#gonorrhea treatment
Text
Significance of Chlamydia Treatment: What Doctors Say
Treating chlamydia is easy. This is a bacterial disease and can be cured completely through a dose of antibiotics. If you have undergone a test on time and received positive results, worry not. Your doctor will chart out a treatment plan for you.
0 notes
Text
the comic is done. im so proud of it
#its cus its an actual structured comic about stuck figures having unprotected sex and getting Disease#but then going to the doctors and getting treatment#i sprinkled in some fun facts to get more information about the disease into the comic its so good#txt#also never search gonorrhea on google images never. never ever. dont do it.
12 notes
·
View notes
Text

Premature Ejaculation is a common sexual condition where a man ejaculates sooner than he or his partner would like, during sexual activity. It can occur with minimal sexual stimulation and before the person wishes it. Premature Ejaculation can be caused by a variety of factors, both psychological and biological.
Psychological Reasons:
* Sexual abuse
* Poor body image
* Depression
* Worrying about premature ejaculation
* Guilt feelings that increase the tendency to rush through sexual encounters
Biological Reasons:
* Abnormal hormone levels
* Abnormal levels of brain chemicals called neurotransmitters
* Inflammation and infection of the prostate or urethra
* Genetic traits that may be inherited
These are potential reasons, and the exact cause can vary from person to person. If you’re experiencing symptoms of Premature Ejaculation, it’s recommended to consult with a healthcare provider for a proper diagnosis and treatment plan.
With the effective treatments available in Dr. Rana’s Medical Hall, you can easily treat Premature Ejaculation with the goodness of Unani-Ayurvedic system of medicines. We are working as a one stop solution for all your sexual problems, since 1960. Moreover, we have facilities for both online consultation & direct consultation. For more information regarding Premature Ejaculation, please do contact Dr. Rana’s Medical Hall. We are all here to help you get through the situation.
Know More : https://ranamedicalhall.com/
WhatsApp us : https://wa.me/918848511462
Online Consultation form : https://ranamedicalhall.com/consultation-form/
#onlineconsultation#kochi#kottayam#thrissur#erectiledysfunction#prematureejaculation#maleinfertility#PenileEnhancement#precounselling#venerealdisease#gonorrhea#Syphilis#herpes#lowspermcount#stamina#syphilistreatment#syphilisawareness#sexologist#treatment
0 notes
Text
The Three Most Prevalent STIs: Chlamydia, Gonorrhea, and HPV
Introduction:
Chlamydia, gonorrhea, and human papillomavirus (HPV) are among the most common sexually transmitted infections (STIs). These infections can cause serious health problems if left untreated and can affect anyone who is sexually active. In this post, we’ll explore the causes, symptoms, and treatments of these three prevalent STIs.
Chlamydia:
Causes and Risk Factors:
Chlamydia is…

View On WordPress
#Chlamydia causes#Chlamydia symptoms#Common STIs#Gonorrhea causes#Gonorrhea symptoms#HPV transmission#HPV types#HPV vaccination#prevalent sexually transmitted infections#regular STI testing#safe sex practices#STI treatment options
0 notes
Text
From the article:
A new study has confirmed what most sexually active gay men will already know: Less of us are using condoms when we have sex compared to ten years ago.
The study, published in AIDS and Behavior, was conducted by researchers at the University of Washington. It drew its data from the American Men’s Internet Survey (2014-2019). It looked specifically at men who have condomless anal sex with men who are not on PrEP.
The number of men in the study having condomless sex rose by 2.2% each year. However, the rise was greater in younger men (rising 7.2% per year for those aged 15-24 years) and Hispanic men (rising 18%).
Overall, condom use remained more popular than PrEP. This might be partly due to barriers to obtaining PrEP, among other factors. Around 15% of the men were taking PrEP.
The vast majority of men questioned believed condoms to be “very effective” (60%) or “somewhat effective” (36%) at preventing HIV transmission.
However, 24% said they “never” used condoms, compared to 50% who said they “always” or “sometimes” used them. The remainder said they rarely used them.
Clearly, there is a large number of guys having condomless sex who are not on PrEP. If their partner is HIV positive and undetectable, they cannot pass on the virus. However, not everyone knows their HIV status or is on treatment.
Besides HIV, condoms can also help prevent the transmission of other STIs. The rise in gonorrhea and syphilis diagnoses in the US in recent years is in part related to declining condom use.
#this focuses on cis men but EVERYONE needs to make sure they practice safe sex#get tested and know your status#use STI prevention methods wherever you can#news#queer news#health news
124 notes
·
View notes
Note
I heard we are now at the cusp of chlamydia being untreatable via antibiotics, fun times
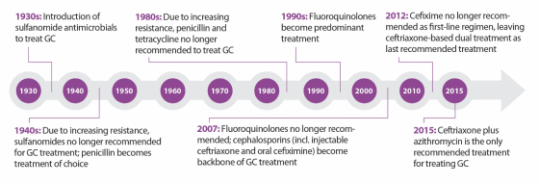
In United States, drug-resistant gonorrhea is a public health problem of national concern. But untreatable gonorrhea isn’t the only STD that has health officials worried.
Earlier this week, the World Health Organization released new treatment guidelines for three common sexually transmitted diseases — chlamydia, gonorrhea, and syphilis— in response to increasing antibiotic resistance.
Gonorrhea has developed the strongest resistance to drugs, but the worries about untreatable syphilis and chlamydia come at a time when rates for the three STDs are rising rapidly in the U.S, especially among young people ages 20 to 24. According to data published by the CDC in 2014, the most recent year available: cases of chlamydia have increased 2.5 percent; gonorrhea 5.1 percent; and syphilis 15.1 percent. This is the first increase in the United States since 2006.
How worried should we be?
“STDs are hidden epidemics of enormous health and economic consequence in the United States,” according to the Centers for Disease Control and Prevention.
In the US, STDs are most frequent among college-age women, the highest prevalence being among women, ages 20 to 24.
According to the CDC, there are about 820,000 new gonorrhea infections each year in the United States. In fact, gonorrhea is the second most commonly reported infectious disease, after chlamydia.
In the past, gonorrhea was successful treated by several classes of antibiotics, including the ubiquitous penicillin. Over time, however, gonorrhea has developed resistance to many of them, and now, we are down to one recommended effective class of antibiotics to treat it.
The problem doesn’t end there. Gonorrhea is even starting to show decreased susceptibility to this “last line” treatment option. This makes this bacterium a multidrug-resistant organism, which are often called “superbugs”.
As for chlamydia and syphilis, drug resistant strains have not become common in the US yet, but the WHO report warns that this is a growing problem in many parts of the world.
How can untreatable STDs be prevented?
Anyone who is sexually active can get an STD.
That said, STDs are preventable and there are steps you can take to keep yourself and your partner healthy. Remember that protecting your health is your responsibility:
Condoms: Use them correctly every time you have sex.
Have fewer partners: Ideally, agree to only have sex with one person who agrees to only have sex with you.
Talk with your partner: Talk with your sex partner about STDs and staying safe before having sex.
Get tested: Make sure you both get tested to know for sure that neither of you has an STD.
Get vaccinated: Safe and highly effective vaccines are available for two STDs: hepatitis B and HPV. HPV is in fact the most common STD. There are specific recommendations for routine and catch up vaccinations for these two STDs.
____________________
This is from 2016 and I cut a bunch out of the middle.
2nd bullet point there probably gonna make some people grumpy, something about suggesting monogamy makes people mad.
102 notes
·
View notes
Text
Things you should know before having SEX
There is absolutely nothing rude or accusatory about asking a new partner about their STD history
Use both a barrier method (male or female condom) AND a hormonal method for the best bet at preventing pregnancy
When you’re considering stopping using condoms with a partner, you can ask them if you can go together to get tested first
Don’t have sex with anyone who would hesitate to slow down or stop if you want to or who would be angry or upset with you because of it
Get tested regularly, every 1–3 months
You can go on PrEP if you feel you are truly at risk of getting HIV
Look at your partner and make sure they do not have cold sores, if they do, don’t kiss/do oral with them!
Always meet in public first
Have boundaries and don’t be afraid of kicking someone out/leaving
It’s easier and cheaper to change condoms than diapers.
If you're planning on having a lot of casual sex, you must accept that you will be exposed to STIs.
There is no such thing as safe sex - just risk reduced.
Pinch the reservoir tip of a condom as you slide it down the penis to make sure there is enough space for the semen to collect
Oral/vaginal/anal sex all have STD risks.
Do NOT use oil-based lubricants with a condom
Abstinence-only is a terrible idea, and statistics show it: STD rates and teen pregnancy rates are higher in areas with abstinence-only sex education programs.
Some people enjoy a little acting or role-playing during sex so it helps to have a pronounced safe word that nobody will say by accident.
Don't dominate on the first physical meeting.
Don't introduce new, undiscussed elements into a scene in the heat of the moment.
Dental dams for oral sex, surgical gloves with LOTS of lubes for fingering, trim your nails, and wash your hands.
Vagina penetration isn't going to be as easy, like they show in porn
it's essential to clean off the semen before putting on another condom.
Buy plenty of condoms
Pee after sex as it is important to prevent UTI.
Throw out everything you see in porn, it's unrealistic and most of the positions are not possible or enjoyable as they look on camera.
Have plenty of foreplay before penetration
When you get on the pill, ask your doc how long that pill takes to be effective.
Cum will drip out of you, and you will look silly waddling to the bathroom to go pee and clean up
If you take any kind of antibiotics, it will render your birth control pills ineffective for the rest of that month.
Never be ashamed to have cleanup supplies near your bed.
Doing kegel squeezes in the restroom really helps push most if not all the cum out.
Two people with a vulva can give each other STIs.
Let someone know where you are and when you'd be back.
Your hookup doesn't have to be for penetrative sex
Don't drink anything you're handed that you don't see poured and doesn't leave your sight.
Oral sex is very risky for things like gonorrhea, chlamydia, and syphilis (especially syphilis and pharyngeal gonorrhea).
Asking for Snapchat always does a good job of weeding out the fakes.
Always bring your own condoms and lube
Always let the person know that you’ll only have sex with condoms before meeting up
Obtain pepper spray just in case you’re put in a dangerous situation.
Clean your toys appropriately, and make sure it's body-safe material (if it starts to smell even after cleanings, throw it away).
Be sure to use the correct kind of lube
For any kind of sex, there generally shouldn't be pain. If there's pain, something is probably wrong.
If you brush your teeth before doing oral, wait till the minty flavor is gone before going down on them
Your pubic hair is normal and healthy. Trimming is fine, shaving I recommend a lot less.
Sex is a marathon, not a sprint
Not liking sex is okay.
HIV is no longer a death sentence. With proper treatment, your viral load can be so low that transition is impossible. You'll have to manage it for the rest of your life, and your partners would have to take PREP and HIV prevention drugs.
If you decide to practice kink, be aware that consent becomes much more explicit and requires a lot of prep to properly establish. Without consent, it's just abuse.
#lgbtq community#lgbt pride#lgbtqia#lesbian#lgbtq#nonbinary#queer#nonbinary lesbian#sapphic#gay girls#transgender#trans#trans femme#trans women#trans pride#transfem#queer community#queer culture#queer nsft#queer pride#queer artist#lgbt#pride#wlw nsft#wlw post#wlw#wlw ns/fw#wlw love#nblw#mlm nsft
110 notes
·
View notes
Text
Gonorrhea has become so antibiotic resistant that there is only one antibiotic class recommended for treatment and new studies/cases have shown that its slowly starting to become resistant to it.
So be careful out there lovelies!
#You and partner(s) should be regularly getting tested#And both should be wearing BARRIER protection
46 notes
·
View notes
Text
Chlamydia Treatment Recommendations by WHO
Chlamydia is a curable bacterial disease. It is transmitted through sexual activity and is one of the commonest STDs around. You need not worry, if you are exposed to this bacterium. A simple course of antibiotics can cure this infection.
0 notes
Text
Medicine may be about to achieve a long-sought goal: a “morning-after pill” to prevent sexually transmitted infections. It could sharply reduce soaring rates of illness and huge health care costs.
The effectiveness of this pill—and it literally is a pill, a 200-milligram tablet of the antibiotic doxycycline—has been studied for a decade, and people have taken it covertly for years. But study results published in The New England Journal of Medicine look likely to tip the pill into clinical practice. In the study, conducted in San Francisco and Seattle, participants who took a single dose within 72 hours of having sex without a condom were only a third as likely to contract chlamydia, gonorrhea, or syphilis as those who didn’t take the pills.
As with everything in medicine, there are footnotes to the findings, and risks to balance the benefits. The study was conducted only among gay and bisexual men, along with transgender women and nonbinary people assigned male at birth. Within those groups, it was limited to people who had been diagnosed with a sexually transmitted infection (STI) in the past year. The study didn’t include cisgender women; in past studies, the preventive antibiotic has not worked as well for them. And the study noted, but didn’t explore in depth, the possibility that routinely administering an antibiotic could provoke resistance either among the bacteria that cause STIs or others carried in participants’ bodies.
All that said, the results have created real excitement among physicians and people who would be eligible to take what’s being called doxyPEP (for doxycycline post-exposure prophylaxis)—even though health authorities, such as the US Centers for Disease Control and Prevention, haven’t yet made formal recommendations for its use.
“I think this is a real game-changer,” says Paul Adamson, an infectious disease physician and assistant clinical professor of medicine at the University of California, Los Angeles. “We have a huge amount of bacterial STIs in the US. Gay and bisexual men who have sex with men are disproportionately burdened by them. And we have not had a lot of tools that we can use to help.”
To understand why doxyPEP could be so significant, it’s important to consider what’s been happening with STIs. Briefly: They’re skyrocketing. Since 2017, according to the CDC, the most important of these diseases have reached historic highs: Gonorrhea has increased by 28 percent, and syphilis by 74 percent. And while chlamydia diagnoses haven’t quite returned to their pre-Covid levels, the agency worries that might be due to pandemic disruptions to care, rather than to an actual decrease in transmission. All of those infections have profound long-term consequences if they are not diagnosed and treated, including making people more vulnerable to HIV infection. Collectively, they cost the US health care system more than $1 billion per year.
Meanwhile, congenital syphilis—passed from mother to infant at birth, a sign that the pregnant person never received adequate prenatal care—caused 220 stillbirths and infant deaths in 2021, the last year for which there are national figures. Gonorrhea is gaining resistance to the last antibiotics currently available to treat it.
In medicine, prevention is almost always preferable to treatment: Vaccines and other prophylactic measures are less expensive, and can be planned in advance. So it has been a research goal to find uncomplicated prevention for STIs—something that, like the morning-after pill for pregnancy, can be taken a short time after sex and doesn’t rely on the user making decisions in the moment.
The first test of doxyPEP, a small US trial that took place in 2011 and 2012, was published in 2015, and showed that HIV-positive men who took the post-exposure dose cut their rate of STIs by three-fourths. Fairly soon after that, social networks of men who have sex with men picked up on the findings, and began sharing knowledge about using preventive doxycycline off-label. A large 2017 French study of men using pre-exposure prophylaxis for HIV, known as PrEP, included within it a study of STI rates among men taking post-exposure doxycycline; it showed that doxyPEP could cut rates of syphilis and chlamydia infection by almost 70 percent. And last summer and this spring, the two largest international HIV conferences included presentations that confirmed the doses were successful in most circumstances.
Several of those presentations were drawn from the San Francisco and Seattle study just published in NEJM. Its results were so dramatic that the authors stopped the trial earlier than planned, in May 2022: They revealed that, among 501 men who were either living with HIV or taking HIV PrEP, consuming that single dose of doxycycline within 72 hours of sex without a condom reduced the combined incidence of the three major STIs by roughly two-thirds.
“Our goal was to understand this in a real-world setting, in a heterogeneous population of people taking HIV PrEP but also living with HIV—which biologically aren’t different populations, but may be different in terms of sexual behaviors, sexual networks,” says Anne Luetkemeyer, one of the study’s principal investigators and a professor of medicine at the University of California, San Francisco. Combined with the French research, she adds, “we now have two studies that really showed very remarkably similar efficacy in this population.”
Those two sets of results may be enough to let doxyPEP enter mainstream medicine. In some places, it already has. Last October, San Francisco’s public health department became the first local department to support doxyPEP use in its jurisdiction. And after the NEJM paper, individual physicians tweeted they would begin prescribing doxyPEP because the results looked so solid—something they can do off-label because the Food and Drug Administration already approved the drug decades ago to treat a range of infections.
When a new way of controlling a disease seems likely to enter the US mainstream, the CDC is expected to weigh in. So far, the agency hasn’t published official guidelines regarding the use of doxyPEP. Following the release of preliminary data at conferences, the CDC published “considerations for individuals and healthcare providers,” a strategy for sharing what’s known so far, as well as an acknowledgment that doxyPEP already is being used off-label. A CDC spokesperson told WIRED by email that formal draft guidance for physicians could come “by the end of the summer.”
When that guidance does arrive, it isn’t expected to recommend doxyPEP for everyone. “We should consider offering this to people who have an elevated risk” of STIs, Luetkemeyer says. “And that group is men who have sex with men, on PrEP, or living with HIV, who've had a history of STIs. I think that's a reasonable group.”
And eligible people may not want to take it. Like almost all antibiotics, doxycycline has side effects: sun sensitivity, diarrhea, serious nausea. And it hasn’t worked equally well for everyone. In the trial done in French men, the antibiotic did not suppress gonorrhea infections, even though it had a dramatic effect on reducing syphilis and chlamydia. In the one trial done so far among cis women, launched in Kenya in 2021, doxycycline prophylaxis (known in this case as dPEP) had no effect on suppressing STIs.
That was disappointing; women who are at high risk of STIs need prevention as much as men do. Equally, it was mystifying for the researchers, who now are poring through their data to see what might have made a difference: whether the 449 participants had difficulty taking the drug at the right time, for instance, or whether doxycycline behaves differently in female organs than in men’s. “We had more than 200 women show up to hear the results, and they were so shocked and disappointed,” says Jenell Stewart, the study director and a physician-scientist and assistant professor at Hennepin Healthcare in Minneapolis. “We are very focused on understanding these results before we say this doesn’t work for women.”
One thing that might have played a role in Kenya and France—and is raising red flags for doxyPEP use in the US—is antibiotic resistance. Stewart says 100 percent of the gonorrhea isolates tested so far from women who became infected while on dPEP showed high levels of resistance to tetracycline, the drug family that doxycycline belongs to; at the time of the French study, the background rate of resistance in gonorrhea there was 56 percent. In the US, where doxycycline isn’t the first-line treatment for gonorrhea, the rate of resistance is only 20 percent. That may provide a clue to why doxyPEP worked better in the US trial than in any other. But it also immediately raises the concern that if doxyPEP goes into wide use, it might make resistance worse.
The US study could not provide an answer: Though some men in the trial did contract gonorrhea while taking doxyPEP, not enough testing was done to confirm whether their strains were resistant to the medication and thus not knocked out by the single dose. Tests did suggest the drug might be affecting other bacteria in participants’ bodies, but the results were contradictory. Those taking doxyPEP ended up harboring 40 percent less staph bacteria—something that all of us carry—than those not taking the drug; but the staph they were still carrying showed “modestly higher” resistance. Whether killing some bacteria was more beneficial than making others potentially hazardous, the trial didn’t last long enough to say.
So the calculation inherent in doxyPEP may not be risk versus benefit, as much as it is risk versus risk: preventing an infection while provoking resistance through small doses, or contracting an infection that requires larger doses over a longer period of time. “We’re not comparing doxyPEP to no antibiotics,” says Adamson, who researches drug-resistant gonorrhea and has prescribed doxyPEP for some patients. “We’re comparing doxyPEP to potentially significant amounts of ceftriaxone, or penicillin, or doxycycline perhaps, if somebody’s getting infections a lot.”
It’s a question that research will have to answer—because, no matter how the CDC weighs in, doxyPEP use is moving ahead. Joseph Osmundson, a microbiologist and author in New York City—where STI rates are rising just as they are nationally—recently sought a prescription from his regular physician. As a queer sexual-health activist, he says, it only made sense, not only to prevent infections and antibiotic side effects for himself, but also to keep from increasing infection rates in an already overburdened city.
“When people want an intervention to have a healthier sex life, you cannot not give it to them,” he says. “Withholding the intervention will not prevent people from having the kind of sex that they enjoy. The question is: Are they going to be provided with as many interventions as possible to have that type of sex with less risk of infectious disease?”
110 notes
·
View notes
Text
when i found out I had gonorrhea I felt like I was a dirty, disgusting human (and not in the sexy sense). I don't know how I got it when I'd done everything that sex ed taught me to do (besides the 'no sex' part). To this day I can't tell you who gave it to me (all of my past partners to that point had told me that they were either clean or virgins- not saying virgins couldn't have STIs, but I was extremely naive).
I had a horrible break down and felt like my life was over. Surely my then girlfriend wanted to leave me for being unclean. And future partners? Forget about it. I was tarnished for life.
I found out through planned parenthood's free testing. They also treated me, for free. Then tested me again! Just to tell me that I didn't have to worry any more!!
The stigma we have around STIs is disgusting. If you have one or have had one, you're not less of a person. You're not dirty or unclean. They happen. People get sick. We can cure a fuck ton of them, and there's lots of long term treatments out there for the lifelong ones! Please, be mindful with sex- but also be mindful with how you treat and love yourself!
10 notes
·
View notes
Text
"Years after it was first proven to work, a new tool for preventing sexually transmitted infections (STIs) is now closer than ever to entering mainstream medicine.
That tool is doxyPEP, an antibiotic that works like a morning-after pill — but instead of preventing pregnancy within hours of unprotected sex, it prevents STIs like chlamydia and syphilis. Ever since a 30-person trial first suggested hope for the strategy in 2015, people worldwide have begun trying doxyPEP for themselves, often without the approval or supervision of a medical provider.
...
Why did it take so long for the CDC to get behind doxyPEP?The major obstacle has beenthe fear that doing so wouldtouch off a perilous game of infectious disease whack-a-mole — that in trying to mitigate one public health crisis, we’ll worsen another one.
Doxycycline, the medication in doxyPEP, is an antibiotic. Worldwide antibiotic resistance is a major problem — and doxyPEP runs the hypothetical risk of exacerbating it. Disease-causing bacteria can evolve resistance when exposed to certain antibiotics, becoming more dangerous.
...
Doxycycline has plenty of street cred in the STI world. A week’s worth of the medication is the first-line treatment of choice for chlamydia, and a two-week course is the best syphilis treatment choice for people allergic to penicillin. (Doxycycline also sometimes works against gonorrhea, although the germ’s growing resistance to the medication means it is no longer recommended as a treatment for that infection.)
In contrast, doxycycline PEP is for preventing infection, not for treating it. “PEP” stands for post-exposure prophylaxis: The idea is that if a person takes a single dose of the medication soon enough after unprotected sex, any bacteria that might cause an STI would be killed before entrenching enough to cause a full-blown infection."
23 notes
·
View notes
Note
dear mr.horsepussy,
I caught chlamydia from this 19 year old wannabe bi sexual. I'm pretty sure it was him bc the last 2 guys I let raw me were clean and I foolishly assumed just bc he was deflowered a weeks ago, he wouldn't have anything and now peeing hurts. at least I got doxycycline for the treatment but I'm scared that I might have something else that the urgent care clinic I went to wouldn't have the means to test for (they just test for trich, gonorrhea and chlamydia) my hoe hubris has come, do you have any words of advice???
Uh ok. I'm not the best example in this area. I never paid attention to any of this and I like had AIDS and diabetes and herpes and shit for who knows how many years until I almost died on the couch cuz I never once went to a regular doctor. I always went to Emergency Rooms and then skipped out on the bill for decades. I don't think you can do that anymore cuz hospitals send everything to collections now and I don't think they do VD shit unless it's like monkey pox making your dick fall off. You think you got any of the Heps or Aids, I'd seek out Planned Parenthood or maybe an Aids charity and they know where to direct you on the cheap and preferably anonymous so the local health department doesn't fuck with you. I'm sure a private diagnostic lab could run a panel if you are rich or have insurance.
Again I'm not the best person to dole out health advice so don't sue me if something falls off. Good luck!
20 notes
·
View notes
Text
The problem with having story ideas is that I’ll be like “modern-ish film noir homage.” And then I’ll be like “there should be a subplot about having a mildly frustrating time seeking medical treatment for gonorrhea.” And then I have to admit that never happens in Double Indemnity or whatever.
12 notes
·
View notes
Text
I Refuse! (3)
/== Table of Contents ==/
“So, Dr Peach, how is our newest resident?” Ozpin asked as he stood in the door of the picture crowded office of Beacon’s resident medical doctor. “Did she weather her journey… well?”
“If you’re trying to ask if her virginity is intact, then stop trying to be polite.” Dr Peach replied. “Anyway in response to your question, yes she has been untouched vaginally, however…”
“She has been molested.”
“Yes. She tested positive for gonorrhea of the throat, and there is evidence of anal penetration.” Dr Peach had a look of relative anger on her face. “I have provided the needed medications, and arranged for her to speak to Dr Primrose.”
“I will pass this information on to the VPD. Maybe they can add some charges.”
“I have to ask. What are your plans for her?” Dr Peach gave the Headmaster with undisguised suspicion and accusation in her voice.
“I am giving her asylum to her at Beacon, if she agrees to enroll as a student. That will prevent her mother or the Winchesters from forcing her return to Ansel.”
“That is a risky move. The Winchesters have a decent amount of influence with in the council, and even the Arcs in their destitute state have many who would like to curry favor with them.” Peach sighed, “They may try and force your hand.”
“Yes, it is possible that will be the route they attempt, and they may even reach out to the Nikos and Schnee families to add even further pressure.”
“So, how are you going to deal with that possibility?”
“Simply. Beacon will not interfere with the marital contracts, we are only offering to keep her safe, and as long as she wished to remain on our grounds we will enforce her rights to dispute the contract.”
“That sounds like we will be getting involved.”
“We won't be. We will be providing no financial or legal support. We will just be guaranteeing her safety.” Ozpin answered, “So aside from the signs of sexual abuse, and treatment for the STI, is there anything else I should be made aware of?”
“No, the rest of her tests came back negative and good. So aside from concerns about her mental health, physically she is good.”
“Will she be able to take part in initiation?”
“I’m hesitant to say it, but yes, she is medically cleared to take part.”
“Thank you. I will pass on to Glynda to schedule Joan times for sessions with Dr Primrose, once initiation is complete.”
/==/
Joan didn't know what to think, let alone do. She was at Beacon, pretending to be a guy. The Headmaster had offered her asylum, meaning her mother couldn’t force her to return to Ansel as long as she agreed to attend the academy, and then that the nutcase of a Headmaster had flung her from a cliff. Thankfully, her new partner Pyrrha Nikos stepped in before Joan was forced to use her semblance.
Then there was the Deathstalker; which she was never going to admit to anyone, that it was her fault; and the Nevermore which was definitely not her fault. Now she was the leader of a team of supercharged teens. Why she didn't understand. It's not like Pyrrha, Ren, or Nora wouldn't have figured out how to take down the Deathstalker. She just noticed it first.
Why that made her leadership material, she had no clue. She never travelled to Vale to become a huntress, no, her goal was to buy her sisters time for her family to deal with her late father’s debits.
7 notes
·
View notes
Text
[“When Elaine was hired at the Nook, they learned about her arrest and demanded she produce a clean bill of health. Not only did Elaine not have a health certificate to show, worse, her symptoms had returned. Desperate, she wrote to the WPA and explained that she was “doctoring it with potassium permanganate ‘internal baths,’ drinking no coffee, tea or alcoholic liquors; leaving salt, pepper, and spices alone; [and] drinking quarts of milk and water.” Pitifully, she ended the letter, “I don’t know what else to do.”
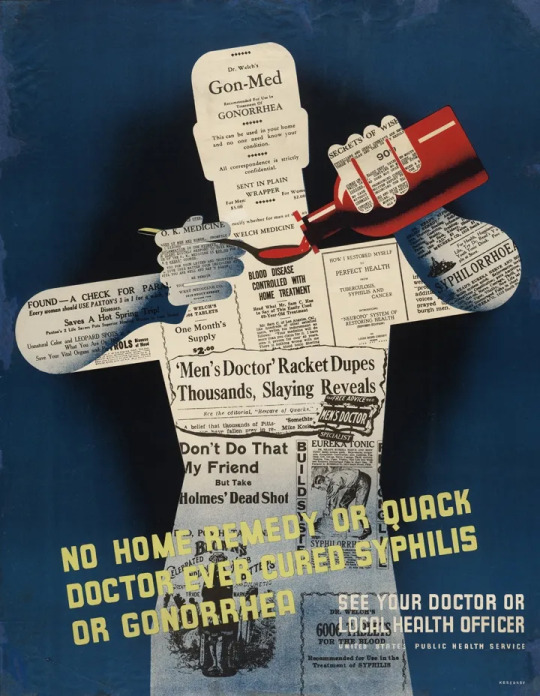
Of course, she had no access to or money for a doctor. Douching with potassium permanganate was a common treatment for venereal disease, despite the fact that it was toxic when taken intravaginally, causing “acute gastroenteritis” and in extreme cases “circulatory collapse.” But it was no worse than the drugs that doctors generally prescribed, which ran the toxic gamut from arsenic to mercury. The first real treatment for gonorrhea would arrive with the sulfa class of drugs, which were tested (nonconsensually) on incarcerated prostitutes at the House of D, starting in 1938—too late to help Elaine.
The WPA recommended Elaine return to New York and get tested, which she did. On May 13, 1935, she tested positive for gonorrhea again. That was the end of her summer dreams—her waitress gig at the Nook had come with a small room, and without that, Elaine could no longer afford to play country bohemian with the richer denizens of Greenwich Village. Instead, the WPA arranged for Elaine to be sent to Inwood House, which was like a homeless shelter where women with sexually transmissible infections were kept until cured. Elaine disliked the place from the very beginning, particularly the curfew, and disappeared her first night there. She spent one night on the floor of La Violette’s room, and the next she tried to sleep in the New York Times building in Midtown (where her friend Alice had once given her a tour). When that didn’t work, she joined the other street girls who slept rough in Bryant Park, and for a few weeks, she disappeared.
If Elaine had only lasted one night at Inwood House, she would have discovered the next day that there had been a mistake: her test was clean; she never had gonorrhea, and she was free to return to Woodstock to pursue her dreams of being an artist’s assistant (and eventually, she hoped, an artist herself). Instead, she ended up on the doorstep of a man she had briefly dated, whom she described as “bi-sexual” and “look[ing] like a rugged sailor edition of Rudy Vallee.” When she discovered he had inherited some $4,000, she made the spur of the moment decision to accept his marriage proposal. By July, they had left New York, and it was only via Elaine’s friend Alice that the WPA learned the pair ended up in Los Angeles.”]
hugh ryan, the women’s house of detention: a queer history of a forgotten prison, 2022
55 notes
·
View notes