#immune response
Text
The Power of Immunotherapy: A Deep Dive into Cancer Treatment
Immunotherapy, a groundbreaking approach in cancer treatment, has been making waves in the medical world. 🌟 But what exactly is it, and how does it work? Let's delve into the intricacies of this cutting-edge therapy. 💉
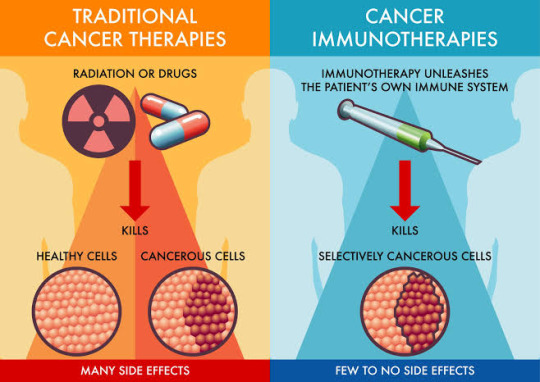
Immunotherapy at a Glance: 🔬 Immunotherapy, or immuno-oncology, is a therapeutic strategy that harnesses the body's immune system to combat cancer cells. Unlike traditional treatments like chemotherapy, which target both healthy and cancerous cells, immunotherapy is highly targeted, making it a game-changer in the fight against cancer.
Key Players in Immunotherapy: 🦠
Tumor Antigens are molecules found on cancer cells that act as red flags, signaling the immune system to attack. 👥
T Cells: The immune system's soldiers. They are trained to recognize and destroy threats, including cancer cells.
💡 Checkpoint Inhibitors: Proteins that, when blocked, enhance the immune response against cancer. 🧬
CAR-T Cell Therapy: Genetic engineering to supercharge T cells for precision attacks on tumors.
How Does Immunotherapy Work? Immunotherapy comes in various forms, but they all aim to accomplish one goal: boost the immune system's ability to recognize and eradicate cancer cells. Whether through checkpoint inhibitors, vaccines, or CAR-T cell therapy, the goal remains: empower the immune system's fighters!
Immunotherapy is a testament to the power of science and innovation, offering new hope to cancer patients worldwide. 🌍
Let's continue to explore, research, and advance this remarkable field to improve the lives of those affected by cancer.
References:
Postow, M. A., Callahan, M. K., & Wolchok, J. D. (2015). Immune Checkpoint Blockade in Cancer Therapy. Journal of Clinical Oncology, 33(17), 1974–1982. doi:10.1200/jco.2014.59.4358
Rosenberg, S. A., Yang, J. C., & Restifo, N. P. (2004). Cancer immunotherapy: moving beyond current vaccines. Nature Medicine, 10(9), 909–915. doi:10.1038/nm1100
June, C. H., & Sadelain, M. (2018). Chimeric Antigen Receptor Therapy. New England Journal of Medicine, 379(1), 64–73. doi:10.1056/nejmra1706164
#immunotherapy#science#biology#college#education#school#student#medicine#doctors#health#healthcare#immune system#cancer#disease#immune health#immune response
58 notes
·
View notes
Text
T for Tolerant
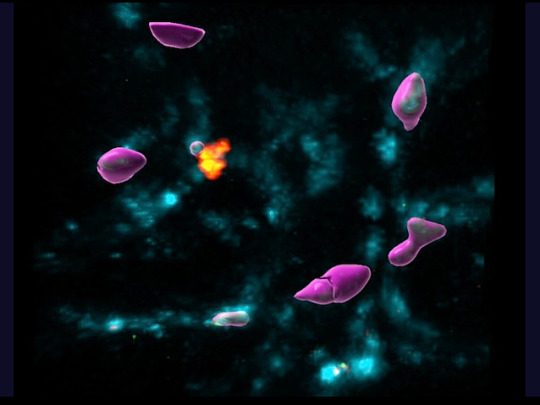
Single cell analyses and live-imaging in mouse gut reveals mechanisms underlying tolerance of the immune system's regulatory T cells to chronic bacterial infection and the intestinal niches where this takes place. Greater understanding of the disruption of tolerance which results in colitis
Read the published research article here
Still from video from work by Yisu Gu and Raquel Bartolomé-Casado, and colleagues
Kennedy Institute of Rheumatology, NDORMS, University of Oxford, Oxford and Wellcome Sanger Institute, Wellcome Genome Campus, Hinxton, Cambridge, UK
Video originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Nature, April 2024
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#biology#immunity#immune response#colitis#inflammation#gut bacteria#microbiome
11 notes
·
View notes
Text
Remember that time when Saitama got stung by mosquito?
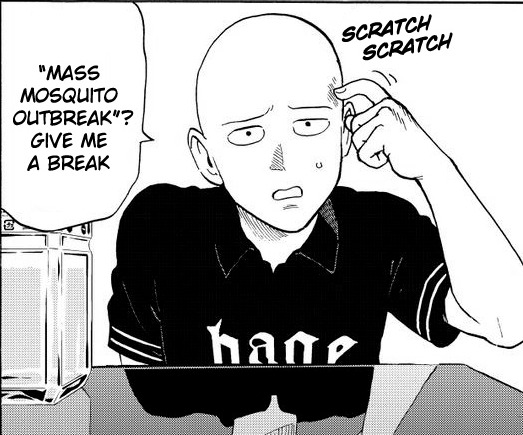
Something so beneath him to notice, on a conscious level. We might notice if some bug lands on us, but not a mosquito sting before its too late and they've already drawn blood.
Notably, Saitama did not notice the sting and it created the immune response to the bite. Remember, Saitama still has human body underneath all that supposed impenetrability.
Ergo, it penetrated his automatic defences and he didn't even notice it.
Keep this in mind, if we're gonna thread the needle at some point in the future.
22 notes
·
View notes
Text

I'm just wondering...
...where the Water is in Earth, Wind & Fire?
...why ancient Greece kept its wisdom to itself?
...where the b-sides can be found on playlists?
...how the immune response to right-wing extremism can be better stimulated?
...why the functioning of a door is apparently so difficult to understand?
...why there is a difference between "just wanting to" and "just doing it"?
...why we seem to be more interested in foreign planets than our own?
...why my teenager has to smell like teen spirit?
...why 2024 can't be boringly normal?
...why it has to be my fault?
#thoughts#my thoughts#aperçu#funny#just wondering#earth wind and fire#ancient greece#wisdom#b side#playlist#immune response#right wing#difficult to understand#difference#just do it#wanting to do something#foreign planet#planet earth#teenagers#teen spirit#2024#being normal#my fault#just asking
2 notes
·
View notes
Text
X
December 16th 2022
#mass disabling event#mass disabling#covid#pandemic#covid pandemic#immunology#immune response#crutches and spice#immunity debt
8 notes
·
View notes
Text
The knowledge that I wasn't lucid enough to proofread so much as a sentence of my own fic these past few weeks...
...has neutralised any guilt I might have had over not trying to WFH during that time.
#me#acute illness#(now *there's* a tag i don't usually use :P)#immune response#...it's pretty hardcore
3 notes
·
View notes
Text
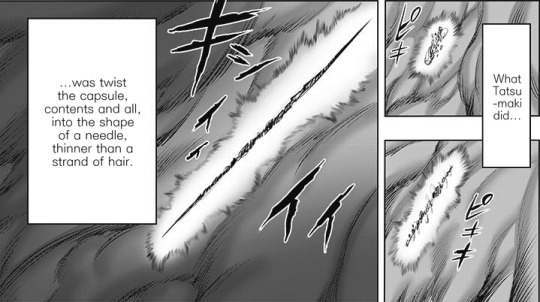
Prostanoids enemies forever: we'll keep on fighting (IL-)2 exhaustion 'TIL cancer cells will die
Tumors actively prevent the formation of immune responses by so-called cytotoxic T cells, which are essential in combating cancer. In cancer, tumors often impair the body’s immune response. For example, they can prevent immune cells from perceiving cancer cells as a threat or render them inactive. Immunotherapies aim to overcome these mechanisms and stimulate the immune system, in particular the…

View On WordPress
#cancer cells#cell receptors#checkpoint therapy#immune receptor#immune response#interleukin-2#lymphocytes#prostaglandin E2
0 notes
Text
Absolute Eosinophil Count: A Key Marker in Allergic Diseases and Beyond
Eosinophils are a type of white blood cell involved in the immune response against parasites, allergens, and infections. Absolute Eosinophil Count (AEC) is a measure of the number of eosinophils present in a microliter of blood. AEC is an important parameter used in diagnosing and monitoring various medical conditions.
Normal Range of AEC:
The normal range of Absolute Eosinophil Count (AEC) may vary slightly depending on the laboratory and the method of analysis used. However, in general, the normal range for AEC is between 30 to 350 eosinophils per microliter of blood.
Clinical Significance:
Elevated AEC levels, known as eosinophilia, can indicate several underlying health conditions, including allergies, parasitic infections, autoimmune diseases, and certain types of cancers. Conversely, low AEC levels may be observed in conditions such as aplastic anemia, drug toxicity, or overwhelming infections.
Causes of Elevated AEC:
1. Allergic Disorders:
Allergic conditions such as asthma, allergic rhinitis, atopic dermatitis, and allergic reactions to medications can cause eosinophilia.
2. Parasitic Infections:
Helminth infections, such as roundworms, tapeworms, and flukes, are common causes of eosinophilia.
3. Autoimmune Diseases:
Conditions like eosinophilic granulomatosis with polyangiitis (formerly known as Churg-Strauss syndrome) and systemic lupus erythematosus can lead to elevated AEC levels.
4.Hypereosinophilic Syndrome (HES):
HES is a rare disorder characterized by persistent eosinophilia and organ damage. It requires careful evaluation and management by a healthcare professional.
Diagnostic Evaluation:
When eosinophilia is detected, further diagnostic tests are often conducted to identify the underlying cause. This may include:
- Comprehensive medical history and physical examination
- Laboratory tests such as complete blood count (CBC), serum immunoglobulin levels, and specific IgE testing
- Imaging studies like chest X-rays, CT scans, or ultrasound to assess organ involvement
- Biopsy of affected tissues, if necessary
Treatment and Management:
The treatment of eosinophilia depends on the underlying cause. In cases of allergic conditions, antihistamines, corticosteroids, and allergen avoidance measures may be recommended. Parasitic infections are treated with anthelmintic medications. In more severe cases, immunosuppressive therapy or targeted biologic agents may be prescribed to modulate the immune response.
Conclusion:
Absolute Eosinophil Count is a valuable marker used in the diagnosis and management of various medical conditions. Understanding the significance of AEC levels and their association with underlying diseases, healthcare professionals are providing timely and appropriate interventions for patients.
It is important to note that AEC results should always be interpreted in conjunction with clinical findings and other laboratory tests to make an accurate diagnosis and formulate an effective treatment plan. Patients with persistently elevated AEC levels should seek medical attention for further evaluation and management.
0 notes
Text
MIT scientists use a new type of nanoparticle to make vaccines more powerful
New Post has been published on https://thedigitalinsider.com/mit-scientists-use-a-new-type-of-nanoparticle-to-make-vaccines-more-powerful/
MIT scientists use a new type of nanoparticle to make vaccines more powerful


Many vaccines, including vaccines for hepatitis B and whooping cough, consist of fragments of viral or bacterial proteins. These vaccines often include other molecules called adjuvants, which help to boost the immune system’s response to the protein.
Most of these adjuvants consist of aluminum salts or other molecules that provoke a nonspecific immune response. A team of MIT researchers has now shown that a type of nanoparticle called a metal organic framework (MOF) can also provoke a strong immune response, by activating the innate immune system — the body’s first line of defense against any pathogen — through cell proteins called toll-like receptors.
In a study of mice, the researchers showed that this MOF could successfully encapsulate and deliver part of the SARS-CoV-2 spike protein, while also acting as an adjuvant once the MOF is broken down inside cells.
While more work would be needed to adapt these particles for use as vaccines, the study demonstrates that this type of structure can be useful for generating a strong immune response, the researchers say.
“Understanding how the drug delivery vehicle can enhance an adjuvant immune response is something that could be very helpful in designing new vaccines,” says Ana Jaklenec, a principal investigator at MIT’s Koch Institute for Integrative Cancer Research and one of the senior authors of the new study.
Robert Langer, an MIT Institute Professor and member of the Koch Institute, and Dan Barouch, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center and a professor at Harvard Medical School, are also senior authors of the paper, which appears today in Science Advances. The paper’s lead author is former MIT postdoc and Ibn Khaldun Fellow Shahad Alsaiari.
Immune activation
In this study, the researchers focused on a MOF called ZIF-8, which consists of a lattice of tetrahedral units made up of a zinc ion attached to four molecules of imidazole, an organic compound. Previous work has shown that ZIF-8 can significantly boost immune responses, but it wasn’t known exactly how this particle activates the immune system.
To try to figure that out, the MIT team created an experimental vaccine consisting of the SARS-CoV-2 receptor-binding protein (RBD) embedded within ZIF-8 particles. These particles are between 100 and 200 nanometers in diameter, a size that allows them to get into the body’s lymph nodes directly or through immune cells such as macrophages.
Once the particles enter the cells, the MOFs are broken down, releasing the viral proteins. The researchers found that the imidazole components then activate toll-like receptors (TLRs), which help to stimulate the innate immune response.
“This process is analogous to establishing a covert operative team at the molecular level to transport essential elements of the Covid-19 virus to the body’s immune system, where they can activate specific immune responses to boost vaccine efficacy,” Alsaiari says.
RNA sequencing of cells from the lymph nodes showed that mice vaccinated with ZIF-8 particles carrying the viral protein strongly activated a TLR pathway known as TLR-7, which led to greater production of cytokines and other molecules involved in inflammation.
Mice vaccinated with these particles generated a much stronger response to the viral protein than mice that received the protein on its own.
“Not only are we delivering the protein in a more controlled way through a nanoparticle, but the compositional structure of this particle is also acting as an adjuvant,” Jaklenec says. “We were able to achieve very specific responses to the Covid protein, and with a dose-sparing effect compared to using the protein by itself to vaccinate.”
Vaccine access
While this study and others have demonstrated ZIF-8’s immunogenic ability, more work needs to be done to evaluate the particles’ safety and potential to be scaled up for large-scale manufacturing. If ZIF-8 is not developed as a vaccine carrier, the findings from the study should help to guide researchers in developing similar nanoparticles that could be used to deliver subunit vaccines, Jaklenec says.
“Most subunit vaccines usually have two separate components: an antigen and an adjuvant,” Jaklenec says. “Designing new vaccines that utilize nanoparticles with specific chemical moieties which not only aid in antigen delivery but can also activate particular immune pathways have the potential to enhance vaccine potency.”
One advantage to developing a subunit vaccine for Covid-19 is that such vaccines are usually easier and cheaper to manufacture than mRNA vaccines, which could make it easier to distribute them around the world, the researchers say.
“Subunit vaccines have been around for a long time, and they tend to be cheaper to produce, so that opens up more access to vaccines, especially in times of pandemic,” Jaklenec says.
The research was funded by Ibn Khaldun Fellowships for Saudi Arabian Women and in part by the Koch Institute Support (core) Grant from the U.S. National Cancer Institute.
#aluminum#antigen#Beth Israel Deaconess Medical Center#Cancer#cell#Cells#chemical#Chemical engineering#covid#covid 19#cytokines#defense#drug#drug delivery#experimental#framework#hepatitis#how#immune cells#immune response#immune system#inflammation#Israel#it#Koch Institute#LED#macrophages#Manufacturing#medical#metal
0 notes
Text
youtube
#immune system#immune#innate immune system#adaptive immune system#immune system for kids#immune system overview#specific immune system#boost your immune system#system#boost immune system#t cells immune system#immune response#woman's immune system#med surg immune system#immune system busters#healthy immune system#immune cells#the human immune system#acquired immune system#immune system function.#immune system animation#stress and immune system#the miraculous power of fruit and vegetables#diet based on fruit and vegetables#nails#hair#skin#teeth#Youtube
0 notes
Text
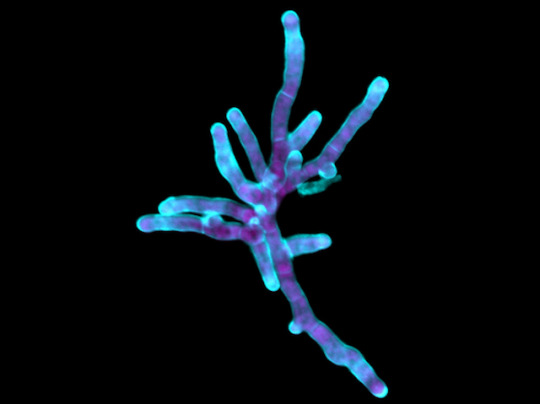
Phantom Threads
Aspergillus fumigatus is a common fungus found in the soil. While it's usually harmless, it can infect people with weakened immune systems, killing over half of its victims. This infection depends on hyphae – branching threads of fungal cells used to collect nutrients and spread through the body. A healthy immune system attacks these structures to stop the fungus in its tracks, as do some antifungal drugs. But the molecular details of hyphae growth during A. fumigatus infections are still unclear. Here we see A. fumigatus growing as hyphae. These cells were genetically modified to produce more of a protein called ZfpA and have more branches and stronger cell walls (blue) versus normal cells. Researchers discovered that ZfpA increases the growth of hyphae during A. fumigatus infections, thereby protecting the fungus from our immune systems and antifungal drugs. Learning more about how this protein works could help scientists develop more effective treatments for A. fumigatus.
Written by Henry Stennett
Image from work by Taylor J. Schoen and colleagues
Department of Medical Microbiology and Immunology, University of Wisconsin-Madison, Madison, WI, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in PLOS Pathogens, May 2023
You can also follow BPoD on Instagram, Twitter and Facebook
7 notes
·
View notes
Text
I forgot to post this about Oscar here the other day….
Oscar had an adventure today. He had his annual checkup at the vet. He was SO loud in the car, both ways. He made it known that he wasn’t happy. Lol. But he was so well behaved and got the all clear. He got his boosters and is good for another year. The vets were so sweet, making sure he has adjusted since losing his sister, and giving me hugs and condolences. Anyway, he’s happy to be back home. Lol.

I got my flu and Covid vaccines yesterday and boy am I feeling it. My arm is killing me and my fatigue is worse than usual. Yay immune response! /only partially sarcastic.
I’m all ready for Christmas and so excited. I wrapped all my gifts last night and helped mom wrap hers and dad’s this morning. Getting gifts is great, yeah, but I love giving presents. It brings me such joy to see someone open their present from me and be happy or excited about it.
#personal#cats#sweetboyoscar#vet visit#checkups#vaccines#flu shot#flu vaccine#covid vaccine#covid boosters#immune response#chronic fatigue#chronic fatigue syndrome#christmas#family#giving gifts
1 note
·
View note
Text
Exploring the Gut-Brain Connection: New Insights into Mental Health
Introduction:
Depression and anxiety are not only common but also complex mental health challenges, affecting millions globally. Cutting-edge research is now shining a light on an unexpected influencer of mental health: our gut microbiota, often dubbed the “second brain.” In this comprehensive guide, we’ll explore the intricate ties between gut health and mental health conditions such as…
View On WordPress
#anxiety#depression#diet#Gut health#gut-brain axis#immune response#inflammation#lifestyle modifications.#Mental Health#neurotransmitters#nutrition#prebiotics#probiotics#stress response
1 note
·
View note
Text
Dear science side of tumblr,
All things being equal, do disease symptoms appear earlier in individuals with stronger or weaker immune systems? I figure a stronger immune system might detect food poisoning or infection quicker and mount a faster, stronger response. On the other hand, a weaker immune system might be overwhelmed more quickly at lower pathogen load, which could also lead to earlier symptoms. I guess part of the question also involves separating host immune response vs symptoms directly caused by pathogens. Presumably, depending on the relative strength of host immune response vs pathogen symptoms, we can guess whether someone’s immune system is stronger than another’s?
#disease#symptom#immune system#immune response#pathogen#science side of tumblr#<- attempt at summon my target audience#I have attempted to find answers by Googling#and have been unsuccessful
1 note
·
View note
Text
December 16th 2022
X
#immunity debt#covid#pandemic#covid pandemic#immune response#immunology#immunocompromised#umnia_#commentary
2 notes
·
View notes
Link
1 note
·
View note