#Vasculitis
Text
#SARSCoV2 is a very weird virus 🦠
https://www.medscape.com/viewarticle/1000302
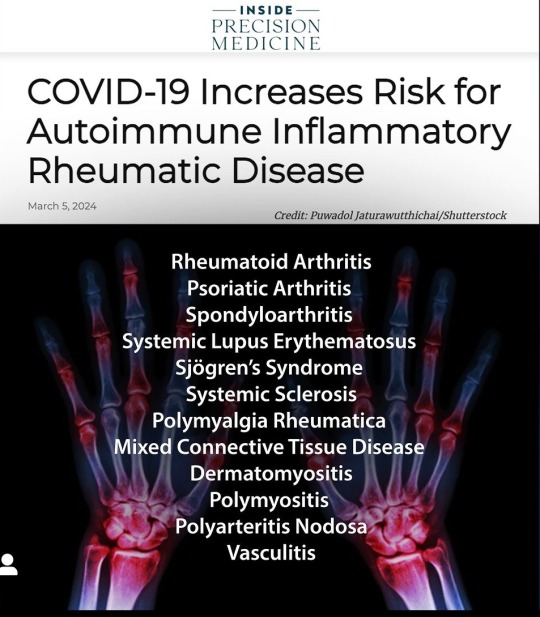
#COVID19 may lead to #AutoimmuneInflammatoryRheumaticDiseases (#AIRDs) like #RheumatoidArthritis, #lupus, and #vasculitis, study published in the Annals of Internal Medicine.
https://www.acpjournals.org/doi/10.7326/M23-1831
#sars cov 2#covid 19#autoimmune disease#autoimmune inflammatory rheumatic disease#AIRD#rheumatoid arthritis#lupus#vasculitis
14 notes
·
View notes
Text

ON THE WEBSITE I EVEN SUGGESTED IT AWWWW
7 notes
·
View notes
Text
I'm going off the chemo treatment now! It's finally time! 🥳
Well, it's more like switching one problem for another. But still.
17 notes
·
View notes
Text
As part of my extensive medical testing, this winter I had an ANCA panel. The only unusual result was elevated proteinase 3, which was 50 AU/mL, which is fairly high, as anything above 26 is considered positive for vasculitis.
The doctor said since the rest of the panel was negative he wasn’t worried, but that we could retest in about two months. Since we were casting such a wide net, he got distracted and forgot. I had it retested this week and my PR3 was high again — 37 AU/mL.
I think it would be pretty obvious if I had Wegener granulomatosis, so these results are kind of baffling to me.
The doctor asked if I’ve seen a rheumatologist yet — I have, but he only tested for lupus and RA and didn’t seem to know much about anything else so I’m not keen to see him again.
I’ve taken the opportunity to request a referral to the big hospital rheumatology department — I already asked for a referral there from my GP, but they wanted me to justify yet another referral and I don’t have the energy to argue my case, especially with my existing medical trauma.
I was prescribed fludrocortisone for my POTS-like symptoms over the winter and I did take it for a bit with some good results, but it significantly worsened my Raynaud’s syndrome and I didn’t like being on a steroid so I stopped taking it. I’m guessing I’m probably going to be put back on it, or a similar medication, in the near future. Not thrilled about that.
#moss-opossum#disability#chronically ill#chronic illness#disabled#physically disabled#chronic pain#chronic health issues#vasculitis
9 notes
·
View notes
Text
PIP assessor or little Britain character?
Got the report from my pip assessor.
Me: I really struggle to chop veg
Assessor: Yeah but you can drive a manual car so I think you can chop veg.
Me: I struggle to remember to do things, I miss appointments and leave the washing machine unemptied. Forget to eat, drink or pee sometimes.
Assessor: Yeah but you can drive a manual car and you are here at this appointment. So I think you can concentrate enough to do things.
Me: I struggle to communicate and sometimes I can't speak when I'm overwhelmed.
Assessor: Yeah but you are talking now and can drive a manual car. So you can communicate.
Me: I forget to take my meds and only remember when I start to get symptoms
Assessor: Yeah but you drive a manual car and have told me about your conditions so I think you can remember to take meds.
Me: I'm not doing that movement it hurts.
Assessor: Yeah but you drive a manual car and took your Jacket off when you got here. So I think you could do that if you wanted.
Me: I have bad joint pain and right sided weakness.
Assessor: Yeah but you drive a manual car.
I could go on.
I will be challenging the decision.
#mental health#actually autistic#plural system#living with cptsd#plurality#adhd#did system#functional neurological disorder#chronic fаtiguе ѕуndrоmе#autism#autoimmine disease#vasculitis#pip assessment#personal independence payment#dwp#ableism#fnd
16 notes
·
View notes
Text
Well, well, well if it isn't my spoon debt coming to collect
3 notes
·
View notes
Text
Disability does not. Fucking. Pay. Enough.
#disabled#disability#pots#vasculitis#behcet's disease#bipolar type 2#asd#autistic#autoimmune disease
15 notes
·
View notes
Text
2 notes
·
View notes
Link
From 2021.
Patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) present with a range of symptoms including post-exertional malaise (PEM), orthostatic intolerance, and autonomic dysfunction. Dysfunction of the blood vessel endothelium could be an underlying biological mechanism, resulting in inability to fine-tune regulation of blood flow according to the metabolic demands of tissues. The objectives of the present study were to investigate endothelial function in ME/CFS patients compared to healthy individuals, and assess possible changes in endothelial function after intervention with IV cyclophosphamide.
Symptoms frequently present following an event such as infection, physical trauma or exposure to environmental factors (4), and there is evidence of a genetic predisposition (8, 9). Research suggests the involvement of the immune system (10, 11), an impaired energy metabolism (12–14) and alterations in the gut microbiome (15). Orthostatic intolerance and autonomic dysfunction are also frequently reported, and can present with symptoms such as light-headedness, nausea, concentration difficulties, sweating, palpitations, dyspnea, and chest pain after prolonged sitting or standing.
It has been suggested that a dysfunction of the blood vessel endothelium could be a contributing mechanism, possibly associated with inadequate fine-tuned regulation of blood flow according to the metabolic demands of tissues (16, 17). One possible explanation for such endothelial dysfunction could be a reduced bioavailability of nitric oxide (NO) derived from endothelial cells. NO is a messenger molecule and neurotransmitter with important effects on vasodilation, thus contributing to the regulation of blood flow to tissues. NO is involved in many biologic processes, including effects on cognitive function, smooth muscle tone in the gastrointestinal and urogenital tracts, cardiac contractility, skeletal muscle and mitochondrial function (18, 19). Non-invasive measures for endothelial function include flow-mediated dilation (FMD) of the large arteries, which is believed to reflect the release of NO from endothelial cells caused by shear stress in vessel walls (20–22). As part of an FMD investigation, it is recommended to also measure endothelium-independent vasodilation, reflecting smooth muscle function, through the administration of sublingual nitroglycerin (20, 21). In the microcirculation, the measure post-occlusive reactive hyperemia (PORH) is understood to represent a more complex response involving nervous and myogenic responses as well as several vasodilators including NO (23).
There is growing evidence for endothelial dysfunction in autoimmune diseases (20, 24, 25) and fibromyalgia (26). However, research into blood vessel function in ME/CFS is limited so far. A study by Newton and colleagues (16) showed reduced FMD and PORH in a group of ME/CFS patients compared to healthy controls. This finding was confirmed by Scherbakov et al. who reported peripheral endothelial dysfunction in 18 of 35 (51%) ME/CFS patients compared to 4 of 20 (20%) healthy controls. This study also indicated a correlation between endothelial dysfunction and disease severity (17). In contrast, another study of 24 ME/CFS patients and 24 sedentary controls, using a different assessment method, found no significant difference in peripheral endothelial function at rest or after exercise (27).
This study investigated endothelial function in ME/CFS, and was the first to describe the changes in endothelial function before and after therapeutic intervention with IV cyclophosphamide in ME/CFS patients. Endothelial function measurements at baseline indicated that at the group level, the patients had significantly reduced large and small vessel endothelial function compared to healthy individuals, in line with results from previous studies (16, 17). Although more than half of the patients met the criteria for clinical response during the study, we were unable to detect any significant associations between clinical response and changes in endothelial function from baseline to 12 months follow-up.
Flow-mediated dilation (FMD) is the “gold-standard” method for large vessel endothelial function assessment (21), and the measurements have followed a well-established protocol.
One might speculate that endothelial dysfunction in ME/CFS could be associated with inadequate autoregulation of blood flow according to the demands of tissues, with resulting local hypoxia and lactate accumulation upon limited exertion. The clinical symptoms of ME/CFS suggest inadequate regulation of autonomic functions including blood flow. In a recent study of invasive cardiopulmonary exercise testing in upright position in ME/CFS patients, two types of peripheral neurovascular dysregulation were demonstrated; reduced cardiac output due to impaired venous return with low ventricular filling pressure (“preload failure”), and arterio-venous shunting with impaired peripheral oxygen extraction (53). These physiological changes are plausible contributors to several hallmark symptoms of ME/CFS, such as post-exertional malaise, and are associated with microcirculatory dysregulation, possibly related to small-fiber neuropathy (53).
Measures of known metabolites associated with endothelial function in cardiovascular diseases (Arg, hArg, ADMA, and SDMA) showed no significant differences between ME/CFS patients and healthy controls. This may argue for a different mechanism underlying the observed endothelial dysfunction in ME/CFS. We speculate that among ME/CFS patients, many of whom are relatively young women, the endothelial dysfunction could be related to an initial abnormal immune response, rather than atherosclerosis.
Further research is required in order to reach firm conclusions on any possible associations between ME/CFS symptoms and endothelial function. Future studies should aim to integrate objective activity measures as a supplement to validated patient-reported outcome measures, in order to control for the effect of physical activity or inactivity.
In conclusion, this study showed an association between ME/CFS and reduced endothelial function, both in large vessels assessed by FMD, and in small vessels by PORH. In this relatively small study, there were no significant associations between clinical response after cyclophosphamide and changes in FMD or PORH. Continued research efforts are warranted to further understand the possible circulatory disturbances involved in ME/CFS.
#ME/CFS#MECFS#chronic fatigue syndrome#cyclophosphamide#vasculitis#endothelial dysfunction#science journal#small fiber neuropathy
1 note
·
View note
Text
In general, the presence of vasculitis should be considered in patients who present with systemic or constitutional symptoms in combination with evidence of single and/or multiorgan dysfunction. The diagnosis of the individual vasculitides is generally based on patterns of organ injury, the size of the vessels affected, histopathological features, and characteristic findings on diagnostic imaging.
Diagnostic evaluation for a case of possible vasculitis should include a detailed history, including drug use, infectious disease exposure, and symptoms of manifestations that may characterize or exclude a suspected diagnoses; a careful physical examination to identify potential sites of involvement of vasculitis and determine the extent of vascular lesions; general laboratory testing to help identify the degree of organ involvement and exclude another disease; additional laboratory testing, depending on the suspected diagnosis and findings, such as tests for antinuclear antibodies (ANA), complement levels, ANCA; a chest radiograph or high-resolution computed tomography (HRCT) of the chest; electromyography; a lumbar puncture; a biopsy of the involved tissue if possible; and vascular imaging.
Patients with nonvasculitic disease processes may present with symptoms and findings that closely mimic various vasculitides. Perhaps most common are systemic rheumatic diseases, such as systemic lupus erythematosus, atherosclerotic disease, drug reactions, and vaso-occlusive processes. Among the most important diseases to exclude are infections and malignancies since immunosuppressive therapy could worsen these conditions and a delay in diagnosis can be extremely dangerous.
2 notes
·
View notes
Text
AI and big data enhance understanding of systemic vasculitis

- By Nuadox Crew -
Researchers from Trinity College Dublin’s School of Medicine and the ADAPT Centre have made a significant breakthrough in understanding autoimmune diseases, particularly systemic vasculitis.
By leveraging AI and big data techniques, the EU-funded FAIRVASC project connects vasculitis patient registries across Europe, enabling seamless data sharing and advanced analysis.
This approach addresses major challenges in diagnosing and treating these rare and severe diseases.
Read more at Trinity College Dublin
Scientific paper: Karl Gisslander et al, Data-driven subclassification of ANCA-associated vasculitis: model-based clustering of a federated international cohort, The Lancet Rheumatology (2024). DOI: 10.1016/S2665-9913(24)00187-5
Read Also
AI companies are merging or collaborating to even out the gap in access to vital datasets
1 note
·
View note
Text
AI-driven big data research improves insights into systemic vasculitis

- By InnoNurse Staff -
Researchers from Trinity College Dublin, in collaboration with Lund University, have made a significant breakthrough in vasculitis research, as published in The Lancet Rheumatology.
The study, part of the FAIRVASC project, utilizes advanced AI and big data to improve the diagnosis and treatment of systemic vasculitis, a group of rare autoimmune diseases.
By connecting patient registries across Europe, researchers accessed a much larger dataset, enabling them to identify new disease clusters and develop a novel classification method. This method enhances the prediction of outcomes and personalizes treatment strategies.
Read more at Trinity College Dublin
///
More recent news and insights
AI detects cancer and viral infections with nanoscale accuracy (Centre for Genomic Regulation)
Johns Hopkins, CareFirst, and Techstars introduce a healthcare AI accelerator (Healthcare Dive)
#ai#big data#vasculitis#medtech#health tech#cancer#oncology#nanotechnology#genomics#rare disease#autoimmune disease#startups#innovation
0 notes
Text
https://drgouravseth.livejournal.com/496.html
#DrGauravSeth#rheumatology#rheumatologist#immunology#immunologist#immuno#ImmunoCare#immunocare#vasculitis#vasculitisawareness#treatment#treatmentplan#treatmentoptions#bestrheumatologistindelhi#BestArthritisDoctorinDelhi#LupusTreatmentinDelhi
0 notes
Text
Doctors have agreed for me to have an ANA blood test. Now if I'm right and diagnosis has been delayed because of them gaslighting me...

#autoimmune#anti nuclear antibodies#ANA blood test#systemic lupus erythematosus#vasculitis#mental health#actually autistic#medical gaslighting
2 notes
·
View notes
