#journals publishing Medicine case reports
Text
Medicine Journal of Case Reports: Imaging in Medicine is a peer-reviewed journal established for ensuring the rights and benefits of Medicine specialists. Medicine Journal of Case Reports: Imaging in Medicine is devoted to the promotion of health sciences and related disciplines.
Manuscript Submission
Authors may submit their manuscripts through the journal's online submission portal: https://www.literaturepublishers.org/submit.html
(or) Send an e-mail attachment to the Editorial Office E-mail Id: [email protected]
#case reports in Medicine#case reports journal in Medicine#journal of Medicine case reports#journals publishing Medicine case reports#journals accepting Medicine case reports#where to submit or publish Medicine case reports#imaging journal in Medicine
0 notes
Text
Case Reports in Medicine Journal

Journal Publishes Case Reports in Medicine encourages publication of Case Reports in Medicine for physicians and medical aspirants to share different results in the form of clinical image articles and Case Reports in Medicine, which have been encountered in different medical sub-specialties or cases which leads to a higher understanding of the medical conditions, medicines, diagnosis and management.
Journal Homepage: https://www.literaturepublishers.org/
Case Reports in Medicine is a peer-reviewed, Open Access journal that publishes case reports and case series in all areas of clinical medicine. Case Reports in Medicine Journal is a continually updated, evidence based review journal covering internal medicine and its subspecialties. Case Reports in Medicine Journal is an authoritative and comprehensive resource that provides all clinicians, irrespective of specialty, with ready access to up-to-date information on mechanisms of disease, diagnosis and management so that patient care may be optimized.
Case Reports in Medicine Journal covers internal medicine and its sub-specialties, in addition to clinical topics such as poisoning, nutrition, ethics, communication skills, and clinical pharmacology. Irrespective of your medical specialty, Case Reports in Medicine Journal provides you with access to trusted information on mechanisms of disease, diagnosis and management options. With the core information provided in this singular resource, you can focus on being a confident and competent physician. Case Reports in Medicine Journal is a continually updated, evidence-based learning resource for trainees.
Manuscript Submission
Authors may submit their manuscripts through the journal's online submission portal: https://www.literaturepublishers.org/submit.html
(or) Send an e-mail attachment to the Editorial Office E-mail Id: [email protected]
0 notes
Text
Case Reports in Medicine Journal

Case Reports in Medicine Journal encourages publication of Case Reports in Medicine for physicians and medical aspirants to share different results in the form of clinical image articles and Case Reports in Medicine, which have been encountered in different medical sub-specialties or cases which leads to a higher understanding of the medical conditions, medicines, diagnosis and management.
Journal Homepage: https://www.literaturepublishers.org/
Case Reports in Medicine is a peer-reviewed, Open Access journal that publishes case reports and case series in all areas of clinical medicine. Case Reports in Medicine Journal is a continually updated, evidence based review journal covering internal medicine and its subspecialties. Case Reports in Medicine Journal is an authoritative and comprehensive resource that provides all clinicians, irrespective of specialty, with ready access to up-to-date information on mechanisms of disease, diagnosis and management so that patient care may be optimized.
Case Reports in Medicine Journal covers internal medicine and its sub-specialties, in addition to clinical topics such as poisoning, nutrition, ethics, communication skills, and clinical pharmacology. Irrespective of your medical specialty, Case Reports in Medicine Journal provides you with access to trusted information on mechanisms of disease, diagnosis and management options. With the core information provided in this singular resource, you can focus on being a confident and competent physician. Case Reports in Medicine Journal is a continually updated, evidence-based learning resource for trainees.
Manuscript Submission
Authors may submit their manuscripts through the journal's online submission portal: https://www.literaturepublishers.org/submit.html
(or) Send an e-mail attachment to the Editorial Office E-mail Id: [email protected]
0 notes
Text
Physicians are using excuses to intentionally dissuade people with disabilities from their practices, researchers say in a new study exposing just how pervasive discrimination against this population is in health care.
In focus groups, doctors described making strategic choices to turn away individuals with disabilities. They reported telling patients with disabilities that they would require specialized care and that “I am not the doctor for you.” In other cases, physicians said they simply indicate that “I am not taking new patients” or “I do not take your insurance.”
The findings come from a study published this month in the journal Health Affairs. It is based on focus groups conducted in late 2018 by researchers at the Northwestern University Feinberg School of Medicine, the University of Massachusetts and Harvard Medical School with 22 primary care and specialist doctors who were selected from a national database.
Many of the participants described accommodating people with disabilities as burdensome and some used outdated language like “mentally retarded.” Doctors frequently indicated that individuals with disabilities account for a small number of patients, making it hard to justify having accessible equipment. They also had little knowledge of their obligations under the Americans with Disabilities Act, with one suggesting that the law works “against physicians.”
The latest study builds on findings published earlier this year from a survey of 714 doctors that was done by some of the same researchers. Just 56% of physicians who participated in the survey said they welcome people with disabilities at their practices and only 41% indicated that they could provide such patients with a similar quality of care to others. Meanwhile, more than a third of doctors queried said they had little or no knowledge of their legal obligations under the ADA.
“Taken together, the focus groups and survey responses provide a substantive and deeply concerning picture of physicians’ attitudes and behaviors relating to care for people with disabilities,” the study authors note.
The findings suggest that bias continues to greatly influence health care more than 30 years after passage of the ADA, which prohibits discrimination against people with disabilities, including in medical services.
Tara Lagu, a professor of hospital medicine and medical social sciences at Northwestern University and an author of the study, described the doctors’ attitudes toward the ADA in particular as “upsetting and disappointing.”
“Our body of work suggests that physician bias and discriminatory attitudes may contribute to the health disparities that people with disabilities experience,” Lagu said. “We need to address the attitudes and behavior that perpetuate the unequal access experienced by our most vulnerable patients.”
8K notes
·
View notes
Text

By: Leor Sapir and Colin Wright
Published: Jun 9, 2023
A federal court on Tuesday temporarily blocked enforcement of a Florida law that prohibits the administration of sex-change procedures on children under 18. The opinion, by Judge Robert L. Hinkle, leans heavily on medical and scientific rationales to argue that it is unconstitutional to ban the use of puberty blockers, cross-sex hormones and surgery on teenagers who feel alienated from their bodies.
Twenty states maintain age restrictions on sex-change procedures, and the problem they face is explaining to judges that American medical associations aren’t following the best available evidence. This is known to European health authorities and has been reported in such prestigious publications as the British Medical Journal. But American judges need some way to evaluate conflicting scientific authorities—especially as institutions responsible for ensuring that medical professionals have access to high-quality research aren’t functioning as they should.
A case in point: Springer, an academic publishing giant, has decided to retract an article that appeared last month in the Archives of Sexual Behavior. The retraction is expected to take effect June 12.
The article’s authors are listed as Michael Bailey and Suzanna Diaz. Mr. Bailey is a well-respected scientist, with dozens of publications to his name. The other author writes under a pseudonym to protect the privacy of her daughter, who suffers from gender dysphoria.
Their new paper is based on survey responses from more than 1,600 parents who reported that their children, who were previously comfortable in their bodies, suddenly declared a transgender identity after extensive exposure to social media and peer influence. Mr. Bailey’s and Ms. Diaz’s sin was to analyze rapid onset gender dysphoria, or ROGD. Gender activists hate any suggestion that transgender identities are anything but innate and immutable. Even mentioning the possibility that trans identity is socially influenced or a phase threatens their claims that children can know early in life they have a permanent transgender identity and therefore that they should have broad access to permanent body-modifying and sterilizing procedures.
Within days of publication, a group of activists wrote a public letter condemning the article and calling for the termination of the journal’s editor. Among the letter’s signatories is Marci Bowers, a prominent genital surgeon and president of the World Professional Association for Transgender Health, an advocacy organization that promotes sex changes for minors.
Nearly 2,000 researchers and academics signed a counter letter in support of the article. Springer nonetheless decided to retract the paper without disciplining its editor. Springer initially asserted that the study needed approval from an institutional review board. But it quickly abandoned that rationale, which was false.
The publisher now maintains that the retraction is due to improper participant consent. While the respondents consented to the publication of the survey’s results, Springer insists they didn’t specifically agree to publication in a scholarly or peer-reviewed journal. That’s a strange and retrospective requirement, especially considering that Springer and other major publishers have published thousands of survey papers without this type of consent.
Anyone familiar with the controversy over transgender medicine knows what is going on. Activists put pressure on Springer to retract an article with conclusions they didn’t like, and Springer caved in. We’ve become accustomed to seeing these capitulations in academia, media and the corporate world, but it is especially disturbing to see in a respected medical journal.
Rather than appreciate the long-term risk to itself and the scientific community from doing the bidding of activists, Springer has instead agreed to evaluate and retract all survey papers that lack the newly required consent. If Springer follows through on its promise, hundreds of authors who chose to publish in Springer’s journals may have their research retracted.
The publications that support what they call “gender-affirming care” rely heavily on surveys. The U.S. Transgender Survey of 2015, for instance, has generated several influential papers. As it happens, the USTS didn’t inform participants that their answers would be published in peer-reviewed journals.
This kind of double standard runs through gender-medicine research. Papers advocating “gender transition” are readily accepted by leading scientific journals despite having grave methodological flaws and biases. Work that questions gender-transition orthodoxy stands almost no chance of being published in the best-known journals. Every now and then, an errant research paper slips past the censors, but should it prove significant enough to threaten the settled science narrative, retribution is swift and merciless. The researcher Lisa Littman learned this lesson in 2018, when she was widely attacked after publishing on the topic. Mr. Bailey and Ms. Diaz are learning it now.
The idea is to manufacture the appearance of scientific consensus where there is none. The pseudo-consensus then allows such American medical associations as the American Academy of Pediatrics and the Endocrine Society to recommend body-altering procedures for children.
While many Americans have heard news about the wave of states passing legislation that curbs sex changes for the young, few realize that an equally fierce, and arguably far more important, battle is raging: the battle for the integrity of the scientific process. It is a fight for the ability to have censorship-free scientific debate as a means to advance human knowledge.
==
Here's the thing: even if it's wrong, you refute it by making a better scientific case, with better evidence. You show where the flaws are. You don't throw a hissy-fit and cry until it goes away.
#Leor Sapir#Colin Wright#medical corruption#academic corruption#ROGD#rapid onset gender dysphoria#social contagion#gender ideology#genderwang#queer theory#religion is a mental illness
151 notes
·
View notes
Text
Grace Hills at Kansas Reflector:
TOPEKA — Attorney General Kris Kobach filed a civil lawsuit Monday against pharmaceutical company Pfizer, alleging that “Pfizer misled the public that it had a ‘safe and effective’ COVID-19 vaccine,” violating the state’s Consumer Protection Act.
The state seeks “civil monetary penalties, damages, and injunctive relief from misleading and deceptive statements made in marketing its COVID-19 vaccine,” Kobach said.
In the complaint, Kobach alleges that Pfizer willfully concealed, suppressed and omitted material facts relating to the COVID-19 vaccine, the “most egregious” ones regarding safety of the vaccine for pregnant people, in regard to heart conditions, its effectiveness against variants and its ability to stop transmission.
“Pfizer marketed its vaccine as safe for pregnant women,” Kobach said. “However, in February of 2021 (they) possessed reports of 458 pregnant women who received Pfizer’s COVID-19 vaccine during pregnancy. More than half of the pregnant women reported an adverse event, and more than 10% reported a miscarriage.”
The percentage of “adverse events” — which is a term that means any negative reaction — was higher in pregnant women than the general population by roughly 17 percent, according to a study published in the journal Medicine in February 2022.
An earlier study published in the New England Journal of Medicine in April 2021 offered preliminary findings that did not show any significant safety concerns among pregnant individuals who received the mRNA COVID-19 vaccine, indicating that observed miscarriages were not unusual and likely not a direct result of the vaccine.
Kobach says that Pfizer marketed the vaccine as safe in terms of heart conditions such as myocarditis and pericarditis. He referenced a question Albert Bourla, Pfizer CEO was asked in January 2023 of if the vaccine caused severe myocarditis, to which Bourla responded “we have not seen a single signal, although we have distributed billions of doses.”
“However, as Pfizer knew, the United States Government, the United States Military foreign governments and others have found that Pfizer’s COVID-19 vaccine caused myocarditis and pericarditis,” Kobach said.
According to the CDC, cases of myocarditis and pericarditis caused by the COVID-19 vaccine are rare, and most patients experienced resolution of symptoms by hospital discharge.
Kobach says Pfizer marketed its vaccine as effective against COVID-19 variants, “even though data available at the time showed Pfizer’s vaccine was effective less than half the time.”
His final allegation in the complaint was that the company falsely marketed the vaccine as preventing transmission.
Kansas AG Kris Kobach (R) files politically-motivated lawsuit against Pfizer and their COVID vaccine to score brownie points with anti-vaxxer extremists.
#Kris Kobach#Pfizer#Coronavirus Vaccines#Vaccines#Anti Vaxxer Extremism#Kansas#Myocarditis#Pericarditis
13 notes
·
View notes
Text
Yesterday CNN published an article by senior writer Tara John about the UK National Health Service’s newly skeptical stance toward youth gender medicine. The main takeaway, which is big news to observers of this debate, is that the NHS will no longer provide puberty blockers to young people, other than in research contexts. (As for cross-sex hormones, a relatively strict-seeming regime is set to be implemented, and they will be offered to youth only “from around their 16th birthday.”)
As myself and a number of others pointed out, the article contains a sentence that is, in context, rather wild: John writes that “Gender-affirming care is medically necessary, evidence-based care that uses a multidisciplinary approach to help a person transition from their assigned gender — the one the person was designated at birth — to their affirmed gender — the gender by which one wants to be known.” But of course, whether youth gender medicine is medically necessary and evidence-based is exactly the thing being debated, and anyone who has been following this debate closely knows that every national health system that has examined this question closely, including the NHS, has come to the same conclusion: the evidence is paltry. That’s why so many countries, including Sweden, Finland, the UK, and Norway have significantly scaled back access to these treatments for youth. So it’s very strange to see this sentence, which reads as though it comes from an activist press release, published in a news article in CNN, an outlet that generally adheres to the old-school divide between news and opinion.
There’s a strong case to be made that CNN’s sentence, as written, is false. Gender medicine is at best unproven, when it comes to the standards society (and regulatory bodies) expects medical researchers to adhere to. The situation with youth gender medicine is particularly dicey, given that this is a newer area of medicine suffering from an even severer paucity of quality studies.
It would be bad enough for this sentence to have appeared in one article on one of the most important news websites in the world. But here’s the thing: this wasn’t the first time. Rather, this exact sentence, and close variants of it, has been copied and pasted into dozens of CNN.com stories over the last few years, as a Google search quickly reveals.
This sentence, and its close variants, appear over and over and over. I asked my researcher to create a list of all the instances he could find. Here’s what he sent back, in reverse chronological order [...]
I haven’t triple-checked every single one of these, but it’s undeniable that effectively the same words have appeared in about three dozen CNN articles since May of 2022, which was already years after the present wave of European nations rethinking these treatments had begun.
When I asked CNN about this, I heard back from someone there who explained on background that it’s standard for outlets to provide reporters with guidance about accurate and appropriate language. While that’s true, it doesn’t really answer my question. Sure, it’s not unusual for an outlet to have a house style, sometimes enshrined in a stylebook, that provides rules about how to refer to, for example, individuals in the United States who lack legal status. They used to be called “illegal immigrants,” and now they’re often called “undocumented immigrants,” or language to that effect. This is a fairly normal process by which language changes and, sometimes as a result of a push-pull between outlets and advocacy groups, outlets decide which changes to make and when. So you may or may not agree with the fact that many outlets have switched from “biological sex” to “sex assigned at birth” when discussing trans issues, but the underlying process of switching from one phrase to another is standard and occurs in many areas.
This is quite different. You do not generally see the same complex sentence pasted over and over and over into news stories written by different authors and published in different sections. I asked CNN if it could provide me any other examples of CNN.com publishing the same sentence in multiple stories by different authors, and posed the same question in an email to Virginia Moseley, the CNN executive editor who, according to the website, “oversee[s] international and domestic news operations across platforms.” I didn’t hear back about this.
This copy-paste job is journalistically problematic for a number of reasons. For one thing, it suggests that CNN has decided, at the editorial level, that its institutional stance is that youth gender medicine is “medically necessary” and “evidence-based.” While they’re being used somewhat colloquially in these articles, these terms have fairly specific definitions in certain medical and legal contexts, and treatments only qualify for such designations if they have exceeded a certain evidentiary benchmark based on solid published research. That is not the case here — far from it, actually. As written, this is a deeply misleading sentence.
The language also puts CNN writers in an awkward position. Does each and every bylined author of these stories believe that youth gender medicine is “medically necessary” and “evidence-based”? Maybe they do (which would be disturbing), but the fact is that they didn’t write these sentences — they, or one of their editors, grabbed that language from somewhere else and pasted it in. They are effectively outsourcing their own judgment on a hotly contested controversy to their employer. This is not what journalists are supposed to do, and, at the risk of repeating myself, it’s significantly different from a reporter rolling their eyes when using language like “undocumented immigrant” or “sex assigned at birth,” rather than their own preferred verbiage. Those are rather small-stakes linguistic quibbles, different not only in degree but in kind from the question of whether or not youth gender medicine is medically necessary and evidence-based. And it goes without saying that a CNN reporter who does develop doubts about youth gender medicine is likely to be deterred from investigating further by the fact that their bosses have already decided that this is the way they’re going to cover this subject — say the line, Bart. Why bother?
It’s a pattern, unfortunately. Many outlets dug themselves into a deep hole on this issue by simply acting as stenographers and megaphones for activist groups rather than doing their jobs. And now that there is ever-mounting evidence undercutting the loudest activist claims, climbing out of this hole is going to be awkward. But there’s no other option, really. Because right now there’s absolutely no reason to take CNN.com seriously on this issue — the site has proven, demonstrably, that it doesn’t take itself seriously on this issue.
21 notes
·
View notes
Text
Paris 2024 Was Supposed to Be ‘Normal’—But You Can’t Compete With COVID - Published Aug 2, 2024
Some athletes are taking their own precautions, but the responsibility shouldn’t be solely on them
In the lead-up to the Paris Games, we couldn’t escape how “normal” it was all supposed to be: Media outlets touted the return of cheering spectators in place of empty stadiums, a hyped opening ceremony packed with hundreds of thousands of fans, arrivals of friends and families to help athletes celebrate huge wins (and process tough losses)—and no masks in sight.
All in all, as the Associated Press wrote at the beginning of July, the Paris Games would mark the return to “post-pandemic” “normal,” following “a stretch when host cities turned into closed-off shells of themselves, depriving those who had earned their way inside the so-called Olympic ‘bubble’ of a true Olympic experience.”
But as we’re learning as the 2024 Summer Games go on, popping that bubble might have been more than a little premature—and the athletes could be the ones paying the price.
To be clear, the lack of spectators, family support, and ability to connect with others wasn’t easy for the athletes. As fencer Kat Holmes told SELF, the atmosphere was “very restrictive.” “In Rio, it was like, ‘We’re here together, we’re gonna get to know each other,’” she said. “In Tokyo, it was like, ‘Oh my God, don’t breathe on me.’” So we totally get the desire to avoid that—it’s just that, unfortunately, COVID hasn’t gotten the memo.
The strict rules of Tokyo and Beijing didn’t exactly make it to Paris.
In Tokyo, the rules for the athletes were strict, so much so that the term “intimacy ban” kept getting thrown around. The reason for the “safety first” policies, according to a 70-page playbook released one month before the 2020 Games (which actually happened in 2021), was to protect all athletes, participants, and the people of Japan from the spread of COVID-19. As such, it detailed policies including mask wearing “at all times” (except for sleeping, eating or drinking, training, or competing); avoiding the “3 C’s” (spaces that are confined, crowded, or involve close contact); testing regularly for COVID-19, whether you were symptomatic or not; and isolating yourself if you do test positive, among others.
Strict, yes, but also effective. According to the annual report released by the IOC in 2021, there were only 33 cases of COVID-19 out of 11,300 athletes—and no confirmed spread of the virus between Games participants and the local population. As a result, those learnings went on to influence the policies for the Winter Games in Beijing in 2022, which maintained many of those strict rules too.
Fast forward two years later. We’re now several variants away from the virus that was circulating during the Tokyo and Beijing Games, and while fewer people are dying from the current strain, it’s definitely not “just a cold.” It’s still dangerous, linked to heart problems and lung damage, and the threat of long COVID is real too. Folks with underlying conditions are particularly at risk, and while you may not realize it, that includes a lot of athletes—yep, even those at the top of their game. According to a 2023 review in the Scandinavian Journal of Medicine & Science in Sports, about 15 to 30% of Olympians have asthma, and, recently, athletes like Suni Lee and Katie Ledecky have shared their own experiences living with chronic illnesses. And anyone, even seemingly healthy adults, can get seriously ill from it, whether that’s from the infection itself or the long COVID that can come after it.
Problem is, pandemic fatigue is real, and folks are understandably ready to get back to that elusive “normal.” But you can’t just wish away COVID—something other sporting events have been forced to acknowledge. In July, the Tour de France got rocked by COVID, with several top cyclists getting sick and withdrawing from competition. The Tour even reinstated mask mandates, requiring race organizers, media, and guests to wear them around contact with riders and team staff, Bicycling reported.
While the Games started just a couple weeks later (and in the same country!), the guidelines didn’t follow suit: According to Reuters, there’s no strict policy for COVID-19 at the Paris Games. “We have a protocol (that) any athlete that has tested positive has to wear a mask and we remind everyone to follow best practices, but in terms of monitoring COVID, cases are quite low in France,” Anne Descamps, Paris 2024 chief communications director, told Reuters.
When SELF asked Paris Games organizers on July 15 whether the Tour’s reinstatement of COVID prevention measures and mask mandates would influence theirs, a spokesperson simply said: “Paris 2024 is following the evolution of public health issues closely, together with the French Ministry of Health and Santé Publique France (Public Health France).” On July 19, Julie Dussliere, chief of Paralympics for the US Olympic and Paralympic Committee (USOPC) told SELF that while Team USA was encouraging a lot of “proactive behaviors for people to stay healthy,” like wearing masks on the plane “if they’re comfortable doing so” and “consistently using hand sanitizer,” there are “no specific COVID protocols in place from Paris 2024 for either the Olympics or the Paralympics.”
“Our team USA campaign for the games actually is called Don’t Let A Cold Keep You from the Gold,” Dussliere said. “And so we’ve provided a little travel packet to all members of our delegation athletes and coaches with things like hand sanitizer and masks, eye masks, earplugs for sleeping on the plane, things of that nature, to help with their travel and to try to keep them healthy while they’re traveling.”
So unlike the Tokyo Games, where visual reminders of COVID-19 were everywhere—from the empty stands to the masks athletes wore on podiums—Paris kicked off looking a lot more like a pre-2020 Games. Dig a little deeper, though, and it’s a different story.
To read the rest of the article, follow either link!
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#public health#wear a respirator
16 notes
·
View notes
Text
Medicine Journal of Case Reports: Imaging in Medicine

Medicine Journal of Case Reports: Imaging in Medicine accepting journal of Medicine, case reports in Medicine, case reports journal in Medicine, journal of Medicine case reports, journals publishing Medicine case reports, journals accepting Medicine case reports, where to submit or publish Medicine case reports, imaging journal in Medicine etc. Medicine Journal of Case Reports: Imaging in Medicine is a continually updated, evidence based review journal covering internal medicine and its subspecialties. Medicine Journal of Case Reports: Imaging in Medicine is an authoritative and comprehensive resource that provides all clinicians, irrespective of specialty, with ready access to up-to-date information on mechanisms of disease, diagnosis and management so that patient care may be optimized.
Journal Homepage: https://www.literaturepublishers.org/
Medicine Journal of Case Reports: Imaging in Medicine is a peer-reviewed journal established for ensuring the rights and benefits of Medicine specialists. Medicine Journal of Case Reports: Imaging in Medicine is devoted to the promotion of health sciences and related disciplines.
Manuscript Submission
Authors may submit their manuscripts through the journal's online submission portal: https://www.literaturepublishers.org/submit.html
(or) Send an e-mail attachment to the Editorial Office E-mail Id: [email protected]
#journal of Medicine#case reports in Medicine#case reports journal in Medicine#journal of Medicine case reports#journals publishing Medicine case reports#journals accepting Medicine case reports#where to submit or publish Medicine case reports#imaging journal in Medicine#clinical medicine#clinical images
0 notes
Text
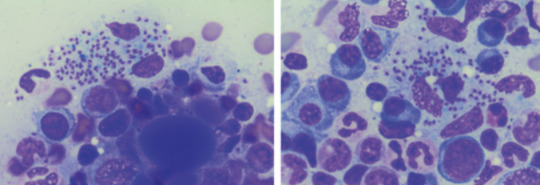
Leishmaniasis
Case Reports, like we're on a episode of house
23M in Kenya, presenting with months of LOW, persistent fevers, and abdo fullness, found to have massive splenomegaly.
examination: massive splenomegaly (10 cm below costophrenic margin, and will definitely cross midline) and hepatomegaly
pancytopaenic on bloods, plt's down to 40s
diagnosis confirmed on BMAT (parasite seen)
normal HIV, liver and kidney function
Bodies seen on the BMAT below are part of the lifecycle of the parasite that is intracellular, hence you can see the macrophages/neutrophils loaded with them, even bursting
What is it:
think of it when you get a patient with pancytopaenia and hepatosplenomegaly, who either traveled to or is in/from a tropical/subtropic region (where sand flies are)
cause - protozoa parasite Leishmania, transmitted by infected sandflies
Epidemio (when to consider it)
tropics, subtropics (South America, Asia, AFrica), Southern Europe
Microbiology/Transmission
parasite, replicates intracellularly (Leishmania donovani)
transmitted in sand flies (can be unnoticeable and usually bite in dawn or dusk - evenings or night), can also be transmitted via needles/blood
more common in rural areas
I've simplified this, but is more extensively covered in StatPearls and Wiki (there's different species of Leish and sandflies that transmit it)
once bitten, the protozoa are phagocystosed by skin macrophages, which then becomes full of the "bodies" (part of the lifecycle). Eventually these burst to release more of the bodies that infect more macrophages
they eventually are spread via blood to liver/spleen/BM and LNs
Random history:
ancient, records of disease date back to Egyptian mummies from 3000 BC --> positive DNA amplication for Leishmania and on papyrus from 1500 BC
multiple physicians from different times have described the disease, but it's named for 2 who described the parasite's intracellular ovoid body stage in smears from infected patients in India: Lt General William Boog Leishman and Captain Charles Donovan (Ronald Ross named the bodies after the 2 --> "Leishman Donovan bodies"
significant disease in Allied troops in Sicily in WWII, called "jericho buttons" (image on wiki from a WWI trooper serving in the middle east)

Leishman: Scottish pathologist and British Army medical officer, later it's director general in the 20s, did extensive research into the parasite named for him by Sir Ronald Ross. He mistook the parasite he observed for trypanosomes (cause of Chagas in South America and African sleeping sickness in Africa)
Donovan: Irish parasitologist, medical officer in India, observed an epidemic across India just after the rebellion of 1857, discovered the "bodies" in spleen tissue as the causative agent for what the locals called "kala azar" (severe visceral leishmaniasis - see below)
Donovan also discovered the "bodies" of Klebsiella granulomatis, hence these too are named after him (cause of ulcerative granulomas)
It became scandalous as both wanted credit for the "discovery" of this newly identified organism. So Sir Ronald Ross named it for both of them.
Sir Ron, by the way, won a Nobel in Medicine for discovering that malaria is transmitted via mossies (this was also a source of scandal, he was meant to share it with another physician who he accused of fraud - and they never received the award)
finally, it was actually a Russian physician who identified it first, but well, he published in a little known Russian journal which was promptly forgotten.
Clinical features
cutaneous type vs visceral organ type (spleen, liver, bones)
From wiki

can be asymptomatic
cutnaeous: can be there for years and resemble leprosy, causes an open chronic wound (most common), incubation 2-4 weeks on average (nodules at site of inoculation that eventually form ulcers), can heal spontaneously in 2-5 yrs
in diffuse cutaneous cases, can affect face, ears, extensor surfaces
can be muscosal = eg nasal symptoms/epistaxis, severe: perforated septum, this occurs in 1/3 after resolution of cutaenous symptoms (can be severe/lifte threatning, as it can affect vocal cords and cartilage, but oddly not bone)
visceral (incubation periods of up to years until immuncompromise): fever, weight loss, hepatosplenomegaly (spleen more than liver), pancytoaepnia, high total protein and low albumin with hypergammaglobulinaemia
this has seasonal peaks related to sandfly habits and humidity
interestingly it is an infective cause of massive splenomegaly, such that it crosses the midline
Extreme - but noticeable hepatosplenomgealy/abdo fullness, from medscape

can be atypical in HIV co infected patients, LAD in seom regions like Africa
Kala azar = black fever in some severe cases (fatal due to secondary mycobacterial infection or bleeding), refers to damage fto spleen, liver and anaemia
invstigations:
serology not great (minimal humoral response to the parasite), so often requires histopath (tissue sample) for which BMAT is safest in visceral organ involvement
visualisation of amastigotes (or Leishman-Donovan bodies), as intracellular --> can be seen in macrophages (small round bodies) post Giemsa staining
PCR of DNA also possible (as done in the Egyptian mummies)
Image source:

Treatment
liposomal amphotericin B (holy shit strong stuff) in visceral, PO: miltefosine (caution in pregnancy), all have significant ADRs, or paromycin. however, mortality of 10% if visceral left untreated
mixed results with azoles
in HIV co infection - start the HAARTs! can improve survival, mortality is 30% in HIV patients
cutaneous: stibolgluconate (have never heard of these drugs) and megluaine antimoniate, but limited disease often spotnaeously gets cleared by the innate system
prevention:
use DEET insect repellant at dawn and dusk
loose fitting clothing that covers all skin
no vaccine (were attempts at vaccinating dogs, which decreased rates)
sandflies are smaller than mossies, so requires small netting

Differentials for hepatosplenomegaly

Sources:
WHO guidelines
CDC guidlelines
Wiki - Haven't covered pathophysio, but wiki does extensively
StatPearls
DermNet - great resource for all things derm, that my derm colleagues pointed out to me
9 notes
·
View notes
Text
Book Release: The Reliability of UFO Witness Testimony (With a Chapter by Cláudio Tsuyoshi Suenaga)
V.J. Ballester-Olmos & Richard W. Heiden (Eds.)
For 76 years, casual observers around the world have reported sightings of aerial phenomena unexplainable to them. More elaborate personal experiences have been reported by others whose testimony speak of close interactions with fantastic flying machines that land, from which strange beings descend, and even kidnap the onlookers. In the absence of compelling physical evidence of the reality of these narrations, how should science study immaterial observations and test these claims? The very standard of reputable witness reliability is at stake here.
The Reliability of UFO Witness Testimony is the first major book to comprehensively focus on the discussion and current views on problems and challenges posed by the reliability of UFO testimonies. This is a cross-disciplinary compendium of papers by 60 authors from 14 different countries. They are specialists in social, physical, and biological sciences, including psychology (predominantly) as well as psychiatry, sociology, anthropology, history, philosophy, folklore, religion, journalism, engineering, computing, medicine, education, analysts with experience in the critical study of UFO perceivers, and other professionals. This volume shares thematically convergent ideas about the plausibility of alternate explanations for an alleged close-range UFO phenomenon.
The 57 chapters in this book are divided into seven section headings: Case Studies, Psychological Perspectives, On Witness Testimony, Empirical Research, Anthropological Approach, Metrics and Scaling, and Epistemological Issues. There, the subject matter is analyzed from statistical work to clinical assessment, psychometrics, comparative and evaluation inquiry, and other topic perspectives.
Some extracts from the Foreword, written by Dr. Leonard S. Newman, Professor of Psychology at Syracuse University:
"The contributors to this book include some very smart people. There are all sorts of issues to which they could be devoting their intellectual energy, and all sorts of scholarly and research contributions they could make. They don’t have to write thoughtful and rigorous chapters for a book called The Reliability of UFO Witness Testimony, but this is what they have done. And so, the work continues, as attested to by the papers in this volume. I’m not sure if there exists any collection of papers on any topic that can claim to comprehensively summarize everything that is currently known about it. But this one comes pretty close."
This 711-page book has been released online in the Academia.edu portal, from where it can be downloaded for free:
Simultaneously, UPIAR Publishing House (Turin, Italy) has published two softcover, A4 format print editions, one in black & white, another in full color (ISBN: 9791281441002). The book can be purchased through this link:
Four outstanding academics have provided praise notes to this volume. This is what they said:
Elizabeth Loftus, Ph.D., Distinguished Professor of Psychology at the University of California, Irvine, USA:
"When ordinary citizens claim to have extraterrestrial encounters, such as seeing UFOs or meeting with alien beings, what should we think? Did the alien abduction really happen or was it a hoax? Is someone deliberately lying? Are they false memories? Readers will be enthralled by the fascinating case histories that are presented in The Reliability of UFO Witness Testimony*, a volume where sixty experts examine these issues with depth and insight. These cases teach us a great deal about how humans come to believe they have experienced bizarre events that may have never occurred at all."
Steven Jay Lynn, Ph.D., Distinguished Professor of Psychology, Binghamton University (SUNY), USA:
"This captivating book will appeal to anyone interested in UFOs (and who isn’t?), the vagaries of memory, eyewitness perception and misperception, critical analysis of puzzling phenomena, and evaluating scientific vs. pseudoscientific claims. This volume ranks in the elite category of essential reading for students, scientists, and the seriously curious among us, and therefore has my highest recommendation. Bravo!"
Henry Otgaar, Ph.D., Professor of Legal Psychology, Maastricht University, the Netherlands, and Leuven Catholic University, Belgium:
"Claims of UFO sightings and experiences continue to fascinate us. This book has collected a unique and diverse set of case studies and critical articles on how such experiences unfold and what the authenticity of these claims is. The collection of these different articles is truly groundbreaking and is the first-ever complete assemblage concerning the validity of UFO testimony."
Benjamin E. Zeller, Ph.D., Professor and Chair of Religion, Lake Forest College, Illinois, USA:
"In referring to extraterrestrial contact, Carl Sagan said that extraordinary claims require extraordinary evidence. This fine book seeks to contextualize what such evidence entails. Its contributors analyze UFO sightings and cases both famous and obscure, recent and historical, and quite international in scope. They draw from an impressive range of methodological, academic, and scientific perspectives, and consider such topics as the nature of cognition, memory, types of belief and testimony, psychology, and the rationality of belief. Skeptics, believers, and scholars of ufology will all find this book fascinating!"
For additional information please contact:
UPIAR Publisher: [email protected]
Editor: V.J. Ballester-Olmos, [email protected]




The Objectivity of Witnesses and the Subjectivity of Testemonies
Cláudio Tsuyoshi Suenaga
I had the honor of being one of the select few invited by the distinguished Vicente-Juan Ballester Olmos, one of the organizers and editors of this impressive scientific-academic book, together with the equally distinguished Richard W. Heiden, to write a paper on the "reliability of the testimony of witnesses of UFOs", a crucial aspect of ufological research, since, in the absence of material evidence of the phenomenon, this is the primary source we deal with, the "raw material", so to speak, to permeate our analyses, even more so for those who not only deals with "second-hand" reports, but gathers them directly from the witnesses themselves, in sometimes harsh and hostile field conditions.
In my contribution entitled "The Objectivity of Witnesses and the Subjectivity of Testimonies", I carried out a critical analysis of the general reference base of the UFO problem, the testimony, seen as a cultural source authentic and indisputable, but which presents serious distortions. One of the main points questioned by me was the exact value of the testimonies, which form the basis of the reports and, therefore, of the UFO phenomenon. I tried to give an adequate scientific treatment to these data and factors relegated to the background by ufologists: the subjective observational parameters, the perceptive aspects, the language and the historical-cultural context of the witness and the psychosociological variables, that is, everything that was disparagingly called "background noise", the "sociological reject" despised in detriment of the "signal".



Consult and keep close at hand, therefore, this, the first major book to comprehensively focus on the discussion and current views on problems and challenges posed by the reliability of UFO testimonies. A cross-disciplinary compendium of papers by 60 authors from 14 different countries.
(large format, 711 pages)
You can download the full 711-page book on my Patreon:
#ufologia#ufos#ufo phenomenon#ufo sightings#ovnis#extraterrestres#história#aliens and ufos#antropologia#sociology#historia#psicologia#religi��o#testemunho#livro#classic academia#books and libraries#science#skepticism#ceticismo#testimony#the witness#suenaga yoroshiku onegaishimasu
28 notes
·
View notes
Text
Do pain patients on long-term opioid therapy make irrational decisions? Is their mental capacity so diminished by opioids that they shouldn’t be involved in treatment decisions with their doctors?
The answer to both questions is often yes, according to a controversial new op/ed published in JAMA Internal Medicine. At issue is a recent update to the CDC’s opioid prescribing guideline, which calls for shared decision-making (SDM) when a prescriber considers tapering a patient or abruptly discontinuing their opioid treatment. The guideline was revised last year after reports of “serious harm” to patients caused by forced tapering.
“In situations where benefits and risks of continuing opioids are considered to be close, shared decision-making with patients is particularly important,” the 2022 guideline states.
But that advice about consulting with patients goes too far, according to the lead author of the JAMA op/ed, Mark Sullivan, MD, a professor of psychiatry at the University of Washington and a longtime board member of Physicians for Responsible Opioid Prescribing
“The value of SDM has been recognized for many years but also has its limitations, including where patients make irrational or short-sighted decisions,” Sullivan wrote. “Long-term opioid therapy induces a state of opioid dependence that compromises patients’ decisional capacity, specifically altering their perception of the value and necessity of the therapy; and although patients with chronic pain are not usually at imminent risk of death, they often can see no possibility of a satisfying life without a significant and immediate reduction in their pain.”
Sullivan and his two co-authors, Jeffrey Linder, MD, and Jason Doctor, PhD, have long been critical of opioid prescribing practices in the U.S. In their conflict of interest statements, Sullivan and Doctor disclose that they have worked for law firms involved in opioid litigation, a lucrative sideline for several PROP members...
...“In the case of opioid prescribing, and especially opioid tapering, working to persuade the patient is almost always the best clinical strategy. But there are circumstances (opioid use disorder, diversion, serious medical risks) where tapering should occur even if the patient objects,” Sullivan wrote.
Opioid diversion by patients is actually rare. The DEA estimates that less than one percent of oxycodone (0.3%) and hydrocodone (0.42%) will be used by someone they were not intended for.
As for patients on opioids behaving “irrational,” Sullivan and his co-authors cite an op/ed published 33 years ago in The New England Journal of Medicine (NEJM). But that article doesn’t even discuss opioids or tapering, it’s about whether patients and doctors should collaborate in making decisions about end-of-life medical care. It also makes an important disclaimer that “even the irrational choices of a competent patient must be respected if the patient cannot be persuaded to change them."
Sullivan rejects that approach to opioid treatment...
...In a rebuttal to Sullivan’s op/ed also published in JAMA Internal Medicine, Mitchell Katz, MD, and Deborah Grady, MD, disputed the notion that a patient’s choices shouldn’t be respected.
“Primary care professionals generally highly value the inclusion of the patient’s perspective in decision-making, consistent with the principles of patient autonomy and self-determination, and are loathe to go against a patient’s wishes,” they wrote.
“As primary care professionals, we have found it helpful to tell patients that it is not recommended to take more than a specific threshold of opioids and that we do not want to prescribe something that is not recommended. However, that does not mean sticking to rigid cut points for dose and duration of opioid use, abandoning patients, or having them undergo too rapid a taper.”
Others questioned JAMA’s decision to publish Sullivan’s op/ed.
“While I recognize the editors’ legitimate intellectual interest in providing a forum for open discussion on the opioid policy space, I question their decision to publish an editorial that represents an ongoing call for broad, ill-defined reductions in opioid prescribing,” said Chad Kollas, MD, a palliative care specialist who rejects the idea that patients shouldn’t be involved in their healthcare choices.
“Errantly embracing a lower evidentiary standard for medical decision-making capacity creates an unacceptable risk for harm to patients with pain by violating their rights of medical autonomy and self-determination.” (Full article at link)
So essentially a man with a bias against opioids and who makes money litigating against uses a 33 year old op ed to assert pain patients shouldn't have a say in their medical care because we irrational. Proof of that irrationality is that if we have to deal with severe chronic pain with no relief, we may contemplate suicide. So fucking irrational, right? 🤬
This man is fucking cruel and inhumane. He works for an organization (PROP) that has had direct influence on the 2016 CDC Opioid Guidelines which lead to many pain patients committing suicide or dying from complications due to forced tapering and withdrawals. And this man has been given a platform to assert that our desire to not exist in severe daily pain is irrational. Fuck him!
#disability#chronic pain#ableism#opioids#chronic illness#medical bias#suicide cw#forced tapering#spoonies#PROP#cdc guidelines#article
27 notes
·
View notes
Text
"Laumer explained that the plant and related liana species, found in tropical forests of Southeast Asia, are known for their pain-relieving, anti-inflammatory, and other properties important to wound healing.
The plants are used in traditional medicine to treat various diseases, such as malaria, dysentery and diabetes, said Laumer, first author of the study published in the journal Scientific Reports.
The researchers observed no signs of wound infection in the days following the injury. They also saw that the wound closed within five days and fully healed within one month."
#healing#health#animals#asia#self healing#self help#first aid#medical#medicine#animal#animalrights#econotego#ecology#science#ausgov#politas#auspol#tasgov#taspol#australia#fuck neoliberals#neoliberal capitalism#anthony albanese#albanese government#healthcare#health and wellness#healthylifestyle#mental health#environmental#environment
2 notes
·
View notes
Text

By: SEGM
Published: Jun 21, 2023
In a new peer-reviewed commentary published in the Journal of Sex & Marital Therapy, author, Dr. Sarah Jorgensen, argues that the medical community has a professional responsibility to recognize detransitioners as survivors of iatrogenic harm and provide them with the comprehensive medical and supportive care that they deserve.
Jorgensen notes that proponents of gender-affirming medical interventions have attempted to downplay regret and detransition as vanishingly rare based on outdated studies that are not applicable to cohorts of adolescent trans identifying females presenting to gender clinics today. They refuse to admit that the gender-affirming model is failing some patients and have instead tried to reframe detransition as neutral or even positive outcome, proposing euphemisms such as “gender journey,” “identity exploration,” or “dynamic desires for gender-affirming medical interventions,” to replace the term “detransition."
“Rather than acknowledging the severity of the problem or that the medical community bears responsibility for the harm done to these young people, the message is that there have been no mistakes - the situation is dynamic.”
Instead of asking what went wrong, what was missed, and what could have been done differently to prevent inappropriate medical transitions, proponents of gender-affirming care repeatedly make appeals to authority, “every major medical association in the United States supports gender-affirming care for minors,” seemingly oblivious to the move away from American-style affirmation-on-demand in many European countries:
“A growing number of health authorities in countries that were once proponents of youth medical transition are now changing practice and prioritizing psychotherapy and treatment of co-occurring developmental, psychosocial, and mental health problems after their own systematic reviews found the evidence supporting gender-affirming medical interventions to be weak and uncertain.”
Many detransitioners report that they find it challenging to access clinicians who can advise them on what to expect when discontinuing hormones or who have the knowledge and training to manage enduring adverse effects of hormonal therapies and surgical complications. Jorgensen notes that there is currently no guidance on best practices for clinicians involved in the care of detransitioners:
“The World Professional Association for Transgender Health (WPATH) recently published its eighth Standards of Care document and chose not to include a chapter on detransition (Coleman et al., 2022). Likewise, the Endocrine Society’s Clinical Practice Guidelines for Gender-Dysphoria/Gender-Incongruence offers no advice on how to safely stop hormonal therapies (Hembree et al., 2017). The American Academy of Pediatrics failed to acknowledge the possibility of regret and detransition in their policy statement on care for children and adolescents with gender dysphoria (Rafferty et al., 2018).”
Jorgensen highlights multiple areas of uncertainty that will require open discussion and a commitment to clinical collaboration and research to resolve.
“We do not know what is driving the sharp rise in the number of young people being diagnosed or self-diagnosing with gender dysphoria (Cass, 2022; Kaltiala-Heino, Bergman, Tyolajarvi, & Frisen, 2018; Zucker, 2019). Likewise, we do not know why the case mix has rapidly shifted from predominantly young boys and middle-aged men to primarily adolescent females with complex mental health problems and neurodiversity (Aitken et al., 2015; Kaltiala-Heino et al., 2015; Zucker, 2019). The natural trajectory of transgender identification in this novel cohort is uncertain and we cannot predict who will be helped by gender-affirming medical interventions or who will be harmed. The long-term safety and effectiveness of these interventions is yet unknown (Hembree et al., 2017; Ludvigsson et al., 2023; NICE, 2020a, 2020b).”
Importantly, Jorgensen emphasizes that “we miss out on urgently needed data that could improve the outcomes of future patients by ignoring detransitioners.”
SEGM's Thoughts
The rate of medical detransition in the Western countries currently stands at 10-30% and is expected to grow. A number of the detransitioned patients will have permanent unwanted changes to the bodies and adverse long-term impacts on their physical and psychological health.
There is an urgent need to recognize detransition as a new phenomenon, and to structure the healthcare system in order to support this vulnerable patient population. However, due to the novelty of the detransition phenomenon, no diagnostic or procedure codes currently exist that either accurately capture the detransitioned patients' condition, or ensure provider reimbursement for the medical and mental health services that patients will need.
For this reason, it is urgent that the medical community initiate a conversation about what types of diagnostic and procedure codes are necessary to ensure the provision of high quality care to the individuals who detransition.
#SEGM#Society for Evidence Based Gender Medicine#detrans#detransition#iatrogenic harm#sex trait modification#medical malpractice#medical scandal#medical transition#medical corruption#transition regret#gender ideology#ideological corruption#ideological capture#queer theory#genderwang#religion is a mental illness
48 notes
·
View notes
Note
Hi, I’m a big fan of your work. I think you are helping at lot of women by bringing attention to the things going on in society. I was wondering if you had any plans to talk about the results of the Cass review and the backlash Dr. Hilary Cass is receiving?
Wish you the best.
Hi! Thanks so much for the ask and for watching my videos! I'm actually working on a review of the Cass review right now. The problem is that it is very long, and I'm still trying to figure out how to cover it in a way that gives justice to the entire situation- from the social situation which spawned it, to actual contents of and the reception of it.
For example, here's an excerpt from my current script:
This obfustication of language comes alongside a radical decrease in literacy and critical thinking ability. As reported on Snopes.com, "Literacy rate" is defined by UNESCO Institute for Statistics as “the percentage of the population of a given age group that can read and write.” A 2019 study ranked the US as 125th for literacy, while data collected by the U.S. Department of Education published in 2020 found that 130 million adults in the country have low literacy skills. In other words, more than half (54%) of Americans between the ages of 16 and 74 read below the equivalent of a sixth-grade level. According to an empirical study by Xiaohua Hu and Hongwei Zhang, published in the Journal of Language Teaching and Research, it was found that “...improvements in critical thinking are paralleled by improvements in reading comprehension. They believe that the presence of such a strong relationship may be due to the fact that critical thinking and reading are both cognitive abilities which have some identifiable cognitive skills in common…” In other words, if one goes up, so does the other; and if one goes down….
It should come as no surprise then, that many gender idealogues are unable or unwilling to read the Cass Review, and to understand why it is critical of many of the arguments, studies and other writings of support of transitioning. In addition, many people prefer not to read a three hundred page report before making an opinion on it; they prefer instead to have someone else do the hard work, and to base their opinion off of theirs. While it is fair to trust a reviewer to help you decide an opinion on a movie you don’t plan to watch, or on a book you haven’t read, in cases like these, regarding a difficult topic such as the Cass Report, it would be best to read not just one perspective, or one report, but many, and if possible, to refrain from making judgments without reading the original source material. Claims of heterocissexism, transphobia and other forms of bigotry become obviously unfounded when even those who staunchly agree with you are admitting to the validity of the report you so disavow. Of course, one of the most common critiques is that the Cass report found that many studies in support of gender transitioning to be bad studies. In the weeks after the report, the NHS has made changes in policy to reflect this. Although these changes are slow and often small, it marks an important change in the handling of gender related services, as in the past few years scientific rigor has been replaced with emotion based guidelines, and a refusal to critically examine, or even cautiously proceed with experimental medicine.
I do hope to get this out soon, but I'm also hoping to cover some non-trans related topics first, including some retrospectives about war.
5 notes
·
View notes
Text
Radiation from nail dryers may damage DNA and cause cancer-causing mutations in human cells, a study has found — and that might have you wondering whether your regular gel mani-pedi is worth the risk.
Some dermatologists say the findings, in a study published in January in the journal Nature Communications, aren’t new when it comes to concerns about ultraviolet, or UV, light from any source. In fact, the results reaffirm the reason why some dermatologists have changed the way they get their gel manicures or have stopped getting them altogether.
“The findings contribute to data already published regarding the harmful effects of (ultraviolet) radiation and show direct cell death and damage to tissue that can lead to skin cancer,” said Dr. Julia Curtis, an assistant professor of dermatology at the University of Utah, who wasn’t involved in the study.
“Tanning beds are listed as carcinogenic and UV nail lamps are mini tanning beds for your nails in order to cure the gel nail,” Curtis said.
A form of electromagnetic radiation, ultraviolet light has a wavelength ranging from 10 to 400 nanometers, according to the UCAR Center for Science Education.
Ultraviolet A light (315 to 400 nanometers), found in sunlight, penetrates the skin more deeply and is commonly used in UV nail dryers, which have become popular over the past decade. Tanning beds use 280 to 400 nanometers, while the spectrum used in nail dryers is 340 to 395 nanometers, according to a news release for the study.
“If you look at the way these devices are presented, they are marketed as safe, with nothing to be concerned about,” said corresponding author Ludmil Alexandrov in the news release. “But to the best of our knowledge, no one has actually studied these devices and how they affect human cells at the molecular and cellular levels until now.” Alexandrov holds dual titles as associate professor of bioengineering and cellular and molecular medicine at the University of California, San Diego.
Researchers exposed cells from humans and mice to UV light, finding that a 20-minute session led to 20% to 30% of cells dying. Three consecutive 20-minute exposures made 65% to 70% of the exposed cells die. The remaining cells experienced mitochondrial and DNA damage, resulting in mutations with patterns that have been observed in skin cancer in humans.
The biggest limitation of the study is that exposing cell lines to UV light is different from conducting the study on living humans and animals, said dermatologist Dr. Julie Russak, founder of Russak Dermatology Clinic in New York City. Russak wasn’t involved in the study.
“When we’re doing it (irradiating) inside human hands, there’s definitely a difference,” Russak said. “Most of the UV irradiation is absorbed by the top layer of the skin. When you irradiate cells in the petri dish directly, that’s slightly different. You don’t have any protection from the skin, from corneocytes or the top layers. It’s also very direct UVA irradiation.”
But this study, taken with previous evidence — such as case reports of people developing squamous cell carcinomas, the second most common form of skin cancer, in association with UVA dryers — means we should “definitely think harder about just exposing our hands and our fingers to UVA light without any protection,” said Dr. Shari Lipner, an associate professor of clinical dermatology and director of the nail division at the NewYork-Presbyterian Hospital/Weill Cornell Medical Center. Lipner wasn’t involved in the study.
If you’re concerned about gel manicures but don’t want to give them up, there are some precautions you can take to mitigate the risks.
“Apply broad spectrum sunblock that contains zinc and titanium around the nails, and wear UV gloves with the fingertips cut off when it is time to cure your nails,” said Curtis, who doesn’t get gel manicures. “I would recommend alternatives to gel nails, such as the new wraps that are available online.” (Gel nail wraps or strips are stick-on gel nail products that don’t always require being set by UV nail dryers.)
Some salons use LED lights, which “are thought to emit either no UV light or much, much lower amounts,” Lipner said.
Lipner gets regular manicures — which typically last her seven to 10 days — not in an effort to avoid UV light but rather because she doesn’t like the nail-thinning acetone soaking involved with gel manicures.
“Regular manicures are just dried in the air,” she added. “Gel manicures have to be curated or sealed, and the polymers in the polish have to be activated, so that can only be done with the UVA lights.”
If you have regularly gotten gel manicures, Lipner recommends seeing a board-certified dermatologist who can examine your skin for any skin cancer precursors and treat them before they become serious problems. (Ultraviolet light can also age the skin, showing up as sunspots and wrinkles, she said.)
There isn’t enough data for experts to weigh in on how often people can get gel manicures without putting themselves at risk, Lipner said. But Curtis recommended saving them for special occasions.
Russak doesn’t get gel manicures very often but uses sunscreen and gloves when she does, she said. Applying serums rich in antioxidants, such as vitamin C, beforehand might also help, she added.
“As a dermatologist, I change gloves probably three, four times with just one patient. And with a regular nail polish, after three, four glove changes, the nail polish is gone,” Russak said. “The gel manicure definitely has a much better longevity, but is it really worth the risk of photoaging and development of skin cancer? Probably not.”
People with a history of skin cancers or who are more photosensitive due to fairer skin or albinism, medications or immunosuppression should be more careful about taking precautions, experts said. But whatever your risk, the dermatologists CNN spoke with urged caution.
“Unfortunately, full protection is not possible, so my best recommendation is to avoid these dryers altogether,” said Dr. Joshua Zeichner, an associate professor of dermatology at Mount Sinai Hospital in New York City.
#they went soft on this obv but uh. stop fucking doing this altogether should be the message#my sister and i are genetically elevated risk for skin cancer but she won’t fucking stop these nails#and she never ever goes to the derm or does self skin check and i’m so worried for her
8 notes
·
View notes