#diabetic nephropathy
Text

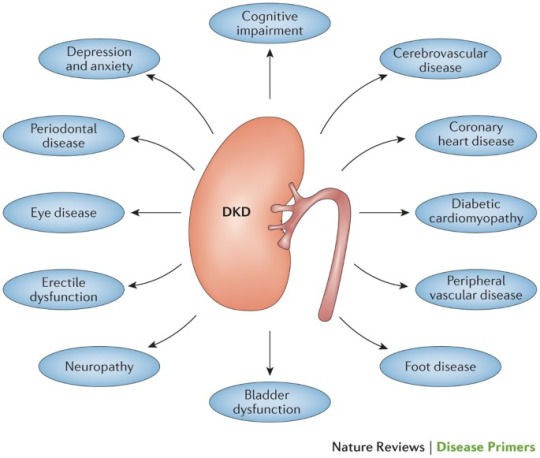
10 Complications of Diabetes Mellitus
Diabetes is a metabolic disorder, caused by the body’s inability to use the insulin produced by its own pancreas or insufficient insulin production. As glucose begins to accumulate in the bloodstream, it begins to damage the blood vessels in organs large and small across the body.
Read more how to Reduce Complication of Diabetes: https://www.freedomfromdiabetes.org/blog/post/10-complications-of-diabetes-mellitus/2713
#10 Complications of Diabetes Mellitus#Diabetes and Alzheimer's Disease#Diabetic Nephropathy#Diabetes and Cardiovascular Disease#Diabetic Retinopathy#Diabetic Neuropathy#Diabetes and Oral Health#Diabetes in Pregnancy#Diabetes and infertility#Diabetes and Hypertension#Obesity and Diabetes#complications of diabetes mellitus#chronic complications of diabetes mellitus#long term complications of diabetes
0 notes
Text

Dr. Mudit Khurana, a seasoned Nephrologist and Renal Specialist, boasting an impressive 9-year journey in this domain. His educational foundation is robust, having accomplished MBBS from MGM Medical College, Indore in 2012, followed by MD in General Medicine from University College of Medical Sciences, Delhi University in 2015. Dr. Khurana’s pursuit of excellence led him to achieve DM in Nephrology from Sanjay Gandhi Postgraduate Institute of Medical Sciences in 2020. Dr. Mudit Khurana stands as the best nephrologist in Agra, showcasing unparalleled expertise in renal care. His proficiency extends to being the finest kidney specialist in Agra, bringing forth a combination of years of experience and exceptional education
Chronic Kidney Disease
Acute Kidney Failure
Diabetic Nephropathy Kidney Infections (Pyelonephritis) Cystic Kidney Disease Kidney Stones Glomerulonephritis Urinary Tract Infection Hypertension Dedicated Nephrology Practice Complete Solutions to Patient
#Chronic Kidney Disease#Acute Kidney Failure#Diabetic Nephropathy#Kidney Infections (Pyelonephritis)
1 note
·
View note
Text
Ce médicament est un « bon médicament » pour prévenir l’apparition de l’urémie ! L’utilisation précoce présente de nombreux avantages!
1 note
·
View note
Text
Clinical Diagnostic Recommendations for DKD
Exclusion of Non-Diabetic Kidney Diseases
The guidelines from the American Diabetes Association (ADA) in 2022, the Kidney Disease Improving Global Outcomes (KDIGO) organization in 2020, and the Asia-Pacific Society of Nephrology (APSN) in 2020 all assert that Diabetic Kidney Disease (DKD) refers to the occurrence of proteinuria and/or renal function decline in diabetic patients, with the exclusion of kidney damage caused by other underlying reasons.
In actual clinical diagnoses of DKD patients, a subset frequently presents with coexisting non-diabetic kidney diseases (NDKD). This may include scenarios where diabetes or DKD coexists with conditions like IgA nephropathy, membranous nephropathy, lupus nephritis, hepatitis B-related nephritis, vasculitis-related kidney injury, and even renal amyloidosis.
A meta-analysis incorporating 48 studies, involving 4,876 cases of kidney biopsies in DKD patients, revealed a non-diabetic kidney disease (NDKD) occurrence rate of approximately 36.9%. The occurrence rate of diabetic nephropathy (DN) combined with non-diabetic kidney disease (NDKD) was about 19.7%. Consequently, the guidelines recommend that before diagnosing DKD in type 2 diabetes patients, a comprehensive assessment, incorporating medical history, clinical manifestations, relevant laboratory tests, especially serum immunology, and imaging examinations, should be conducted to rule out non-diabetic kidney diseases (NDKD). Only after excluding NDKD can a diagnosis of DKD be confirmed.

Measurement of Urinary Albumin/Creatinine Ratio (UACR) and eGFR
Internationally, guidelines from organizations such as the American Diabetes Association (ADA) in 2022, the Kidney Disease Outcomes Quality Initiative (KDOQI) in 2007, the 2021 Clinical Diagnosis and Treatment Guidelines for Diabetic Kidney Disease, and the 2021 edition of the Chinese Guidelines for the Prevention and Treatment of Diabetic Kidney Disease recommend the repetition of UACR and eGFR measurements three times within a 3–6 month period. A clinical diagnosis of Diabetic Kidney Disease (DKD) is considered when, during these repeated measurements, UACR increases (>30mg/g) and/or eGFR falls below 60mL/min/1.73m² on two or more occasions. However, it is important to note that factors such as intense physical activity, infection, fever, congestive heart failure, etc., can cause transient proteinuria.
Taking into account domestic and international guidelines, after excluding factors causing transient proteinuria, a diagnosis of DKD can be established if, during the 3–6 month period with three repeated measurements, UACR increases (>30mg/g) and/or eGFR is consistently below 60mL/min/1.73m² on two or more occasions.
In clinical practice, some DKD patients may not meet the diagnostic criteria based on urine tests, but their eGFR is below 60mL/min/1.73m². The 2021 Clinical Diagnosis and Treatment Guidelines for Diabetic Kidney Disease, the Chinese Guidelines for the Prevention and Treatment of Diabetic Kidney Disease (2021 edition), and the 2022 ADA guidelines suggest that after excluding factors such as infection, obstructive kidney disease, medications, malignant hypertension, and other causes of acute kidney injury, a diagnosis of normoalbuminuric diabetic kidney disease (NADKD) can be made if, during the 3–6 month period with three repeated measurements, urine tests are normal but eGFR remains below 60mL/min/1.73m² on two or more occasions.
In a 2021 meta-analysis of 31 studies (including 18 cross-sectional studies, 11 cohort studies, and 2 case-control studies), the overall prevalence of normoalbuminuric diabetic kidney disease (NADKD) in patients with type 2 diabetes and chronic kidney disease (CKD) was 45.6%. Within the DKD patient population, the prevalence of NADKD was 24.7%. A long-term follow-up study also found that regardless of proteinuria, diabetic patients with CKD stage 3 or later could experience varying degrees of further decline in kidney function after 10 years.
0 notes
Text
Managing Diabetic Nephropathy Treatment During Fasting
As the holy month of Ramadan approaches, it is important for individuals with diabetic nephropathy to be extra cautious about their health. Diabetic nephropathy is a serious complication that affects the kidneys of people with diabetes. It is characterized by damage to the small blood vessels in the kidneys, leading to kidney failure if not managed properly.
During fasting, it is crucial to…

View On WordPress
0 notes
Text
Is Diabetic Nephropathy Reversible?
Diabetic nephropathy is a common complication of diabetes that affects the kidneys. It is a type of kidney disease that occurs when high blood sugar levels damage the blood vessels in the kidneys, leading to kidney damage and eventually kidney failure. One common question that many people with diabetic nephropathy ask is whether the condition is reversible. In this article, we will explore this question and provide some insights into the management and treatment of diabetic nephropathy.
Is Diabetic Nephropathy Reversible?
The short answer is that, unfortunately, diabetic nephropathy is not reversible. Once the kidneys have been damaged, the damage is usually permanent. However, this does not mean that there is no hope for people with diabetic nephropathy. There are several treatment options available that can help slow the progression of the disease and improve the quality of life for people with the condition.
Treatment Options for Diabetic Nephropathy
The treatment options for diabetic nephropathy are focused on managing blood sugar levels and controlling blood pressure to help slow the progression of the disease. Some of the most common treatment options for diabetic nephropathy include:
Blood sugar control: One of the most important steps in managing diabetic nephropathy is to control blood sugar levels. This can be achieved through a combination of diet, exercise, and medication. Keeping blood sugar levels within the target range can help slow the progression of the disease and prevent further damage to the kidneys.
Blood pressure control: High blood pressure can damage the blood vessels in the kidneys and worsen diabetic nephropathy. Controlling blood pressure through lifestyle changes and medication can help slow the progression of the disease and protect the kidneys.
Medications: There are several medications that can be used to treat diabetic nephropathy, including angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs). These medications can help protect the kidneys and slow the progression of the disease.
Dialysis and kidney transplant: In some cases, diabetic nephropathy may progress to kidney failure, which requires dialysis or a kidney transplant. These treatments can help manage the symptoms of kidney failure and improve the quality of life for people with the condition.
Conclusion
In conclusion, diabetic nephropathy is a serious complication of diabetes that can lead to kidney damage and kidney failure. Unfortunately, once the kidneys have been damaged, the damage is usually permanent and cannot be reversed. However, there are several treatment options available that can help slow the progression of the disease and improve the quality of life for people with the condition. It is important for people with diabetic nephropathy to work closely with their healthcare team to manage their blood sugar levels, control their blood pressure, and follow a treatment plan that is tailored to their individual needs. With proper management and care, people with diabetic nephropathy can live full and healthy lives.
0 notes
Text
Lupine Publishers | Lymphocele after Renal Transplantation: A Contemporary Review and a Modern Approach for Prevention and Treatment

Abstract
A lymphocele is a common finding after renal transplantation. The majority of patients are asymptomatic. However, once a lymphocele has become symptomatic, this condition has to be treated. Lymphoceles may originate either from the lymphatic system of the recipient or the transplanted kidney. The most sensible measures to prevent their occurrence therefore seems to be to restrict the transplant bed to the smallest permissible level with careful ligature of the lymphatic vessels in the area of the kidney hilum.
Therapy of a lymphocele after renal transplantation should commence with minimally invasive measures and continue with invasive procedures only if these are unsuccessful, namely, puncture and drainage then sclerotization, and then laparoscopic or open marsupialization.
Keywords: Lymohocele; kidney; transplantation; recipient
Introduction
Lymphocele is a well-known complication of renal transplantation occurring in 0,6% to 22% of the recipients [1- 4]. Lymphocele may require surgical intervention because of the complications they cause urinary obstruction, leg edema, deep vein thrombosis, pelvic discomfort, herniation, and lymph leakage through the wound [5]. There are many contributing factors to lymphocele occurrence after kidney transplantation. One of these is donor renal lymphatics. It has been proposed that meticulous ligation of severed lymphatics of the kidney graft in the back table especially in the laparoscopically procured kidneys may decrease the lymphatic complications after transplantation [6].
Although various methods of diagnosis, management, and prevention have been discussed in the literature, the primary focus has been on treatment and no review has summarized all issues together. The aim of this study was to summarize the current strategies for the prevention and management of lymphoceles.
Etiologies and surgery related factors
The development of lymphoceles after renal transplantation is well documented. The etiology of lymphoceles remains unclear, although they are present in all kidney transplant experiences [7]. The old controversy whether lymphocele is the result of lymph leakage from either the severed recipient iliac lymphatic vessels or the grafted kidney lymphatics seems to favor the latter [8]. A physiological review shows that lymphatic capillaries are more abundant in the kidney cortex compared to the medulla. They run along the intralobular, arcuate and interlobar arteries; not only beside theses arteries but also within their walls [9]. At the renal hilum, 2 to 5 lymphatic ducts are found in close proximity to the main vessels (renal artery and vein).
The well-known and commonly cited contributing factors for lymphocele formation include: the type of immunosuppression used [10], high dose steroid use, use of diuretics, extensive perivascular dissection of the iliac vessels, acute rejection episodes, delayed graft function, source of graft (cadaveric vs living related donor), the etiology of the patient’s renal failure such as adult polycystic kidney disease, re transplantation, and some pediatric population [2, 7, 11].
Concerning the pediatric population, in a retrospective single institution review of 241 pediatric kidney transplants performed from 2000 to 2013; Giuliani et al. showed that older age (≥11 yr), male gender, BMI percentile for age ≥95%, and multiple transplantations were Significant risk factors for lymphocele formation [12]. The formation of post-transplant lymphoceles obviously originates in the surgical transection of lymphatic ducts. As demonstrated by lymphangiography two sources of lymphatic leak have been proposed: injured lymphatics in recipient’s iliac space and injured lymphatics in the kidney graft [13,14].
A possible distinction between these two origins is feasible by analyzing their composition. In fact, reports showed higher levels of creatine kinase in lower limbs lymphatics vessels compared to renal lymphatics [15-17]. It was believed that the perivascular lymphatics dissection along the iliac vessels was a determining factor for lymphocele development, and that lymphocele could be prevented by ligation of these vessels. Despite many reports showing absence of lymphocele after an accurate ligation of the iliac lymphatics [18], things are still unclear. Many studies were published concerning the influence of some surgical aspects in decreasing the lymphocele incidence. Indeed, one prospective study suggested a cephalad implantation of the renal graft using vascular anastomoses on the common iliac vessels to minimize lymphocele incidence, but this technique has not yet gained wide exposure [11]. The same concept was reevaluated in another study. This time, a significant reduction of the incidence of lymphocele from 8.5% to 2.1% was noted in 140 patients operated with the new technique versus 140 patients in the control group operated with the standard method [14].
Another retrospective study done by Saidi et al, evaluated the impact of laparoscopic living donor nephrectomy on lymphatic complications after kidney transplantation. They concluded that the incidence of prolonged lymphatic leak is higher in recipients who received kidney grafts procured laparoscopically. These observations may indicate that the major source of persistent lymphatic leakage is lymphatics of the allograft rather than severed recipient lymphatics. More meticulous ligation of severed lymphatics of the kidney graft in the back table, especially in the laparoscopically procured kidneys, may decrease the lymphatic complications after kidney transplantation [13]. To our date, many researchers are still questioning whether surgical preparation of the kidney with accurate ligature of the hilar lymphatic vessels would effectively reduce its incidence. Hence, a clear answer is reported in our study favoring lymphatic vessels ligation over non preparation of the kidney graft on lymphocele incidence. Indeed, acute rejection rates dropped significantly from 15 to 6.3%, and incidence of symptomatic lymphocele decreased from 17.5% to 0%.
Diagnosis and Clinical Aspects
Ultrasound is currently the preferred method for diagnosis of lymphoceles after the renal transplantation. In complicated cases, radioisotope imaging, computed tomography and magnetic resonance imaging are additional methodologies commonly used [5]. Lymphoceles may lead to deterioration of renal function and the patient with a lymphocele may be inappropriately treated for allograft rejection. Other clinical findings associated with lymphoceles in renal allograft recipients include lower abdominal swelling or mass, edema over the allograft or of the ipsilateral leg, hypertension, drainage from the incision, enlarged allograft, fever without an obvious source of infections, urinary frequency, ipsilateral ileo femoral thrombo phlebitis, and weight gain [4].
Prevention
Prevention of lymphocele formation primarily involves the best method for controlling perivascular lymphatic leaks. A study comparing surgical ties to ultrasonic devices in the surgical dissection technique for control of lymphatics failed to show a statistical advantage to either technique when groups were compared based on patient age, gender, graft source, or repeat transplant [19].
Berardinelli et al. demonstrated the effectiveness of a synthetic polyethylenglycol(PEG) sealant to prevent lymphocele formation after kidney transplantation [20].
Treatment
Lymphoceles are usually asymptomatic and diagnosed incidentally by ultrasound. In most cases, lymphocele disappear spontaneously without any need for a treatment. Several important factors can guide our choice of treatment: severity of the symptoms, lesion size, potential post-therapeutic complications, and the clinical condition of the patient. For the conservative treatment of posttransplant lymphoceles, percutaneous needle aspiration, continuous drainage over a period of time via various kinds of catheters, and sclerotherapy with various agents have been proposed [21].
Aspiration
Ultrasound-guided aspiration can be used as a diagnostic tool or treatment. to both diagnose and treat a lymphocele. It can be used as the initial treatment modality to relieve urinary obstruction, recover kidney function, and prevent emergency situations. Although simple, safe, and economical, a repeated treatment may be necessary with a low a low risk of infection in each aspiration. A systematic review by Lucewicz et al. [4] looking at over 20 studies, reported that simple aspiration alone has a recurrence rate ranging between 10% and 95% [ 22].
External drain placement
A lymphocele can also be treated by external drainage by placing a drain. However, this procedure takes a long time and can cause problems related to major fluid loss and secondary infection (particularly in immunosuppressed transplant recipients). External drainage has an efficacy of 50% and a recurrence rate of 20%–60% [23].
Sclerotherapy
The instillation of a sclerosing agent is another treatment approach. These include povidone iodine, fibrin glue, 95% ethanol, fibrinogen, bovine protease inhibitor, human thrombin, calcium chloride, gentamy sodium tetradecyl sulphate and tetracycline]. The sclerosing agent has been instilled and kept in situ for varying periods ranging from 5 min to 24 h [24,25]. Tasar et al., reported a mean therapy duration of 17 days and a mean alcohol volume of 30 cm3 per session. Out of 18 cases, there was one recurrence, one graft loss, and ten minor complications including local discomfort and low- grade fever. The authors concluded that this method of sclerotherapy was safe and cost effective [25]. Another analysis of 30 lymphocele patients demonstrated that alcohol injection was a safe and cost-effective treatment, with a success rate of 94%. The authors reported two cases of recurrence and all complications were minor, including catheter-induced infections and catheter displacements [26]. Povidone iodine has been used also as a sclerotherapy agent with a failure rate of less than11%, but it takes 20–30 days for leaking to cease and iodine induced acute kidney failure may occur [27]. Limited success has been reported using tetracycline as a sclerosing agent [28].
Instillation of sclerosing agents improves the rate of success of percutaneous management; however, it may cause a dense scar around the renal transplant with potential problems in the longterm [21]. Continuous drainage as well as repeated instilling of sclerosants could be done if needed, by placing a percutaneous drain. However, the main problem encountered during repeated installation of sclerosants is the risk of introducing infection. Furthermore, several case reports have reported direct graft injury and graft loss as a result of sclerosant installation [25]. Hence, with the cost of repetition, it is worthwhile emphasizing that external drainage or sclerosing therapy are not correct options.
Post-transplant lymphoceles have also been treated with a combination of percutaneous aspiration and sclerotherapy. Although this reduced the recurrence rate, recurrences were still reported in 20% of cases [22].
-Surgery: Byron et al. [29] first described open surgical internal drainage in 1966, and these techniques have successfully been used in many patients; however, they still reflect an invasive procedure. The operative strategy is to perform a peritoneal fenestration through a laparotomy, minilaparotomy, or via a laparoscopic approach. Some authors suggest the use of an omentum flap to decrease the risk of lymphocele relapse, but others do not [30]. Open surgical drainage of lymphocele is required in the presence of infection (external drainage) or where laparoscopic fenestration is not possible (internal drainage to the peritoneum). The open procedure is safe and 100% effective because the lymphocele can be localized accurately. However, the recurrence rate is still 15%. This may be attributed to the high rate of lymph vessel injuries incurred during the open method. The recurrence rate of the laparoscopic method is lower (0%– 10%) because the rate of lymph vessel injuries is lower. Also, the hospitalization period is shorter in this method [31]. In a meta-analysis, Lucewicz et al reported that 12% of laparoscopic operations had to be converted to open surgery, due to technical difficulty in reaching the lymphocele, peritoneal adhesions, thick, impenetrable lymphocele capsule and injury to abdominal viscus [21]. Indeed, it would be helpful in some cases to use an intra-operative ultrasound can avoid organ injury during laparoscopy. Schips et al reported a technique by which the lymphocele was laparoscopically fenestrated under diaphanoscopic guidance and the lymphocele cavity was dilated through the injection of a sterile fluid. Using this approach, the authors were able to determine the exact site of the incision by detecting the light of the cystoscope [32]. Laparoscopic fenestration can cause intestinal herniation into the peritoneal window leading sometimes to strangulation requiring urgent intervention. However, in this era of laparoscopy, open drainage is only of historical importance. in addition, the effectiveness of the laparoscopic approach along with its, low recurrence rate, and low complication rate make it the treatment of choice when other methods fail [28].
Conclusions
Lymphoceles are common and well-known complications that occur in up to 26% of kidney transplant recipients. The cause of lymphocele formation is unclear, but it is believed to result from transection of the lymphatic vessels accompanying the external iliac vessels during transplantation surgery and subsequent lymph accumulation in a nonepithelialized cavity in the extra-peritoneal plane adjacent to the transplanted kidney. In order to prevent the formation of a lymphocele, preparative steps should be kept to the necessary minimum, and lymph vessels in the vicinity of the kidney hilus carefully ligatured. Therapy of a lymphocele after renal transplantation should commence with minimally invasive measures and continue with invasive procedures only if these are unsuccessful, namely, puncture and drainage then sclerotization, and then laparoscopic or open marsupialization.
For More Lupine Publishers Open Access Journals Please visit our Website:
https://lupinepublishers.com/index.php
For more Journal of Urology & Nephrology Studies articles please click here:
https://lupinepublishers.com/urology-nephrology-journal/index.php
#lupinepublishers#lupine journals#journal of urology & nephrology studies#renal replacement therapy#diabetic nephropathy#Dialysis#hemofiltration#submissions#articles#open access journals
0 notes
Photo
Nephrology is the subspecialty of internal medicine that focuses on the diagnosis and treatment of diseases of the kidney. Lexington Renal Care Physicians Services in Kentucky We provide services that help you with the prevention and treatment of kidney disease.
#Hypertension#Proteinuria and Hematuria#Diabetic nephropathy#kidney disease#Glomerular diseases#Acute and chronic renal failure#Inherited renal diseases#polycystic kidney disease#Evaluation#management of kidney transplant#recipients and donors#Disorders of fluid#electrolyte and acid-base#Nephrolithiasis#kidney stones#disorders of calcium#parathyroid hormone#Osteoporosis#metabolic bone disease#dialysis#In-center dialysis#peritoneal dialysis#home hemodialysis#nocturnal hemodialysis#Managing anemia#chronic kidney disease
0 notes
Text
everyone is in the hospital today. My aunt’s in her 10th hour of labor with this baby- at her own insistence, she refuses any alternatives. My grandma passed out in her living room on our way to get her to see my aunt. My brother was already in hospital, but had to be taken into the emergency room all of a sudden on our way over- we got a call from the hospital and thought it was something about the baby, but turns out one of the holes in his kidney has opened back up- apparently one appeared in his liver too. Its a lot right now.
Mom keeps yelling at me in the waiting area in between yelling at hospital staff- about incompetence in “these liberal run hospitals that care more about killing babies than birthing them” (her words, not mine) about dad leaving her behind with two kids and a house to take care of, about me not doing enough. She’s panicking. She was like this when they first discovered the holes in Ed’s kidney, she was like this when dad died. It still sucks. Everything sucks today. And I know nothing I do- even if I were to disappear- will help.
#personal#family drama#hospital#medical problems#nephropathy#non diabetic#ventricular septal defect#medical mystery
1 note
·
View note
Text
https://sajhi.com/blogs/70532/Diabetic-Nephropathy-Market-Research-Analysis-Business-Opportunities-and-Latest-Innovations
Diabetic Nephropathy Market Research, Analysis, Business Opportunities and Latest Innovations 2030
Diabetic Nephropathy Market share was valued USD 2.48 billion in 2021 and is expected to reach USD 3.43 billion by 2030 at 6.20% CAGR during the forecast period 2022-2030.
0 notes
Text
Ayurvedic Diabetic Nephropathy Treatment- Ayurveda Yogashram
Ayurveda Yogashram is a leading Ayurvedic Diabetic Nephropathy treatment center providing advice and guidance on the diagnosis, prevention in India
Full Details:- https://ayurvedayogashram.com/diabetic-nephropathy/

#diabetic nephropathy treatment#ayurvedic diabetic nephropathy treatment#best kidney failure ayurvedic treatment#nephrotic syndrome treatment#ayurvedic clinic#ayurvedic treatment#yoga center
0 notes
Text

Diabetic nephropathy: A serious complication of diabetes
High blood sugar affects almost every organ in your body, but the kidneys are perhaps the most susceptible. Diabetics are hugely at risk of kidney damage. But proper monitoring and a corrective lifestyle can help keep kidney problems at bay.
For more info: https://www.freedomfromdiabetes.org/blog/post/diabetic-nephropathy/2643
#diabetic nephropathy#diabetic nephropathy stages#treatment of diabetic nephropathy#diabetic nephropathy symptoms
0 notes
Text
Finding a Nephrology Specialist
We specialize in the diagnosis and treatment of kidney diseases.
Our Services:
✅Chronic Kidney Disease
✅Dialysis
✅Renal Transplant
✅Glomerulonephritis
✅Hypertension Management
✅Other Conditions We Treat
Contact us:
SAN DIMAS OFFICE: (909) 542-2777
PASADENA OFFICE: (626)-357-9805
COVINA OFFICE: (626) 332-2777
UPLAND OFFICE: (909) 542-2779
Visit us: https://californiakidneyspecialists.com/
#californiakidneyspecialists #california #nephrologistsandimas #nephrologistpasadena #nephrologistcovina #nephrologistuplandca #kidneytransplantation #diabetic #diabetics #kidneypain #kidneydisease #kidneystones #kidneyinfection #kidneyhealth #kidneytransplantation #postkidneytransplant #dialysis #nephrologist #nephrology #nephrologynursepractitioner #nephrologistnearme #nephrologistdoctor #kidneytransplantationcenter
#nearby nephrologist#nephrology near me#kidney doctors near me#kidney specialists near me#nephrologist dr near me#glomerulonephritis treatment in California#glomerular disease treatment in California#diabetic nephropathy treatment in California#dialysis center in California#southern kidney specialists#nephrology IN SAN DIMAS#nephrology IN PASADENA#nephrology IN COVINA#nephrology IN UPLAND
0 notes
Text
#Abdominal Aortic Aneurysm#Aortic Aneurysms#Arteriosclerosis#Blood Clot Symptoms#Brain Aneurysm Symptoms#Carotid Artery#Carotid Artery Disease#Carotid Stenting#Diabetic Ulcers#Endovascular Surgery#Femoral Aneurysms#Femoral Artery#Hemodialysis#Hypotension#Ischemic Heart Disease#Ischemic Nephropathy#Lymphedema#Mesenteric Ischemia#Occlusive Disease#Peripheral Arterial Disease#Peripheral Vascular Disease#Renal Artery Disease#Renal Stents#Vascular Dementia#Vascular Surgery#Vein Ablations#Venous Insufficiency#Venous Reconstructive Surgery#Venous Stasis
0 notes
Text
Breakfast Choices for Individuals with Diabetic Kidney Disease
Managing daily life and dietary choices can be challenging for those dealing with diabetic kidney disease, a common chronic condition. Breakfast, often hailed as the most important meal of the day, holds particular significance for individuals living with both diabetes and kidney disease. This article explores dietary strategies for the breakfast of individuals with diabetic kidney disease, aiming to assist them in better managing their condition and enhancing their overall quality of life. Whether you are personally managing diabetes or a concerned family member, the information provided here can be valuable to you.
1.Egg Custard with Mixed Vegetables
Seafood Egg Custard (60g egg, 10g dried shrimp, 2g sesame oil)
Colorful Vegetable Mix (150g, including purple kale, bell peppers, and leafy greens)
Whole Wheat Bread (2 slices, 50g)
1 cup of milk (250ml)
This meal offers a diverse array of vegetables and high-quality protein from seafood and eggs, providing a well-rounded nutritional profile.

2.Broccoli with Chicken
Broccoli Salad (150g broccoli, a pinch of salt, a drizzle of sesame oil)
Chicken Breast Slices (50g chicken breast, 2ml light soy sauce, a touch of sesame oil)
1 cup of soy milk (300ml)
Half a Red Date and Sweet Potato Steamed Bun (30g small bun, 1 red date, 20g sweet potato flour, made from a mixture of wheat and sweet potato flour, fermented and steamed)
This meal includes a variety of vegetables, lean protein from chicken, and whole grains. Adjust the portion of chicken and broccoli for those with smaller appetites.

3.Seaweed Rice Roll with Yogurt
Seaweed Rice Roll (150g cooked rice, 1 sheet of seaweed, half a carrot, a little ham, 1 egg, a moderate amount of sesame oil, a pinch of black sesame seeds, half a cucumber, and a lettuce leaf)
1 cup of unsweetened yogurt
The seaweed rice roll combines the main carbohydrate source with various vegetables. Paired with yogurt, it becomes a convenient and nutritious breakfast option, especially suitable for individuals with diabetes on the go.
4.Oatmeal Porridge
Oats are renowned for their stomach-nourishing and lung-moistening properties, helping prevent post-meal high blood sugar. Oatmeal porridge, often referred to as the “longevity porridge,” is favored by many centenarians. Adding millet to the oats creates a fragrant and soft porridge with calming and sleep-enhancing effects, along with stomach nourishment and lung moisturization. Oats are high in dietary fiber, providing a satisfying feeling of fullness without causing spikes in blood sugar levels, making it an excellent choice for preventing post-meal high blood sugar.

#Diabetic Kidney Disease#Finerenone#diabetic nephropathy#Diabetic#long-term diabetes#Kidney Disease#DKD#CKD#blood sugar#protein in the urine#kidney failure#eGFR#Blood Sugar Control#Obesity#Hypertension
0 notes