#interpersonal neurobiology
Text
Green light heidi offers interpersonal neurobiology courses that you can purchase. These classes are designed to provide an insight on how mind works and the relationship between mind, and body. Learn from an expert psychotherapist, green heidi. Learn how neurobiology works and shapes the way you think. You can use the knowledge to improve your life. You can learn so much from these classes than at school. For more details, visit the website.
0 notes
Note
I have always been wary of the psychiatric industry, but its only very recently that i started to read anti-psychiatric works. Your blog is the first time i saw that the "chemical imbalances causing mental illness" is a myth, and honestly its something im having a hard time wrapping my head around.
Is it that mood regulation struggles, labelled as a mental illnesses, has more to do with outside factors instead of the person "just being that way"? Is it therefore unlikely for someone to have struggles with mood regulation if they cant identify any external causes that would cause them to be, for example, extremely agoraphobic or to have anger management issues? Im asking this for myself mainly, cause i always had intense agoraphobia no matter how i often go outside my home (in fact it was worse when i was a teen and i was outside the house in even more back then). I cant think of any reason for me to be like this than chemical imbalances in my brain.
the specific 'chemical imbalance' myth i was talking about in this post is the idea that depression is caused by low serotonin, and that therefore SSRIs—serotonin re-uptake inhibitors, ie drugs that cause a higher level of serotonin in the brain—ought to cure or at least ameliorate depression. this conjecture is belied by the fact that SSRIs don't, at a population level, reliably perform better than placebo.
although a neurobiological cause of 'mental illness' has long been the holy grail of psychiatry, the serotonin imbalance myth is far from the only hypothesis that psychiatrists and neuroscientists have proposed. so, a critique of the serotonin myth is not synonymous with, or generalisable to, a critique of every neurobiological mechanism purported to explain psychiatric diagnoses. you may be interested to know, though, that genomics and neuroscience have not identified a biological cause of any psychiatric diagnosis (p. 851).
all human experiences are biologically instantiated, including in the brain and wider nervous system. we are embodied beings. however, it is a leap to assume that such instantiation is automatically equivalent to a causal explanation or disease etiology. in other words, to deny that psychiatric diagnoses are known to be biologically caused does not mean we deny that thoughts and thought patterns express in the physical matter of neuroanatomy. this is a major philosophical sticking point to keep in mind whenever you're looking at something like, eg, a study that purports to show 'brain differences' in those assigned a certain psychiatric diagnosis. another thing to consider is whether these papers are plagued with methodological issues or financial conflicts of interest.
i can't possibly tell you why you exhibit agoraphobia. however, when i talk about social, economic, and environmental factors that may contribute to the patterns of behaviour labelled as 'mental illness', i'm talking about much more than the individual choice to leave your house. since phobias are 'anxiety disorders', i might start by probing into questions like: is the world you live in safe? do you perceive it as safe? do you or your community face existential threats that may confront you more obviously when you go outside? are you nervous around other people, and if so, might that be connected to fears (well-founded or not) about interpersonal violence and harm? do you think any of these anxieties may be connected to the hostility and inaccessible design of the social environment and economic conditions?
human behaviour and thought varies. some of those variations may be totally benign; others may be helpful or harmful to the person living with them. it would be weird if every single one of the 8 billion people on earth experienced precisely the same amount of anxiety about any situation, no? all of this is to say: yeah, it's entirely possible you have been, for one reason or another (genetic, neuroanatomical, social, &c) predisposed to experience high, even debilitating levels of anxiety when leaving your home. most human characteristics develop from a tangle of social, environmental, material causes—ie, from a combination of 'nature' and 'nurture'. what doesn't follow, though, is the claim that there is therefore a discrete, 'diseased' element of your brain or brain functioning that can simply be cured or eliminated through psychiatric intervention.
it is a critical point of anti-psychiatry to challenge psychiatric and neuroscientific claims to neurobiological determinism where psychiatric diagnoses are concerned. this is for many reasons, including: a) that these claims have not been demonstrated to actually be true [see above]; b) that they rob pathologised people of agency and self-determination [see: you're too sick to know you're sick, and the doctor will fix you now]; c) that they are often pushed by pharmaceutical companies with financial interests, or grant-funded researchers with... financial interests; d) that they are politically seductive in various eugenic, hereditarian discourses that seek to eliminate the biologically 'unfit' element from society.
1K notes
·
View notes
Text
[“An unfortunate reality that still permeates many psychotherapy offices is the archaic belief that these trauma-bonded relationships can be remedied by teaching problem-solving strategies, communication skills, and conflict-management techniques. While these teachings are beneficial and certainly have their place when working within dysfunctional relationships, it is my personal and professional experience that these interventions do not access the core of what is disconnecting partners, nor do they get to the heart of the matter regarding the pathways that create meaningful change.
During my early years of counseling, helping couples and individuals on their relationship issues, I would also teach my clients how to apply these old techniques and strategies, but I felt a sense of insufficiency and guilt. I knew there was more underneath the surface of what they shared with me, which signaled the deeper issues that were so clear to me I could almost touch them. I knew that these painful tethers bonding my clients in fear and distress were the hidden patterns of unmet needs. I knew this. But how could I help my clients not just understand what was happening but deeply experience it and become conscious of it enough to reach out to their partner with vulnerability and clarity, to show up for their partner with openness and acceptance and make meaningful changes?
So I went on an exploration. I dove into clinical approaches like attachment theory and emotion-focused therapy. I studied somatic therapies and microexpressions and learned the language of the emotional body. I became a student of ancient philosophies, spirituality, and esoteric wisdom to acquaint myself with the meaning of life and become comfortable discussing existential truths that can sometimes paralyze us. I studied interpersonal neurobiology and various sciences to help me conceptualize the human brain and body in a state of connection or disconnection. I absorbed it all. One key takeaway I learned from my immersion into the human experience is this: Our relationships act as a mirror into the depths of our own selves. They show us what we accept, what we reject, and what we hide, sometimes even from ourselves. Our relationship dramas are the reenactments of unresolved traumas still locked within our mind and body, signaling our conscious mind where healing can take place. In this way, the journey to connection with another must be a simultaneous journey through reconnection with the self. This book is that journey.”]
laura copley, from loving you is hurting me: a new approach to healing trauma bonds and creating authentic connection, 2023
148 notes
·
View notes
Text
Going a little more in depth with this past journal, reading more about maladaptive self-control and stumbled upon “overcontrolled” individuals.
This has little to do with being controlling or manipulative of others, and has everything to do with having very strict control towards oneself.
Like the trap of selflessness, having self-control is considered a good trait to have and cultivate. A skill people should aim to achieve. And like with selflessness, there’s almost no research in the harmful aspects of when it gets too much. People are left without resources and help is nonexistent. Because it’s not considered a “problem”. The more self-control you have, the better.
Indeed, self-control is often equated with success and happiness—and failure in self-control characterizes many of the personal and social problems afflicting modern civilization. Yet, emerging research shows that too much self-control can be equally problematic. Excessive self-control often results in social isolation, poor interpersonal functioning, and severe and difficult-to-treat mental health problems (…) they are unable to let go of control even when they desperately desire to do so and they struggle to form long-lasting intimate bonds that are essential for emotional well-being. Thus, overcontrol works well when it comes to sitting quietly in a monastery or building a rocket to fly to the moon, but it creates problems when it comes to social connectedness.
(…) Core bio-temperamental (genetic) differences between people may help explain why so many of our treatment approaches have proven to be less effective in treating overcontrolled problems—that is, you cannot simply do, think, or accept your way out of a brain-based behavioral problem.
(…) When you’re lonely, it’s hard to feel happy no matter how much you might try to accept, reappraise, or change your circumstances, keep busy, exercise, or distract yourself. In the long run, we are tribal beings—and we yearn to share our lives with other members of our species. It is what we were born to do. (x)
The whole issue isn’t that you’re doing something wrong or that your approach is incorrect. You’re probably stuck inside of your own mind, unable to do much to change.
(…) Many treatments focus inward, attempting to help people better regulate their emotions, change dysfunctional thinking, or learn to restrain problematic impulses. However (…) people with excessive self-control don’t need to learn to work harder, think more correctly, or better restrain their emotions (…) Overcontrol can severely disrupt the fluid and natural give-and-take that is part of relationships when they are functioning well. (x)
It doesn’t matter how social you are - that’s not the problem - if you fail to achieve the safety you need to be able to connect, then it’s likely you won’t be able to connect properly with others. And being strict as you are, makes it harder, because you may seem unapproachable, among other things.
(…) individual wellbeing is inseparable from the feelings and responses of the larger group or community. Thus, what a person feels or thinks inside or privately is considered less important (…) what matters most is how a person communicates or socially signals inner or private experience to other members of the tribe and its impact on social connectedness.
(…) overcontrolled individuals have a heightened bio-temperamental threat sensitivity that makes it more difficult for them to enter into their neurobiologically based social-safety system. When individuals feel safe, they naturally experience a desire to explore and flexibly communicate with others.
(…) emotional loneliness secondary to social-signaling deficits represent the core problem for disorders of overcontrol (x)
Again, if you have failed to learn how to signal socially, the unwritten rituals and rules. It will increase feelings of otherness, despite attempts to stay close. Maybe you over control to compensate for what you’re lacking, it gives you a sense of safety after all; and maybe the emotional loneliness is most likely due to repeated episodes of neglect and rejection from peers.
Overcontrol is a problem of emotional loneliness (…) not necessarily lack of social contacts but lack of social connectedness (x)
Overcontrol is associated with a number of difficult-to-treat disorders, such as OCD, Treatment-Resistant Depression, eating disorders, anxiety disorders and Cluster A and C Personality Disorders (OCPD, SZPD, PPD, AVPD).
(…) Part of the problem is the disorders of over-control are often not recognized; the price of prosocial behavior may come at an enormous cost to an individual in terms of flexiblity of cognition, feelings of safeness, interpersonal connectedness, and sense of being valued and appreciated, but these costs often have social benefit to the larger community, so others may not recognize the signals of the person who is suffering when their contributions and habits of mind are costing them too much.
(…) Whereas under-control is linked to substance abuse, criminal activities, domestic violence, financial difficulties, teen pregnancy, smoking, obesity and other difficulties; over-control is pro-social and often valued. (x)
Introversion or shyness can mask overcontrolling behaviour, and it’s probably very difficult to pinpoint where it stops being diligence and starts becoming an actual disordered coping mechanism.
(…) people who have the overcontrol trait have the following four’ core deficits’:
Lack of Receptivity and Openness— You tend to be risk-averse and hyper-vigilant. You may avoid new and novel experiences and can be dismissive of other people’s input and feedback.
Lack of Flexible Responding— You may have a compulsive need for structure and order. You plan and rehearse everything. Your life may be governed by rigid rules you impose on yourself. You may also censor yourself and other people’s behavior with high moral standards.
Lack of Emotional Expression and Awareness— You inhibit spontaneous emotional expression, or maybe you have expressions that do not match how you feel on the inside (e.g. you smile when you are distressed). You also tend to diminish your own distress and be stoic about everything.
Lack of Social Connectedness and Intimacy— You may appear distant and aloof and keep people at arm’s length. You may also compare yourself with others often and feel envious and bitter.
(…) Interacting with people and building intimacy involves many factors that are outside of your control, and the fear of losing control may cause you to withdraw further from the social world. You may have a lot of social ‘contact’, but not genuine, deep, and whole-hearted connections. This leaves you in a place of deep loneliness. You may appear normal, but the longing for someone who truly ‘gets’ you remain.
Overcontrol is often not recognized. Unlike people who are under-controlled, those who are over-controlled are private and reserved. Their ability to tolerate the high amount of pain and distress means they rarely seek help. Even within the mental health field, people who are over-controlled are not causing a scene or drawing any attention to themselves. This means they often slip through the net and do not receive the help they deserve.
(…) Instead of being on the ‘anxious’ spectrum, people who severely fear losing control are more likely to have avoidance attachment patterns — at least in terms of their behaviors. Through early experiences, you might have developed a schema that tells you reaching out for help is futile, or even dangerous. When you reach out for help, you were dismissed or even punished. Thus, you have learned to rely on absolutely no one but yourself. The message you have internalized is that vulnerability puts you at risk, so it is best that you hide it, suppress it, so no one can take advantage of you. Even as a child, ’emotional over-regulation, rather than under-regulation, is observed in your behaviors (Martins et al., 2012). If you have adopted this survival strategy as a child, you may continue with the same pattern. Even now, you see yourself as being completely self-reliant. You tend to hide your true self and avoid close bonds. Instead of support from others, self-restraint, discipline, the accumulation of knowledge, resources, and power are what you rely on to feel safe in life.
(…) When a child is chronically neglected, or when their primary caregivers are not responsive to or reject their needs, they may learn to diminish and reject their own needs and feelings as a way of coping. Emotions are there to signal us what we need; but if your experience has taught you that there is ‘no point’ in knowing your needs, for they will never be met, you would of course find it easier if you are no longer aware of your needs. After all, continuing to be made aware of our needs and not having them met is a painful state to be in. You may recognize the value of relationships and have a strong desire for them, but have difficulty trusting others. Even inside you feel anxious and worry about others leaving you (Anxious attachment style), you would rather not risk seeking out the attachment and be rejected. Instead, you fall back on the set of trialed- and true overcontrol strategies to try and get your needs met. (x)
57 notes
·
View notes
Text
will you still love me when i’m no longer young and beautiful’ ive never wanted anything more than you fat and old and wrinkled and at the apex of a life we created together. i love you like the sun loves brown eyes. i love you like the piano loves the spotlight. are you listening to me? you are to me what heartbreak is to a country singer. i love you like innumerable generations of girls in rooms have loved each other in darkness and in peace. the love i carry for you lives in the same place as my love for the ocean. it lives before words, before consciousness, before knowledge.
in university they teach us about interpersonal neurobiology. that love lives deeper in the brain than anything other than breath and water. it is not a lecture where i learn this lesson but instead waking up with you the morning before class. i learn it in eating sunshine and your eyelashes for breakfast. am i being clear? loving you is contingent on nothing so paltry as the corporeal. it’s not dimmed by age spots or creaking joints. you will always be the most beautiful woman in the world but never more than when i get to see our history hidden behind crow’s feet and aching knees
3 notes
·
View notes
Text
ADHD Informative Post Pt. 2
Causes
As stated in the first part (on @fqiryinfo Instagram), a heavily theorized cause of ADHD is a lack of dopamine to the pre-frontal cortex. Genetics obviously play a major role in that, however scientists are also researching the possibility of brain injuries, exposure to environmental risks (like lead) during pregnancy or early childhood, alcohol or tobacco use during pregnancy, premature delivery, and low birth weight as possible risk factors. Having these risk factors does not necessarily equal having ADHD. Another neurotransmitter besides dopamine that may contribute to ADHD symptoms is norepinephrine. Certain parts of the brain have been noted to be decreased in volume, as well as low iron and zinc levels causing a higher risk for ADHD symptoms and even a higher severity of symptoms. Despite common misconceptions, ADHD has *no* connection with sugar currently noted and has nothing to do with parental styles.
Treatment - Medication
Medicated treatment is typically broken down into three groups. These are long-lasting stimulants (like Adderall XR, Vyvanse, Biphentin, and Concerta), long-lasting non-stimulants (like Strattera), and short/immediate-acting stimulants (like Dexedrine, Dexedrine Spansule, Ritalin, and Ritalin SR). XR stands for extended release while SR stands for sustained release. This is not necessarily a medication, but iron supplements have been noted to help allivieate ADHD symptoms which makes sense with the noted iron deficiency being a risk. However, zinc supplements didn't have as much of a positive effect.
Treatment - Non-Medication
Psychoeducation: strategy instruction (sleep management, anger contron, etc.), self-talk development, organizational skills developments, information on ADHD, community resources, and support groups
Behavioral Intervention: rewards and consequences, environmental management, ADHD coaching, and lifestyle changes
Social Intervention: social skills training and parenting skills training
Psychotherapy: self-talk strategies, cognitive behavioral therapy (CBT), interpersonal therapy, family therapy, expressive arts therapy, and supportive counseling
Educational/Vocational Accomodations: academic remidation and specialized academic/workplace interventions
Comorbidities
"More often than not, ADHD is further complicated by comorbidity with one or more psychiatric disorders.... An adult with ADHD is six times more likely to have at least one other psychiatric disorder than an adult without ADHD." (Thomas E. Brown, PH.D.). A quote from a book to all those who would like to argue against those who believe comorbidities don't exist. Even a study found 70% of 579 children carefully diagnosed with ADHD fully met the diagnostic criteria for one or more psychiatric disorders. Cases of ADHD not complicated by another disorder are rare.
As for the disorders ADHD is often comorbid with, that would be learning disorders, anxiety disorders, mood disorders (especially Bipolar Disorder), OCD, ODD, conduct disorder, substance use disorders, and personality disorders. Bipolar disorder especially, but but mood disorders in general stem from similar neurobiology so it makes for them to be so comorbid. (Bipolar 1 is even more comorbid than Bipolar 2.) Personality disorders are reported to be present in more than 50% of adults with ADHD. Of that 50%, the most common are cluster B and C disorders with 25% of them having two or more personality disorders. Of the papers I've read, none of them mention Autism as an actual comorbidity of ADHD however that's probably because it falls under the other disorders of early childhood they frequently mentioned.
Our Own Experiences
We are professionally diagnosed with ADHD. We have genetic links on both sides of our family, as well as a lack of iron (not diagnosed with iron deficiency but we do experience symptoms at times). We were diagnosed at 13 with the inattentive type. Originally we tried Strattera as a medication, but it didn't work so we switched to another medicine and it's been working ever since (heavy dissociation messes with the effectiveness though). We have recently decided to ask to start taking iron supplements to help with symptoms. As for comorbidities, we have a comorbid mood disorder (depression however the disorder type was never specified), generalized anxiety disorder, and social anxiety disorder diagnosed. We also experiences symptoms of BPD, but it's not been talked about with the mental health group we talk to so we avoid saying for sure we have it despite the genetic and trauma links. Obviously this is just in regards to this post, but yeah!
18 notes
·
View notes
Text
Given I have seen people say DID is not usually caused by trauma, here is a bit of educational content. If you have any sources that you believe disprove these you are absolutely free to share, but I do request you consider if they actually disprove these things.
There is currently no empirical evidence to support the idea that Dissociative Identity Disorder (DID) can form naturally without any sort of trauma or adverse experience. DID is believed to be a disorder that results from severe and repeated trauma, rather than a naturally occurring phenomenon (American Psychiatric Association [APA], 2013; Nijenhuis, 2014).
Recent studies have provided further support for the trauma model of DID. For example, a study published in 2018 found that individuals with DID reported significantly higher levels of childhood trauma compared to individuals without DID (Brand et al., 2018). Another study published in 2019 found that childhood physical abuse was a significant predictor of the severity of dissociative symptoms in individuals with DID (Borowiecka-Kluza & Domowicz, 2019).
In a recent review of the literature on DID, published in 2020, the authors concluded that "the presence of severe and repeated interpersonal trauma in childhood is the most commonly reported and well-supported etiological factor for DID" (Myrick et al., 2020, p. 114). The authors noted that while some studies have reported cases of DID in the absence of overt trauma, these cases are rare and typically involve some form of neglect or emotional abuse.
In summary, the current scientific evidence supports the trauma model of DID and there is no empirical evidence to suggest that DID can form naturally without any sort of trauma or adverse experience.
References:
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Borowiecka-Kluza, J., & Domowicz, K. (2019). The association between childhood trauma and dissociation in adult patients with dissociative identity disorder. Journal of Trauma & Dissociation, 20(4), 492-506. doi:10.1080/15299732.2019.1577442
Brand, B. L., Lanius, R. A., Vermetten, E., Loewenstein, R. J., Spiegel, D., McNally, R. J., ... & Middleton, W. (2018). Where are we going? An update on assessment, treatment, and neurobiological research in dissociative disorders as we move toward the DSM-5. Journal of Trauma & Dissociation, 19(5), 555-573. doi:10.1080/15299732.2018.1464956
Myrick, A. C., Webermann, A. R., Loewenstein, R. J., Lanius, R. A., Putnam, F. W., & Brand, B. L. (2020). Advances in the treatment of dissociative identity disorder: A review of recent research. Current Psychiatry Reports, 22(12), 1-13. doi:10.1007/s11920-020-01177-y
Nijenhuis, E. R. (2014). Dissociation and trauma: An update on the theory. In P. F. Dell & J. A. O'Neil (Eds.), Dissociation and the dissociative disorders: DSM-V and beyond (pp. 107-130). New York, NY: Routledge.
A note of consideration: I used ChatGPT to help me locate the sources and construct the explanation of their contents in an accessible manner. This does not invalidate the actual contents of the study, but I believe it is important for the sake of transparency. You are by all means free to look and see if this summary was a correct portrayal, and I actually encourage you to do so as fact checking is important regardless of the involvement of AI.
10 notes
·
View notes
Text
Books I look forward to reading this year!
(In whichever order I can obtain them~) My brother is gifting me one for sure!
Post-Traumatic Stress Disorder and Art Therapy by Amy Backos
Art Therapy, Trauma, and Neuroscience: Theoretical and Practical Perspectives by Juliet L. King
Netter's Neuroscience Coloring Book by David L. Felten MD PhD (Author), Mary Summo Maida Ph.D.
The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization (Norton Series on Interpersonal Neurobiology) by Onno van der Hart Ph.D., Ellert R. S. Nijenhuis Ph.D., et al.
Mexican Sorcery: A Practical Guide to Brujeria de Rancho by Laura Davila
#complex post traumatic stress disorder#complex ptsd#neuroscience#trauma#osdd#did osdd#books to read#brujeria#witchblr
9 notes
·
View notes
Text




Nonfiction Thursday: About Your Brain
The Illusionist Brain by Jordi Camí & Luis M. Martínez
How do magicians make us see the impossible? The Illusionist Brain takes you on an unforgettable journey through the inner workings of the human mind, revealing how magicians achieve their spectacular and seemingly impossible effects by interfering with your cognitive processes. Along the way, this lively and informative book provides a guided tour of modern neuroscience, using magic as a lens for understanding the unconscious and automatic functioning of our brains.
We construct reality from the information stored in our memories and received through our senses, and our brains are remarkably adept at tricking us into believing that our experience is continuous. In fact, our minds create our perception of reality by elaborating meanings and continuities from incomplete information, and while this strategy carries clear benefits for survival, it comes with blind spots that magicians know how to exploit. Jordi Camí and Luis Martínez explore the many different ways illusionists manipulate our attention―making us look but not see―and take advantage of our individual predispositions and fragile memories.
The Phantom God by John C. Wathey
Does neuroscience have anything to say about religious belief or the existence of God? Some have tried to answer this question, but, in doing so, most have strayed from the scientific method. In The Phantom God, computational biologist and neuroscientist John C. Wathey, Ph.D., tackles this problem head-on, exploring religious feelings not as the direct perception by the brain of some supernatural realm, nor as the pathological misfiring of neurons, but as a natural consequence of how our brains are wired.
Unlike other neurobiological studies of religion and spirituality, The Phantom God treats mysticism not as something uniquely human and possibly supernatural in origin, but as a completely natural phenomenon that has behavioral and evolutionary roots that can be traced far back into our vertebrate ancestry. Grounded in evolutionary and behavioral biology, this highly original and compelling book takes the reader on a journey through the neural circuitry of crying, innate knowledge, reinforcement learning, emotional bonding, embodiment, interpersonal perception, and the ineffable feeling of certainty that characterizes faith.
When Brains Dream by Antonio Zadra & Robert Stickgold
Questions on the origins and meaning of dreams are as old as humankind, and as confounding and exciting today as when nineteenth-century scientists first attempted to unravel them. Why do we dream? Do dreams hold psychological meaning or are they merely the reflection of random brain activity? What purpose do dreams serve?
When Brains Dream addresses these core questions about dreams while illuminating the most up-to-date science in the field. Written by two world-renowned sleep and dream researchers, it debunks common myths; that we only dream in REM sleep, for example—while acknowledging the mysteries that persist around both the science and experience of dreaming.
Antonio Zadra and Robert Stickgold bring together state-of-the-art neuroscientific ideas and findings to propose a new and innovative model of dream function called NEXTUP—Network Exploration to Understand Possibilities. By detailing this model’s workings, they help readers understand key features of several types of dreams, from prophetic dreams to nightmares and lucid dreams.
Visual Thinking by Temple Grandin
A quarter of a century after her memoir, Thinking in Pictures, forever changed how the world understood autism, Temple Grandin—the “anthropologist on Mars,” as Oliver Sacks dubbed her—transforms our awareness of the different ways our brains are wired. Do you have a keen sense of direction, a love of puzzles, the ability to assemble furniture without crying? You are likely a visual thinker.
With her genius for demystifying science, Grandin draws on cutting-edge research to take us inside visual thinking. Visual thinkers constitute a far greater proportion of the population than previously believed, she reveals, and a more varied one, from the photo-realistic object visualizers like Grandin herself, with their intuitive knack for design and problem solving, to the abstract, mathematically inclined “visual spatial” thinkers who excel in pattern recognition and systemic thinking. She also makes us understand how a world increasingly geared to the verbal tends to sideline visual thinkers, screening them out at school and passing over them in the workplace.
Rather than continuing to waste their singular gifts, driving a collective loss in productivity and innovation, Grandin proposes new approaches to educating, parenting, employing, and collaborating with visual thinkers. In a highly competitive world, this important book helps us see, we need every mind on board.
#psychology#science#nonfiction books#nonfiction#reading recommendations#reading recs#book recommendations#book recs#library books#tbr#tbrpile#to read#booklr#book tumblr#book blog#library blog
6 notes
·
View notes
Text
Anxiety Disorders
Anxiety = feeling of concern or worry, with responses such as increased muscle tension, restlessness, impaired concentration, sleep disturbances, and irritability.
- Can be a necessary stimulus for optimum performance in everyday situations (e.g. it encourages more study before an exam).
- However, when anxiety increases beyond a certain level, performance deteriorates noticeably.
{note: see my Educational Psychology posts for more information about stress being a motivator at a certain level and a hindrance at a higher level}
- Strong link exists between anxiety and depression
DSM-5: Anxiety Disorders
Generalized Anxiety Disorder
Panic Disorder
Specific Phobia
Social Anxiety Disorder (Social Phobia)
Agoraphobia
Included previously in DSM-4 (until 2013):
Post-Traumatic Stress Disorder
Obsessive-Compulsive Disorder
Etiology of Anxiety Disorders
Genetics
Stressful experiences
Medical conditions
Drugs (alcohol, caffeine, benzodiazepine dependence)
Generalized Anxiety Disorder (GAD)
- Individuals show signs of constant worry and continuously predict, anticipate, or imagine dreadful events.
- Life is generally stressful, and even minor events provoke worry.
- The chronic anxiety reduces the individual’s performance on many tasks and decreases pleasure.
Panic Disorder
Panic attacks = individual experiences all the effects of a fear reaction without a threatening stimulus, accompanied by strong arousal of the sympathetic ANS (autonomic nervous system).
Symptoms: elevated heart rate and/or chest pain, sweating, shortness of breath, fainting, choking, fear of losing control or dying
- These symptoms can last anywhere from minutes to hours.
- The word “panic” comes from Pan, the Greek god of pastures and shepherds.

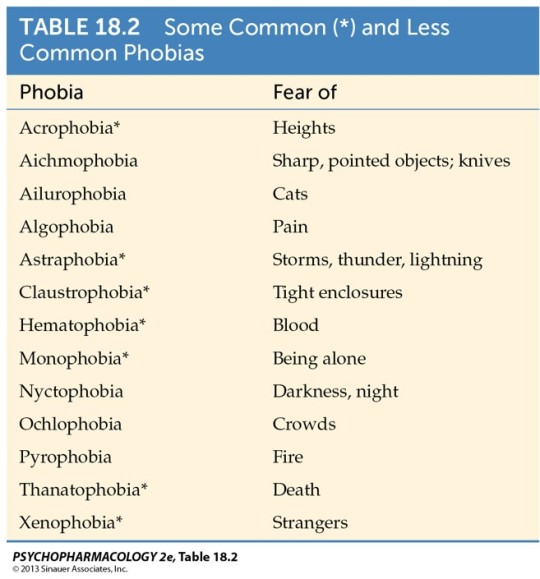
Specific Phobias
Phobia = a persistent and excessive fear of an object or situation.
- Focus on specific objects or situations such as high places or enclosed spaces, snakes or other animals, etc.

Cynophobia (extreme fear of dogs)
- Phobias can usually be treated with behavioral desensitization: presenting the fear-inducing stimulus in gradual increments, allowing the individual to maintain a relaxed state while confronting the source of the fear.
- A more contemporary version utilizes exposure therapy in a virtual reality setting.
Social Anxiety Disorder (SAD)
- Extreme fear of being evaluated or criticized by others
- Sufferers tend to avoid most interpersonal situations. When these situations are unavoidable, they suffer extreme anxiety.
- Onset is typically at a young age, with half of affected individuals developing symptoms by age 11.
Post-Traumatic Stress Disorder (PTSD)
- Listed in DSM-5 under section 1.2.7 (Trauma- and stressor-related disorders)
- Appears after a person survives or witnesses a traumatic event
- Symptoms can persist for months or years after the event. Symptoms include...
Nightmares & flashbacks about the event
Sleep disturbances
Increased physiological reactivity to reminders of the trauma
Avoidance of stimuli associated with the trauma
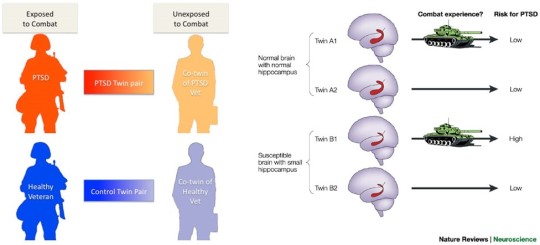
- Genetic component: children whose parents have PTSD are at an increased risk of developing PTSD themselves
Obsessive Compulsive Disorder (OCD)
- Listed in DSM-5 under section 1.2.6 (Obsessive-compulsive and related disorders)
- OCD is characterized by...
Obsessions = unreasonable thoughts and fears
Compulsions = repetitive behaviors in an effort to ease stress
- Obsessions lead to compulsions.
Ex. If a person fears contamination by germs, they may compulsively wash their hands over and over until they’re sore and chapped.
Neurobiology of Anxiety
- The amygdala is a major component of several emotion processing circuits.
- The amygdala aids in formation of emotional memories --> conditioned fear or conditioned emotional response.
- It receives highly processed sensory and cognitive information from the sensory thalamus, sensory and association cortices, and hippocampus.
- The amygdala orchestrates the components of fear: autonomic nervous system activation, enhanced reflex, increased vigilance, stress response, etc.
- Activation of the sympathetic autonomic nervous system produces increased heart rate, sweating, and other signs of “fight-or-flight” response.
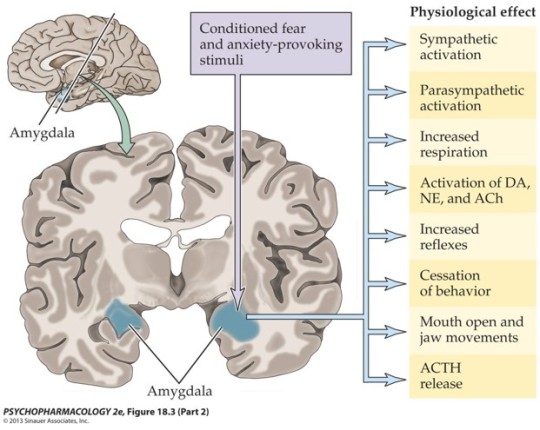
- Patients with generalized anxiety disorder (GAD) have increased volume of the amygdala.
- PET scans show greater amygdala activity with exposure to negative stimuli in GAD and phobia patients than in healthy individuals.

- The amygdala also contributes to memory consolidation through its connections with the hippocampus.
- The hippocampus may have a role in some anxiety disorders because reciprocal connections with the amygdala modulate emotional responses.
- Smaller hippocampus can predict PTSD.
- The prefrontal cortex (PFC) exerts inhibitory control over the emotional subcortical regions.
- Anxiety disorders are often considered to arise from an imbalance between emotion generating centers and higher cortical control.
Neurochemistry of Anxiety Disorders
Multiple neurotransmitters and hormones are implicated in the pathophysiology of anxiety disorders.
- Monoamines
Serotonin
Dopamine
Noradrenaline
- GABA; anti-anxiety drugs are GABA agonists.
- Stress hormones (cortisol)
Treatments for Anxiety Disorders
(A) Pharmacological Treatments
Benzodiazepines
Anti-depressants
(B) Deep-Brain Stimulation (for OCD)
(C) Cognitive Behavioral Therapy (CBT)
as effective as medication in treating chronic anxiety disorders
(D) Other Treatments
Electroconvulsive therapy (damages memory)
Transcranial magnetic stimulation
GABA Receptor Agonists
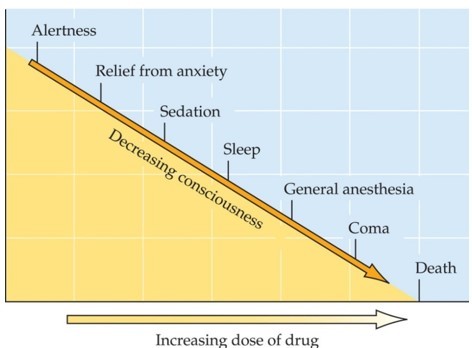
- Drugs that relieve anxiety are called anti-anxiety agents or anxiolytics.
Benzodiazepines (minor tranquilizers) are often given to people who are undergoing some major life stress.
- Sedative-hypnotic drugs include barbiturates and alcohol.
Barbiturates are sometimes prescribed as sleep aids, but most often used to induce anesthesia before surgery.
- Both sedatives and anxiolytics are CNS depressants; all of these drugs reduce brain activity.
The GABA (a) receptor has two sites:
Sedative-Hypnotic site = targeted by alcohol and barbiturates, directly influences Cl- influx
Anti-Anxiety site = targeted by benzodiazepines, enhances binding effects of GABA. Effect is dependent upon amount of GABA present.
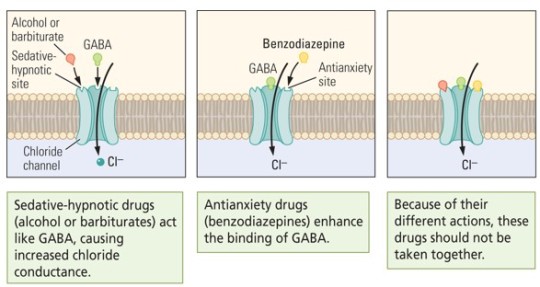
- Combining sedative-hypnotics (alcohol, barbiturates) with benzodiazepines (ex. Valium) is extremely dangerous and can result in coma or death, due to:
the double inhibitory effect
enzyme competition (for cytochrome P450)
Barbiturates
- clinically introduced in 1904 and become popular sleep aids
- Between the 1920s and the mid-1950s, barbiturates were practically the only drugs used as sedatives and hypnotics.
- Today they have been largely replaced by benzodiazepines for medicinal uses, such as...
General anesthetic
Sleep aids
Anti-anxiety drugs
Anti-convulsant (to suppress seizures)
- Examples include...
Pentrobarbital (Nembutal)
Secobarbital (Seconal)

- Side effects include...
altered sleep
loss of judgment, mental “cloudiness”
slowed reflexes
- High doses lead to severe intoxication. Coma and death result from respiratory depression. Barbiturates are extremely dangerous when combined with alcohol.
- Barbiturates produce significant physical dependence and potential for abuse.
- Terminating drug use after extended treatment produces a potentially fatal withdrawal syndrome similar to that for alcohol.
- For these reasons, they are no longer prescribed as anxiolytics or hypnotics.
Benzodiazepines
- relieve physical symptoms of anxiety, along with sense of worry and fear
- first choice for short-term treatment of anxiety, or for acute anxiety
- The introduction of benzodiazepines in 1955 led to a decrease in the prescription of barbiturates, and by the 1970s they had largely replaced the older drugs for sedative-hypnotic and anxiolytic uses.
- They target anxiety without producing excessive sedation, loss of judgment, loss of motor coordination, and produce less mental cloudiness (compared to sedative-hypnotics).
- Examples include:
Alprazolam (Xanax)
Diazepam (Valium)
- Longer-acting BDZs are useful hypnotics to aid sleep.
- Some BDZs are useful muscle relaxants and others are anti-convulsants for the management of epilepsy.
- They can also prevent acute alcohol or barbiturate withdrawal symptoms.
- BDZs do not induce liver enzymes, resulting in less tolerance.
- There is a lower risk of dependence and abuse, but it does happen.
- Reinforcement is much lower than with barbiturates, but BDZs with rapid onset can be self-administered by animals.
- Recreational use of BDZs is often combined with alcohol, opioids, or other CNS depressants, which can be highly toxic.
Anti-Depressants for Anxiety
- Antidepressants including tricyclic antidepressants, MAOIs, and SSRIs can treat both anxiety and depression, which often occur together.
- SSRIs are the first choice for chronic anxiety because they have fewer troubling side effects, a high therapeutic index, and low abuse potential.

MDMA for PTSD
- also known as “ecstasy,” “molly,” or “mandy” (in the UK)
- currently illegal, no approved medicinal use
- increases sociability, empathy, emotional awareness {note: it was developed for use in family & couples therapy.}
- August 2017: FDA designates MDMA as “breakthrough therapy” for PTSD.
- MDMA is currently in Phase 3 trials, the final stage before FDA approval. Learn more about that here: https://maps.org/mdma/ptsd/phase3/
#neuroscience#Drugs and Behavior#anxiety#phobias#social anxiety#generalized anxiety#PTSD#OCD#my notes#study blog
7 notes
·
View notes
Note
ah. another day, another braindead sysmed thinking that 'oh the science SAYS endos aren't real!'
okay then we'll bite. where in the science and the studies done on plurality (PLURALITY, and not DID/OSDD-1 because those are two different things) does it say that non-traumagenic systems can't exist? and I don't mean some rando's carrd - I mean where are the actual scientific studies that says without a shadow of a doubt that non-traumagenic systems are impossible? if you're so fucking confident in your hate and ignorance, you'll have no problem backing up your statement with facts yeah?
go on, we'll wait.
Plurality is an internet term. I don’t know how you expect people to find scientific sources that include a non-scientific term. That’s fuckin dumb. If there’s no known scientifically proven variants of the disorder, as there’s no reason to question since there’s only a few proven without a doubt causes, then how am I supposed to find a source? You’re grasping at straws. Sources that discuss DID are good sources actually, because it discusses the process of creating systems as a whole and disproves any external causes for the system creating process. But that isn’t good enough for you, because you want to debate upon something purely hypothetical- and thus useless. Goddamn cocky bastard
Anyways this source is good.
Two quotes:
1. “Dissociative identity disorder (DID) is a chronic post-traumatic disorder where developmentally stressful events in childhood, including abuse, emotional neglect, disturbed attachment, and boundary violations are central and typical etiological factors.”
The quote itself does not imply any other unknown factors, it is a list of known factors.
2. “Given the current evidence, DID as a diagnostic entity cannot be explained as a phenomenon created by iatrogenic [illness created from the medical examination process] influences, suggestibility [easily swayed/easily influenced by others] malingering [faking illness], or social role-taking [illness created to compensate roles that are not present or are needed] . On the contrary, DID is an empirically robust chronic psychiatric disorder based on neurobiological [condition of the neurons], cognitive [thought], and interpersonal [internal] non-integration as a response to unbearable stress. While current evidence is sufficient to firmly establish this etiological stance [a set reason for existence], given the wide opportunities for innovative research, the disorder is still understudied.”
The only hope for your argument is to grasp strongly into the last line, where it admits DID/OSDD is understudied. But of course every other field except philosophy is against hypotheticals, and requires definitive proof, instead of individual accounts, and in psychology it is dependent on multiple and many accounts; instead of a singular account. One account may go against the study’s findings, but if that outlier is just an outlier and not a trend, it can be considered a special case and not relevant. Science focuses on the whole. Hypothesis’ can be considered hypotheticals by whatever logic, but hypothesis are there to be proven or disproven via evidence. An inconclusive result is like having never began.
Or, you could claim that you don’t have a system at all, since OSDD/DID/and other forms of the disorders are the only understood and proven forms. If that’s the case, what are you even here for?
2 notes
·
View notes
Text
From an interpersonal neurobiology (IPNB) perspective, cognition is not "superior." IPNB emphasizes integration and the equal importance of all brain functions.
The brain and nervous system work best when integration occurs between different parts (cognitive, emotional, sensory, etc.). Rather than a hierarchy where cognition is "superior" to emotion, IPNB holds that emotions and cognition are both vital,
and they influence each other in a *bidirectional* manner. For example, emotional states can shape cognitive processes, and cognition can help regulate emotions, but neither is "superior."
Research, including findings from affective neuroscience, suggests that emotions often arise before cognitive processes. Emotions are quick, automatic responses that prepare the body to act. Cognition comes in afterward to evaluate or make sense of emotional experiences. In this way, cognition doesn’t dominate emotion but helps us reflect on emotional states and decide how to respond.
From an IPNB standpoint, emotions are deeply connected to bodily sensations (somatic experience) and are not just mental phenomena. Emotion is not something that needs to be mediated or controlled by cognition, but rather it needs to be experienced and integrated. Sometimes, emotions are better regulated by grounding in the body or connecting with others rather than relying on cognitive evaluation alone.
Rather than cognition “making an object” of emotion to mediate it, IPNB would suggest that cognition and emotion co-create meaning. Cognitive processes can help make sense of emotion, but emotions also guide cognitive functions like decision-making, problem-solving, and attention. Both are needed for whole-brain integration and optimal functioning.
Emotions are often shaped and processed through relationships and social interactions. IPNB highlights that emotions are not isolated from context; they are deeply tied to social engagement. Cognition alone doesn’t mediate emotions; co-regulation with others is a significant factor in how emotions are experienced and processed.
From an IPNB perspective, the statement misses the mark by implying a hierarchical relationship where cognition is "superior" and mediates emotion. In contrast, IPNB holds that both cognition and emotion are essential and interdependent. Healthy emotional regulation occurs when integration happens across the different parts of the brain, body, and within relationships, rather than through one domain dominating the other.
0 notes
Text
The Role of Art Therapy in ADHD Treatment: Exploring Creative Expression with Physicians like Dr. Hanid Audish
Art therapy offers a unique and effective approach to supporting children and adolescents who experience challenges with focus, impulsivity, and hyperactivity. This therapeutic method harnesses the power of creative expression to promote emotional regulation, enhance self-awareness, and improve overall well-being. By engaging in artistic activities under the guidance of trained therapists, young individuals can explore their thoughts and feelings in a supportive environment. This blog delves into the role of art therapy in addressing behavioral and emotional difficulties commonly associated with neurodevelopmental conditions, fostering personal growth and resilience.
Art therapy provides a non-verbal outlet for children and adolescents to express complex emotions and experiences that may be difficult to articulate verbally. Through painting, drawing, sculpting, and other creative mediums, participants can externalize their inner world, gaining insights into their emotions and behaviors. This process of externalization helps individuals with challenges in attention and impulse control to develop coping strategies, improve self-regulation, and build confidence in their abilities to manage stress and frustration.
Enhancing Emotional Regulation Through Creative Activities
One of the primary benefits of art therapy in treatment is its capacity to enhance emotional regulation skills. Children and adolescents with difficulties in regulating their emotions often find traditional talk therapy challenging. Art therapy offers an alternative approach where individuals can process and manage their feelings through creative activities. Doctors such as Dr. Hanid Audish mention that by engaging in structured art exercises, such as creating mood boards, emotion wheels, or guided imagery through art, participants learn to identify and express their emotions in constructive ways. This process fosters greater self-awareness and emotional resilience, equipping young individuals with effective tools to navigate interpersonal relationships and academic challenges.
Moreover, creative expression in art therapy stimulates the brain's reward system, releasing endorphins that promote relaxation and a sense of accomplishment. This neurobiological response helps to counteract feelings of anxiety and restlessness commonly experienced by children and adolescents with behavioral difficulties. Through consistent participation in art therapy sessions, individuals may experience improvements in mood stability, attention span, and overall emotional well-being. The structured yet flexible nature of art therapy sessions allows therapists to tailor interventions to meet each participant's unique needs and therapeutic goals.
Developing Social Skills and Communication Abilities
Art therapy also plays a crucial role in developing social skills and communication abilities among children and adolescents. Many individuals with behavioral challenges associated with neurodevelopmental conditions struggle with social interactions, leading to feelings of isolation or misunderstanding. Art therapy sessions provide a supportive environment for practicing social skills such as turn-taking, active listening, and cooperation. Physicians like Dr. Hanid Audish convey that group art activities encourage participants to collaborate, share ideas, and respect each other's creative expressions, fostering a sense of belonging and camaraderie.
Furthermore, art therapy promotes verbal and non-verbal communication skills through the interpretation and discussion of artwork. Therapists facilitate meaningful dialogues about the emotions, themes, and symbols present in participants' artwork, encouraging self-reflection and interpersonal connection. For children and adolescents who find verbal communication challenging, art serves as a bridge to express thoughts and feelings indirectly, gradually building their confidence in expressing themselves verbally as well.
Integrating Art Therapy with Cognitive Behavioral Techniques
Integrating cognitive behavioral techniques with art therapy enhances the therapeutic benefits for children and adolescents facing behavioral challenges. Cognitive behavioral therapy (CBT) principles focus on identifying and modifying negative thought patterns and behaviors through structured interventions. When combined with art therapy, CBT techniques such as cognitive restructuring and problem-solving skills training can be applied in creative contexts. For example, participants may create visual representations of their thought patterns or use art to practice relaxation techniques and coping strategies in response to stress triggers.
This integrative approach helps young individuals develop adaptive coping mechanisms and resilience in managing symptoms associated with behavioral difficulties. By addressing cognitive distortions and promoting positive behavioral changes through art-based interventions, therapists empower children and adolescents to take an active role in their treatment journey as noted by physicians including Dr. Hanid Audish. The collaborative nature of integrating art therapy with CBT encourages participants to apply new skills learned in therapy sessions to real-life situations, promoting long-term emotional and behavioral stability.
Supporting Academic Success and Self-Esteem
Art therapy can positively impact academic success and self-esteem among children and adolescents struggling with behavioral challenges. By fostering a sense of accomplishment and competence through creative achievements, participants build confidence in their abilities to overcome obstacles and achieve academic goals. Engaging in art activities promotes cognitive skills such as problem-solving, spatial awareness, and visual-spatial reasoning, which are essential for academic performance and learning readiness.
Moreover, art therapy encourages self-expression and self-discovery, reinforcing a positive self-concept and healthy self-esteem. As children and adolescents experience validation and acceptance of their artistic creations in therapy, they internalize feelings of competence and worthiness. This positive self-perception extends beyond the therapy room, influencing how individuals perceive themselves in academic settings and social interactions. Doctors like Dr. Hanid Audish express that by nurturing a sense of agency and resilience through creative exploration, art therapy empowers young individuals to embrace their strengths and potential for growth.
Art therapy offers a valuable therapeutic approach for children and adolescents navigating behavioral challenges associated with neurodevelopmental conditions. Through creative expression, emotional regulation, social skill development, and integration with cognitive behavioral techniques, art therapy supports holistic growth and well-being. The structured yet flexible nature of art therapy sessions enables participants to explore their emotions, enhance self-awareness, and develop effective coping strategies in a supportive environment. As part of a comprehensive treatment plan, art therapy empowers young individuals to cultivate resilience, achieve academic success, and thrive in their personal and social lives as highlighted by physicians such as Dr. Hanid Audish. By harnessing the transformative power of creative expression, art therapy contributes to the positive development and emotional stability of children and adolescents facing behavioral difficulties.
0 notes
Text
[“There is no such thing as a baby,” the British pediatrician D. W. Winnicott once said, explaining, “If you show me a baby, you certainly show me someone else who is caring for the baby . . . One sees a ‘nursing couple’ . . . The unit is not the individual, the unit is the individual-environment set-up.” Or, in Ashley Montagu’s words, “When a baby is born, a mother is born. There is considerable evidence that at this time, and for months thereafter, her needs for contact exceed those of the infant.”
Good thing, too: Were there not built-in physiological and emotional incentives for the ones doing the caregiving, parenthood would be even more of a slog than it already is. Fewer babies would have their survival needs met if fulfilling those needs were not rewarding for parents. With its usual brilliance, our interpersonal-biological makeup dictates that our requirements be mutual. (One of the unfortunate impacts of our culture’s way of doing things is that stress tends to whittle down these innate rewards, making parenting more frustrating and daunting than it rightly ought to be.)
The poet Adrienne Rich expressed the profound joys of this reciprocal design: “I recall the times when, suckling each of my children, I saw his eyes open full to mine, and realized each of us was fastened to the other, not only by mouth and breast, but through our mutual gaze: the depth, calm, passion, of that dark blue, maturely focused look. I recall the physical pleasure of having my full breast suckled at a time when I had no other physical pleasure in the world except the guilt-ridden pleasure of addictive eating.” Neurobiologically, Rich was right on target. On imaging studies, a baby’s smile will light up the same reward areas in the mom’s brain activated by junk foods or addictive drugs, releasing the same pleasure chemicals and triggering the same high. Nature, that unscrupulous drug-pusher.
Like all complex brain structures, mammalian bonding systems—whether of whales or chimps or rats or humans—are experience-dependent for their development and activation. For the brain circuits of nurturing to function—to “come on line,” as it were—the environment must evoke and then sustain them. Both men and women have latent child-nurturing circuits in their brains, “waiting for the right environment to amplify their potentials,” in the words of neuroscientist Jaak Panksepp—he of the PANIC/GRIEF, PLAY, and CARE nomenclature. Dr. Panksepp identified and mapped the specific brain centers, circuits, connections, and associated neurochemicals that choreograph what he called “the enchanting ballet of emotions between a mother and her infant.” These include chemical messengers such as vasopressin, oxytocin, and endorphins—the body’s natural opiates—all of which awaken in parents nurturing habits that are essential to the survival of the young. Recall, these are the chemicals that, blended, form a “love cocktail” released by natural labor. Skin-to-skin contact and suckling also elicit their flow in the mother. The physiology of infant and parent is thus co-regulated by their interactions, and the effect of these interactions—or their absence—can be imprinted in the young human for a lifetime. Likewise, in the dearth of such interactions, parenting instincts may become muted, with long-term consequences for the parent-child relationship. In this, as in other crucial ways, our culture has become contact-starved.”]
gabor maté, from the myth of normal: trauma, illness, and healing in a toxic culture, 2022
#gabor maté#brainspace#currently reading#mothers can and do love mothering and denying them access to mothering is violence
118 notes
·
View notes
Text
Exploring Healing Connections Therapy: Nurturing Bonds For Emotional Wellness
🏔️✨In the complex tapestry of human existence, emotional wounds often linger beneath the surface, impacting our relationships, behaviors, and overall well-being. Recognizing the profound impact of interpersonal connections on mental health, Healing Connections Therapy emerges as a beacon of hope, offering a transformative approach to healing through nurturing bonds and meaningful relationships. To get more details about healing connections therapy, you may check it here http://mtshastaspiritualtours.com/. 🏔️✨
🌀🌌At its core, Healing Connections Therapy operates on the fundamental principle that authentic, supportive relationships serve as catalysts for emotional growth and healing. Developed by pioneers in the field of psychology, this therapeutic modality draws inspiration from attachment theory, interpersonal neurobiology, and relational psychology, weaving together insights from various disciplines to create a holistic framework for healing.🌀🌌

🌿🌟Central to Healing Connections Therapy is the concept of the therapeutic alliance—a collaborative partnership between therapist and client built on trust, empathy, and mutual respect. Within this safe and supportive environment, individuals are encouraged to explore their thoughts, feelings, and experiences without fear of judgment or rejection. Through compassionate listening and genuine empathy, therapists help clients navigate their inner landscapes, uncovering deep-seated emotions and fostering a sense of self-awareness and acceptance. 🌿🌟
🌱🙏One of the distinguishing features of Healing Connections Therapy is its emphasis on the relational aspect of healing. Rather than viewing individuals in isolation, this approach recognizes the interconnected nature of human experience, acknowledging the profound impact of past relationships on present-day functioning. By exploring patterns of attachment and interpersonal dynamics, clients gain insight into how their past experiences shape their current relationships and behaviors, paving the way for profound transformation and growth. 🌱🙏
✨Healing Connections Therapy encompasses a range of therapeutic techniques tailored to meet the unique needs of each individual. From experiential exercises and expressive arts therapy to mindfulness practices and somatic techniques, therapists draw from a diverse toolbox of interventions designed to facilitate healing on multiple levels—mind, body, and spirit.
Through these modalities, clients learn to cultivate self-compassion, regulate their emotions, and develop healthier ways of relating to themselves and others. To get more details about laser halo treatment, you may check it here.🏔️🌿

✨Moreover, Healing Connections Therapy extends beyond the therapy room, empowering clients to integrate newfound insights and skills into their daily lives. Through homework assignments, journaling exercises, and interpersonal experiments, individuals are encouraged to apply therapeutic principles in real-world settings, fostering greater self-awareness and relational competence.
In essence, Healing Connections Therapy offers a profound paradigm shift in how we approach healing and personal growth. By recognizing the transformative power of nurturing relationships and fostering authentic connections, this innovative approach holds the promise of healing emotional wounds, restoring wholeness, and cultivating a deeper sense of connection and fulfillment in our lives. 🌲🕊️
1 note
·
View note
Text

Schore A. N. (2021). The Interpersonal Neurobiology of Intersubjectivity. Frontiers in psychology, 12, 648616. https://doi.org/10.3389/fpsyg.2021.648616
0 notes