#Bladder and bowel dysfunction
Explore tagged Tumblr posts
Text
#Stroke recovery#Physical disability#Motor impairments#Hemiparesis#Hemiplegia#Paralysis#Muscle weakness#Balance issues#Coordination problems#Spasticity#Contractures#Sensory loss#Speech difficulties#Dysphagia (swallowing difficulties)#Chronic pain#Fatigue#Cognitive impairments#Stroke rehabilitation#Neuroplasticity#Functional recovery#Stroke-related fatigue#Post-stroke depression#Stroke complications#Walking difficulties#Vision problems#Bladder and bowel dysfunction#Post-stroke care#health & fitness
5 notes
·
View notes
Note
How has wearing 24/7 affected your life? Like pros and cons
I’ll try to be as realistic as possible 😅
The pros are never having to use a public 🚻 restroom, being extra warm in the winter 🥶, the crazy amount of diapers that come in different prints 😍(now is the time to be alive for abdl as I’ve said), the wholesome community and friends that I absolutely cherish (this is the biggest), I feel like diapers have given me that hourglass figure 🥹 it’s a body shaper! It has helped me relax my bladder and which has helped pain I’ve experienced because of pelvic hip dysfunction. When I can get into little space diapers make that happen super fast! 💨 (haven’t been able to be vulnerable in awhile 💔) for reasons you already know. I feel like this list would be extended if I had a daddy to share the fun with 💕
The cons.. lol
I have developed some chicken skin around the area the plastic hits on my side, the secrecy bothers me and the anxiety of someone finding out🥴🫣, planning my bowel movements (I will cheat in some circumstances) I wonder if the plastic or chemicals in the diapers will cause cancer or anything else bad (this circulates in my own head), the stereotypes and flack we get for wearing diapers sucks. Finding clothing or items that make it discreet enough.
I might add to this more later 💞
250 notes
·
View notes
Text
another anti-psych post from your neighborhood patient-therapist
In my last post I talked about the kinds of basic needs people and communities have, and asked what it might look like in your community to meet those needs as a baseline. This time we're going to talk more about what happens when communities and individuals are chronically un-/under-served.
Okay so let's break it down this way. We're gonna try looking at just one medical symptom of chronic stress: autonomic dysregulation. It's not going to feel like we are, but I promise that's all we're doing. This is a *serious* symptom and it often comes clustered with others due to the way it functions within the body, which is why I think it is a useful case study here. Autonomic dysfunction, especially chronic dysfunction, can temporarily (though for long spans of time if the dysfunction remains chronic rather than acute) alter the functioning of other systems within the body such as the endocrine system, the reproductive system, cognitive functioning through the hippocampus and amygdala, and muscle functioning, nerve functioning, and others. It is no joke to suggest that long term autonomic dysfunction can often lead to major long term health consequences that are life altering for the person experiencing them. While some can be treated, managed, or even cured, not all can be and this is something I want us all to keep in mind as we consider the need for building communities that do not cause this kind of harm to their people.
Let's look at some potential medical outcomes of autonomic dysfunction, per the Mayo Clinic:
Dizziness and fainting when standing, caused by a sudden drop in blood pressure.
Urinary problems, such as difficulty starting urination, loss of bladder control, difficulty sensing a full bladder and inability to completely empty the bladder. Not being able to completely empty the bladder can lead to urinary tract infections.
Sexual difficulties, including problems achieving or maintaining an erection (erectile dysfunction) or ejaculation problems. In women, problems include vaginal dryness, low libido and difficulty reaching orgasm.
Difficulty digesting food, such as feeling full after a few bites of food, loss of appetite, diarrhea, constipation, abdominal bloating, nausea, vomiting, difficulty swallowing and heartburn. These problems are all due to changes in digestive function.
Inability to recognize low blood sugar (hypoglycemia), because the warning signals, such as getting shaky, aren't there.
Sweating problems, such as sweating too much or too little. These problems affect the ability to regulate body temperature.
Sluggish pupil reaction, making it difficult to adjust from light to dark and seeing well when driving at night.
Exercise intolerance, which can occur if your heart rate stays the same instead of adjusting to your activity level.
Some common comorbid conditions may include Diabetes, Polycystic Ovarian Syndrome, Parkinson's, Irritable Bowel Syndrome, or an autoimmune disorder. In each of these cases I want you to remember the lens of an individual body being denied, in some way, its base needs (an edocrine hormone, a nutritional component, the internal security of homeostasis, etc), to such an extent that it begins to experience an internal catastrophic failure, as this lens may often be supportive of accommodating your disabled comrades, or yourself, in the future.
I also want us to consider some common social statistics relevant to these conditions. Nearly 4% of the world experiences and autoimmune disorder. Most are women, and Indigenous, Black, and Latina women are at risk than most for several of these. In the United States, there are suspected to be 37.3 million people with diabetes. Diabetes is also considered an autoimmune disorder by researchers, and is one that the Indigenous, Filipino, Indian, Latine, and Black communities are all at higher risk for than white people are, however, risk is also heavily influenced by poverty, and by a family's location with respect to food deserts which grow more and more common. In a truly wild statistic, 80% of lesbians versus 32% of heterosexual women had polycystic ovaries in one study, and 33% of lesbians versus 14% of heterosexual women had progressed to PCOS. Some studies find that transmasculine folks are more likely to PCOS as well.
When we consider the marginalization these groups experience, and the way that marginalization plays out in the social forum, the political forum, in the financial forum, and in the emotional forum, are we really surprised to learn that it plays out in the embodied forum too?
This is what people mean when they talk about social murder. These are health conditions that don't just change lives, they end them. A system that churns out people so chronically sick that their bodies are desperately killing themselves trying to stay alive is a society that has become desperately sick. Diabetes is something we have attributed to individuals, to families, and even every once in a while to corporations, but at what point have we sat down and looked at a society that produces this murderous autoimmune disorder at such high rates and asked the real question: how are we making so many people sick?
The answers are many, and that can feel overwhelming, but I encourage you to start in one place and learn your way around it as well as you can before you even consider moving on. Maybe start with food deserts. They're probably familiar to you, you've heard about them in passing before I imagine, even if you're not really too into this stuff. But ask yourself WHY food deserts are able to exist? What are the mechanics of one being born? How does one stay free from the stain of a grocery store or food market? Are there any places like that near you? If so, what points of leverage might there be in that location for you to break the homeostasis of the food desert? How can you add your weight to efforts already occurring, or stir up sentiment around the idea of a new homeostasis where a grocery store exists? Can you put up flyers or attend town hall meetings? Can you knock doors or phone bank? Can you bring some sugar by your neighbors and comment how frustrating it is you all have to go so far to get your groceries and wonder what's up with that and maybe start scheming together? What kind of store should it be? Bring in a local market? A chain? Build a co-op or merchant's stalls for a four season farmer's market?
Get really into one idea, and get others in on it with you. I bet you aren't the only one who'd like a better status quo.
152 notes
·
View notes
Text
PROSTATE CANCER AWARENESS
Prostate cancer is one of the most common cancers in men, but detecting it early is a game changer.
I'll explain all you need to know about this condition in simple terms, I try to answer some famous questions you may have..
What is Prostate cancer?
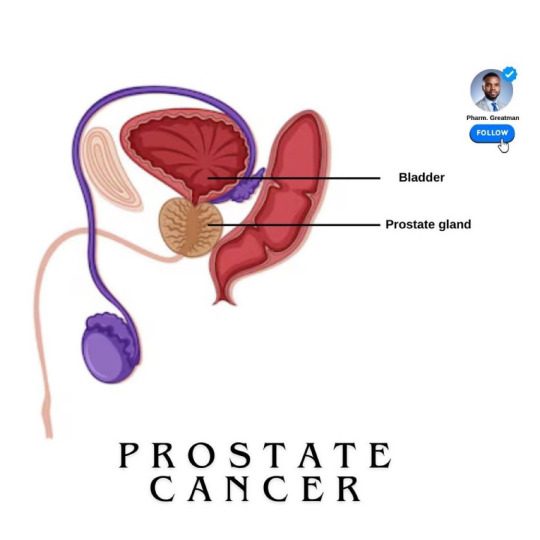
It is a type of cancer that begins in the prostate gland The prostate gland is part of the male reproductive system.
It is located below the bladder. This gland is responsible for producing the fluid that nourishes and transports sperm.
Prostate cancer is one of the most common cancers as they age.

What are the risk factors?
The exact cause of prostate cancer is unknown, but the risk factors are certain, they include:
- Age is a major risk factor for prostate cancer, with most cases occurring in men over 50.
- family history; as men with close relatives who had prostate cancer are at a higher risk. Having a father or brother with prostate cancer more than doubles a man’s risk of developing this disease.
- there are changes that could occur in your genes that can also increase your risk.
- men of African descent face an even greater risk and are more likely to be diagnosed at an advanced stage
A study showed that 1 in 4 black men will have prostate cancer in their lifetime, scary

Stages of Prostate cancer
Based on how far it has spread, it is classified into stages from stage I to IV
- Stage I is early and confined to the prostate, while Stage IV indicates the cancer has spread to other parts of the body, like the bones
Knowing the stage of cancer helps your doctor determine the best way to treat
Can regular sexual intercourse prevent prostate cancer, or prostate issues?
Important to state that “regular ejaculation alone is not a guaranteed preventive measure for prostate cancer”
Some studies suggested that regular ejaculation, whether through sex, masturbation, or nocturnal emissions, may reduce the risk of prostate cancer.
Research, including a notable study by Harvard University, found that men who ejaculated 21 or more times per month had a 20% lower risk of prostate cancer than those who ejaculated less frequently. The reasons are not fully understood, possibly that frequent ejaculation might help clear potential toxins or reduce inflammation in the prostate.
However, while this association exists, it’s still under investigation.
More evidence is needed… for example, a study in 2008 revealed that frequent sex in younger men increases prostate cancer risk compared to older men…

Stay active and monitor your health with Inspire 3, a tracker that supports prostate health by encouraging regular activity, reducing stress, improving sleep, and tracking key wellness metrics.
~~~~
Treatment Options
It depends on the stage of cancer and overall health. Options include:
- monitoring the cancer (active surveillance) - surgery to remove the prostate - radiation to destroy cancer cells - hormone therapy to reduce hormones that fuel cancer growth, and chemotherapy.
Treatments for prostate cancer can lead to side effects like difficulty controlling urine, erectile dysfunction, and bowel issues.
They must be communicated to patients beforehand
11 notes
·
View notes
Note
Do you have any information and/or resources on the link between Adult Autism and Bladder and/or Bowel Incontinence?
I was wondering because I feel like my Adult Autism which is high functioning has seemed to make me Incontinent and I’m not always aware when I have to go or when I am it is VERY VERY Urgent?
Hi there, I found some sources talking about this.
One article states:
* Relatively little is known about bladder and bowel dysfunction (BBD) among adults with autism spectrum disorder (ASD). The authors compared urinary incontinence, nocturnal enuresis, and bowel disturbances among 22 adults and 13 teenagers with ASD with a sample of typically developing (TD) controls. Urinary incontinence was present in 85% of children and 82% of adults with ASD versus just 5.7% of TD controls. Nocturnal enuresis, fecal incontinence, and constipation were also common, impacting 59%, 36%, and 68%, respectively, of adults with ASD (vs 0%, 0%, and 9%, respectively, of TD controls), and were similar to rates observed in teens with ASD.
* Intellectual disability and mood disorders were highly prevalent among those with BBD. It is not clear to what extent treatment of concomitant mood disorders results in a beneficial impact on BBD in this complex patient population.
Here are some more sources I found. It does talk about children, I think it can be helpful for adults/teens too.
I hope these sources can help. Many neurodivergent individuals have GI issues (me included, constapation suuucks).
Maybe my followers can give some more information and help with this? The only time I’ve experienced incontinece is after my seizures. I sometimes wet my bed…
Anyway, I hope this helps answer your question. I’m sure you not alone here, so I’m calling on my lovely followers to give advice and insight too.
I hope this helps answer your question. Thank you for the inbox. I hope you have a wonderful day/night. ♥️
29 notes
·
View notes
Text
By: Michael Searles
Published: May 26, 2024
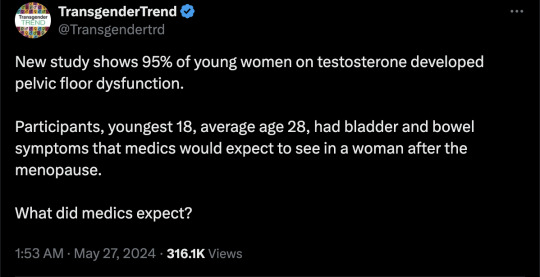
Transgender men are suffering from “postmenopausal” problems like incontinence in their 20s because of taking testosterone, a study has revealed.
Experts analysed 68 transgender men who were taking the cross-sex hormone to change their identity from female to male and found that 95 per cent had developed pelvic floor dysfunction.
The participants, who were as young as 18 and had an average age of 28, had bladder and bowel symptoms that medics would expect to see in a woman after the menopause.
Experts said the impact of the sex-changing drugs on bodily functions are under-researched and under-reported, with people “not being informed of the risks at gender clinics”.
Around 87 per cent of the participants had urinary symptoms such as incontinence, frequent toilet visits and bed-wetting, while 74 per cent had bowel issues including constipation or being unable to hold stools or wind in. Some 53 per cent suffered from sexual dysfunction.
The researchers said the rate of urinary incontinence, where urine unintentionally leaks, was around three times higher in transgender men than women, affecting around one in four compared to eight per cent of the general female population.
Other trans men suffered from frequent urinating including during the night, burning sensations, hesitancy, urgency and difficulty in going, while others had issues defecating.
Almost half had an “orgasm disorder”, while a quarter suffered from pain during sexual intercourse.
Experts warned that the drugs were putting young people on “exactly the same trajectory” as those going through the menopause. A third of the participants in the study were students.
Elaine Miller, a pelvic health physiotherapist and member of the Chartered Society of Physiotherapy, said: “A lot of women are absolutely fine until the menopause and then they start to get leaky. That appears to be exactly the same trajectory for female people who take cross-sex hormones, but there hasn’t been much in the way of research.”
She said she had worked with around 20 detransitioners who sought help for pelvic floor issues - and many more from around the world had been in touch - but that there was a “stigma” around incontinence and that people were “embarrassed” and minimised the issue.
“Wetting yourself is something that just is not socially acceptable, and it stops people from exercising, it stops them from having intimate relationships, it stops them from travelling, it has work impacts,” she said.
“The impact a bit of leaking has on these young people’s lives is huge. It really needs to be properly discussed within gender clinics because I would expect that almost 100 per cent of female people that take cross-sex hormones will end up with these problems,” she added, noting that the study was “robust” and probably underplayed the issue.
“It’s really sad when we hear people say, ‘nobody ever told me this’, and they should have been informed of the risks in gender clinics.”
The menopause causes a loss of muscle mass and body strength, which affects the pelvic floor and can cause incontinence.
Women who start the menopause early or prematurely, under the age of 45, should be offered Hormone Replacement Therapy (HRT) on the NHS because the oestrogen can help prevent the onset of conditions such as coronary heart disease, osteoporosis and dementia.
Taking testosterone may accelerate the menopausal process because it stops the ovaries from functioning and reduces the amount of oestrogen the body produces.
Testosterone is also known to affect muscle mass and hair loss, and has been linked to blood clots and gallstones, but there has been little research into pelvic floor issues and incontinence.
Ms Miller said the treatment for trans men was “the same as with any other postmenopausal female, which seems kind of ludicrous when you’re talking about people that are in their early 20s”.
“It’s making sure they are not constipated, getting them into a routine where they are not dehydrating themselves because they’re worried about having an accident. A lot of it is about bladder and bowel education about what is normal, and doing pelvic floor exercises, which can make a big difference,” she added.
Kate Barker, chief executive at the LGB Alliance, said the group had “consistently spoken out about the damage done by these experimental surgeries, the overwhelming majority of which are carried out on LGB [lesbian, gay and bisexual] people”.
“Our annual conference has heard testimony from detransitioners who live every day with the consequences of actions they took when they were very young - sometimes in their teens - including permanent sterilisation and loss of sexual function,” she said. “This has finally been officially confirmed by the Cass Review.”
The Cass Review saw the NHS stop prescribing puberty blockers outside of clinical trials and a pause to cross-sex hormones being given to under 18s. It called for more care to be given in the treatment of under 25s and the health service is reviewing adult clinics as a result.
The authors of the study, led by Lyvia Maria Bezerra da Silva at the Federal University of Pernambuco, Brazil, said the findings “showed a high frequency of at least one of the pelvic floor dysfunction symptoms” and that more research into the impact of testosterone was needed because the “long-term effects are still unknown”.
The research was published in the International Urogynecology Journal.
[ Via: https://archive.today/wNl3q ]

--
Abstract
Introduction and Hypothesis
The objective of this research is to explore the effects of hormone therapy using testosterone on pelvic floor dysfunction (PFD) in transgender men. We hypothesize that PFD might be prevalent among transgender men undergoing hormone therapy. Therefore, this study was aimed at verifying the frequency of these dysfunctions.
Methods
A cross-sectional study was conducted between September 2022 and March 2023 using an online questionnaire, which included transgender men over 18 years old who underwent gender-affirming hormone therapy. Volunteers with neurological disease, previous urogynecology surgery, active urinary tract infection, and individuals without access to the internet were excluded. The questionnaire employed validated tools to assess urinary symptoms, such as urinary incontinence (UI), as well as sexual dysfunction, anorectal symptoms, and constipation. The data were analyzed descriptively and presented as frequencies and prevalence ratios with their respective confidence intervals (95% CI), mean, and standard deviation.
Results
A total of 68 transgender men were included. Most participants had storage symptoms (69.1%), sexual dysfunction (52.9%), anorectal symptoms (45.6%), and flatal incontinence (39.7%). Participants with UI symptoms reported moderate severity of the condition.
Conclusions
Transgender men on hormone therapy have a high incidence of PFD (94.1%) and experience a greater occurrence of urinary symptoms (86.7%).
#Colin Wright#Transgender Trend#medical scandal#medical mutilation#medical malpractice#testosterone#exogenous testosterone#female biology#pelvic floor dysfunction#menopause#hormones#sex hormones#wrong sex hormones#cross sex hormones#urinary incontinence#incontinence#religion is a mental illness
6 notes
·
View notes
Text
Restore Balance and Strength: The Benefits of Pelvic Floor Physiotherapy
Pelvic floor physiotherapy is an often-overlooked but critical component of overall wellness. At Townline Physiotherapy in Abbotsford , we specialize in helping individuals restore balance, strength, and functionality to their pelvic floor muscles. Whether you're navigating postpartum recovery, addressing incontinence, or managing chronic pain, our expert team is here to guide you on your journey to better health.
Knowing the Pelvic Floor
The pelvic floor is a group of muscles at the bottom of the pelvis. These muscles are crucial in supporting pelvic organs, controlling bladder and bowel functions, and contributing to core stability. When these muscles become weak, tight, or dysfunctional, it can lead to a range of issues, including:
Urinary incontinence
Chronic pelvic pain
Pelvic organ prolapse
Pain during intercourse
Postpartum complications
Thankfully, pelvic floor physiotherapy presents specific treatments that could work wonders for these conditions.
Conditions We Treat Using Pelvic Floor Physiotherapy
We treat various conditions at Townline Physiotherapy in Abbotsford. Here are some examples:
Recovery After Childbirth: Giving birth puts a tremendous amount of pressure on the pelvic floor. Sometimes it can weaken or even tear the tissues. Pelvic floor physiotherapy assists in recovery of strength and function after delivery.
Urinary Incontinence: Leaking of urine when coughing, sneezing, laughing, or exercising is an all too common but perfectly treatable condition.
Pelvic Organ Prolapse: If the pelvic organs slip due to weak muscles, symptoms can be controlled and further advancement prevented by physiotherapy.
Chronic Pelvic Pain: Conditions like endometriosis or interstitial cystitis often accompany pelvic floor dysfunction, and specialized therapy can help alleviate.
Post-Surgical Rehabilitation: After surgeries such as hysterectomies or prostatectomies, pelvic floor physiotherapy helps in recovery and reduces complications.

What to Expect During a Pelvic Floor Physiotherapy Session
At Townline Physiotherapy, we ensure that your care is personalized and compassionate. Here's what you can expect:
Comprehensive Assessment: Our skilled physiotherapists conduct an in-depth evaluation, including a discussion of your medical history and physical assessment of pelvic floor function.
This customized treatment plan may include, but is not limited to, manual therapy, biofeedback, targeted exercises, and lifestyle modifications based on your unique needs.
We can provide you with education regarding proper posture, breathing techniques, and strategies to prevent such problems in the future.
Advantages of Pelvic Floor Physiotherapy
Pelvic floor physiotherapy will help you in gaining various benefits, such as:
Quality of Life Improved. Gain back your confidence and independence with issues like incontinence or pain.
Improved Physical Strength: Strengthening the pelvic floor contributes to better posture, stability, and overall fitness.
Faster Postpartum Recovery: New mothers can safely rebuild strength and function, improving their physical and emotional well-being.
Prevention of Future Problems: Early intervention can prevent conditions like prolapse or chronic pain from worsening over time.
Why Choose Townline Physiotherapy in Abbotsford?
At Townline Physiotherapy, our team is committed to providing you with exceptional care tailored to your needs. Here's what sets us apart:
Expertise: Our physiotherapists specialize in pelvic health and have extensive training in addressing a wide range of conditions.
State-of-the-Art Facility: We use advanced techniques and equipment to ensure optimal outcomes.
Compassionate Care: We prioritize your comfort and privacy, fostering a supportive and welcoming environment.
Take the First Step Towards Better Pelvic Health
Pelvic floor issues can severely impact your daily life, but they don't have to define it. With the right support and treatment, you can restore balance and strength, enhancing your overall well-being.
If you are seeking expert Pelvic Floor Physiotherapy in Abbotsford, contact Townline Physiotherapy today. Our team is ready to help you reclaim your health and vitality.
#physiotherapy in abbotsford#physiotherapy clinic in abbotsford#exercise#pelvic floor therapy#pelvic floor physical therapy#townline physiotherapy
3 notes
·
View notes
Text
situational/selective mutism list thing
Temperamental Inhibition
Social Anxiety Symptoms
Social Being: most have 'age-appropriate social skills'; some don't
Physical Symptoms: stomach, joints, head, chest etc. (will add the SM Throat Pain™)
Appearance: blank face, stiff body, freeze; some appear relaxed perhaps because sympathetic nervous response.
Emotional: depends on age/social acceptability of mutism
Developmental Delays: motor, communication, social (asd, pdd)
Sensory Integration Dysfunction (DSI)
Common symptoms: sensory problem, defiant behaviour, hesitant to respond, social withdrawal, focus on academics
Behavioural: maladaptive coping mechanisms, inflexible, moody, stubborn
Co-Morbid Anxieties
Social Engagement Difficulties
source: selective mutism pdf by Dr Elisa Shipon-Blum. elmtreeclinic
long long post with more detail. seriously very very long🌹🌹
1. Temperamental Inhibition: Timid, cautious in new and unfamiliar situations, restrained, usually evident from infancy on. Separation anxiety as a young child.
2. Social Anxiety Symptoms: Over 90% of children with Selective Mutism have social anxiety. Uncomfortable being introduced to people, teased or criticized, being the center of attention, bringing attention to himself/herself, perfectionist (afraid to make a mistake), shy bladder syndrome (Paruresis), eating issues (embarrassed to eat in front of others).
3. Social Being: The majority of children/teens with SM have age appropriate social skills and are on target developmentally, although some do not. Most children on the autism spectrum struggle with speech/language skills, social skills and have developmental challenges.
4. Physical Symptoms: MUTISM, tummy ache, nausea, vomiting, joint pains, headaches, chest pain, shortness of breath, diarrhea, nervous feelings, scared feelings.
5. Appearance: Many children with Selective Mutism have a frozen-looking, blank, expressionless face and stiff, awkward body language with lack of eye contact when feeling anxious. This is especially true for younger children in the beginning of the school year or then suddenly approached by an unfamiliar person. They often appear like an animal in the wild when they stand motionless with fear! The older the child, the less likely he/she is to exhibit stiff, frozen body language. Also, the more comfortable a child is in a setting, the less likely a child will look anxious. For example, the young child who is comfortable and adjusted in school, yet is mute, may seem relaxed, but mutism is still present. One hypothesis is that heightened sympathetic response causes muscle tension and vocal cord paralysis.
6. Emotional: When the child is young, he/she may not seem upset about mutism since peers are more accepting. As children age, inner turmoil often develops and they may develop the negative ramifications of untreated anxiety (see below).
7. Developmental Delays: A proportion of children with Selective Mutism have developmental delays. Some have multiple delays and have the diagnosis of an autistic spectrum disorder, such as Pervasive Developmental Disorder, or Autism. Delays include motor, communication and/or social development.
8. Sensory Integration Dysfunction (DSI) symptoms, Processing Difficulties/Delays: For many children with SM, sensory processing difficulties are the underlying reason for being 'shut down' and their mutism. In larger, more crowded environments where multiple stimuli are present (such as the classroom setting), where the child feels an expectation, sensory modulation specifically, sensory defensiveness exists. Anxiety is created causing a 'freeze' mode to take place. The ultimate 'freeze mode' is MUTISM.
9. Common symptoms: Picky eater, bowel and bladder issues, sensitive to crowds, lights (hands over eyes, avoids bright lights), sounds (dislikes loud sounds, hands over ears, comments that it seems loud), touch (being bumped by others, hair brushing, tags, socks, etc), and heightened senses, i.e., perceptive, sensitive, Self-regulation difficulties (act outing, defiant, disobedient, easily frustrated, stubborn, inflexible, etc).
10. Common symptoms within a classroom environment: Withdrawal, playing alone or not playing at all, hesitation in responding (even nonverbally), distractibility, difficulty following a series of directions or staying on task, difficulty completing tasks. Experience at the Smart Center dictates that sensory processing difficulties may or may not cause learning or academic difficulties. Many children, especially, highly intelligent children can compensate academically and actually do quite well. MANY focus on their academic skills, often leaving behind 'the social interaction' within school. This tends to be more obvious as the child ages. What is crucial to understand is that many of these symptoms may NOT exist in a comfortable and predictable setting, such as at home. In some children, there are processing problems, such as auditory processing disorder, that cause learning issues as well as heightened stress.
11. Behavioral: Children with Selective Mutism are often inflexible and stubborn, moody, bossy, assertive and domineering at home. They may also exhibit dramatic mood swings, crying spells, withdrawal, avoidance, denial, and procrastination. These children have a need for inner control, order and structure, and may resist change or have difficulty with transitions. Some children may act silly or act out negatively in school, parties, in front of family and friends. WHY? These children have developed maladaptive coping mechanisms to combat their anxiety.
12. Co-Morbid Anxieties: Separation anxiety, Obsessive Compulsive Disorder (OCD), hoarding, Trichotillomania (hair pulling, skin picking), Generalized Anxiety Disorder, Specific phobias, Panic Disorder.
13. Communication Difficulties: Some children may have difficulty responding nonverbally to others, i.e., cannot point/nod in response to a teachers question, or indicate thank you by mouthing words. For many, waving hello/goodbye is extremely difficult. However, this is situational. This same child can not only respond nonverbally when comfortable, but can chatter nonstop! Some children may have difficulty initiating nonverbally when anxious, i.e., have difficulty or are unable to initiate play with peers or go up to a teacher to indicate need or want.
14. Social Engagement Difficulties: When one truly examines the characteristics of a child with Selective Mutism, it is obvious that many are unable to socially engage properly. When confronted by a stranger or less familiar individual, a child may withdraw, avoid eye contact, and 'shut down,' not only leaving a child speechless but preventing him/her from engaging with another individual. Greeting others, initiating needs and wants, etc., are often impossible for many children. Many shadow their parents in social environments often avoiding any social interaction at all. The common example given is; 'A child in grocery story can sing, laugh and talk loudly, but as soon as someone confronts him/her, the child freezes, avoids and withdraws from social interaction. As the child ages, freezing and shutting down rarely exist, but the child remains either noncommunicative or will respond nonverbally after an indeterminate amount of warm up time.
source: selective mutism pdf by Dr Elisa Shipon-Blum. elmtreeclinic
#situational mutism#selective mutism#mentalheathawareness#sensory processing#communication#sm tag#chaos-exhausted
24 notes
·
View notes
Text
Dabi’s somatic nervous system was damaged. It’s why he can’t feel pain and likely he struggles to feel the thing she touches.
With this comes muscle spasms and twitches from the loss of control of the SNS. His muscle probably randomly spasm when he’s just chillin. (But it seems like Dabi’s damage is more leaning toward the sensory nerves rather than the motor nerves).
Other symptoms that dabi may suffer from because the the sensory nerve damage: Muscle weakness, shakiness, numbness, sexual dysfunction, bladder and bowel dysfunction.
#bnha#my hero academia#boku no hero academia#mha#luuuuzers.thoughts#my hero headcanons#dabi#touya todoroki
18 notes
·
View notes
Text
youtube
URINE TROUBLE because of your POOP?! | How to get rid of constipation ft. Dr. Kumkum Patel | IG Live What is constipation exactly? And how does it occur? How can it affect you and your urine? We answer these questions and more, in this November Bladder Health Month Instagram Live! Make sure you follow me in Instagram so you won't miss out on these IG LIVEs where I collaborate with other doctors specializing in other parts of the body and how those parts interact with the Urinary System! https://ift.tt/AxikcFL Also, don't forget to check out Dr. Kumkum Patel's Instagram: https://ift.tt/uAWF5It Thanks for watching!! Schedule an appointment: https://ift.tt/0AeqDnB Become a premium member: https://ift.tt/Q2YI98n Come back EVERY MONDAY for a NEW video Buy your very own Take Care of Yourself water bottle or coffee mug: https://www.youtube.com/@RenaMalikMD/... Design by Ben Precup https://ift.tt/g0SeiOw https://ift.tt/wRuGyFs Timestamps 0:00 Introduction 1:09 How constipation affects bladder function 2:07 What is constipation? 3:39 How to get rid of constipation? 4:26 How pelvic floor dysfunction affects your bladder and bowels 6:02 When do you do a colonoscopy for constipation? 6:40 What is anorectal manometry? 8:53 What laxatives do you recommend? 10:06 How much fiber do you need? 12:46 How do you manage children with constipation? 14:17 What if you can't afford pelvic floor physical therapy? 15:20 Not everyone should do kegel exercises! 15:49 What about ginger and peppermint oil for hard stools? 16:17 When should you see a gastroenterologist? Subscribe: https://www.youtube.com/c/RenaMalikMD/?sub_confirmation=1 Share this video with a friend: https://youtu.be/wLd6zBqE_2M ------------------------------------------------------ Check out these Playlists: Penis Problems?! Erectile Dysfunction, Premature Ejaculation & More: https://bit.ly/3wwivzS Overactive Bladder Treatment: https://bit.ly/3hMzBoP How to Increase Testosterone: https://bit.ly/2T9QJKV All my REACTION videos: https://youtu.be/_Dl46d7I1uI Reacting to Grey's Anatomy: https://youtu.be/LiDevzHnoos ------------------------------------------------------ DOWNLOAD YOUR LIST OF BLADDER IRRITANTS https://ift.tt/fGckwPs ----------------------------------------------------- Check out my Amazon storefront (affiliate links included): https://ift.tt/eCBmuLs Coupons & Discount codes (affiliate links included): https://ift.tt/03AgKwC ----------------------------------------------------- Let's Connect!: WEBSITE: https://ift.tt/N9T7Ueq I INSTAGRAM: @RenaMalikMD https://ift.tt/lA8GiFB TWITTER: @RenaMalikMD http://twitter.com/RenaMalikMD FACEBOOK: @RenaMalikMD https://ift.tt/YsPbkVZ LINKEDIN: https://ift.tt/LJA4KBY PINTEREST: https://ift.tt/TtlU9ma ------------------------------------------------------ DISCLAIMER: This video is purely educational and does not constitute medical advice. The content of this video is my personal opinion and not that of my employer(s). Use of this information is at your own risk. Rena Malik, M.D. will not assume any liability for any direct or indirect losses or damages that may result from the use of the information contained in this video including but not limited to economic loss, injury, illness, or via YouTube https://www.youtube.com/watch?v=wLd6zBqE_2M
4 notes
·
View notes
Text
Physical Therapy Clinic in New York City
Ehlers-Danlos Syndrome - Fatigue
Fatigue is particularly common in hypermobile EDS (hEDS). Contributing factors can include sleep disorders, muscle deconditioning (loss of muscle tone and endurance), headaches, and nutritional deficiencies. It is important to exclude other causes, such as anemia or a chronic infection.
The primary cause of EDS is related to defects in the synthesis, structure, or processing of collagen or other components of the extracellular matrix, which are essential for providing strength, support, and elasticity to various tissues, including skin, joints, blood vessels, and organs.
Can EDS cause extreme fatigue?
Conditions commonly seen in EDS and which may manifest as or exacerbate fatigue include sleep disorder, chronic pain, deconditioning, cardiovascular dysregulation, bowel and bladder dysfunction, psychological issues, and nutritional deficiencies. Feb 10, 2017
EDS is generally classified into several major types, including:
Classical EDS (cEDS): Caused by mutations in the COL5A1 or COL5A2 genes, leading to abnormalities in Type V collagen.
Hypermobile EDS (hEDS): This type is associated with hypermobility of joints and is believed to have a genetic component, although the specific gene mutations are not well-defined.
Vascular EDS (vEDS): Caused by mutations in the COL3A1 gene, leading to abnormalities in Type III collagen. vEDS is the most severe form of EDS and is associated with a high risk of arterial and organ rupture.
Kyphoscoliotic EDS (kEDS): Caused by PLOD1 or FKBP14 gene mutations, leading to collagen processing abnormalities.
Arthrochalasia EDS (aEDS): Caused by mutations in the COL1A1 or COL1A2 genes, leading to abnormalities in Type I collagen.
Dermatosparaxis EDS (dEDS): Caused by mutations in the ADAMTS2 gene, leading to abnormalities in the processing of collagen.
The genetic mutations in EDS result in weakened or structurally abnormal connective tissues, leading to the various symptoms and manifestations of the syndrome, including joint hypermobility, skin hyperextensibility, and vascular and organ problems.
Fatigue is a common symptom in individuals with EDS. While its exact cause is not fully understood, it likely results from a combination of factors, including chronic pain, poor sleep quality due to pain and joint instability, autonomic dysfunction, and the challenges of living with a chronic condition. Fatigue can significantly impact the quality of life for individuals with Ehlers-Danlos Syndrome, and its management is an essential aspect of their overall care.
Fatigue is a state of extreme tiredness, weariness, or lack of energy. It is a normal and common sensation that most people experience occasionally, especially after physical or mental exertion, lack of sleep, or periods of stress. However, when fatigue becomes chronic and persistent, lasting for an extended period despite adequate rest and sleep, it may indicate an underlying medical condition or other factors that require attention.
Fatigue can manifest in various ways, and its symptoms can include:
Physical tiredness: Feeling physically weak, heavy, or drained of energy.
Mental exhaustion: Difficulty concentrating, memory problems, or impaired cognitive function.
Sleep disturbances: Fatigue can disrupt sleep patterns, leading to difficulty falling asleep or staying asleep.
Reduced motivation: A lack of interest in activities and reduced productivity.
Irritability: Feeling easily annoyed or impatient.
Muscle weakness: Physical weakness or difficulty performing usual tasks.
Headache: Frequent headaches or migraines.
Dizziness: Feeling lightheaded or dizzy.
Slowed reflexes: Reduced reaction time and impaired coordination.
Mood changes: Fatigue can lead to feelings of sadness, anxiety, or depression.
Causes of fatigue can be numerous and may include:
Lack of sleep: Insufficient or poor-quality sleep can lead to fatigue.
Medical conditions: Chronic fatigue can be a symptom of various medical conditions, such as anemia, thyroid disorders, chronic pain, infections, and autoimmune diseases.
Psychological factors: Mental health issues like stress, anxiety, and depression can contribute to fatigue.
Medications: Certain medications may cause fatigue as a side effect.
Lifestyle factors: Poor nutrition, lack of physical activity, and excessive alcohol or caffeine consumption can contribute to fatigue.
Chronic illnesses: Conditions like fibromyalgia, chronic fatigue syndrome (CFS), and some autoimmune disorders can cause persistent fatigue.
It's important to differentiate between normal fatigue, which typically improves with rest and self-care, and chronic fatigue, which can be a symptom of an underlying health issue that requires medical attention. If you experience persistent fatigue or if it significantly interferes with your daily activities, discussing it with a healthcare professional to identify any underlying causes and receive appropriate evaluation and treatment is essential.
#physical health#physical therapy#ehlers danlos syndrome physical therapy#ehlers danlos syndrome#hypermobile ehlers danlos#back pain#chronic fatigue#chronically fatigued#health#health and wellness
3 notes
·
View notes
Text

𝑪𝒆𝒓𝒗𝒊𝒄𝒂𝒍 𝒔𝒑𝒐𝒏𝒅𝒚𝒍𝒐𝒔𝒊𝒔 𝒊𝒔 𝒂 𝒄𝒐𝒎𝒎𝒐𝒏 𝒄𝒐𝒏𝒅𝒊𝒕𝒊𝒐𝒏 𝒕𝒉𝒂𝒕 𝒂𝒇𝒇𝒆𝒄𝒕𝒔 𝒕𝒉𝒆 𝒄𝒆𝒓𝒗𝒊𝒄𝒂𝒍 𝒔𝒑𝒊𝒏𝒆 (𝒏𝒆𝒄𝒌 𝒓𝒆𝒈𝒊𝒐𝒏) 𝒂𝒏𝒅 𝒊𝒔 𝒄𝒉𝒂𝒓𝒂𝒄𝒕𝒆𝒓𝒊𝒛𝒆𝒅 𝒃𝒚 𝒕𝒉𝒆 𝒅𝒆𝒈𝒆𝒏𝒆𝒓𝒂𝒕𝒊𝒐𝒏 𝒐𝒇 𝒕𝒉𝒆 𝒗𝒆𝒓𝒕𝒆𝒃𝒓𝒂𝒆 𝒂𝒏𝒅 𝒊𝒏𝒕𝒆𝒓𝒗𝒆𝒓𝒕𝒆𝒃𝒓𝒂𝒍 𝒅𝒊𝒔𝒄𝒔. 𝑷𝒉𝒚𝒔𝒊𝒐𝒕𝒉𝒆𝒓𝒂𝒑𝒚 𝒑𝒍𝒂𝒚𝒔 𝒂 𝒔𝒊𝒈𝒏𝒊𝒇𝒊𝒄𝒂𝒏𝒕 𝒓𝒐𝒍𝒆 𝒊𝒏 𝒎𝒂𝒏𝒂𝒈𝒊𝒏𝒈 𝒂𝒏𝒅 𝒕𝒓𝒆𝒂𝒕𝒊𝒏𝒈 𝒄𝒆𝒓𝒗𝒊𝒄𝒂𝒍 𝒔𝒑𝒐𝒏𝒅𝒚𝒍𝒐𝒔𝒊𝒔.
𝑯𝒆𝒓𝒆 𝒂𝒓𝒆 𝒔𝒐𝒎𝒆 𝒄𝒐𝒎𝒎𝒐𝒏 𝒔𝒚𝒎𝒑𝒕𝒐𝒎𝒔 𝒂𝒔𝒔𝒐𝒄𝒊𝒂𝒕𝒆𝒅 𝒘𝒊𝒕𝒉 𝒍𝒖𝒎𝒃𝒂𝒓 𝒔𝒑𝒐𝒏𝒅𝒚𝒍𝒐𝒔𝒊𝒔: 1. Neck Pain 2. Stiffness 3. Headaches 4. Reduced Range of Motion 5. Numbness and Tingling 6. Muscle Weakness 7. Balance Issues 8. Bladder or Bowel Dysfunction 9. Radiating Pain 10. Muscle Spasms
𝑻𝒉𝒆𝒔𝒆 𝒂𝒓𝒆 𝒕𝒉𝒆 𝒏𝒐𝒓𝒎𝒂𝒍 𝒑𝒉𝒚𝒔𝒊𝒐𝒕𝒉𝒆𝒓𝒂𝒑𝒚 𝒕𝒓𝒆𝒂𝒕𝒎𝒆𝒏𝒕𝒔 𝒇𝒐𝒓 𝒍𝒖𝒎𝒃𝒂𝒓 𝒔𝒑𝒐𝒏𝒅𝒚𝒍𝒐𝒔𝒊𝒔: 1. Pain Management 2. Neck Exercises 3. Posture Correction 4. Manual Therapy 5. Stretching Exercises 6. Strengthening Exercises 7. Education and Lifestyle Modifications 8. Use of Devices 9. Traction
#physiotherapy#lucknow#fasanakabir#physicaltherapy#painrelief#healing#exercise#physicalpain#treatment#medication#spondylosis#stiff neck
2 notes
·
View notes
Text
I don't know if this is gonna be my last "post" for awhile on my Tumblr blog that nobody reads lol.
But life has been a lot lately whether I am awake or asleep, everything seems surreal.
I try to focus on the good, but a lot has happened and I haven't opened up much about it, but (luckily it isn't fatal) but I have been dealing with multiple issues (some diagnosed, some undiagnosed) such as - chronic infections, Interstitial Cystitis, Pelvic Floor Dysfunction, Asthma, Acid Reflux, Irritable bowels, and headaches (for my physical issues) which cause kidney pain at times, muscular pain, sometimes (luckily it's rare now) an insane urge to use the bathroom (but no UTI) and small parts of my bladder lining actually shedding in the toilet..bladder pain, etc. (you get the point) since I was 17 (and finally done with being homebound and bedbound from the pain when I was 18 1/2 to 19 and getting my GED as well as working at that time period with no help from doctors). I also struggle with mental issues such as - Bipolar 2, Depression, Anxiety, CPTSD, OCD, and ADHD. (and possibly even more issues)..Life has been a difficult journey (the most difficult being the Bipolar and the Interstitial Cystitis), but they are ALL difficult nonetheless and coping has been hard but I am trying each and every day and that's what matters. (Luckily the insane urge to use the bathroom has went away mostly too, but it still comes back every so often when I am "flaring" with no UTI, just pain .. but I just try and stay positive, looking forward and soaking in the good days.
2 notes
·
View notes
Text
Pelvic Floor Physiotherapy Calgary: A Proven Solution for Women’s Health, Incontinence, and Core Strength

Women’s health encompasses a wide range of physical, emotional, and social factors that evolve over a lifetime. From puberty and pregnancy to menopause and beyond, women face unique physiological changes that can significantly impact their well-being. Among the most under-discussed yet critically important aspects of women’s health is pelvic floor function. Despite being foundational to core stability, bladder control, sexual function, and even posture, the pelvic floor is often overlooked—until a problem arises.
Pelvic floor dysfunction is remarkably common, affecting millions of women globally. Issues such as urinary incontinence, pelvic organ prolapse, painful intercourse, and postpartum recovery challenges can all stem from a weakened or overly tight pelvic floor. Fortunately, awareness is growing, and so is access to effective treatment.
That’s where pelvic floor physiotherapy Calgary comes into play. With its evidence-based, personalized approach, pelvic floor physiotherapy has emerged as a frontline solution for women looking to regain control, comfort, and confidence. In Calgary, a growing number of physiotherapy clinics are specializing in pelvic health, helping women of all ages restore function and enjoy a higher quality of life.
What Is the Pelvic Floor?
The pelvic floor is a group of muscles, ligaments, and connective tissues that span the bottom of the pelvis. These muscles support the bladder, uterus, and rectum, much like a hammock. In women, the pelvic floor has the added responsibility of accommodating childbirth and hormonal changes throughout life.
Functions of the pelvic floor include:
Supporting pelvic organs
Maintaining continence (urine and feces)
Stabilizing the core
Aiding in sexual sensation and function
Supporting spinal and pelvic alignment
When these muscles are too weak, tight, or uncoordinated, it can lead to a range of symptoms—from minor discomfort to debilitating dysfunction.
Common Signs of Pelvic Floor Dysfunction
Many women silently endure symptoms that could be significantly improved—or even eliminated—through pelvic floor physiotherapy. Some common signs include:
Leaking urine when sneezing, coughing, or laughing (stress incontinence)
Sudden, intense urge to urinate (urge incontinence)
Frequent urination or waking at night to go to the bathroom
Pelvic pressure or a feeling of heaviness (possible prolapse)
Pain during intercourse
Difficulty fully emptying the bladder or bowel
Lower back, hip, or groin pain with no clear cause
If any of these symptoms sound familiar, know that you're not alone—and that help is available.
What Is Pelvic Floor Physiotherapy?
Pelvic floor physiotherapy is a specialized branch of physical therapy focused on assessing and treating issues related to the pelvic floor muscles. Practitioners are trained to address both hypertonic (tight) and hypotonic (weak) pelvic floor conditions using a variety of techniques, including:
Manual therapy (external and internal techniques)
Biofeedback
Breathing and relaxation training
Postural education
Pelvic floor and core strengthening
Stretching and mobility exercises
Education on bladder and bowel habits
In pelvic floor physiotherapy Calgary, licensed professionals create customized treatment plans based on each individual’s anatomy, lifestyle, and goals.
Why Is Pelvic Floor Physiotherapy Important for Women’s Health?
1. Pregnancy and Postpartum Recovery
Pregnancy and childbirth put enormous stress on the pelvic floor. Hormonal changes, increased abdominal pressure, and the physical trauma of vaginal delivery can lead to muscle weakness, tearing, or nerve damage.
Pelvic floor physiotherapy during and after pregnancy helps:
Prevent or reduce incontinence
Promote faster postpartum recovery
Improve core strength and posture
Reduce pelvic and low back pain
Address scar tissue from C-sections or episiotomies
Safely return to exercise
Calgary-based clinics often work in tandem with midwives, obstetricians, and doulas to support holistic maternal care.
2. Managing Urinary and Fecal Incontinence
Incontinence can be embarrassing and isolating, but it’s more common than many realize. One in three women experiences urinary incontinence at some point in their lives. Physiotherapy offers a non-surgical, medication-free option for regaining bladder control.
A pelvic floor physiotherapist can teach clients how to:
Properly engage and strengthen pelvic floor muscles
Identify and correct faulty bladder habits
Use biofeedback to improve awareness and coordination
Implement behavioral strategies like timed voiding
With consistent therapy, many women see a dramatic reduction in leakage episodes and a boost in confidence.
3. Pelvic Organ Prolapse Support
Pelvic organ prolapse occurs when one or more pelvic organs descend into the vaginal canal due to weakened support structures. Symptoms may include pressure, bulging, or a sensation of something “falling out.”
While severe cases may require surgery, mild-to-moderate prolapse can often be managed through physiotherapy. Strengthening the pelvic floor can improve support and reduce symptoms, helping women avoid or delay surgery.
4. Pain and Sexual Health
Painful intercourse (dyspareunia), vaginismus, and pelvic pain syndromes can be rooted in tight, overactive pelvic floor muscles. In these cases, strengthening exercises alone may not be appropriate. Instead, therapy focuses on:
Relaxation techniques
Internal manual therapy to release muscle tension
Stretching and breathing exercises
Desensitization techniques
Education on anatomy and safe movement patterns
Women in Calgary seeking pelvic floor therapy for pain relief often report improved intimacy, reduced anxiety, and a better understanding of their bodies.
5. Core Stability and Back Pain
The pelvic floor works in coordination with the diaphragm, abdominal muscles, and lower back muscles to create a stable core. Dysfunction in one part of this system can affect the others.
Pelvic floor physiotherapists assess core integration and help retrain muscle coordination, leading to:
Better posture
Improved athletic performance
Reduced risk of injury
Relief from chronic back or pelvic pain
What to Expect During a Session
If you’ve never seen a pelvic floor physiotherapist, it’s normal to feel nervous. A typical first appointment in pelvic floor physiotherapy Calgary clinics includes:
Detailed History: The physiotherapist will ask about symptoms, lifestyle, childbirth history, bladder and bowel habits, and goals.
External Examination: Assessment of posture, breathing, core engagement, and general movement patterns.
Internal Examination (with consent): This may be conducted vaginally to assess pelvic floor muscle tone, strength, endurance, and coordination.
Education: The therapist explains the findings and outlines a personalized treatment plan.
Initial Exercises or Manual Techniques: These may include relaxation, core training, or biofeedback-based work.
Sessions are private, professional, and respectful. Clients are encouraged to ask questions and go at their own pace.
Who Can Benefit from Pelvic Floor Physiotherapy?
Pelvic floor physiotherapy is beneficial at every stage of life. In Calgary, women seek care for a variety of reasons, including:
Teenagers with early signs of dysfunction (e.g., leakage during sports)
Pregnant women preparing for labor or experiencing pain
New moms recovering from birth or C-sections
Perimenopausal and menopausal women facing hormonal shifts and increased risk of incontinence or prolapse
Athletes wanting to optimize core stability and prevent injury
Post-surgical patients recovering from hysterectomy or other procedures
Even women with no current symptoms can benefit from pelvic health education to maintain long-term well-being.
Why Choose Pelvic Floor Physiotherapy in Calgary?
Calgary is home to a growing network of pelvic health specialists who combine clinical expertise with compassion. Reasons to choose pelvic floor physiotherapy Calgary include:
Access to certified pelvic health physiotherapists
Multidisciplinary care (collaborations with OB-GYNs, urologists, dietitians)
Clinics offering direct billing and flexible hours
Tailored programs for different stages of life
Emphasis on client education and empowerment
Whether you live in downtown Calgary, the suburbs, or the surrounding communities, there are clinics nearby offering comprehensive pelvic floor care.
Addressing Myths and Stigma
Unfortunately, pelvic floor issues are still surrounded by stigma. Many women believe:
“It’s normal to leak after childbirth.”
“Pain during sex is just something you live with.”
“Surgery is the only option for prolapse.”
“Kegels are enough.”
Pelvic floor physiotherapy challenges these myths with facts, science, and empathy. It teaches women to reconnect with their bodies, understand their symptoms, and take control of their health.
Long-Term Benefits
The results of pelvic floor physiotherapy often extend beyond symptom relief. Long-term benefits include:
Better quality of life
Increased physical activity
Improved mental and emotional health
Enhanced self-image
Greater independence in aging
Many women report feeling empowered and reassured after treatment, knowing they have the tools and knowledge to manage their pelvic health throughout life.
Final Thoughts: Your Health, Your Power
Pelvic floor issues may be common, but they are not something women have to live with. With early assessment and tailored treatment, it’s possible to regain strength, function, and freedom. Whether you're healing postpartum, managing incontinence, or seeking better core control, pelvic floor physiotherapy offers a path to healing and empowerment.
Pelvic floor physiotherapy Calgary provides a professional, evidence-based solution for women who are ready to invest in their health. Through compassionate care and personalized treatment plans, Calgary’s pelvic health specialists are changing lives—one muscle, one breath, one movement at a time.
0 notes
Text
The Hidden Connection: How Pelvic Floor Health Impacts Core Strength

When most people think of core training, they picture crunches, planks, or sculpted abs. But there's a key player in core strength that often gets overlooked — the pelvic floor. This deep group of muscles is not only essential for bladder control and organ support, but it also plays a critical role in core stability. Understanding the link between pelvic floor health and core strength can unlock a new level of functional fitness, injury prevention, and total-body wellbeing.
What Is the Pelvic Floor?
The pelvic floor is a group of muscles and connective tissue that form a hammock-like structure at the base of the pelvis. These muscles support the bladder, uterus (in women), rectum, and prostate (in men). They are essential for controlling urination, bowel movements, and sexual function.
When the pelvic floor is strong and functioning well, it supports your internal organs and contributes to good posture and core engagement. However, when it's weak or imbalanced, it can lead to problems like urinary incontinence, pelvic pain, and even back issues.
Understanding the Core: It’s More Than Abs
Your “core” is more than your six-pack muscles. It includes:
Transverse abdominis (TVA) – the deepest layer of abdominal muscles.
Multifidus – small muscles along your spine.
Diaphragm – the primary muscle for breathing.
Pelvic floor – the base of your core unit.
These muscles work together to stabilize your trunk, protect your spine, and transfer force between your upper and lower body. A well-functioning core enhances balance, coordination, and power — all without a single crunch.
How the Pelvic Floor and Core Work Together
The pelvic floor and the deep core muscles are part of a pressure system called the “core canister”. At the top is the diaphragm, the pelvic floor forms the bottom, and the abdominal and back muscles wrap around like a corset.
When you inhale, the diaphragm contracts and pushes pressure down. The pelvic floor lengthens in response. When you exhale or lift something heavy, the pelvic floor contracts, and so do the deep core muscles — bracing and supporting your spine.
In other words, a strong core starts from the inside out — and from the bottom up.
Signs of Dysfunction: When One Area Affects the Other
If your pelvic floor or core is out of sync, you may notice:
Pelvic floor dysfunction: leaking urine when you sneeze or jump, a sensation of heaviness or pressure in the pelvis, pain during intimacy.
Core dysfunction: chronic back pain, poor posture, difficulty with balance or stability exercises.
Ignoring one area can lead to a domino effect. For example, if your pelvic floor is weak, your body might overcompensate with your abdominals, leading to tightness and back pain.
The Benefits of Training Both Together
By addressing both the pelvic floor and the deep core together, you can:
Improve posture and spinal support
Enhance athletic performance and movement efficiency
Reduce risk of injury, especially to the lower back
Manage or prevent urinary incontinence
Support better recovery post-pregnancy or surgery
Whether you're an athlete, new mom, or simply looking to move better, training this connection brings major payoff.
Top Exercises for Pelvic Floor and Core Synergy
Here are a few exercises that activate both systems together:
Diaphragmatic Breathing
Lie on your back with knees bent. Inhale deeply into your belly. Feel your ribs and belly expand, and your pelvic floor lengthen.
Exhale slowly, gently lifting the pelvic floor and drawing your belly button in.
Pelvic Floor Contractions (Kegels)
Gently squeeze and lift the muscles as if trying to stop the flow of urine. Avoid tightening the abs, thighs, or glutes.
Dead Bug (with pelvic floor engagement)
On your back, arms and legs in tabletop. As you lower opposite arm and leg, exhale, engage your core and lift the pelvic floor.
Bridge with Pelvic Tilt
As you lift your hips into a bridge, focus on gently lifting your pelvic floor and engaging your glutes and abs together.
These moves are subtle but powerful — focus on control, not speed.
Daily Life Integration Tips
Strengthening these muscles isn't limited to workouts. You can support this connection during:
Lifting groceries or kids – Exhale and engage your core/pelvic floor before lifting.
Standing or sitting – Think tall, avoid slouching, and gently engage your lower belly.
Walking – Practice rhythmic breathing and awareness of pelvic alignment.
Avoid holding your breath, clenching your abs all day, or constantly doing Kegels. It’s all about balance.
When to Seek Professional Support
If you’re dealing with chronic pain, incontinence, or are unsure how to properly activate your pelvic floor, consider working with a pelvic floor physical therapist. These specialists offer personalized assessments and can teach you how to connect your breath, pelvic floor, and core safely and effectively.
This is especially helpful:
Postpartum (even years later)
After abdominal or pelvic surgery
If symptoms persist despite exercise
Conclusion: Strong from the Inside Out
The pelvic floor is not just a niche muscle group — it’s a foundational part of your core strength and overall function. By tuning into this often-ignored connection, you can build stability, prevent injury, and feel stronger and more confident in everyday life.
Start small: Try diaphragmatic breathing today. From there, work your way toward a stronger, more connected core — from the inside out.
#theragurus#pelvic floor therapy#The Hidden Connection: How Pelvic Floor Health Impacts Core Strength
0 notes
