes my kidney to not regulate my blood pressure correctly. Yeah, did you know that your kidneys regulate your blood pressure?! I mean, I did, but I'm wondering if you did.
This mutation causes Liddle's Syndrome, but my mutation is so rare that my symptoms don't entirely match up with the disease. Which is why it has taken doctor's 36 years to diagnose me- but, not really diagnose me, because I don't see my actual doctor until Friday... But, it's pretty clear that the mutation causes issues. So. Yeah.
It's incurable. There are only two drugs approved for its treatment- and they are rather cheap, so that's nice.
I feel like Dorthy Zbornak (Golden Girls) after she got her diagnosis of chronic fatigue syndrome. I had been blown off by doctors for YEARS because I was young and, somewhat, average in weight. I had insane blood pressure and they just... Ignored it? When I pointed out to a doctor that I still had high blood pressure after they increased the dosage of meds (that didn't work), she literally told me in the most condescending voice- "What do you want, more pills?" She also told me that I couldn't be having migraines because they lasted more than four hours and- "Migraines don't last more than four hours, you have something else." A cardiologist told me over a ten minute zoom call that I was fat and stupid, and that was why I had high blood pressure before changing a med that I took for ANXIETY to a different drug that turns out has been upsetting my gastrointestinal track for the last year (and also didn't work). It was the first time I met her. And, she told me to follow up in a week, which I couldn't and never did because she literally never had an open appointment slot over the following YEAR!
And if it needs to be said, this was in America.
But, I probably have a diagnosis now.... So, I can be a case study? Fun.
#medical trauma#liddle's syndrome#hypertension#medicine#healthcare#chronic illness#I never wanted to be special#But it was thrust upon me#and it fucking sucks.
4 notes
·
View notes