#Genetic Associations With Anxiety and Depression
Explore tagged Tumblr posts
Text
Critical Thinking in Witchcraft and Spirituality: Some Logical Fallacies You Might Find
Ad Hominem: Asserting that something is true or false depending on its source. If someone claimed that gravity obviously isn't real because it came from Isaac Newton, an occultist, that would be an Ad Hominem attack.
Appeal to Anecdotal Evidence: It's not that anecdotes can't contain meaningful information, per se. It's that anecdotes don't always tell the whole story, and they aren't inherently trustworthy - consider all of the people who said they were beaten as kids and grew up just fine. Likewise, if someone tells you that they recovered from cancer after filling their room with crystals and meditating regularly, it doesn't inherently suggest that crystals and meditation cured their cancer. This person might have experienced spontaneous remission.
Appeal to Common Belief: When someone claims that a thing must be true (or is especially likely to be true) because many people believe in it. For example, "many people believe Earth has been visited by extraterrestrials in ancient times, there must be something to it." In reality, the reason many people believe this is because there is a proliferation of media that claims it happened.
Appeal to Emotion: When someone argues that the way a thing makes you feel is essentially evidence for or against it. An example of this are spiritual leaders/guides who tell you that you can discern truth by asking yourself whether it makes you feel good and uplifted, or whether it makes you feel fearful or angry. In reality, cult leaders often engage in practices that manipulate people's emotions, effectively conditioning them to associate certain feelings with whatever they want. This isn't to say that your feelings are unimportant and you should never listen to them, but you should always apply critical thinking before making any big decisions or deciding what you should believe.
Another form of this fallacy is assuming that if someone is passionate, then they must be right. "He was really passionate about what he said, he spoke with a lot of conviction, therefore there must be truth in what he said" - again, this is how a lot of cult leaders getcha.
It can include thinking that feeling bad must mean you're on the right track. "When the pastor talked about sin, I felt so guilty and knew I needed God's divine grace" - lots of people can make you feel guilty, it doesn't mean they're right.
This fallacy can include the absence of feelings, too. "He spoke so calmly, I knew he had to be completely rational." That's how a lot of pseudointellectuals getcha.
Appeal to Irrelevant Authority: When someone claims that a thing must be true because a famous and respected person believed in it. For example, "Isaac Newton believed in God, therefore God must exist." Rather than examining Newton's particular reasons for believing in God, the person making this argument just expects you to assume that Newton's (allegedly) superior intellect made him incapable of error, and that you should just outsource your own thinking to him.
Appeal to Nature: When someone claims something must be good because it's (at least supposedly) natural. For example, "herbal remedies are superior because they're all natural." While it's true that herbal remedies can be useful, it doesn't follow that they're inherently better - much less safer. Kava, which has been used to treat anxiety and depression, has caused severe liver damage in some cases. Lead and UV rays are also 100% natural.
Appeal to Tradition: Asserting that something must be correct or better because it's traditional. For example, "the ancients believed the earth was flat, so it must have been true." Also, "people have believed in Hell for thousands of years, so it must exist."
Genetic Fallacy: Asserting that something must be good/bad or true/false depending on where it came from. While it's true that claims that come from known bad faith actors should be given extra scrutiny, it doesn't follow that everything they say must be wrong. The world doesn't spontaneously turn flat just because the worst person you know said it was round. A visualization exercise isn't inherently bad for you just because a New Ager came up with it.
Misleading Vividness: Constant exposure to certain types of information or certain types of people can create a false impression about the world at large. An well-known example of this is when people on Tumblr assume that the average person out there in the world has an opinion on (insert topic of Tumblr discourse here).
Here's another example: when you go through Law of Assumption success stories and see numerous people claiming they manifested all of this amazing stuff, it's easy to think that this practice must be working really well for everyone. But if you're on a blog or tag where success stories are curated, there's going to be a huge selection bias here. And with how many people are shamed and bullied into silence when they come forward and say that the LOA didn't work for them, and with Living in the End providing an incentive for people to claim success they might not actually have, it's difficult to be sure what the actual success to failure ratio actually is.
Post Hoc: When someone claims that if X happened after Y then X caused Y without providing any supporting evidence, that's the Post Hoc fallacy. For example, "I knew a girl who cast a money spell, and one week later her grandpa died! This is proof that magic calls on evil forces and always comes with a price!" is this fallacy.
Critical questions to avoid falling for these fallacies:
Is this the whole picture, or is something being left out?
Has this been repeatedly tested to see if the same results happen each time?
Is this really how things always work, or are there counterexamples?
Where is the research? Where is the actual data?
123 notes
·
View notes
Text
❀ A little possum approaches with a gift!
{PT: A little possum approaches with a gift!}
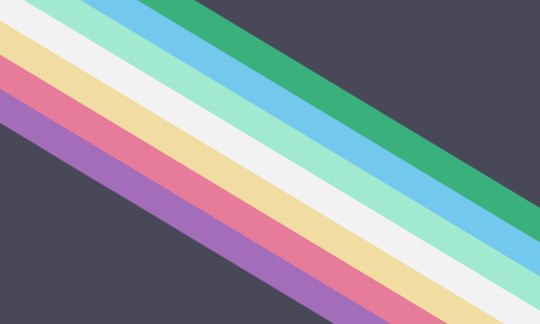
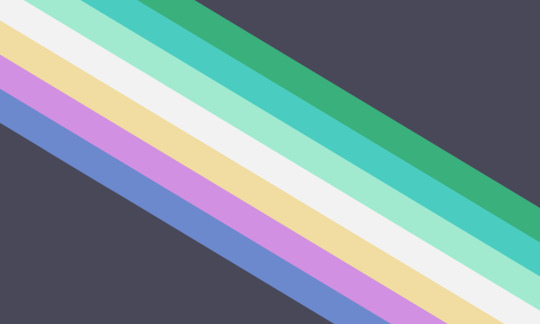
❀ Disability Pride Flag Recolors (And Additions!)
{PT: Disability pride flag recolors, and additions!}
❀ Stripe Meanings:
Purple - Degenerative Disorders / Aging ; ex. loosing vision through your life, worsening joint pain, chronic illness, developing Alzheimers. As far as I’m aware, degenerative disorders can be acquired at any point in life, not just with old age- but the two often are related, hence why I included them together.
Red / Teal - Trauma / Injury ; ex. loosing use of limbs following an accident, mobility issues, anxiety from traumatic events. Red is commonly associated with trauma and injuries, but teal is the awareness color for a large majority of traumatic experiences, so I didn’t want to exclude it.
Yellow - Natural Variation ; ex. Autism, learning disabilities, motor disorders. I suppose this category means disorders present since birth/form in early childhood, and can be seen as just evolution causing variation. Help clarifying this would be appreciated!
White - Complex, Unknown, and Hidden Disabilities ; self explanatory- disorders with complex causes, invisible to others, and just being disabled but not knowing what disability! Catch all for every disability as well :)
Mint Green - Genetic ; ex. Down syndrome, chromosomal disorders, asthma, cystic fibrosis, scoliosis. Similar to natural variation, but for those who prefer to identify it more as disorders or disabilities, instead of being ‘different kinds of people’, and conditions that present later in life.
Blue / Indigo - Situational ; feeling as though you’re no different from others, and the real disability is a lack of accommodations. Inspired directly by the post referenced below, which explains it much better than I can. Additionally, this could also include episodic disabilities like epilepsy, bipolar disorder, or reoccurring illness.
Green - Environmental / Illness ; ex. getting asthma following severe respiratory illness, nerve damage from cancer, birth defects from dangerous conditions during fetal development. This can also include seasonal disabilities, like seasonal depression or pollen allergies.
Grey - Rage about those who have suffered as a result of discrimination, same as the original meaning.
{PT: Stripe meanings. Purple, meaning degenerative disorders or aging. Examples include, loosing vision through your life, worsening joint pain, chronic illness, or developing Alzheimers. As far as I’m aware, degenerative disorders can be acquired at any point in life, not just with old age- but the two often are related, hence why I included them together. Red or teal, meaning trauma or injury. Examples include, loosing use of limbs following an accident, mobility issues, or anxiety from traumatic events. Red is commonly associated with trauma and injuries, but teal is the awareness color for a large majority of traumatic experiences, so I didn’t want to exclude it. Yellow, meaning natural variation. Examples include, autism, learning disabilities, or motor disorders. I suppose this category means disorders present since birth, or in early childhood, and can be seen as just evolution causing variation. Help clarifying this would be appreciated! White, meaning complex, unknown, and hidden disabilities. Self explanatory. Disorders with complex causes, invisible to others, and just being disabled but not knowing what disability! Catch all for every disability as well. Mint green, meaning genetic. Examples include, down syndrome, chromosomal disorders, asthma, cystic fibrosis, or scoliosis. Similar to natural variation, but for those who prefer to identify it more as disorders or disabilities, instead of being different kinds of people, and conditions that present later in life. Blue and indigo, meaning situational. Feeling as though you’re no different from others, and the real disability is a lack of accommodations. Inspired directly by the post referenced below, which explains it much better than I can. Additionally, this could also include episodic disabilities like epilepsy, bipolar disorder, or reoccurring illness. Green, meaning environmental or illness. Examples include, getting asthma following severe respiratory illness, nerve damage from cancer, or birth defects from dangerous conditions during fetal development. This can also include seasonal disabilities, like seasonal depression or pollen allergies. Grey, meaning rage about those who have suffered as a result of discrimination, same as the original meaning.}
The meanings of each of the stripes is inspired by this post by @ipso-faculty , which i highly recommend looking at, as the meanings and definition are detailed and fascinating! The colors are based on the awareness ribbon colors/general associations. My version is meant to represent the origins, causes, or unique factors for categories of disabilities. Additionally, I’ve also included different forms of disability at the bottom for those who prefer the original meaning, but ipso’s comment really stuck out to me and i resonate with deeply.
“It’s been my experience of disability community that attitudes about disability tend (in general) to be linked more to when/how we were disabled rather than mental/physical/sensory/etc.”
The disability models confused me upon first research, so until I understand more, they aren’t explicitly included- though including them in the future would be nice! And to me, the cause of my disabilities greatly affects how i feel towards them. For example, my autism has always been a part of me, and I can’t imagine myself without it- but my OCD developed from childhood trauma, and I remember a time before I had it, and wish to be like that again. The distinction is important to me, even if not to anybody else.
These flags were made for fun, and I haven’t directly referenced or spoken to other disabled people about the color meanings and representation. If you have things to suggest, please do so! I’m learning, and would love to make this more accessible!! Just please be nice!
{PT: These flags were made for fun, and I haven’t directly referenced or spoken to other disabled people about the color meanings and representation. If you have things to suggest, please do so! I’m learning, and would love to make this more accessible! Just please be nice!}
And, in reference to the second flag, alternative meanings! Indigo for neurological, purple for psychiatric (in reference to mad pride), yellow for neurodivergence, white for invisible disabilities, mint green for sensory (because mint green gives me good visual sensory), teal for medical (not meaning how doctors treat disabilities as things to be fixed. I specifically mean disorders that arent visible externally but are still very much physical, such as hormonal disorders. Chosen with my mom in mind.), and green for episodic disorders! Unless clarified, theres no explicit reason a disability category was assigned to a given color, (aside from previous or common associations), and was chosen based on vibes. Indigo just feels like a neurological color to me.
Tagging: @radiomogai (thank you for the permission!! Hopefully you dont mind :D)
#is there a difference between effects and affects??#disability#mogai flag#flag recolor#disability pride#disability pride flag#suggestions welcome#i just wanted to make the colors more pleasing to my brain#i didnt like the grey#it felt#a bit out of place#image id in alt text#queergutz
39 notes
·
View notes
Text
Wilhelm's Mental Health; Autism or Borderline Personality Disorder?
Wilhelm’s mental health status is a complex issue that has been heavily commentated on by the fandom, from what I've observed within the YR fandom, a large number of fans headcanon Wilhelm as having autism but I hope to explore autism and it's symptomology outside of the white male perspective that is defaulted upon in autistic representation by overviewing symptoms that contribute to the interpretations of Wilhelm having either Borderline Personality Disorder (BPD) or Autism Spectrum Disorder (ASD). These two disorders can show up in similar forms, and often get misdiagnosed (especially women and non-white people are immediately pointed toward the BPD diagnosis rather than ASD due to assessor’s prejudice and society's higher expectations for minority groups to mask autistic traits while in public but that’s another story). A key difference between the two is that ASD is a genetic disorder while BPD is a disorder that develops due to childhood trauma. Both disorders have a high likelihood for comorbidity with other mental disorders such as depression, anxiety, and PTSD.
Content Warning: Frank commentary of symptoms associated with Borderline Personality Disorder and Autism Spectrum Disorder, including: self-harm, substance abuse, and emotional dysregulation.
Disclaimer: I am not a mental health professional but I am autistic, and I’ve known quite a number of people with either BPD or autism [Years ago, I stayed at a long-term DBT-based treatment center, a therapeutic specialty for created to address BPD that has been expanded to treat other mental health struggles and disorders that go hand-in-hand with BPD symptoms (Substance abuse, self-harm, OCD, etc.)]. This is also solely based on what is seen in the show, not actors' interpretations that are expressed through interviews.
Throughout the series Wilhelm (W) is seen engaging in a multitude of behaviors and experiences feelings that he expresses verbally that could be interpreted as fitting as symptoms of both.
Notably the scene where W is seen smacking his temple with his palm (1x05) can be interpreted as either: purposeful self-harm (a common self-destructive coping mechanism for overwhelming emotions in BPD; his alcohol and drug use could be described similarly) or a self-stimulatory behavior (stimming), a characteristic of ASD to aid in regulating or expressing intense emotions (while W is only seen engaging in this with a “negative” emotion, stimming can be used with all emotions), other example include his chest-rubbing, and frequent caressing of different textures.
Intense mood-swings, anger, and difficulties with emotion processing, this is quite evident in W's actions, emotional responses, and feelings he expresses verbally. Both disorders have been observed to have intense changes of emotions at a “drop of a hat.” ASD mood-swings are typically related to exposure to sensory input that is quite uncomfortable, overstimulation, and/or meltdowns (breakdowns due to a culmination of intense feelings, sensory input and/or overwhelming experiences). BPD mood-swings and impulsive actions are more related to triggers of trauma responses, and a lack of regulatory measures
Symptoms Specific to Each Disorder:
BPD:
Attachment to Favorite Person (FP), a symptom of BPD where one idolizes one person in their life to an extreme degree, wanting to spend all their time with their FP, and intense anger and despair with perceived betrayals/slights against them/mistakes. W goes through 2 FPs (Erik and Simon). He adores Erik, and feels betrayal when Erik leaves him at Hillerska. Simon quickly becomes a FP, seeing him as perfect and feeling betrayal when Simon messes up (drug dealing) and the utter despair and hopelessness when Simon needs space and starts dating Marcus; “It feels like I’m going to die” (2x04) (Could be a consequence of being utterly isolated due to being Royal and latching onto anyone who shows care to him)
Unstable / Ineffective Relationships (Simon, Kristina, Minou, and other hierarchy figures): BPD is often associated with people with the disorder lashing out against "completely innocent" people for "no reason", while this can be accurate, it does not account for the triggering of such episodes (See above)
Substance Abuse: People with BPD may utilize alcohol and/or other substances to "numb themselves" from BPD symptoms or distance themselves from harmful memories (autistic people also experience substance abuse and addiction at higher rates than the general allistic population but it is often seen as a crutch to cope with the constant stress of existing in an allistic world which is not implied in what draws W to substance use throughout the show)
ASD:
Expansion on Sensory Issues: W seemingly wears the same sweater-button up combo often, just with different sweater colors — Grey, teal, and that god-awful bright orange — ensures safe textures when buying new items but he might just have a clothing stylist with horrid taste. W's struggles with the suffocating feel of the suit (2x05). He rarely utilized the overhead lights in his room, instead relied on his string lights, lamps or natural lighting (Florescent and LED lights can trigger light sensitivity and contribute to sensory processing difficulties in autistic people)
Preoccupation with the concept of normalcy (1x01), as a kid being autistic often ostracizes you from your peers, being deemed the “weird kid” is very damaging thus W may have been enticed by the prospect attending a regular high school to like "normal people" (this concept is intrinsically tied to social class throughout the show, W wants normalcy of a lower class while Sara wants conform to a higher class but that's a different spiel). This can lead to masking; the act of forcing oneself to hide their autistic traits in order to fit into Allistic norms. (My one dispute to this interpretation is he's seemingly more disgruntled by the pomp and circumstance of being Royal that "others" him rather than peers judging him)
Lack of social cues (Not even going to waste my time explaining this one, the man had no game, absolutely none, it’s a wonder that he pulled Simon)
This far from a full list of symptoms seen in W's characterization but it's a broad overview of the signs I saw from an autistic lens. I lean towards Wille having Borderline Personality Disorder based on the fact that significant aspects of Autism Spectrum Disorder can be correlated to his unfortunate circumstance of being royalty.
#young royals#young royals analysis#prince wilhelm#wilmon#Was this entire thing inspired by a Wille / BoJack Horseman edit I saw on tiktok? Yes yes it was
77 notes
·
View notes
Text
Please note, the photos are NOT exact.
This is a Creepypasta OC
Name*ੈ✩‧₊˚༺☆༻*ੈ✩‧₊˚Info Full Name: Poe Nakahara Name Pronunciation: "Po" "Nah-Kah-Har-ah" Name meaning: The Peacock (or bird of color) in the wheat fields Other Names: The Cursed Writer Poe Po-po (hehe...) Speciesﮩ٨ـﮩﮩ٨ـ♡ﮩ٨ـﮩﮩ٨ـInfo Species Family: Mortal Species Sub-Family (optional): None Species: Human [Genetically / Forcefully enhanced (hide spoiler)] Sub-Species(Optional): None Physical* ੈ✩‧₊˚Descriptions Skin color: Pale, like a vampire Schela(Eyewhites) color: White Iris color(eyecolor): Purple Pupils: Black, normal Hair color: Brown Hair length: Neck Hair style:

Common clothing ("Disguise"):

Formal clothing ("Work"):

Ears: Rounded Hands: Normal Piercings: Earrings Rings: One, left ring finger

Hat: Fedora (Only worn on special occasions)

Special⁺‧₊˚ ཐི⋆♱⋆ཋྀ ˚₊‧⁺Markings None Personal⋆♱✮♱⋆Info Age: 24 Height: 5'6" Weight: 120 lbs Gender: Male Sexual Preference: MlM Occupation: Author? Status: MIA (Missing in Action) °•★°« Disorders / Illnesses »°•★° Schizophrenia/Psychosis -- Delusions, incoherent speech, Episodes of panic and mumbling. This character often talks with his delusions. Insomnia -- Severe disability to fall asleep or stay asleep, when they do, they always have bad dreams or feel watched, often seen in young teenagers with cruel families (As far as this character can see). Attention Deficit Hyperactivity Disorder (ADHD) -- Easily distracted, tends to fidget. Always focusing on the wrong tasks unless he is ordered to do what he needs to do. Very mild Autism -- Struggles to fit in with society, even after death, this character almost never makes eye contact, and seems really... strange. Anxiety -- This character always feels watched, often times not talking to anybody in real life, always scared of what's going to happen, or if he messes up. Depression -- Severe feelings of doubt and regret, often seen with silence, (Also known as Masked Depression), this character tends to hide away their sadness, to make others happy. "Anxiety Induced Tick Disorder" (AITD or "Nervous Ticks") -- This character twitches in stressful situations, often seen in their neck and head twitching / jerking in unnatural ways, Legs or other limbs spasming, or his eye twitching (Triggers: Nervousness, cold, certain spots itching, tiredness, nausea, certain injuries) ˙⋆𓆩Abilities and Personality𓆪⋆˙ Poe is a fairly nice individual, until part of his family is threatened, he tends to hide his true feelings with a mask of calm, dissocialized emotionless-ness. In truth he suffers from episodes of insanity and anger issues, though he is very skilled in coping with them. Though Poe doesn't seem friendly on the outside, if you get to know him, you'll discover he's actually just somebody who's suffering from rumors and accusations, that you don't really know if they are true. Poe has a strange ability... well.. more of a curse, any book he writes, it seems to be laced with dark magic and those who read it, either die from things like poisoning or going insane to the point they try to become on of the characters, most commonly associating with the villains of Poe's stories. Other than that.. Poe is a fairly "normal" person, though he appears to be strangely agile and athletic, and even without gloves, his skin seems tough enough it's hard for a simple thing like a rose thorn to pierce it, of course, Poe will always have his weaknesses as well.
愛Historical Information愛 [Childhood] saga: Poe was separated from his parents at the age of 2, being raised by his grandparents, who refused to support him in his wish to write stories. As a rebellion Poe wrote in secret, often on his school computer or in his notebooks, which his grand parents never checked. [Teenhood] arc: Poe lost his uncle at the age of 15, and it had sent him into a deep depression, he debated doing {CENSORED} but the people at his school stopped him from doing anything. [Adulthood] arc: Poe had his first book published at the age of 20, it was a murder mystery, but what he didn't expect, was for it to become on of his most popular books, but there was a catch. Police started to realize the people who were "killed" had one of Poe's books on their shelves, so they questioned him, when they found no sign of him being guilty, they set him free. ["Death"] saga: Around the age of 22, Poe suddenly went missing, though books kept getting published under his name, people assumed Poe had secretly had a child, that took on his position. ✗Picture✗ Coming soon ✩₊˚.Quotes ⁺₊✧ "To be ignored... it hurts." "A book... for you, I hope you... enjoy." "Please note, I am a writer, anything you say I have full right to use in a story."
#creepypasta#creepypasta fandom#creepypasta oc#ocs#tumblr polls#my art#my ocs#creepypasta art#creepypasta au#artists on tumblr#oc artist#small artist#digital artist#art on tumblr#drawing#illustration#artwork
13 notes
·
View notes
Text
THIS IS VITAL. Do not convince yourself that you have "insomnia" or go into bed thinking you're going to have trouble sleeping. Even if you've been professionally diagnosed. Doctors don't care about you the same way you care about yourself, so keep this in mind. You're one of many patients to them so you need to take control of your own health, and sometimes that means completely rejecting their advice and diagnoses. You need to tell yourself that you're simply going through a rough period and sleep might be difficult, but you're fine. I can't stress how important it is to psychologically believe that things are fine and/or will get better. A major component of insomnia for people who suffer from anxiety is the very anxiety around not being able to sleep. The anxiety compounds the issue and it thus becomes a self-fulfilling prophecy. It's one of the many cases in humans where if you believe it's a problem, it WILL be a problem.
You need to find a way to, over time, decouple the association between sleep and whatever negative delusional spin you're putting on it. Do not predict the future with false and irrelevant evidence from the past. A bad night of sleep, or no sleep the day before does not mean it's going to repeat in the future. This is highly ILLOGICAL, but your brain won't care about this, it will force those thoughts on you. Be aware of your own cognitive behaviors and beat them out with clear, logical thinking. Obviously, this will be difficult since emotional states cause us to think delusionally, and insomnia along with the accompanying sleep deprivation will make it worse, but the big takeaway is to realize that you can't really trust your brain at this time because it isn't functioning properly and is under a lot of stress. This process can take time, be patient with yourself, especially if you think nutrition might be a factor. It's vitally important to remember that YOU CAN FALL ASLEEP. EVERY HUMAN HAS THIS ABILITY unless you have extremely rare genetic disorders or severe nutritional deficiencies that can EASILY be corrected.
You need to realize that it's ENTIRELY NORMAL to have problems falling asleep for days, weeks or even months at a time. Your case is likely NOT UNIQUE, and many millions of people over millenia have suffered and successfully recovered from this disturbance. It is scary because it is happening to YOU, but take comfort in the fact that it is also common and treatable. This is not blind hope, or lying to yourself, these are FACTS THAT YOU NEED TO CONSTANTLY REMIND YOURSELF OF because your brain will already be doing a great job of bringing you down with negative thoughts. You must truly believe that you're going to get better and fix the problem, while taking every possible step you can to move the dial in the right direction towards progress.
Take comfort in the fact that many people have sleepless periods like this for various reasons. Stress, nutritional deficiencies, terrible diets, anxiety, grieving, depression, breakups, divorces, etc. It's crucial to remember that all psychological stresses will diminish over time and you will return to normalcy. Your brain is constantly adjusting towards homeostasis, so YOU WILL HEAL IN TIME. YOU MUST KNOW THIS. Don't get obsessive over how long your recovery is taking, or set arbitrary goalposts (e.i. "I should be fine in a week"). Take things one day at a time.
Also be aware that stress depletes magnesium, which is responsible for reining in ruminating thoughts and relaxing you. Again, I urge anyone with insomnia and/or anxiety to do ample research on magnesium. It is absolutely a life safer.
[x]
52 notes
·
View notes
Text
Tourette Syndrome Awareness Month starts today (May 15) to June 15, so here’s some facts people might not know:
-Tourette Syndrome is a neurological disorder, not a mental disorder.
-There is no cure for Tourette Syndrome, and there is currently no drug used to treat it specifically.
-The exact cause of Tourette Syndrome is not fully understood, but is believed to be a combination of genetic and environmental factors.
-Some researchers suggest an imbalance in neurotransmitters like dopamine and serotonin.
-Tourette Syndrome is believed to result from a dysfunction of the thalamus, basil ganglia and frontal cortex regions of the brain.
-While not life-threatening, severe motor tics like violent head jerking, could lead to accidents and self-injury. Tics are also considered ‘socially inappropriate’, which can lead to bullying, social stigma, and isolation, affecting self esteem and social development. Living with this disorder and its associated challenges can attribute to anxiety, depression, and other mental health concerns.
-One in 100 children have some form of Tourette Syndrome or a tic disorder.
-Less than 10 percent of people with TS swear, which is known as coprolalia.
-TS causes people to have tics. Tics are sudden twitches, movements or sounds that they do repeatedly. People with TS cannot stop these tics.
-No two people with TS will have the same tics. Each person with TS is as different as every snowflake.
-More than 86 percent of people with TS also have co-morbid conditions — ADD, ADHD, OCD, anxiety disorders, sensory processing disorder (SPD) and dysgraphia, just to name a few.
-There are two types of tics, motor and vocal. Motor tics are movements of the body, such as blinking, shrugging of shoulders, limb movements, etc. Vocal tics are sounds people make, such as barking, sniffing, throat clearing, random words, etc.
-Tics can be simple or complex. Simple tics involve just a few body parts, such as eye blinking or sniffing. Complex tics involve several parts of the body and can have a set pattern, such as bobbing head while jerking arms, then finishing with a jump.
-Tics wax and wane and can increase and decrease and change throughout a person’s lifetime. Tics a person has an a young child could be different and at a different severity than when they are a teenager.
-Tics usually start around the age of 5 to 10 years old. The first tics are usually motor tics.
-Tics are usually worse during times of stress or excitement. They tend to improve when a person is calm and focused on an activity.
-Even though symptoms can change or appear or disappear, the condition is chronic.
-TS effects males 3 to 5 times more than females.
-A misconception is that people can learn to stop their tics. They can, at times, hold them in (suppression), but eventually have to release them.
-Individuals with TS are aware of an urge to time, similar to that of a sneeze or an itch. They describe it as a build up of tension, pressure or energy. The actual tic is a means of releasing or relieving this tension.
-TS does not affect the intelligence of a person. In fact, most children with TS have above normal to high intelligence levels.
-Children who try to suppress their tics while at school have a hard time focusing on what the teacher is teaching. Suppression of tics is physically exhausting, making it hard for them to live up to their potential at school.
3 notes
·
View notes
Text
There was a lot of interest yesterday re: the episodes that came out on the Migraine World Summit about Sleep and Comorbidities
I took the time and transcribed the episodes. The one about comorbidities is here under the cut
The one about sleep will be posted once I feel less like I'm gonna puke
Remember, I literally just transcribed what I heard, so if there's weird sentences, that's not on me!
I hope someone finds this helpful and/or interesting.
Migraine Comorbidities: A Look At Associated Conditions
Did you know that for people with chronic migraine nearly 90% of them also struggle with another chronic condition,
and for 40% of these people it’s not just one condition, it’s 4 or more.
And while some of these conditions may seem completely unrelated, they all share one common thread - they all exist in the same body
What does comorbid mean?
A cormobid condition or two comorbid conditions exist in an individual at a rate greater than predicated by chance.
We all can have multiple medical conditions, but if you had migraine and diabetes, or migraine and toenail fungus, there’s no association that we’ve mapped out for those, those are two unrelated things that are both in the same body
A comorbidity is something that is related to the migraine in some way, so comorbidities could be unidirectional – one condition causes another – or they can be bidirectional – there’s a relationship back and forth
They can spring from common genetics, and there’s over 75 now and it keeps increasing, some new and exciting ones we’re looking into,
but there’s over 75 disease or diagnoses that are comorbid or run with migraine,
so we doctors really need to know what conditions are comorbid or run with migraine because it informs us about how we treat patients, how we talk to patients, how we counsel them, what meds we put them on,
so there’s a lot of ramifications for understanding comorbdities
I was surprised to hear that diabetes wasn’t a comorbid condition, are there any others that are sort of shocking that they are not associated with migraine?
Well, when there’s 75 different diagnoses and more added all the time it seems almost everything is.
I went for the diabetes example because we have some strong evidence that that is not associated - in fact, interesting and maybe to the aside, diabetes is slightly protective against migraine
so it’s the opposite of a comorbidity
That is surprising, is that for both T1 and t2 diabetes?
No, interestingly that’s for T2, we’re not sure about T1
I feel like with a lot of other conditions, so many that overlap with migraine, you see migraines listed as a symptom of that disease, is that a true result, why is that a thing?
Sometimes true, sometimes its not migraine but it’s more headache
Headache is, 90% of us will have some headache,
even though only about 12% of the population has migraine,
so sometimes migraines might be listed as running with a certain condition,
for example, depression is highly comorbid with migraine, people who have migraine have more commonly or more likely to have depression, people with depression are more likely to have migraine
however, people with depression are much more likely to have headache in general, so it’s hard to know
It gets a bit complicated; we do know, for example, migraine is comorbid with certain types of heart disease, particularly migraine with aura is associated with some cardiovascular disease
The number 1 most common associated comorbidity with migraine is anxiety
So if you look at studies about 2 to 5 times more prevalent migraine is in people who have anxiety
and so being informed that the number 1 comorbidity with migraine is anxiety, we go a little slower and gentler sometimes with our treatment, we screen for it
we think about anxiety in the context of migraine because the migraine worry brain, someone who has both migraine and anxiety, they take meds in sort of differently than those who don’t have anxiety
so again, it informs us in how we treat, we go a little gentle with them
Since there are so many comorbidities of migraine, I’m gonna go through a few and let me know if there’s a connection if there’s lifestyle factors or meds that can improve or worsen migraine, or just any connections you may think of?
Is there a connection between rheumatoid arthritis (RA) and migraine?
Multiple types of pain are comorbid with migraine, and that’s one of the OG’s that’s been known for a long time
Fibromyalgia’s the most common pain associated with migraine
Trigeminal neuralgia, nerve pain on the face, also strongly comorbid
and TMJ tempromandibular joint disorder, very common
Painful arthritis, oesteo or rheumatoid, is also comorbid with migraines
You had me on a few years ago talking about the autoimmune connection in migraine and that is real, there’s an inflammation in migraine and there’s an inflammation in many of these autoimmune conditions, so that stands to reason
Again, it informs us if we understand that somebody with RA and migraine the two co exist because NSAIDs (non steroidal anti inflammatories) may be very helpful daily for someone with RA, but NSAIDS daily for a person with migraine disease might cause a rebound or medication overuse headache,
so again, the understanding of comorbidities helps to give us an idea of how we interact with and treat our patients, and how we educate them
I feel like it’s difficult to figure out where the pain is coming from, especially since migraine has a lot of referred pain and areas like the jaw or the neck or joints in general and especially allodynia as as a symptom of migraine and so many of these other chronic pain conditions come in – how do we decipher is this migraine or something else?
The answer is yes. It could be migraine, could be the other or a combination.
It gets difficult; we know that from the shoulders up there is a whole lot of interaction with the body parts from the shoulders up and migraine.
So people who have a tooth abscess that’s likely to trigger migraine,
people with TMJ can be a trigger for migraine in those who are genetically wired for migraine
Osteoarthritis or degenerative disease of the neck or spine, that can be a trigger
and the so called cervicogenic headache, provided it is throbbing with nausea, etc, that is a cervicogenic migraine
The unifying principle here can be central sensitisation,
because you can have central sensitisation from multiple different pain sources, and so one can have pain in the neck/in the TMJ/trigeminal pain, etc, and it’s all leading to a brain central sensitisation.
Again we would be thinking about what meds or therapeutic interventions can we use to decrease that central sensitisation, we could probably knock down all the different pain indications
The other worth noting in this context of course is trauma and PTSD
We know that trauma and PTSD are comorbid and run with chronic migraine very strongly, and also a little less so with episodic migraine as well
I had a patient once who came to see me to treat her chronic migraine and she said
‘you treat that, but I have 7 other pains and I have other doctors treating those’
and I said
‘what other pains do you have?’
she said
‘I have TMJ, I have neck pain, noncardiac chest pain, IBS, interstitial cystitis bladder pain, plantar fasciitis of my feet’
already I started thinking there’s probably a tie there
I said rather than having 8 different pain syndromes, they’re all tied together and out of all of the docs, no one had asked about prior trauma
and trauma gets buried in your brain and it comes out as chronic pain
So sometimes knowing the comorbidity in a chronic migraine patient in particular, particularly a chronic migraine patient with other pain syndromes, you could be the only doctor to ask ‘hey life is sometimes unfair, have you ever had anything bad happen to you in your life?’
We have so taken that mantle up here at our practice that we have trauma therapists on our staff, we have EMDR abilities, we have a ketamine infusion program, so we are the ones who look out for that kind of stuff
That’s rare for a doc to even ask, even if we say ‘im also dealing with all of this’ they say ‘well I can’t help you with that’
Is there anything we could say to make a doctor try to listen or understand, are there any questions we should be asking in that situation?
I think that even someone who is just focused on headache medicine, or course they understand that the migraine/headache doesn’t exist in a vacuum, that there is a whole person here. And my philosophical approach is to treat the whole patient
if someone needs surgery, they’ll go to a surgeon, dentistry they’ll go to a dentist, but we know anxiety is so comorbid, a headache specialist should be good at treating anxiety
depression is so comorbid we should know how to treat depression.
If we get to a point we’re not comfortable with our skill set we can then refer out, but why not be the person taking care of that?
Particularly if anxiety is one of the drivers of migraine, if they’re in a panic or social setting it triggers a migraine, I’d like to take care of that
More recently, and we had a discussion of this at one of the headache meetings, obesity is another risk factor for chronic migraines, so it’s a comorbid condition.
What about these GLP-1 drugs, Ozempic and the others?
This is cutting edge stuff, should headache specialists be writing GLP-1s? and I strongly say yes
Not just in migraine, but as you know, there’s a condition of increased pressure in the brain called idiopathic intercranial hypertension, not always but they’re usually someone with a high body mass index, reducing their BMI gets rid of their headache
Some migraine sufferers it’s the same thing, and so can you legitimately prescribe ozempic? (insurance coverage is another issue) but can you prescribe them for persons with chronic migraine? I say yes
Is there any connection with autism?
So that is interesting, the most common so called neuropsychiatric conditions that are comorbid as we mentioned, anxiety is number one, depression, bipolar disorder and PTSD
There is some literature that there is an association with autism and migraine.
It’s not as strong yet and I think there’s more work to be done on that, another one a cousin that’s in that general ballpark there is an association between ADHD and migraines
I’ve always found that very interesting, for a couple of reasons
One, when you treat somebody with ADHD, the most common class of meds you use are the stimulants. A known side effect of stimulants is headache and if you have migraine it can trigger your migraines
Not always, but this is what’s important to know, it’s also some interesting idea borrowed from Andy Blumenthal another headache specialist, that a lot of adults say they’ve also been diagnosed in addition to their migraine with ADHD.
When you ask why, they say
‘because I have concentration, focus issues, etc’
and he says maybe they have ADHD, legit, or maybe they have an inter ictal between migraine burden that they still have some leftover of the migraine that’s making them not think as sharply
So interesting to think about. It could be, we know migraine and ADHD are comorbid, but some people may be calling ADHD what is actually just leftover inter ictal non pain migraine
We’re starting to focus now more on the cognitive effect of migraine
The migraine is not a pain disorder, migraine is a brain disorder
In some of my patients the headache is a small part of the trouble, the pain part. The big difficulty is the irritability, the mood changes, the cognitive issues, the focus difficulties, so I think we’re beginning to talk about that more
I think brain fog and fatigue in between attacks or during attacks are so common and when we have other conditions we have no idea if it’s migraine, if it’s one of a million different conditions, it’s difficult to parse that out
I think we should get away from labelling migraine as a headache condition
And the fellowship says headache fellowship, it’s really not
Migraine is this brain disorder that’s fascinating and multifaceted and a whole host of different symptoms, dizziness, vertigo, visual loss, confusion, and I think we should be focusing now more on those
Migraine and POTS or dysautonomia?
POTS clearly is comorbid with migraine
Particularly in younger people with a higher incidence in girls and women more than boys and men particularly those who have a lower BMI
We think of POTS as a wonky autonomic nervous system
It can at times be developmental - some people in their teenage years have a lot of POTS and by the time they’re in their mid twenties their symptoms are almost gone, the prognosis in many cases isn’t all that bad
Some of the meds we use for migraine can worsen POTS
Some meds we use for migraine in the right setting can help POTS - if someone has a very rapid heart rate because of POTS, low dose beta blocker can help migraine and can help the POTS
Again, these are the therapeutic 2 for 1s that we can do once we understand and screen for these comorbidities
We encourage all our migraine patients to really hydrate well, well our POTS patients have to even hydrate more, it becomes more of an issue in someone with comorbid POTS
Its interesting that, syncope is not an actual medical condition, but syncope runs with migraine - people who have migraine are 3 times more likely to pass out than people who don’t have migraine
I think some of those probably have a wonky autonomic system like POTS
Now, more recently there’s these overlapping circles of diagnoses that can include POTS, migraine, and ehlers-danlos syndrome, particularly the hypermobile form – that’s a connective tissue disorder and they can have widespread pain, some are asymptomatic, but you can have dislocations of your shoulder and neck pain and other pain, they have a higher incidence of migraine and a higher incidence of POTS
Now we have overlapping circles of 3 different conditions that can all interact with each other
Can you tell us more about the meds typically used for POTS that can worsen migraine?
I’ve found ivabradine which is very effective in POTS can cause headache as the side effects.
I think fludrocordisone, which is another med that can help POTS patients, sometimes can trigger headaches and migraines in my migraine patients
It’s more often going the other way, that if you drop someone’s BP with a BP med for migraine, you’re not going to be doing their POTS any good because they tend to drop their pressure anyway
If I do it, I would do it cautiously - make sure they’re hydrating, using compression stockings on their thighs, all these things we tell our POTS patients
I’d introduce a migraine med that might exacerbate POTS in a very tiny dose
Again, knowing comorbidities informs how you dose, not just the meds you choose, but how fast you might ramp up a particular med
Some meds like topiramate, venlafaxine, amitriptyline, could potentially worsen the symptoms of POTS, but sometimes you can use those in small doses, giving the patient the confidence they can interact with you as often as they need to, and sometimes when people were told not to use those meds I can have success with them, not always, but it’s not black and white its grey
Long covid and migraine?
Covid itself has been known to worsen migraines in persons with migraine disease
I just had a patient today who told me that for the 1st time - she got it a few weeks ago going to a conference and she thinks she got it on the plane - her migraines that were 4 to 5 a month have gone to 20+ a month, and the severity has gone up too
I said to her, its been my experience, again a lot of this stuff the hard science is trickling in, it’s been my experience anecdotally, that when ones migraines are flared up by covid it tends to wind down.
The bad news is it takes a long time, it can take many weeks to several months or more for it to settle down.
Sometimes we use a pretty generous taper of oral steroids and occasionally that can reset them back to their lower set point of number of migraine days
The other thing that we see, and there’s been lots written about this, is covid long haul syndrome
There’s a number of different manifestations, but in the stuff we do as neurologists, brain fog is very common, and we see that with migraine
Dysautonomia is very common
The other big one is gut issues with post covid long haul
We’ve known for years that, compared to people without migraine, persons with migraine disease have relative gastroparesis, their stomach doesn’t move along as well even between migraine attacks, certainly within migraine attacks we know that,
but even in between, their guts are sensitive. It’s no surprise, we know that IBS runs very strongly with migraine.
In fact, IBS has been renamed lately; it’s now called ‘disorders of gut-brain interface’
Because it emphasises that there’s nothing intrinsically wrong with the organs of the gut, in someone with IBS you can put a scope down them, do biopsises, it’s all fine, it’s the nerve supply from the brain
So when we see a post covid long haul person the questions we wanna ask are,
- is your migraine pain worse,
- are you developing autonomic symptoms,
- what’s happening in your gut
and again going back to this holistic approach, there are meds that can symptomatically treat all of those things
Meds that can help the gut along, help the autonomic nervous system, up our game on the pain.
Someone may have never had nerve blocks, we’ll do nerve blocks. Someone who hasn’t had prednisone, we’ll do prednisone
With the meds treating autonomic symptoms, will that help the autonomic symptoms they experience as a result of a migraine attack and is the vagal nerve affected by any of this?
Yes and yes
When you help the autonomic nervous system, it almost doesn’t matter with the dysregulation is, these meds can prove to be helpful
and of course the vagus nerve, which is arguably the most important of the 12 cranial nerves, it’s the longest, it goes all around the body, goes to the heart, the guts, the sweat glands, there’s a lot that the vagus nerve does, it’s clearly involved
Anything we can do in our day to day life to effect the vagus nerve or autonomic symptoms??
Yes, there’s an interplay between vagal nerve function and integrity, and autonomic nervous system function and integrity, and how we are doing
I think that mindfulness, meditation, stress reduction, getting good restful deep sleep, we certainly know that exercise helps dysautonomia of any kind, sometimes with our most impacted POTS patients they need to do certain exercises like recumbent exercises so they don’t get drops in their BP, increases in their heart rate, but those are some of the things we can do ourselves
The other thing, knowing that persons with migraine their number 1 comorbid condition is anxiety is getting them to have a match of how stressed they are about a particular condition to how bad it is
Sometimes there’s a mismatch.
Sometimes a patient who has a dysautonomia and migraine and has anxiety, because we screen them for it and we found, they have a sense that the magnitude of the problem the danger of the potential lethality of it is there and it freaks them out, because they’re feeling really abnormal
So what we try to do and we have Phd psychologists here who do biofeedback and that sort of thing, we try to say ‘alright, lets reset you so that you drop down how much you’re freaked out to match the condition’
‘Its not your fault, you did nothing to deserve it, and it’s real, but it’s not life threatening and we’re gonna help you through it’, you reframe it for them
Can you tell me a list of newer research or newer comorbidities?
I think the Ehlers-Danlos stuff is very fascinating to me and there’s more and more work on that
A paper that was really quite elegant is now about 3 years old or so, by Richard Lipton and Don Bues, was the mast study, they prospectively looked at it was a web based interview of 1500 people with and without migraine, and they looked to see what’s different about this group once you match them for age and sex, etc
It turns out that the group who had migraine, self-indentified migraine, were 4 times more likely to have insomnia, that’s a big problem in our migraine patients
over 3 times more likely to have anxiety
3 times more likely to have depression
interestingly, 3 times more likely to have ulcers or GI bleeding
and also more likely to have epilepsy or a seizure disorder
So, again, things to think about. We sometimes use NSAIDS, sometimes our patients themselves without asking us use a lot of NSAIDS, and NSAIDs is the number 1 reason for admission to the hospital with a GI bleed,
so knowing now based on the study that going into it, your patients with migraine are 3 times more likely than non migraine patients to have a GI bleed, I use NSAIDs with my patients, but I’m careful and I educate them,
so that is something that study that web based survey can alter how you do your practise, how you deal with your patients, it’s a great study
I think the whole idea of understanding comorbidities is for out of frame treatments, how to select meds, how to make sure you’re not using meds that are going to worsen the other comorbid condition
and then asking questions that you may not have asked before
the biggest one I think is when we talked about asking a simple question about trauma and getting a sense of whether there’s PTSD
That I’ve found has been one of the most impactful questions, once I understood the comorbidity of trauma and chronic migraine
Are there any pieces of advice you’d have for patients who are very overwhelmed or they don’t know where to start in managing so many different conditions at once?
Yes, the good news is these conditions are by and large not dangerous and not lethal
the bad news is like migraine they’re usually chronic
the good news is they can be impacted to some degree
we all get anxious, we all don’t have anxiety - it’s when the anxiety overwhelms you and gets in the way of your quality of life and your ability to function
we can slide somebody down the scale of anxiety to the normal anxiousness that we all have,
we can take somebody with POTS and we can treat them symptomatically so that they barely have POTS
these are the things that clinicians should be doing
I always tell patients, I try to empower them that, make your doctor work.
And say ‘these things are important to me, I need your help with them’ and make sure that they’re hearing that they’re listening to you and that they’re hearing you
because you know increasingly you have to be your own healthcare advocate, so don’t settle for somebody who’s not going to listen to you
it may be the 2nd or 3rd doc you find, but find someone who validates you, listens to you, is okay with thinking outside the box and wants to be creative in partnership with you to try to take on the whole person because you’re more than just a migraine disorder, you are a human who’s got other things going on too
#migraine world summit 2025 day three#migraine world summit 2025#migraine world summit#migraines#chronic migraines#migraine and comorbidities#i feel pukey
2 notes
·
View notes
Text
Kleptomania

Kleptomania is a psychological disorder in which a person experiences a compulsive urge to steal things, even if they have no financial need to do so and do not derive any particular pleasure from the act. This is an obsessive behavior that often results from an uncontrollable desire to steal, even though the person understands that the act is wrong.
In kleptomania, the person is unable to resist the urge to steal, even though they do not actually need the stolen goods. This makes it different from ordinary stealing or theft, which is often related to financial or other practical reasons.
A kleptomaniac may feel guilt and shame after stealing, but this feeling usually does not stop them from stealing again. They may also feel relief or excitement at the moment of stealing.
A kleptomaniac does not usually steal valuable items, but may steal small items that do not have much financial value.
Kleptomania is not fully understood, but it is believed to be a combination of biological, psychological, and environmental factors. Genetic predisposition, brain chemical imbalances, and past trauma may contribute to the development of the disorder. It may also be associated with other mental health disorders, such as anxiety disorders, depression, or personality disorders.
Kleptomanian hoito voi sisältää psykoterapiaa, kuten kognitiivista käyttäytymisterapiaa (CBT), joka auttaa muuttamaan varkauden taustalla olevia ajatusmalleja. Joissain tapauksissa lääkitys voi olla tarpeen, erityisesti jos häiriöön liittyy muita mielenterveyshäiriöitä, kuten masennusta tai ahdistusta.

Kleptomania on psykologinen häiriö, jossa henkilö kokee pakonomaista tarvetta varastaa tavaroita, vaikka hänellä ei olisi siihen taloudellista tarvetta eikä hän saa varastamisesta mitään erityistä nautintoa. Tämä on pakkomielteinen käyttäytyminen, joka johtuu usein hallitsemattomasta halusta varastaa, vaikka henkilö ymmärtää teon olevan väärin. Kleptomaniassa henkilö ei pysty vastustamaan halua varastaa, vaikka hän ei oikeastaan tarvitse varastettuja tavaroita. Tämä tekee siitä eroavan tavallisista varastamisesta tai varkaudesta, jotka usein liittyvät taloudellisiin tai muihin käytännöllisiin syihin. Kleptomaani voi tuntea syyllisyyttä ja häpeää varastettuaan, mutta tämä tunne ei yleensä estä häntä varastamasta uudelleen. Hän voi tuntea myös helpotusta tai jännitystä varkauden hetkellä.Kleptomaani ei yleensä varasta arvokkaita tavaroita, vaan se voi olla pieniä esineitä, joilla ei ole suurta taloudellista arvoa.
Kleptomaniaa ei täysin ymmärretä, mutta sen uskotaan olevan yhdistelmä biologisia, psykologisia ja ympäristötekijöitä. Geneettinen alttius, aivojen kemialliset epätasapainot ja aiemmat traumat voivat vaikuttaa häiriön kehittymiseen. Se voi myös liittyä muihin mielenterveyshäiriöihin, kuten ahdistuneisuushäiriöihin, masennukseen tai persoonallisuushäiriöihin.
3 notes
·
View notes
Note
Do you think Kakashi has OCD? The whole handwasching thing looks like a compulsion to me.
Ooh, good question!
*First, as a caveat and disclaimer, it’s hard to diagnose a fictional character and I am not making light of any IRL diagnoses, as OCD can be debilitating. So any and all answers are for entertainment-educational purposes only. If anyone suspects they may need additional services or therapy, please seek local professional help or if in immediate crisis, in the US, call 988*
As for your question.
Obsessive-Compulsive Disorder is considered an anxiety disorder or part of the anxiety family. Kakashi does have numerous symptoms of anxiety: he has anxiety attacks; displays symptoms of social anxiety; uses a security object in Icha Icha; has self-derogatory behaviors, etc….So with that said, there is such a thing as trauma-induced OCD, in which a person can develop OCD or OC symptoms following a trauma, and Kakashi has a ton of trauma. Couple that trauma with someone who already has a genetic predisposition to anxiety and depression (his dad displayed severe anxiety and depression) and you will have someone who is at increased risk of developing trauma-induced OCD.
For OCD, you have the obsessive and/or compulsive components. For example with the handwashing there’s usually an obsession that yields distress or discomfort, (e.g., being dirty, feeling contaminated, or something to that effect) and the compulsion, or action to relieve the distress of the obsession (e.g., the handwashing to remove the contamination). So, for Kakashi, what was his obsession? He had intrusive thoughts of seeing Rin’s blood to where those intrusive thoughts became an obsession. Would his washing Rin’s blood off be seen as a compulsion? Yes. It relieved his distress associated with intrusive thoughts of seeing Rin’s blood on his hands. What was his reasoning for the handwashing? To relieve distress.

When treating OCD, one of the first things assessed is if there is a history of trauma because untreated intrusive thougts can become obsessive thoughts. So,for Kakashi, did he have intrusive thoughts – Yes, definitely. Did the intrusive thoughts become obsessive – Yes. Now, here’s the tricky part, to be diagnosed with OCD, the person needs to have the presence of obsessional thoughts and/or compulsions, which Kakashi did have. However, the obsessions and compulsions must: 1) be time-consuming, last more than an hour a day, and 2) cause significant distress, and 3) impair work or social functioning. Does Kakashi meet this criteria? Yes, he had obsessions and compulsions. Do we know how much of his day they occupied – later we do, but more about that in a minute. Or how much his work and/social life was impaired? More about that later, as well.
If left untreated, OCD symptoms potentially last YEARS or even a lifetime. And we know how great nonexistent a mental healthcare system the shinobi world had, so Kakashi's would have been untreated. So, theoretically, if Kakashi has OCD, his symptoms would have lasted for years, into OG Naruto and into Shipudden, right? So, did his compulsions last for years? Or was it a one-time thing? More on that later. I know, so much left for later discussion, huh?
Obsessions and compulsions are often (spontaneously) replaced with new ones – it’s typically not just one and true OCD usually does not just go away on its own, just the obsessions and compulsions tend to cycle, with new ones appearing to replace the old ones, so, to outsiders, it looks like the disorder disappears. So, his handwashing may not have lasted years - that we know of. However, and a big HOWEVER, one can argue that he replaced his handwashing with visiting the graves of his loved ones for HOURS. EVERY. SINGLE. DAY and that DID, in fact, last for years and DID affect his work and social life functioning – he was HOURS late to everything because he was arguably compulsing at the gravesites/memorial stone.
Along the same line, the reasons he was at the graves - he has obsessive thoughts about being considered a "bad person," as demonstrated in the war arc when he keeps repeating that he's trash and scum and tells Obito he's right. Odds are those thoughts are always present, or preoccupy a lot of headspace and time, but he doesn't verbalize them publicly (usually only at the graves/memorial stone). That would be considered obsessive behavior.
One can potentially argue that wearing his mask in public could constitute OC behavior - as it appeared to cause marked distress to him if he was faced with removing the mask - even at an early age. Note it's not uncommon for adults with OC behavior to display OC behavior as children, but that's another answer... And yes, he doesn't wear a mask as Sukea, but he wears makeup and gets to "hide," so in essence, it's another mask.
So, all of that just to say in this very long answer, that, yes, in all likelihood, Kakashi has symptoms congruent with trauma-induced OCD with potential OC symptoms/behaviors beginning in early childhood. Or you could say that he already had OC behaviors as a kid, but trauma made it worse.
#kakashi hatake has ocd#kakashi hatake#hatake kakashi#anime therapy#kakashi needs therapy#naruto therapy#naruto#kakashi has ocd
24 notes
·
View notes
Text
Agoraphobia is an anxiety disorder characterized by a fear of being in public places, crowds, or situations where escape might be difficult. Here's a comprehensive overview:
# Definition and Diagnosis
Agoraphobia is a type of anxiety disorder that involves a fear of being in situations where escape might be difficult or embarrassing. To be diagnosed with agoraphobia, an individual must experience:
1. *Fear or anxiety*: A persistent fear or anxiety about being in public places, crowds, or situations where escape might be difficult.
2. *Avoidance behaviors*: Avoiding situations or places that might trigger anxiety, such as shopping malls, public transportation, or crowded events.
3. *Panic or anxiety*: Experiencing panic or anxiety when in a feared situation, which can lead to avoidance behaviors.
# Causes and Risk Factors
The exact causes of agoraphobia are unknown, but several factors can contribute to its development:
1. *Genetics*: Family history of anxiety disorders, including agoraphobia.
2. *Brain chemistry*: Imbalances in neurotransmitters, such as serotonin and dopamine.
3. *Traumatic events*: Experiencing a traumatic event, such as a panic attack or a embarrassing situation, in a public place.
4. *Learned behavior*: Learning to associate certain situations or places with anxiety or fear.
# Symptoms
Symptoms of agoraphobia can vary widely, but common experiences include:
1. *Panic attacks*: Experiencing panic attacks in feared situations, which can lead to avoidance behaviors.
2. *Anxiety*: Feeling anxious or fearful in situations where escape might be difficult.
3. *Avoidance behaviors*: Avoiding situations or places that might trigger anxiety.
4. *Dependence on companions*: Needing a companion to accompany them in public places.
5. *Limitations in daily life*: Avoiding daily activities, such as shopping or socializing, due to anxiety.
# Treatment
Treatment for agoraphobia typically involves a combination of psychotherapy, medication, and lifestyle changes:
1. *Psychotherapy*:
- Cognitive-behavioral therapy (CBT): helps individuals identify and change negative thought patterns.
- Exposure therapy: involves gradually exposing individuals to feared situations or places.
2. *Medication*:
- Selective serotonin reuptake inhibitors (SSRIs): can help reduce symptoms of anxiety and depression.
- Benzodiazepines: can help reduce symptoms of anxiety, but should be used with caution due to the risk of dependence.
3. *Lifestyle changes*:
- Regular exercise: can help reduce symptoms of anxiety and depression.
- Healthy eating habits: can help stabilize mood and energy.
- Mindfulness practices: can help reduce stress and increase self-awareness.
# Complications
If left untreated, agoraphobia can lead to various complications:
1. *Social isolation*: Avoiding social situations and public places can lead to social isolation and loneliness.
2. *Depression*: Agoraphobia can increase the risk of developing depression.
3. *Anxiety disorders*: Agoraphobia can increase the risk of developing other anxiety disorders, such as panic disorder or social anxiety disorder.
4. *Substance abuse*: Agoraphobia can increase the risk of developing substance use disorders.
# Prognosis
With proper treatment and support, individuals with agoraphobia can experience significant improvements in symptoms and quality of life:
1. *Reduced symptoms*: Treatment can help reduce the frequency and intensity of agoraphobic symptoms.
2. *Improved functioning*: Individuals with agoraphobia can experience improvements in daily functioning, including socializing and participating in activities.
3. *Increased self-awareness*: Treatment can help individuals with agoraphobia develop greater self-awareness, including understanding their triggers and coping mechanisms.
# Resources
If you or someone you know is struggling with agoraphobia, there are many resources available:
1. *National Alliance on Mental Illness (NAMI)*: A comprehensive resource for information on mental health conditions, including agoraphobia.
2. *Anxiety and Depression Association of America (ADAA)*: A non-profit organization providing resources, support, and treatment options for individuals with anxiety disorders, including agoraphobia.
3. *Crisis Text Line*: A 24/7 text messaging service providing support and resources for individuals in crisis.
2 notes
·
View notes
Text
Serotonin is a neurotransmitter, a chemical messenger that helps transmit signals in the brain. It plays a crucial role in various functions, including mood regulation, appetite, sleep, and overall emotional well-being. Serotonin is often referred to as the "feel-good" neurotransmitter because of its impact on mood.
Individuals who may experience low serotonin levels could include those with:
1. Depression: Low serotonin is often associated with depressive disorders, and many antidepressant medications aim to increase serotonin levels in the brain.
2. Anxiety disorders: Serotonin imbalances are linked to anxiety disorders, and medications that target serotonin are sometimes prescribed to manage anxiety.

3. Insomnia: Disruptions in serotonin levels can affect sleep patterns, contributing to insomnia or sleep disturbances.
4. Eating disorders: Conditions like bulimia and anorexia nervosa have been associated with alterations in serotonin levels, impacting appetite regulation.

5. Migraines: Serotonin is involved in the regulation of blood vessels, and low levels may contribute to migraines in some individuals.

It's important to note that serotonin levels can be influenced by various factors, including genetics, lifestyle, and environmental factors. If someone suspects they have low serotonin levels and it's affecting their mental health, it's advisable to consult with a healthcare professional for proper evaluation and guidance.
20 easy ways to boost your serotonin levels:
1. Regular exercise: Physical activity triggers the release of serotonin, promoting a positive mood and overall well-being.
2. Balanced diet with complex carbohydrates: Foods rich in tryptophan, like whole grains, contribute to serotonin synthesis, supporting emotional balance.
3. Mindfulness meditation: Practicing mindfulness reduces stress, leading to increased serotonin levels and improved mental health.
4. Adequate sleep: Consistent and quality sleep is crucial for serotonin regulation, influencing mood stability.
5. Exposure to natural sunlight: Sunlight stimulates serotonin production, positively impacting mood and sleep patterns.
6. Socializing and maintaining positive relationships: Positive social interactions foster feelings of connection and contribute to serotonin release.
7. Acts of kindness and helping others: Engaging in altruistic acts activates pleasure centers in the brain, boosting serotonin levels.
8. Engaging in hobbies: Pursuing activities you enjoy promotes a sense of accomplishment, positively influencing serotonin.
9. Listening to music: Music has the power to evoke emotions, triggering the release of serotonin and enhancing mood.
10. Spending time in nature: Nature exposure has been linked to improved mood and increased serotonin production.
11. Massage and touch: Physical touch, like massage, can stimulate serotonin release, promoting relaxation and well-being.
12. Deep breathing exercises: Practices like deep belly breathing reduce stress, supporting serotonin regulation.
13. Gratitude journaling: Reflecting on positive aspects of life enhances feelings of gratitude and potentially boosts serotonin.
14. Laughing: Laughter releases neurotransmitters, including serotonin, contributing to a positive mood.
15. Omega-3 fatty acids: Foods rich in omega-3s, like fatty fish, support serotonin production and overall brain health.
16. Yoga: Combining physical activity with mindfulness, yoga is associated with increased serotonin levels.
17. Regular sleep patterns: Consistent sleep schedules and quality sleep are crucial for serotonin regulation.
18. Limiting caffeine and alcohol: Moderation in caffeine and alcohol intake helps maintain optimal serotonin levels.
19. Positive affirmations: Practicing positive self-talk and affirmations contributes to a positive mindset and serotonin release.
20. Visualization: Imagining positive scenarios stimulates the brain to release serotonin, promoting a sense of well-being.
6 notes
·
View notes
Note
Hi Christina!! I know of conservative and democrat but I don’t know where my own political beliefs lay. I’m a mix of both red and blue pill. I believe in gun bans, free world class health care (im from Australia so I’ve always had that and feel so sorry for u guys that u don’t have it), I believe in welfare and upping the welfare so people can actually live of it, upping the minimum wage, helping students and those less fortunate. But I also believe in only two genders, not confusing children about genders in school, and I think people shouldn’t be allowed to transition to another gender as I believe they are severely mentally ill, and no happy person would ever want to change sex. I’m not religious btw. Idk what to call myself politically
In the US we would generally call that a moderate or someone who is center-left? You might also describe it as being socially conservative but economically liberal.
But (and my apologies for hijacking this ask, but if you've been around here for any amount of time, you knew this was coming) I want to talk a little bit about your position on the trans community. Why does maintaining a binary set of genders matter so much to you that it excludes trans people from your goal of "helping the less fortunate"? What are you afraid will happen if trans people are allowed to live the lives that are authentic to them? How are you imagining that will impact your life, and why are you so scared of that impact that you feel like it needs to be banned entirely?
Trans people aren't "severely mentally ill". They're just people who don't relate to the biopsychosocial gender role that they were assigned at birth. Trans, gender non-conforming, and intersex people have always existed. Many cultures have historically recognized more than two genders. Even within Western culture, we recognize lots of different gender expressions amongst cis people- girls can be tomboys or girly girls, women can be femme or butch, people can be androgynous... for a while, "metrosexual" was even a term for men who put effort into their appearance. All of those concepts are just gender expressions. The line at which they go from being "cis" to "trans" really just depends on culture and the person's perception of their own experience.
While there isn't a lot of research on why some people are trans and some aren't, but the research we do have seems to suggest that trans people are just born that way. It seems that being trans is, in part, genetic, and that trans people's brain structures are (on average) more similar to the brain structures of other people of the gender they identify as, rather than the gender they were assigned at birth. Being trans is not a "severe mental illness". It's just a different way of existing in the world. But even if it were a "severe mental illness" (which, again, it is not), don't mentally ill people have the right to seek treatment that will alleviate their suffering? Because that's what transitioning does. It alleviates suffering and discomfort associated with conforming to gender roles that don't align with a person's gender identity. You're right that very few people who are happy would undergo a medical transition to change their body. But the root of that unhappiness isn't mental illness. The root of that unhappiness is feeling like you don't belong in the body you have or the gender role that you've been given. And so transitioning alleviates that unhappiness.
And there's scientific data to back this idea up. Per the American Psychiatric Association, transgender individuals who transition experience long-term mental health benefits, including reduced anxiety, depression, and suicidality. And, per the Stanford University School of Medicine, trans people who start their transition as teenagers have better mental health than those who start their transition as adults. If you want trans people to "recover" from the "severe mental illness" you perceive them as having... transitioning is the way to let them do that.
But even if you don't care at all about trans people's health and wellbeing (and let's be real, I'm not convinced that you do), why should that mean that transitioning "shouldn't be allowed"? We let adults make all sorts of decisions about their bodies that they may regret down the line. For example, cis women are allowed to get boob jobs- gender affirming care within itself- regardless of whether or not they might regret it in the future. Cis women are allowed to take hormones in order to alter their menstrual cycle - often starting when they're in their teens- and we accept that they understand the long-term risks and benefits to their health that come with that choice. Why should trans people's choices about their bodies be any different? They're making informed decisions about the medical care they (and their doctors!) think will benefit them. Who are you to take that decision away from them?
There's a lot more I can say here and a lot of studies I can cite. I can tell you that every major U.S. medical and mental health organization, including the American Medical Association, the American Academy of Pediatrics, and the American Psychological Association, plus global health organizations including the Endocrine Society, the Pediatric Endocrine Society, the Society for Adolescent Health and Medicine, and the World Medical Association, and the World Health organization support access to age-appropriate, individualized medical transition for transgender youth and adults. The Australian Psychological Society is also included in that group, in case you were curious. I can tell you that the evaluations that trans people undergo in order to receive gender affirming care are extensive, even moreso for trans children. I can walk you through the reasoning behind introducing discussions of gender into classrooms early, and explain that children often have an understanding of gender by the age of three. I can talk about how the points people bring up when talking about trans people are the same ones they used about gay people fifteen years ago, and the world didn't end when countries started legalizing gay marriage. But I don't know if any of that will make a difference, because the reaction people have to trans people isn't really based in fact (no matter how much people will try to insist that it is). It's based in emotion.
So instead, I want to wrap up by asking this. How do you know that you are the gender you are? What makes you feel like a man or a woman? Are those things innate, are they cultural, are they both? How would you feel if one day, everyone started calling you a name of the opposite gender (for example, Michael instead of Michelle or vice versa) and insisting that you adopt the social roles of the opposite gender? What if you were forced into activities that you don't enjoy, with people who aren't like you? That would suck, right? You'd probably want to do whatever you could to be seen the way you feel on the inside, right? That's all trans people really want- to be seen for who they are. You can think that they're mentally ill or cringe if you want (although I really hope you won't), but don't legislate away their ability to pursue their happiness, even if you don't get why they would want that.
If you're interested in learning about trans issues more in-depth, I highly recommend ContraPoints' channel. She does a really good job of discussing transphobia and gender critical ideas while still being incredibly entertaining and fun.
youtube
3 notes
·
View notes
Text
Physical Therapy Clinic in New York City
Ehlers-Danlos Syndrome - Fatigue
Fatigue is particularly common in hypermobile EDS (hEDS). Contributing factors can include sleep disorders, muscle deconditioning (loss of muscle tone and endurance), headaches, and nutritional deficiencies. It is important to exclude other causes, such as anemia or a chronic infection.
The primary cause of EDS is related to defects in the synthesis, structure, or processing of collagen or other components of the extracellular matrix, which are essential for providing strength, support, and elasticity to various tissues, including skin, joints, blood vessels, and organs.
Can EDS cause extreme fatigue?
Conditions commonly seen in EDS and which may manifest as or exacerbate fatigue include sleep disorder, chronic pain, deconditioning, cardiovascular dysregulation, bowel and bladder dysfunction, psychological issues, and nutritional deficiencies. Feb 10, 2017
EDS is generally classified into several major types, including:
Classical EDS (cEDS): Caused by mutations in the COL5A1 or COL5A2 genes, leading to abnormalities in Type V collagen.
Hypermobile EDS (hEDS): This type is associated with hypermobility of joints and is believed to have a genetic component, although the specific gene mutations are not well-defined.
Vascular EDS (vEDS): Caused by mutations in the COL3A1 gene, leading to abnormalities in Type III collagen. vEDS is the most severe form of EDS and is associated with a high risk of arterial and organ rupture.
Kyphoscoliotic EDS (kEDS): Caused by PLOD1 or FKBP14 gene mutations, leading to collagen processing abnormalities.
Arthrochalasia EDS (aEDS): Caused by mutations in the COL1A1 or COL1A2 genes, leading to abnormalities in Type I collagen.
Dermatosparaxis EDS (dEDS): Caused by mutations in the ADAMTS2 gene, leading to abnormalities in the processing of collagen.
The genetic mutations in EDS result in weakened or structurally abnormal connective tissues, leading to the various symptoms and manifestations of the syndrome, including joint hypermobility, skin hyperextensibility, and vascular and organ problems.
Fatigue is a common symptom in individuals with EDS. While its exact cause is not fully understood, it likely results from a combination of factors, including chronic pain, poor sleep quality due to pain and joint instability, autonomic dysfunction, and the challenges of living with a chronic condition. Fatigue can significantly impact the quality of life for individuals with Ehlers-Danlos Syndrome, and its management is an essential aspect of their overall care.
Fatigue is a state of extreme tiredness, weariness, or lack of energy. It is a normal and common sensation that most people experience occasionally, especially after physical or mental exertion, lack of sleep, or periods of stress. However, when fatigue becomes chronic and persistent, lasting for an extended period despite adequate rest and sleep, it may indicate an underlying medical condition or other factors that require attention.
Fatigue can manifest in various ways, and its symptoms can include:
Physical tiredness: Feeling physically weak, heavy, or drained of energy.
Mental exhaustion: Difficulty concentrating, memory problems, or impaired cognitive function.
Sleep disturbances: Fatigue can disrupt sleep patterns, leading to difficulty falling asleep or staying asleep.
Reduced motivation: A lack of interest in activities and reduced productivity.
Irritability: Feeling easily annoyed or impatient.
Muscle weakness: Physical weakness or difficulty performing usual tasks.
Headache: Frequent headaches or migraines.
Dizziness: Feeling lightheaded or dizzy.
Slowed reflexes: Reduced reaction time and impaired coordination.
Mood changes: Fatigue can lead to feelings of sadness, anxiety, or depression.
Causes of fatigue can be numerous and may include:
Lack of sleep: Insufficient or poor-quality sleep can lead to fatigue.
Medical conditions: Chronic fatigue can be a symptom of various medical conditions, such as anemia, thyroid disorders, chronic pain, infections, and autoimmune diseases.
Psychological factors: Mental health issues like stress, anxiety, and depression can contribute to fatigue.
Medications: Certain medications may cause fatigue as a side effect.
Lifestyle factors: Poor nutrition, lack of physical activity, and excessive alcohol or caffeine consumption can contribute to fatigue.
Chronic illnesses: Conditions like fibromyalgia, chronic fatigue syndrome (CFS), and some autoimmune disorders can cause persistent fatigue.
It's important to differentiate between normal fatigue, which typically improves with rest and self-care, and chronic fatigue, which can be a symptom of an underlying health issue that requires medical attention. If you experience persistent fatigue or if it significantly interferes with your daily activities, discussing it with a healthcare professional to identify any underlying causes and receive appropriate evaluation and treatment is essential.
#physical health#physical therapy#ehlers danlos syndrome physical therapy#ehlers danlos syndrome#hypermobile ehlers danlos#back pain#chronic fatigue#chronically fatigued#health#health and wellness
3 notes
·
View notes
Text
Unveiling the Mind's Green Secret: How Endocannabinoids Shape Mental Health
World Suicide Prevention Day 10th September

Introduction
Mental health is a complex and multifaceted aspect of our overall well-being. Various factors contribute to the development and maintenance of mental health disorders, including genetics, environment, and neurobiology. In recent years, there has been growing interest in the role of endocannabinoids in influencing mental health. Endocannabinoids are naturally occurring compounds within our bodies that interact with the endocannabinoid system, which plays a crucial role in regulating various physiological processes. This article aims to explore the influence of endocannabinoids on mental health, focusing specifically on their effects beyond the medical use of CBD.
Understanding the Endocannabinoid System
To comprehend how endocannabinoids influence mental health, it is essential to have a basic understanding of the endocannabinoid system (ECS). The ECS consists of three main components: endocannabinoids, receptors, and enzymes. The two primary endocannabinoids are anandamide (AEA) and 2-arachidonoylglycerol (2-AG), which bind to cannabinoid receptors (CB1 and CB2) located throughout the central nervous system and peripheral tissues. These receptors modulate various physiological processes, including mood, stress response, and cognitive function.

How endocannabinoids influence mental health
Regulating Emotional States: Endocannabinoids have been linked to the regulation of emotional states, including mood and anxiety. Studies suggest that anandamide, one of the primary endocannabinoids, interacts with CB1 receptors in brain regions associated with emotional processing, such as the amygdala and prefrontal cortex. By modulating neurotransmitter release and synaptic plasticity, endocannabinoids contribute to the regulation of mood and emotional responses.
Stress and Resilience: Stress is a significant factor that can impact mental health, and the ECS appears to play a crucial role in modulating the stress response. When faced with stress, the release of endocannabinoids is enhanced, which helps to dampen the stress response and restore homeostasis. The activation of CB1 receptors in brain regions involved in stress regulation, such as the hypothalamus and hippocampus, can reduce the release of stress hormones, thereby promoting resilience and emotional stability.

Neuroplasticity and Neurogenesis: Neuroplasticity, the brain's ability to reorganise and form new connections, is fundamental for learning and memory processes. Endocannabinoids have been found to play a role in modulating neuroplasticity by facilitating synaptic plasticity and neuronal communication. Furthermore, emerging evidence suggests that endocannabinoids may also promote neurogenesis, the formation of new neurons in certain brain regions, including the hippocampus. These processes are essential for mental well-being and cognitive function.
Endocannabinoids and Mental Disorders: Given the involvement of endocannabinoids in various aspects of mental health regulation, it is unsurprising that alterations in the ECS have been associated with mental disorders. Studies have linked dysregulation of the ECS to conditions such as depression, anxiety disorders, post-traumatic stress disorder (PTSD), and schizophrenia. Understanding these associations provides insights into potential therapeutic targets and the development of novel treatments.
Conclusion
Endocannabinoids play a significant role in influencing mental health by regulating mood, stress response, cognitive function, and reward-related behaviours. Understanding the intricate interplay between endocannabinoids and the endocannabinoid system can provide valuable insights into the development and treatment of mental health disorders. Further research is needed to fully comprehend the complexities of this system and its potential therapeutic implications. By unravelling the mysteries of endocannabinoids, we may pave the way for novel approaches to enhance mental well-being.
If you want to help raise awareness about mental health, you can donate here to Mental Health UK.
#health#mental health#mental health awareness#endocannabinoids#endocannabinoidsystem#cbd#cannabis#health and wellness#feelgreatagain#budandtender
2 notes
·
View notes
Text
Anti-Anxiety Drug Market Size, Share, Trends, Key Drivers, Demand and Opportunities
Executive Summary Anti-Anxiety Drug Market:
The Anti-Anxiety Drug Market Market research report concentrates on the foremost competitors of the global market and delivers information about the company overview including contacts, product portfolio, key developments, price, cost, value, volume, revenue, capacity, and production. Furthermore, businesses can decide upon the strategies about the product, customer, key player, sales, promotion or marketing by acquiring a detailed analysis of competitive markets. Charts, TOC, graphs and tables included in the report help understand the market size, share, trends, growth drivers and market opportunities and challenges. In the Anti-Anxiety Drug Market Market report, the complete and crystal clear outline of the Anti-Anxiety Drug Market Market is penned down which is useful for many businesses.
Discover the latest trends, growth opportunities, and strategic insights in our comprehensive Anti-Anxiety Drug Market Market report. Download Full Report: https://www.databridgemarketresearch.com/reports/global-anti-anxiety-drug-market
Anti-Anxiety Drug Market Market Overview
**Segments**
- On the basis of drug class, the global anti-anxiety drug market can be segmented into SSRIs (Selective Serotonin Reuptake Inhibitors), SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors), Benzodiazepines, Beta Blockers, and Others. SSRIs are one of the most commonly prescribed drugs for anxiety disorders due to their effectiveness and lower risk of dependence compared to benzodiazepines. SNRIs are also widely used to treat anxiety and depression by affecting the levels of neurotransmitters in the brain. Benzodiazepines act quickly to reduce anxiety symptoms but are associated with a higher risk of tolerance and dependence. Beta blockers are primarily used to control physical symptoms of anxiety such as rapid heartbeat and trembling.
- Based on distribution channel, the market is divided into hospital pharmacies, retail pharmacies, and online pharmacies. Hospital pharmacies are crucial in providing anti-anxiety drugs to inpatients and outpatients under medical supervision. Retail pharmacies serve as a convenient source for patients to obtain their prescribed medications for anxiety disorders. Online pharmacies are gaining popularity for their accessibility and convenience, allowing patients to order medications from the comfort of their own homes.
- By indication, the market is categorized into generalized anxiety disorder, panic disorder, social anxiety disorder, obsessive-compulsive disorder, and others. Generalized anxiety disorder is one of the most prevalent anxiety disorders characterized by excessive worrying and anxiety about various aspects of life. Panic disorder involves recurrent, unexpected panic attacks leading to intense fear and physical symptoms. Social anxiety disorder is marked by extreme self-consciousness in social situations, while obsessive-compulsive disorder entails recurring thoughts and behaviors.
**Market Players**
- Some of the key players in the global anti-anxiety drug market include Pfizer Inc., GlaxoSmithKline plc, Eli Lilly and Company, Johnson & Johnson Services, Inc., AstraZeneca, Novartis AG, Merck & Co., Inc., Sanofi, AbbVie Inc., and Bristol-Myers Squibb Company. These major market players focus on research and development activities to introduce novel anti-anxiety drugs with improved efficacy and safety profiles. They also engage in strategic collaborations, partnerships, and acquisitions to expand their product portfolios and geographical presence in the competitive market landscape.
Moreover, there is a growing focus on the development of precision medicine approaches for the treatment of anxiety disorders. Precision medicine involves tailoring treatment strategies based on individual genetic, environmental, and lifestyle factors to optimize therapeutic outcomes. By leveraging advances in genomics, biomarker research, and artificial intelligence, pharmaceutical companies are exploring new avenues for identifying biomarkers associated with anxiety disorders and developing targeted therapies that offer improved efficacy and reduced side effects. This personalized approach to treating anxiety not only enhances patient responses to medication but also aids in the prediction of treatment outcomes, leading to more effective and individualized care for individuals suffering from anxiety disorders.
Moreover, there is a rising emphasis on precision medicine approaches tailored to treat anxiety disorders by considering individual genetic, environmental, and lifestyle factors. Pharmaceutical companies are leveraging advancements in genomics, biomarker research, and artificial intelligence to identify biomarkers associated with anxiety disorders and develop targeted therapies with improved efficacy and reduced side effects. This shift towards personalized medicine not only enhances patient responses to treatment but also aids in predicting treatment outcomes, leading to more effective and individualized care for those suffering from anxiety disorders.
Another significant factor shaping the anti-anxiety drug market is the increasing awareness and destigmatization of mental health concerns globally. As societies become more open to discussing mental health issues and seeking help for psychological conditions, the demand for anti-anxiety medications and mental health services is on the rise. Governments, advocacy organizations, and healthcare providers are actively promoting mental health awareness campaigns, education initiatives, and early intervention programs to address anxiety disorders proactively. This shift towards a more supportive and understanding approach to mental health is driving the adoption of anti-anxiety medications and psychotherapeutic interventions, thereby fueling market growth and expanding access to treatment options for individuals with anxiety disorders.
Furthermore, the COVID-19 pandemic has significantly impacted the global anti-anxiety drug market, with heightened stress, uncertainty, and social isolation leading to a surge in mental health issues, including anxiety disorders. The pandemic has accelerated the need for effective pharmacological treatments and mental health support systems to address the psychological repercussions of the crisis. This has spurred the development and adoption of new anti-anxiety drugs, digital mental health platforms, and telepsychiatry services to meet the increasing demand for anxiety treatment in the post-pandemic era.
In conclusion, the global anti-anxiety drug market is witnessing transformative changes driven by digital therapeutics, precision medicine, mental health awareness initiatives, and the consequences of the COVID-19 pandemic. As stakeholders in the healthcare industry collaborate and innovate to address the complexities of anxiety disorders, the market is poised for growth, evolution, and advancements in patient care moving forward.
The Anti-Anxiety Drug Market Market is highly fragmented, featuring intense competition among both global and regional players striving for market share. To explore how global trends are shaping the future of the top 10 companies in the keyword market.
Learn More Now: https://www.databridgemarketresearch.com/reports/global-anti-anxiety-drug-market/companies
DBMR Nucleus: Powering Insights, Strategy & Growth
DBMR Nucleus is a dynamic, AI-powered business intelligence platform designed to revolutionize the way organizations access and interpret market data. Developed by Data Bridge Market Research, Nucleus integrates cutting-edge analytics with intuitive dashboards to deliver real-time insights across industries. From tracking market trends and competitive landscapes to uncovering growth opportunities, the platform enables strategic decision-making backed by data-driven evidence. Whether you're a startup or an enterprise, DBMR Nucleus equips you with the tools to stay ahead of the curve and fuel long-term success.
This comprehensive report provides:
Improve strategic decision making
Research, presentation and business plan support
Show emerging Anti-Anxiety Drug Market Marketopportunities to focus on
Industry knowledge improvement
It provides the latest information on important market developments.
Develop an informed growth strategy.
Build technical insight
Description of trends to exploit
Strengthen competitor analysis
By providing a risk analysis, you can avoid pitfalls that other companies may create.
Ultimately, you can maximize your company's profitability.
Browse More Reports:
Global Hair Gel Market Global H2 Receptor Antagonist Market Global Gummy Multivitamins Market Global Gummy Candy Market Global Grid Controller Market Global Green Cell Foam Market Global Graphene Market Global Gout Treatment Market Global Glycosidases Market Global Glycerinee Market Global Glamping Market Global Gesture Control Software Market Global Geriatric Medicines Market Global Gel Permeation Chromatography (GPC) Market Global Gambling Market Global Functional Safety Products Market Global Food Testing, Inspection and Certification Market Global Food Grade Lubricants Market Global Food Enzymes Market Global Food Disinfection Equipments Market
About Data Bridge Market Research:
An absolute way to forecast what the future holds is to comprehend the trend today!
Data Bridge Market Research set forth itself as an unconventional and neoteric market research and consulting firm with an unparalleled level of resilience and integrated approaches. We are determined to unearth the best market opportunities and foster efficient information for your business to thrive in the market. Data Bridge endeavors to provide appropriate solutions to the complex business challenges and initiates an effortless decision-making process. Data Bridge is an aftermath of sheer wisdom and experience which was formulated and framed in the year 2015 in Pune.
Contact Us: Data Bridge Market Research US: +1 614 591 3140 UK: +44 845 154 9652 APAC : +653 1251 975 Email:- [email protected]
Tag
Anti-Anxiety Drug Market Market Size, Anti-Anxiety Drug Market Market Share, Anti-Anxiety Drug Market Market Trend, Anti-Anxiety Drug Market Market Analysis, Anti-Anxiety Drug Market Market Report, Anti-Anxiety Drug Market Market Growth, Latest Developments in Anti-Anxiety Drug Market Market, Anti-Anxiety Drug Market Market Industry Analysis, Anti-Anxiety Drug Market Market Key Player, Anti-Anxiety Drug Market Market Demand Analysis
0 notes
Text

Earwax contains a treasure-trove of information about our health—including cancer status. _ Emma Suttie
We all likely take earwax for granted—and prefer not to think about it. However, the under-appreciated substance does more than keep your ears clean and free of debris—scientists have discovered that it contains a goldmine of health data. Beyond that, earwax might be able to signal diseases like diabetes and cancer.
Cerumen is the technical term for earwax. Ceruminous and sebaceous glands secrete a substance in the external auditory canal that mixes with sweat, hair, dust, and other debris. The purpose of cerumen is to keep the ears lubricated and clean and create a barrier to discourage the entry of bugs and other foreign objects that might infiltrate and wreak havoc.
In 2006, a landmark study discovered that earwax varies between people, finding a single nucleotide polymorphism (SNP) that determines what type of earwax a person has—wet or dry. Of note, a SNP (pronounced “snip”) is the most frequent type of genetic variation among people, and each SNP signifies a difference in a single DNA building block (nucleotide).
Subsequent work found that earwax type also varies among different ethnic groups. Dry earwax is prevalent among East Asians, and the wet type is most common among those of European and African descent.
Interestingly, the gene that determines earwax type is also responsible for whether your armpits smell, and those with the dry type generally produce less sweat and body odor—traits found more in East Asian populations.
The Science of Cerumen
In recent years, earwax has gone from a relatively untapped biological resource to the focus of scientific study, particularly diagnostics.
In 2019, scientists developed a new way to detect cancer using earwax, publishing their findings in Nature. The researchers called the new method the Cerumenogram. The study collected earwax from two groups: people with cancer (lymphoma, carcinoma, or leukemia) and those without cancer.
When tested, 27 biological markers could discriminate between cancer patients and healthy controls 100 percent of the time. The new test has the potential to be a quick, non-invasive, inexpensive, and highly accurate test for cancer diagnosis.
In a subsequent study, published in April, the authors expanded on their findings, demonstrating the Cerumenogram’s effectiveness in detecting metabolic changes associated with cancer.
Nelson Roberto Antoniosi Filho, a professor of chemistry at the Federal University of Goiás in Brazil and an author of both studies, explained the findings and their implications for finding cancer early.
In 2019, he and his colleagues demonstrated that earwax could be used to diagnose any cancer at any stage, which they have since verified by studying more than 1,000 samples, he said. Their most recent research showed that the same method can detect pre-cancer stages, diagnose metabolic remission of cancer, and distinguish between benign and malignant tumors.
Filho says he and his colleagues have found that their method detects cancer earlier than traditional tests or expensive imaging, meaning that treatment can start sooner, be less aggressive, and cost less—often before the cancer fully develops—significantly improving the chances of success. For patients in remission, it also clearly shows the moment they are cured, ending years of anxiety and uncertainty, which often last for 5 years or more of follow-up.
Filho says he and his team are currently focusing their studies on metabolic disorders like diabetes mellitus, xeroderma pigmentosum, cancer, and Parkinson’s and Alzheimer’s diseases. They are also beginning to focus on autism and depression.
A 2020 study led by Dr. Andrés Herane-Vives, a psychiatrist, scientist, and lecturer at University College London and King’s College London in the UK, collected earwax and measured for cortisol comparing it with standard measurements using hair. Although hair samples are typically used to measure long-term cortisol levels in chronic stress or endocrine dysregulation conditions, the study’s results indicated that using earwax samples may yield more accurate results.
In another 2020 study using earwax, Herane-Vives and his team found that glucose levels reflected in earwax matched levels found in blood, and that earwax glucose reflected short- and long-term blood glucose with 59 percent more accuracy than the HBA1c test, the standard blood test used to measure blood sugar levels as well as monitoring and diagnosing diabetes.
Herane-Vives explained why earwax is unique and offers a more complete picture for tracking certain conditions over time.
“We needed a new specimen to reflect chronic levels of different biomarkers, because so far, the samples that we’ve got—like saliva, urine, or blood—are not able to accumulate substances, and only give us a snapshot,” he told The Epoch Times.
One of the ways earwax was collected in both studies was using a self-sampling device that Herane-Vives has since further developed through his biotech company, Trears Biomarkers. The device allows patients to collect their earwax in the comfort of their homes, which can then be sent through the post to a lab for analysis.
The Earwax Self-Sampling Device developed by Trears Biomarkers. Courtesy of Dr Andrés Herane-Vives
Herane-Vives says the future of cerumen research and Trears, is to improve diagnosis so people get the treatments they need.
“We don’t need new treatments, we need better diagnosis,” he said.
The device could change the game for many patients with chronic diseases like diabetes, allowing them to collect samples at home for regular testing, making it easier, more reliable, and vastly less expensive, in addition to easing an enormous financial burden on the health care system.
The only challenge of using earwax may be that some people lack a sufficient amount, making testing difficult.
“A few people produce little earwax or don’t produce earwax at all. In this regard, we are also finalizing studies to overcome this problem,” Filho said.
The combination of tests like the Cerumenogram and self-sampling devices that allow people to collect their earwax without having to visit a doctor’s office or lab offers an exciting vision of the future of medicine.
Filho said there is no doubt that earwax analysis will become routine in the coming years.
In Brazil, the approach is already being used to diagnose tumor development, including both cancerous stages and pre-cancerous conditions, as well as to assess whether the cancer is in remission, he said.
“This examination has been routinely applied in one of the largest oncology hospitals in the country or Hospital Amaral Carvalho (Jaú-São Paulo), and we are working to ensure that in the next 5 years, all public educational and research institutions in the country offer this examination at the lowest possible cost to the entire population.”
For the rest of the world, he said, the Cerumenogram will become as common as a blood test within the next decade.
“Perhaps in the future, while we listen to music through headphones, those headphones will diagnose our health conditions and tell us what precautions we need to take. I suggest that a samba be played to indicate that health is good!”
0 notes