#Clinical Research Associate Training
Text
Clinical Research Associate Training - The Key to Becoming a Certified Professional

An ideal option for people who wish to build a solid career in the medical field, the clinical research associate profession brings many financial benefits and also a set of personal satisfactions, allowing practitioners to sustain their professional activity for the benefits of the community. Apart from the main function of monitoring clinical trials, the clinical research associate profession involves a wide variety of roles, such as verifying clinical site activities, making regular on site visits, reviewing and checking the accuracy of case report forms, as well as permanently interacting with clinical research investigators, all activities having to respect the imposed clinical protocols and good clinical practice guidelines.
It is important to note that the clinical research associate profession involves a lot of responsibility and dedication, rendering a long-term career in the branch quite demanding. However, clinical research associates have the opportunity to work in a clean and structured environment, to permanently interact with people and to ensure the protection of the rights, safety, health and well-being of human study subjects that participate in clinical trials.
The basic role of a clinical research associate, also referred to as a monitor, is to supervise the entire progress of clinical trials, initiated and conducted by physicians at hospitals, clinics, physician's offices and other medical establishments. Apart from being responsible for the health and well-being of clinical study participants, clinical research associates have to ensure the accuracy, quality and integrity of the scientific data collected during trials. The extensive set of roles and duties characteristic to practicing clinical research associates include ensuring that the physicians respect good clinical practices and study protocols, checking the required documentation for each study participant, ensuring that all side-effects and adverse physical responses are appropriately reported and filed and ensuring the proper filing of various regulatory documents.
Clinical research associates are generally employed by pharmaceutical companies, medical research organizations and other institutions in the medical field. The profession involves a lot of field work, practitioners having to visit various sites and to maintain permanent connection with clinical study coordinators and investigators.
Persons who wish to follow the career of clinical research associate attend rigorous training programs to show good practical, decisional and communicational skills in the process. All persons who possess the skills and abilities required by the clinical research associate profession can easily obtain the proper training by attending clinical research associate training programs, regardless of their previous level of experience in the medical field.
Official clinical research training programs allow attending trainees to rapidly familiarize with the theoretical curriculum, and polish their practical skills and abilities required in their future profession. Instructor-led clinical research associate training programs are well-structured in a comprehensive manner, facilitating the process of learning and allowing graduates to leave with a complete baggage of knowledge and practical experience. A set of course examinations, self study and evaluations further prepare students for their final exams. The keys to becoming a well-trained, clinical research associate are attending to a proper clinical research training program and rigorously preparing for the final exams.
CCRPS is a medical research company that claims to provide accredited, outsourced on-demand regulatory training solutions for organizations to assure staff compliance in education for ICH GCP, clinical research associates/monitors, clinical research coordinators, research assistants, and drug safety/pharmacovigilance officers.
So, if you want to find out more information about clinical research associate or about clinical research associate training visit here on our official site and check everything in detail manner.
0 notes
Text
Please help my partner, a black multiply disabled lesbian, get their autonomy back!
‼️URGENT ACTION NEEDED IN 48 HOURS ‼️
01/03/2024
my partner @800-dick-pics is a multiply disabled black lesbian in need of urgent funds for a service dog and the costs associated with travel!!
This is all so sudden and short notice, they happened upon this prospect while doing research and it fell into their lap, a puppy in a breed with the best temperament and size for their mobility needs. This is opportunity is huge for the independence of my fiancé.
For years now, my fiancé has been fighting with the medical system, I've seen them struggle to be believed by doctors due to medical racism, turned away and ignored at the ER, gaslight by ED clinics and multiple times I've physically caught them when they've passed out during a POTS episode. Their POTS EDS and CFS have rendered them housebound in this past year, unable to leave the house by themselves and it's gotten to the point where we both are afraid for their safety when they're alone in any capacity. I worry for them so greatly when I have to leave them for more than 20 minutes at a time because anything could happen.
This has been years in the making, even before we were together even. We've had to put this on hold for countless reasons throughout the years and at this point it can no longer be put off for the sake of my fiance' autonomy independence and quality of life. They're tired of not being able to hold a job or go out with friends or even just experience life outside of the walls of the house. This is incredibly important and this is our chance to change their life forever.
We need to meet this goal THIS WEEK, to be able to secure this opportunity including flight tickets, hotel room, training toys for the dog and food

We would not be asking if it wasn't so urgent, this can't be put on hold and all my fiance wants is to have a life again. Please help us if you're able, this opportunity means the world to my partner!
CA: $sleepyhen
VM: wildwotko
DM me for p@y pal
$0/2600 goal
#sorry we are poor#they got back to us super quick and were ready to do business immediately so the past 24 hrs have been nerve wracking!!#all i want is to see my partner thrive and be happy and get back to the things they love#please this is important
851 notes
·
View notes
Text



skincare practices
skincare refers to the practice of maintaining and improving the health and appearance of your skin. this post is a guide on where to start!
having a routine (starting with simple practices)
cleanser: begin and end your day by washing your face with a gentle, sulphate-free cleanser. even if your skin feels clean, this step removes any impurities.
moisturizer: apply a fragrance-free moisturizer twice a day. hydration is crucial for maintaining a healthy skin barrier.
sunscreen: protect your skin from uv damage by using a mineral- or chemical-based sunscreen with at least spf 30. apply it in the morning.
skin types
there are 5 primary skin types, each with unique characteristics and needs.
normal skin is balanced and not too oily or dry. it's like the goldilocks of skin types! maintain it with a gentle routine. if your skin is generally normal, opt for a lotion. as you age, consider switching to a cream-based moisturizer for added hydration.
dry skin lacks hydration, feels tight, and may have flakiness. opt for richer moisturizers with ingredients like hyaluronic acid and ceramides. for dry skin, skip lotions and go for creams or ointments. these provide more moisture and help preserve water in the skin.
oily skin produces excess oil, especially in the t-zone (forehead, nose, and chin). use lightweight, oil-free products and consider salicylic acid for acne-prone areas. if you’re prone to oiliness, choose a light gel-based moisturizer to avoid clogging pores.
combination skin is a mix of oily and dry areas. focus on balancing - light moisturizers for oily zones and richer ones for dry areas. treat your face as two zones. moisturize the dry areas and skip the oily ones. remember to look for spf 30 or higher for sun protection!
sensitive skin is prone to redness, irritation, and reaction. choose fragrance-free, hypoallergenic products and patch-test any new products.
common skincare mistakes
skipping sunscreen. sunscreen is non-negotiable! protect your skin from uv damage by using spf 30 or higher daily. if you live in a sunny environment, make sure to reapply before you go outside!
not cleansing before bed: properly cleanse your face before sleeping. it removes dirt, makeup, excess oil, and pollution remnants, preventing breakouts and maintaining healthy skin.
sleeping with makeup on. gross! no! remove your makeup before you go to bed to prevent clogged pores and skin irritation.
using too many products. overloading with products can overwhelm your skin, so learn how to simplify your routine. additionally, using products that are not right for your skin may have negative effects - creating more issues instead of solving them.
overusing acne products. be gentle with acne treatments. overuse can lead to dryness and irritation.
using harsh products. avoid aggressive ingredients that strip your skin. opt for gentle formulations.
remember - healthy skin starts with mindful habits.
further reading
understanding skin - skin types and conditions | eucerin
what are skin types? | verywellhealth
↑
this link has a 'determining your skin type' section
how to pick the right moisturizer for your skin | american academy of dermatology association
combination skin care (youtube video) | dr. aanchal md
how to build a skincare routine for beginners | arizona dermatology
skin care: 5 tups for healthy skin | mayo clinic
end notes
thank you for reading! i get a lot of skincare practice asks, so i figured it was about time i had a good response.
as always - if you're troubled by your skin take yourself to see a professional. they are specially trained to help you with your problems. this post will only be able to share with you what i have researched. definitely have a look into some of the 'further reading' links - it's so important to learn about (and determine your skin type).
if you'd like to have a look at more of my skincare posts, check out 'how to reduce acne - and what is acne?' and 'how to properly wash your face'. feel free to send any questions to my ask box!
❤️nene
#nenelonomh#that girl#becoming that girl#student#productivity#student life#chaotic academia#academia#study blog#health#healthcare#health and wellness#healthy life#healthy lifestyle#wellness and health#mental health#healthylifestyle#wellness#prevention#skincare#glowingskin#skincare routine#skin treatment#it girl#it girl aesthetic#it girl energy#dream girl#pretty girl#clean girl#hot girl walk
53 notes
·
View notes
Text
Re Fox “not a psychologist” Mulder
He has a very valid point when he says this.
While in the pilot he is described as “an Oxford educated psychologist” and utilizes his knowledge of psychology for profiles in the violent crimes unit and on the x-files, he is very much not a psychologist.
At least here in the US, you earn the title of “psychologist” after you have obtained a masters degree or higher (such as a PhD or PsyD) and/or accreditation from a society/state/etc. (PsyD is a doctor of psychology which is different from an MD who practices psychiatry- psychology and psychiatry have differences as well) This is very nuanced and in laymen terms is questionably acceptable to use the term psychologist in reference to Fox Mulder, however, technically he is correct— he is not a psychologist.
The reason is due to credentialism and ethics, anyone can get an associates or bachelors in psychology but “higher education” is a way to gatekeep the profession and to protect the utilization of the knowledge you learn as a psychology student due to the nature of the study. There is higher moral and ethical stakes the more educated you are so only the highest educated may claim the title of psychologist. This concept falls into “scope of practice” and is most applicable in medical and related fields.
(Disregarding moral and societal implication of this act- it’s a complicated issue)
For example, You shouldn’t try hypnosis on someone until you’ve been adequately trained on the technique and consequences (neutral term). These standards are often set by entities such as the American psychological association and is often why you cannot practice psychology without a license- a degree alone is not enough to prove capability and responsibility.
In Dreamland 2 we see his diploma from Oxford University and he has a bachelor’s of science in psychology. He is not trained in clinical psychology, educational psychology, industrial psychology, school psychology, etc. His degree in psychology is one of science so it’s very likely his education had a focus on research and statistics more so than broad theory and principles. (Difference between a Bachelors of Science and a Bachelors of Arts in psychology).
All in all, yes he has a degree in psychology but he is not a psychologist. It’s very likely he would have had the time to get at least a masters before recruitment to the FBI but it is never established he has more than a bachelors from Oxford. I am also not well versed on psychology degrees in the UK and how the education and credits transfer to the US.
#re I have a bs in psychology and spent a year prepping for a higher degree in psychology#my experience and knowledge is my own and some may disagree or have different experiences and knowledge#there’s a lot of licensing involved in practicing psychology and calling yourself a psychologist#the x files#txf#fox mulder#not a psychologist
108 notes
·
View notes
Note
i think you said somewhere you volunteer - do you have any tips on how to start doing that? ive been wanting to start both to help people out myself and to push my social boundaries but i get stuck in my head before i even get in the door somehow. do you have any tips lol? i think im overthinking this...
Hey no worries, I really like that you’re genuinely interested and trying to gather resources. I actually have some thoughts I’d like to share on this:
There are two types of volunteering: long-form volunteering and short-form volunteering. Short-term volunteering looks like participating in the occasional phone bank, helping raise donations every now and then, attending a food drive on a blue moon. Long-form volunteering is typically something like volunteering at a place on at least a weekly basis. A lot of the time that requires that the place actually train you so you’re of use to them. Before you look up places to volunteer, consider which type of volunteering suits your schedule the most. I do both, but I understand how not everyone’s workload can accommodate that.
When it comes to long-term volunteering, understand that just because it’s not paid work doesn’t mean it shouldn’t be taken seriously. You can’t do frequent callouts or blow off tasks because they’re not paying you to be there. A lot of the places that do social justice work—providing free food and medical care to homeless people, providing services to refugees—unfortunately do not have the necessary funding to support a whole lot of employees most times. Whatever your time commitment looks like, it remains a time commitment that needs to be honored regardless of pay.
With that said, it really is best to find something you’re actually passionate about, not something that you’re doing for the brownie points. One way to do that is to work towards a cause you have a personal connection to. For example, I volunteer weekly at a refugee center for middle eastern refugees. I also participate in a plethora of events with a view to assist Palestine in whatever ways I could. Because I’m an Arab girl, one w Iraqi heritage (also a war-torn Arab country), obviously all these things will be of personal importance to me. It’s easy for me to be incentivized to care about them, because I have this preordained connection to them. Personal connection makes it that much easier to be passionate about a cause.
But it’s equally important to mention that relatability isn’t the only way to care, nor should it be. I also volunteer at a clinic that provides service to homeless people weekly. I’m not homeless. I still care. I volunteer at my city’s Alzheimer’s research center. I don’t have Alzheimer’s. I still care. We don’t have to only associate ourselves with people we personally relate to. In fact, and this goes for life in general, you really should seek to befriend, interact with, and be curious about people who’re not like you. You should find their experiences intriguing: a window into another perspective you perhaps hadn’t thought of before. You should not always be surrounding yourself with an echo chamber of yesmen and homogeneity. Be curious about people who’re not like you. Try to put yourself in their shoes. And then learn to care about them.
It’s okay to frame volunteering as a way to benefit you too. It’s not a one-way street. There’s nothing more fulfilling than devoting yourself to something that’s solely rooted in your humanity. Not in the desire to be paid, not in the desire for acclaim, but simply in the desire to help. It makes you feel better. It boosts your self-confidence. It helps you form long-lasting connections with other people who’re also doing it out of the sheer kindness of their heart; out of the fact that they find it in themselves to care. And it reminds you of what really matters.
The biggest mistake is overwhelming yourself w 82727 resources and 72627 organizations. Start with something simple and stick with it, then go from there if you have the time to get more involved. A lot of the places that need volunteers would be happy with as little as one day a week, so long as you’re consistent about it.
It���s okay if you don’t have the time for long-form volunteering. Volunteering every now and then at one-and-done events still makes a huge difference. A lot of people make the mistake of thinking it has to either be this grand commitment or nothing. Please don’t think that way; organizations know life could be busy, and they’re happy to have you even if it’s only for the occasional event. Just make sure you’re doing something if you can.
42 notes
·
View notes
Text
mRNA vaccines have gained widespread attention for their crucial role in fighting the COVID-19 pandemic. Yet, even before the pandemic, researchers at Memorial Sloan Kettering Cancer Center were investigating the potential of mRNA vaccine technology in the fight against cancer.
Leading this innovative research is Dr. Vinod Balachandran, a physician-scientist associated with the David M. Rubenstein Center for Pancreatic Cancer Research, the Human Oncology and Pathogenesis Program, and the Parker Institute for Cancer Immunotherapy.
Dr. Balachandran's groundbreaking efforts have paved the way for a clinical trial focused on using mRNA vaccines to treat pancreatic cancer, offering new hope to patients confronting this challenging disease.
Neoantigens in Pancreatic Tumors
At the heart of this innovative approach lies the concept of neoantigens, proteins found within pancreatic tumors that serve as alarm bells, alerting the immune system to the presence of cancer cells. These neoantigens play a pivotal role in rallying the immune response to keep pancreatic cancer at bay.
Unlike traditional vaccines, which are one-size-fits-all, these mRNA vaccines are tailored to each individual, with the aim of stimulating the production of specific immune cells known as T cells. These T cells are trained to recognize and target pancreatic cancer cells, reducing the risk of cancer recurrence following surgical removal of the primary tumor.
Intriguingly, the results of this groundbreaking research have shown remarkable promise. Among the 16 patients studied, eight experienced activation of T cells that recognized their own pancreatic cancers.
Importantly, these patients demonstrated delayed recurrence of their pancreatic cancers, providing tantalizing evidence that the T cells activated by the vaccines may be effectively holding the cancer at bay.
Dr. Balachandran's work in pioneering mRNA vaccines for pancreatic cancer received a significant boost through collaboration with BioNTech, the company responsible for developing the Pfizer-BioNTech COVID-19 vaccine.
When asked about the inspiration behind using a vaccine to combat pancreatic cancer, Dr. Balachandran explained, "There has been great interest in using immunotherapy for pancreatic cancer because nothing else has worked very well. We thought immunotherapy held promise because of research we began about seven years ago."
This research, spanning seven years, revealed that a select group of pancreatic cancer patients managed to defy the odds and survive after tumor removal surgery. Upon close examination, it was observed that these tumors harbored an unusually high number of immune cells, particularly T cells.
These immune cells were drawn to the tumors by signals emitted from within. These signals, as it turned out, were neoantigens—proteins that T cells recognize as foreign invaders, prompting an immune system assault on the cancer.
Even more intriguing was the discovery that T cells recognizing these neoantigens persisted in the bloodstream of these fortunate patients for up to 12 years after tumor removal.
This sustained immune response resembled an autovaccination, with T cells retaining a memory of the neoantigens as a threat, akin to the way vaccines confer long-term protection against pathogens. This finding sparked the idea of artificially inducing a similar effect in other pancreatic cancer patients.
Unlocking the Potential of mRNA Vaccines
To understand how mRNA vaccines can combat pancreatic cancer, one must delve into their intricate mechanisms. Dr. Balachandran and his team published their findings on immune protection in long-term pancreatic cancer survivors in the prestigious journal Nature in November 2017. During this time, they were also exploring methods to deliver neoantigens to patients in the form of vaccines, with a particular focus on mRNA vaccines.
Unlike traditional vaccines, which introduce weakened or inactivated pathogens into the body, mRNA vaccines leverage a piece of genetic code known as messenger RNA (mRNA).
This genetic code instructs cells in the body to produce a specific protein, thus triggering an immune response. Coincidentally, BioNTech's co-founder and CEO, Uğur Şahin, expressed interest in the research conducted by Dr. Balachandran's team, initiating a collaboration that would prove pivotal.
In late 2017, Dr. Balachandran and his team journeyed to Mainz, Germany, where BioNTech is headquartered. Over dinner, they discussed the potential of mRNA vaccines in the context of pancreatic cancer treatment. This marked the beginning of a journey that held immense promise for cancer patients worldwide.Scientist, CEO and co-founder of BioNTech Ugur Sahin. (CREDIT: BERND VON JUTRCZENKA/POOL/AFP via Getty Images)
The intricacies of designing an effective cancer vaccine are manifold. Given that cancer arises from the body's own cells, distinguishing proteins in cancer cells as foreign entities is a formidable challenge for the immune system. Nevertheless, advances in cancer biology and genomic sequencing have paved the way for the design of vaccines capable of discerning the difference.
Dr. Balachandran's team, in conjunction with BioNTech and Genentech, capitalized on these advances, recognizing the critical role played by tumor mutations in triggering immune responses. Their optimism in the potential of mRNA vaccines for pancreatic cancer was well-founded, setting the stage for their groundbreaking research.
Personalized mRNA Vaccines: A Tailored Approach
The personalized nature of mRNA vaccines for pancreatic cancer is a testament to their efficacy. After a patient undergoes surgical removal of a pancreatic tumor, the tumor is genetically sequenced to identify mutations that generate optimal neoantigen proteins—those that appear most foreign to the immune system.
Subsequently, an mRNA vaccine is meticulously crafted, containing the genetic code specific to these neoantigens present in the individual's tumor.
During the vaccine production process, patients receive a single dose of a checkpoint inhibitor drug. This combination is intended to enhance the immune response to tumors. Once the mRNA vaccine is administered into the bloodstream, it prompts dendritic cells—an essential component of the immune system—to produce the neoantigen proteins.
These dendritic cells simultaneously educate other immune system components, including T cells, to recognize and attack tumor cells bearing the same neoantigen proteins. With T cells primed to seek out and destroy cells displaying these proteins, the chances of cancer recurrence are diminished.
Overcoming Challenges: The Road to Success
The road to realizing personalized mRNA vaccines for pancreatic cancer was fraught with challenges, not least of which was the complexity of the manufacturing process. Unlike mass-produced vaccines like those for COVID-19, the mRNA cancer vaccine had to be custom-made for each patient based on the unique characteristics of their tumor.Neoantigens are an important feature of cancer cells and help to stimulate anti-cancer immune responses. (CREDIT: Technology Networks)
This necessitated an intricate series of steps, including the surgical removal of the tumor, shipping the tumor sample to Germany for sequencing, manufacturing the vaccine, and returning it to New York—all within a tight timeframe.
Thankfully, Dr. Balachandran's team and their collaborators rose to the occasion, successfully enrolling the target total of 20 patients nearly a year ahead of schedule. Their unwavering dedication and meticulous planning ensured that the personalized mRNA vaccines could be provided to those in dire need.
As if the hurdles of personalized vaccine production weren't enough, the emergence of the COVID-19 pandemic added an unprecedented layer of complexity to the clinical trial. Dr. Balachandran and his team recognized the urgency of adapting swiftly to ensure that patients were not adversely affected.
Under the leadership of Cristina Olcese and with the unwavering support of individuals such as Department of Surgery Chair Jeffrey Drebin and Hepatopancreatobiliary Service Chief William Jarnagin, the team orchestrated the logistics required to maintain the trial's momentum.
Remarkably, what was initially estimated as a two-and-a-half-year trial was completed in a mere 18 months. The tireless efforts of Dr. Drebin, Medical Oncologist Eileen O'Reilly, Physician-Scientist Jedd Wolchok, Biologist Taha Merghoub, Computational Biologist Ben Greenbaum, and the support from Stand Up 2 Cancer/Lustgarten Foundation were instrumental in making this trial a reality amidst the challenges posed by the pandemic.
A Bright Future for mRNA Vaccines in Pancreatic Cancer Treatment
The recent findings from this pioneering research offer a beacon of hope for patients grappling with pancreatic cancer. Dr. Balachandran affirms that "an mRNA vaccine can trigger the production of T cells that recognize pancreatic cancer cells."
The prospect of personalized vaccines enlisting the immune system in the fight against pancreatic cancer—a disease in dire need of improved treatments—holds tremendous promise. Moreover, these developments may extend their impact to other forms of cancer as well.
Looking ahead, Dr. Balachandran and his team are committed to further analyzing the data obtained from the clinical trial. This analysis will provide valuable insights into the factors that facilitate the vaccine's efficacy in patients. Armed with this knowledge, they aim to refine the vaccines to make them more effective and applicable to a broader spectrum of pancreatic cancer patients.
In a testament to the forward-thinking vision of the Memorial Sloan Kettering Cancer Center, this pioneering work exemplifies their commitment to bringing cutting-edge treatments to cancer patients.
Through their partnership with BioNTech and Genentech, and with the support of Stand Up 2 Cancer/Lustgarten Foundation, a larger study is already in the pipeline, aiming to test personalized mRNA vaccines in a more extensive cohort of pancreatic cancer patients.
As Dr. Balachandran notes, they were at the forefront of mRNA vaccines before their popularity surged, leveraging scientific discoveries to make a tangible impact on patients' lives. The future indeed looks brighter for those facing the formidable challenge of pancreatic cancer, thanks to the relentless pursuit of innovation in the field of mRNA vaccines.
Key Takeaways
Some people with pancreatic cancer survive many years after diagnosis.
In these patients, the immune system keeps the cancer from returning.
A messenger RNA vaccine based on this concept is being tested in combination with another type of immunotherapy.
Early results suggest the vaccine is having the desired effect on the immune system.
12 notes
·
View notes
Text
Trans History (long post sorry)
This post uses "transsexual" in place of "transgender" as this was the widespread accepted terminology until fairly recently and is what was used in the original source for this information.
In 1885 the Criminal Law Act was passed which made homosexual behavior illegal in the UK. Transvestites within the gay movement were easier to identify publicly and became easy targets.
Ernest "Stella" Boulton and Fred "Franny" Park were arrested in 1870 for indecent behavior and attempted to be persecuted on the grounds of cross dressing instead of sodomy. They were let go.
Because of these laws, homosexual transvestites began to seek out doctors to "cure" them. These doctors and researchers were called sexologists. Krafft-Ebbing (1840-1902), professor of psychiatry at Vienna was one of the first to be interested in transvestitic behavior.
Magnus Hirschfeld was another, a Germon sexologist, and his works were considered groundbreaking during the times.
At Hirschfeld's clinic, Dr. Felix Abraham performed the first transsexual operations in 1926 on an unnamed trans man, penectomy on his domestic servant Dora in 1930, and vaginoplasty on Lili Elbe who would die from complications from the procedure.
Christine Jorgeson, former American GI, underwent several transsexual operations and drew attention from the media. The media immediately focused on the appearance of Christine, "Ex-GI Becomes Blonde Beauty". This essentially was effective marketing and brought transsexualism into the public eye. Jorgeson's psychiatrist, Dr. Hamburger (yes really) began to receive a ton of letters from people wanting to change their sex because they wanted to escape homophobia or live in/be associated with the gender roles associated with the other sex.
This caused a bunch of doctors to start their own clinics because they smelled money, such as endocrinologist Harry Benjamin (who trained at Hirschfield's clinic). He went on to publish the first medical textbook on transsexuality called the Transsexual Phenomenon in 1966 and personally began training a bunch of other doctors in the subject. His clinic was based in New York. Dr. Elmer Belt opened up clinics in Los Angeles. Dr. Georges Burou specialized in penicile skin inversion vaginoplasty in Casablanca.
Janice Irvine wrote of transsexualism's "widespread public and professional acceptance" as early as the 1970s. While gay men and women practicing transvestitism were originally criticized (because it was essentially homosexual people defying gender norms associated with their sex), transsexuality on the other hand was almost immediately accepted. Transsexualist origins lie in doctors attempting to "correct" the genitalia of people with disorders of sex development, homosexual people fearing for their lives and attempting to escape incarceration for being homosexual, and (mostly homosexual) people feeling wrong for not conforming to the mannerisms, expressions, and style associated with their sex, culturally.
While the beginnings of transsexual medicine began in the 1950s, with interest in the subject by psychiatrists dating back since the early 1900s, most "treatment facilities" for homosexuality, paraphilias, and gender nonconformity transsexuals became widespread in the 1960s and 1970s. Ira Pauly in 1965 who was a professor of psychiatry at the University of Oregon counted a total of 603 "male to female" transsexuals and 162 "female to male" transsexuals. He then reported on post-operative adjustment of 121 of these people, describing it as successful. He voiced a cautious psychiatric support for transsexualism based on this, stating that since psychology seems to have failures in reverting it and until alternative procedures or treatments are discovered, it was the best approach society had for this demographic.
I mentioned disorders of sex development (DSDs, commonly called "intersex conditions") above. Transsexualism has been closely associated with people with DSDs. In the 1950s, protocols were established for doctors to determine the sex of infants with DSDs, which was a rare anomaly. These infants bodies would then be modified to "correctly" correspond with whatever sex they were assigned by doctors. Transsexualism and the correction of "intersexualism" overlapped because doctors studying transsexualism borrowed procedures used to "correct" infants with DSDs.
Robert Stoller, a professor of psychiatry in California and considered to be a famous transsexual expert by the 1970s, began to focus on badly constructed genetalia. John Hopkins Hospital in Baltimore became a headquarters for "treating" both "intersexuality" and "transsexuality". More texts were published: Transsexual Sex Reassignment (1969) by Richard Green and John Money, and The Transsexual Experiment (1975) by Robert Stoller. French psychoanalyst Catherine Millot commented, "there was a sense in which there was no transsexuality before experts like Benjamin and Stoller 'invented it'." There was rare support for transsexuality in 1965, but by 1975 about twenty major medical centers were offering treatment to thousands of transsexual people.
It took until 1977 for transsexual surgeries to be presented to the American Psychiatric Association. By that time "normalization of sex reassignment" was institutionalized and thus "assumed" by John K. Meyer and Donna J. Reter of the APA.
However, when Reter and Meyer by their very forced hands assumed the "normalization" of sex reassignment, they at the same time cast public doubt on it and it's "almost routine acceptance".
While medical doctors and psychiatrists pushed sex reassignment surgery, psycho-analysts almost always remained doubtful of it. A well-known psychoanalyst from New York, Lawrence S. Kubie, publicly rejected and renounced the term "transsexual" completely, suggesting "genital transmutation" was a more accurate fit. He criticized the term "transsexual" stating that the word was too simple for such a complex phenomenon, and falsely alluded that problems had been solved when in reality, they weren't. He illuminated that there were many men at this time that wish to appear as women but to consider themselves and be considered as men who "simulate women", but needed to present themselves as "textbook transsexuals" in order for physicians to agree to alter them. So, these transvestites fell under pressure to conform as transsexuals.
Kubie and his co-author James B. Mackie argued that the concept of transsexualism was a combination of both false diagnoses and lack of clarity on patients, with "emotionally charged" and "dramatic" medical intervention.
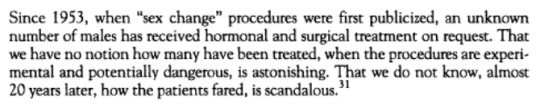
Even Robert Stoller in 1973 voiced his own unease in an article he wrote for the American Journal of Psychiatry, describing a "carnival atmosphere that prevails in the management of male transsexualism". Just the patient's request for sex reassignment brought immediate acceptance. By this point, many homosexual transvestites were educating themselves on SRS and HRT to have their sex modified to avoid homophobic persecution, and many even knew more about these procedures than their doctors. Stoller went on to write:
The conservative view among medical professionals at this time was to convince transsexual people/transvestites that they were really the other sex.
Homosexual sociologist Edward Sagarin wrote in a book on "deviants" in 1969 that male-to-female transsexuals suffered from "doubly unacceptable" self-imagery in being both homosexual and feminine, and that the solution was to convince them that they were really women and not men.
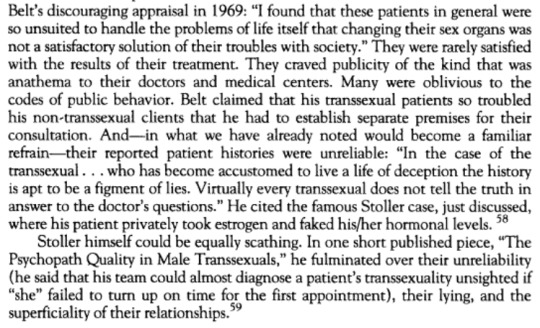
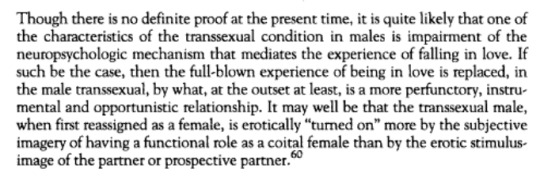
Additionally, there were striking observations made of the behaviors of a subset of people seeking sex-reassignment surgeries and hormone treatments:
John Money, the sexologist who infamously forcibly transitioned an intersex child by the name of David Reimer, also described transsexual male people as "devious, demanding, and manipulative"
Meanwhile, L.M. Lothstein who pioneered a study on female-to-male transsexuals in the 1970s and 1980s diagnosed FTM transsexuality as a "profound psychological disorder", describing most as having personality disorders and while not psychotic, having thought disorders that affect their ability to relate to others and sense their reality. Lothstein felt that the solution to help transsexual people didn't lie in surgeries or hormone treatments, but in psychotherapy. He hesitantly felt that it was possible SRS and HRT was needed before psychotherapy to "disrupt their rigid defensive structure".
I'm writing a lot so I'll stop here. Sorry for the abrupt end. I might add more later as a reblog. But here is the primary source that I essentially heavily paraphrased.
#trans#transgender history#trans history#transsexual history#transsexualism#ftm trans#mtf trans#mtf#ftm#enby#non binary#gender identity#gender#transitioning#LGBT history#transvestite history#actually mtf#actually ftm
115 notes
·
View notes
Text
Erin Reed at Erin In The Morning:
Over the past few weeks, Dr. Hillary Cass has begun giving interviews in the United States to defend her report targeting transgender care. The Cass Review has faced criticism for its alleged anti-trans political ties, biased findings, promotion of conversion therapists, and poor treatment of evidence regarding transgender care. In an interview with NPR, Dr. Cass claimed that transgender individuals' care should be judged by their "employment," rather than their satisfaction with the care received. Later, during an interview with The New York Times, Cass misleadingly stated that she had not been contacted by any lawmakers or U.S. health bodies, despite having met with political appointees of Gov. Ron DeSantis to discuss banning trans care before her report was published. In response, both the American Academy of Pediatrics and the Endocrine Society have categorically rejected the review as a justification for bans on care and have challenged many of its alleged findings.
In a statement released by the Endocrine Society, they reiterated that they stand by their guidelines around the provision of gender affirming care for transgender youth: “We stand firm in our support of gender-affirming care. Transgender and gender-diverse people deserve access to needed and often life-saving medical care. NHS England’s recent report, the Cass Review, does not contain any new research that would contradict the recommendations made in our Clinical Practice Guideline on gender-affirming care… Medical evidence, not politics, should inform treatment decisions.”
[...]
Similar sentiments were shared by Dr. Ben Hoffman, president of the American Academy of Pediatrics, who responded to the Cass Review, “What we’re seeing more and more is that the politically infused public discourse is getting this wrong and it’s impacting the way that doctors care for their patients. Physicians must be able to practice medicine that is informed by their medical education, training, experience, and the available evidence, freely and without the threat of punishment. Instead, state legislatures have passed bills to ban and restrict gender-affirming care, which means that right now, for far too many families, their zip code determines their ability to seek the health care they need. Politicians have inserted themselves into the exam room, and this is dangerous for both physicians and for families.”
Transgender care saves lives. A Cornell review of more than 51 studies determined that trans care significantly improves the mental health of transgender people. One major study even noted a 73% lower suicidality among trans youth who began care. In a recent article published in the Journal of Adolescent Health in April of 2024, puberty blockers were found to significantly reduce depression and anxiety. In Germany, a recent review by over 27 medical organizations has judged that “not providing treatment can do harm” to transgender youth. The evidence around transgender care led to a historic policy resolution condemning bans on gender affirming care by the American Psychological Association, the largest psychological association in the world, which was voted on by representatives of its 157,000 members.
Interestingly, Cass herself advocated against care bans in her most recent New York Times interview released today, where she stated, “There are young people who absolutely benefit from a medical pathway, and we need to make sure that those young people have access,” although she added a caveat that those young people should be forced to consent to research in order to access care, leaving many to question the ethics of such an approach.
Regardless of Cass’s statements, her review is being used to justify bans in the United States and worldwide.
Both the Endocrine Society and the American Academy of Pediatrics came out to reject bans on gender-affirming care in the wake of the anti-trans Cass Review by Dr. Hilary Cass.
Dr. Cass herself advocated against bans on gender-affirming care in a recent New York Times interview; however, her report is being used as justification for bans on gender-affirming care worldwide.
See Also:
LGBTQ Nation: Cass Review author says leading medical org only supports trans health care under “political duress”
#Hilary Cass#Cass Review#Gender Affirming Healthcare#Transgender#Transgender Health#American Academy of Pediatrics#Endocrine Society
9 notes
·
View notes
Text
Well, isn’t this interesting...
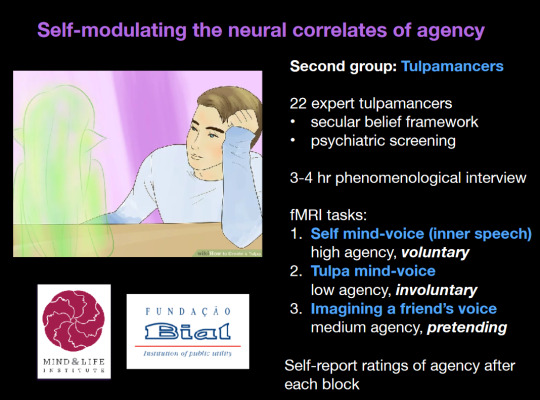
Looks like the tulpa studies might finally be coming out… Here’s the author’s quote.


Edit: I actually managed to get a copy of the article itself.
The communities comprised:
...
b. Tulpamancers, who create invisible companions, or “tulpas” (interviewed at Stanford University). Tulpamancers usually assume that they have brought their tulpas into existence through deliberate imaginative techniques, and that the human and the tulpa(s) share one human body.
...
The following features were more or less common rules across communities to identify thoughts that did not originate from the human, but were understood to originate from the supernatural (or nonhuman) source:
1. The thought is more sudden/spontaneous than ordinary thoughts
2. The thought feels more autonomous/not created by the self
3. The thought is stronger/louder than ordinary thoughts
4. The thought feels vivid
5. The thought feels intentional, as if something is communicated
...
In this light, it may be helpful to point out that some features of thought treated in the literature on psychosis as features of psychosis are, in fact, features of thought itself. Some ordinary human thoughts can be described as more vivid, more spontaneous, more loud, more intentional, than other thoughts. Ordinary human thought has texture. This texture is utilized by these communities to describe what kind of thoughts people experience and to identify them as communications from invisible others.
Moreover, the practices of these communities and the experiences that their members report suggest that cognitive expectations and sensory techniques change the quality of thought events. As researchers continue to ask about the experiential pathways through which people come to the events—psychosis, hypnosis, absorption, sleep—it is crucial to attend to cognitive expectations and sensory practice.
...
Two primary hypotheses emerge from these observations. First, the way the experience is identified (or discerned) may shape its character. Our authorship group shared the general sense (now framed in terms of predictive coding) that there is a relationship between expectation and, for want of a better term, experience, even as we acknowledge that for some who end up in these communities, the onset of the experiences is unbidden.
Second, specific practices of sensory attention may alter the character of these experiences. We saw two dominant forms of attention trained within these communities: talking to invisible beings as if they were present, and attending to one’s inner senses in order to experience these beings more vividly. Ethnographic and historical research are clear that spiritual practices change spiritual experience; increasingly, experimental work also documents changes as well.
...
These two hypothesis suggest two ways in which these communities update beliefs: a “top down” process in which others provide testimony, hearsay, teaching and, as a result, a means to interpret sensation; and a “bottom up” process in which subjects experience an altered sensory flow. The recognition of a difference between more interpretation-like teaching and more practice-like repetition might suggest hypotheses that could be distinguished in a predictive coding framework. One fruitful locus for this work may be the shared circuitry implicated in explicit expectation, social cognition, associative learning, placebo effects, and voice-hearing.
We suggest that attention to the socialization processes we have outlined may provide an important “level of explanation,” to use a framework suggested by Hughdahl and Somer. Such knowledge may complement and sharpen clinical, neuroscientific, and even molecular investigations. As we search for a deeper understanding of the nature of psychosis, of dissociative pathology, and of their potential mechanisms, it may be helpful to learn from the social communities in the general population in which people believe that spirits and beings communicate, and in which they learn how to hear them do so.
Seems like we’re still waiting on the fmri part, but we have a couple hints from Lifshitz... He’s only got some results from the scans of Christians to show so far.

66 notes
·
View notes
Text

By: SEGM
Published: Jun 21, 2023
In a new peer-reviewed commentary published in the Journal of Sex & Marital Therapy, author, Dr. Sarah Jorgensen, argues that the medical community has a professional responsibility to recognize detransitioners as survivors of iatrogenic harm and provide them with the comprehensive medical and supportive care that they deserve.
Jorgensen notes that proponents of gender-affirming medical interventions have attempted to downplay regret and detransition as vanishingly rare based on outdated studies that are not applicable to cohorts of adolescent trans identifying females presenting to gender clinics today. They refuse to admit that the gender-affirming model is failing some patients and have instead tried to reframe detransition as neutral or even positive outcome, proposing euphemisms such as “gender journey,” “identity exploration,” or “dynamic desires for gender-affirming medical interventions,” to replace the term “detransition."
“Rather than acknowledging the severity of the problem or that the medical community bears responsibility for the harm done to these young people, the message is that there have been no mistakes - the situation is dynamic.”
Instead of asking what went wrong, what was missed, and what could have been done differently to prevent inappropriate medical transitions, proponents of gender-affirming care repeatedly make appeals to authority, “every major medical association in the United States supports gender-affirming care for minors,” seemingly oblivious to the move away from American-style affirmation-on-demand in many European countries:
“A growing number of health authorities in countries that were once proponents of youth medical transition are now changing practice and prioritizing psychotherapy and treatment of co-occurring developmental, psychosocial, and mental health problems after their own systematic reviews found the evidence supporting gender-affirming medical interventions to be weak and uncertain.”
Many detransitioners report that they find it challenging to access clinicians who can advise them on what to expect when discontinuing hormones or who have the knowledge and training to manage enduring adverse effects of hormonal therapies and surgical complications. Jorgensen notes that there is currently no guidance on best practices for clinicians involved in the care of detransitioners:
“The World Professional Association for Transgender Health (WPATH) recently published its eighth Standards of Care document and chose not to include a chapter on detransition (Coleman et al., 2022). Likewise, the Endocrine Society’s Clinical Practice Guidelines for Gender-Dysphoria/Gender-Incongruence offers no advice on how to safely stop hormonal therapies (Hembree et al., 2017). The American Academy of Pediatrics failed to acknowledge the possibility of regret and detransition in their policy statement on care for children and adolescents with gender dysphoria (Rafferty et al., 2018).”
Jorgensen highlights multiple areas of uncertainty that will require open discussion and a commitment to clinical collaboration and research to resolve.
“We do not know what is driving the sharp rise in the number of young people being diagnosed or self-diagnosing with gender dysphoria (Cass, 2022; Kaltiala-Heino, Bergman, Tyolajarvi, & Frisen, 2018; Zucker, 2019). Likewise, we do not know why the case mix has rapidly shifted from predominantly young boys and middle-aged men to primarily adolescent females with complex mental health problems and neurodiversity (Aitken et al., 2015; Kaltiala-Heino et al., 2015; Zucker, 2019). The natural trajectory of transgender identification in this novel cohort is uncertain and we cannot predict who will be helped by gender-affirming medical interventions or who will be harmed. The long-term safety and effectiveness of these interventions is yet unknown (Hembree et al., 2017; Ludvigsson et al., 2023; NICE, 2020a, 2020b).”
Importantly, Jorgensen emphasizes that “we miss out on urgently needed data that could improve the outcomes of future patients by ignoring detransitioners.”
SEGM's Thoughts
The rate of medical detransition in the Western countries currently stands at 10-30% and is expected to grow. A number of the detransitioned patients will have permanent unwanted changes to the bodies and adverse long-term impacts on their physical and psychological health.
There is an urgent need to recognize detransition as a new phenomenon, and to structure the healthcare system in order to support this vulnerable patient population. However, due to the novelty of the detransition phenomenon, no diagnostic or procedure codes currently exist that either accurately capture the detransitioned patients' condition, or ensure provider reimbursement for the medical and mental health services that patients will need.
For this reason, it is urgent that the medical community initiate a conversation about what types of diagnostic and procedure codes are necessary to ensure the provision of high quality care to the individuals who detransition.
#SEGM#Society for Evidence Based Gender Medicine#detrans#detransition#iatrogenic harm#sex trait modification#medical malpractice#medical scandal#medical transition#medical corruption#transition regret#gender ideology#ideological corruption#ideological capture#queer theory#genderwang#religion is a mental illness
48 notes
·
View notes
Text


02.07.24 — day 38/366
my days have been eventful since i last updated :)
attended general orientation for our department
got my internship logbook
got persuaded into joining a uni-wide quiz bee (therefore ill be absent on my 2nd day at my rotation)
got my schedule for pre internship training/lectures — certifications for the hospitals im rotating isn't necessary compared to the first hospitals the first batch went to so i don't think i'll be having that
got a commission work :)
completed my laboratories, imaging and medical exam – got my medical certificate from the university physician as fit to work (also blood levels are great !!! as an anemic that's something to be proud of)
our study got revised again so from focusing on healthcare-associated pneumonia we shifted to ventilator-associated pneumonia which is great with how much literature's already been published about it
day 3 of my pre internship today anddd im just reading through the presentations, will be making my notes tomorrow or the weekend
got some documents notarized
submitted the clinical internship form for the hospital i'm assigned to
attended lectures ofc
studied on oxygen therapy protocols (but unfortunately wasn't the topic for the lec day it was supposed to be)
today i was able to complete my commission work, revisions of our intro and literature andd research design :)
#r-ene#r ene#studyblr#respiratory therapy major#respiratory therapy#study#collegeblr#uniblr#college student#uni#respiratory therapy student#respiratory#research#university student#uni life#university life#university#uni student#uni studyblr#university studyblr#collegeblog#college blog#college life#college#college studyblr#studies#studying#students#student#studyblr community
15 notes
·
View notes
Text
Satanic Panic
I saw a post about Satanic Panic, so I felt the need to write an overview of what actually happened for those who don’t know.
What is Satanic Panic?
Satanic Panic can be viewed as either part of the Memory Wars or as an entirely separate entity. If viewed as aligned with the False Memory movement, it might be seen as proof of False Memories and a near complete lack of the existence of ritual abuse. The other takes Satanic Panic as still harmful, but removes the blame from those claiming to have experienced it.
I believe that a crucial part of enabling healing is giving survivors the benefit of the doubt. People who are speaking out about abuse might be doing so for the first time, and are particularly vulnerable to disbelief even if they have told their story before. Talking about maltreatment takes a lot of courage, especially when a stigma already exists around the topic.
Fundie Satanism
That said, the Satanic Panic was weaponized by Christian groups expecting to gain power from it. Some genuinely believed Satanic Ritual Abuse was a primary concern, others knew it was only a face for the politics.
Fundamentalist groups wanted to have the kind of attention they were no longer getting, and the instatement of mandated reporter laws and influx of unsupervised children gave them a fighting cause. They saw that child abuse was becoming popular in media, and they used it as leverage to frighten well-meaning folks into their way of thinking.
Satanic was the word for non-Christian, and Christians were quick to disown anything that hinted at rot within their own organization. Christianity was still popular, and nobody wanted to believe they could be involved with a group that caused harm. So they took any religious abuse, and some non-religious abuses, and slapped Satanic on it.
Satanic Ritual Abuse
Ritual abuse refers to maltreatment that is both standardized and associated with symbols or ideologies. At the time, many kinds of organized (involving multiple perpetrators and victims) and/or coercive (intentionally manipulative) abuse were grouped under that name. Extreme abuse was also called ritual abuse, and we still don’t have a solid definition for that one.
Given that all ritual abuse would have been considered Satanic, fundies basically screwed over anyone who was abused in this specific way. Ritual abuse as we know it now did and does happen. An abuser doesn’t have to believe in their symbolism or ideology to misuse it, and many forms of religion and other structured beliefs can be applied to hurt and intimidate people.
RAMCOA
Ritual Abuse, Mind Control, and Organized Abuse are grouped together under a metric ton of buzz words. The survivors of this collection of abuses are left with research that is out of date, chock full of misinformation, and unable to communicate with people outside of the community.
I know the words are conspiratorial. I get that the books have fear-mongering content. I need people to understand that there is no better option, and pretending bad things don’t happen doesn’t make them go away.
Government Mind Control
Mind control is manipulation with intent. Coercion. Using psychology to get your way. Implanting false memories would be mind control. Again, it doesn’t sound good because cultural contexts have evolved over time and clinical language for this kind of abuse has not. Not all mind control is abusive at all. McDonald’s using targeted ads is mind control. But also training children like dogs is mind control.
There have been government-sponsored projects on mind control. There probably still are. Governments do sketchy things like that for military advancement and because they don’t face consequences, and there was a time where government employees admitted to it. Similar to McDonald’s and their hot coffee campaign, there were some strategic moves to look better to newcomers.
The government has sponsored lots of things they don’t want to acknowledge, and people are still suffering the effects. People in poverty, black and brown communities, and so on can probably agree that government is not synonymous with benevolent.
One of the things the government did was talk to criminal organizations. I don’t know if this is news to anyone, but it was a good way to get information and resources. There were wartime experiments on drugs and interrogation, and those were mind control.
Enough survivors agree about their experiences that it doesn’t seem worthwhile to dismiss them, so until there’s better information we would do well to try to understand them. You don’t have to agree full heartedly to sit with people in their own stories.
Cult Mind Control
I would describe a cult as any group that uses unhealthy practices as a defining feature of their cultural norms. Not everyone agrees on what is or isn’t a cult, and that mostly fine. This is the definition I’m using because it makes the most sense to me in context.
Cults members are not the only ones to use or receive mind control tactics, but the post I saw mentions cults this way. The specific technique is called Trauma Based Mind Control, which is the application of psychological responses to danger and overwhelm for the purposes of an abuser.
TBMC is the primary method for what the RAMCOA survivor community calls programming. Programming is the use of cues associated with PTSD triggers to achieve a desired response in a subject. When programming is done to a small child (under age 6-12, depending on the source), a common response is Dissociative Identity Disorder.
HC-DID
Abusers create alternate self-states within one body to react to the cues given. Depending on how knowledgeable the perpetrator(s) is/are, a child might have a very structured system of alters with little control allocated to them. These systems are designed by and for abusers to create long term obedient subjects.
Not every DID system is formed this way. Most are naturally developed with the induction of trauma in a child’s life. Some organic systems have complex structures anyway, but not for anyone but themselves. These systems are polyfragmented, or C-DID systems.
The level of control and organization found within a programmed system is almost always more than those found in organic systems. In the RAMCOA community, this is called HC-DID. The key difference isn’t true complexity, but the type of prerequisites to qualify.
Highly Complex DID isn’t particularly difficult to groom in a child, but it does require intent. Cult groups, as well as other high control groups, are quite capable of figuring it out by sheer cruelty and observation.
Why Does It Matter?
Making blanket statements about what abuse is and isn’t real doesn’t actually help anyone. While people prone to worry who didn’t experience RAMCOA might feel temporarily safer, it’s likely they’ll figure out they were lied to.
People who did experience it struggle with doubt and disbelief from others, and may have been told that nobody would care. This field is still considered taboo, and there are victims of torture and adjacent who are ashamed or afraid because of the state of the larger population.
I survived RAMCOA. My family and friends survived RAMCOA. Not all of my friends survived RAMCOA. Watch yourself.
#did osdd#dissociative identity disorder#traumagenic system#actuallydid#ramcoa#tw ramcoa#did system#polyfragmented system#osddid#satanic panic#satanic ritual abuse#child abuse#tw child abuse#sysblr#system stuff#ritual abuse
35 notes
·
View notes
Text
A new group of health professionals hopes to make abortion care more accessible to New Brunswickers.
The New Brunswick Abortion Care Network, whose 20 founding members are in nursing, obstetrics, family practice, pharmacy and health administration, launches Saturday — the 35th anniversary of the Supreme Court of Canada's Morgentaler decision, which decriminalized abortion.
The group aims to train more professionals and to raise awareness, said spokesperson Martha Paynter, a researcher and associate professor of nursing.
"The number one problem with access in New Brunswick is information," she said.
Despite provincial restrictions that limit Medicare coverage of surgical abortions to three hospitals, New Brunswick has had some "incredible advancements" in recent years, said Paynter, citing the introduction of self-referral in 2014 as an example.
No referral required, abortion pill covered
"So for almost 10 years you haven't needed to speak to a family doctor … [or] go to a walk in clinic, to be referred.
"You just call the [the two hospitals in Moncton or the one in Bathurst] and get an appointment. And people do not know that, so we want people to know that," said Paynter.
In 2017, New Brunswick also became the first province to offer the abortion pill Mifegymiso free of charge. So unlike other prescription medications, people don't have to put it through their insurance or pay for it out of pocket, she said. [...]
Continue Reading.
Tagging: @politicsofcanada
54 notes
·
View notes
Text

On Tuesday, Sept. 20, just in time for Bisexual Visibility Week, a diverse group of 15 bisexual and pansexual activists met with officials from the White House and the Department of Health and Human Services (HHS), including Melanie Fontes Rainer, the director of the Office of Civil Rights at HHS.
The 15 advocates comprised a wide cross-section of the bisexual community, including nonbinary, transgender, female, young, older, Black, Asian and Muslim advocates, people with disabilities and parents. We came from many walks of life: Academia, education, research, health care, advocacy, law, media and community activism. This isn’t unusual: Bisexual people comprise more than half of all LGBT people, totally approximately 12.5 million bisexual adults in the U.S. Strikingly, 15 percent of all GenZ adults — nearly 1 in 6 — identify as bisexual. People of color are more likely to identify as bisexual, as are cisegender women and transgender people in general.
It has been a painful six years since the Executive Branch last met with bisexual activists (you do the math.) Those meetings, like this one, were the product of tireless advocacy from a population with zero paid organizational staff and less than one percent of all philanthropic dollars earmarked for the LGBT community. It was these stats and others that we shared at HHS on Sept. 20.
Bisexual and pansexual people face specific disparities in mental and physical health, intimate partner violence and monkeypox prevention, treatment and care. Did you know, for example, that nearly half of bisexual women report having been raped? And did you know that federal reporting on monkeypox doesn’t disaggregate between gay and bisexual men and men who have sex with men, despite evidence that bisexual men are uniquely vulnerable to MPX and other infectious diseases.
Khafre Abif is a Black bisexual educator, father and person living with HIV. At the meeting with agency officials, Abif shared the story of how staff at his HIV-care clinic initially denied him the monkeypox vaccine, despite Abif being bisexual and thus in a population of special focus for the vaccine.
“This meeting has been a long time coming for the bi+ community,” said Abif. “I’m looking forward to a dialogue with federal officials about solving some of the health issues we face.”
In order to begin remedying these disparities and more, we presented the administration with a set of benchmarks, including the creation of a Federal Interagency Bisexual Liaison and a Federal Interagency Bisexual Working Group. Other benchmarks included training for HHS staff on bisexual disparities and remedies thereof, funding streams for bisexual-specific funding and interventions, and the disaggregation of data on specific health disparities.
Robyn Ochs is a pillar of bisexual and pansexual community organizing. At HHS, Ochs shared more about her specific expertise. “Research has made clear our health disparities and invisibility. It’s time for federal interventions to catch up with what we already know through research and lived experience.”
Frustrated by years of inaction by the federal government to release bisexual-specific data, target the bisexual and pansexual community with tailored interventions, or recognize the importance of bi+ health in general, we are cautiously excited by this opportunity to share critical data and remedies.
Heron Greenesmith is the Senior Research Analyst for LGBTQI+ Justice at Political Research Associates, and the co-founder of BiLaw and the Polyamory Legal Advocacy Coalition. Find Greenesmith on Twitter @herong.
#bisexuality#bisexual community#lgbtq community#lgbtq#bi#support bisexuality#lgbtq pride#pride#bi tumblr#bisexuality is valid#bisexual#bi pride#bisexual nation#bisexual pride#bisexual education#bisexual youth#support bisexual people#bisexual men#respect bisexual people#bisexual rights#bisexual activist#queer activist#bisexual women#bisexual people#Robyn ochs#white house#bisexual visibility#bi visibility
83 notes
·
View notes
Text
U.S. Rep. Dan Crenshaw, a Republican from Texas, on Wednesday hotly debated a witness about what he called the “elephant in the room” during a hearing about federal funds for pediatricians’ education. Whereas the House Committee on Energy and Commerce typically stays within the lanes of science, in this hearing it devolved into the right-wing culture war on transgender people, Democrats noted.
Crenshaw questioned Yale School of Medicine assistant professor Meredithe McNamara, a pediatrician with expertise in gender-affirming medicine, about his new proposal to remove federal funding from training hospitals that provide gender-affirming care to minors, such as puberty blockers, cross-sex hormones, or surgery.
The Children’s Hospitals Graduate Medical Education program funding is reauthorized every five years, and 58 hospitals receive it, training most pediatricians. Since 1999, it has been reauthorized five times.
“This is the issue of our time,” Crenshaw said, parroting anti-trans right-wing talking points.
“This is my bill, and what it does it withholds funding from these hospitals if they engage in what they call gender-affirmation therapy,” he said. “These physical changes to a child’s physiology, permanently disfiguring them through either puberty blockers or even surgical modifications.”
Gender-affirming surgeries are not performed on children.
He added, “It is indeed compassionate to stop kids from being permanently physically altered based on little to no evidence that it will improve their underlying mental condition.”
All major credible medical associations have endorsed gender-affirming care as science and evidence-based, proven essential medical treatment for people suffering from gender dysphoria.
“This is the hill we’re going to die on,” Crenshaw said.
“This is taxpayer money, and when 70% of taxpayers opposed these barbaric treatments on minors, then taxpayers should not fund it,” he asserted.
youtube
However, McNamara laid out the flaws with the GOP talking points and explained why gender-affirming care is not only proven but essential for the well-being of patients.
“As a physician with a commitment to patient care, I’m honored to be able to do more for them here than I can do in the office,” she said. “The past few years mark a rapidly shifting hostile political climate towards medical care for transgender people with, a harsh focus on youth care. That should be a private matter for families, patients, and providers is now being directed by legislators based on unsupported fears and misinformation. I understand that this care may be confusing to those who are not medical providers with expertise in treating this population or those who do not have a personal connection to a transgender person.”
She said that as a medical practitioner and a member of a vast community of experts in this type of care, she sees five categories of misinformation as responsible for the attacks on medical care for patients in distress: denial of the medical condition of gender dysphoria, false claims about standard practice, false claims about the evidence that backs care, false claims about the safety of treatments, and an attack on medical authority.
“I’m here to ensure that you have the facts to address this misinformation,” she said. “Gender dysphoria, the long-standing and significant distress that many transgender people have from the incongruence between their gender identity and the sex they have at birth, is real. It’s a recognized and serious medical condition. Transgender people of all ages exist. Their health care is based on established standards of care and clinical practice guidelines, which are themselves based on substantial medical research and evidence as well as decades of clinical practice. Based on these standards, youth and parents receive informed counseling about the risks and the benefits of specific treatments, and every major medical organization has endorsed this care.”
Miriam Grossman, a psychiatrist who advocated in the hearing for a conversion therapy approach, stated that most kids with gender dysphoria need counseling and nothing else. She admitted under friendly questioning by Crenshaw that his proposal appears to be a government overreach.
Grossman is part of the fringe group Do No Harm, made up of medical professionals and activists who stand in opposition to widely accepted care for kids with gender dysphoria.
“Medicine is unfortunately permeated with politics at this point,” Grossman said. “Now, ideally, we wouldn’t be stepping in. Who wants the government stepping in between doctors and parents and children? But when there’s something that is so wrong that is going on, then I think we have to.”
The American Medical Association this week came out strengthening its support for gender-affirming care for transgender youth.
McNamara tells The Advocate that giving voice to a witness who peddles in actual dangerous practices is detrimental to the conversation.
“One thing that I was deeply disheartened by was how [the hearing] heavily platforms somebody was who espouses conversion practices, which are dangerous and discredited,” she says. “And also quite simply ineffective.”
Conversion therapy is the discredited practice of attempting to change somebody’s sexual orientation, gender identity, or gender expression. It is a dangerous and harmful technique that has been outlawed for use on minors in states across the country and places around the world.
“Science shows over and over again, study by study, that youth who qualify for and desire gender-affirming care and have the support of their loved ones and their parents, they thrive,” McNamara says. “I am hopeful, seriously hopeful, that will no longer be a contentious issue soon.”
But Republicans appear to have picked their culture war issue, and they’re sticking to it.
“This is the hill we are going to die on. It is too important,” Crenshaw quipped.
#us politics#news#advocate#Rep. Dan Crenshaw#republicans#conservatives#gop platform#gop policy#gop#2023#House Committee on Energy and Commerce#Meredithe McNamara#gender affirming surgery#gender affirming care bans#Children’s Hospitals Graduate Medical Education program funding#gender dysphoria#Miriam Grossman#The American Medical Association#Do No Harm#lgbtqia+ rights#lgbtqia+#Youtube
13 notes
·
View notes
Text
Children at risk of depression are associated with body dissatisfaction.

A recent longitudinal study led by UCL researchers reveals a connection between body dissatisfaction at age 11 and an elevated risk of depression by age 14. The study, published in The Lancet Psychiatry and supported by Wellcome, focused on 13,135 participants from the Millennium Cohort Study—a nationally representative birth cohort study spanning those born between 2000 and 2002.
The findings indicate that concerns about body image significantly contribute to the link between body mass index (BMI) and depression in children, particularly in girls. High BMI at age seven is associated with increased depressive symptoms by age 14, along with greater body dissatisfaction at age 11. Notably, body dissatisfaction explains 43% of the association between BMI at age seven and subsequent depressive symptoms.
The study highlights that all three associations are more pronounced in girls compared to boys. Lead author Dr. Francesca Solmi emphasizes the need for a nuanced approach to childhood weight management, considering potential mental health impacts and avoiding stigmatization. The study did not explore other factors contributing to the association between high BMI and depressive symptoms but suggests biological (e.g., inflammation) or environmental (e.g., bullying) pathways could play a role.
Emma Blundell, the first author and a trainee clinical psychologist at UCL Psychology & Language Sciences, raises concerns about public health strategies that may inadvertently foster feelings of guilt or shame. While promoting healthy diet and exercise is essential, interventions should prioritize not increasing body dissatisfaction and harming children’s mental health.
The researchers propose that targeting body image concerns in early adolescence may prevent depression, especially in girls, and suggest exploring interventions like psychological approaches or media literacy training. They emphasize the importance of further research to effectively address body image concerns in young people. The collaborative study involved researchers from UCL Great Ormond Street Institute of Child Health, UCL Institute of Epidemiology & Health Care, MRC Unit for Lifelong Health & Ageing at UCL, and Imperial College London. The Millennium Cohort Study is based at the UCL Centre for Longitudinal Studies in the IOE, UCL’s Faculty of Education & Society.
Remember, if you need further guidance or support, don’t hesitate to reach out to your mental health professional or contact us for assistance.
#chiropractic#apdss#neckpain#neurostar#depressionhelp#back pain#pain management#medicine#mental health#health
3 notes
·
View notes