#high creatinine levels
Text
Comprehending Chronic Kidney Disease (CKD)
The kidneys are vital organs for filtering waste and excess fluids from the blood. Kidney problems, whether acute kidney injury (AKI) or chronic kidney disease (CKD), can lead to a range of health issues, including swelling due to kidney failure. While conventional treatments are commonly prescribed, more individuals are exploring alternative approaches to kidney health, including homeopathy kidney treatment.
Understanding Kidney Function and Kidney Conditions
Before discussing homeopathic remedies, it is essential to understand the role of the kidneys and the distinction between acute and chronic kidney conditions.
Kidney Function:
The kidneys perform several crucial functions in the body, including the filtration of waste products, maintenance of fluid balance, regulation of electrolytes, and secretion of hormones that control blood pressure. When the kidneys are impaired, these functions can be compromised, leading to a buildup of waste in the body and other health complications.
Acute Kidney Injury (AKI):
AKI is a sudden loss of kidney function that typically occurs as a result of an injury, infection, or certain medications. It is characterized by a rapid decline in kidney function, leading to an accumulation of waste products in the bloodstream. Acute kidney injury
requires immediate medical attention and can sometimes be reversible with timely intervention.
Chronic Kidney Disease (CKD):
CKD, on the other hand, is a long-term condition where the kidneys gradually lose their ability to function over time. It progresses through stages, and in advanced cases, it can lead to kidney failure, also known as end-stage renal disease (ESRD). Chronic kidney disease
often requires lifelong management and may ultimately necessitate dialysis or kidney transplantation.
Swelling Due to Kidney Failure
One common and distressing symptom of kidney failure is swelling, medically referred to as edema. Edema occurs when excess fluid accumulates in the body, leading to swelling in various areas, including the hands, legs, face, and abdomen. This swelling due to kidney failure can be uncomfortable and impact a person's quality of life. Homeopathic remedies may offer a gentle approach to alleviate edema associated with kidney failure.
Homeopathy for Kidney Health
Homeopathy is a holistic system of medicine that focuses on treating the individual and addressing the underlying causes of health issues. Homeopathic medicine for kidney disease are made from highly diluted natural substances and aim to stimulate the body's innate healing abilities.
When it comes to kidney health, homeopathy can offer several potential benefits:-
Symptom Management:
Homeopathic remedies can help manage the symptoms associated with kidney conditions, including high creatinine levels, swelling, high blood pressure, and urinary issues. By addressing these symptoms, individuals may experience improved comfort and well-being.
Individualized Treatment:
Homeopathic treatment is highly individualized, with remedies chosen based on the specific symptoms, constitution, and emotional state of the patient. This personalized approach takes into account the unique aspects of each person's condition.
Minimal Side Effects:
Homeopathic remedies are highly diluted and generally well-tolerated, making them a gentle and safe option for individuals with kidney conditions. They can be used alongside conventional treatments if necessary.
Homeopathic Remedies for Kidney Conditions
Several homeopathic remedies may be recommended for individuals dealing with kidney issues, including those with swelling due to kidney failure. These remedies are chosen based on the patient's specific symptoms like creatinine and constitution.
It's important to consult a qualified homeopathic practitioner to assess your specific condition and prescribe the most suitable remedy.
Conclusion
Homeopathy offers a natural and holistic approach to managing kidney conditions, including acute kidney injury, chronic kidney disease, and the associated swelling due to kidney failure. While it may not replace conventional medical kidney treatments in all cases, it can be a valuable complementary therapy or an alternative for those seeking a gentler and less invasive approach to kidney care. If you or a loved one are dealing with kidney-related issues, consider consulting a qualified homeopath to explore the potential benefits of kidney treatment by homeopathy in your journey to better kidney health. Effective treatment requires individualized assessment and guidance from a healthcare professional experienced in homeopathy.
If you want to know for kidney treatment homeopathy, then you can visit my original blog. The link has been provided below:
https://bharathomeopathy.com/disease/kidney-failure-treatment
#chronic kidney disease (CKD)#Low creatinine#High creatinine levels#normal creatinine levels#creatinine levels#Kidney treatment by homeopathy#Kidney treatment
0 notes
Text

Lexington Renal Care
Provides comprehensive care for patients who are facing kidney disease, kidney transplant hospital in Lexington, KY transplants, dialysis, and hypertension.
Our patients are our highest priority. We understand that each
the patient is unique and individual needs will be considered when deciding on treatment options.
#Nephrolithiasis Pain Diagnosis Medicine#kidney problems detected blood test in lexington#Kidney Disease & Diagnosis in Lexington#Chronic Kidney Disease Tests in Lexington#Tests to Measure Kidney Function near me#kidney stones treatment Lexington care#Physicians for renal calculi Ttreatment in Lexington#Treatment for renal stone disease#Proteinuria Causes#Symptoms#Tests & Treatment in Lexington#High creatinine levels test in Lexington#kidney transplant hospital in Lexington#KY
0 notes
Text
#Kidney#creatinine#serum creatinine#normal creatinine levels#high creatinine level#what is creatinine?#creatinine means
0 notes
Text
here's a perfect example of how medical misogyny kills women
for anyone who can't watch the video, he's basically saying that high levels of creatinine can indicate kidney problems, which is why it's key feature for determining who needs a liver transplant first. the issue with this is that it doesn't account for creatinine-to-muscle ratios, meaning that men typically have artificially higher numbers because they typically have more muscle mass. while women's numbers may look low, they're actually high in relation to their muscle mass. basically, the system was designed based on male bodies
940 notes
·
View notes
Text
The kontext situation hits especially hard because the circumstances of his death so closely mirror my dad's. A few months ago, I was in New York, telling my friend Reese Piper about my dad's refusal to look after his health -- and how it killed him. It killed him the same way his own father's refusal to quit smoking killed him, and the way his grandpa's failure to reduce his alcoholism killed him.
And then a little later into the night, I shared with Reese my (at the time) steadfast denial that my high red blood cell count, high hemotocrit, high hemoglobin, and high creatinine were at all a problem, and my outrage that a doctor had told me I'd need to donate blood to deal with it.
And an awful little cheshire cat smile spread across Reese's face and she observed I was behaving just like any other man in my family.
All those same levels are high in my blood again. Again I am going to donate blood, not begrudgingly this time, but thankfully. I am more aware now what a gift that it is to have a medical condition that can be explained and easily treated. I even feel lucky that the treatment itself is a benefit to others. How convenient to have a problem that can be fixed for free and meets others' needs in the process. There is no need to run away from having a body with ailments and needs. Jesus, ignoring reality could kill me, like it killed kontext and my dad. And my grandpa. and great grandpa. And my mom's best friend. I am breaking the cycle.
102 notes
·
View notes
Text
Published Dec 8, 2020
Quick description of condition:
Thrombotic Microangiopathy (often known simply as TMA) is a rare but serious medical disease. It is a pattern of damage that can occur in the smallest blood vessels inside many of your body’s vital organs – most commonly the kidney and brain. “Microangiopathy” literally translates to “small blood vessel problem.” “Thrombotic” means that blood clots are involved.
This small study showed 89% of it's participants had developed TMA.
Our leaders had information as early as 2020 that opening schools without precautions would harm children
Abstract
Most children with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection have mild or minimal disease, with a small proportion developing severe disease or multisystem inflammatory syndrome in children (MIS-C). Complement-mediated thrombotic microangiopathy (TMA) has been associated with SARS-CoV-2 infection in adults but has not been studied in the pediatric population. We hypothesized that complement activation plays an important role in SARS-CoV-2 infection in children and sought to understand if TMA was present in these patients. We enrolled 50 hospitalized pediatric patients with acute SARS-CoV-2 infection (n = 21, minimal coronavirus disease 2019 [COVID-19]; n = 11, severe COVID-19) or MIS-C (n = 18). As a biomarker of complement activation and TMA, soluble C5b9 (sC5b9, normal 247 ng/mL) was measured in plasma, and elevations were found in patients with minimal disease (median, 392 ng/mL; interquartile range [IQR], 244-622 ng/mL), severe disease (median, 646 ng/mL; IQR, 203-728 ng/mL), and MIS-C (median, 630 ng/mL; IQR, 359-932 ng/mL) compared with 26 healthy control subjects (median, 57 ng/mL; IQR, 9-163 ng/mL; P < .001). Higher sC5b9 levels were associated with higher serum creatinine (P = .01) but not age. Of the 19 patients for whom complete clinical criteria were available, 17 (89%) met criteria for TMA. A high proportion of tested children with SARS-CoV-2 infection had evidence of complement activation and met clinical and diagnostic criteria for TMA. Future studies are needed to determine if hospitalized children with SARS-CoV-2 should be screened for TMA, if TMA-directed management is helpful, and if there are any short- or long-term clinical consequences of complement activation and endothelial damage in children with COVID-19 or MIS-C.
#covid in children#mask up#covid#covid 19#covid isn't over#pandemic#covid conscious#long covid#covid is airborne#wear a mask#coronavirus
5 notes
·
View notes
Note
Ask for kidney function tests. Even if they did them. This sounds like my mom's end stage kidney disease & eventual cancer. *hugs* ♡
They keep repeating them and the only things coming up high are my MCH & MCHC levels (which are related to haemoglobin but I'm not anaemic (yet) as in my folate and b12 are fine) so I'm so confused myself haha.
My urea is verging on low and creatinine verging on high but nothing outside the "normal" limits (yet).
I'm so tired of arguing with them 😔 you guys advocate for me more than any doctor has! ♥️ I'll make sure they repeat everything soon tho x
12 notes
·
View notes
Text
i haven’t posted here in a while, mostly due to life taking up my time. i just wanted to get off my chest that harley has been getting way worse very abruptly recently, so we took him to the vet today and his kidney values are like. Insanely high. the creatinine levels were the highest the vet had ever seen. he’s lost a ton of weight the last month or so, despite being on an appetite stimulant. there’s not much they can do, and what they can do would be extremely taxing for him, may not even work, and would possibly give him a few more weeks at best. so the right thing to do is to let him pass while he’s still himself, still eating and drinking and purring and curling up in our laps even though he must feel tremendously bad. it’s extremely difficult and ive been crying all day and it just. sucks. ive known him since he was 6 days old and could fit in the palm of my hand. he’s been with me through several moves back and forth across the country and through some really shit times in my life and several relationships and just been such a constant for the last near-decade. ive been steeling myself for the grief ever since he got the diagnosis but it doesn’t help. i don’t know what else to say.
#animal death#<- since i know some people have that blacklisted#his last day will probably be monday. im so sad i want to throw up
7 notes
·
View notes
Text
Nothing in my day-to-day job shows me the limits of modern medicine like vancomycin does. And it makes me insane.
(extremely long, somewhat incoherent nerd rant below the cut)
See, vanc is really good at, like, three things: treating MRSA (when given IV), treating ampicillin-resistant enterococcus (when given IV), and treating c diff (when administered orally ONLY). Most every use outside of that, like when it’s used to treat methicillin-susceptible staph aureus for “penicillin allergic patients” (don’t get me started on PCN allergies), actually has data that it increases risk of morbidity and mortality (i.e. harm and DEATH).
Unfortunately, due to the prevalence of multi-drug resistant organisms, vancomycin is empiric therapy for a lot of presumed infections. And it's a lot more difficult to actually tell if someone has an infection than you'd think. A lot of medical conditions imitate each other and when time is of the essence to identify what's going on, the most ethical thing is to start an antibiotic and rule out infection as the hospitalization continues. Lab techniques have gotten a lot quicker: I can remember 8 years ago, it would take 3 days just to identify what microbe the patient had in their presumed infection. These days, anno domini 2023, PCR comes back in a matter of hours, identifying gram positive/gram negative staph/strep/bacilli/etc, and it's the sensitivities that take 2-3 days. (Don't get me started on contaminated cultures.) But even with improvements in lab technique, we might not culture any microbe at all or the provider might keep vancomycin on "just in case" because we don't know IF the patient is infected, WHAT they're infected with, or if the infection will get better with a different drug.
And vancomycin is terrible on kidneys. Extremely nephrotoxic. It isn’t as bad as the 80s when the drug first came out and was called Mississippi Mud colloquially, but it will fuck the patient up if not monitored closely.
But finding the correct dose for each patient in a timely manner is nigh impossible. This is because vancomycin is renally eliminated. We have to mathematically estimate how well the kidneys are working. Unfortunately, our mathematic equation is next to useless if you are:
-Less than 50 kg
-Shorter than 5 foot tall
-Have a BMI of more than 40
-Are an adult younger than 45 (twenty-year-olds get astronomical doses that would be destructive in an older patient)
-Are older than 65 (the official definition of 'geriatric', i'm relatively sure)
-Are female (this is really only applicable if the patient is less than 50 kg or older than 65 - think: little old frail lady - we have absolutely no fucking idea how their kidneys are doing until we order the serum drug level. It is next to impossible to accurately dose vancomycin in little old ladies on the first try.)
-Are missing limbs (lots of leg amputations in the older and impoverished diabetic population!!)
-Have a lot of muscle mass (think bodybuilder or really tall guys)
Fun fact: we estimate renal function by looking at height, weight, age, birth gender (few, if any, studies on trans patients taking HRT), and a lab value called serum creatinine. Creatinine is a byproduct of muscle metabolism, I don't know the fine details, but we can generally estimate how well kidneys are working by seeing how much creatinine is in the blood: low creatinine usually means kidneys are excreting it as they 'should' be. High creatinine means there's something wrong, the kidneys aren't able to excrete it as efficiently as they 'should' be. But the effect of low muscle mass and high muscle mass haven't been studied enough to be able to adjust our mathematical equation to compensate for them. And with high BMI: we often overestimate their renal function because we don't know how to estimate their muscle mass vs their body fat.
(I work out in the boonies. ~70% of our patients have diabetes. ~80% of our patients have a BMI of greater than 35. So what I'm trying to say here is: we are shooting in the fucking dark when we're estimating the renal function of the vast majority of our patients.)
Complicating this: vancomycin is useless until it reaches steady-state concentration in therapeutic range. On one side of this problem: a lot, if not most, medical providers assume that vancomycin starts working its magic from the first dose. So we sometimes get orders for "vancomycin 1 gram now and see how the patient is doing in the morning". That isn't going to solve jack shit! That's just going to increase the incidence of microbial resistance!!
OR, like in the multiple situations I dealt with this afternoon, you make an educated guess on what regimen is going to work for the patient. You get a level 48 hours after the dose starts. And you find out that you fucking guessed wrong and the patient is subtherapeutic. It has been two fucking days and the patient hasn't started being treated for their (presumed) infection yet!! And we've increased the possibility of microbial resistance! *muffled screaming in frustration*
So what I'm trying to say here is: on almost every presumed infection that comes into the hospital (which we're guessing like 30%? 50%? of the time), we're starting an extremely toxic drug, oftentimes 100% guessing what regimen will be therapeutic, only finding out in 2 days that it is not therapeutic, and it can sometimes take days and days to titrate the dose sufficiently to find a therapeutic regimen. And sometimes we're really fucking unlucky and we destroy the patient's kidneys temporarily (or permanently! but kidneys can be very resilient so that's thankfully rare) because we guessed a regimen that's too high!! This is a fucking nightmare!!!!!!!!
And if all of this wasn't bad enough, we don't really have any drugs that do what vancomycin does therapeutically. We have things that can be used to cover some of what vancomycin does, but nothing that's equivalent AND less toxic.
Like, to fix this situation, we need:
-Better education to providers on what drugs are appropriate empiric therapy for different presumed infections (we're working on it, we are working on it)
-Better ways to estimate kidney function (there needs to be more research on kidney function in patients with BMI greater than 35!! And little old ladies!! And patients with low body weight and high body weight and amputations and...)
-Better prognostic tools to tell 1. when the patient is infected (looking at you, sepsis!!!) 2. what they're infected with
-Less-toxic antibiotics AND/OR better ways to treat infection (this would be the evolution of medicine as we know it)
And I want to be clear: vancomycin isn't bad. It's an extremely effective tool when used correctly but we often either don't have enough data to use it correctly or the provider doesn't understand that this tool is fucking useless for the job they're trying to perform.
#some days i'm just smacked in the face by the limits of modern medicine#there is so much we don't know!!!#we're doing the best we can!!!#negativity#personal#us healthcare#i understand other hospitals will have a different experience than this#but my corporation is extremely stingy and we get all the new grads#so educating providers and nurses is a never-ending wheel at my facility#and we don't treat anything complicated except orthopedic surgeries#some days I just get overwhelmed by how little we know#if you can guess my profession on the first try please keep it to yourself i'm trying to maintain a low profile here okay#also if you ask me medical questions don't expect an answer#i was a Cs Get Degrees student all I know i've learned on the job and I don't know shit
6 notes
·
View notes
Text
I'm on OB rotation again. I asked the attending what are things the PCP should know about prenatal and postpartum pts. Stuff we discussed:
SSRIs can be continued during pregnancy. I often see patients on Zoloft during pregnancy if they need an antidepressant. In fact, I just started a prenatal patient on Zoloft the other day in clinic. It is safe to continue SSRIs during pregnancy because you should treat the patient's depression. Babies can come out sort of jittery because of the SSRI, but that goes away.
Postpartum patients will have bleeding somewhat similar to a menstrual period right after giving birth. It starts to decrease and becomes like a brownish color and can last up to 6 weeks postpartum. Any bleeding beyond that point is abnormal.
There is some evidence that if you have estrogen-containing birth control, it can decrease milk supply. Actually, I had a patient in clinic recently who was seen by an attending and he started her on a progesterone only birth control so that it would not affect her milk supply. Estrogen decreases the patient's milk supply, so patients who plan to breast-feed should not be started on estrogen-containing birth control. Right after giving birth, your body has increased amounts of estrogen, so you would not start estrogen containing birth control until at least 6 weeks postpartum anyway. Increasing estrogen immediately postpartum increases risk of blood clots. For patients who plan to breastfeed and want to be on an oral contraceptive, use progesterone only oral contraceptives until she stops breastfeeding.
If the mother is breastfeeding at least every 4 hours, then this can be used for contraception. It's about 80% effective. Once baby starts sleeping through the night or once baby starts feeding more than every 4 hours, this method won't work! If you go more than 4 hours without breastfeeding, breastfeeding will not protect you from pregnancy! You can also ovulate before your menstrual period returns, so you can't say you can't get pregnant because your period has not returned yet!
I asked the attending I worked with today about how she goes about prescribing birth control. She said she will usually start with Sprintec. It's usually covered by insurance and if it's not covered, it's pretty affordable. She also said Junel is pretty well tolerated. Certain progestins in certain brands of birth control may work better for certain things like acne control, but she didn't have as much knowledge on that. I'll ask another attending again about that. I usually start people on Sprintec as well.
PCP should know that alkaline phosphatase is high in pregnant patients. It comes from the placenta. So don't be freaked out by that.
You should know HTN in pregnancy and preeclampsia workup. High BP is 140/90. Severely high BP is 160/110. Swelling occurs in many pregnant pts, but that should also alert you to start preeclampsia workup.
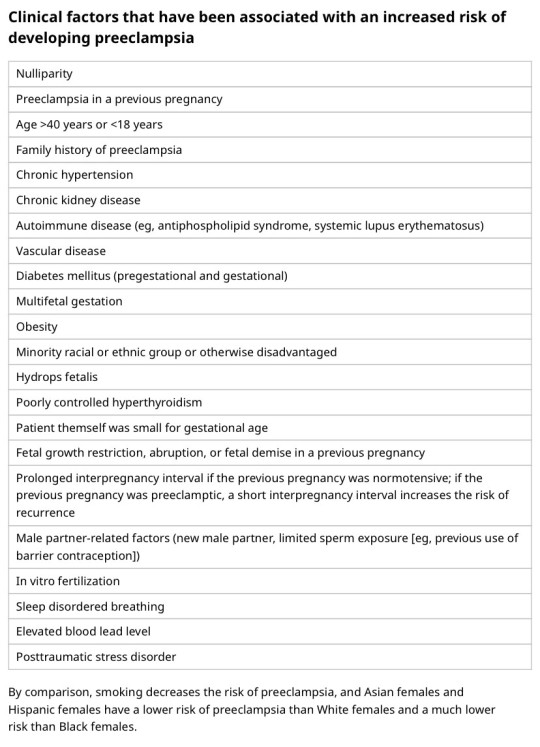
[Preeclampsia w/u from UpToDate:
Diagnostic evaluation
•Laboratory – Patients with suspected preeclampsia should have a complete blood count with platelets, creatinine level, liver chemistries, and determination of urinary protein excretion.
•Fetal status – Fetal status is assessed concurrently or postdiagnosis, depending on the degree of concern during maternal evaluation. At a minimum, a nonstress test or biophysical profile is performed if appropriate for gestational age. Ultrasound is used to evaluate amniotic fluid volume and estimate fetal weight, given the increased risk for oligohydramnios and growth restriction.
•Consultation with the neurology service is generally indicated in patients with neurologic deficits/abnormal neurologic examination, which may include ocular symptoms or a severe persistent headache that does not respond to initial routine management of preeclampsia.]
An important thing to review is physiology of pregnancy. Blood volume increases during pregnancy, so there are lots of new RBCs and that will throw off a HgbA1c reading, therefore HgbA1c is not measured during pregnancy and will not be accurate! My attending today told me there was a midwife who offered pts either HgbA1c or oral glucose tolerance tests to screen for gestational DM. The HgbA1c is not accurate in pregnancy, so this should not be done. That would be bad to miss a diagnosis of gestational diabetes. You have to wait until 3 months postpartum to measure HgbA1c to get an accurate reading. Had a pt who did not have a PCP prior to getting pregnant, was on insulin during the pregnancy, and after giving birth, still needs to establish with PCP for diabetes f/u. After you give birth, you insulin needs drastically change, so you don't need as much as you did when you were pregnant. So I stopped her insulin and advised that she f/u with her new PCP for diabetes care.
I still need to review fetal heart tracings. The attending today said the first thing to look at is the baseline (the baseline HR should be about 160 beats/min), then the variability, then look for accelerations and decelerations. If more than 32 weeks GA, accelerations are 15 beats/min above the baseline lasting at least 15 seconds. Early decelerations are representative of compression of the fetal head, which is normal during labor as baby moves down the pelvis/birth canal. Variable decelerations look sharper like a "V" and can represent compression of the umbilical cord. Late decelerations represent placental insufficiency.
ACOG has very helpful practice bulletins.
I can't take screen shots on my work laptop, so I'm just going to summarize gestational HTN w/u from UpToDate:
Gestational HTN: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions 4 hours apart after 20 weeks of gestation in a previously normotensive individual
And:
No proteinuria
No signs/symptoms of preeclampsia-related end-organ dysfunction (eg, thrombocytopenia, renal insufficiency, elevated liver transaminases, pulmonary edema, cerebral or visual symptoms)
Preeclampsia: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions at least 4 hours apart after 20 weeks of gestation in a previously normotensive individual. Patients with systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg should have blood pressure confirmed within a short interval (minutes) to facilitate timely administration of antihypertensive therapy.
And:
Proteinuria (≥300 mg per 24-hour urine collection [or this amount extrapolated from a timed collection], or protein:creatinine ratio ≥0.3, or urine dipstick reading ≥2+ [if other quantitative methods are not available]).
In a patient with new-onset hypertension without proteinuria, the diagnosis of preeclampsia can still be made if any features of severe disease are present.
Preeclampsia with severe features: In a patient with preeclampsia, presence of any of the following findings are features of severe disease:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg on 2 occasions at least 4 hours apart (unless antihypertensive therapy is initiated before this time)
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
Progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL [97 micromol/L] or doubling of the serum creatinine concentration in the absence of other renal disease)
Pulmonary edema
Persistent cerebral or visual disturbances
Eclampsia: A generalized seizure in a pt with preeclampsia that cannot be attributed to other causes.
HELLP syndrome: hemolysis, elevated liver enzymes, low platelets. Hypertension may be present (HELLP in such cases is often considered a variant of preeclampsia).
Chronic (pre-existing) hypertension: hypertension diagnosed or present before pregnancy or on at least 2 occasions before 20 weeks of gestation. Hypertension that is first diagnosed during pregnancy and persists for at least 12 weeks postpartum is also consider chronic hypertension.
Blood pressure criteria during pregnancy are:
Systolic ≥140 mmHg and/or diastolic ≥90 mmHg
Prepregnancy and 12 weeks postpartum blood pressure criteria are:
Stage 1 – Systolic 130 to 139 mmHg or diastolic 80 to 89 mmHg
Stage 2 – Systolic ≥140 mmHg or diastolic ≥90 mmHg
Chronic HTN with superimposed preeclampsia*:
Any of these findings in a patient with chronic hypertension:
A sudden increase in blood pressure that was previously well-controlled or an escalation of antihypertensive therapy to control blood pressure
New onset of proteinuria or a sudden increase in proteinuria in a patient with known proteinuria before or early in pregnancy
Significant new end-organ dysfunction consistent with preeclampsia after 20 weeks of gestation or postpartum
*Precise diagnosis is often challenging. High clinical suspicion is warranted given the increase in maternal and fetal-neonatal risks associated with superimposed preeclampsia.
Chronic hypertension with superimposed preeclampsia with severe features:
Any of these findings in a patient with chronic hypertension and superimposed preeclampsia:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg despite escalation of antihypertensive therapy
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
New-onset or worsening renal insufficiency
Pulmonary edema
Persistent cerebral or visual disturbances
A reduction in blood pressure early in pregnancy is a normal physiologic occurrence. For this reason, women with chronic hypertension may be normotensive at their first few prenatal visits. Later in pregnancy, when their blood pressure returns to its prepregnancy baseline, they may appear to be developing preeclampsia or gestational hypertension if there are no documented prepregnancy blood pressure measurements.
BP: blood pressure.
* Blood pressure should be elevated on at least two occasions at least four hours apart. However, if systolic pressure is ≥160 mmHg or diastolic pressure is ≥110 mmHg, confirmation after a short interval, even within a few minutes, is acceptable to facilitate timely initiation of antihypertensive therapy.
¶ The onset of preeclampsia and gestational hypertension is almost always after 20 weeks of gestation. Preeclampsia before 20 weeks of gestation may be associated with a complete or partial molar pregnancy or fetal hydrops. Postpartum preeclampsia usually presents within two days of delivery. The term "delayed postpartum preeclampsia" is used for signs and symptoms of the disease leading to readmission more than two days but less than six weeks after delivery.
Δ Significant proteinuria is defined as ≥0.3 g in a 24-hour urine specimen or protein/creatinine ratio ≥0.3 (mg/mg) (34 mg/mmol) in a random urine specimen or dipstick ≥1+ if a quantitative measurement is unavailable.
◊ Almost all women with the new onset of hypertension and proteinuria at this gestational age or postpartum have preeclampsia, but a rare patient may have occult renal disease exacerbated by the physiologic changes of pregnancy. An active urine sediment (red and white cells and/or cellular casts) is consistent with a proliferative glomerular disorder but not a feature of preeclampsia. Women with chronic hypertension who had proteinuria prior to or in early pregnancy may develop superimposed preeclampsia. This can be difficult to diagnose definitively, but should be suspected when blood pressure increases significantly (especially acutely) in the last half of pregnancy/postpartum or signs/symptoms associated with the severe end of the disease spectrum develop.
§ Photopsia (flashes of light), scotomata (dark areas or gaps in the visual field), blurred vision, or temporary blindness (rare); severe headache (ie, incapacitating, "the worst headache I've ever had") or headache that persists and progresses despite analgesic therapy; altered mental status. Seizure occurrence upgrades the diagnosis to eclampsia.¥ The differential diagnosis of preeclampsia with severe features includes but is not limited to:
Antiphospholipid syndrome
Acute fatty liver of pregnancy
Thrombotic thrombocytopenic purpura (TTP)
Hemolytic uremic syndrome (HUS)
The laboratory findings in these disorders overlap with those in preeclampsia with severe features. (Refer to table in the UpToDate topic on the clinical manifestations and diagnosis of preeclampsia.) The prepregnancy history, magnitude and spectrum of laboratory abnormalities, and additional presence of signs and symptoms not typically associated with preeclampsia help in making the correct diagnosis, which is not always possible during pregnancy.
In addition, a variety of medical disorders may be associated with hypertension and one or more of the signs and symptoms that occur in women with preeclampsia with severe features. These patients can usually be distinguished from patients with preeclampsia by taking a detailed history, performing a thorough physical examination, and obtaining relevant laboratory studies.‡ In contrast to preeclampsia, gestational hypertension is not associated with end-organ involvement, so neither proteinuria nor the symptoms or laboratory findings of preeclampsia are present.
#OB#OBGYN#birth control#gestational HTN#preeclampsia#eclampsia#breastfeeding#gestational diabetes#fetal heart tracing#FHT
2 notes
·
View notes
Text
Lupus?
I have a lot of symptoms which match with lupus. I've had lots of infections this year...8 so far.
I found out yesterday that my mum had a positive ANA (anti-nuclear antibodies) blood test in the 1990s and again in early 2000s. Docs haven't really followed up on this though.
So today I've got put on my big girl pants and sent a message to my GP surgery with all of my symptoms and some pics of rashes and white fingers. I've done this in hope that I am not blown off and told I'm just stressed or anxious.
Like I am anxious about my health because I feel like shit and I've had 8 infections this year. EIGHT!
So I think my anxiety is founded and proportional to the issue.
If they don't offer me an ANA I'm going to pay for one next year. To rule out autoimmune issues if nothing else.
I just can't deal with more medical gaslighting. After being told last time I raised this it was all because I was stressed.
If anyone's interested here are my symptoms:
* Hair loss
* Fatigue (debilitating)
* headaches and migraines
* Joint pain and stiffness and inflammation
* hearing loss
* dry gritty, itchy eyes (in the middle) which water at the edges.
* rash on checks and nose and sometimes chin
* skin which goes red, then pink and then loses pigment although. Leaving white patches.
* Serum creatinine levels at the highest reference point or just over. Have been for over a year.
* stage two liver disease
* cardiomyopathy
* digestive problems
* three recent UTIs
* One recent skin infection
* three recent respiratory infections
* one recent ear infection
* one abnormal ESR recently
* one high CRP recently
* feeling generally unwell often
* apparent but as yet undiagnosed Raynauds.
#medical gaslighting#actually autistic#mental health#plural system#living with cptsd#chronic fаtiguе ѕуndrоmе#functional neurological disorder#autoimmune#systemic lupus erythematosus#lupus symptoms
4 notes
·
View notes
Text
Comprehending Chronic Kidney Disease (CKD): Indications, Signs, and Treatment
A Holistic Approach to Kidney Treatment: Exploring Homeopathy for Kidney Health
Kidney-related diseases, such as chronic kidney injuries (AKI) along with chronic kidney disease (CKD) are becoming more prevalent in the world. The kidneys play a crucial part in maintaining overall health by filtering out waste substances and excessive fluids out of the blood. If kidney function is impaired in any way, the accumulation of waste substances can cause serious health problems.
Understanding Creatinine Levels
First, let's understand what is creatinine? Creatinine is an unneeded waste product that is produced during the metabolism of muscles and is eliminated by kidneys. Monitoring the creatinine levels in the blood is a commonly used test to determine kidney function. The Normal creatinine levels remain within a particular range that can vary little from one lab to another, but usually is in the range of 0.6 to 1.2 milligrams per deciliter (mg/dL) for men of adult age as well as 0.5 up to 1.1 mg/dL for women of adult age. Abbreviations from these ranges could indicate kidney problems.
Low Creatinine Levels
Lower levels of creatinine are less frequent, but they can be a sign of certain health issues. Conditions like muscle atrophy, malnutrition or underlying illnesses that affect the mass of muscles can cause decreased levels of creatinine. In certain instances it could be the result of a decrease in creatinine production because of liver diseases that are severe. In general, Low creatinine are not the primary issue for treatment of kidneys, however it is important to monitor them because they may be connected with other health problems.
High Creatinine Levels
However high creatinine levels are an obvious sign of kidney failure. If the kidneys aren't efficiently removing waste from the blood, the creatinine levels increase and causes elevated levels in blood. Creatinine levels that are high could be the result of a myriad of factors like dehydration kidney infections obstructions in the urinary tract, or injuries caused by conditions such as AKI or CKD.
Acute Kidney Injury (AKI)
An Acute Kidney Injury, also called acute renal failure is a sudden and pronounced impairment of the kidney's function. It is usually the result of an event that is traumatic such as a serious injury, infection or reaction to a medication. AKI is defined by a rapid rise in creatinine levels. This may cause a variety of symptoms, including reduced urine output, decreased electrolyte and fluid retention imbalances. It is essential to seek immediate medical attention in the event that AKI is suspected because immediate intervention could help to avoid further damage to the kidneys.
Chronic Kidney Disease (CKD)
However, Chronic Kidney Disease is an ongoing condition that progresses in time and is usually marked by the gradual loss of kidney function. CKD is commonly called an "silent disease" because symptoms are not evident until the disease is in advanced levels. Creatinine levels increase gradually in CKD and early detection via regular blood tests is vital for a successful treatment. Lifestyle changes, diet modifications and medical treatments are often utilized to slow the progression of CKD and treat the symptoms.
If you want to know for kidney treatment homeopathy, then you can visit my original blog. The link has been provided below:
https://bharathomeopathy.com/disease/kidney-failure-treatment
#Kidney treatment by homeopathy#Kidney treatment#creatinine levels#chronic kidney disease (CKD)#Low creatinine#High creatinine levels#normal creatinine levels
0 notes
Text
(I use he/they/it pronouns and am intersex. I am not a woman)
Sorry I keep posting angrily about disability but like. My best friend (she/they) fell down the stairs at her apartment complex. They can't afford to go to a doctor and the last time they did go they were told nothing is wrong. She fell down the stairs because their knee locked up and gave out. She's covered in bruises now and can't work. I'm so frustrated with the medical system here. She is disabled but has been refused treatment for years because she's only in her twenties, they're too young to be disabled. Fucking bullshit.
They see anyone young and tell us we're fine as long as the labs look mostly okay. I say mostly okay because my creatinine levels are fucked up every time I go in but they continue to ignore that and the pain I've been experiencing even tho I continue to tell them I need help. All they care is that I'm not diabetic. I'm fat so that's all that matters, I'm not diabetic yet which is good. But hey my fucking creatinine levels have been high for literal months can someone maybe give a shit?
I first started having physical issues when I was still a kid, roughly 11 or 12. They attributed it to puberty for years. I have multiple conditions that affect me. Yes, one is PCOS and started showing symptoms at puberty. But they refused to treat me for the pain and menstrual issues until I was 18 fucking years old. But how is the literal brain damage I have caused by puberty? The deformity in my legs that -they knew about prior to my puberty-? The stricture in my throat? None of it is puberty's fault, but I'm AFAB and I'm fat so it must be my period and it must be my weight and it must be anxiety.
This is all just anger. I'm sorry. I'm just so fucking angry anymore.
#important#fatphobia#ableism#vent#this is just me being pissed at doctors#identity tag#cripple shit#cripple punk
4 notes
·
View notes
Text
Does Metformin, a glucose-lowering drug, hurt the kidneys?
Metformin is a biguanide compound that reduces blood sugar mainly by reducing hepatic glucose output, improving insulin resistance, and reducing glucose absorption in the small intestine. It is currently one of the world's most widely used oral hypoglycemic drugs. Drug safety evaluation studies have found that Metformin has a good safety profile, no carcinogenic or mutagenic effects, and no evidence that Metformin can increase the risk of lactic acidosis. Medicilon has a professional team and experience in preclinical drug safety evaluation services, providing high-quality data and a fast turnaround time to support all drug safety evaluation studies.
Many patients are concerned about the effects of long-term metformin use on the kidneys. The drug does not directly damage the kidneys but can lead to drug accumulation when taken by patients with existing kidney damage. Both the Chinese Guidelines for the Prevention and Treatment of Type 2 Diabetes (2017 edition) and the Expert Consensus on the Clinical Application of Metformin (2016 edition) suggest that Metformin is the drug of choice for the treatment of type 2 diabetes in the absence of contraindications and intolerance, and should always be retained in the glucose-lowering regimen.
1, Benefits of Metformin.
Metformin can reduce hyperglycemia with no hypoglycemic effect on those with regular blood sugar; the drug has the following benefits in addition to hypoglycemia.
(1), Metformin has the effect of reducing body weight.
(2) Metformin has apparent cardioprotective effects and reduces the risk of cardiovascular disease in newly diagnosed and established type 2, diabetes patients.
(3) Metformin can improve lipid synthesis, metabolism, and lipid profile.
(4) Metformin significantly improved liver serological enzyme profile and metabolic abnormalities in patients with non-alcoholic fatty liver.
2, Adverse reactions and countermeasures
The main adverse reactions of Metformin are diarrhea, nausea, vomiting, gastric distension, and other gastrointestinal responses, which mainly occur in the early stage of treatment (the majority happen in the first ten weeks). Most patients can gradually tolerate them, or their symptoms disappear as the duration of treatment increases. Start taking small doses, gradually increase the amount, adjust the quantity at the right time, take with meals, and choose enteric preparations and other methods, which can reduce gastrointestinal reactions.
Three 、Does Metformin hurt the liver and kidney?
Metformin has no hepatic and renal toxicity; Metformin is absorbed through the gastrointestinal tract for blood circulation, almost does not combine with plasma albumin, does not go through liver metabolism, does not compete with liver P450 enzymes, and does not degrade in the body, but acts directly on the liver and muscle, reducing hepatic glucose isomerism and increasing muscle glucose enzymes. Therefore, Metformin is not hepatotoxic.
Metformin is mainly excreted from the urine in its original form by the kidneys and is cleared rapidly, with approximately 90% clearance in 12-24h. The renal clearance of Metformin is about 3.5 times higher than that of creatinine, and renal tubular excretion is the main route of metformin clearance. Therefore, Metformin itself is not harmful to the kidney.
However, caution should be exercised when using Metformin in people with impaired liver and kidney function. Metformin should be avoided when serum transaminases exceed three times the upper limit of normal, and patients with renal insufficiency need to adjust the dose by estimating the level of glomerular filtration rate. Clinicians or pharmacists can assess the above.
4, long-term use of Metformin, the need for appropriate supplementation of vitamin B12
Studies have shown that: the incidence of vitamin B12 deficiency in glucose patients using Metformin is 5.8%, while the incidence of vitamin B12 deficiency in glucose patients not using Metformin and people without diabetes is 2.4% and 3.3%, respectively. Therefore, long-term metformin users should monitor vitamin B12 concentration regularly and increase the intake of vitamin B12-rich foods appropriately (vitamin B12 is mainly contained in animal proteins, such as meat, animal liver, fish, shellfish, eggs, etc.) to prevent and correct vitamin B12 deficiency. If this condition occurs, vitamin B12 should be supplemented in an appropriate amount under the guidance of professional doctors.
Five 、Stop taking Metformin 48 hours before and after doing a CT examination
Diabetic patients should stop taking Metformin 48 hours before and after doing enhanced CT because it is necessary to play contrast agent before doing CT. The contrast agent belongs to macromolecular substances excreted through the kidneys. If you retake Metformin, it will increase the burden on the kidney and cause contrast nephropathy.
6, the icing on the cake: combined with other glucose-lowering drugs
There are several different drugs when taking glucose-lowering drugs, often more than Metformin. This is because the combination of glucose-lowering medications mutually increases the hypoglycemic effect, improves insulin resistance, or reduces adverse reactions.
All diabetic patients should choose the appropriate hypoglycemic drugs according to their different conditions and pay attention to the indications and contraindications of each type of drug. At the same time, it is essential to emphasize that diet therapy and diet control are the cure for diabetic patients and must be adhered to for life. Diet therapy should not be relaxed or abandoned because of oral hypoglycemic drugs or increased dosages of hypoglycemic medications.
3 notes
·
View notes
Text
bluuuugh dad has to go back to the hospital so they can run more tests
his creatinine levels are higher than they should be, not as high as they were back in the winter when this all first started, but still higher than they should be
#doc said he goes in tomorrow#which is infinitely better than last time when it was 'you need to go RIGHT THE FUCK NOW'
4 notes
·
View notes
Text
lupine publishers|Modulating Serum Lipids with Berberine in Naturopathic Clinical Practice
Modulating Serum Lipids with Berberine in Naturopathic Clinical Practice
Abstract
Medical intervention to reduce the risk of atherosclerosis using lipid modulating medications has been a target for reducing cardiovascular risk for over 40 years. Lipid lowering medications, HMG-CoA reductase inhibitors (Statin’s), and more recently PCSK9 inhibitors (PCSK9i (protein convertase subtilisin/kexin type 9 inhibitors) are now and in the future will be the main stay therapy for reducing Atherosclerosis. However, the uncertainty of statin induced myalgia and other bad publicity via the media and internet reports has caused many patients to opt out of statin therapy. Berberine and is quinoline alkaloid has had several clinical trials demonstrating potential in managing cardiovascular disease risk. Berberine is a safe and natural alternative for modulating circulating lipids including LDL-C, however possible drug interactions, due to its effects on P450 enzymes, does indicate some caution should be exercised.
Introduction
Dyslipidemia and cardiovascular disease have been identified by the World Health Organisation as the number one cause of death globally, and high levels of LDL cholesterol [1] are a major risk factor contributing to this. Numerous studies have identified cardiovascular medications as the best way to achieve this goal. A meta-analysis by Baigent etal in 2010 reviewed 26 cholesterol clinical trials which included 170,000 participants1. Their results showed a relative risk reduction in total mortality of 10% per 1 mmol/L reduction in LDL-C with a P value< 0.0011. In their review a significant reduction in deaths from coronary disease and a further reduction in major vascular events which equated to a 22% reduction per 1 mmol/L of circulating LDL-C. Current clinical data supports [2] the belief that LDL-C is the real target for reducing CVD risk [2]. Another cross-sectional CVD study in the Netherlands, involving 1249 patients with heterozygous familial hypercholesterolemia (heFH), only 21 % of patients achieved an LDL-C target of 2.5 mmol/L considered to be a safe target level for these patients3. A similar failure is found in severe primary hypercholesterolemia patients, including those with familial hypercholesterolemia. Familial [3] hypercholesterolemia (FH) is an autosomal dominant disorder involving mutations in the LDL receptor gene leading to defective plasma LDL-C catabolism and increased levels of circulating LDL-C 4,5.
Berberine In Cardiovascular Therapy
Myalgia still remains the most common adverse [4] event reported with statin therapy. Statin -myositis is associated with muscle symptoms and a in severe cases a substantially elevated serum creatinine kinase (CK). In rare circumstances statinassociated myopathy is found to occur at a 1 in 1000 to 1 in 10,000 people on statin treatment 6. In contrast, statin-associated muscle symptoms (SAMS) in which CK concentrations are normal or only slightly elevated, are [5] much more common and have prevalence of 7–29 %6. The most promising natural product that results in cholesterol lowering, based on recent clinical trials, is Berberine, and is quinoline alkaloid, commonly found in several medicinal herbs including Copts sentences, Hydrates canadensis and Rhododendrons amongst others 7. Most recently Berberine has been shown to be a natural inhibitor of PCSK9 (protein convertase subtilisin/kexin type 9), acting in a similar fashion as other PCSK9 Inhibitors Eg Vedolizumab, a monoclonal antibody targeting PCSK9 in hyperlipidaemia which often lowers LDL below 1.5mmol/L8. Interestingly, Berberine has also [6] been demonstrated to lower fasting triglyceride (TG) levels and in a clinical trial, reduced body weight as well as improve dyslipidemia in high fat diet-fed (HFD) rats. Hence, the understanding the cardiovascular protective effects of Berberine appears to be mounting [8]. In several recent clinical trials Berberine has shown significant reductions in LDL-C. One study found total cholesterol to drop from 5.4mmol/l to 4.6mmol/L after 18 weeks with the LDL-C concentration dropping from 3.5 mmol/L to 2.7mmol/L 9. Also, a systematic review, in 2013 examining [7] Berberine supplementation, evaluated eleven randomized controlled trials (including a total of 874 participants) the review identified a significant reduction in total cholesterol, triglycerides and LDL-C except for HDL-C which was increased across the 11 trials with an average LDL-C reduction of 0.65mmol/ L10.
An important consideration when using Berberine is its drug interactions. A study examining the effect of longterm administration of 900mg a [8,9] day of Berberine identified significantly decreased CYP2D6 activity with mild modification of CYP2C9 and CYP3A4 activities, but no effect on CYP1A2 and CYP2C19 function11. The CYP2D6 enzyme metabolizes a quarter of all prescribed drugs. It is recognised that 5-10% Individuals homozygous for two inactive copies of CYP2D6 are known as poor metabolisers resulting in higher plasma concentrations of the substrate drugs when compared to the wild type CYP2D6 alleles. Individuals heterozygous for one inactive allele of CYP2D6 are known as [10] intermediate metabolisers, and homozygous individuals with active copies of active CYP2D6 alleles are known as ultrarapid metabolisers. Thus, in any population a number of individuals given prescribed Berberine doses of 1500mg/day will possibly have drug interactions with their other prescribed medications if they are modified by CYP2D6. My data with [11] Berberine administered to eight (8) adult individuals for 12 weeks at 500mg of Berberine three times a day, showed an avrage reduction in LDL-C of 0.65mmol/L (reported in Table 1. Seven out of the eight (8) individuals had varying reductions of LDL-C over 12 weeks. One patient who had no reduction in LDL-C had an adverse reaction with the Berberine. He exhibited [12] total inhibition of his Hydroxyurea being administered for controlled Essential Thrombocythemia. There had been no reported adverse effects reported for Hydroxyurea and CYP2D6. This observation requires further investigation. Vacuumed is a human monoclonal antibody that inhibits PCSK9 binding to the LDL-C receptor on the hepatocytes and disrupts LDL-C / PCRK9 receptor complex increasing [13] LDL-C receptor recycling to the surface of the hepatocyte and its removal of LDL-C.
Table 1: Case reports for an uncontrolled group of volunteers four (4) females and four (4) males, aged 50 to 70 years, given 500mg of Berberine, 3 times a day with meals for 12 weeks. The average reduction with LDL-C was 0.65mmol/L. This reduction was in line with the metaanalysis completed in 2013[10]. Case 9 is a patient given biweekly injections of 140 mg/mL of evolocumab, for 12 weeks
Another important [14] consideration with Berberine is that it is poorly absorbed into circulation with most of an oral Berberine dose accumulating in the gut. Its absorption depends on the conversion of Berberine to dihydroberberine which requires the enzyme nitro reductase for this to occur12. Hence, an important factor in Berberine absorption is the intestinal microbiota, the metabolite dihydroberberine has been shown to have a 5-10-fold higher absorption rate than Berberine. In the absence of Nitro reductase producing bacteria this conversion does not occur. Enterococcus faecium [15] and Bacteroides fragilis have both been shown to produce nitro reductase enzymes and in culture have been shown to convert Berberine to dihydroberberine. Animal data supports dehydroarene possesses a stronger lipid-lowering effect, indicating that the gastrointestinal tract is a potential target for increasing the hypolipidemic effect of Berberine12. Both Berberine and dihydroberberine have recently shown to have antiinflammatory effects modulated by NF-κB and MAPK signaling pathways [13] and this effect adds to their use in cardiovascular disease.
Conclusion
Berberine is a useful for lowering LDL-C, but the degree is variable. The effectiveness of the biological effect is linked to the gut biome and the presence of nitro reductase enzyme producing bacteria. The probable adverse reaction with other prescription medicines via P450 enzymes especially CYP2D6 may limit its use in many circumstances and the observed inhibition of Hydroxyurea by Berberine needs to be confirmed.
The PURE study showed that socioeconomic factors play an important role in CVD and stroke14. So, lifestyle change with better dietary choices and frequent exercise, should be part of our recommendations for reducing CVD risk. There is enough evidence to recommend combinations of complementary medicines like Bergamot, Berberine, phytosterols, Niacin and fibre add additional approaches to lifestyle change to improve lipid profiles and deliver more available and appropriate CVD risk reduction measures. It is important to remember that changes in circulating lipids do take time and it would be unrealistic to expect significant change in LDL-C and its atherogenic subfractions with Berberine in less than 6 months of intervention [15].
For more information about Open Access Journal of Complementary & Alternative Medicine archive page click on below link
https://lupinepublishers.com/complementary-alternative-medicine-journal/archive.php
For more information about lupine publishers page click on below link
https://lupinepublishers.com/index.php
#lupine publishers#lupine publishers group#lupine publishers LLC#open access journal of complementary & alternative medicine
3 notes
·
View notes