#total parenteral nutrition
Text
My J tube clogged today. This is the second time it has happened. I’ve had my GJ tube for a little less than 4 months and I’m already having problems with it.
That isn’t even going into the frustration that I’m still underweight and malnourished since my body isn’t tolerating feeds well. I don’t know what to do anymore.
A part of me wonders if I should try to bring up the topic of TPN again. My nutritionist says it’s dangerous for the kidneys and liver, but is it a bigger risk compared to me starving to death? Thoughts?
#feeding tube#feedingtube#gjtube#GJ Tube#pegj tube#TPN#Total Parenteral Nutrition#gi disorder#chronically ill#chronic illness#actually disabled#malnutrition#starvation#underweight
2 notes
·
View notes
Text
Parenteral Nutrition Market is Anticipated to Witness High Growth Owing to Rising Prevalence of malnutrition

Parenteral nutrition, also known as intravenous feeding, is a life-saving process that delivers nutrients such as vitamins, minerals, carbohydrates, fats and amino acids directly into the bloodstream. It is primarily used for patients who cannot be fed enterally (through the gastrointestinal tract) due to diseases like inflammatory bowel disease, short bowel syndrome or cancer. The global parenteral nutrition market is primarily driven by the rising cases of malnutrition across the world. Malnutrition afflicts one in three people globally and negatively impacts health outcomes and productivity. Moreover, growing prevalence of chronic diseases such as cancer that often impair normal eating and nutrient absorption further propel the demand for parenteral nutrition.
The global parenteral nutrition market was valued US$ 4,548.7 Mn in 2023 and is expected to reach US$ 7,251 Mn by 2031 growing at a compound annual growth rate (CAGR) of 6% from 2024 to 2031.
Key Takeaways
Key players operating in the Parenteral Nutrition are AbbVie Inc., Danone, Fresenius Kabi AG, GENTAG, Inc., GSK plc., Nestlé SA, Nutricia, Sun Pharmaceutical Industries Ltd, Pfizer Inc., Sanofi, Otsuka Holdings Co., Ltd., and Otsuka Holdings Co., Ltd. These players are focusing on new product launches and geographical expansion to gain more market share.
The key opportunities in the market include growing demand from developing countries due to rising chronic disease burden and increasing focus on home parenteral nutrition to reduce healthcare costs. The home parenteral nutrition segment is estimated to witness fastest growth during the forecast period on account of advanced formulas being less susceptible to contamination and longer shelf life.
The Parenteral Nutrition Market Size exhibits high potential in the Asia Pacific region owing to significant patient pool, improving healthcare infrastructure and increasing healthcare spending in developing countries such as India and China. Many global players are expanding their operations in these countries to tap unmet needs and gain first-mover advantage.
Market drivers- Rising prevalence of malnutrition across the world due to various socio-economic factors is a key driver. Moreover, growing geriatric population prone to chronic conditions increases the potential patient base.
Market restrains- Inconsistent reimbursement policies and high costs associated with parenteral nutrition continue to limit widespread adoption, especially in developing regions. Moreover, risks of infection and catheter-related complications with long-term use of parenteral nutrition poses restraints.
Segment Analysis
This Parenteral Nutrition Companies can be segmented by nutrient type, end user and geography. Based on nutrient type, the carbohydrate segment is dominating as it provides energy to the body and accounts for around 30% of total calories. Carbohydrates are an important macronutrient that can help improve clinical outcomes in patients receiving parenteral nutrition.
Based on end user, hospitals segment dominates the market as hospitals are the main clinical setting where parenteral nutrition is administered. Many serious medical conditions and surgeries require a patient to receive total nutrient support intravenously in a hospital setting.
Global Analysis
Regionally, North America dominates the parenteral nutrition market with the highest market share. Factors such as the increasing prevalence of chronic diseases requiring nutrient support in the US and Canada are driving market growth. However, Asia Pacific is expected to grow the fastest between 2024-2031. Rapidly developing healthcare infrastructure and rising medical tourism in India and China are creating increased demand for parenteral nutrition in Asia. Overall, developing regional markets will drive future market growth as healthcare access improves globally.
Get more insights on Parenteral Nutrition Market
Vaagisha brings over three years of expertise as a content editor in the market research domain. Originally a creative writer, she discovered her passion for editing, combining her flair for writing with a meticulous eye for detail. Her ability to craft and refine compelling content makes her an invaluable asset in delivering polished and engaging write-ups.
(LinkedIn: https://www.linkedin.com/in/vaagisha-singh-8080b91)
#Coherent Market Insights#Parenteral Nutrition Market#Parenteral Nutrition#Intravenous Nutrition#IV Nutrition#Total Parenteral Nutrition#TPN#Clinical Nutrition#Nutritional Support#Artificial Nutrition#Intravenous Feeding
0 notes
Text
STATE OF SHOCK AND INJURY: A release of the catecholamine epinephrine suppresses response to insulin.
Basal metabolic rate increases 7% for every degree rise in fever.
OBESITY: Obesity starts at a BMI of 30kg/m^2 (3 classes of obesity. BMI of 40kg/m^2 or > is Class III obesity). There are 3,500 calories per pound of body fat, so start with a deficit of 500cal/day for weight loss of 1 pound per week.
Initial rapid weight loss is water weight, due to glycogen stores pulled out from the liver (for every gram of carbohydrate stored, 3g of H2O are stored w/it)
You cannot spot lose fat. Plateau (can't continue to lose weight) occurs because BMR has dropped in order to match loss of weight.
DEFICIENCIES: stomatitis due to riboflavin (B2) deficiency
PREGNANCY: Pregnancy-induced hypertension begins at 20th week. But sodium restriction NOT recommended as the intervention.
TUBE FEEDS: Deadly to feed into an ileus. Elemental formulas = more expensive.
4-hour hang time for open systems (concern for pathogenic activity/growth). 24-48 hours for closed systems.
Nasogastric tube for short-term enteral access (for those with NORMAL GI function who require nutrition support for 3-4 weeks). Bolus, intermittent, or continuous infusions.
Naso-duodenal OR naso-jejunal feeds for those unable to tolerate gastric tube feed (recall it is best to do gastric if possible to mimic body's natural eating functions).
Give 1cc of H2O per calorie ingested. Formulas that are 1 calorie per cc are 80-86% water.
Peripheral parenteral nutrition (AKA total parenteral nutrition/TPN -- LAST resort due to the fact that it is like foie gras to the body, with implications of liver issues developing) is via small surface veins, which is short-term nutrition support. Includes protein and fat (a 10% solution of intravenous fat provides 1.1 calories per cc. A 20% solution provides 2.0 calories per cc. Think about propofol, delivered in a fat medium).
Solutions have dextrose, which provides 3.4 cal/g.
# of calories from a volume of dextrose = mL provided × % dextrose × 3.4
PPN/TPN is used to achieve anabolism when patients cannot eat by mouth and you cannot do an enteral tube feed.
Long-term central access occurs via cephalic, subclavian, or internal jugular vein and feed ls into superior vena cava.
PPN/TPN concerns: Bacterial translocation because you are bypassing the gut, which would normally kill bacteria that is ingested per os. Bacteria can travel through bloodstream and lead to SEPSIS.
In TPN, protein is provided for anabolism at 1g of nitrogen for every 150 calories ingested. The percent concentration tells you # of grams of protein per in 100mL of TPN solution (a 3% solution provides 3g of protein in 100mL of TPN solution).
Glucose infusion rate for dextrose in TPN should not exceed 4-5mg/kg/min for hyperglycemia prevention.
Fat is added to prevent essential fatty acid deficiency.
Begin tapering TPN for EN slowly, when enteral feeds provide 1/3 to 1/2 of nutrient requirements. When 60% of needs can be tolerated enterally, discontinue TPN.
BEWARE OF REFEEDING SYNDROME (starved cells take up nutrients, shifting K+, phos, and magnesium into the cell, causing HYPOKALEMIA, HYPOPHOSPHATEMIA, and HYPOMAGNESEMIA).
Overfeeding dextrose can lead to hyperglycemia
Dietary Reference Intake (DRI) reflects current population needs.
Recommended Dietary Allowance (RDA) is goals for healthy individuals.
Estimated Average Requiremenr (EAR) assesses group nutritional adequacy.
Upper Limit (UL) offers guidance on safe upper limits for nutrients such as vitamins.
Dietary Guidelines made to prevent chronic disease. DG written by USDA and HHS. Community nutrition programs use Dietary Guidelines to develop their plans (variety in eating, nutrient density, serving sizes, limit calories from saturated fats and added sugars, reduce sodium intake.
Healthy Eating Index (by USDA) is a measure of overall diet quality. Measures how well we follow the recommendations.
My Plate (USDA) shows essential food groups. Recommendations: balancing calories, foods to increase in the diet, foods to reduce.
Healthy People Program (HHS) identifies broad goals and specific objectives for improving health of the public. Focuses on disease prevention by changing behaviours.
The three steps in planning programs:
1) Mission Statement - describes the philosophy of the program. Need/Problem Statement describes the current situation, who says it's a problem, and what will occur if nothing is done.
2) Goals - goals are statements of broad direction and general purpose. Determine which health problems have nutritional implications. Determine what the high risk groups are. Determine what the most critical needs are.
3) Objectives - must be measurable. Objectives are more specific and defined than goals. Include specific target dates for completing specific projects. Evaluate alternative strategies available using cost effectiveness analysis.
Budget controls and coordinates activities. Indicates how and at what rate money should be expended.
Public health departments derive a portion of their income from general revenue taxes. Federal, local, and foundation grants are other sources of income.
Intervention via community nutrition programs relates to the 3 domains of learning: Cognitive, Affective, and Psychomotor.
Enabling makes it easier for people to act. Use the 4 Ps of marketing: Product, Price, Place, Promotion.
A strategy which involves psychomotor learning is helping people develop the skills needed to make and sustain new habits (e.g. how to budget, how to find the services they need.
Monitoring and Evaluation = the 4th step in the Nutrition Care Process (NCP)
Nutrition care outcomes represent results that the practitioner and nutrition care impacted individually. They can be linked to nutrition intervention goals. They're measurable and occur in a reasonable time period. They are attributed to the nutrition care provided. They're logical stepping stones to other health care outcomes.
Nutrition care outcomes are distinct from other health care outcomes b/c they represent the nutrition practitioner's specific contribution to care. They are grouped into 4 categories:
1) Food and Nutrition Related History
2) Lab Data and Medical Tests
3) Anthropometrics
4) Nutrition-Focused Physical Findings
#dietetics#clinical#notes#basal metabolic rate#nutrition care process#tube feeds#tube feedings#tpn#ppn#total parenteral nutrition#peripheral parenteral nutrition#vitamins#minerals#budget#sales#marketing#obesity#kidney#kidneys#renal#glucose infusion rate#GIR#enteral#enteral nutrition#nutrition programs#programs#dextrose#pregnancy#preeclampsia
0 notes
Text
long overdue update
Hello everyone,
So, it’s been a while since we’ve done an update to this blog. We are currently in the hospital with a central line infection and a UTI. We came in last Sunday to the ER, and they told us we were fine, so we went home. I saw my bloodwork and all was not fine. Our white blood cells were crashing and the platelets were dropping too. They just sent us home with an oral antibiotic and…
View On WordPress
#central line#chronic illness#chronically ill#EDS#gastroparesis#hospital#total parenteral nutrition#TPN
0 notes
Text
Wound Care
Ok so, take this with a BIG grain of salt, because I may be a medical doctor BUT you need to know how much wound care training we get in medical school: none. Zip. Zilch. There may be medical schools where you do, but mine wasn't a bozo factory and there was NO wound care training. Everything I know I learned from one of several sources: an intensive 2-day wound care course I did in residency (highly recommend), the local Home Health wound care nurse (highly recommend), a completely batshit insane old white male doctor who started our learning sessions by yelling Vietnam War stories at me (do not recommend), a hospital wound care nurse (highly recommend), and experience (oh god do not recommend).
The first thing you need to know is that wound healing varies dramatically across the course of a lifespan. Kids? Kids will heal. If they don't, get their ass to a pediatrician because there's something genetic going on. Young adults will heal. Middle-aged adults will heal. You know who doesn't heal for shit? The elderly, and people with severe illnesses, and people with uncontrolled type II diabetes.
Your body needs several things in order to heal. It needs macronutrients, so you need to be able to EAT protein, fat, and carbs. If you are on total parenteral nutrition, aka TPN, aka IV nutrition, you are going to be worse at healing. If you are starving yourself, you are going to be worse at healing. If your body is desperately funneling all the calories you take in to surviving your COPD or cancer, you are going to be worse at healing.
It also needs micronutrients. If your diet sucks, you won't heal. Take a multivitamin once in a while.
There are two CRITICAL skin components to healing: collagen and elastin. Guess what we stop making as we age. Promoting collagen isn't just good for "anti-aging," it's good for NOT ripping your skin apart. Taking oral collagen is probably bullshit because your body is going to have to disassemble it to get it across the intestinal membranes to absorb, but it's also harmless, and if your diet REALLY sucks, who knows. Give it a try. Collagen is made of amino acids; think protein.
Another absolutely crucial component is blood flow. As people age, they start to develop cholesterol plaques lining arteries that eventually pick up calcium deposits. This makes blood vessels less elastic, which is a problem, but eventually also blocks them off, which is a much bigger problem. If someone has the major blood flow to their feet decreased by 90% by arterial stenosis, they are not going to heal for shit AND their foot's gonna hurt.
One component of blood flow I hadn't thought about before going into medicine is fluid retention. The way your body works, blood exits the heart at a very high velocity, but slows to a crawl by the time it gets into capillaries, the smallest blood vessels in the body. Water is a very small molecule and can leave the blood vessel, especially if there aren't big, negatively-charged molecules like proteins like albumin in the blood vessels to hold the water there. And we're built for this--some water is supposed to leak out of our blood vessels when it gets to real little vessels. It gets taken back up by the lymphatic system and eventually dumped back into the bloodstream at the inferior vena cava. But if you aren't making albumin--for instance, in liver failure--you may leak a LOT of fluid into the tissue, so much that your legs get swollen, tight, the skin feeling woody and strange. This isn't fixable by drainage because the fluid is everywhere, not in a single pocket we can drain. And because it puts so much pressure on the tissues of the skin, it often results in ulcers. Congestive heart failure, liver failure, kidney failure--these are all common causes of severe edema, aka swelling due to fluid in the tissues. And they're a real bitch when it comes to wound care, because we have such limited resources for getting the fluid back out, which is a necessary first step to healing.
Pressure is another common cause of wounds. Pressure forces blood out of those little capillaries, so you starve the cells normally fed by those capillaries, and they die. It's called pressure necrosis. Very sick people who can't turn themselves over--people in the ICU, people in nursing homes--are especially prone to these wounds, as are people with limited sensation; pressure wounds are common in wheelchair users who have lost some feeling in the parts of their bodies that rub against those surfaces, or diabetics who don't notice a rock in their shoe.
So, if you're trying to treat wounds, the questions to ask are these:
Why did this wound happen?
-Was it pressure? If it's pressure, you have to offload the source of the pressure or else that wound will not heal. End of story. You can put the tears of a unicorn on that thing, if you don't offload the pressure it won't heal.
-Was it fluid? If it's fluid, you have get the fluid out of the issues or else it won't heal. You can sometimes do that with diuretics, medications that cause the body to dump water through the kidneys, but that's always threading a needle because you have to get someone to a state where they still have juuuuust enough fluid inside their blood vessels to keep their organs happy, while maintaining a very slight state of dehydration so the blood vessels suck water back in from the tissues. You can use compression stockings to squeeze fluid back into the vessels, but if they have arterial insufficiency and not just venous insufficiency, you can accidentally then cause pressure injury. The safest option is using gravity: prop the feet up above the level of the heart, wherever the heart is at, at that moment, and gravity will pull fluid back down out of the legs. Super boring though. Patients hate it. Not as much as they hate compression stockings.
-Was it a skin tear because the skin is very fragile? This is extremely common in the elderly, because they're not making collagen and elastin, necessary to repairing skin. If this is the case, make sure they're actually getting enough nutrition--as people get into their 80s and 90s, their appetites often change and diminish, especially if they're struggling with dementia. And think about just wrapping them in bubble wrap. Remove things with sharp edges from their environments. I have seen the WORST skin tears from solid wood or metal furniture with sharp edges. Get rid of throw rugs and other tripping hazards. I had somebody last week who tried to a clear a baby gate and damn near destroyed their artificial hip.
The next critical question: why isn't it healing?
-Are you getting enough nutrients? Both macro and micro?
-Are you elderly?
-Are you ill?
-Do you have a genetic disorder of collagen formation?
Fix why it's not healing and almost anything will heal. If you're diabetic, find a medication regimen that improves your sugars and stick to it. If you're anorexic, get treatment for your eating disorder. If you have congestive heart failure, work with your doctor on your fluid balance. Wear the damn pressure stockings. Prop up your feet.
If, after those two unskippable questions are done, you want to do something to the wound--apply a dressing, do a treatment--that's a whole other kettle of fish. I'll write that later. The dryer just sang me its little song and I need to put away the laundry.
673 notes
·
View notes
Text
I’m creating an informational series on tube feeding on my Instagram @ paralyzedguts and I’d like to get some questions and perceptions from orally fed people on tube feeding! I’d like to create something like a FAQ and a common misconceptions post about enteral nutrition.
Tell me in the tags what you know (or think you know) about feeding tubes! Do you have a feeding tube? If so what kind? You can shoot me an ask as well.
I have a GJ (gastrojejunostomy) tube for gastroparesis. I take all my nutrition through the tube (100% tube fed).

Image description:
A silhouette of a human demonstrating multiple routes of nutrition.
The person has a pink bottle with a route line going through the mouth, down the esophagus, and into the stomach to represent oral nutrition.
They have a grey feed bag with multiple route lines to represent enteral nutrition. One from the bag in the nose, down the esophagus and into the stomach representing an NG (nasal-gastric) tube. Another from the bag into the stomach, representing a G (gastrostomy) tube. And a third from the bag to the intestine, representing a J (jejunostomy) tube.
They have an orange parenteral bag with two route lines. The first from the bag to the person’s arm, representing total or partial parenteral nutrition via a PICC line. The second one from the bag to the person’s heart, representing TPN/PPN via a port.
End image description
1K notes
·
View notes
Note
Possibly(?) easy question if you're inclined: Beyond saline, are there some common IV nutrients/supplements a person might be likely to be given if they've been in a physically stressful situation for a while (where they haven't been able to take good care of themself/have lost some weight) and have now reached medical care but are going to need to be going into surgery in the near future?
We don't typically give nutrients IV. If a person can't use their mouth to eat we typically give them an NG tube into their stomach so we can give tube feed. If they can't use their whole digestive system, we might give TPN (total parenteral nutrition) via IV but TPN is somewhat dangerous and very expensive, so we'll exhaust a lot of options prior to this method.
What we might do is if the person has very low protein in their blood, we can give protein in the form of human albumin. It is important to have protein in the blood to both maintain blood pressure and to be able to use certain medications. Human albumin is a blood product, meaning it is derived from donated blood.
We may also give an IV solution called lactated ringers. This is kind of like an IV sports drink, and it replaces many lost electrolytes. If there are any particular electrolytes (like potassium or magnesium) that need replaced, those may also be given, either orally or in IV form.
53 notes
·
View notes
Note
Only asking this bcs it's simular to your most recent coin so feel free to reject if to repetitive but could you make a flag for transtpn (total parenteral nutrition)

TRANS TPN



When one identifies as using a Total Parental Nutrition .
For whatever specified / unspecified reasons .
TransAbled . ECT ECT

If already coined consider as an alt . Req by @1s334ng3ls .
No DNI . Just be nice / civil about it . Free for anyone .

#you stepped on a landmine#radqueer#transid#pro radq#pro radqueer#pro transx#radq safe#radqueer community#radqueer safe#radqueers please interact#rq community#radq#radq coining#radq interact#radqueer coining#radqueer interact#radqueer please interact#rqc🌈🍓#rqc#pro rq 🌈🍓#rq 🌈🍓#rq safe#rq coining#rq please interact#rq interact#rqc 🌈🍓#pro rqc#rqc 🍓🌈#transid community#transid safe
21 notes
·
View notes
Note
Buckshot Anon here! At long last, it is time to talk about Alastor’s recovery period after the events of the Spawn of Evil AU (for all those who don’t know what that AU is, it basically involves Alastor suffering an ectopic pregnancy by Roo, and Lucifer helping to keep him alive. I got asked its logistics a while back, and now that's a constant).
The recovery on this is interesting because it is simultaneously pretty simple and complicated. The best place to start is with the surgery itself, because delivery would not be able to happen in a natural way, and would need to be done through surgery, though not a cesarean in the traditional way. Because the part of the small intestine the parasite child latched onto would be incredibly damaged by virtue of the warping necessary for the child to grow (which would have caused a rupture unless angelic blood has medicinal properties), the procedure would be treated as an intestinal resection surgery, where the effected area of the small intestine would be outright removed. Specifically an open surgery, making a cut of about 6-8 inches in the stomach. A cesarean would have 4-6 inches normally, so if you’re going with a happy medium, an incision of 6 inches. After the damaged area and the child are removed, the healthy parts of the small intestine on either end would be stitched or stapled together. This whole procedure would probably not take more than two hours, but could go upwards of four hours if there is damage in the surrounding areas of the intestines and other organs.
Once the surgery was finished, Alastor would on average stay in the hospital for a week, both to recover and make sure there had been no complications or damage to other organs. Some people can go home within three days, but due to the nature of the situation, he would be asked to stay longer. He would need to receive nutrition through an IV for a period of time before being allowed to go on a liquid diet. I will elaborate on that more in a minute, but there are some other things that should be brought up.
After being discharged from the hospital, Alastor would not be allowed to continue work at the hotel for another 4-6 weeks. There is some wiggle room in this, he may be able to return to work within 2-3 weeks provided that work is strictly paperwork, but anything physical he would need to wait a while to avoid reopening the stitching on his intestines and the incision area, or causing a hernia. He will also be encouraged to walk regularly every day, for reasons including:
Boosting blood flow, which helps to prevent blood clots.
Lessening his chances of illness.
Preventing a buildup of excessive abdominal scar tissue that could hinder movement and cause more blockages in the intestines. Scar tissue is something that will happen and in itself isn’t a problem, but scar tissue can and will become excessive if given the chance, and being sedentary while it is building up can make that worse.
Regaining muscle mass he would have lost from months on bedrest.
Avoiding constipation. Awkward to talk about but that is an important reason.
Alastor also would not be allowed to have sex for 2-6 weeks. I doubt he would be heartbroken by this information.
If angel blood truly does have a medicinal property that could heal him, he can mostly skip this part, and go straight into the complicated part.
Remember when I said I would elaborate more on the nutrition IV and the liquid diet? That’s where this comes into play. Alastor ate minimally if at all for the majority of the estimated 7.5 months (30 weeks, give or take) of pregnancy, and that makes the situation more complicated than it traditionally would be. Being generous and saying he was able to eat solids for the first 6 weeks, after which the blockage would make that very painful, and another 2 weeks would make even a liquid diet technically doable but difficult, Alastor would be living off of angel blood and nutrition IVs, specifically Total Parenteral Nutrition (TPN).
That in itself is doable. People can be TPN-dependent for upwards of three years and still have a 65-80% survival rate. It can replace eating for as long as necessary. However, there is a caveat to that. Surviving TPN-dependent is one thing, but once someone is taken off it and needs to adjust to eating again, they can be at high risk of what is called refeeding syndrome.
Refeeding syndrome is an interesting topic with a lot of complicated factors, but the main thing to know is the body adapts quickly to having little to no food. Metabolism drastically changes, and certain organs will begin to function differently as a result. Alastor can’t immediately begin to eat like he did before all of this because his body is no longer equipped to do so. If he were to try binge-eating or even just eating something normal after being discharged from the hospital, the symptoms he would suffer vary but consistent ones tend to be seizures and coma, sometimes even cardiac arrest or respiratory failure that result in death.
To get around this, the best way to go about it is to very gradually reintroduce food into his diet over the course of 2 weeks, starting by eating about 14-28% of the calories he would normally need, and building upwards over those few weeks. Reteaching his body how to digest food and restore a healthy intestinal tract can usually happen within 2 weeks, but when accounting for how long he wasn’t eating solid food and the damage he needs to heal from, he might be recommended to do this for 3 weeks to be on the safe side. His best bet would be light soups and maybe yogurt.
Most of this would be handled in the hospital, the process of weaning him off the TPN, by the second or third day reintroducing liquids, then soft foods. Doctors would still want to keep tabs on him for this process once discharged, and would be able to make a better judgement call with his situation specifically on when he can return to eating normally. Normally, as in a reasonable meal, not eating multiple people or even one person in one sitting, that would have to wait the 4-6 weeks after discharge.
He would need to have multiple check-ins with his primary doctor for various reasons to make sure everything is going smoothly, make sure his physical therapy and regaining of muscle mass is going well, and that he is eating properly and healing. Doctors would also be searching for any signs of stress and psychological distress that may negatively impact Alastor’s health and cause thoughts of harming the child, which would result in a postpartum depression screening and/or a post-traumatic stress disorder screening. Debates on if Alastor would even consider the child as one aside, that does not change the need to carefully monitor his mental state and try to improve his quality of life as well as prevent any loss of life or actions he may regret.
In summary: Alastor would have an open intestinal resection surgery, spending his first week in the hospital and after that point focusing on resting while recovering muscle mass, as well as slowly reintroducing his body to food after being taken off the IV. He should be able to eat regularly (in moderation, don't eat a person) within 2-3 weeks, with the rest of his healing taking somewhere between 4-6 weeks. He would not make a full recovery for a few months, but provided his recovery goes smoothly while monitored, he could return to his daily life with minimal issue within 6 weeks.
(Note: The stress and trauma of the whole experience could hinder recovery severely because an increase in stress causes wounds to heal significantly slower and weakens the immune system. If this happened, it would increase Alastor’s recovery time by roughly 25%, but could be increased by up to 60% depending on the severity of that stress. Prioritizing a stress-free environment would be crucial to his recovery.)
(Another note: The pregnancy duration was estimated at give or take 30 weeks, the reason for that is pregnancy weeks are weird. It’s calculated from the date of the last menstrual period, not the date of conception. Alastor does not have the equipment for having it traced the normal way, that’s half the problem, so it would be based on the objective weeks since conception. Unlike the average pregnancy where it’s a gamble if the mother knows the conception date, Alastor would undoubtedly know.)
👀
20 notes
·
View notes
Text
Why Does Escher Sound Normal?
Unlike the other NPC cyberhead characters who have voicelines (like DOTEXE, or the cyberhead Classic Oldhead, or cyberhead civilians you can run into…) Escher has little to no robotic voice filter over his voicelines.
https://youtu.be/dxqQAeN2kwo Escher voicelines
https://youtu.be/MskVzMtpFtU DOTEXE member voicelines
Honestly, the cleanest explanation for the voice difference is, “Cyberheads can just choose how they want their electronic voices to sound, and some want it to sound more electronic--and Escher just wanted to sound less electronic”. However, I’m not looking for a clean explanation here- I very much like making up shit that could be plausible.
Long-winded headcanon explanation(?) under the cut for length and also due to spoilers for the plot of Bomb Rush Cyberfunk:
Given that the standard cyberhead appears to be able to support a fully functioning human head inside of it, while more or less being able to work like a normal cyberhead (vision through the four eyes, breathing, etc) it may be possible that individual cyberheads may have differing amounts of head left depending on how they got beheaded (intentionally or otherwise). Getting guillotined by a (insert bladed thing here) doesn’t have to be the One and Only way of losing your mind.
Anyways, I imagine that Escher has enough of his body’s original head to have a functioning larynx, mouth, and nasal cavities/passages, which would allow him to sound more like a regular human.
Let’s take a look at some headcanons in detail:.
How could you lose only part of your head in such a way that leaves, more or less, the entire rest of your mouth and nose intact? Since Escher is a sniper, perhaps he (or whoever had his body originally, depending on whether you interpret him to have the downloaded memories of, or be a completely different person from, the original owner of the body) got detected on a mission and, unfortunately for him, got hit by a headshot above his nose/mouth (though, it’d have to be angled to not hit the lower parts of the mouth and throat, and also be from a weapon with a smaller caliber--if it was too large his whole head would be uh. vaporized)
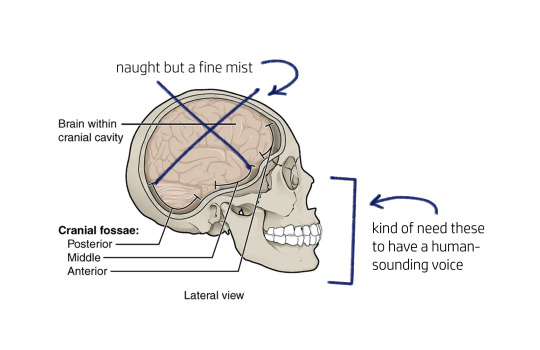
With a fully intact body but the brain turned into naught but a fine mist, he’d probably be a prime candidate for a cyberhead… (something something even death may not free you from the military-industrial complex something something)
On to the cyberhead itself. With little to no use for the remaining cranial cavity and any remaining chunks of eyes, excess parts of the skull could be cut away. The AI and other mechanical components could be placed where the brain was, though some nerve and artificial muscle connections would need to be made to ensure the lips, jaw, and tongue move correctly, as those are needed in forming sounds. Additional connections would need to be made between the AI/other components and the spinal cord, other nerves down to the body, so on and so forth. Just add a small mic with no modulation to get over the “muffled” sound of a person with something like a helmet over their face and voila-
a cyberhead who sounds very human.
But wait a minute… if he has a mouth that works, could he eat normally?
Well, probably. I’d love to get deeper into oral, enteral, and parenteral nutrition in cyberheads, but that’s a topic for another day. At the time of writing this, I still need a bit more research to familiarize myself with the topic before presenting any in-depth headcanons.
If there’s anything I can say about the subject, I’ve seen several people present the headcanon that the two plates making up the “face” of the standard cyberhead are hinged and can swing apart, like so:
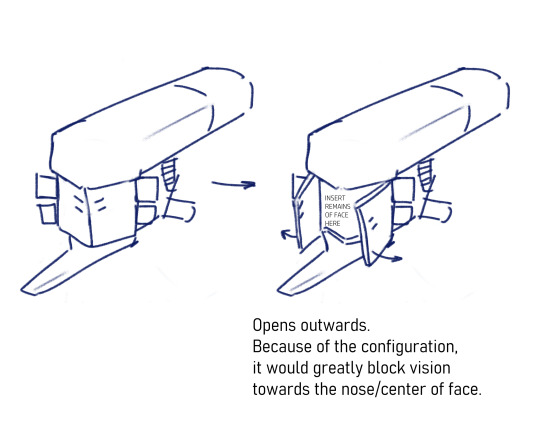
This definitely would allow eating, albeit awkwardly, since the plates are big enough to totally block vision towards the center of the face. Eating in this way would mean he’d be unable to see what he’s putting in his mouth directly, and instead would either have to hold food slightly to the left or to the right of the central faceplates, or angle his head to see it.
(Any activity that blocks the vision of a sniper is not ideal; I wonder if there are sniper-specific cyberhead configurations, military-produced, that don’t have this problem?)
Whatever’s left of his face in there is probably not pretty, either- I imagine he isn’t the kind to eat in front of other people, though there may be individual cyberheads with a similar head model and face configuration who Don’t Care About That and are 100% fine with opening their face plates to have a snack in front of anyone.
WAIT. Could he… kiss?
It would probably be difficult and more than a little awkward for everyone involved, but probably yes? The hinged faceplate configuration as described above would make it difficult- opening the faceplates so they extend parallel to the chin would make it annoying for another person to get their face in closer; opening the faceplates further, to be perpendicular to the chin, would completely and totally block his vision. Maybe just kissing someone’s hand may be a little easier given the faceplate configuration? Not that it’s any of my business.
Hey, what about Red? If Red and Escher have almost the same cyberhead, wouldn’t Red have, at some point, figured out how to open the faceplates?
Even though they both seem to have standard cyberheads, it’s possible that individual standard cyberheads could be customized based on the needs of the beheaded individual, with a variety of different customization options. I get the feeling that purchasing a cyberhead for use is a little like buying a car- an expensive purchase with a lot of customization options for different needs or wants, with more customization increasing the price. Since Red’s head was apparently from the Versum Hill scrap heap, maybe it was originally for a 100% beheaded individual who didn’t have any need for hinged faceplates, who could take in food via tube.
One last note: Though Red/Felix has a fully functional head with a functioning larynx and mouth hidden within a standard cyberhead, he sounds very electronic. But, given Flesh Prince and DJ Cyber wanted his existence to be kept secret, it wouldn’t be too far out to say that they intentionally added voice modulation to more closely get him to resemble a regular cyberhead.
#courts talks#bomb rush cyberfunk#brc#brc escher#started typing this at like 10 PM yesterday and here we are#it's been a while since i've had enough motivation(?) to write short headcanon essays like this lol
31 notes
·
View notes
Text
Dude, I'm missing Artfight in the hospital... WAAAAAAA. Gastric Emptying Test tomorrow ='-( I'm scared 1) They will see nothing wrong, or, 2) The eggs Hurt My Stomach Bigly. I can't eat or drink before the test. Sad.
I'm grateful to both the chicken and the egg... it makes me feel sad to eat it. I wish it was just a banana.
I snuck a THC puff today because I was fainting in the bathroom, and you can't have Fentanyl (legally, for pain, in an IV) before a GET. They stole what I did for Calprotectin testing. My intestines hurt so bad right now, even though...
So far, neither my Endoscopy or Colonoscopy saw anything, and they took a lot of biopsies which haven't come back yet. My bloodwork's inflammatory markers are negligible, but I'm low in Thiamine, Protein, Potassium, Sodium, and Glucose. My Glucose won't stay up at all. It is constantly racing to twenty even when I successfully kept down an entire bag of Skittles. I have severe bradycardia to the point of getting to 26 beats per minute. My blood pressure is trending downwards randomly. My right arm has two separate IVs, one a Sodium Chloride, one a Total Parenteral Nutrition, an allergy band, admission bracelet, two band-aids and a Freestyle Libre continuous Glucose monitor.

At least I got Compiz set up in Gnome Extensions so now my windows Jiggle...
youtube
6 notes
·
View notes
Text
Only a few days to go until my bowel resection surgery, and I'm feeling pretty nervous. I'm not sure how complicated life will be after my ileostomy and what the learning curve will be like.
My doctor gave me an estimate of around two months before I could get my reversal surgery, so at the very least, I can take solace in the fact that my stoma won't be permanent. The things I am most looking forward to are not being in horrible pain anymore and being able to eat solid foods again!
My doctor gave me the okay to stop my Total Parenteral Nutrition infusions for now, but I'll still have my PICC Line until I check into the hospital next week. We're flushing the line with saline and heparin every day so I don't end up with a blood clot right before surgery.
I have my "delicious" bowel prep to do on Monday, and then on Tuesday morning, we'll be getting ready to drive over to the hospital. I will most likely be spending 5 to 7 days recovering in the hospital before I'm discharged.
This is my first surgery for Crohn's Disease, so I'm not quite sure what to expect. I'll be sure to update you all again once I'm out of the hospital!
#personal#crohn's disease#bowel resection#disability#ostomy#ileostomy#crohn's problems#i'll still have my queue going and i'll post on my phone from time to time#i'm looking forward to eating solid food again#it's been a long 6 weeks#tw: medical#about me
11 notes
·
View notes
Text

#dietetics#PN#TPN#parenteral nutrition#total parenteral nutrition#nutrition#lipid#lipids#omega 3#Omegaven
0 notes
Text
Medical Abbreviations on Pharmacy Prescriptions
Here are some common medical abbreviations you may see on pharmacy prescriptions:
qd - once a day
bid - twice a day
tid - three times a day
qid - four times a day
qh - every hour
prn - as needed
pc - after meals
ac - before meals
hs - at bedtime
po - by mouth
IV - intravenous
IM - intramuscular
subQ - subcutaneous
mL - milliliter
mg - milligram
g - gram
mcg - microgram
stat - immediately, right away
NPO - nothing by mouth
cap - capsule
tab - tablet
susp - suspension
sol - solution
amp - ampule
inj - injection
Rx - prescription
C - Celsius
F - Fahrenheit
BP - blood pressure
HR - heart rate
RR - respiratory rate
WBC - white blood cell
RBC - red blood cell
Hgb - hemoglobin
Hct - hematocrit
PT - prothrombin time
INR - international normalized ratio
BUN - blood urea nitrogen
Cr - creatinine
Ca - calcium
K - potassium
Na - sodium
Cl - chloride
Mg - magnesium
PO2 - partial pressure of oxygen
PCO2 - partial pressure of carbon dioxide
ABG - arterial blood gas
CBC - complete blood count
BMP - basic metabolic panel
CMP - comprehensive metabolic panel.
ECG - electrocardiogram
EEG - electroencephalogram
MRI - magnetic resonance imaging
CT - computed tomography
PET - positron emission tomography
CXR - chest x-ray
CTX - chemotherapy
NSAID - nonsteroidal anti-inflammatory drug
DMARD - disease-modifying antirheumatic drug
ACE - angiotensin-converting enzyme
ARB - angiotensin receptor blocker
SSRI - selective serotonin reuptake inhibitor
TCA - tricyclic antidepressant
ADHD - attention deficit hyperactivity disorder
COPD - chronic obstructive pulmonary disease
CAD - coronary artery disease
CHF - congestive heart failure
DVT - deep vein thrombosis
GI - gastrointestinal
UTI - urinary tract infection
OTC - over-the-counter
Rx - prescription
OD - right eye
OS - left eye
OU - both eyes.
TID - thrombosis in dementia
TDS - ter die sumendum (three times a day)
BOM - bilaterally otitis media (infection in both ears)
BT - body temperature
C&S - culture and sensitivity
D/C - discontinue or discharge
D/W - dextrose in water
ETOH - ethyl alcohol
FUO - fever of unknown origin
H&P - history and physical examination
I&D - incision and drainage
I&O - intake and output
KVO - keep vein open
N&V - nausea and vomiting
PERRLA - pupils equal, round, reactive to light and accommodation
PR - per rectum
QAM - every morning
QHS - every bedtime
QOD - every other day
S/P - status post (after)
TPN - total parenteral nutrition
UA - urinalysis
URI - upper respiratory infection
UTI - urinary tract infection
VO - verbal order.
XRT - radiation therapy
YOB - year of birth
BRBPR - bright red blood per rectum
CX - cervix
DVT - deep vein thrombosis
GB - gallbladder
GU - genitourinary
HCV - hepatitis C virus
HPI - history of present illness
ICP - intracranial pressure
IVP - intravenous pyelogram
LMP - last menstrual period
MRSA - methicillin-resistant Staphylococcus aureus
MVA - motor vehicle accident
NKA - no known allergies
PEG - percutaneous endoscopic gastrostomy
PRN - pro re nata (as needed)
ROS - review of systems
SOB - shortness of breath
TAH - total abdominal hysterectomy.
TIA - transient ischemic attack
Tx - treatment
UC - ulcerative colitis
URI - upper respiratory infection
VSD - ventricular septal defect
VTE - venous thromboembolism
XR - x-ray
w/c - wheelchair
XRT - radiation therapy
ASD - atrial septal defect
Bx - biopsy
CAD - coronary artery disease
CKD - chronic kidney disease
CPAP - continuous positive airway pressure
DKA - diabetic ketoacidosis
DNR - do not resuscitate
ED - emergency department
ESRD - end-stage renal disease
FFP - fresh frozen plasma
FSH - follicle-stimulating hormone.
GCS - Glasgow Coma Scale
Hct - hematocrit
Hgb - hemoglobin
ICU - intensive care unit
IV - intravenous
JVD - jugular venous distension
K - potassium
L - liter
MCH - mean corpuscular hemoglobin
MI - myocardial infarction
Na - sodium
NGT - nasogastric tube
NPO - nothing by mouth
OR - operating room
PCN - penicillin
PRBC - packed red blood cells
PTT - partial thromboplastin time
RBC - red blood cells
RT - respiratory therapy
SOA - short of air.
SCD - sequential compression device
SIRS - systemic inflammatory response syndrome
STAT - immediately
T - temperature
TPN - total parenteral nutrition
WBC - white blood cells
ABG - arterial blood gas
A fib - atrial fibrillation
BPH - benign prostatic hypertrophy
CBC - complete blood count
CO2 - carbon dioxide
COPD - chronic obstructive pulmonary disease
CPR - cardiopulmonary resuscitation
CT - computed tomography
CXR - chest x-ray
D5W - dextrose 5% in water
Dx - diagnosis
ECG or EKG - electrocardiogram
EEG - electroencephalogram
ETO - early termination of pregnancy.
FHR - fetal heart rate
GSW - gunshot wound
H&P - history and physical exam
HCG - human chorionic gonadotropin
I&D - incision and drainage
IBS - irritable bowel syndrome
ICP - intracranial pressure
IM - intramuscular
INR - international normalized ratio
IOP - intraocular pressure
LFT - liver function test
LOC - level of consciousness
LP - lumbar puncture
NG - nasogastric
OA - osteoarthritis
OCD - obsessive-compulsive disorder
OTC - over-the-counter
P - pulse
PCA - patient-controlled analgesia
PERRLA - pupils equal, round, reactive to light and accommodation.
PFT - pulmonary function test
PICC - peripherally inserted central catheter
PO - by mouth
PRN - as needed
PT - physical therapy
PT - prothrombin time
PTSD - post-traumatic stress disorder
PVC - premature ventricular contraction
QD - once a day
QID - four times a day
RA - rheumatoid arthritis
RICE - rest, ice, compression, elevation
RSI - rapid sequence intubation
RSV - respiratory syncytial virus
SBP - systolic blood pressure
SLE - systemic lupus erythematosus
SSRI - selective serotonin reuptake inhibitor
STAT - immediately
TB - tuberculosis
TIA - transient ischemic attack.
TID - three times a day
TKO - to keep open
TNTC - too numerous to count
TPN - total parenteral nutrition
URI - upper respiratory infection
UTI - urinary tract infection
V-fib - ventricular fibrillation
V-tach - ventricular tachycardia
VA - visual acuity
WNL - within normal limits
AED - automated external defibrillator
ARDS - acute respiratory distress syndrome
BID - twice a day
BP - blood pressure
BUN - blood urea nitrogen
CAD - coronary artery disease
CHF - congestive heart failure
CVA - cerebrovascular accident
D/C - discontinue
DKA - diabetic ketoacidosis.
DM - diabetes mellitus
DVT - deep vein thrombosis
EGD - esophagogastroduodenoscopy
ER - emergency room
F - Fahrenheit
Fx - fracture
GI - gastrointestinal
GTT - glucose tolerance test
HCT - hematocrit
Hgb - hemoglobin
HRT - hormone replacement therapy
ICP - intracranial pressure
IDDM - insulin-dependent diabetes mellitus
IBS - irritable bowel syndrome
IM - intramuscular
IV - intravenous
K - potassium
KVO - keep vein open
L&D - labor and delivery
LASIK - laser-assisted in situ keratomileusis.
ROM - range of motion
RT - radiation therapy
Rx - prescription
SCD - sequential compression device
SOB - shortness of breath
STD - sexually transmitted disease
TENS - transcutaneous electrical nerve stimulation
TIA - transient ischemic attack
TSH - thyroid-stimulating hormone
UA - urinalysis
US - ultrasound
UTI - urinary tract infection
VD - venereal disease
VF - ventricular fibrillation
VT - ventricular tachycardia
WBC - white blood cell
XRT - radiation therapy
XR - x-ray
Zn - zinc
Z-pak - azithromycin (antibiotic).
AAA - abdominal aortic aneurysm
ABG - arterial blood gas
ACS - acute coronary syndrome
ADL - activities of daily living
AED - automated external defibrillator
AIDS - acquired immunodeficiency syndrome
ALS - amyotrophic lateral sclerosis
AMA - against medical advice
AML - acute myeloid leukemia
APAP - acetaminophen
ARDS - acute respiratory distress syndrome
ASCVD - atherosclerotic cardiovascular disease
BPH - benign prostatic hyperplasia
BUN - blood urea nitrogen
CABG - coronary artery bypass graft
CBC - complete blood count
CHF - congestive heart failure
COPD - chronic obstructive pulmonary disease
CPAP - continuous positive airway pressure
CRF - chronic renal failure.
CT - computed tomography
CVA - cerebrovascular accident
D&C - dilation and curettage
DVT - deep vein thrombosis
ECG/EKG - electrocardiogram
EEG - electroencephalogram
ESRD - end-stage renal disease
FSH - follicle-stimulating hormone
GERD - gastroesophageal reflux disease
GFR - glomerular filtration rate
HbA1c - glycated hemoglobin
Hct - hematocrit
HIV - human immunodeficiency virus
HPV - human papillomavirus
HTN - hypertension
IBD - inflammatory bowel disease
IBS - irritable bowel syndrome
ICU - intensive care unit
IDDM - insulin-dependent diabetes mellitus
IM - intramuscular.
IV - intravenous
LFT - liver function test
MI - myocardial infarction
MRI - magnetic resonance imaging
MS - multiple sclerosis
NPO - nothing by mouth
NS - normal saline
OCD - obsessive-compulsive disorder
OSA - obstructive sleep apnea
PCOS - polycystic ovary syndrome
PMS - premenstrual syndrome
PPD - purified protein derivative
PSA - prostate-specific antigen
PT - prothrombin time
PTT - partial thromboplastin time
RA - rheumatoid arthritis
RBC - red blood cell
RSV - respiratory syncytial virus
SLE - systemic lupus erythematosus
TB - tuberculosis.
It is important to remember that medical abbreviations can vary based on location and specialty.
Healthcare professionals should use medical abbreviations with caution and only when they are familiar with their meanings.
Patients should always communicate any questions or concerns they have about their medications or medical care to their healthcare provider or pharmacist to ensure they receive safe and accurate medical care.

9 notes
·
View notes
Text
This is a hurdle I’ve been seeing a lot lately now that I’m learning more about tubie life but
Fat people can require feeding tubes
Fat people can be malnourished
Fat people are deserving of enteral/parenteral nutrition and the current standard of qualifying for alternate nutrition often demands that fat people face a more extreme depletion of nutrition before they’re given the same interventions as mid-size and skinny people. One of the determinations of tube placement is involuntarily losing 5-10% of your body weight within 6 months, which can be a significant impact for someone whose starting weight is 220lbs vs 120lbs. Starvation can still send the body into metabolic acidosis/starvation ketoacidosis long before the bigger person hits that 5-10% lost threshold.
Weight loss/diet culture compounds with this because any weight lost by a fat person is often seen as a “good” thing and not documented as a medical problem or a negative symptom. I lost so much weight before my tube was placed that I am now mid-size, and it has already had an impact on my treatment. Most nurses and other healthcare providers are now shocked that I’ve lost over 60lbs in a few months, instead of congratulatory. I’m no longer “looking great”, I “look sick”. Despite that, I still had another nurse look at me and say “you look like you can eat and drink, why do you have a feeding tube?” Sorry- I didn’t know you could just look at me and determine that, considering my stomach is paralyzed.
Enteral feeding is also not even developed to be accessible for larger people. G/GJ tubes have approximately 10cm of tube designed for use inside the body (stoma). Fat people sometimes need to move straight to total parenteral nutrition because the devices themselves lack accessibility. TPN is associated with higher risks than enteral feeding and is often used as a “last resort”, but yet a lot of larger people don’t have another option.
#gastroparesis#fatphobia#don’t mind me I just keep seeing other people with gastroparesis denied tube feeding because of their weight#ableism#disability tag
1K notes
·
View notes
Note
Okay so, if you've watched Knives Out, the scene where Marta's giving Harlan his medicine, she's not giving him the shots directly but putting them through a tube thing around his arm. What is that? How does it work? Can/ should I give my recovering from big injuries blorbo one of those?
I have seen Knives Out!
In fact, I did a whole post about it you can read here.
The thing in Harlan's arm was called a PICC, or Peripherally Inserted Central Catheter.
See, unlike in TV and most movies, when someone needs a medication given in a vein (called an intravenous medication), we don't just stick a needle into a vein- it has to go through some type of IV catheter.
An IV catheter (AKA a "peripheral venous catheter") is a thin plastic tube that goes through the skin and into a vein. The part sticking out of the skin can attach to a syringe to "push" medication into a vein, or be hooked up to a set of tubing and a bag of fluids or medication that has to go into the person over time.
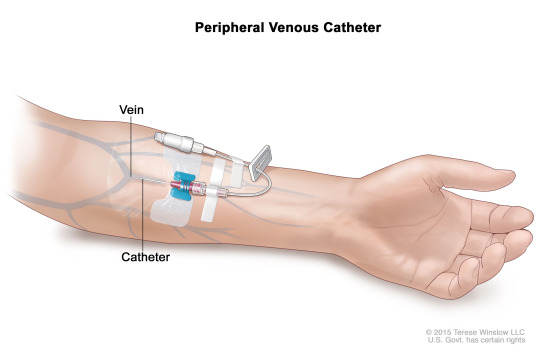
The kind of these you'd get in a typical hospital setting only last about 7 days max, though. So if you need an IV for longer periods (like, say, you need IV antibiotics or chemotherapy infusions over weeks or months), or you need medications that are really irritating to a vein (like total parenteral nutrition or a medication to raise blood pressure), or you have such bad veins that no one can put an IV in you and you're critically ill, you need what is called a central line instead.
There are several types of central lines. The kind Harlan has is a PICC- meaning a central line that is inserted into a peripheral part of the body (usually the upper arm) and goes into a really deep vein. The catheter (thin plastic tube) is much longer than a typical IV catheter, and actually goes all the way to the heart. It is then secured to the skin by stitches and a plastic film that is changed every 5 days or so.
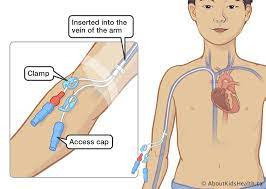

If your blorbo is in an ICU and can't keep his blood pressure up, or needs IV antibiotics to go home on, he might get a PICC or other central line. They do everything a regular IV does, plus they can take more irritating medications that would ruin peripheral IV catheters.
52 notes
·
View notes