#bone spur on achilles tendon
Text
A heel spur is a bony growth that forms on the underside of the heel bone, often causing pain and discomfort, especially when walking or standing for long periods. As a podiatrist in Dubai, Dr. K. P. Meda specializes in diagnosing and treating conditions like heel spurs. With his expertise, patients can expect a comprehensive evaluation to determine the underlying cause of the heel spur and develop a personalized treatment plan. Dr. Meda may recommend conservative measures such as orthotic inserts, physical therapy, and stretches to alleviate symptoms. In severe cases, he may suggest more advanced interventions like extracorporeal shockwave therapy or surgery. By addressing the root cause of the heel spur and utilizing Dr. Meda's expertise, patients can effectively manage their condition and find relief from pain, allowing them to resume their daily activities comfortably.
#heel spur treatment#heel spur surgery#heel spur exercises#shoes for heel spurs#can heel spurs go away#bone spur on achilles tendon#burning pain in heel
0 notes
Text
Just ordered jazz shoes that will hopefully fit and tide me over until I can find character shoes that fit my incredibly fucky feet (medical term) and now I've got Chicago stuck in my head (because jazz).
#adventures in community theatre#we have our first dance rehearsal thursday so hopefully the jazz shoes fit and I won't be dancing in sneakers but idk#I already tried and returned two pairs of character shoes (the 9 was too small and the 9.5 was too big)#I just ordered 3 pairs from amazon try before you buy#so hopefully one of those will fit#and when I say incredibly fucky feet:#I have 'flexible flat feet' (I have an arch when not weight bearing that collapses when I stand)#plus my forefoot is wide and my heel is narrow#and I overpronate like a motherfucker#and I have plantar fasciitis#and bone spurs#and my right achilles tendon is tight#oh and my ankles are weak and prone to rolling#SHOE SHOPPING IS FUN Y'ALL
1 note
·
View note
Text
My ankle journey
I am sharing this with all you good people on the dash because I am so fucking mad it took so long for me to learn it and if I can spare one (1) person the agony it will be worth it.
So for like...oh, 8 or 9 months, I've been struggling with pain/inflammation/tendinitis in my left Achilles tendon. I don't know what caused it. It just started up (welcome to middle age, this shit happens). It wasn't severe enough to be debilitating, but it was annoying and limiting. It was also intermittent, in that some days it would be very painful and other days hardly at all. The kind of shoe I was wearing affected it a lot.
Now, I have bone spurs on both heels (it's just a thing that happens as you get older sometimes). I'm also aware that heel pain is usually the result of tight calf muscles that pull and irritate the tendon. I tried stretching that calf muscle. You know the stretch, this bitch right here:

I did it all the time. I also iced the ankle after walking for awhile, hoping to avoid inflammation. Results were...unsatisfying.
I went to:
A chiropractor
A podiatrist
A physical therapist
A bodywork coach
They all gave me some variation on the "strengthen your calf muscle, stretch your calf muscle" advice. I continued doing this without results.
I was getting frustrated, and a little afraid that this was just my life now. Finally, I thought...maybe some targeted massage might help. I asked for rec on a local FB site and was pointed to a woman who specializes in therapeutic massage including cupping, etc.
I went to her a week ago.
She spent over half our first session working on my left lower leg. Within about 10 minutes of making my eyes water, she uttered the sentence I did not know I had been waiting to hear:
"Oh, it's your soleus."
Excuse me, what?
"It's your soleus that's the culprit. It's all tied up and stiff." She started digging into it and I felt literal sparks run up my leg as she released adhesions and got the muscle moving a little. When she finally put the leg down, it felt like it was on fire with all the blood rushing into it.
She said, "You'll need to stretch your soleus. It'll clear up, but it'll take a bit of time - tendons take ages to heal."
But I HAVE been stretching.
"No, you haven't. The usual straight-leg calf stretch only stretches the gastrocnemius, that's the big belly muscle in your calf. That's not your problem. That stretch doesn't stretch the soleus. Don't worry, I'll show you how to stretch it."
My mind is spinning.
So here are the muscles in question:
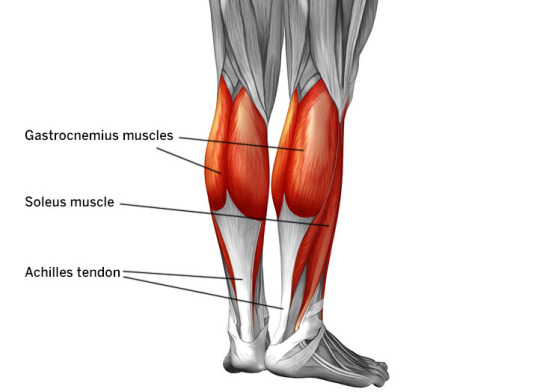
The gastroc (as the pros call it) just attaches down the back but the soleus runs underneath it from the knee around the side to the heel. The lower part above the ankle is where it typically gets tight and forms adhesions.
To stretch it, you do the same calf thing where you put your foot back and press your heel to the ground, but you have to do it with your KNEE BENT:

The bent knee keeps the gastroc from engaging. It's one of those selfish muscles (like traps) - if you give it an inch, it'll just take over and prevent other muscles from working or stretching. There are other ways to stretch the soleus but this is the easiest and you can literally do it anywhere. I've been doing it while standing and waiting for things (the elevator to come, the toast to toast). You just put the heel back and bend the knee. It's kind of like curtseying.
The minute I did this stretch, I could FEEL where it was pulling on my tendon. I knew that THIS had been the problem.
The massage therapist also told me to stop icing my heel. She said icing is for an acute injury, but a more chronic aggravation needs heat, to increase blood flow for healing. She recommended elevation with heat every day (I've been doing it in bed during "phone before bed" time).
I have been doing the soleus stretch at least half a dozen times a day for almost a week, and the ankle is at least 70% better. It is still a little tight and tender, but the improvement is significant. I think a few more weeks will have it feeling normal.
I am...blown away by this. This massage therapist was able to pinpoint an issue in only a few minutes that eluded all the other professionals I saw. I can't wait to go back to her and have her solve all my other problems, tbh.
#massage therapy#soleus muscle#achilles tendon#bodywork#i am so mad i didn't go to her last winter#why did nobody else tell me this#physical therapy
4K notes
·
View notes
Text
So the cortisone shot definitely is helping. I didn't realize the extent to which I was rolling onto the outside edge of my foot to avoid the pain of that bone spur. Now that I'm walking more normally, my calf muscle and achilles tendon are SO MAD. I'm feeling the urge to keep walking wrong because of it! Having a body is such bullshit
5 notes
·
View notes
Text
Whelp I forgot this was even here.
Out of all the things that I have forgotten I forgot that I had this Tumblr XD Brain Fog is a bitch it seems. I guess I could use this as a venting space, what with my shinny Chronic Illness and all. Its still a ongoing brain battle with myself with what I think I can do, and what I should do.
It’s a slow process in getting used to what will mess me up, and what I know will mess me up. Just because I can ignore it doesn’t mean I should. That being said its nice to know that I wasn’t just being a big baby about my chronic pain and that there is actually something wrong.
It’s been a year and a half now and I have to make peace with the mighty Fibromyalgia monster lurking inside my body. I need to stop thinking “Maybe my doctor is wrong and I’m okay,” or “There’s not actually anything wrong with me” because I know there is. Ones body is not actually supposed to be full of pain that has no rhyme or reason after all, and there is only so long someone can ignore the hammering pain that comes out of no where.
Hell I just had a month off of work because they were remolding, all the rest in the world and I’m still bone dead tired, and I wake up with random parts of me burring or twinging. It’s cool that I can still time travel by closing my eyes and falling asleep just about anywhere but my bed. It’s great to randomly feel like I’m going to crash and burn until it comes time for me to actually sleep. I also find it funny that my ankles are still made of garbo, yay for saving up for ankle surgery to get the Right ankle fixed almost as well as the left is now.
To every doctor out there that always told me to either loose weight or to rest and it will get better please kindly go screw you self. To the doctors that told me there was nothing wrong with me or my ankles, you need to listen to your patients and not just assume you know what is going on. I lived with a heel spur growing through my Achilles Tendon , for over eight years before someone listened to me. Do you know what its like to feel like someone is taking a knife to the back of your ankle with every step and that sitting down was the worst part of your day? It’s not fun I can tell you that, and if it would have been looked at sooner, and fixed before it got so bad I wouldn’t have two partial Achilles tears in my medical records and a tendon that is now prone to tearing. But no, because I was over weight, there was nothing wrong with them and I just had pain because I was heavy.
3 notes
·
View notes
Text
I’m constantly tired, angry, and lately in pain.
I found out recently that I have Chronic Achilles Insertional Calcific Tendinopathy (AICT) which is just a very ancy way of saying I’ve had a chronic case of tendinitis for the past ten ish years and the constant strain on the tendon is leading to bone spurs.
Maybe it’s the weather, gloomy at least, some nasty flooding at worse, or maybe it’s because I now have a name for this thing that I’m actually allowing myself to process and acknowledge the pain but it fucking hurts. Sharp mostly, but occasionally a tingly burning.
I work retail.
And I’m so fucking tired guys, so tired, and angry.
Tired because I’m standing all day in pain and angry because all of this plus the precocious puberty. (Yes I’m on this again)
My body is fucking wrecked, and not in the fun way. I have the sort of aches and pains you’d expect from someone in their late 30s at the earliest, mid to late forties more often than not.
The wear and tear is not reversible, the damage is done, all I can do now is manage it and I feel fucking cheated because this was something my doctor was aware of but did nothing about. I was 4’ 6” - 4’ 8” in kindergarten (4yo) the average height of an adult woman (at the time) was 5’ 4” does this not raise concerns? I told this to the orthopedist and she and the medical scribe both had to pause in shock, the scribe actually did a double take to make sure he heard me right.
There was a time where I actually thought I was older than I was being told I was because of my height and size, there was a time where I, barely older than a toddler, was damn near convinced I was being gaslit by everyone around me about my age because of how much bigger I was than my peers.
There is this pit of just, rage and disgust in my stomach and for the life of me I don’t know how to make it go away, I want it to go away. I don’t want to look at my mother and occasionally suddenly feel this wave of resentment that she (inadvertently) let this happen to me, I don’t want to look at myself in the mirror and feel like I’m going to be sick. I want to be able to stand on my own two feet without the worry that the pain will have me in tears.
I’m just so fucking tired, and at this point I’d rather be numb
2 notes
·
View notes
Text
Heel Pain Common Causes and How To Prevent It
Do you feel pain in the movements of your heels or discomfort when you are walking? The possible cause of this might be heel pain, which is a common foot and ankle problem. Heel Pain is a result of any one of the medical conditions that include plantar fasciitis, Achilles tendinitis, or repetitive stress on injuries.
While heel pain does not need any surgery, if ignored and not treated on time, it might develop chronic pain.

Symptoms of Heel Pain
A person might experience heel pain at specific sites or positions of the foot. People usually experience pain at the bottom of the foot or towards the front of the heel.
Some common symptoms of heel pain are as follows:
Acute pain in the heel, usually in the morning or after rest.
Stiffness or tenderness in the heel.
Difficulty walking or putting weight on affected feet.
Different Sites of Heel Pain
You may experience acute or chronic pain in the heel at a particular site. Some points of heel pain are as follows.
Achilles Tendon: Due to repetitive stress, you might feel pain in the tendons on the back of the lower leg. The condition is known as Achilles Tendinitis, which is an injury to the tendons connecting the calf muscles to the heel bone.
Bottom of the heel: This condition is referred to as Plantar fasciitis. When there is excessive pressure on the heel, it damages or tears the tissue, which causes swelling.
Side of the foot: Due to stress fractures, sprain, and TTS, you might suffer from lateral foot pain, which affects the outside of the heel or foot, and medial foot pain damages the inside edge.
Causes of Heel Pain
The severity of the heel pain depends on the location where you are experiencing the pain. Depending on the site and severity of the pain, the bone doctor will provide you with the treatment.
Some causes of the heel pain are as follows:
● Haglund’s Deformity
Prolonged stress and swelling lead to irritation, and it causes an enlarged bony bump to grow at the back of your heel. This condition is known as Haglund’s Deformity. The heel pain worsens when you wear a shoe or any tight footwear.
● Sever’s Disease
The pain that results from the stress or compression on the growth plate of the heel bone. This disease is more prominent in children aged between 8 to 16. Excessive jumping, running, or exercise causes swelling in the growth pain, which leads to heel pain.
● Bursitis
The fluid-filled sacs that cushion the joints for movement are called bursae. A condition when these fluid-filled sacs swell is known as bursitis. This is caused by excessive stress on your heels, and you may feel a bruise-like growth at the back of your heels.
● Achilles Tendinitis
Achilles Tendinitis is more common among athletes, runners, and basketball players. The fibrous tissue that connects the calf muscle to the heel bone is known as Achilles' Tendons. This repetition and overuse causes inflammation, which leads to pain in the heels.
Some other indirect causes that lead to hell pain are as follows.
Heel Spurs
Diabetes
Obesity
Gout
Gait is an abnormal walking style, such as rolling the feet inwards.
How to Prevent Heel Pain
In order to cure your heel pain and minimize the stress and sprain on your heels, you must take specific preventive measures, which are as follows:
Stretching exercises help to maintain flexibility and reduce pressure on the calf muscles and Achilles Tendon.
Wearing supportive footwear with good arch and cushions.
Maintaining a healthy weight reduces the pressure on the heel.
Use medical tape or athletic tape to support your heels.
Using ice packs to heal the inflamed portion.
Avoiding heavy training exercises if you are experiencing pain.
If you are experiencing excessive pain and inflammation, you can take nonsteroidal anti-inflammatory drugs as suggested by an ortho specialist doctor.
If you are experiencing pain or trouble with your ankle, you must seek consultation from orthopedics in Delhi and take the preventive measures suggested by your doctor.
0 notes
Text
The Role of Imaging in Diagnosing Sports Injuries

The clock starts ticking when an athlete gets injured. The sooner a precise diagnosis is made, the faster the road to recovery begins. This is where imaging technology comes in handy to change how sports injuries are treated and diagnosed. For instance, pinpointing torn ligaments or finding minute fractures can be done using advanced imaging technologies like MRI, CT scans, and ultrasounds so athletes can return to the game. In this blog we will look into some of these diagnosing modalities that not only allow doctors to see through but also assist in developing effective treatment plans in order for athletes to recover fast and safely back to their best level.
Sports injuries can be complex, often requiring more than just a physical examination to accurately diagnose and treat. This is where medical imaging plays a crucial role. The best doctors for sports injury in Nairobi use advanced imaging techniques for detailed views of bones, soft tissues, and internal structures. This allows for precise diagnosis and tailored treatment plans.
X-rays: The First Line of Defense
X-rays are often the initial imaging test performed for sports injuries, particularly when a fracture is suspected. They provide clear images of bones and can reveal:
1. Fractures or stress fractures
2. Dislocations
3. Degenerative changes in joints
4. Bone spurs
While X-rays are excellent for bone imaging, they have limitations when it comes to soft tissue injuries. This is where more advanced imaging techniques come into play.
Magnetic Resonance Imaging (MRI): Soft Tissue Specialist
MRI is a powerful tool in sports medicine, offering detailed images of soft tissues without using ionizing radiation. The best orthopaedic surgeons in Nairobi use MRIs for diagnosing:
1. Ligament and tendon injuries (e.g., ACL tears, rotator cuff injuries)
2. Cartilage damage
3. Muscle strains and tears
4. Bone stress injuries before they become visible on X-rays
5. Labral tears in the shoulder or hip
MRI can also detect subtle changes in tissues, making it valuable for identifying overuse injuries and early signs of conditions like osteoarthritis.
Computed Tomography (CT): 3D Bone Imaging
CT scans use X-rays to create detailed, three-dimensional images of bones and joints. They are particularly useful for:
1. Complex fractures
2. Subtle bone injuries not visible on standard X-rays
3. Evaluating healing of fractures
4. Assessing bony alignment in joints
“While less commonly used than MRI for sports injuries, CT scans can be valuable in specific situations, especially when detailed bone imaging is required”, shares Dr Ankit Dave, one of the best doctors for sports injury in Nairobi.
Ultrasound: Real-Time Imaging
Ultrasound has gained popularity in sports medicine due to its ability to provide real-time, dynamic imaging. Dr Ankit Dave, one of the best orthopaedic surgeons in Nairobi, uses it for:
1. Tendon injuries (e.g., Achilles tendonitis, tennis elbow)
2. Muscle strains and tears
3. Joint effusions (fluid in joints)
4. Guiding injections or aspirations
Ultrasound also allows for side-by-side comparison with the uninjured side and can be used to assess tissue healing over time.
Bone Scintigraphy: Detecting Overuse Injuries
While less common, bone scans can be valuable for detecting certain types of injuries, particularly:
1. Stress fractures not yet visible on X-rays
2. Overuse injuries in bones
3. Infections in bones or joints
This technique involves injecting a small amount of radioactive material and then using a special camera to detect areas of increased bone metabolism, which can indicate injury or healing.
Positron Emission Tomography (PET): Metabolic Imaging
PET scans are not routinely used in sports medicine but can be valuable in specific situations, such as:
1. Assessing muscle metabolism
2. Evaluating complex regional pain syndrome
3. Research applications in sports science
Choosing the Right Imaging Modality
The best doctors for sports injury in Nairobi, Dr. Ankit Dave share that the choice of imaging technique depends on various factors, including:
1. The type of injury suspected
2. The body part involved
3. The athlete’s symptoms and physical examination findings
4. The need for detailed soft tissue vs. bone imaging
5. Availability and cost of different imaging modalities
Often, a combination of imaging techniques may be used to get a comprehensive picture of an injury.
Benefits of Advanced Imaging in Sports Medicine
The use of these imaging techniques in sports medicine offers several advantages:
1. Accurate diagnosis: Imaging can confirm or rule out suspected injuries, leading to more precise treatment plans.
2. Early detection: Some injuries can be identified before they become symptomatic, allowing for preventive interventions.
3. Treatment planning: Detailed imaging helps surgeons plan procedures and choose the most appropriate treatment approach.
4. Monitoring healing: Follow-up imaging can track the progress of healing and guide return-to-play decisions.
5. Research applications: Advanced imaging contributes to our understanding of sports injuries and helps develop new treatment strategies.
Conclusion
Imaging plays a vital role in the diagnosis and management of sports injuries, offering the best orthopaedic surgeons in Nairobi a window into the body’s internal structures. From the basic X-ray to advanced techniques like MRI and ultrasound, each imaging modality provides unique insights that guide treatment decisions and help athletes return to play safely.
As technology continues to advance, we can expect even more sophisticated imaging techniques to emerge, further enhancing our ability to diagnose and treat sports injuries with precision. However, it’s important to remember that imaging is just one tool in the sports medicine toolkit. A comprehensive approach that combines clinical assessment, patient history, and appropriate imaging leads to the best outcomes for athletes at all levels.
0 notes
Text
Expert Foot Care in Pembroke Pines: Your Guide to Choosing the Right Foot Doctor
The Importance of Foot Health
Your feet are the foundation of your body, supporting you through daily activities and helping maintain balance and posture. Neglecting foot health can lead to a variety of issues, including pain, discomfort, and mobility problems. Common foot problems such as bunions, heel spurs, and ingrown toenails can significantly impact your daily life if left untreated. A qualified foot doctor, or podiatrist, specializes in diagnosing and treating these conditions, ensuring you stay on your feet and in good health.
Common Foot Conditions Treated by Podiatrists
Foot doctors in Pembroke Pines are trained to handle a wide range of foot and ankle conditions. foot doctor pembroke pines Some of the most common issues they treat include:
Plantar Fasciitis: Inflammation of the plantar fascia, causing heel pain.
Bunions: Bony bumps that form on the joint at the base of the big toe.
Heel Spurs: Calcium deposits that cause a bony protrusion on the underside of the heel bone.
Ingrown Toenails: A condition where the toenail grows into the surrounding skin, causing pain and infection.
Achilles Tendonitis: Inflammation of the Achilles tendon, often due to overuse or injury.
Choosing the Right Foot Doctor in Pembroke Pines
When selecting a foot doctor, it’s crucial to consider several factors to ensure you receive the best possible care:
Qualifications and Experience: Look for a podiatrist who is board-certified and has extensive experience in treating a variety of foot and ankle conditions. Check their credentials and ask about their experience with cases similar to yours.
Reputation and Reviews: Research the podiatrist’s reputation in the community. Read online reviews and ask for recommendations from friends, family, or your primary care physician. Positive reviews and testimonials can provide insight into the quality of care you can expect.
Range of Services: Choose a foot doctor who offers a comprehensive range of services, from diagnostic assessments and conservative treatments to surgical interventions if necessary. A well-rounded podiatrist can address all your foot health needs.
Personalized Care: Opt for a podiatrist who takes the time to understand your specific concerns and develops a personalized treatment plan. toe fungus laser treatment Individualized care ensures that your unique needs are met, and you receive the most effective treatment.
Convenient Location and Office Hours: Select a podiatrist with a conveniently located office and flexible hours that fit your schedule. This makes it easier to attend appointments and stay committed to your treatment plan.

0 notes
Text
Effective Relief from Plantar Fasciitis: Tips and Exercises
Plantar fasciitis is a prevalent condition characterized by inflammation of the plantar fascia, a thick band of tissue that connects the heel bone to the toes. It causes significant heel pain, especially with the first steps in the morning or after prolonged periods of rest. This comprehensive guide explores effective tips and exercises for managing plantar fasciitis, emphasizing practical strategies to alleviate symptoms and promote recovery.
Plantar fasciitis typically develops due to repetitive strain and micro-tears in the plantar fascia, resulting from activities that involve prolonged standing, walking, or running. Biomechanical factors such as high arches, flat feet, or abnormal walking patterns can also contribute to increased stress on the plantar fascia. Moreover, individuals who are overweight or obese, as well as those who wear inadequate footwear, are at higher risk of developing this condition.

Understanding Plantar Fasciitis
Plantar fasciitis is characterized by pain and tenderness along the bottom of the foot, specifically near the heel. The pain is often described as sharp or stabbing, particularly upon taking the first steps in the morning or after prolonged periods of rest. This discomfort gradually decreases with activity but may return after long periods of standing or walking. The underlying cause of plantar fasciitis involves inflammation and degeneration of the plantar fascia, exacerbated by repetitive stress and strain.
Symptoms of Plantar Fasciitis
The primary symptom of plantar fasciitis is heel pain, typically localized near the underside or front of the heel bone. This pain is most severe upon initial weight-bearing activities, such as getting out of bed in the morning or standing up after sitting for an extended period. The pain may diminish as the foot limbers up with activity but often returns after prolonged weight-bearing. In some cases, the pain can radiate along the arch of the foot. Swelling and tenderness along the plantar fascia may also be present, particularly with palpation or pressure.
Diagnosis and Assessment
Diagnosing plantar fasciitis involves a thorough clinical examination and may include imaging studies to rule out other potential causes of heel pain. During the examination, healthcare providers assess the location and severity of pain, examine foot mechanics, and palpate the plantar fascia for tenderness and swelling. X-rays are commonly used to evaluate the structure of the foot and rule out other conditions such as fractures or bone spurs. In some cases, magnetic resonance imaging (MRI) or ultrasound may be recommended to visualize soft tissue structures and confirm the diagnosis.
Tips for Relief from Plantar Fasciitis
Effective management of plantar fasciitis focuses on reducing pain and inflammation while promoting healing of the plantar fascia. Conservative treatment options include:
Rest and Ice: Resting the affected foot and applying ice packs to the heel for 15-20 minutes several times a day can help alleviate pain and reduce inflammation.
Footwear: Choosing supportive shoes with good arch support and cushioning is essential. Avoid flat shoes or those with worn-out soles that provide inadequate support.
Night Splints: Using night splints to keep the foot dorsiflexed overnight can stretch the plantar fascia and Achilles tendon, reducing morning pain.
Orthotic Inserts: Custom orthotic inserts or over-the-counter arch supports can provide additional cushioning and support to the arch of the foot, alleviating strain on the plantar fascia.
Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen may be used to reduce pain and inflammation. Topical treatments, such as menthol creams or gels, can also provide temporary relief.
Weight Management: Maintaining a healthy weight reduces stress on the plantar fascia and can help prevent exacerbation of symptoms.
Strengthening and Stretching Exercises
Incorporating specific exercises into a daily routine can help strengthen the muscles of the foot and calf while improving flexibility of the plantar fascia. These exercises include:
Calf Stretch: Stand facing a wall with one foot forward and the other foot back, keeping both heels flat on the floor. Lean forward, bending the front knee, until you feel a stretch in the calf of the back leg. Hold for 30 seconds and repeat several times on each side.
Plantar Fascia Stretch: Sit with one leg crossed over the other and pull the toes back toward the shin until you feel a stretch along the bottom of the foot and heel. Hold for 30 seconds and repeat several times on each foot.
Towel Curls: Sit in a chair with a towel on the floor in front of you. Use your toes to scrunch up the towel toward you. Repeat several times to strengthen the muscles of the toes and arch.
Toe Raises: Stand barefoot and rise up onto your tiptoes, holding for a few seconds before slowly lowering back down. Repeat 10-15 times to strengthen the muscles of the calves and ankles.
Prevention Strategies
Preventing recurrence of plantar fasciitis involves addressing risk factors and maintaining foot health:
Gradual Activity Progression: Avoid sudden increases in activity level or intensity, particularly high-impact activities like running or jumping.
Proper Footwear: Wear supportive shoes with cushioning and good arch support appropriate for your foot type and activity level. Replace worn-out shoes regularly.
Warm-Up and Cool-Down: Incorporate gentle stretching and warm-up exercises before physical activity to prepare the muscles and plantar fascia for exertion. Afterward, cool down with stretching to promote flexibility and reduce muscle tension.
Cross-Training: Alternate high-impact activities with low-impact exercises such as swimming, cycling, or yoga to reduce repetitive strain on the plantar fascia.
Foot Care: Regularly inspect your feet for signs of irritation, blisters, or changes in skin color or texture. Keep your feet clean and moisturized, and trim toenails straight across to prevent ingrown nails.
Conclusion
In conclusion, effective management of plantar fasciitis involves a combination of pain relief strategies, stretching and strengthening exercises, and preventive measures to alleviate symptoms and promote healing. By understanding the causes and symptoms of plantar fasciitis and incorporating these practical tips and exercises into daily routines, individuals can effectively manage their condition and improve foot health. Consulting with a healthcare provider for personalized treatment recommendations and ongoing management is essential for optimizing outcomes and achieving long-term relief from plantar fasciitis. With proper care and attention, individuals can regain mobility, reduce pain, and maintain an active lifestyle free from the constraints of plantar fasciitis.
0 notes
Text
Growing Older as a Gay Man
June 27th, 2024
Happy Pride on the 27th day of the month. I’m 61 years old, soon to be 62 in December. It’s been on my mind a lot lately about aging, so here we go.
I’m not what I used to be. It’s hard not to judge my body and have body dysmorphia. Combine that with the feeling that I am becoming more and more invisible in my community and add a dash of regret at not having a relationship by now and you get my recipe for disaster… a time for a new outlook… dealing with death…? The questions could go on and on.
What is the best way to deal with a feeling of loss? Is it like losing a partner, a dad, etc.? I look at myself in the mirror and I see some issues on the right side of my body. I have an Achilles Tendon that has healed after being torn in two, but my calf is now smaller than the other. My right heel constantly cracks and needs constant care, along with my Achilles Tendon scar that juts out enough to cause some discomfort. My right foot has had toe nail fungus since my AC was torn - I can’t seem to get rid of it. Finally, my right pectoral muscle has separated from my sternum. It’s an odd injury as most pectoral injuries occur from the shoulder. Just looking at it makes me feel out of kilter. My right shoulder is often sore and feels out of sync with my other one. Granted both collar bones have arthritis spurs that require shots every six months and I’m waiting on surgery. I even had a cyst on my right eyelid that was removed a few weeks ago. A week ago, my right thumb starting clicking - trigger finger. I’ve had it before…
I can’t unsee these things - they are where my eyes go in the rare times that I stand in front of a mirror. Which brings up a few other things - my grey hair, my cheeks aren’t as full as they used to be. This is the time that the body dysmorphia hits me hard. Friends tell me that I am a handsome man and have a great body. Why can’t I always see that? I mean, I don’t think that I am ugly, I just don’t get the handsome part. I’ve kept my body in the best shape that I can - even though my chest isn’t anywhere near what it was - it’s now about 2/5 inches less in size.
This brings up the issue of others seeing it. I hate taking my shirt off in the changeroom at the gym. I worry about potential partners in bed and how they will see my chest - do they think I am a mutant, like I sometimes think I am?
I’ve written about this before in my blog - I even had a guy from Facebook read it and told me that I had no reason to feel what I was feeling. I know he was projecting his own issues onto me, but the last thing that I want is to sound like I am complaining. What I’m really trying to do is to find a solution to the dysmorphia.
There is an operation for my chest, but my doctor has not found someone willing to do it - so far. I know he has even been looking to the USA. My right calf could be a focus in my leg work out. I’d need a Personal Trainer more skilled than I. My toe nails could be removed and allowed to regrow (painful as that sounds) or I continue the nightly regiment of putting a treatment liquid on it. The eyelid cyst is gone and there doesn’t seem be scarring. My right shoulder could use some physiotherapy as well. Botox for my forehead? Forget it! Fillers for my cheeks - Yikes.
One option that I have - mainly around the chest issue is potentially resigning myself to living with it. The other things may or may not change. I am going to write something that I felt when this happened with my chest. I asked myself who would love a man who look like a mutant? I’ve come to realize that I am not a mutant - I’m just a 61 year old gay man who doesn’t fit the norm of the average younger gay man - buff, energetic, good looking and full of vitality. I’m not shallow either to believe that someone would not accept me for my chest injury. If they did, then clearly they are not worth having around.
I see the selfies on Facebook and Instagram of the hot, muscular, sexy guys. Hell, I used to take selfies like that myself. I stopped after my cancer because I did a ton of work on myself and came to realize that I don’t need that external validation. What I do need is self validation - accept myself for who I am at this moment in time and live my life. It makes sense! I’m fairly good at it - I’ve planned my retirement, planned my activities including travel and more. What I have done for the first time in my life is planning travel on my own. Sure, I’m off to Bear Week in Provincetown but I’ll be with my bestie, Seann. I’ll be going to Palm Springs Leather Pride and Gay Pride, but I’ll be with my other bestie, Gary.
What’s different is my potential trip to Costa Rica. I plan on going by myself, except Finn will go with me. I’ll be gone a month. That’s a big step for me - travelling to somewhere I’ve never been… on my own.
I know I’ve shifted topics here, but they are related. I have this thought that I might be single for the rest of my life. On side of me says, oh well! Go live your life. The other side says, you’ve got to try harder to find a man. One side says to hell with all the injuries - they won’t prevent me from travelling. The other side says it may be the reason why I’ll be single because it is not just hard to find someone in the small town where I live. It’s doubly hard for an introvert who is just learning to get out there. Finally, that other side thinks that the injuries will prevent me from finding someone as well.
Writing this out is helping. If there is anyone reading this, please contact me and let me know your thoughts about body dysmorphia. I think that I can accept the fact that I am now a senior. I just got a discount at the local pharmacy- last Thursday of every month is 20% for anyone older than 55! Over all, I have a very positive outlook on who I am and where I am going. This one little piece of the puzzle is something that I need to work on.
For Pride, I am celebrating getting older! There are some really great bonuses to being my age. There are a few not so great - such as forgetting why I went upstairs the other day… I am also celebrating June 27 as the day that there was Royal Assent on a bill here in Canada that decriminalized homosexual acts. It came into force on August 26,1969. By the way, June 27, 1969 was one day before the Stonewall Riots took place in New York. Also, June 27, 2015 was when the U.S. Supreme Court gave same-sex couples the right to marry.
Carpe diem, everyone.
1 note
·
View note
Text
Heel Pain Treatment Chennai — Injury / Ache — Shri Bone & Joint Clinic
Introduction to Heel Pain
Heel pain is a standard foot and ankle problem. It can make it difficult to walk and participate in daily activities. Most painful heel conditions improve with nonsurgical treatments, but your body needs time to recover.
Heel pain can disrupt mobility, work, exercise, and daily activities, potentially leading to a sedentary lifestyle and weight gain. Inactivity may also contribute to feelings of depression due to limitations in engaging in enjoyable activities.
Untreated Achilles tendonitis can progress to tendinosis, causing the Achilles tendon to weaken and potentially tear or rupture over time, possibly necessitating surgery.
Anatomy of the Heel
Calcaneus (Heel Bone)
The calcaneus is the most prominent bone in the foot and forms the foundation of the heel. It provides stability and support to the foot and is essential for weight-bearing activities.
Achilles Tendon
The Achilles tendon is a thick tissue band connecting the calf muscles to the heel bone. It is the largest and strongest tendon in the body and is essential for walking, running, and jumping.
Plantar Fascia
The plantar fascia is a thick band of connective tissue that runs along the bottom of the foot, from the heel to the toes. It supports the foot arch and helps absorb shock during walking and running.
Fat Pad
The heel contains a fat pad that cushions and protects the heel bone. It helps absorb shock and reduces pressure on the heel during weight-bearing activities.
Muscles
Several foot and lower leg muscles attach to the heel bone and help support and move the foot. These include the calf muscles, which are responsible for plantarflexion (pointing the foot downward), and the muscles of the sole, which help control movements such as walking and running.
Common Conditions Causing Heel Pain
Plantar Fascia
Achilles Tendinitis
Heel Spurs
Bursitis
Stress Fractures
Arthritis
Tarsal Tunnel syndrome
Symptoms of Heel Pain
Pain
Tenderness
Swelling
Stiffness
Difficult to walk
Pain with activity
Pain that improves with stress
Heel spurs
Warmth
123456
Diagnostic Procedures
Diagnosing heel pain may include a physical examination, imaging test (X-rays, CT scan, MRI scan or ultrasound), and sometimes blood tests to rule out conditions like arthritis or infections.
Imaging helps identify issues like plantar fascia, heel spurs, fractures or Achilles tendonitis. Treatments depend on the underlying cases.
Treatment Options
Injections
Physical Therapy
Orthotics
Stretching
Night splints
Non-steroidal anti-inflammatory drugs
Proper footwear
Rest
Ice
Steroidal Injections
Surgery
Preventive Measures
Proper footwear
Healthy weight
Stretching
Gradually increase in activity
Foot care
Proper technique
Orthotic devices
Warm-up and cool down
Regular exercise
Listen to your body
Rehabilitation and Recovery
Rehabilitation for heel pain typically involves rest, ice, and gentle stretching exercises.
Strengthening exercises for the foot and ankle may also be beneficial. Orthotic devices and proper footwear can support and reduce heel strain. Physical therapy can help improve flexibility and strength.
Activity modification and pain management techniques are often used.
Recovery time varies depending on the cause and severity of the heel pain, but with proper treatment, most people can expect to recover within a few weeks to a few months.
Why Choose Shri Bone & Joint Clinic for Heel Injury Treatment in Chennai?
Shri Bone & Joint Clinic provides the best heel injury treatment in Chennai. Here, we have the best orthopedic specialists. Our doctors are well-trained and have more than ten years of experience in the Orthopedic field.
Here, we accepted all kinds of emergency walk-ins. Also, patience and friendly manners are equally important to all patients. Compared to other hospitals, the medical charges are affordable and reasonable.
Best Doctor / Specialist for Heel Pain Treatment in Chennai
Dr Shri Krishnamoorthy from Shri Bone & Joint Clinic in Chennai is the best doctor for treating heel pain and other knee-related problemsbest doctor for treating heel pain and other knee-related problems. He is a national board-certified orthopedist. He has ten or more years of experience in this field.
He treats all the patients equally and provides the best treatment for their problems. To get immediate relief for all kinds of knee-related problems, visit us.
0 notes
Text
What Does a Podiatrist Do?
Curious about the role of a podiatrist? “What does a podiatrist do?” is a common question.
Podiatrists are medical specialists who help with problems that affect your feet or lower legs. They can treat injuries as well as complications from ongoing health issues like diabetes. You might hear them called a podiatric physician or doctor of podiatric medicine.
What conditions can podiatrists treat?
Conditions Podiatrists Treat:
Podiatrists treat people of any age for many foot-related conditions, including:
Fractures and sprains:
Podiatrists regularly treat these common injuries when they affect the foot or ankle. They also work in sports medicine, treating foot problems athletes have and recommending ways to avoid them.
Bunions and hammertoes:
These are problems with the bones in your feet. A bunion happens when the joint at the base of your big toe gets bigger or is knocked out of place. That makes the toe bend toward the others. A hammertoe is one that doesn’t turn the right way.
Nail disorders:
These include issues like an infection in your nail caused by a fungus or an ingrown toenail. That’s when a corner or side of a nail grows into your toe instead of straight out.
Diabetes:
This is a condition in which your body either doesn’t make a hormone called insulin or doesn’t use it the way it should. Insulin helps you digest sugar. Diabetes can damage the nerves in your feet or legs, and you might have trouble getting enough blood to your feet. Diabetes can cause serious complications. More than 65,000 people a year need to have their feet amputated by a doctor because of diabetes. A podiatrist can help prevent that. If you have diabetes, make sure to get any sores or calluses on your feet checked out.
Arthritis:
This results from inflammation, swelling, and wear and tear on your joints. Each foot has 33 joints. A podiatrist might recommend physical therapy, drugs, or special shoes or inserts to help with your arthritis. Surgery might also be an option if other treatments don’t work well for you.
Growing pains:
If your child’s feet turn inward or appear flat, or if their toes don’t align properly, a podiatrist could provide helpful solutions. This might involve recommending exercises, insoles, or braces. In some cases, they might even suggest surgery as an option.
Heel pain:
Heel pain often results from heel spurs due to excess calcium buildup. Activities like running, ill-fitting shoes, or excess weight trigger them. Plantar fasciitis is inflammation along the foot’s underside, often tied to sports and improper footwear. Overpronation, or excessive bending in walking, affects athletes. Achilles tendinitis, causing pain where the tendon attaches, is also common. Initial solutions involve pain relief, orthotic inserts, and surgery for severe cases.
Morton’s neuroma:
Nerve issues between the third and fourth bones of your foot can bring about pain, a burning sensation, and even the feeling that something is inside your shoe. This is particularly common among runners and tends to worsen with tight shoes and overpronation. For relief, a podiatrist can offer anti-inflammatory shots, help you discover the right orthotic, and, in more severe cases, suggest surgical removal if needed.
Reasons to See a Podiatrist
Your feet do a lot of work. By the time you’re 50, you’ll have walked 75,000 miles on them. Feet are complex structures with many bones, tendons, and ligaments that have to work together perfectly to keep you moving.
When should a client see a podiatrist?
Individuals with healthy feet should still visit a podiatrist once every year. The doctor can identify potential issues and recommend steps you can take to avoid problems and maintain healthy feet. Patients who have specific foot or ankle conditions, such as a history of foot ulcers, should see a podiatrist more often.
Do podiatrists cut toenails?
Your podiatrist can safely cut your nails and remove fungus without spreading it. They can also prescribe antifungal creams and sprays to help the nail heal.
How does a podiatrist diagnose?
These specialized doctors play a pivotal role by skillfully determining the optimal approach for addressing and recuperating from various lower extremity medical conditions and injuries. This involves conducting X-rays and lab tests, proficiently performing surgeries, prescribing necessary medications and orthotic devices, and engaging in a host of other essential activities.
Why do older people need a podiatrist?
Seniors are often unaware of the injuries they may sustain on their feet. Upon closer inspection of the feet and ankles, a local podiatrist can properly inspect the feet for cuts, bruises, swelling, or any other injuries that may otherwise go unseen.
Benefits of Podiatry Service:
Podiatrists Are Experts in Foot and Ankle Care
Enjoy Healthy Feet and Ankles
Relieve Foot Pain
Support Your Feet with the Right Footwear
FREQUENTLY ASKED QUESTIONS
FAQ About Podiatrist
ARE PODIATRISTS AND CHIROPODISTS THE SAME?
What is the difference between a chiropodist and a podiatrist?
There is no difference between a chiropodist and a podiatrist. The terms are simply different names for the same profession. The word "podiatrist" is more commonly used in the United States. At the same time, "chiropodist" is more widely used in the United Kingdom and other parts of the world.
In some countries, such as Australia, the term "chiropodist" is no longer used. All podiatrists in Australia are now referred to as podiatrists.
Is a podiatrist a doctor?
Yes, a podiatrist is a doctor. Podiatrists are medical professionals who specialize in diagnosing and treating foot and ankle disorders. They have completed accredited podiatry training and are licensed to practice in their respective countries.
Like those who have received a Doctor of Medicine academic degree (MD), podiatrists have a four-year doctorate in podiatric medicine (DPM). They also complete a three- to four-year residency in podiatry. They train in various clinical settings during residency, including hospitals, clinics, and private practices.
Podiatrists can perform various procedures, including surgery, injections, and casting. They can also prescribe medications and order physical therapy.
Podiatrists are essential members of the healthcare team. They are vital in preventing, diagnosing, and treating foot and ankle problems.
Do you need a referral to see a podiatrist?
You do not need a referral to see a podiatrist. Podiatrists are primary healthcare providers, so you can make an appointment directly.
However, your family physician may refer you to a podiatrist if you have a complex foot or ankle problem that requires specialized care.
For example, your doctor may refer you to a podiatrist if you have diabetes and are at risk of developing foot complications.
Suppose you are still determining whether you need a referral to a podiatrist. In that case, you can always ask your family doctor or the podiatrist's office.
Here are some of the benefits of seeing a podiatrist without a referral:
● You can get an appointment sooner.
● You can save time and money by avoiding seeing your doctor first.
● You can choose the podiatrist who is right for you.
Can a podiatrist remove calluses?
Yes, a podiatrist can remove calluses. Podiatrists have the training and experience to safely and effectively remove calluses.
There are a few different ways that a podiatrist can remove a callus. The most common method is using a sterile scalpel to shave the thickened dead skin away. The podiatrist may also use a callus shaver, a sandpaper-like tool, or a pumice stone to remove the callus.
If the callus is deep or painful, the podiatrist may inject a local anesthetic to numb the area before removing the callus. Once the callus has been removed, the podiatrist will apply a bandage or dressing to the site.
Here are some of the benefits of having a podiatrist remove your calluses:
● It is safe and effective.
● It is quick and painless.
● It can help to prevent calluses from coming back.
● It can help to improve the appearance of your feet.
Can podiatrists give cortisone shots?
Yes, podiatrists can give cortisone shots. Cortisone shots are injections of a corticosteroid medication, such as cortisone or prednisone. Corticosteroids are powerful anti-inflammatory drugs that can help to reduce pain and swelling.
Podiatrists may give cortisone shots to treat a variety of foot and ankle conditions, including:
● Arthritis
● Bunions
● Bursitis
● Carpal tunnel syndrome
● Gout
● Heel spurs
● Plantar fasciitis
● Tendinitis
Cortisone shots are usually very effective at reducing pain and inflammation. However, they do not cure any of the conditions listed above. The effects of a cortisone shot typically last for several weeks to months.
Suppose you are considering getting a cortisone shot. In that case, talking to your podiatrist about the risks and benefits is essential. Cortisone shots can have some side effects, such as:
● Pain and swelling at the injection site
● Skin discoloration
● Increased blood sugar levels
● Weakening of the bones
● Increased risk of infection
Suppose you have any underlying medical conditions, such as diabetes or high blood pressure. In that case, it is essential to let your podiatrist know before getting a cortisone shot.
Suppose you are considering getting a cortisone shot for your foot or ankle pain. In that case, I encourage you to talk to your podiatrist.
Can a podiatrist write a prescription?
Can a podiatrist write a prescription?
Yes, a podiatrist can write a prescription. Podiatrists are qualified healthcare professionals with the same ability as other physicians to write drug prescriptions. They can write prescriptions for medications to address a range of issues in the foot and ankle, such as:
● Swelling and discomfort
● Infection
● foot issues brought on by diabetes
● ailments of the skin
● Infections with fungi
● disease of the nails
For long-term ailments like gout and arthritis, podiatrists can also write prescriptions for medicines.
A podiatrist will consider the patient's needs and medical background when prescribing a prescription. They will also take into account any additional drugs the patient is taking.
Does a podiatrist deal with toenails?
Yes, Toenails are treated by a podiatrist. Podiatrists are medical specialists who identify and treat conditions affecting the feet and ankles, including nails on the toes.
Podiatrists can treat a variety of toenail conditions, including:
Ingrown toenails: An ingrown toenail is one in which the nail’s edge grows into the skin. Pain, swelling, and redness may result from this.
Fungal nails: A fungus that affects the toenails causes fungal nails. The nail may develop thick, discolored, and brittle layers. To treat fungal nails, podiatrists might recommend antifungal medicines.
Thickened toenails: Several things, such as injury, infection, and other medical disorders, can result in thickened toenails. Podiatrists can thin the nail and offer advice to stop it from becoming thicker in the future.
Brittle nails: Brittle nails are simple to snap. Aging, dry skin and certain medical disorders are just a few of the things that might contribute to this. To help strengthen brittle toenails, podiatrists might provide advice.
Additionally, podiatrists can trim toenails and offer guidance on correct toenail care.
How much does a podiatrist cost?
We, HolisticHealing4Life, offer podiatrist treatment. Our Subsequent Podiatry visit costs $60+ tax, and our Initial Podiatry Visit costs 80.00 + tax.
You can visit the “Orthotics & Foot Care” section for details.
1 note
·
View note
Text
A Comprehensive Guide Understanding and Heel Pain Treating
A Comprehensive Guide Understanding and Heel Pain Treating is a common complaint that can range from mildly irritating to severely debilitating. It can occur for a variety of reasons, from overuse and improper footwear to underlying medical conditions. Understanding the causes and treatment options for heel pain can help individuals find relief and prevent future issues.
Causes of Heel Pain
Plantar Fasciitis: This is the most common cause of heel pain. It occurs when the plantar fascia, the band of tissue that connects the heel bone to the toes, becomes inflamed or irritated.
Achilles Tendinitis: This condition involves inflammation of the Achilles tendon, which runs down the back of the lower leg and attaches to the heel bone. It is often caused by overuse or improper footwear.
Heel Spurs: These are bony growths that develop on the underside of the heel bone. They are often associated with plantar fasciitis but can also occur on their own.
Stress Fractures: Tiny cracks in the heel bone can cause significant pain, especially with weight-bearing activities.
Bursitis: Inflammation of the bursa, a fluid-filled sac that cushions the heel, can cause pain and swelling.
Arthritis: Various forms of arthritis, including rheumatoid arthritis and osteoarthritis, can affect the joints in the heel and cause pain.
Treatment Options
Rest: Resting the affected foot can help reduce inflammation and allow the tissues to heal. Avoiding activities that worsen the pain, such as running or standing for long periods, is recommended.
Ice Therapy: Applying ice to the heel for 15-20 minutes several times a day can help reduce pain and inflammation.
Stretching Exercises: Gentle stretching exercises for the calf muscles and plantar fascia can help improve flexibility and reduce pain.
Orthotic Inserts: Custom orthotic inserts can provide support and cushioning to the heel, reducing pressure on the affected area.
Proper Footwear: Wearing supportive shoes with good arch support and cushioning can help alleviate heel pain.
Physical Therapy: A physical therapist can provide specific exercises and treatments to help alleviate heel pain and prevent recurrence.
Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help reduce pain and inflammation.
Surgery: In severe cases, surgery may be necessary to relieve pressure on the heel or repair damaged tissues.
Prevention Tips
Maintain a healthy weight to reduce pressure on the heels.
Wear supportive shoes that fit properly and provide adequate cushioning.
Gradually increase the intensity of physical activities to avoid overuse injuries.
Stretch and strengthen the calf muscles and plantar fascia regularly.
Listen to your body and seek medical attention if you experience persistent heel pain.
Heel pain can significantly impact daily activities, but with proper treatment and preventive measures, it can be effectively managed. If you are experiencing heel pain, consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
0 notes
Text
This Update is a Bit Behind
_This Update is a Bit Behind_ Why I've been non-present for the past couple months. #writing #reading #mentalhealth
So, I am dealing with increasing levels of pain due to my body hating me. That is, I have arthritis and other problems going on with my knees, lower back, and most recently, my goddamn Achilles tendons. (Bone spurs. I think, but can’t confirm that the bone spur situation is related to the feeling that my Achilles has been beaten with a baseball bat.)
It should be noted that at least a few of…
View On WordPress
0 notes
Photo

Hello Semihamoo Peninsula 👋 Suffering from foot pain? 🦶 👨⚕️ Have you been diagnosed with Plantar Fasciitis, Achilles are Plantar Tendonitis, Bone Spurs, Calf or Heel Pain, Numbness in the toes or Arthritis of the ankle or feet? Then you might want to take advantage of our “Arch Madness” Foot Pain Relief Exam offer for Only $97. ✅ Foot Health History ✅ Exam ✅ Foot Scan ✅ 1st treatment session That’s a savings of $65 to $75. 👏 Covered by most extended healthcare plans. Why wait any longer? 📱 Call today 604-535-7373 or learn more online at https://bit.ly/42JsfYS
0 notes