#birth control during perimenopause
Text
Perimenopause Panic: Ultimate Guide | Dr. Kelly Culwell | MomCave LIVE
Hold on to your hot flashes, folks! We’ve got the amazing Dr. Kelly Culwell in the MomCave, where the coffee is strong, and sanity is on a coffee break. Dr. Kelly, not just your typical doctor—she’s the OBGYN rockstar with a prescription for laughter and a cure for the chaos that is perimenopause. Buckle up for a rollercoaster of hormones, hilarious anecdotes, and maybe a few tips on how to…
View On WordPress
#birth control and menopause symptoms#birth control diaphragm#birth control during perimenopause#birth control junel#birth control perimenopause symptoms#birth control sprintec#birth control without hormones#perimenopause bloating#perimenopause dizziness#perimenopause fatigue#perimenopause joint pain#perimenopause missed period#perimenopause quiz#perimenopause symptoms#taking birth control during perimenopause
0 notes
Text
Health update
I am feeling fine. I did experience some skin inflammation which I am now convinced it is hormonal. I think it is caused by increased progesterone levels associated with the luteal phase.
I really think it's due to estrogen and progesterone activity, which starts during puberty and continues to cycle throughout a woman's reproductive years. This explains why I got my first flare during puberty when I was 12 (it was minor and I remember it being on my right pointer and ring fingers only. It lasted for a few months in 2008 and then disappeared, but I remembered I used to rub my fingers on the carpet a lot to relieve the itchiness). My skin inflammation is genetic and I'm 29 so not yet menopausal. But my mom said her eczema disappeared when she reached perimenopause. I've also noticed my skin inflammation gets worse during my luteal phase, with no changes to my diet, supplements, environment, weather, lifestyle, and skin care. I got bad rashes on my face and neck and ears (mostly on the left side) and my left hand broke out in oozy and inflamed skin (I could not close my hand in a fist as a result).
Below is a graph of how hormones change within the menstrual cycle. I experienced itchiness last Tuesday (Aug 20, which would have been day 17 for me). I experienced some itchiness during week 2, so from days 9 until 11).

Source: PALM Health St. Louis
In July I got a steroid shot on day 12 of my cycle, took steroid pills for 5 days after (so until day 17). The inflammation was gone at the time, but came back aggressively a few days later (day 20). It's hard to assess cycling inflammation when I take steroids because it suppresses it.
Below is a graph of how estrogen and progesterone levels cycle throughout a woman's life. As I said, my flares began at puberty (12 years old), stopped for the rest of my teens, and came back when I was 20 and is still ongoing. My mom stopped getting flares at perimenopause, when estrogen and progesterone levels decline. I'm convinced the cycling and general activity of estrogen/progesterone are playing a role here.

Source: Jennis
Both hormones start cycling a bit during puberty, and begin to cycle in a stable manner during the fertile years (even though the graph lines are straight, both hormones do cycle during that timeframe due to the menstrual cycle). However, I'm not quite sure what happens exactly between puberty and fertile years based on this graph. I have not gotten any flares as a baby/young child (birth-11), and none between the ages of 13-19.
Here's another similar graph, but it shows progesterone levels specifically:

Source: Hall and Klein, 2017
Below is a graph how steroidal hormones are made from cholesterol:

My skin inflammation got much worse with intermittent fasting. Some studies show that fasting in women decrease estrogen and progesterone levels.
So this is all a lot of information, but I do believe hormones are responsible for my skin inflammation. In what way? I don't know. Whenever I experience peaks in hormone levels, mainly progesterone, I experience inflammation. I'm not quite sure if peaking estrogen levels during ovulation are contributing in this case.
I'm going to ask my doctor about all this. I hope I can find a solution that isn't birth control. But I know I'll figure this out.
I'm so happy I'm healing this year!!
0 notes
Text
Having Unbalanced Periods, Talk to Gynecologist near Me

Hormonal anomalies, stress, structural problems, birth control or contraceptive methods, and medical issues can all contribute to irregular periods. Menstrual periods can be disrupted by thyroid problems, PCOS, and hormonal changes during perimenopause. Inadequate diet, stress management, and structural flaws can also lead to irregular periods. See a gynaecologist near me for individualized treatment options and discuss your underlying medical issues or drugs…
0 notes
Text
What is Abnormal Uterine Bleeding Disorder? Causes & Its Treatment
Abnormal uterine bleeding disorder is a condition where a woman experiences heavy or unusual bleeding from the uterus. The event can take place at any time during the month.
The following are a few scenarios where bleeding is considered abnormal:
When menstruation lasts more than 35 days or less than 21 days (normal menstruation lasts five to seven days and occurs every 21 to 35 days)
Bleeding lasts more than 7 days
No period for 3 to 6 months
Bleeding after menopause
It is one of the most common gynecologic problems among women. However, it is important to remember not everyone who experiences abnormal uterine bleeding reports their symptoms.
Now after gaining the basic understanding of the issue, it is also crucial to understand the causes behind the vaginal bleeding or spotting.
So, let’s start with the causes.
What Causes Abnormal Uterine Bleeding?
Hormonal imbalance is often the cause of abnormal uterine bleeding. In addition to this reason, there are several other reasons for the problem, which are as follows:
Fibroids or polyps (Lumps in the lining of the uterus)
Polycystic ovary syndrome ( A condition when cysts grow on the ovaries)
Miscarriage
Ovulatory dysfunction
Ectopic pregnancy
Blood clotting disorders
Use of contraceptives
Remember, this list is not exhaustive. The specific cause of AUB can vary depending on individual factors. This is why the importance of a gynecologist cannot be overstated. They can perform a comprehensive examination, analyze patients' medical history, and potentially recommend tests to pinpoint the exact cause of AUB.
Treatment of Abnormal Uterine Bleeding
Medication
The treatment of abnormal uterine bleeding depends on the cause and the patient's situation. However, drugs are usually the first thing your doctor will try.
For instance, if the cause behind the bleeding is hormonal imbalance, a gynecologist may suggest taking birth control pills. It is a common option for those not trying to conceive or in perimenopause.
But for women trying to conceive or avoid hormone side effects, the following medications are used instead of hormones:
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Tranexamic acid
Procedure
Intrauterine device (IUD): This is a common practice where a device is inserted inside the woman's uterus to prevent pregnancy. And there is one such type of it that releases hormones and is used to treat abnormal uterine bleeding.
Remember: Sometimes, IUDs can be the cause of abnormal bleeding. So, consult with your gynecologist if you experience something like this.
Dilation and curettage (D&C): This procedure involves stretching the cervix to allow the surgeon to place a surgical instrument inside the uterus and scrape away the lining. Its best part is that it stops heavy bleeding and helps identify and treat the bleeding's cause.
Endometrial ablation: If bleeding continues after a D and C, this procedure that destroys or removes the lining of the uterus through the use of a laser, heat, electricity, microwave energy, or freezing can often help control bleeding.
Remember: In some women, it causes scarring of the endometrium (Asherman syndrome); scarring can cause menstrual bleeding to stop (amenorrhea) and make biopsy of the endometrium difficult later.
If the problem persists, uterus removal is the next option.
After reading the above information, you might get an idea about the subject's complexity. That is why it is important for students preparing for university examinations to have an in-depth knowledge of each method and the best clinical practices.
However, sometimes, it can be tough for students to access the resources and understand the topics in detail.
But here’s the solution, enroll in an obgyn md course created by Dr. Aswath Kumar Raghu, the Chief Editor of OBGYN MD.
About the OBG course Offered by DigiNerve
If you aim to become an MD in obstetrics and gynecology, this course is best for you. During the course, students are encouraged to learn based on concepts and approaches that cater to their individual learning needs.
Over the course, you will access a variety of materials including online video lectures on OBGYN, lecture notes, MCQs for self-assessment, and more.
So, visit DigiNerve now and register for the OBGYN MD course.
#obg course#md obstetrics and gynaecology#md in obg#obgyn md#online video lectures on obgyn#obgyn md course#importance of gynecologist#gynecologic problems#hormonal imbalance#Ovulatory dysfunction#vaginal bleeding or spotting#Asherman syndrome#Infection or inflammation
0 notes
Text
Beyond The Calendar: Exploring The Reasons Behind Missed Periods

Menstruation is a natural and essential part of a woman’s reproductive health cycle. For many, it arrives predictably, like clockwork, every month. However, there are times when this cycle gets disrupted, and a missed period can be a cause for concern or confusion. While a missed period is often associated with pregnancy, numerous other factors can contribute to irregularities in menstrual cycles.
In this blog, let’s answer a common question “Why periods are missed?”
1. Stress and Lifestyle Factors:
Stress can cause havoc on the body, leading to irregular periods or even the complete absence of menstruation. High stress levels can disrupt the delicate hormonal balance necessary for menstruation. Factors such as work pressure, relationship issues, or major life changes can all contribute to increased stress levels. Additionally, extreme changes in lifestyle, such as sudden weight loss or intense exercise regimens, can also impact menstrual cycles.
2. Hormonal Imbalances:
Hormonal imbalances can indeed lead to irregularities in menstrual cycles, including late periods. The menstrual cycle is regulated by a delicate interplay of hormones, primarily estrogen and progesterone. Any disruption in this balance can result in delayed menstruation. Several factors can contribute to hormonal imbalances, including stress, changes in weight, excessive exercise, thyroid disorders, polycystic ovary syndrome (PCOS), and certain medications.
3. Medications:
Certain medications can interfere with the menstrual cycle. Birth control pills, for example, work by altering hormone levels in the body, which can sometimes lead to irregular bleeding or missed periods, especially when starting or stopping a new type of birth control. Other medications, such as antidepressants or antipsychotics, can also impact hormone levels and menstrual regularity.
4. Nutritional Deficiencies:
A balanced diet is important for overall health, including reproductive health. Nutritional deficiencies, particularly of iron, vitamin D, and B vitamins, can affect hormone production and regulation, leading to irregular periods or amenorrhea (the absence of menstruation). Eating disorders such as anorexia nervosa or bulimia can also disrupt menstrual cycles due to severe caloric restriction or purging behaviours.
5. Medical Conditions and Illnesses:
Certain medical conditions can directly affect the menstrual cycle. Chronic illnesses like diabetes or inflammatory bowel disease can disrupt hormone levels and lead to irregular periods. Similarly, conditions such as endometriosis or uterine fibroids can cause heavy or irregular bleeding, which may be mistaken for a missed period. Additionally, infections or illnesses that cause high fever can temporarily halt menstruation.
6. Perimenopause and Menopause:
As women approach menopause, typically in their late 40s to early 50s, menstrual cycles may become irregular or sporadic. This phase, known as perimenopause, marks the transition to menopause, the cessation of menstrual periods. Fluctuating hormone levels during perimenopause can cause missed periods, along with other symptoms like hot flashes and mood swings.
7. Weight Changes:
Significant weight changes, whether it’s rapid weight loss or substantial weight gain, can profoundly influence hormone levels and disrupt menstrual regularity. When the body undergoes significant changes in weight, it can alter the balance of hormones such as estrogen and progesterone, which are essential for regulating the menstrual cycle. Rapid weight loss, for instance, can lead to a decrease in estrogen levels, potentially causing irregular or missed periods. Conversely, significant weight gain can result in increased estrogen production, leading to hormonal imbalances and menstrual irregularities. Additionally, excess body fat can produce hormones called adipokines, which can further disrupt the menstrual cycle.
The Finale:
A missed period is not always a cause for immediate alarm, as numerous factors can contribute to irregularities in menstrual cycles. However, it’s essential to pay attention to any persistent changes or accompanying symptoms and consult with your gynecologist if necessary. By understanding the various reasons behind missed periods, women can better navigate their reproductive health and address any underlying issues effectively. Remember, beyond the calendar, there’s a complex interplay of factors influencing menstrual cycles, and listening to your body is key to maintaining overall well-being.
0 notes
Text
When to Visit a Gynecologist like Dr. Archana Singh?
Women's intimate health is a very sensitive and important topic, and regular visits to a gynecologist like Dr. Archana Singh plays a crucial role in maintaining overall well-being. Many women often wonder when is the right time to schedule an appointment with a gynecologist. In this blog, we will explore when a woman can plan to visit the gynecologist. From adolescence to menopause, understanding when to seek professional medical advice from an expert gynecologist like Dr. Archana Singh can contribute to early detection and prevention of potential health issues.
Adolescence and the Onset of Menstruation
As young girls transition into adolescence, the onset of menstruation is a significant event in a girl’s life that marks the beginning of reproductive health concerns. It is advisable for girls to have their first gynecological visit between the ages of 13 and 15, or when they start menstruating. This initial visit provides an opportunity for the gynecologist to discuss menstrual health, address any concerns, and educate the patient about maintaining proper hygiene.
Birth Control and Family Planning
For women who are sexually active and considering birth control or family planning, consulting a gynecologist like Dr. Archana Singh is essential. Whether it's exploring different contraceptive methods or discussing family planning options, a gynecologist like her can offer personalized guidance based on individual health considerations and lifestyle choices.
Sexually Transmitted Infections (STIs)
If a woman becomes sexually active, it is crucial to schedule regular checkups with an expert gynecologist like Dr. Archana Singh checkups to screen for sexually transmitted infections (STIs). Early detection and treatment of STIs are essential for preventing complications and maintaining reproductive health.
Pregnancy and Prenatal Care
When planning for pregnancy, scheduling a preconception visit to a gynecologist is beneficial. This allows the healthcare provider to assess overall health, discuss lifestyle changes, and provide guidance on optimizing fertility. Once pregnant, regular prenatal visits are vital to monitor the health of both the mother and the developing fetus, ensuring a healthy and successful pregnancy.
Menstrual Irregularities and Pelvic Pain
Menstrual irregularities or persistent pelvic pain should not be ignored. These symptoms could indicate underlying reproductive health issues such as endometriosis, polycystic ovary syndrome (PCOS), or other conditions. Seeking the expertise of a gynecologist like Dr. Archana Singh can help diagnose and address these concerns, promoting early intervention and effective management.
Perimenopause and Menopause
As women approach perimenopause and menopause, hormonal changes can lead to various symptoms such as hot flashes, mood swings, and changes in libido. Gynecological visits during this phase are essential to discuss symptoms, explore hormone replacement therapy options, and address any concerns related to bone health, heart health, and overall well-being.
Postpartum Care
After giving birth, women should schedule postpartum checkups with their gynecologist to address any physical or emotional concerns. Discussions may include family planning for future pregnancies, postpartum depression, and recovery from childbirth.
Gynecological Cancers
Regular gynecological checkups are essential for the early detection of gynecological cancers, such as cervical, ovarian, and uterine cancers. Pap smears, pelvic exams, and other screenings are vital components of preventive care that can help identify abnormalities before they progress.
Understanding when to visit a gynecologist like Dr. Archana Singh is crucial for maintaining optimal reproductive health throughout a woman's life. From adolescence to menopause, regular gynecological check ups empower women to take control of their well-being, address concerns proactively, and prevent potential health issues. By prioritizing reproductive health and seeking professional guidance, women can ensure a healthier and more fulfilling life. Remember, it is always advisable to consult with a healthcare professional for personalized advice based on individual health needs and circumstances.

0 notes
Text
How does age impact menstrual patterns?

Age significantly impacts menstrual patterns, with changes occurring at different life stages:
Puberty:
Menstruation begins during puberty (ages 9 to 16), with initial irregularities as the reproductive system matures.
Adolescence:
Menstrual cycles stabilize, but variations may persist for a few years after the first period.
Reproductive Years (20s to 40s):
Cycles are generally regular, lasting 21 to 35 days, with bleeding for 2 to 7 days.
Mid-30s and Beyond:
Mid-30s bring hormonal fluctuations, leading to potential irregularities in flow and frequency.
Perimenopause:
In the late 40s, perimenopause sees increased irregularities, skipped periods, and changes in bleeding.
Menopause:
Officially reached when no menstruation occurs for 12 consecutive months; bleeding ceases.
Postmenopause:
Postmenopausal women no longer experience menstrual cycles but should monitor unexpected bleeding.
Pregnancy and Postpartum:
Pregnancy halts cycles temporarily, and the return of menstruation postpartum varies.
Hormonal Contraception:
Methods like birth control may influence menstrual patterns, leading to lighter or regular periods.
Individual variations exist, influenced by genetics, health, and lifestyle. Consult a healthcare provider for deviations from normal patterns, ensuring timely monitoring and addressing menstrual health concerns across life stages.
For additional details, seek guidance from Dr. Arohi Tasgaonkar, recognized as one of the top Gynaecologists in Thane.
#gynecologist in thane#dr. arohi tasgaonkar#complete women’s care#gynecologist in manpada#gynecologist in ghodbunder road thane#gynecologist in waghbil#gynecologist in ghodbunder road thane.#gynecologist in kasarvadavali#gynaecologist in hiranandani estate thane#gynaecologist in bethany hospital thane.#menstrual problems
0 notes
Text
Fertility Challenges - Female Infertility Tests and Diagnosis
Ovulation is unquestionably controlled through seminal liquid add together hormones. Any moment a high profile this kind of hormone levels are often plagued, this kind of ovulation is usually affected. Majority of the young women have anovulatory month to month durations by way of their copy life. Such a event might be more widespread with regards to females of nearly every age who's simply just obtained their period, and also adult women on its way menopause. Of which staying stated, anovulatory durations could also come about with regards to balanced women who's usual periods.
Fertility support supplements A variety of women experiences long-term anovulation; young adults assess for this specific sophisticated food items diet plan problem, comparable to polycystic ovary problem (PCOS), generates normal appreciation much more difficult.
A great abnormal as well as absent period is usually a manifestation of most probably ovulation problems. Quite a few components is probably during an original new offer for any hormonal imbalance getting an effect on ovulation. Some examples are frequently major excess fat move, stress, over-exercise, as well as illness. As a result, it is always advisable to get natural health practice fertility support.
When the balanced female together with usual durations works by using ovulation assessments or use the Original Sexual interest Check out as well as discovers a infrequent anovulatory method, don't periods nervousness: that may be normal. Of which staying stated, should you can't know the specific LH enhance together with ovulation assessments with regards to many persistent assessments, all of them are the best should you talk with any professional fertility support Perth.
Should your time period amid sum ovulation plus the start out the subsequent period measurement little (less as compared with 10 days), this indicates could even if you'll be capable of have got youngsters, the specific fertilized ovum is unquestionably obtained lessen before it's born. Can have decide to put through the divider for any uterus. It's event that will you notice if you happen to go with a ovulation try or even a seminal liquid add together monitor.
After owning reached the change of life, giving birth seems to have ended currently being possible. Inside period before the change of life (perimenopause), it can be difficult in order to conceive. Should your mom travelled via the change of life extremely beginning, most probably are frequently inspired by using this make a difference whenever well. Check out to discover with regards to simply just strangely grow older this kind of mom reached menopause. Any moment she's obtained catastrophe the change of life, we recommend that any individual check out this kind of forth-coming giving birth basics together with healthcare fertility support western Australia.
0 notes
Text
What Are The Reasons Behind Late Periods? Discover Here!
What Are The Reasons Behind Late Periods? Discover Here!
Many women believe that a late period means there's a chance of being pregnant. However, this isn't always the case, and it is important to recognise that each woman's body is unique. Various factors, such as hormonal imbalances or menopause, can cause late periods.
It is normal for periods to be delayed by up to 38 days, but they usually last for 28 days. If your period arrives after 38 days, it is considered late. Do you want to know why your period may have been delayed? Then read on to discover the possible reasons!
What Indicates Delayed Periods?
The following factors that indicate late periods are:
1. Being Pregnant
When you become pregnant, your uterus lining thickens to support the baby, causing periods to stop. However, when you are not pregnant, the lining of the uterus discharges blood, which causes periods.
2. Polycystic Ovary Syndrome (PCOS)
An ovarian disorder called PCOS prevents the egg from being released during ovulation. Females with this syndrome typically experience irregular, late, and reduced menstrual flow.
PCOS also causes several additional symptoms, including hair loss, pimples and acne, blackening of the neck, facial hair, difficulty losing weight and unusual weight gain, and excessive fat deposition in the abdomen.
3. Extreme Diet And Exercise
A proverb states that excess of something can have adverse effects. Diet and exercise follow the same rules. It is perfect if you follow the requirements for food and exercise. Extreme nutrition and practice, though, may cause your periods to be late sporadically.
As the saying goes, “Too much of anything can be bad,” this applies to diet and exercise. It is important to adhere to a balanced diet and exercise routine. However, excessive changes to your nutrition and physical activity can lead to irregular menstrual cycles. Anorexia or bulimia, calorie-restrictive diet, rapid weight reduction, intense exercise, and training are additional causes of amenorrhea.
4. Pills For Birth Control
Birth control tablets can result in withdrawal bleeding, often known as fake periods. Most doctors advise women to take birth control pills for a set length to have regular periods because they include oestrogen and progestin, which prevent pregnancy and thus aid in getting a period.
5. Stress
Stress can be caused by work, family, workplace environment, and work pressure. It can negatively affect the mind and contribute to health issues. Delayed periods can also be caused by stress.
6. Perimenopause
Many women can tell they are going through menopause or perimenopause if their periods become late or stop altogether. During this time, periods may also become lighter, heavier, or less frequent, depending on the woman. On average, menopause starts around age 51.
7. Breastfeeding
It is typical for breastfeeding to provide sufficient nutrition for a baby, but it is common for a mother to have irregular periods and reduced blood flow during this time. It is also possible to become pregnant while breastfeeding, as the nursing phase is not a reliable form of contraception, as shown in a study. It is important to have regular periods while breastfeeding.
What Are The Foods That Can Cause Periods?
Here are some foods that can cause periods:
1. Jaggery
During winter, jaggery is often consumed due to its heat-generating properties. Additionally, it contains iron which can help increase the body's haemoglobin levels. It should be noted that consuming jaggery may result in induced periods.
2. Ginger
Ginger can induce periods and promote the menstrual cycle by raising body temperature and improving its regularity.
3. Pineapple
Pineapple contains bromelain, a substance that can help to soften the uterine lining and stimulate periods. As a result, it is often considered a fruit that can aid in period regulation.
4. Turmeric
Turmeric is often regarded as a traditional food that can potentially induce periods due to its antispasmodic properties. These properties are believed to influence the uterus, encouraging it to shed its lining and initiate menstruation.
5. Papaya
Raw and ripe papaya are known for their ability to induce periods. It is commonly advised to avoid consuming papaya during pregnancy due to its high estrogen content, which can trigger the onset of menstruation.
When Should I See A Doctor?
If your periods are late for a long time, it is important to see a doctor. This is especially crucial if you have recently had sex and there is a chance of pregnancy. Visiting a healthcare provider is also necessary if you experience sudden changes in your menstrual cycle, ongoing irregularity, or other symptoms such as severe pain or excessive bleeding.
The Final Say
Delayed periods can potentially cause health issues. It is generally considered normal for a period to be delayed by 1, 2, or 3 days, as well as for periods that are delayed by 28 to 38 days.
However, if a period is delayed by more than 38 days, it may cause concern. In such cases, visiting the gynaecology department at Bansal Hospital for further evaluation and guidance is recommended.
About Bansal Hospital
Bansal Hospital is a multispeciality hospital and is one of the leading, reputable and reliable healthcare providers trusted by patients and their families across the region. It has all the major departments, including cardiology, neurology, oncology, orthopaedics, gastroenterology, urology, liver transplant, bone marrow transplantation, nephrology, gynaecology and more. The hospital is equipped with state-of-the-art facilities and technology and has a team of highly qualified and experienced doctors and medical staff who provide round-the-clock care to the patient.
Visit Our Website

0 notes
Text

Irregular periods or menstrual irregularities can be caused by various factors. These factors can disrupt the normal hormonal balance in a woman's body, affecting the regularity of her menstrual cycle. Here are some common factors that can lead to irregular periods:Stress: High levels of physical or emotional stress can impact hormone production and regulation, leading to irregular periods.Weight Fluctuations: Significant weight loss or gain can affect hormonal balance, particularly if it disrupts the normal functioning of the hypothalamus-pituitary-ovary axis.Polycystic Ovary Syndrome (PCOS): PCOS is a common hormonal disorder that can cause irregular periods along with other symptoms like acne, excessive hair growth, and ovarian cysts.Thyroid Disorders: Thyroid imbalances, such as hypothyroidism or hyperthyroidism, can disrupt the menstrual cycle by affecting hormone levels.Excessive Exercise: Intense physical activity, especially when combined with low body fat, can lead to irregular periods due to its impact on hormones.Chronic Illness: Certain chronic conditions like diabetes, celiac disease, and inflammatory diseases can influence hormonal regulation and cause irregular periods.Medications: Some medications, including certain contraceptives, antipsychotics, and chemotherapy drugs, can affect hormonal balance and lead to irregular menstruation.Birth Control: Starting, stopping, or changing birth control methods can initially cause irregular periods as the body adjusts to the changes in hormone levels.Perimenopause: The transitional period leading to menopause, known as perimenopause, can cause irregular periods as hormone levels fluctuate.Uterine or Ovarian Issues: Conditions like fibroids, polyps, or ovarian cysts can interfere with normal menstruation.Eating Disorders: Disorders like anorexia nervosa or bulimia can disrupt hormonal function and lead to irregular periods.Excessive Caffeine or Alcohol Consumption: High intake of caffeine or alcohol can potentially affect hormone production and lead to menstrual irregularities.Travel or Time Zone Changes: Rapid changes in time zones or extensive travel can temporarily disrupt the body's internal clock, affecting hormonal patterns.Breastfeeding: During breastfeeding, the hormonal changes required for milk production can cause irregular periods.Genetic Predisposition: A family history of irregular periods or hormonal disorders can increase the likelihood of experiencing menstrual irregularities.
#aurawomen#aura#fertility#ivf#infertility#iui#irregular periods#maternity#menstrual cycle#menstruation#menstrual health#period products
1 note
·
View note
Text
It is possible to get Pregnant After Menopause?
Menopause is a natural biological process that occurs when a woman's reproductive years come to an end. Women typically experience a decline in hormone production in their late 40s to early 50s, resulting in the cessation of menstruation. Many women consider menopause to be the end of their childbearing years, but is it truly impossible to conceive after menopause? In this article, we will look at the possibility of conception after menopause, the various methods for achieving it, and the factors to consider.
Before we get into the topic of pregnancy after menopause, let's first define menopause. Menopause is officially declared when a woman has gone 12 months without having a menstrual period. It is a natural transition caused by a decrease in estrogen and progesterone production in the ovaries. Women experience a variety of physical and emotional changes as their hormone levels drop, including hot flashes, mood swings, and changes in bone density.
Menopause and Fertility
During a woman's reproductive years, her ovaries release eggs in each menstrual cycle, offering the possibility of conception. However, as menopause approaches, the ovaries start to release fewer eggs, and eventually, they stop releasing eggs altogether. As a result, a woman becomes infertile after menopause, and natural conception becomes highly unlikely.
Can You Get Pregnant After Menopause?
While natural conception after menopause is improbable, there have been rare cases of post-menopausal pregnancies. In these cases, women have become pregnant without medical intervention. These occurrences are known as "spontaneous post-menopausal pregnancies" and are exceedingly rare. The likelihood of conceiving naturally after menopause is less than 1%.
Post-Menopausal Pregnancy: Medical Interventions
For women who desire to conceive after menopause, advancements in medical technology offer potential solutions. One such method is in vitro fertilization (IVF). IVF involves the retrieval of eggs from a donor or frozen eggs that were collected before menopause. These eggs are then fertilized with sperm in a laboratory and the resulting embryos are implanted into the uterus of the woman, allowing her to carry the pregnancy.
Natural Conception After Menopause
While natural conception is unlikely, some women have reported irregular menstrual cycles during perimenopause, which is the transitional phase leading up to menopause. During this time, women may still release eggs sporadically, leading to unexpected pregnancies. Therefore, it is crucial for women in their late 40s and early 50s to use birth control if they wish to avoid pregnancy.
Risks and Considerations
Pregnancy after menopause, whether achieved naturally or through medical intervention, carries several risks and considerations. The health risks for both the mother and the baby increase with age. Older women may have pre-existing health conditions that can complicate the pregnancy. Additionally, the risk of genetic abnormalities in the baby rises with maternal age.
Emotional and Psychological Aspects
Deciding to pursue pregnancy after menopause can be emotionally and psychologically challenging. It is essential for women and their partners to consider the emotional impact of such a decision. The process of fertility treatments and potential pregnancy can be both exciting and stressful, and it is crucial to seek support and guidance throughout the journey.
Support and Guidance
Couples considering pregnancy after menopause should consult with fertility specialist. These experts can assess the woman's overall health and discuss the available options, risks, and success rates. They can also provide emotional support and answer any questions or concerns the couple may have.
Lifestyle Factors and Fertility
Maintaining a healthy lifestyle is vital for women seeking to conceive after menopause. A balanced diet, regular exercise, and managing stress can positively impact fertility. It is also essential to avoid smoking, excessive alcohol consumption, and other harmful habits that can affect fertility and overall health.
Conclusion
In conclusion, while natural conception after menopause is highly improbable, medical advancements in fertility treatments have opened up possibilities for women to conceive post-menopause. Methods like in vitro fertilization have enabled many women to experience the joys of motherhood later in life. However, it is crucial to consider the risks and emotional aspects associated with post-menopausal pregnancy. Seeking professional guidance and maintaining a healthy lifestyle are vital steps in this journey.
FAQs
Is it common for women to get pregnant after menopause naturally?
No, it is exceptionally rare for women to conceive naturally after menopause. The likelihood is less than 1%.
What is in vitro fertilization (IVF), and how does it work for post-menopausal women?
IVF involves fertilizing eggs with sperm outside the body and then transferring the resulting embryos into the woman's uterus, allowing her to carry the pregnancy.
Is emotional support essential for couples pursuing pregnancy after menopause?
Yes, pursuing pregnancy after menopause can be emotionally challenging. Seeking emotional support and guidance throughout the process is crucial.
What lifestyle changes can enhance the chances of conception after menopause?
Maintaining a healthy lifestyle with a balanced diet, regular exercise, and stress management can positively impact fertility.
0 notes
Text
Most Common Questions to Ask Your Gynecologist

A different smell down there? Sex during the period? Vaginal itching? Leaky bladder? All of these questions often promote women straight to the gynecologist they are comfortable with. Does this sound awkward? It is completely fine to feel awkward, but remember, speaking up about your doubts is your job. Your doctor’s responsibility is to answer awkward and uncomfortable questions. There are some questions mentioned below that you must ask your gynecologist.
A Question to Ask About Menstruation
A woman’s period begins between the ages of 8 and 15 and lasts until she reaches menopause.
How heavy or light should my menstrual flow be?
Women are different when it comes to their period cycle, from heaviness to the length and time of their blood flow. A woman’s blood flow range remains from heavy to light, but it varies as per her hormones, diet routine, lifestyle factors, activity level, etc. If you are experiencing heavy flow for more than 15 days, then you must visit the best gynecologist near you ASAP.
How many times do I menstruate?
A woman menstruates once a month regularly until she starts to walk into the menopause phase. Missing periods can be a sign of pregnancy, perimenopause, stress, or different kinds of changes in your daily health and lifestyle. If you experience such symptoms, you must consult the best Gynec around you, Diva is one of the Best Gynecology Hospitals in Ahmedabad with a well-experienced team of doctors.
Is it a fearful thing to have irregular periods?
Most women face irregularities in their period cycle that are caused by various factors. It also reflects their lifestyle factors and hormonal changes that come with age. It is best to consult with your gynecologist if you are experiencing irregular periods for a long period, as PCOS and PCOD can be the reasons for this problem.
Questions to Ask About Your Regular Check-up?
How can I reduce my risk of breast cancer?
Experts advise that women must know the signs and symptoms of breast cancer. Also, if she notices any changes in her breast, such as pain, redness, nipple discharge, or a mass, she should consult with a gynecologist she is comfortable with.
Test for BRCA Mutations?
A woman has a higher risk of ovarian and breast cancer if she inherits BRCA 1 and BRCA 2 gene mutations. However, it is also essential to note that not every woman with this gene will develop cancer. Hence, having a conversation with your doctor could help you with early detection, which can further help to treat cancer more effectively.
A Question to Ask About Safe Sex
Protection Options
There are various options available for both women and men if they are looking to prevent pregnancy or STIs. The best-known birth control methods are condoms, birth control pills, and many more. Consult your gynecologist about the best and most appropriate option for you based on your health conditions.
Do I need any kind of vaccinations?
Your gynec would suggest you have a vaccination if you are sexually active, just to reduce the risk of infection during intimation.
How to know about STIs?
The most common symptoms of STIs involve genital pain, vaginal discharge, abdominal pain, and painful urination. However, STIs can be asymptomatic, so you must visit your doctor to get the treatments done at the right time.
Questions to Ask Related to Pregnancy
How long will it take to get pregnant?
Discussing getting pregnant with your gynecologist is normal for both you and your husband, and you will learn what to expect before you expect too much. If you live in Ahmedabad or near Ahmedabad, contact Diva Women’s Hospital, the best maternity hospital in Ahmedabad with the best gynecologists. As soon as a couple tries to conceive, this process doesn’t happen right away as it takes time. A woman between the ages of 25 and 30 has a 20% chance of getting pregnant in a month.
How can I increase my fertility?
Knowing your fertility status and tracking this regularly is the best way to enhance the chances of getting pregnant when you try to conceive. Within 28 days of your cycle, ovulation occurs on one day between the 11th and the 21st day of your cycle. The best gynecologist always suggests using a fertility tracker so that you can have an insight into your fertility.
How to get rid of using birth control:
If you are using birth control methods such as; pills, IUDs, patches, or any kind of protection, then you must consult with your doctor about when to stop using them, when trying to conceive. This is the most asked question, and the answer varies from woman to woman based on their body and the birth control methods they are using.
When can I go for fertility treatment?
There are various options available for a woman if she wants to have a baby with the help of technology if she is not able to conceive naturally. Ask your gynecologist about which fertility treatment would be good for you based on your health and wellness.
Questions to Ask During Pregnancy?
What can I do to keep my baby healthy?
The best way to keep your baby healthy is to make sure you are healthy. For this, have a proper meal, have a proper rest, and avoid heavy exercise or any kind of heavy physical activity. Make sure you consult your doctor before taking any kind of supplements or medication, as it can negatively affect your baby’s health.
How to figure out if I am having labor?
The most important question to ask your gynecologist is when you should expect labor pains or symptoms and what they might feel like. Also, your gynec is the best resource to know whether your body is fit for vaginal delivery or not. Feel free to mention different stages of your labor to your gynecologist so that you can make an informed decision on when to go to the hospital.
A woman faces different kinds of problems and experiences throughout her life that require the proper advice of experts who can guide her throughout her journey of being a mother. Have the best child and maternity services at one of the best women’s hospitals in Ahmedabad, Diva Women’s Hospital.
1 note
·
View note
Text
Hormonal Balancing in Females

Hormones are our body’s chemical messengers. They travel through our bloodstream to various tissues and organs. Hormones affect different bodily processes:
· Growth and development
· Metabolism
· Sexual Health
· Mood
· Reproduction
The Endocrine Glands synthesize hormones. The major endocrine glands are the pineal, thymus, pituitary, thyroid, adrenal, and pancreas. In addition, men produce hormones in their testes, and women have them in their ovaries.
Hormonal Imbalance
Hormonal Imbalance occurs when the endocrine glands produce too much or too few hormones. Hormones are solid chemical messengers, and a slight change in the levels can affect your bodily functions. Imbalances in hormones like insulin, steroids, growth hormones, and adrenaline affects both males and females. Additionally, females may experience imbalances in estrogen and progesterone levels, while males are more likely to experience inequalities in testosterone levels.
Symptoms of Hormonal Imbalance in Females
Some of the significant symptoms in Females are:
· Insomnia
· Mood swings
· constipation or diarrhea
· infertility
· low sexual drive
· irregular menstrual cycle
· Insomnia
· abdominal or back pain during menstruation
· unexplained weight gain or weight loss
· brittle bones
· hirsutism, or excessive hair growth
· rashes on the skin
A significant symptom in females of hormonal Imbalance is Weight Gain. Obesity is the root cause of important health issues like Diabetes, Cardiovascular diseases, Stroke, Depression, Cancer, Respiratory diseases, Cognitive difficulties, Musculoskeletal Disorders, and many more. Shedding your extra pounds in Gym can be strenuous. We at ULTRA BODY take a different approach to your weight loss journey. We plan on naturally balancing your hormones and eliminating bad habits while working with your lifestyle to build a program that works for you. Our Plan is fully customized to meet your weight loss goals while relieving hormonal and adrenal imbalance symptoms.
Causes of Hormonal Imbalance
We all experience natural periods of hormonal Imbalance or fluctuations from time to time. Chronic Hormonal Imbalance occurs when the endocrine glands are not functioning correctly. Several Medical Conditions, Lifestyle Habits, and Environmental Factors can cause hormonal Imbalance.
Hormonal Imbalance is seen in patients with Diabetes, Addison’s disease, Hyperthyroidism, Hypothyroidism, Hyperglycemia, Hypoglycemia, Iodine deficiency, Hereditary pancreatitis, Cushing’s syndrome, solitary thyroid nodules, congenital adrenal hyperplasia, Turner syndrome and many more.
Females naturally experience hormonal Imbalance during Puberty, Menstruation, Pregnancy, Childbirth, Breastfeeding, Perimenopause, Menopause, and Postmenopause. Certain medical conditions in females, like PCOS, hormone replacement or birth control medications, hormonal imbalance treatment, Ovarian cancer, and primary ovarian insufficiency, can cause hormonal Imbalance.
Ways to balance your hormones
· Getting enough sleep
· Avoiding too much light at night
· Managing Stress
· Exercising
· Cutting down on sugary foods
· Eating healthy fats
· Eating lots of fiber
· Eating plenty of fish
· Avoiding overeating
· Drinking green tea
· Quitting smoking
At ULTA BODY, our supplements act as a “vitamin” to support your hormone, thyroid, and adrenal production at levels optimal for YOUR body. Our organic products nourish your adrenals, thyroid, and hormonal system to achieve their optimal performance. Ultra Body’s supplements are designed to realign estrogen, progesterone, and testosterone levels so that you can lose weight, eliminate symptoms and support a healthy stress response.
1 note
·
View note
Text
Egg white cervical mucus with brown tinge

When the fertilized egg attaches itself to the uterine lining it can cause a small amount of bleeding, more commonly known as “implantation bleeding”. If you notice a small amount of brown discharge or spotting a couple of days before you are expecting your period it could be a sign that you are pregnant. This spotting can be light red, pink or brown in colour as it often mixes with the clear egg white type cervical fluid present around the time of ovulation. When the egg leaves the follicle during ovulation or as a result of the changing hormone levels it is common for some women to notice some mild spotting. Seeing brown spotting mid-way through your cycle could be a sign that you have just ovulated. If you are noticing prolonged periods of this or are experiencing other side effects such as nausea, weight gain, sore or swollen breasts and mood changes, then it is best to let your doctor know as they will be able to recommend a birth control method that better suits your body. If you have just started using a new hormonal birth control method or forgot to take your birth control pill for a day or two, you may experience brown discharge. The drawback to this hormonal interference is that they can cause some unwanted side effects. Most hormonal birth control methods work by interfering with your bodies natural hormonal cycle to prevent your body from ovulating. However, if this becomes a regular occurrence then it is best to let your doctor know. While it might appear alarming, in most cases it is nothing to worry about. This is just the rest of the endometrial cells being expelled. Over the course of your next cycle, you might notice pink or brown spotting in your underwear or when you wipe. Sometimes, your body isn’t able to completely expel all the endometrial lining immediately leaving a small amount in the uterus. Menstruation occurs when your hormones tell your body that you haven’t gotten pregnant this cycle causing your body to expel the endometrial lining in preparation for your next cycle. It might be caused by something as simple as a delayed period, your hormonal contraceptive or the onset of perimenopause, some other potential reasons include: It is often perfectly natural to notice brown discharge during your cycle. See also: Discharge Before Period: What Does it Mean? However, if you are experiencing other symptoms along with brown discharge or if you are noticing brown discharge mid-cycle then you should talk to a parent or see a doctor as it might the sign of PCOS or an infection. If you have recently started your period, having a small amount of brown discharge is often nothing to be concerned about. The middle of your cycle marks the time around ovulation. The colour of your discharge changes over the course of your menstrual cycle due to fluctuations in your hormones, from red/brown during your period, to thick and white just after your period and clear, like egg white during the middle of your cycle. See also: Yellow Vaginal Discharge: Should you be Worried?Ī common question and cause for concern for many girls experiencing their first or second year of menstruation is that their period blood is not always red. This is because the circumstances and symptoms that accompany brown discharge often shed more light on the cause of the brown discharge than the discharge itself. Whether or not there is a chance that she is pregnant.Whether she using hormonal birth control.When a woman comes to my office and is concerned about brown discharge the first step I take is to get a better understanding of her personal situation, this includes: While it may be a sign of a health problem, in the majority of cases, it's nothing to worry about! Also, experiencing a small amount mid-cycle can be a sign of ovulation or pregnancy (implantation bleeding) - a positive sign if you are trying to conceive. Most of the time, brown discharge is just blood from your last period taking a little longer to be expelled.Īlthough for many, the sight of unexpected discharge in our underwear or when we wipe can be a cause for alarm. In the vast majority of cases having a little bit of older blood in your discharge is perfectly fine and nothing to worry about. Treatment is also available in line with clinical guidelines. Check your vaginal health from home with our at-home Vaginitis Test.

0 notes
Text
Periods in your 20's v/s 40's

Most of us may think that isn't it the same bleeding, cramps and PMS. But no, your menstrual cycle changes as you grow and here's how periods can differ in your 20's and 40's.
Periods in your 20's
In your teens, when you just started bleeding, you re still adjusting to the cycle and there's always an unexpected surprise apperance. But as you reach your 20's, your cycle gets more consistent.
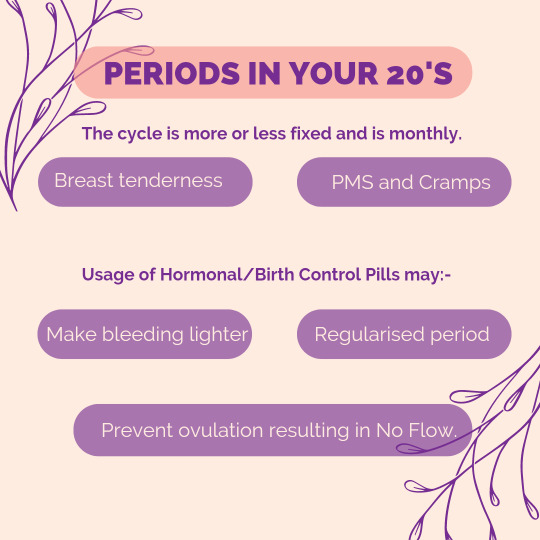
The cycle is more or less fixed and is monthly. Not to mention the start of the unpleasant symptoms of breast tenderness, PMS and nasty cramps. Many menstruators around this age start taking hormonal pills due to various reasons. The pill triggers changes to your flow, making it lighter, less pain and PMS or more regularised periods.
In fact, birth control pills prevent ovulation, and without ovulation, there's no uterine lining buildup that has to be shed, this can result in no flow.
Periods in your 40's
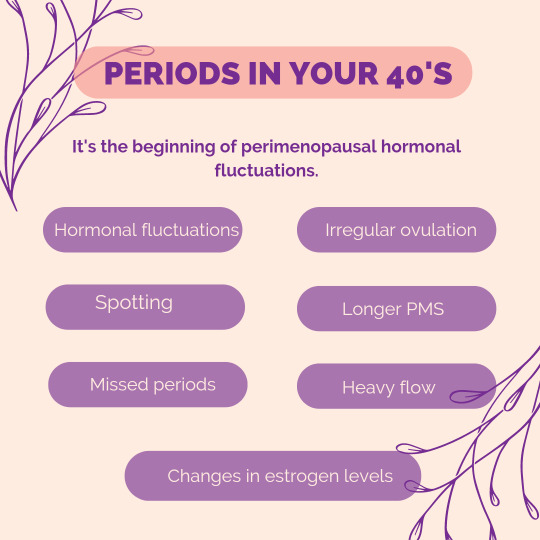
It's the beginning of more changes, including perimenopausal hormonal fluctuations, which are precursors to menopause. Your body starts preparing for menopause. These hormone fluctuations cause ovulation to be more irregular, and your estrogen level change means you could start experiencing missed periods, a heavier flow, spotting between periods, and longer stretches of PMS.
During perimenopause your periods can be less predictable and even if ovulation is erratic, you can still get pregnant. A woman isn't in menopause until her periods have ceased for at least a year.
Take care and make sure to note your change in cycle.
~Lokeshwari H Naidu
Team @lemmebegirls
#lemmebe#justlemmebe#positivity#lets talk#health#mensturators#menstrual talk#period talk#period problems#menstrual cups#menstruators#hormones#estrogen#periodpositive#stopthestigma#pms#periodpain#period cramps#menstrual cycle
3 notes
·
View notes
Text
11 Women With PMDD Share What It's Really Like
Premenstrual dysphoric disorder is the evil cousin of PMS. They share the same types of symptoms—moodiness, increased hunger, cravings, fatigue, cramps, pain, brain fog, and depression, among others—but for PMDD sufferers, those symptoms get so bad they can cripple a woman's ability to lead a normal life.
While up to 85 percent of women get PMS, according to the US Department of Health, only about 5 percent of women experience PMDD, according to the American Journal of Psychiatry.
We asked women with PMDD what it's really like living with the disorder. Here are their stories:
"I was diagnosed with PMDD last summer. Six months prior to my diagnosis, I started taking a certain birth control and soon every month I was experiencing severe PMS issues. I am a generally happy person, but during those few days I was someone entirely different. I was extremely depressed and anxious, having much more frequent panic attacks, and was super sensitive and lonely. I was even suicidal, which was terrifying. And the worst part was I was convinced that I had always been this miserable, and that I would always be this miserable, and it was never going to change. It felt as if someone had completely burned out the light in me and all happiness and joy and hope was gone. I didn't make the connection that it was related to my period but thankfully a close friend did. I have since switched birth control, which helped a lot, and increased the dosage of my anti-anxiety and anti-depressant meds. Most importantly, I am aware of the way I feel those few days so I know to expect it, and I can logically remind myself that I will stop feeling that way soon. Looking back, I realize that I've probably always had pretty bad PMS or PMDD. The birth control worsened it but it was also causing a lot of issues I wasn't aware of previously as well." —Katherine H., 22, Edmonds, WA
———————————
"PMDD is out of control. I cry really easily for about a week. My biggest issue is that I am convinced that I am failing at everything—being a wife, a mom, work projects, fitness, my whole life! And even though it feels so real I constantly have to question if my feelings are valid or if they are amplified by my cycle. I just set an alert in my phone to remind me to consider my hormones the next time I feel that way." —Krysten B., 32, Toronto, CA
———————————
"A week before my period, I become a complete psycho, completely unlike myself. I'm tearful, want to eat everything that's sweet or salty, have absolutely no tolerance for anything other than perfection, and prefer to be left completely alone. I already take an antidepressant but my PMDD was a complete nightmare so my doctor gave me Prozac to take for just 10 days a month. Basically, I start it when I start to get that irrational feeling and keeping taking it until my period starts. And that's just the emotional stuff. On the physical side, I have debilitating cramps, backaches, and headaches that last for days. Yep. I'm a peach." —Kristen L., 40, Knoxville, TN
———————————
"In the past, PMDD almost made me suicidal and totally broke my spirit. Yes it wasthat bad. Every month. Eventually I got tired of being a 'crazy PMS woman' and decided I needed to fix this. Since I don't like to take pharmaceuticals, I branched out to homeopathic remedies and I discovered St. John's Wort and essential oils, especially clary sage and Doterra Calm-Its. It's a lot better now but I still have my hard days." —Amy S., 43, Zebulon, NC
———————————
"My PMDD got so bad I had to go to a psychiatrist and be put on Prozac along with another antidepressant I was already taking. I was a mess—anxious, crying randomly over the smallest thing, and eating everything in sight. One example is someone made a YouTube mashup of the Age of Ultron trailers with Pinocchio footage and the 'I've got no strings on me' song and that wrecked me for weeks. Every time I thought about scenes from Pinocchio I would start panicking and crying at my work desk. It's been a few years and I'm better now. I'm off birth control and weening myself off the Prozac. I notice a week before my period I will sob during any sad part in a movie or book I'm reading, and a day or two before, I notice I'm more likely to be anxious." —Kate W., 36, Alaska
———————————
"This has impacted my ability to work effectively. My pet peeve is when people say 'it must be close to your time of the month' when they simply don't like what I'm saying. I have run into that problem a lot at previous jobs and it makes it really hard to be taken seriously. It's bullshit because my feelings are valid regardless and also PMDD is not a joke. I am so lucky now to have a male boss who understands but it wasn't always that way. I have also have found a lot of relief with naturopathic and herbal remedies." —Amalia F., 28, Vancouver, Canada
———————————
"My PMS was tolerable until my second child was born and then everything went off the rails. I'd be looking forward to plans with others, happy, and then about 10 to 14 days before my flow would start, my mood would turn on a dime. I'd be horrible—crying, screaming that ~nobody understands~, just so much emotional pain. I'd basically lock myself up in the bedroom for a full day to cry, get angry, and feel sorry for myself. It took three doctors before I finally found one who would listen to me before I was finally diagnosed with PMDD. I took Prozac for three years for it but it made me feel numb, like a zombie and not like myself. So I quit and my family just deals with me now. As I've gotten closer to menopause the PMDD is not as bad, but can be very unpredictable due to hormonal swings from perimenopause. The worst part now is I feel like my friendships have suffered. I always seem to have episodes around major holidays and events and I end up bumming everyone out if I do show up so I end up staying home a lot." —Colleen T., 50, St. Paul, MN
———————————
"I'm overly emotional for the week before my period. Saying that makes it sound like it's not that bad but I get so distraught that my fiance has actually scheduled it in his phone as 'blood sport' to remind himself what's coming. I'm thankful that he's patient because I also feel like everyone hates me that week, too." —Kenlie T., 36, New Orleans, LA
———————————
"All month long I'm fine and feel even and calm and then suddenly, the week before my period, I can't handle even the tiniest little thing. My irritability goes through the roof (which is not great since I have a 5-year-old) and I feel like I have no friends. It really makes me sad." —Jessica S., 28, Broomfield, CO
———————————
"I know my period is coming because all of a sudden all of my joints hurt, especially my knees and ankles. I also get crazy gnarly cramps and once I even had a cyst that ruptured while I was on a date and the guy had to take me to the hospital! It was so embarrassing. Thankfully my husband now is very understanding when this time rolls around each month. The worst part is people who just think I make this stuff up. Some months are better than others and sometimes the pain is completely debilitating! My emotions are also a rollercoaster. Anytime I see something cute or inspiring, I burst into tears." —Ivie C., 21, Rexburg, ID
———————————
"My PMDD manifests in both mental and physical symptoms. From the time I got my period at age 12, I've had extreme cramps and heavy bleeding. I'd leak at school through a super maxi pad every class so I'd tie sweatshirts around my waist and have to scrub my clothes when I got home. It was super humiliating. I'd have to take six to eight ibuprofen at a time to deal with cramps, and if I didn't I'd end up on the floor sweating like I had the flu. Sometimes I'd even throw up. This meant I ended up spending a lot of time sick in bathrooms and knew where every restroom was at all times. Birth control helped manage the PMDD and other issues, but as soon as I was done having kids, I had a hysterectomy. That was the best thing I've ever done." —Mandy P., 39, Mendon, UT
https://www.womenshealthmag.com/health/a19972132/premenstrual-dysphoric-disorder/
#premenstrual dysphoric disorder#PMDD#pmdd awareness#living with pmdd#actually pmdd#mental health awareness#mental health#women's health#pms#premenstrual syndrome#afab problems
23 notes
·
View notes